Abstract
Introduction
Sepsis, the leading cause of acute kidney injury (AKI), is associated with a high morbidity and mortality. Alkaline phosphatase (ALP) is an endogenous detoxifying enzyme. A recombinant human ALP compound, ilofotase alfa, showed no safety or tolerability concerns in a phase 2 trial. Renal function improvement over 28 days was significantly greater in the ilofotase alfa group. Moreover, a significant relative reduction in 28-day all-cause mortality of >40% was observed. A follow-up trial has been designed to confirm these findings.
Methods and analysis
This is a phase 3, global, multi-centre, randomised, double-blind, placebo-controlled, sequential design trial in which patients are randomly assigned to either placebo or 1.6 mg/kg ilofotase alfa. Randomisation is stratified by baseline modified Sequential Organ Failure Assessment (mSOFA) score and trial site. The primary objective is to confirm the survival benefit with ilofotase alfa by demonstrating a reduction in 28-day all-cause mortality in patients with sepsis-associated AKI requiring vasopressors. A maximum of 1400 patients will be enrolled at ∼120 sites in Europe, North America, Japan, Australia and New Zealand. Up to four interim analyses will take place. Based on predefined decision rules, the trial may be stopped early for futility or for effectiveness. In addition, patients with COVID-19 disease and patients with ‘moderate to severe’ chronic kidney disease are analysed as 2 separate cohorts of 100 patients each. An independent Data Monitoring Committee evaluates safety data at prespecified intervals throughout the trial.
Ethics and dissemination
The trial is approved by relevant institutional review boards/independent ethics committees and is conducted in accordance with the ethical principles of the Declaration of Helsinki, guidelines of Good Clinical Practice, Code of Federal Regulations and all other applicable regulations. Results of this study will determine the potential of ilofotase alfa to reduce mortality in critically ill patients with sepsis-associated AKI and will be published in a peer-reviewed scientific journal.
Trial registration number
EudraCT CT Number 2019-0046265-24. US IND Number 117 605 Pre-results. ClinicalTrials.gov number: NCT04411472.
Keywords: COVID-19, intensive & critical care, nephrology, acute renal failure
STRENGTHS AND LIMITATIONS OF THIS STUDY.
Apart from the primary endpoint, results of this trial may also illustrate the efficacy of ilofotase alfa on renal endpoints and other organ-specific clinical outcomes.
The trial was designed with input from or review by the US Food and Drug Administration, the European Medicines Agency, Japanese Pharmaceuticals and Medical Devices Agency and several national medicinal regulatory authorities in Europe, Australia and New Zealand.
The group sequential trial design allows for the results to be reported in case the trial is terminated prematurely for futility.
In the additional separate COVID-19 and ‘moderate to severe’ chronic kidney disease cohorts, therapeutic efficacy on clinical endpoints is likely underpowered to reach statistical significance.
Introduction
Sepsis, defined as a dysregulated host response to infection causing organ dysfunction, is the leading cause of death worldwide.1 2 Sepsis is also the leading cause of acute kidney injury (AKI).3–5 Patients with sepsis who develop AKI have a higher mortality, while an improved outcome is observed in patients with resolving AKI.6 7 Patients who survive a sepsis-associated AKI episode are at risk of developing chronic kidney disease (CKD), resulting in a high burden for both the patient and society.8–10 AKI is a multi-factorial condition with inflammatory, direct nephrotoxic and ischaemic insults combining with other pathogenic responses to rapidly cause dysfunction or failure of the kidney.11–14 Currently, there are no pharmacological interventions approved for the treatment of sepsis-associated AKI, and renal replacement therapy is the only supportive treatment option available for these patients.15
Alkaline phosphatase (ALP) is an endogenous homodimeric enzyme present in many cells and organs (eg, intestines, placenta, liver, bone, kidney and granulocytes) with detoxifying effects through dephosphorylation of endotoxins16 17 and other pro-inflammatory compounds such as ATP.18 19 Local ALP concentrations reflect the host defence against endotoxin in the kidney.20 During ischaemia, ALP levels are markedly depleted, which is associated with the development of AKI.21 Apart from local effects in the kidney, ALP may attenuate the innate immune response, as dephosphorylation of endotoxin abolishes its biological activity and the dephosphorylated endotoxin acts as a toll-like receptor 4 antagonist.22 In animal models of sepsis, ALP administration attenuates the inflammatory response and reduces mortality.23 24 There is increasing evidence that ALP plays a significant role in host defence and innate immunity, particularly against inflammatory reactions due to endotoxin release.25
Recombinant human ALP (recAP and ilofotase alfa)
Ilofotase alfa is a full-length human chimeric ALP produced by recombinant technology. It is encoded by a human intestinal ALP sequence (highest biological activity)26 wherein the sequence encoding the crown domain has been substituted with the corresponding human placental ALP sequence (longest half-life).26 Ilofotase alfa has a mass of approximately 105 kDa based on the amino acid sequence derived from the DNA sequence and approximately 130 kDa as a fully glycosylated molecule.
A large phase 2a/2b proof-of-concept and dose-finding trial (‘STOP-AKI’, n=301) was conducted with ilofotase alfa in SA-AKI after two small phase 2 trials27 28 with bovine ALP demonstrated attenuation of excretion of tubular injury markers and improvement in renal function. While the improvement in endogenous creatinine clearance over the first week in the STOP-AKI trial was not significantly greater in the treatment group compared with placebo, treatment with ilofotase alfa was associated with a more pronounced long-term improvement of kidney function and lower 28-day mortality.29
Trial objectives
The significant effect on 28-day mortality observed (as an exploratory endpoint) in STOP-AKI requires confirmation in a larger adequately powered, placebo-controlled, multi-centre trial. Therefore, the primary objective of REVIVAL (Recombinant human alkaline phosphatase SA-AKI survival trial) is to confirm or refute the study’s primary endpoint, a reduction in 28-day all-cause mortality, in patients with sepsis-associated AKI treated with 1.6 mg/kg ilofotase alfa.
Methods and analysis
Patients
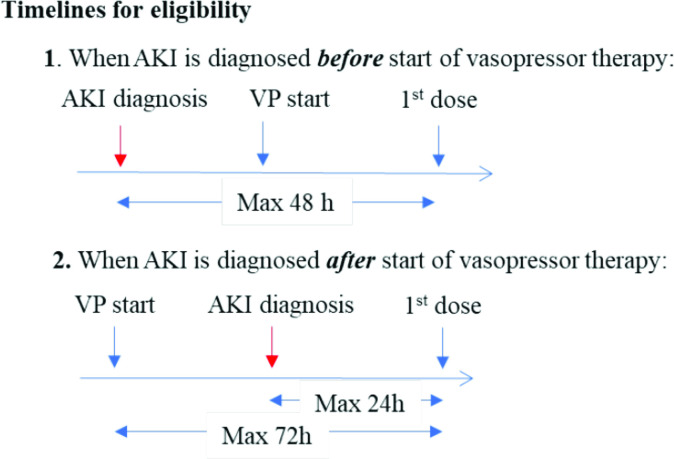
The target patient population is adult patients in the Intensive Care Unit (ICU) or intermediate care unit with sepsis requiring vasopressor support and recent onset AKI. Vasopressor support is defined as need for ≥0.1 µg/kg/min norepinephrine or equivalent for sepsis-induced hypotension for at least 1 hour despite adequate fluid resuscitation according to clinical judgement. AKI is defined by the KDIGO criteria.30 If the patients are receiving vasopressor support and develops AKI, the study drug infusion must start within 24 hours following the AKI diagnosis. If the patient presents with AKI, the time window is 48 hours.
There is no upper age limit for this trial. Consecutive patients will be systematically screened for AKI as soon as possible following the initiation of vasopressor treatment. Informed consent will be sought in all eligible patients with sepsis-associated AKI. Inclusion criteria are described in box 1, with the full eligibility criteria in online supplemental file 1. The first patient was enrolled on 2 November 2020. If the trial continues to recruit to target sample size, it is anticipated to run for 3 years.
Box 1. Short list of inclusion criteria.
Inclusion criteria
18 years or older.
In the ICU or intermediate care unit for clinical reasons.
-
Have sepsis requiring vasopressor therapy, that is:
-
Suspected or proven bacterial or viral infection.
and
On vasopressor therapy (≥0.1 µg/kg/min norepinephrine or equivalent) for sepsis-induced hypotension for at least 1 hour despite adequate fluid resuscitation according to clinical judgement.
-
-
Have AKI according to at least one of the below KDIGO criteria, a to d:
-
An absolute increase in serum or plasma creatinine (CR) by ≥0.3 mg/dL (≥26.5 µmol/L) within 48 hours.
or
-
A relative increase in CR to ≥1.5 times the pre-AKI reference CR value, which is known or presumed to have occurred within prior 7 days days.
or
-
A decrease in urinary output to<0.5 mL/kg/hour for a minimum of 6 hours hours following adequate fluid resuscitation.
or
If the patient does not have a known history of CKD and there is no pre-AKI reference CR value available from the past 12 months: a CR value ≥1.5 times the age/gender/race adjusted normal value (presented in online supplemental file 1), with the increase in CR presumed to have occurred within prior 7 days days.
-
Provision of signed and dated informed consent form in accordance with local regulations.
bmjopen-2022-065613supp001.pdf (160.6KB, pdf)
Trial oversight
A Trial Steering Committee (TSC) has been established by the Sponsor AM-Pharma to facilitate design of the trial, provide leadership and oversight of trial conduct in a blinded fashion, and make recommendations to the sponsor. Likewise, a Data Monitoring Committee (DMC), consisting of independent critical care and nephrology experts not otherwise involved in the trial and a statistician, has been established to evaluate safety data at regular intervals throughout the trial and notify the sponsor and the TSC in case of safety concerns that lead to a recommendation to stop or modify the trial. The DMC will also review the interim analyses reports for efficacy and notify the sponsor and the TSC in case a futility or success threshold is reached. The DMC and TSC both follow agreed charters.
Patient and public involvement statement
Reflecting the acute and unpredictable nature of sepsis-associated AKI there are no specific patient advocacy groups at present; closest are organisations that represent kidney diseases or sepsis in general and, although they are aware of our programme, they were not specifically consulted on the design of this study.
Trial design
This is a phase 3, multi-centre, randomised, double-blind, placebo-controlled, 2-arm parallel-group-sequential design pivotal trial in which patients with SA-AKI are randomly assigned in a 1:1 ratio to either ilofotase alfa or matching placebo. The intended ilofotase alfa dose is 1.6 mg/kg (1000 U) of patient body weight up to 120 kg (a fixed dose of 192 mg >120 kg) administered as a 1-hour infusion once daily for 3 consecutive days. The first infusion is to start as soon as feasible after randomisation.
There will be three distinct SA-AKI trial populations:
The main trial population: patients with sepsis-associated AKI and a pre-AKI reference estimated glomerular filtration rate (eGFR) ≥45 mL/min/1.73 m2 and no proven or suspected COVID-19 at time of randomisation.
A ‘moderate to severe’ CKD population: patients with sepsis-associated AKI a pre-AKI reference eGFR ≥25 mL/min/1.73 m2 and <45 mL/min/1.73 m2 and no proven or suspected COVID-19 at time of randomisation.
A COVID-19 population: patients with proven or suspected COVID-19 at time of randomisation with or without ‘moderate to severe’ CKD.
Participating sites that formally stated that they would commit to follow the internationally accepted standard of care guidelines for sepsis,31 and those for AKI30 32 were selected. If new versions of these guidelines are published during the trial, these will be adopted.
A minimum of approximately 450 and a maximum of 1400 patients in the main trial population are planned to be enrolled at approximately 120 sites predominantly across Europe, North America, Japan, Australia and New Zealand. Additionally, approximately 100 patients in the ‘moderate to severe’ CKD population and up to 100 patients in the COVID-19 population are planned to be enrolled to generate exploratory data on safety and effects of ilofotase alfa in these populations. The final number of patients enrolled will depend on the recommendations of the DMC based on the safety data reviews and interim analyses applying predefined decision rules to determine futility/success.
There will be a maximum of four interim analyses during the trial and enrolment continues during the interim analysis. The interim analyses will take place after approximately 400, 700, 850 and 1000 evaluable patients (ie, treated patients in the main trial population who have reached day 28). At the first interim analysis, the trial may be stopped for futility only. At subsequent interim analyses, the trial may be stopped for futility, or success (ie, early demonstration of superiority of ilofotase alfa over placebo on 28-day all-cause mortality). More details of the safety data reviews and the interim analyses are provided in the DMC charter and Statistical Analysis Plan (SAP), which were finalised before the first safety data review.
The trial includes a pre-treatment period, during which the patient is screened, baseline assessments are performed and the patient is randomised, a treatment period from day 1 to day 3, during which the patient receives a daily 1 hour continuous intravenous infusion of 50 mL trial drug (ilofotase alfa 1.6 mg/kg or placebo) and a follow-up period from day 4 to day 180, during which trial specific assessments and data collection are performed. The trial drug is provided on top of standard of care specified by the Surviving Sepsis Campaign guidelines and KDIGO guidelines. Safety is followed up until study day 28 (inclusive). All serious adverse events that occur after study day 28 will be reported to the sponsor or designee only if the Investigator considers them possibly, probably or definitely related to the trial drug. All deaths will be recorded up to study day 180. The trial design is presented in figure 1, the timelines for eligibility in figure 2, the trial flow for the individual patient in online supplemental figure 1 and the schedule of activities in online supplemental file 2.
Figure 1.
Trial design. Up to 1400 patients in the main trial population, up to approximately 100 patients in the ‘moderate to severe’ CKD population and up to approximately 100 patients in the COVID-19 population will be enrolled. There will be a maximum of four interim analyses, after approximately 400, 700, 850 and 1000 evaluable patients (ie, treated patients in the main trial population who have reached day 28), respectively. At the interim analyses, the trial may be stopped for futility or, from 700 patients onwards, for success (ie, pre-defined p value for primary endpoint met in the main trial population). Safety will also be assessed at regular intervals and the trial may be stopped or modified for safety concerns1. In the ‘moderate to severe’ CKD population and in the COVID-19 population, only safety will be assessed at the interim analyses. If the trial is not stopped at one of the interim analyses, a database snapshot will be executed after 1400 patients in the main trial population have reached day 28 to determine if the primary endpoint was met. No further analyses will be performed at this time. An interim lock will take place after all patients in the main trial population have reached day 90. Endpoints defined up to and including day 90 will be analysed and the results used to start the preparation of the CTR. The final DBL will take place after all patients have completed the trial (ie, all patients have completed day 180 or have withdrawn/are lost to follow-up prior to day 180). If patients in the ‘moderate to severe’ CKD population have not completed the trial at the time of the interim lock at day 90 and/or final DBL at day 180 for patients in the main trial population, a separate interim lock at day 90 and/or final DBL at day 180 may be performed for patients in the ‘moderate to severe’ CKD population in order for the analysis of data in the main trial population to commence. A separate interim lock may also be performed for the COVID-19 population. 1A full safety review at the time of the 850-patient interim analysis will only be performed if a futility or success threshold is reached. CKD, chronic kidney disease; CTR, clinical trial report; DBL, database lock; eGFR, estimated glomerular filtration rate; ICF, informed consent form; mSOFA, modified Sequential Organ Failure Assessment score (excluding Glasgow coma score); recAP, recombinant human alkaline phosphatase.
Figure 2.
Timelines for eligibility. To be eligible for the trial, patients must have both sepsis requiring vasopressor therapy and AKI. (1) When AKI is diagnosed before the start of vasopressor therapy, infusion of first dose of trial drug must start within 48 hours of AKI diagnosis. (2) When AKI is diagnosed after start of vasopressor therapy, infusion of first dose of trial drug must start within 24 hours of AKI diagnosis and no more than 72 hours from start of continuous vasopressor therapy for sepsis-induced hypotension. Start of AKI is defined as the timepoint where the patient for the first time meets any one of the inclusion criteria 4a–4d. Start of vasopressor therapy is defined as the start time of any dose of vasopressor in the first vasopressor treatment period that includes a continuous infusion of ≥0.1 µg/kg/min norepinephrine (or equivalent) for sepsis-induced hypotension for at least 1 hour in patients who have received adequate fluid resuscitation in accordance with clinical judgement and the recommendations of the surviving sepsis campaign guidelines. A minimum of 12 hours without any vasopressor is needed to consider start of vasopressor therapy as a new episode. AKI, acute kidney injury; recAP, recombinant human alkaline phosphatase; VP, vasopressor.
bmjopen-2022-065613supp002.pdf (68.2KB, pdf)
bmjopen-2022-065613supp003.pdf (235.4KB, pdf)
Statistical considerations
The primary efficacy endpoint is ‘28-day all-cause mortality’, defined as the probability to die (from any cause) up to and including day 28. The primary analysis will be based on a logistic regression model with site as a random effect, treatment as a fixed effect, mSOFA score as an ordered categorical variable and eGFR at baseline as the single continuous covariate.
The primary, secondary and tertiary/explorative endpoints are listed in table 1. Summary of statistical analyses and definitions of endpoints are described in online supplemental file 3.
Table 1.
Primary and secondary endpoints
| Objectives | Endpoints |
| Primary | |
| To demonstrate an effect of recAP on 28-day all-cause mortality. | 28-day all-cause mortality |
| Secondary | |
| To investigate the effect of recAP on long-term MAKE | MAKE 90: dead by day 90 or on RRT at Day 90 or ≥25% decline in eGFR on both day 28 and day 90 relative to the known or assumed pre-AKI reference level. Receiving RRT through day 28. Rehospitalisation up to and including day 90. |
| To investigate the effect of recAP on use of organ support, that is, MV, RRT, vasopressors or inotropes | Days alive and free of organ support through day 28, that is, days alive with no MV, RRT, vasopressors or inotropes (with death within 28 days counting as zero days) |
| To investigate the effect of recAP on LOS in ICU | Days alive and out of the ICU through day 28 (with death within 28 days counting as zero days) |
| To investigate the effect of recAP on 90-day all-cause mortality | Time to death through day 90 |
| Tertiary/exploratory | |
| To investigate the effect of recAP on 180-day all-cause mortality | Time to death through day 180 |
| To investigate the effect of recAP on organ function in the first week | Change in total and individual organ failure scores through day 7 (based on the mSOFA scores defined as the SOFA score without the GCS component) |
| To investigate the effect of recAP on short and long-term renal function | Days alive and free of RRT through day 28 (with death within 28 days counting as zero days) MAKE 28: dead by day 28 or on RRT at day 28 or ≥25% decline in eGFR on both day 7/ICU discharge (whichever comes first) |
| To investigate the effects of recAP on cardiovascular dysfunction | Days alive and free of vasopressor and inotropes through day 28 (with death within 28 days counting as zero days) |
| To investigate the effect of recAP on pulmonary function | Days alive and free of MV through day 28 (with death within 28 days counting as zero days) |
| To investigate the effect of recAP on LOS in hospital and rehospitalisation | Days alive and out of the hospital through day 90 (with death within 28 days counting as zero days) Incidence of at least one rehospitalisation at any hospital through day 90 |
| To investigate the effect of recAP on QoL | Change in index values, QALY and VAS score based on the EQ-5D-5L questionnaire at day 28, day 90 and day 180 |
| To investigate the effects of recAP on urinary excretion of purines | The urinary levels of purines (ATP, ADP, AMP, cAMP, and adenosine) through day 4 at selected sites |
| PK | |
| To investigate the PK properties of recAP | Population PK |
| Safety | |
| To investigate the safety and tolerability of recAP | Generation of anti-recAP antibodies on day 28 and day 90. Incidence of AEs and SAEs through day 28 |
The following objectives and endpoints are defined for the main trial population. The same objectives and endpoints will also be assessed and explored in the ‘moderate to severe’ CKD population and the COVID-19 population without any formal hypothesis testing.
cAMP, cyclic AMP; CKD, chronic kidney disease; eGFR, estimated glomerular filtration rate; EQ-5D-5L, EuroQoL-5-Dimention-5 Levels; GCS, Glasgow Coma Scale; ICU, Intensive Care Unit; LOS, length of stay; MAKE, major adverse kidney events; mSOFA, modified Sequential Organ Failure Assessment; MV, mechanical ventilation; PK, pharmacokinetics; QALY, quality-adjusted life years; QoL, quality of life; recAP, recombinant human alkaline phosphatase; RRT, renal replacement therapy; SAEs, serious adverse events; VAS, visual analogue scale.
bmjopen-2022-065613supp004.pdf (143.1KB, pdf)
Statistical analyses will be performed by a sponsor-designated statistician, blinded to treatment allocation. Further details of the statistical analyses are described in the SAP, which has been finalised prior to the first safety review of the trial database (online supplemental file 3). A separate DMC SAP describes the analyses to be performed for the safety data reviews and interim analyses. All statistical analyses of efficacy endpoints will be performed on the modified intention-to-treat analysis sets, defined as all patients in the population who are randomly assigned to trial drug and for whom administration of trial drug was started. All statistical analyses of safety endpoints will be performed on the safety analysis sets. Of note, after acceptance of the manuscript, an amended SAP was written and approved prior to the first interim-analysis. This amendmentment, which were not subjected to peer-review, is depicted in online supplemental file 4.
bmjopen-2022-065613supp005.pdf (154.3KB, pdf)
Analysis of data from each population will also be performed and presented separately. Formal analyses (including interim analyses), hypothesis testing and descriptive analyses will be performed on data from the main trial population, whereas descriptive statistics (including an estimate of the treatment effect, two-sided 95% CIs and one-sided p value) will be presented for the combined population, ‘moderate to severe’ CKD population and the COVID-19 population.
The Lan-DeMets approximation of the O’Brien-Fleming alpha spending function was used to determine the critical values for declaring success at interim and final analyses. As safety is evaluated by the DMC on a regular basis throughout the trial and the risk of increased mortality, that is, inferiority of ilofotase alfa compared with placebo, is controlled by the futility analyses, the test for therapeutic efficacy is a superiority test using a one-sided significance level of 0.025. Online supplemental file 3 shows the nominal one-sided significance levels at interim and final analyses for declaring success if data from approximately 700, 850, 1000 and 1400 patients in the main trial population will be available. This trial will be considered a success, and the intervention effective, if the one-sided p value from the primary efficacy analysis model for the treatment term is lower than the respective nominal one-sided significance level. Should the trial be stopped for early success at an interim analysis, then the analysis of the secondary endpoints within the sequential testing will proceed using the nominal one-sided significance level as allocated to the primary endpoint at the time of the analysis. The predictive probability of success at the main trial population’s maximum sample size of 1400 patients will be used to determine if the trial should stop early for futility. Futility stopping recommendation in this trial is considered to be non-binding.
For this trial design, the operating characteristics (type I error probability and power) are derived via simulations for a maximum sample size of 1400 patients in the main trial population, and the group sequential design. Twenty-eight day all-cause mortality probability in the placebo treatment group was set at 35% across all scenarios, which was the observed 28-day mortality in the subgroup of patients with a study baseline eGFR <60 mL/min in STOP-AKI. In case of an 8% absolute survival benefit of the treatment, this trial has 85.6% power and the mean sample size is expected to be 1010 patients due to the probability of early success or futility.
Safety endpoints
Safety parameters will be evaluated on the Safety Set. Incidence of (Serious) Adverse Events and Treatment Emergent Adverse Events categorised by MedDRA System Organ Class and Preferred Term will be summarised by trial drug group. Adverse event seriousness, severity, relationship to trial drug and whether leading to discontinuation of trial drug will also be recorded. Anti-drug antibodies results will be listed, including the results of the screening test and, if needed, the results of the confirmatory test and titre determination per dose group.
Population PK
A population pharmacokinetics (PK) analysis of plasma concentration-time data will be performed using non-linear mixed-effects modelling. Data from this trial may be combined with data from the phase 1 PK, safety and tolerability trial in Caucasian healthy adult volunteers,33 an additional PK, safety and tolerability trial performed in Japan in Japanese healthy adult volunteers, and the phase 2 trial (STOP-AKI) in patients with SA-AKI29 and included in an integrated PK analysis. The structural model will contain clearance and volume of distribution as fixed-effect parameters. The inter-patient variability in the parameter estimates and the random residual error in the data will be estimated with an appropriate model. Available patient characteristics will be tested as potential covariates affecting PK parameters. Details of the analysis will be given in a population PK analysis plan.
Sensitivity analyses and secondary endpoints
Sensitivity analyses, based on baseline disease severity score and time from fulfilling inclusion criteria to time of treatment, will be performed on the primary endpoint. In addition, day 28 all-cause mortality obtained based on Kaplan-Meier curves for time to death up to day 28 will be compiled separately for the mSOFA categories (≤9 vs >9) and combined. Finally, a tipping point analysis in which all ilofotase alfa patients with missing data on survival status on day 28 will be considered as being dead, while all placebo patients with missing data will be considered alive, and all possible combinations of missing data between these two extremes will be considered.
The most relevant secondary endpoint is Major Adverse Kidney Events (MAKE) at day 90, defined as dead, or on renal replacement therapy at day 90, or ≥25% decline of eGFR on day 28 and day 90 relative to the pre-AKI reference level. An additional MAKE90a endpoint was added (prior to unblinding) existing of: death up to and including day 90, >25% decline of eGFR at day 90 relative to pre-AKI reference level, receiving RRT at day 90 or receiving RRT through day 28, rehospitalisation up to and including day 90, and an exploratory analysis to evaluate the influence of pre-existent renal function on the therapeutic efficacy of ilofotase alfa. Additional secondary endpoints are: days alive and free of organ support through day 28 (with death within 28 days counting as zero days), days alive and out of the ICU through day 28 (with death within 28 days counting as zero days) and time to death through day 90.
Tertiary/explorative endpoints are: time to death through day 180, change in total and individual organ failure scores through day 7 and the effect of recAP on short-term and long-term renal function, cardiovascular function, pulmonary function, hospital length of stay and quality of life.
Ethics and dissemination
This trial will be conducted in accordance with the protocol and consensus ethical principles derived from international guidelines, including the Declaration of Helsinki and Council for International Organisations of Medical Sciences’ International Ethical Guidelines; applicable International Conference on Harmonisation GCP Guidelines; and applicable laws and regulations. The protocol, substantial protocol amendments, informed consent form (ICF), investigator’s brochure (IB) and other relevant documents (eg, any other written information regarding this trial to be provided to the patient or the patient’s legal representative) will be submitted to an IRB/IEC by the investigator and reviewed and approved by the IRB/IEC prior to being used in the trial. The Standard Protocol Items Recommendations for Interventional Trials checklist is added in online supplemental file 5.
bmjopen-2022-065613supp006.pdf (90.9KB, pdf)
By the very nature of the trial, it is anticipated that many eligible patients will not be able to give fully informed consent themselves due to various reasons, including disease severity, sedation or unconscious state. In this situation, the patient’s legal representative may provide written consent, as approved by the institutional-specific guidelines and legislation in the respective country. Informed consent may be obtained from an independent consulting physician or based on an emergency study protocol by the investigator in countries where regulation and institution guidelines permit, and the consent procedure has been approved by the institutional review board (IRB)/independent ethics committee (IEC) or national authorities, as applicable in specific countries. In cases where the initial informed consent is obtained from a legal representative, an independent consulting physician, or by the investigator, the patient is asked to give written informed consent with the most current version of the ICF(s) as soon as they are able. The master informed consent form is attached as a online supplemental file 6.
bmjopen-2022-065613supp007.pdf (270.5KB, pdf)
Patients will be assigned a unique patient identification number via the Interactive Response Technology (IRT) system. Any patient records or datasets that are transferred to the sponsor will contain this identifier only; patient names and any information which would make the patient identifiable will not be transferred. All laboratory specimens, evaluation forms, reports and other records will be identified in a manner designed to maintain patient confidentiality.
Irrespective of whether the trial is completed or prematurely terminated, the sponsor will ensure that the trial results will be posted on publicly available clinical trial registries in accordance with their requirements. In addition, results will be presented at international congresses and published in peer-reviewed journals.
In addition to answering the question, whether ilofotase alfa leads to a reduction in 28-day all-cause mortality, the study will provide important information on the effect of ilofotase alfa on MAKE and other clinical outcomes, and significantly expand the safety profile of the drug. Moreover, compared with STOP-AKI where follow-up was limited to 90 days, follow-up of patients for a period of 180 days allows for assessment of potential disease-modifying effects of ilofotase alfa on kidney function and investigation of the long-term effect on mortality and other clinically relevant, patient-centred and health-economic outcomes. Finally, biomarker analysis may improve the understanding of the mechanism of action of ilofotase alfa.
Supplementary Material
Footnotes
Contributors: PP and ALK co-drafted the manuscript, participated in the trial protocol design and are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. DCA, JA, RB, EvdB, JB, MB, KB, JC, CJD, RF, MJ, BF, KD, JAK, P-FL, KL, RLM, PTM, MO, VP, SR, PY and AZ all participated in the trial protocol design (as members of the trial steering committee (TSC), reviewed and edited the manuscript. All authors read and approved the final version of the manuscript prior to submission.
Funding: This work was supported by AM-Pharma.
Competing interests: PP received advisory board consultancy and travel reimbursements from AM-Pharma. DCA and CJD serve as advisory board consultants for AM-Pharma. JA, EvdB and JB are employees of AM-Pharma. RB, MB, KD, BF, JAK, P-FL, VP and PY received advisory board consultancy reimbursements from AM Pharma. KB worked as an employee of Berry Consultants KB and acted as a consultant to numerous pharmaceutical and device companies. KB is currently an employee of and holds stock in AstraZeneca. JC, ALK and SR are consultants to AM-Pharma. RF received advisory board consultancy reimbursements from AM Pharma and additional consulting reimbursements from BioMerieux, Baxter, Pfizer, MSD, Gilead, Shionogi, Grifols and Beckton Dickinson unrelated to the current study. MJ received advisory board consultancy reimbursements from AM Pharma, additional consulting reimbursement from Baxter and Gilead and grant support from Fresenius and Baxter, unrelated to the current study. KL received advisory board consultancy reimbursements from AM-Pharma, owns stock in Amgen and consultant for Biomerieux, Neumora, Seastar and BOA Medical. RLM received advisory board consultancy reimbursements from AM Pharma and additional consulting reimbursement from BioMerieux, Baxter, Nova Biomed, Abiomed, GE Healthcare, Medtronic, Sanofi and Mallinckrodt, unrelated to the current study. PTM received Trial Steering Committee consultancy payments from AM-Pharma. Other consultancy payments: FAST Biomedical, Novartis, Renibus Therapeutics. MO received speaker honoraria from Fresenius Medical Care, Biomerieux, Baxter and Gilead, and research funding from Fresenius Medical Care, Biomerieux, Baxter and LaJolla Pharma and advisory board consultancy reimbursements from AM-Pharma. AZ received advisory board consultancy reimbursements from AM-Pharma. AZ has received consulting and/or lecture fees from Astute Medical/BioMerieux, Fresenius, Paion, Guard Therapeutics, and Baxter, unrelated to the current study. AZ has received grant support from Astute Medical/BioMerieux, Fresenius and Baxter, unrelated to the current study.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Provenance and peer review: Not commissioned; externally peer reviewed.
© Author(s) (or their employer(s)) 2023. Re-use permitted under CC BY-NC. No commercial re-use. See rights and permissions. Published by BMJ.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Ethics statements
Patient consent for publication
Not applicable.
References
- 1.Fleischmann C, Scherag A, Adhikari NKJ, et al. Assessment of global incidence and mortality of hospital-treated sepsis. Current estimates and limitations. Am J Respir Crit Care Med 2016;193:259–72. 10.1164/rccm.201504-0781OC [DOI] [PubMed] [Google Scholar]
- 2.Rudd KE, Johnson SC, Agesa KM, et al. Global, regional, and national sepsis incidence and mortality, 1990-2017: analysis for the global burden of disease study. Lancet 2020;395:200–11. 10.1016/S0140-6736(19)32989-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Angus DC, Linde-Zwirble WT, Lidicker J, et al. Epidemiology of severe sepsis in the United States: analysis of incidence, outcome, and associated costs of care. Crit Care Med 2001;29:1303–10. 10.1097/00003246-200107000-00002 [DOI] [PubMed] [Google Scholar]
- 4.Vincent J-L, Sakr Y, Sprung CL, et al. Sepsis in European intensive care units: results of the soap study. Crit Care Med 2006;34:344–53. 10.1097/01.ccm.0000194725.48928.3a [DOI] [PubMed] [Google Scholar]
- 5.Kellum JA, Prowle JR. Paradigms of acute kidney injury in the intensive care setting. Nat Rev Nephrol 2018;14:217–30. 10.1038/nrneph.2017.184 [DOI] [PubMed] [Google Scholar]
- 6.Peters E, Antonelli M, Wittebole X, et al. A worldwide multicentre evaluation of the influence of deterioration or improvement of acute kidney injury on clinical outcome in critically ill patients with and without sepsis at ICU admission: results from the intensive care over nations audit. Crit Care 2018;22:188. 10.1186/s13054-018-2112-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Matejovic M, Chvojka J, Radej J, et al. Sepsis and acute kidney injury are bidirectional. Contrib Nephrol 2011;174:78–88. 10.1159/000329239 [DOI] [PubMed] [Google Scholar]
- 8.Oppert M, Engel C, Brunkhorst F-M, et al. Acute renal failure in patients with severe sepsis and septic shock -- a significant independent risk factor for mortality: results from the German prevalence study. Nephrol Dial Transplant 2008;23:904–9. 10.1093/ndt/gfm610 [DOI] [PubMed] [Google Scholar]
- 9.Chawla LS, Amdur RL, Amodeo S, et al. The severity of acute kidney injury predicts progression to chronic kidney disease. Kidney Int 2011;79:1361–9. 10.1038/ki.2011.42 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Vaara ST, Korhonen A-M, Kaukonen K-M, et al. Fluid overload is associated with an increased risk for 90-day mortality in critically ill patients with renal replacement therapy: data from the prospective FINNAKI study. Crit Care 2012;16:R197. 10.1186/cc11682 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bonventre JV, Yang L. Cellular pathophysiology of ischemic acute kidney injury. J Clin Invest 2011;121:4210–21. 10.1172/JCI45161 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wen X, Peng Z, Kellum JA. Pathogenesis of acute kidney injury: effects of remote tissue damage on the kidney. Contrib Nephrol 2011;174:129–37. 10.1159/000329382 [DOI] [PubMed] [Google Scholar]
- 13.Gomez H, Ince C, De Backer D, et al. A unified theory of sepsis-induced acute kidney injury: inflammation, microcirculatory dysfunction, bioenergetics, and the tubular cell adaptation to injury. Shock 2014;41:3–11. 10.1097/SHK.0000000000000052 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Verma SK, Molitoris BA. Renal endothelial injury and microvascular dysfunction in acute kidney injury. Semin Nephrol 2015;35:96–107. 10.1016/j.semnephrol.2015.01.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bagshaw SM, Lapinsky S, Dial S, et al. Acute kidney injury in septic shock: clinical outcomes and impact of duration of hypotension prior to initiation of antimicrobial therapy. Intensive Care Med 2009;35:871–81. 10.1007/s00134-008-1367-2 [DOI] [PubMed] [Google Scholar]
- 16.Bentala H, Verweij WR, Huizinga-Van der Vlag A, et al. Removal of phosphate from lipid A as a strategy to detoxify lipopolysaccharide. Shock 2002;18:561–6. 10.1097/00024382-200212000-00013 [DOI] [PubMed] [Google Scholar]
- 17.Koyama I, Matsunaga T, Harada T, et al. Alkaline phosphatases reduce toxicity of lipopolysaccharides in vivo and in vitro through dephosphorylation. Clin Biochem 2002;35:455–61. 10.1016/s0009-9120(02)00330-2 [DOI] [PubMed] [Google Scholar]
- 18.Picher M, Burch LH, Hirsh AJ, et al. Ecto 5’-nucleotidase and nonspecific alkaline phosphatase. two AMP-hydrolyzing ectoenzymes with distinct roles in human airways. J Biol Chem 2003;278:13468–79. 10.1074/jbc.M300569200 [DOI] [PubMed] [Google Scholar]
- 19.Peters E, Geraci S, Heemskerk S, et al. Alkaline phosphatase protects against renal inflammation through dephosphorylation of lipopolysaccharide and adenosine triphosphate. Br J Pharmacol 2015;172:4932–45. 10.1111/bph.13261 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kapojos JJ, Poelstra K, Borghuis T, et al. Induction of glomerular alkaline phosphatase after challenge with lipopolysaccharide. Int J Exp Pathol 2003;84:135–44. 10.1046/j.1365-2613.2003.00345.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Khundmiri SJ, Asghar M, Khan F, et al. Effect of reversible and irreversible ischemia on marker enzymes of BBM from renal cortical Pt subpopulations. Am J Physiol 1997;273:F849–56. 10.1152/ajprenal.1997.273.6.F849 [DOI] [PubMed] [Google Scholar]
- 22.Wy CA, Goto M, Young RI, et al. Prophylactic treatment of endotoxic shock with monophosphoryl lipid A in newborn rats. Biol Neonate 2000;77:191–5. 10.1159/000014215 [DOI] [PubMed] [Google Scholar]
- 23.Beumer C, Wulferink M, Raaben W, et al. Calf intestinal alkaline phosphatase, a novel therapeutic drug for lipopolysaccharide (LPS) -mediated diseases, attenuates LPS toxicity in mice and piglets. J Pharmacol Exp Ther 2003;307:737–44. 10.1124/jpet.103.056606 [DOI] [PubMed] [Google Scholar]
- 24.Su F, Brands R, Wang Z, et al. Beneficial effects of alkaline phosphatase in septic shock. Crit Care Med 2006;34:2182–7. 10.1097/01.CCM.0000229887.70579.29 [DOI] [PubMed] [Google Scholar]
- 25.Verweij WR, Bentala H, Huizinga-van der Vlag A, et al. Protection against an Escherichia coli-induced sepsis by alkaline phosphatase in mice. Shock 2004;22:174–9. 10.1097/01.shk.0000132485.05049.8a [DOI] [PubMed] [Google Scholar]
- 26.Kiffer-Moreira T, Sheen CR, Gasque KC da S, et al. Catalytic signature of a heat-stable, chimeric human alkaline phosphatase with therapeutic potential. PLoS One 2014;9:e89374. 10.1371/journal.pone.0089374 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Heemskerk S, Masereeuw R, Moesker O, et al. Alkaline phosphatase treatment improves renal function in severe sepsis or septic shock patients. Crit Care Med 2009;37:417–23. 10.1097/CCM.0b013e31819598af [DOI] [PubMed] [Google Scholar]
- 28.Pickkers P, Heemskerk S, Schouten J, et al. Alkaline phosphatase for treatment of sepsis-induced acute kidney injury: a prospective randomized double-blind placebo-controlled trial. Crit Care 2012;16:R14. 10.1186/cc11159 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Pickkers P, Mehta RL, Murray PT, et al. Effect of human recombinant alkaline phosphatase on 7-day creatinine clearance in patients with sepsis-associated acute kidney injury: a randomized clinical trial. JAMA 2018;320:1998–2009. 10.1001/jama.2018.14283 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.KDIGO . KDIGO clinical practice guideline for acute kidney injury. Kidney Int Suppl (2011) 2012;2:1–138. [Google Scholar]
- 31.Singer M, Deutschman CS, Seymour CW, et al. The third International consensus definitions for sepsis and septic shock (sepsis-3). JAMA 2016;315:801–10. 10.1001/jama.2016.0287 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kellum JA, Lameire N, KDIGO AKI Guideline Work Group . Diagnosis, evaluation, and management of acute kidney injury: a KDIGO summary (part 1). Crit Care 2013;17:204. 10.1186/cc11454 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Peters E, Heuberger JAAC, Tiessen R, et al. Pharmacokinetic modeling and dose selection in a randomized, double-blind, placebo-controlled trial of a human recombinant alkaline phosphatase in healthy volunteers. Clin Pharmacokinet 2016;55:1227–37. 10.1007/s40262-016-0399-y [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2022-065613supp001.pdf (160.6KB, pdf)
bmjopen-2022-065613supp002.pdf (68.2KB, pdf)
bmjopen-2022-065613supp003.pdf (235.4KB, pdf)
bmjopen-2022-065613supp004.pdf (143.1KB, pdf)
bmjopen-2022-065613supp005.pdf (154.3KB, pdf)
bmjopen-2022-065613supp006.pdf (90.9KB, pdf)
bmjopen-2022-065613supp007.pdf (270.5KB, pdf)