Abstract
Objectives
To identify caregiver and children factors associated with caregiver burden on primary caregivers of children with cerebral palsy (CP).
Design
Systematic review
Data sources
Seven electronic databases, including PubMed, Cochrane Library, Scopus, PsycINFO, Web of Science, CINAHL and Embase, were systematically searched up to 1 February 2023.
Eligibility criteria
Original observational studies reporting caregiver burden and related factors among caregivers of children with CP.
Data abstraction and synthesis
Two reviewers independently screened results and assessed the quality of studies. Title, abstract, full-text screening and data abstraction were done independently by two reviewers. Risk of bias was assessed using the JBI Critical Appraisal Checklist for Analytical Cross-Sectional Studies. The quality of evidence for factors was rated using the Grading of Recommendations Assessment, Development and Evaluation (GRADE) approach.
Results
16 articles were included in the review. All studies were cross-sectional and examined caregiver-reported burden measures. The Zarit Burden Interview was the most commonly used questionnaire. Depression of caregiver and severity of illness in children with CP were moderate quality of evidence for factors contributing to caregiver burden.
Conclusions
Higher caregiver burden is associated with more depressive feelings and worse life quality of the caregiver, and with more severe physical disability of the children. Future studies should focus on high-quality longitudinal research and appropriate assistance to reduce caregiver burden and improve the quality of caregiving for children with CP.
PROSPERO registration number
CRD42021268284.
Keywords: developmental neurology & neurodisability, primary care, rehabilitation medicine
STRENGTHS AND LIMITATIONS OF THIS STUDY.
This review was the first one to provide a comprehensive overview of caregiver burden of children with cerebral palsy.
The protocol was registered on the PROSPERO database (CRD42021268284) and was carried out based on the Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines.
The quality of evidence for factors was judged by the Grading of Recommendations Assessment, Development and Evaluation approach.
Many survey factors of the total care burden were scattered and failed to provide reliable evidence.
The uneven quality of the included studies resulted in many methodological limitations.
Introduction
With the development of perinatal medicine and obstetric technology, the birth prevalence of cerebral palsy in high-income countries had declined to 1.6 per 1000 live births, while the prevalence in low-income and middle-income countries was as high as 3.4 per 1000 live births.1 Cerebral palsy (CP) is defined as a group of disorders of the development of movement and posture, causing activity limitation, that are attributed to non-progressive disturbances occurred in the developing fetal or infant brain. The motor disorders of CP are often accompanied by disturbances of sensation, cognition, communication, perception, behaviour and by a seizure disorder.2 CP is the most common paediatric disability, seriously affecting the children’s self-care ability and social activities.3 4 Thus, children with CP often require lifetime extensive care and rehabilitation training, which will bring heavy psychological, physical and economic burden to their families.5 6
Parents, as the primary caregivers of children with disabilities, bear the arduous caregiving burden. Not only do they have to help the children’s daily activities, but they also need to pay close attention to their changing health conditions, which directly leads to changes in the caregivers’ lifestyle and a decline in their quality of life.7 8 Caregiver burden has been defined as a multidimensional response to physical, emotional, psychological and financial stressors that are associated with caregiving experience.9 Studies have shown that a high level of caregiving burden for children with CP negatively affects the mental and physical health, family functions and social interactions of caregivers, resulting in low quality of care and unmet patient needs.10–13 Paying attention to the burden of caregivers is of great significance.
Relevant factors that affect caregiver burden should be studied in order to propose interventions to support caregivers. In the last decade, there has been an increasing number of studies on the care burden for children with CP, but a comprehensive review of caregiver factors and patient factors influencing caregiver burden is lacking. Therefore, the objective of this study was to systematically review published literature to identify caregiver and patient factors of caregiver burden among primary caregivers of children with CP.
Methods
This systematic review was checked through the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines (online supplemental appendix 1).
bmjopen-2022-065215supp001.pdf (64.1KB, pdf)
Search strategy
The electronic databases PubMed, Cochrane Library, Scopus, PsycINFO, Web of Science, CINAHL and Embase were systematically searched from inception to 1 February 2023. The search string contained four groups of combinations of medical subject headings and text words: Caregiver (MeSH term), care*, parents or mother; Caregiver burden (MeSH term), stress, strain or burnout; Cerebral palsy (MeSH term), CP, disability* or neurodev* disorder*; Children (MeSH term), child* or paediatr* (online supplemental appendix 2). In addition, we also searched for grey literature using the first 500 hits from Google Scholar and Open Grey. References for relevant publications were checked to make sure that no relevant papers had been missed.
bmjopen-2022-065215supp002.pdf (129.4KB, pdf)
Inclusion and exclusion criteria
Original observational studies reporting burden and related factors of caregivers of children with CP were taken as the primary focus of the research. Study participants need to be primary caregivers (over 18 years old) of children (0–18 years old) with CP. Burden had to be assessed with a total caregiver burden construct. Full-text articles published in English or with an English translation in peer-reviewed journals were included. Studies where caregivers of children with different diagnoses and children with adults are grouped together were excluded, unless results were reported separately for caregivers of children with CP. Intervention studies, reviews, non-original research papers and qualitative research studies were not eligible for this review.
Data extraction and quality assessment
The titles/abstracts of citations retrieved using the search strategy were independently assessed by two reviewers. The full-text articles of potentially relevant studies were then independently screened by two reviewers, and any discrepancies were resolved through discussion. The number of studies excluded during each screening phase and the reasons for full-text exclusion will be described in a PRISMA flow diagram. A pre-specified form will be used for the extraction of the data from the included studies. This procedure will be completed by one reviewer, and verified by a second reviewer, with any disagreements being resolved through discussion with a third-party reviewer. We extracted the following data from each included study independently by two researchers: first authors, year of publication, sample size, study design, relevant participant demographics, key predictor and outcome variables, self-administered tools used for measurement, results and associations.
Risk of bias was assessed using the JBI Critical Appraisal Checklist for Analytical Cross-Sectional Studies (online supplemental appendix 3) by the two researchers independently. The checklists include eight questions to evaluate the overall quality of the studies from the research object, disease, measurement of influencing factors and confounding factors, data analysis and so on. The choices of answers were ‘yes’, ‘no’, ‘unclear’ or ‘not applicable’. The overall appraisal of ‘include’, ‘exclude’ or ‘seek further information’ were presented in the last section of the checklist.
Data synthesis
Due to the diversity of outcome measures and factors included in the study, a meta-analysis was not possible. Bivariate associations were described in terms of different statistical analysis. Multivariate associations were described as standardised or unstandardised coefficients (β or b). In studies that applied a logistic regression, the OR was presented. Factors were grouped into caregiver and children characteristics subsequently thematically categorised.
Quality of evidence
We assessed the quality of evidence for each factor measured in at least three studies using the Grading of Recommendations Assessment, Development and Evaluation (GRADE) approach (online supplemental appendix 4). GRADE has four levels of evidence: very low, low, moderate and high. Evidence from observational data starts at low quality. For each of study limitation in risk of bias, imprecision, inconsistency, indirectness and publication bias, researchers have the option of rating down their level of certainty in evidence. Quality of evidence also can be rated up for ‘large effect’ or ‘dose effect’.
Patient and public involvement
Patients or public were not involved in the conduct of this systematic review.
Results
Search and screening
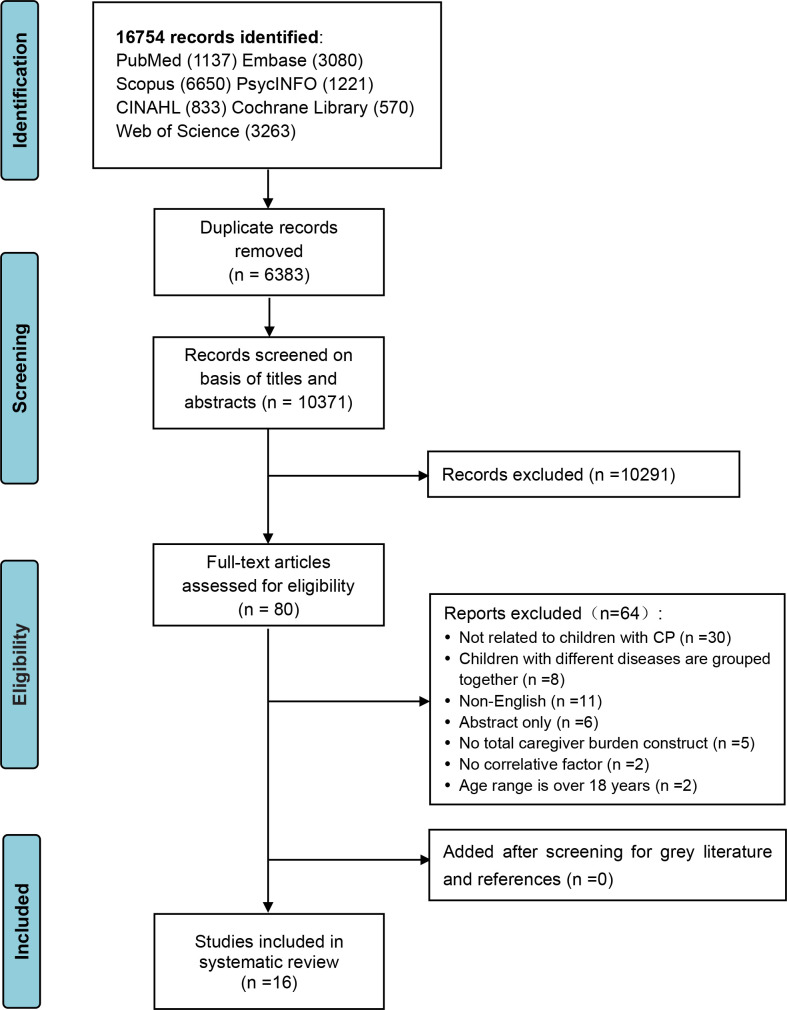
The search identified a total of 16 754 possibly relevant articles. After the removal of duplicates and the abstract screening, a total of 80 studies were selected for full-text review. Finally, 16 studies were left for full inclusion in the review. There were no additional articles met the inclusion criteria when searching the references of the 16 articles. The PRISMA flow diagram for search and screening results are shown in figure 1.
Figure 1.
Flow diagram for a systematic literature review on caregiver burden in children with cerebral palsy (CP).
Risk of bias
Risk of bias scores for studies ranged from 4 to 7 out of a maximum of 8 points. Some articles lacked clear information in items: study subjects and the setting, exposure factors and confounding bias. The methodological quality assessment list is listed in online supplemental appendix 5.
Characteristics of the included studies
The 16 included studies reported on overall caregiver burden and related factors of children with CP. Studies were conducted in 11 different countries between 2011 and 2022, involving in 3109 caregivers (not inclusive of controls). Of these, 14 studies investigated univariate associations; 9 studies were explored in multivariate associations. Caregivers were predominantly female, and 5 of the 16 articles had samples made up exclusively of mothers. Six articles involved fathers. The mean age of caregivers varied from 31 to 42 years. Four studies involved control populations, two of four had caregivers of healthy children as the control group. All studies were cross-sectional surveys. The most used sampling method was convenience sampling. The key characteristics of each study are presented in table 1.
Table 1.
Summary of included studies
| Authors (year) | Country | Design | Caregiver sample size | Caregiver relation to child | Mean age of caregivers M (SD) | Age of children (years) | Measures tool |
| Carona et al (2013)25 | Portugal | Cross-sectional study | 93 | Mothers (83.8%) | 42.34 (5.72) | 8–18 | BM |
| Bella et al (2011)26 | Brazil | Cross-sectional study | 38 | Mothers (–) | 33.3 (7.7) | 4–11 | BI |
| Whittingham et al (2013)27 | Australia | Correlational survey study | 94 | Mothers (90.4%) | – | 2–12 | DPC burden |
| Farajzadeh et al (2021)20 | Iran | Cross-sectional study | 160 | Female (84.4%) | 35.47 (6.59) | 2–14 | CDS |
| Boztepe et al (2019)14 | Turkey | Cross-sectional study | 69 | Mothers (100%) | 34.6 (7.3) | 1–18 | ZBI |
| Omole et al (2019)21 | Nigeria | Cross-sectional study | 209 | Female (91.9%) | 34.6 (9.2) | 1–12 | CDS |
| Terathongkum et al (2020)8 | Thailand | Correlational research | 75 | Female (88.0%) | – | 0–18 | VQ burden |
| Farajzadeh et al (2020)22 | Iran | Cross-sectional study | 203 | Mothers (100%) | 34.48 (6.74) | 4–14 | CDS |
| Wijesinghe et al (2015)23 | Sri Lanka | Cross-sectional study | 375 | Mothers (97%) | 32.4 (7.2) | 1–12 | CDS |
| Barutcu et al (2021)15 | Turkey | Cross-sectional study | 109 | Mothers (98.2%) | 38.53 (9.62) | 1–18 | ZBI |
| Ozkan et al (2018)16 | Turkey | Cross-sectional study | 120 | Mothers (100%) | – | 2–18 | ZBI |
| Gugała et al (2021)24 | Poland | Cross-sectional study | 190 | Female (72.6%) | 40.6 (9.1) | 2–18 | CBS |
| Marrón et al (2013)17 | Spain | Cross-sectional study | 62 | Mothers (88.7%) | 41.98 (5.64) | 1–17 | ZBI |
| Albayrak et al (2019)12 | Turkey | Cross-sectional study | 101 | Mothers (100%) | 34.93 (8.7) | 0–18 | ZBI |
| Santos et al (2012)18 | Brazil | Cross-sectional study | 21 | Female (100%) | 31 (–) | 1–12 | ZBI |
| Moriwaki et al (2022)19 | Japan | Cross-sectional study | 1190 | Mothers (100%) | 37.97 (5.28) | 1–12 | ZBI |
BI, The Burden Interview; BM, The Revised Burden Measure; CBS, Caregiver Burden Scale; CDS, Caregiver Difficulties Scale; DPC Burden, Daily Parenting Tasks Checklist–Parenting Burden; VQ burden, Thai version Viriyaprasart’s questionnaire about burden of care; ZBI, Zarit Burden Interview.
Measures of burden
Seven instruments were used to measure caregiver burden: Zarit Burden Interview (n=7)12 14–19; Caregiver Difficulties Scale (n=4)20–23; Caregiver Burden Scale (n=1)24; The Revised Burden Measure (n=1)25; The Burden Interview (n=1)26; Daily Parenting Tasks Checklist–Parenting Burden (n=1)27; Viriyaprasart’s questionnaire about burden of care (n=1).8
Studied factors in relation to caregiver burden
Overviews of caregiver and children characteristics as factors of caregiver burden are presented in tables 2 and 3. The detailed description is described as follows.
Table 2.
Associations between caregiver factors and caregiver burden
| Factor | Measure factor | Outcome caregiver burden | Bivariate analysis | Bivariate association r/t/F/β/Z | Multivariate association β/b (95% CI) |
N | Ref | |
| Demographics | Age | Years | VQ burden | P | ns | – | 75 | 8 |
| Years | ZBI | P or S | 0.20* | – | 101 | 12 | ||
| Years | ZBI | – | – | ns | 69 | 14 | ||
| Years | CDS | S | ns | – | 209 | 21 | ||
| Years | CDS | R | ns | – | 375 | 23 | ||
| Years | ZBI | P or S | ns | – | 109 | 15 | ||
| Gender | Male/female | CDS | T | −2.01* | – | 209 | 21 | |
| Education | 0–4 level | ZBI | – | – | ns | 69 | 14 | |
| 0–2 level | CDS | A | 4.95** | 2.61** (1.97 to 14.09) | 209 | 21 | ||
| Low education | CDS | R | ns | – | 375 | 23 | ||
| 0–5 level (mother) | ZBI | P or S | ns | – | 109 | 15 | ||
| Monthly income | TL | ZBI | – | – | ns | 69 | 14 | |
| 0–4 level | CDS | A | ns | – | 209 | 21 | ||
| Low income | CDS | R | 8.65*** | 3.69* (–) | 375 | 23 | ||
| 0–2 level | ZBI | P or S | 4.45* | – | 109 | 15 | ||
| No of caregivers | 1/2 | ZBI | P or S | ns | – | 109 | 15 | |
| Socioeconomic status | 0–4 level | CDS | A | ns | – | 209 | 21 | |
| Geographical area | Rural area | CDS | R | 6.27** | 5.35** (–) | 375 | 23 | |
| Mother employment | Yes/no | ZBI | U | ns | – | 1190 | 19 | |
| Additional helper | None or present | ZBI | – | – | ns | 69 | 14 | |
| Daily caring time | Hours | ZBI | P or S | ns | – | 101 | 12 | |
| Emotional functioning | Anxiety | HADS-A | CDS | P | 0.47*** | 0.14*** (nr) | 160 | 20 |
| BAI | ZBI | P or S | 0.29** | – | 109 | 15 | ||
| HADS-A | CBS | P | 0.51**** | – | 190 | 24 | ||
| Depression | BDI | ZBI | P or S | 0.70*** | – | 101 | 12 | |
| HADS-D | CDS | P | 0.51*** | 0.17*** (nr) | 160 | 20 | ||
| BDI | ZBI | – | – | 0.48*** (nr) | 69 | 14 | ||
| BDI-II | CDS | P | 0.64*** | – | 203 | 22 | ||
| BDI-II | ZBI | P or S | 0.41**** | – | 109 | 15 | ||
| HADS-D | CBS | P | 0.38**** | – | 190 | 24 | ||
| BDI-II | ZBI | – | – | 0.36** (0.17 to 0.73) | 62 | 17 | ||
| Mental health | SF-36-MCS | ZBI | P or S | ns | – | 101 | 12 | |
| MHI-5 | BM | nr | −0.51** | −0.20* (nr) | 93 | 25 | ||
| SF-36-RE | BI | S | ns | – | 38 | 26 | ||
| SF-36-MH | BI | S | −0.62* | – | 38 | 26 | ||
| WHOQOL-BREF-PsyH | CDS | P | −0.68*** | – | 203 | 22 | ||
| Perceived stress | PSQ | BI | S | 0.65*** | – | 38 | 26 | |
| PSS-4 | CDS | P | 0.43*** | 0.10*** (nr) | 160 | 20 | ||
| Beliefs of rehabilitation | RBQ | VQ burden | P | ns | – | 75 | 8 | |
| Perceived self-efficacy | PSQ | VQ burden | P | −0.25* | – | 75 | 8 | |
| RSCSE | ZBI | – | – | −0.19** (−0.31 to −0.06) | 62 | 17 | ||
| Experiential avoidance | AAQ-16 | DPC burden | nr | 0.42**** | 0.31** (0.52 to 1.21) | 94 | 27 | |
| Physical functioning | Sleep quality | PSQI | ZBI | P or S | 0.39*** | – | 101 | 12 |
| Pain | NRS | ZBI | P or S | 0.36*** | – | 101 | 12 | |
| SF-36-BP | BI | S | −0.40* | – | 38 | 26 | ||
| Fatigue/vitality | CIS | ZBI | P or S | 0.66*** | – | 101 | 12 | |
| FSS | CDS | P | 0.40*** | – | 203 | 22 | ||
| SF-36-VT | BI | S | −0.54* | – | 38 | 26 | ||
| Physical health | SF-36-PCS | ZBI | P or S | −0.21* | – | 101 | 12 | |
| SF-36-PF | BI | S | ns | – | 38 | 26 | ||
| SF-36-RP | BI | S | ns | – | 38 | 26 | ||
| SF-36-GH | BI | S | −0.44* | – | 38 | 26 | ||
| WHOQOL-BREF-PH | CDS | P | −0.59*** | – | 203 | 22 | ||
| Overall health | Quality of life | VQ well-being | VQ burden | P | −0.50** | – | 75 | 8 |
| WHOQOL-8 | BM | nr | −0.39** | −0.16* (nr) | 93 | 25 | ||
| Social functioning | Social functioning | SF-36-SF | BI | S | −0.61* | – | 38 | 26 |
| WHOQOL-BREF-SR | CDS | P | −0.68*** | – | 203 | 22 | ||
| Environment health | WHOQOL-BREF-E | CDS | P | −0.63*** | – | 203 | 22 | |
| Social support | SSS | BM | nr | −0.35** | −0.41** (nr) | 93 | 25 | |
| SSQ | VQ burden | P | ns | – | 75 | 8 | ||
| Family support | ZBI | U | ns | – | 1190 | 19 | ||
| Others support | ZBI | U | nr** | – | 1190 | 19 | ||
| Home-visit nursing | ZBI | C | nr** | – | 1190 | 19 | ||
| Home care | ZBI | C | nr* | – | 1190 | 19 | ||
| Home-visit rehabilitation | ZBI | C | nr** | – | 1190 | 19 | ||
| Training and treatment | ZBI | C | ns | – | 1190 | 19 | ||
| Short stay | ZBI | C | ns | – | 1190 | 19 | ||
| Mobility support | ZBI | C | nr* | – | 1190 | 19 | ||
| Transportation services | ZBI | C | ns | – | 1190 | 19 | ||
| No social support usage | ZBI | C | nr* | – | 1190 | 19 | ||
| Satisfaction with home-visit nursing | ZBI | C | ns | – | 1190 | 19 | ||
| Satisfaction with home care | ZBI | C | nr* | ns | 1190 | 19 | ||
| Satisfaction with home-visit rehabilitation | ZBI | C | nr** | ns | 1190 | 19 | ||
| Satisfaction with training and treatment | ZBI | C | nr** | ns | 1190 | 19 | ||
| Satisfaction with short stay | ZBI | C | nr** | −0.29* | 1190 | 19 | ||
| Satisfaction with mobility support | ZBI | C | ns | – | 1190 | 19 | ||
| Satisfaction with transportation services | ZBI | C | ns | – | 1190 | 19 | ||
| Coping | CHIP | DPC Burden | nr | ns | ns | 94 | 27 | |
| Individual coping | CDS | R | ns | – | 375 | 23 | ||
| Seeking social support | CDS | R | −8.99*** | ns | 375 | 23 | ||
| Spouse support | CDS | R | −7.44*** | −5.67** (nr) | 375 | 23 |
****p<0.0001, ***p<0.001, **p<0.01, *p<0.05.
A, one-way analysis of variance (ANOVA); AAQ-16, Acceptance and Action Questionnaire; BAI, Beck Anxiety Inventory; BDI, Beck Depression Inventory; BDI-II, Beck Depression Inventory-II; C, chi-squared test; CHIP, Coping Health Inventory for Parents; CIS, Multidimensional checklist individual strength; FSS, Fatigue Severity Scale; HADS, Hospital Anxiety and Depression Scale; HADS-A, HADS-Anxiety Scale; HADS-D, HADS-Depression Scale; MHI-5, Mental Health Inventory-short form; nr, not reported; NRS, numerical rating scale; ns, not significant; P, Pearson correlation coefficient; PSQ, Perceived self-efficacy in the care questionnaire; PSQI, Pittsburgh Sleep Quality Index; PSS-4, Perceived Stress Scale-4 item; R, univariate regression analysis; RBQ, adapted Rehabilitation Belief Questionnaire; RSCSE, Revised Scale for Caregiving Self-Efficacy; S, Spearman’s linear correlation coefficient/Spearman’s Rho correlation; SF-36, 36-Item Short Form Health Survey; SF-36-BP, SF-36-Bodily pain; SF-36-GH, SF-36-General health; SF-36-MCS, SF-36-Mental component summary; SF-36-MH, SF-36-Mental health; SF-36-PCS, SF-36-Physical component summary; SF-36-PF, SF-36-Physical functioning; SF-36-RE, SF-36-Emotional role; SF-36-RP, SF-36-Physical role; SF-36-SF, SF-36-Social functioning; SF-36-VT, SF-36-Vitality; SSQ, adapted Social Support Questionnaire; SSS, Satisfaction with Social Support Scale; T, independent Student’s t-test; U, Mann-Whitney U test; VQ well-being, Thai version Viriyaprasart’s questionnaire about well-being; WHOQOL-8, WHO Quality of Life Assessment 8 item index; WHOQOL-BREF, WHO’s Quality of Life Questionnaire; WHOQOL-BREF-E, WHOQOL-BREF-Environment; WHOQOL-BREF-PH, WHOQOL-BREF-Physical health; WHOQOL-BREF-PsyH, WHOQOL-BREF-Psychological health; WHOQOL-BREF-SR, WHOQOL-BREF-Social relationships.
Table 3.
Associations between children factors and caregiver burden
| Factor | Measure factor | Outcome caregiver burden | Bivariate analysis | Bivariate association r/t/F/β/Z/H/X2 | Multivariate association β/b (95% CI) |
N | Ref | |
| Demographics | Age | Years | VQ burden | P | ns | – | 75 | 8 |
| Years | ZBI | P or S | ns | – | 101 | 12 | ||
| Years | ZBI | – | – | ns | 69 | 14 | ||
| Years | CDS | S | ns | – | 209 | 21 | ||
| Years | CDS | R | ns | – | 375 | 23 | ||
| 1–5/6–12/>12 years old | ZBI | P or S | ns | – | 109 | 15 | ||
| Years | ZBI | U | ns | – | 1190 | 19 | ||
| Gender | Male/female | ZBI | – | – | ns | 69 | 14 | |
| Male child | CDS | T | 3.02** | 0.18** (1.56 to 8.34) | 209 | 21 | ||
| Male child | CDS | R | 3.60* | 3.50* (−) | 375 | 23 | ||
| Male/female | CBS | P or S | ns | – | 109 | 15 | ||
| Going to nursery/school | Yes/no | ZBI | U | ns | – | 1190 | 19 | |
| Residence | Urban/rural | ZBI | U | nr**** | – | 1190 | 19 | |
| Birth order | 1st/2nd/3rd or greater | CDS | A | ns | – | 209 | 21 | |
| First/or not | ZBI | U | ns | – | 1190 | 19 | ||
| No of children | 3 or higher | ZBI | – | – | ns | 69 | 14 | |
| 1/2/3 | CDS | R | ns | – | 375 | 23 | ||
| 1/2/3/4 or more | ZBI | P or S | 0.20* | – | 109 | 15 | ||
| 1/or not | ZBI | U | ns | – | 1190 | 19 | ||
| No of disabled children | 1/or not | ZBI | P or S | ns | – | 109 | 15 | |
| Body mass index | BMI | ZBI | P or S | ns | – | 101 | 12 | |
| Disease related | Type of CP | 5 types | CDS | A | 3.15* | – | 209 | 21 |
| Spastic quadriplegia | CDS | R | 10.62*** | – | 375 | 23 | ||
| Severity of illness | GMFCS | ZBI | P or S | 0.30** | – | 101 | 12 | |
| Severity of illness scale | ZBI | – | – | 0.29* (nr) | 69 | 14 | ||
| GMFCS-ER | CDS | A | 6.87*** | 0.29*** (4.42 to 11.23) | 209 | 21 | ||
| nr | ZBI | – | – | 0.28* (0.04 to 0.35) | 62 | 17 | ||
| 3 levels | ZBI | H | nr** | ns | 1190 | 19 | ||
| Tube/intravenous nutrition | Yes/no | ZBI | C | nr* | ns | 1190 | 19 | |
| Aetiology | 7 types | CDS | A | 2.49* | – | 209 | 21 | |
| Additional physical illness | Absent/present | ZBI | – | – | ns | 69 | 14 | |
| Associated conditions | 0/1/2/3/4 or more | CDS | A | 3.21* | – | 209 | 21 | |
| 0/1 or more | CDS | R | 12.75*** | ns | 375 | 23 | ||
| Functional impairments | No of functional deficits | CDS | R | 3.97*** | 2.64*** (nr) | 375 | 23 | |
| Behavioural functioning | Functional status | FIM | ZBI | P or S | ns | – | 109 | 15 |
| Behavioural problems | SDQ | BM | nr | 0.24* | 0.29** | 93 | 25 | |
| SDQ | DPC burden | nr | 0.38**** | 0.27** (0.06 to 1.43) | 94 | 27 | ||
| Overall health | Quality of life | KIDSCREEN-10 | BM | nr | ns | – | 93 | 25 |
| PedsQL | ZBI | P | 0.40*** | – | 120 | 16 | ||
| Social environment | Social support | SSSS | BM | nr | ns | −0.19* (nr) | 93 | 25 |
| Environment | Space for child locomotion | ZBI | P | nr* | – | 21 | 18 |
****p<0.0001, ***p<0.001, **p<0.01, *p<0.05.
A, one-way analysis of variance (ANOVA); BMI, Body Mass Index; C, chi-squared test; CP, cerebral palsy; FIM, Functional Independence Measure; GMFCS, Gross Motor Function Classification System; GMFCS-ER, Gross Motor Function Classification System–Expanded and Revised; H, Kruskal-Wallis H; KIDSCREEN-10, The shortest version of Kidscreen questionnaires; nr, not reported; ns, not significant; P, Pearson correlation coefficient; PedsQL, Pediatric Quality of Life 4.0 Generic Core Scales; R, univariate regression analysis; S, Spearman’s linear correlation coefficient/Spearman’s Rho correlation; SDQ, Strengths and Difficulties Questionnaire; SSSS, Satisfaction with social support scale for children and adolescents; T, independent Student’s t-test; U, Mann-Whitney U test.
Caregiver factors
Caregiver factors were grouped into five categories, including caregiver demographics, emotional functioning, physical functioning, overall health and social functioning. Caregiver demographical factors included age,8 12 14 15 21 23 gender,21 educational level,14 15 21 23 monthly income,14 15 21 23 number of caregiver,15 socioeconomic status,21 geographical area,23 mother employment,19 additional helper14 and daily caring time.12 Emotional functioning factors included anxiety,15 20 24 depression,12 14 15 17 20 22 24 mental health,12 22 25 26 perceived stress,20 26 beliefs of rehabilitation,8 perceived self-efficacy8 17 and experiential avoidance.27 This category was included in 11 of the 15 studies. Physical functioning factors included sleep quality,12 pain,12 26 fatigue12 22 and physical health.12 22 26 Overall health factors included quality of life.8 25 Social functioning factors included social functioning,22 26 environment health,22 social support8 19 25 and coping.23 27
Children factors
Children factors were grouped into five categories, including children demographics, disease related, behavioural functioning, overall health and social environment. Children demographical factors included age,8 12 14 15 21 23 gender,14 15 21 23 going to nursery/school,19 residence,19 birth order,21 number of children,14 15 23 number of disabled child15 and body mass index.12 Disease-related factors included type of CP,21 23 severity of CP,12 14 17 21 tube/intravenous nutrition,19 aetiology,21 additional physical illness,14 associated conditions21 23 and functional impairments.23 This category was included in 5 of the 15 studies. Behavioural functioning factors included functional statu15wehavioural problems.25 27 Overall health and social environment factors included quality of life,16 25 social support25 and environment.18
Quality of evidence for potential factors
Quality of evidence for potential factors of caregiver burden are presented in online supplemental table. The criteria for compelling evidence are that each factor was measured in at least three studies that reported significant relationships. The details are as follows.
bmjopen-2022-065215supp003.pdf (121.4KB, pdf)
Caregiver factors
The results of evidence synthesis for caregiver factors using the GRADE criteria were that ‘depression’ was the moderate quality of evidence for factor of caregiver burden. ‘Age’, ‘anxiety’ and ‘fatigue’ of caregivers was the low quality of evidence for factors of caregiver burden. Very low quality of evidence was found for the relationship between caregiver burden and ‘education’, ‘monthly income’, ‘mental health’, ‘physical health’ and ‘social support’ of caregivers.
Children factors
The synthesis of the evidence for children factors resulted in moderate quality of evidence between caregiver burden and ‘severity of illness’. The factors for ‘age’ and ‘gender’ of children, and ‘number of children’ were the low quality of evidence for the relations with caregiver burden. Few of the included studies have explored children factors, and fewer factors have been able to perform evidence synthesis.
Discussion
Caring for children with CP is a stressful and difficult task for primary caregivers, especially for their parents. Caregivers of children with CP were under higher pressure than caregivers of healthy children.12 28 29 There were many factors that affect the caregiving burden for children with CP. In our systematic review, we focused on both caregiver characteristics and children characteristics as factors of caregiver burden. There are fewer studies involving children-related factors than caregiver-related factors, possibly because caregiver-related factors are more likely to modify. This review revealed that anxiety and depression of caregiver, and severity of illness in children with CP were moderate quality of evidence for factors contributing to caregiver burden. However, our ability to draw conclusions on remaining caregiver and children characteristics as factors is limited because of low to very low quality of evidence.
Moderate quality was found for the association between caregiver burden and depression symptoms of the caregiver. Feelings of depression are positively correlated with caregiver burden of the caregiver. However, the factor for mental health predicting psychological well-being of the caregiver as well was rated as very low quality of evidence. This may be due to the limited number of studies that did not yield reliable evidence. Three studies included in this review revealed that caregivers, who experience poor psychological condition, are more likely to experience high caregiver burden. This correlation between mental health of caregiver and caregiver burden is consistent with the findings in other children with neurodevelopmental diseases, such as epilepsy and autism spectrum disorder.30–32 Mother caregivers constitutes the majority of caregiving. Long-term care of children with CP and restricted social activity for the mother caregiver predict more psychological conditions such as anxiety, depression and distress in them.33 Caregivers who feel depressed experience a greater burden of care, thereby affecting CP children’s quality of life.16 A study revealed that psychological interventions such as Stepping Stones Triple P therapy, and Acceptance and Commitment Therapy could improve parental mental well-being of parents of children with CP. It is crucial to develop more interventions that focus primarily on the psychological well-being of the parents.34
Low quality of evidence was found for the relationship between caregiver burden and fatigue of the caregiver. Fatigue of caregivers are positively related to caregiver burden. Children with CP are often accompanied by intellectual and physical disabilities. Daily life care and assistance with rehabilitation exercises mean more physical strength and energy for the caregiver, so that caregivers often experience problems such as body pain, fatigue and sleep problems,12 35–38 which seriously affect the physical well-being and reduce the quality of life of the caregiver.39 40 Few studies have focused on interventions for caregivers’ physical conditions. We should actively pay attention to the physical health of the caregiver and take feasible interventions to improve the physical functioning of caregivers of children with CP.
In our systematic review, it is not sufficiently concluded that social support for caregivers is a positive factor in reducing the burden. However, many previous studies have explored the correlation between social support and parenting stress in caregivers of children with CP. Negative associations were found between the levels of stress among parents and social support perceived by them.41–44 Many families faced financial difficulties and restricted access to healthcare services.45 46 Social support from spouses, social organisation and medical institution help prevent and decrease the stressful situation of the family’s experience in providing care to children with CP.43 47 Although parenting stress and caregiver burden have similar meanings, this review focuses on caregiver burden and involves fewer relevant articles about the association between social support and care burden, so more evidence is needed to determine their relevance.
The factor for severity of illness in CP children as moderate quality of evidence is positively correlated with the burden of caregiver. Gross Motor Function Classification System score is most commonly used to measure the severity of disability of children with CP. Children with more severe disabilities require the more support of their caregivers to carry out the activities of daily living. Caregivers will spend more time and physical strength to meet the caregiving demands,38 48 and the caregiver burden will be heavier. In addition, there was no significant correlation between the age of CP children and the caregiver burden. Also, the gender of children with CP may affect the caregiver’s burden. The burden of care for male child is greater than that of female child, probably because of the greater mobility of male children. At present, there are many researches on motor function intervention for children with CP. A guideline synthesised approaches to functional exercise in walking ability and hand mobility in children, indicating whole-task practice combined with assistive devices could increase independence and reduce caregiver burden.49
This systematic review offers insight into factors related to caregiver burden and guides the supportive interventions aiming to reduce caregiver burden, but more additional research into factors associated with caregiver burden is needed.
Strengths and limitations
This review was the first one to provide a comprehensive overview of caregiver burden of children with CP. The protocol was registered on the PROSPERO database and was carried out based on the PRISMA guidelines. The quality of evidence for factors was judged by the GRADE approach. There were also some limitations of the review. First, the included literature used different measurement tools, and the survey factors of the total care burden with/without the burden of each dimension were scattered. Second, due to the uneven quality of the included studies, the quality of the literature is at a medium level, and convenience sampling is often used, which has many methodological limitations.
Conclusion
Caregivers of children with CP generally have a heavy burden of caregiving, which has affected the physical, psychological, social and economic conditions of the caregivers. We summarised factors related to caregiver burden from the aspects of caregiver factors and children factors. The results revealed that depression of caregiver and severity of illness in children with CP were moderate quality of evidence for factors contributing to caregiver burden. At present, the relevant literature on the factors affecting the caregiver burden of children with CP are mostly cross-sectional studies, and there is a lack of longitudinal studies with high demonstration efficiency. In the future, we should focus on carrying out high-quality longitudinal research and verifying the relevant influencing factors of caregiver burden of children with CP. Moreover, by identifying all the factors, healthcare professionals can provide appropriate assistance to relieve caregiver burden and improve the quality of caregiving for children with CP.
Supplementary Material
Footnotes
Contributors: This study was conceived and designed by FL and QS. FL developed the search strategy and performed the literature search. FL and QS performed full-text reviews and extraction of data. FL and MH conducted the statistical analysis with input from QS. FL wrote the first draft. HZ was responsible for project administration and supervision on revised paper. All authors reviewed all drafts and approved the final submitted manuscript. Data extraction and quality assessment adhered to PRISMA guidelines. FL is responsible for the overall content as guarantor.
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Provenance and peer review: Not commissioned; externally peer reviewed.
© Author(s) (or their employer(s)) 2023. Re-use permitted under CC BY-NC. No commercial re-use. See rights and permissions. Published by BMJ.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
All data relevant to the study are included in the article or uploaded as supplementary information.
Ethics statements
Patient consent for publication
Not applicable.
Ethics approval
Not applicable.
References
- 1.McIntyre S, Goldsmith S, Webb A, et al. Global prevalence of cerebral palsy: a systematic analysis. Dev Med Child Neurol 2022;64:1494–506. 10.1111/dmcn.15346 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bax M, Goldstein M, Rosenbaum P, et al. Proposed definition and classification of cerebral palsy, April 2005. Dev Med Child Neurol 2005;47:571–6. 10.1017/s001216220500112x [DOI] [PubMed] [Google Scholar]
- 3.Odding E, Roebroeck ME, Stam HJ. The epidemiology of cerebral palsy: incidence, impairments and risk factors. Disabil Rehabil 2006;28:183–91. 10.1080/09638280500158422 [DOI] [PubMed] [Google Scholar]
- 4.Elbasan B, Duzgun I, Oskay D. Is there any difference in health related quality of life, self care and social function in children with different disabilities living in turkey? Iran J Pediatr 2013;23:281–8. [PMC free article] [PubMed] [Google Scholar]
- 5.Aisen ML, Kerkovich D, Mast J, et al. Cerebral palsy: clinical care and neurological rehabilitation. Lancet Neurol 2011;10:844–52. 10.1016/S1474-4422(11)70176-4 [DOI] [PubMed] [Google Scholar]
- 6.Vargus-Adams J. Parent stress and children with cerebral palsy. Dev Med Child Neurol 2011;53:777. 10.1111/j.1469-8749.2011.04037.x [DOI] [PubMed] [Google Scholar]
- 7.Polack S, Adams M, O’banion D, et al. Children with cerebral palsy in Ghana: malnutrition, feeding challenges, and caregiver quality of life. Dev Med Child Neurol 2018;60:914–21. 10.1111/dmcn.13797 [DOI] [PubMed] [Google Scholar]
- 8.Terathongkum S, Panyatanakun N, Arj-Ong Vallibhakara S. Factors associated with well-being of family caregivers of children with cerebral palsy in Bangkok. J Med Assoc Thai 2020;103:1214–9. 10.35755/jmedassocthai.2020.11.12256 [DOI] [Google Scholar]
- 9.Kasuya RT, Polgar-Bailey P, Takeuchi R. Caregiver burden and burnout. A guide for primary care physicians. Postgrad Med 2000;108:119–23. 10.3810/pgm.2000.12.1324 [DOI] [PubMed] [Google Scholar]
- 10.Ying K, Rostenberghe HV, Kuan G, et al. Health-related quality of life and family functioning of primary caregivers of children with cerebral palsy in Malaysia. Int J Environ Res Public Health 2021;18:2351. 10.3390/ijerph18052351 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Vadivelan K, Sekar P, Sruthi SS, et al. Burden of caregivers of children with cerebral palsy: an intersectional analysis of gender, poverty, stigma, and public policy. BMC Public Health 2020;20:645. 10.1186/s12889-020-08808-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Albayrak I, Biber A, Çalışkan A, et al. Assessment of pain, care burden, depression level, sleep quality, fatigue and quality of life in the mothers of children with cerebral palsy. J Child Health Care 2019;23:483–94. 10.1177/1367493519864751 [DOI] [PubMed] [Google Scholar]
- 13.Lee MH, Matthews AK, Park C. Determinants of health-related quality of life among mothers of children with cerebral palsy. J Pediatr Nurs 2019;44:1–8. 10.1016/j.pedn.2018.10.001 [DOI] [PubMed] [Google Scholar]
- 14.Boztepe H, Çınar S, Ay A, et al. Predictors of caregiver burden in mothers of children with leukemia and cerebral palsy. J Psychosoc Oncol 2019;37:69–78. 10.1080/07347332.2018.1489441 [DOI] [PubMed] [Google Scholar]
- 15.Barutcu A, Barutcu S, Kolkiran S, et al. Evaluation of anxiety, depression and burden on caregivers of children with cerebral palsy. Dev Neurorehabil 2021;24:555–60. 10.1080/17518423.2021.1917718 [DOI] [PubMed] [Google Scholar]
- 16.Ozkan Y. Child’s quality of life and mother’s burden in spastic cerebral palsy: a topographical classification perspective. J Int Med Res 2018;46:3131–7. 10.1177/0300060518772758 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Muñoz-Marrón E, Redolar D, Boixadós M, et al. Burden on caregivers of children with cerebral palsy: predictors and related factors. Univ Psychol 2013;12:767–78. 10.11144/Javeriana.UPSY12-3.bccc [DOI] [Google Scholar]
- 18.Santos AA de S, Araújo JA, Vargas MM, et al. The influence of household environment on caregivers’ overload of children with cerebral paralysis. Acta Sci Health Sci 2012;34:315–20. 10.4025/actascihealthsci.v34ispec.10264 [DOI] [Google Scholar]
- 19.Moriwaki M, Yuasa H, Kakehashi M, et al. Impact of social support for mothers as caregivers of cerebral palsy children in japan. J Pediatr Nurs 2022;63:e64–71. 10.1016/j.pedn.2021.10.010 [DOI] [PubMed] [Google Scholar]
- 20.Farajzadeh A, Dehghanizadeh M, Maroufizadeh S, et al. Predictors of mental health among parents of children with cerebral palsy during the COVID-19 pandemic in Iran: a web-based cross-sectional study. Res Dev Disabil 2021;112:103890. 10.1016/j.ridd.2021.103890 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Omole J, Adegoke S, Omole K, et al. Levels, correlates, and predictors of stress and caregiver burden among caregivers of children with cerebral palsy in Nigeria. J Pediatr Neurol 2019;17:013–21. 10.1055/s-0037-1612639 [DOI] [Google Scholar]
- 22.Farajzadeh A, Maroufizadeh S, Amini M. Factors associated with quality of life among mothers of children with cerebral palsy. Int J Nurs Pract 2020;26:e12811. 10.1111/ijn.12811 [DOI] [PubMed] [Google Scholar]
- 23.Wijesinghe CJ, Cunningham N, Fonseka P, et al. Factors associated with caregiver burden among caregivers of children with cerebral palsy in Sri Lanka. Asia Pac J Public Health 2015;27:85–95. 10.1177/1010539514548756 [DOI] [PubMed] [Google Scholar]
- 24.Gugała B. Caregiver burden versus intensity of anxiety and depression symptoms in parents of children with cerebral palsy as well as factors potentially differentiating the level of burden: a cross-sectional study (Poland). BMJ Open 2021;11:e036494. 10.1136/bmjopen-2019-036494 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Carona C, Crespo C, Canavarro MC. Similarities amid the difference: caregiving burden and adaptation outcomes in dyads of parents and their children with and without cerebral palsy. Res Dev Disabil 2013;34:882–93. 10.1016/j.ridd.2012.12.004 [DOI] [PubMed] [Google Scholar]
- 26.Bella GP, Garcia MC, Spadari-Bratfisch RC. Salivary cortisol, stress, and health in primary caregivers (mothers) of children with cerebral palsy. Psychoneuroendocrinology 2011;36:834–42. 10.1016/j.psyneuen.2010.11.005 [DOI] [PubMed] [Google Scholar]
- 27.Whittingham K, Wee D, Sanders MR, et al. Predictors of psychological adjustment, experienced parenting burden and chronic sorrow symptoms in parents of children with cerebral palsy. Child Care Health Dev 2013;39:366–73. 10.1111/j.1365-2214.2012.01396.x [DOI] [PubMed] [Google Scholar]
- 28.Ramanandi VH, Rao B. Comparison of stress levels in the parents of children with cerebral palsy and parents of normal children in VADODARA region of Gujarat. International Journal of Physiotherapy 2015;2:421. 10.15621/ijphy/2015/v2i2/65252 [DOI] [Google Scholar]
- 29.Wang HY, Jong YJ. Parental stress and related factors in parents of children with cerebral palsy. The Kaohsiung J of Med Scie 2004;20:334–40. 10.1016/S1607-551X(09)70167-6 [DOI] [Google Scholar]
- 30.Pokharel R, Poudel P, Lama S, et al. Burden and its predictors among caregivers of patient with epilepsy. J Epilepsy Res 2020;10:24–30. 10.14581/jer.20005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Lerthattasilp T, Charernboon T, Chunsuwan I, et al. Depression and burden among caregivers of children with autistic spectrum disorder. J Med Assoc Thai 2015;98 Suppl 2:S45–52. [PubMed] [Google Scholar]
- 32.Singh P, Ghosh S, Nandi S. Subjective burden and depression in mothers of children with autism spectrum disorder in India: moderating effect of social support. J Autism Dev Disord 2017;47:3097–111. 10.1007/s10803-017-3233-y [DOI] [PubMed] [Google Scholar]
- 33.Barreto TM, Bento MN, Barreto TM, et al. Prevalence of depression, anxiety, and substance-related disorders in parents of children with cerebral palsy: a systematic review. Dev Med Child Neurol 2020;62:163–8. 10.1111/dmcn.14321 [DOI] [PubMed] [Google Scholar]
- 34.Irwin L, Jesmont C, Basu A. A systematic review and meta-analysis of the effectiveness of interventions to improve psychological wellbeing in the parents of children with cerebral palsy. Res Dev Disabil 2019;95:103511. 10.1016/j.ridd.2019.103511 [DOI] [PubMed] [Google Scholar]
- 35.Czupryna K, Nowotny-Czupryna O, Nowotny J. Back pain in mothers of cerebral palsied children. Ortop Traumatol Rehabil 2014;16:497–505. 10.5604/15093492.1128840 [DOI] [PubMed] [Google Scholar]
- 36.Garip Y, Ozel S, Tuncer OB, et al. Fatigue in the mothers of children with cerebral palsy. Disabil Rehabil 2017;39:757–62. 10.3109/09638288.2016.1161837 [DOI] [PubMed] [Google Scholar]
- 37.Lang CP, Boucaut A, Guppy M, et al. Children with cerebral palsy: a cross-sectional study of their sleep and their caregiver’s sleep quality, psychological health and well-being. Child Care Health Dev 2021;47:859–68. 10.1111/cch.12897 [DOI] [PubMed] [Google Scholar]
- 38.Gokcin Eminel A, Kahraman T, Genc A. Physical workload during caregiving activities and related factors among the caregivers of children with cerebral palsy. Ir J Med Sci 2021;190:701–9. 10.1007/s11845-020-02337-w [DOI] [PubMed] [Google Scholar]
- 39.Kaya K, Unsal-Delialioglu S, Ordu-Gokkaya NK, et al. Musculo-skeletal pain, quality of life and depression in mothers of children with cerebral palsy. Disabil Rehabil 2010;32:1666–72. 10.3109/09638281003649912 [DOI] [PubMed] [Google Scholar]
- 40.Raina P, O’Donnell M, Rosenbaum P, et al. The health and well-being of caregivers of children with cerebral palsy. Pediatrics 2005;115:e626–36. 10.1542/peds.2004-1689 [DOI] [PubMed] [Google Scholar]
- 41.Wang Y, Huang Z, Kong F. Parenting stress and life satisfaction in mothers of children with cerebral palsy: the mediating effect of social support. J Health Psychol 2020;25:416–25. 10.1177/1359105317739100 [DOI] [PubMed] [Google Scholar]
- 42.Lima MBS, Cardoso V dos S, Silva SS da C. Parental stress and social support of caregivers of children with cerebral palsy. Paidéia (Ribeirão Preto) 2016;26:207–14. 10.1590/1982-43272664201608 [DOI] [Google Scholar]
- 43.Alias NA, Razali Azizan NKA, Azizan NA. Relationship between level of stress and social support among parents of children with cerebral palsy. E-BPJ 2020;5:105–10. 10.21834/ebpj.v5i14.2187 [DOI] [Google Scholar]
- 44.Gordon A, Lang C, Larkin R, et al. Effect of social support services on the emotional well-being of caregivers of children with cerebral palsy. Dev Med Child Neurol 2012;54:62–3. [Google Scholar]
- 45.Ismail A, Sk Abd Razak R, Suddin LS, et al. The economic burden and determinant factors of parents/caregivers of children with cerebral palsy in Malaysia: a mixed methods study. Int J Environ Res Public Health 2022;19:475. 10.3390/ijerph19010475 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Ribeiro MFM, Sousa ALL, Vandenberghe L, et al. Parental stress in mothers of children and adolescents with cerebral palsy. Rev Lat Am Enfermagem 2014;22:440–7. 10.1590/0104-1169.3409.2435 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Al-Gamal E, Long T. Psychological distress and perceived support among Jordanian parents living with a child with cerebral palsy: a cross-sectional study. Scand J Caring Sci 2013;27:624–31. 10.1111/j.1471-6712.2012.01071.x [DOI] [PubMed] [Google Scholar]
- 48.Sawyer MG, Bittman M, LA Greca AM, et al. Time demands of caring for children with cerebral palsy: what are the implications for maternal mental health? Dev Med Child Neurol 2011;53:338–43. 10.1111/j.1469-8749.2010.03848.x [DOI] [PubMed] [Google Scholar]
- 49.Jackman M, Sakzewski L, Morgan C, et al. Interventions to improve physical function for children and young people with cerebral palsy: international clinical practice guideline. Dev Med Child Neurol 2022;64:536–49. 10.1111/dmcn.15055 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2022-065215supp001.pdf (64.1KB, pdf)
bmjopen-2022-065215supp002.pdf (129.4KB, pdf)
bmjopen-2022-065215supp003.pdf (121.4KB, pdf)
Data Availability Statement
All data relevant to the study are included in the article or uploaded as supplementary information.