Abstract
Background
Parenting interventions in humanitarian settings have prioritized the acquisition of parenting knowledge and skills, while overlooking the adverse effects of stress and distress on parenting—a key mediator of refugee children's mental health. We evaluated the effectiveness of the Caregiver Support Intervention (CSI), which emphasizes caregiver wellbeing together with training in positive parenting.
Methods
We conducted a two‐arm randomized controlled trial of the CSI with Syrian refugees in Lebanon, with an intent‐to‐treat design, from September 2019–December 2020. A total of 480 caregivers from 240 families were randomized to the CSI or a waitlist control group (1:1). Retention from baseline to endline was 93%. Data on parenting and caregiver psychological wellbeing were collected at baseline, endline, and three‐month follow‐up. Prospective trial registration: ISRCTN22321773.
Results
We did not find a significant change on overall parenting skills at endline (primary outcome endpoint) (d = .11, p = .126) or at follow‐up (Cohen's d = .15, p = .054). We did find a significant effect on overall parenting skills among participants receiving the full intervention—the sub‐sample not interrupted by (COVID‐19) (d = 0.25, p < .05). The CSI showed beneficial effects in the full sample at endline and follow‐up on harsh parenting (d = −.17, p < .05; d = .19, p < .05), parenting knowledge (d = .63, p < .001; d = .50, p < .001), and caregiver distress (d = −.33, p < .001; d = .23, p < .01). We found no effects on parental warmth and responsiveness, psychosocial wellbeing, stress, or stress management. Changes in caregiver wellbeing partially mediated the impact of the CSI on harsh parenting, accounting for 37% of the reduction in harsh parenting.
Conclusions
The CSI reduced harsh parenting and caregiver distress, and demonstrated the value of addressing caregiver wellbeing as a pathway to strengthening parenting in adversity. These effects were achieved despite a pandemic‐related lockdown that impacted implementation, a severe economic crisis, and widespread social unrest. Replication under less extreme conditions may more accurately demonstrate the intervention's full potential.
Keywords: Parenting, refugees, stress, distress, war
Introduction
Robust evidence points to the powerful role of compromised parenting in mediating the impact of armed conflict and forced migration on children's mental health (Bryant et al., 2018; Panter‐Brick, Grimon, & Eggerman, 2014; Sim, Bowes, & Gardner, 2018). In a recent systematic review, Eltanamly, Leijten, Jak, and Overbeek (2019) found that caregiver stress and distress stemming from armed conflict and displacement negatively impact parenting through two primary pathways: an increase in harsh parenting and a decrease in parental warmth and responsiveness. Although the studies in the Eltanamly et al. review are primarily cross‐sectional, recent longitudinal studies of conflict‐affected families have found strong evidence of a pathway leading from caregiver distress to harsh parenting, which in turn predicted emotional and behavioral problems in children (Bryant et al., 2018; Panter‐Brick et al., 2014).
Researchers have also used qualitative methods to explore the impact of chronic adversity on parenting in conflict‐affected families. In their study of Syrian refugees in Lebanon, Sim and colleagues found an increase in harsh parenting and a decrease in warm and responsive parenting stemming from heightened stress due to poverty, inadequate housing, and other environmental stressors (Sim, Fazel, Bowes, & Gardner, 2018). Parents perceived a clear pathway from their increased stress to negative changes in their parenting, to increased behavioral and emotional problems in their children.
Growing recognition of the role of parenting in mediating the impact of war and displacement on children's mental health has fostered interest in strengthening parenting in conflict‐affected communities (Puffer, Annan, Sim, Salhi, & Betancourt, 2017; Singla, Kumbakumba, & Aboud, 2015). This represents a shift beyond the historically dominant focus on direct work with children in humanitarian settings (Miller & Jordans, 2016). This shift reflects a recognition that there is limited value in providing children with therapeutic or preventive interventions, only to send them home to stressful environments that may contribute to their distress and undermine intervention effects (Miller, Jordans, Tol, & Galappatti, 2021).
Despite compelling evidence of a pathway from chronic adversity to caregiver stress and distress to compromised parenting, interventions aimed at strengthening parenting in humanitarian settings have generally prioritized increasing parenting knowledge and skills, while attending only minimally to caregivers' own wellbeing (Puffer et al., 2017). Implicit in this emphasis on parent training is a deficit model, in which suboptimal parenting is regarded not as compromised, but as reflecting a lack of essential knowledge and skills. While we recognize that parenting is difficult and most caregivers can benefit from exposure to evidence‐based parenting methods, we find the relative inattention to caregiver wellbeing inconsistent with what is known about the adverse effects of stress and distress on parenting in conflict‐affected communities (Eltanamly et al., 2019).
We have proposed an alternative model, depicted in Figure 1. This model accounts for the well‐established effect of both acute and chronic adversity on parenting, while also recognizing that cultural norms and childhood experiences of parenting may contribute to unhelpful or even harmful parenting practices. The model posits that under conditions of lower distress and stress‐related arousal, parents will be better able to make use of the parenting knowledge and skills they already possess, as well as newly acquired concepts and methods learned in parenting interventions.
Figure 1.
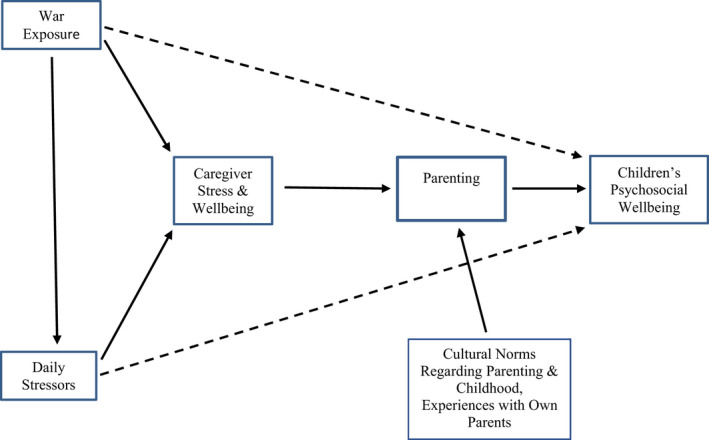
Conceptual model underlying the CSI*. *We recognize that there may be other pathways beyond those depicted in Figure 1 by which daily stressors may impact parenting directly, in addition to exerting effects via parental stress and wellbeing. Figure 1 depicts the conceptual model that guided the development of the CSI; it is not meant to be a comprehensive model capturing the diverse pathways by which external stressors may impact parenting [Color figure can be viewed at wileyonlinelibrary.com]
Guided by the model in Figure 1, War Child developed the Caregiver Support Intervention (CSI), a nine‐session preventive group intervention for primary caregivers of children aged 3–12 affected by armed conflict and forced migration. The CSI aims to strengthen parenting through two pathways: (a) directly, by strengthening participants' knowledge and skills related to evidence‐based parenting methods that have strong cross‐cultural support, and (b) indirectly, by improving the mental health and psychosocial wellbeing of caregivers.
After extensive formative work developing the CSI in Gaza and Lebanon (Miller et al., 2020), we conducted a pilot randomized controlled trial (RCT) with Syrian refugees in North Lebanon (Miller et al., 2020). The pilot included 79 families (72 with both caregivers) and demonstrated the feasibility of all methods.
The aim of this RCT was to evaluate the effectiveness of the CSI on parenting among Syrian refugee caregivers in North Lebanon. Our primary hypothesis was that participants in the CSI arm would show greater improvement in parenting relative to a waitlist control (WLC) group at endline and three‐month follow‐up. Secondarily, we hypothesized that CSI participants would show greater improvement than WLC at endline and three‐month follow‐up in parental warmth and responsiveness, harsh parenting, and parenting knowledge. Our additional hypothesis was that the impact of the CSI on parenting would be partially mediated by reductions in stress and distress and by improvements in stress management and psychosocial wellbeing.
Methods
Study design
This was a parallel group superiority RCT, with an intent to treat design, a 1:1 allocation ratio, and a WLC comparison group.
Participants
Participants in this trial were primarily Syrian refugee caregivers with at least one child between the ages of three and 12. Although up to 25% of the sample was open to Palestinian refugee and/or Lebanese families (in abiding by the Lebanon government's policy of ensuring that humanitarian programming is also available to host communities), 95% of the final sample was comprised of Syrian refugees. Inclusion criteria were: (a) Arabic‐speaking Syrian refugee or host community families with at least one child between the ages of 3–12; (b) both primary caregivers willing to commit to attending all sessions of the CSI if randomized to the intervention arm of the study; (c) not having participated in a parenting or stress management intervention previously.
Setting
This trial was conducted in Tripoli in North Lebanon. Tripoli is an impoverished region and home to a large community of Syrian refugees (Ismail, Wilson, & Cohen‐Fournier, 2017), 75% of whom were already living in poverty prior to the 2019 economic crisis that continues to devastate the Lebanese economy (Hubbard, 2021).
We had planned to conduct all assessments in the offices of two community‐based organizations (CBOs) with strong reputations in the refugee community. As described below, the COVID‐19 pandemic led us to switch to a remote, phone‐based data collection methodology mid‐way through the study.
The trial was registered prospectively with the ISRCTN registry (ISRCTN22321773).
Changes to the methods after the onset of the study
As our trial was getting underway in the summer of 2019, Lebanon entered an economic collapse from which it has yet to emerge. The local currency was severely devalued, resulting in even more extreme economic hardship for Syrian refugees (Sewell, 2020). Many Syrian families, as well as low‐income Lebanese families, could no longer afford to pay rent, buy food, or seek medical care. In response to the growing financial crisis, protests erupted across the country, blocking roads and restricting movement. The government response, initially peaceful, became increasingly violent. For many Syrians, who had fled from a war that began when peaceful protests were met with violence, the situation evoked fears of being caught in another violent conflict.
We had divided our sample into two waves, and were able to successfully complete implementation of the CSI with Wave 1. However, mid‐way through Wave 2 implementation, the COVID‐19 pandemic struck Lebanon, leading to a national lockdown. All field activities were stopped, and we had to end implementation in Wave 2 after providing six of the nine sessions. By shifting to a remote, phone‐based data collection methodology (Chen et al., 2020), we were nonetheless able to successfully complete all scheduled assessments.
Intervention
The CSI is a nine‐session weekly selective preventive group intervention, co‐facilitated by trained and supervised non‐mental health specialists. Groups were offered separately to women and men, with 10–12 participants per group.
We have described elsewhere the iterative process used to develop the CSI and its culturally integrative content (Miller, Koppenol‐Gonzalez, et al., 2020). Briefly, in sessions 1–4, we focus on caregiver wellbeing and introduce the stress management techniques used throughout the intervention. The various techniques, drawn and adapted from the mindfulness literature (Fung, 2015; Hayes, 2002; Tol et al., 2018), focus on recognizing and disengaging from stress‐inducing thoughts, either by re‐focusing attention on the breath or on a specific activity, such as walking, or by using calming visual imagery. Recognizing the discomfort that might arise in the traditional Muslim communities where the CSI was developed, we avoided the term mindfulness, with its Buddhist origins, instead referring to the stress management activities as “relaxation exercises.” Participants learn a new exercise each week, which they are encouraged to practice at least three times weekly using Arabic audio‐recordings. Participants also learn simple anger management techniques that can be used to quickly lower arousal before reacting to emotionally charged situations. In sessions 5–8, we focus on strengthening parenting in adversity, drawing heavily from the literature on positive parenting and early childhood development (Knerr, Gardner, & Cluver, 2013; Ward, Sanders, Garder, Mikton, & Dawes, 2016). We focus in particular on increasing positive parent–child interactions and on decreasing the use of harsh parenting practices. Table S1 lists session topics and the stress management techniques taught in each session.
Control condition
We employed a waitlist condition as the comparison group. Participants in the WLC arm were invited to participate in CSI groups after the three‐month follow‐up assessment. Unfortunately, due to pandemic‐related lockdowns, we were only able to provide WLC participants with six of the nine sessions.
Facilitators
The 20 facilitators were non‐specialist providers, including 10 Syrians, nine Lebanese, and one Palestinian, with an equal number of women and men. Eligibility criteria for becoming a facilitator are described in Table S2. All prospective facilitators participated in a six‐day training, followed by three on‐site observations and weekly supervision by a social worker experienced in psychosocial interventions in humanitarian settings, who in turn was supervised remotely by a clinical psychologist [KM]. Implementation fidelity was assessed with a fidelity checklist, which was completed by the co‐facilitators following each session.
Recruitment
Participant recruitment was conducted from September 2019 to January 2020, in collaboration with local community‐based organizations (CBOs) in two areas of Tripoli that are home to large Syrian refugee communities. Recruitment entailed community breakfasts, door‐to‐door recruitment, outreach visits to settings where men commonly gather, and word of mouth.
Outcomes
Primary outcome
Parenting
Our primary outcome was the total score at endline on the 24‐item Dimensions of Parenting Scale (DPS), developed for this study. Details on the development of the measure, which was designed for primary caregivers of children ages 3–12, are available in a forthcoming manuscript (Chen et al., 2022). Our decision to develop a new parenting measure stemmed from our need for a questionnaire that could be used by caregivers of index children in a fairly broad age range, ages 3–12. Most parenting measures are designed for narrower age ranges. Using two separate measures for caregivers of younger and older children (e.g., ages 3–6 and 7–12) would have either reduced our statistical power significantly or required an unfeasibly large sample to maintain our power. We did identify two widely used questionnaires that seemed initially to meet our needs; however, in focus groups with community members and local mental health experts, it became apparent that the wording of several questions on both measures, particularly on items concerning harsh parenting, would have been offensive to study participants and would likely have elicited anger and/or non‐responsiveness. Consequently, we were strongly encouraged to not use either measure. We, therefore, made the decision to develop our own parenting measure for this study. Beyond meeting the need of our trial, we believe this new measure addresses an unmet need in the literature for an empirically sound, culturally grounded measure of parenting for use with Arabic‐speaking caregivers. The scale yields a total score, and includes two subscales, parental warmth and responsiveness and harsh parenting. The sub‐scales were derived theoretically, and reflect the two most common targets of parent training interventions, as well as the parenting sessions of the CSI. Internal consistency of the full scale in this study was good (Cronbach's α = .85) and test–retest reliability, assessed in a separate sample of 50 Syrian caregivers, was acceptable (ICC = .67, 95% CI: .49–.79). Psychometrics of subscales are provided below under “secondary outcomes.” Sample items from the DPS can be seen in Table S3.
Secondary outcomes
Parental warmth & responsiveness, and harsh parenting
The DPS includes a 14‐item subscale assessing parental warmth and responsiveness, and a five‐item subscale assessing harsh parenting. Internal consistency for the warmth and responsiveness subscale in this study was good (Cronbach's α = .83), and test–retest reliability was acceptable (ICC = .77, 95% CI: .62–.86). Internal consistency of the harsh parenting subscale was acceptable (Cronbach's α = .72), and test–retest reliability was also acceptable (ICC = .69, 95% CI: .51–81). Sample items can be seen in Table S3.
Parenting knowledge
The DPS includes a separate 15 item subscale assessing knowledge of positive parenting and early childhood development, concepts addressed in the CSI. It is scored separately from the other items on the parenting questionnaire, using a simple True/False answer choice option. Test–retest reliability was relatively lower (ICC = .48, 95% CI .09–.70).
Putative mediators of the CSI on parenting
Caregiver psychological distress
The Kessler Psychological Distress Scale‐10 (K10; Kessler et al., 2002) is a 10‐item measure of psychological distress. It has been used extensively in cross‐cultural clinical and epidemiological research. In this trial, it showed good internal consistency (Cronbach's α = .85) and demonstrated acceptable test–retest reliability in our formative research (ICC = .74, 95% CI: .59–.85).
Caregiver psychosocial wellbeing
The Warwick‐Edinburgh Mental Wellbeing Scale (WEMWBS; Stewart‐Brown & Janmohamed, 2008) is a 14‐item measure of adult psychosocial wellbeing that has been used widely in cross‐cultural mental health research. The internal consistency of the WEMWBS in this study was good (α = .82). Test–retest reliability established in our formative research was also good (ICC = .78, 95% CI: .61–.88).
Caregiver stress
Caregiver stress was assessed with an 8‐item scale developed for this study. The scale showed adequate internal consistency in this trial (Cronbach's α = .76), and previously demonstrated good test–retest reliability (ICC = .86, 95% CI: .75–.92). The measure can be found in Table S4.
Stress management
Stress management was assessed using a 10‐item scale developed for this study. Internal consistency was acceptable (Cronbach's α = .73), and test–retest reliability was also acceptable (ICC = .72, 95% CI: .52–.84). The measure can be found in Table S5.
Questionnaire data were gathered at three time points: baseline, endline, and three‐month follow‐up.
During the baseline assessments for both waves and the endline assessment for Wave 1, questionnaire data were gathered with tablets using the software program Kobo, which allows questionnaires to be completed and uploaded digitally (Harvard Humanitarian Initiative; https://www.kobotoolbox.org/). After we switched to a mobile phone‐based assessment system in response to the pandemic‐related lockdowns, the remaining assessments were conducted remotely, with data entered into Google Sheets, which allowed for live monitoring of the data collection by the research supervisors (Chen et al., 2020). Measures were administered in Arabic to each caregiver individually by trained and supervised research assistants.
Ethical considerations
Ethical approval for this trial was obtained from the University of Balamand in Lebanon. Informed consent was obtained at the baseline assessment, prior to gathering any data. The Research Coordinator provided participants with a consent form in Arabic, read it aloud to ensure full comprehension regardless of literacy level, and addressed any questions or concerns. All participants were able to provide written consent.
Statistical power and sample size
A target of 480 caregivers (240 families) were recruited in two waves. We calculated the sample size based on 90% power at a 5% significance level and an attrition rate of 20%. To account for clustering at the family level, the intra‐class correlation was estimated at 0.15 based on a random intercept regression model with total parenting score as the outcome, CSI group as the intervention and adjusting for baseline total parenting score. The STATA command clustersampsi was used for the sample size calculation, yielding a sample of 432 individuals (216 families). Because we aimed to have 12 participants in each CSI group, we increased the sample size to 480 (240 families). Dividing the sample over two waves, with randomization into CSI and WLC in each wave, yielded a total of 10 CSI groups per wave (five for women and five for men), for a total of 20 CSI groups. More details regarding the target population and parameters are available in the study protocol (Miller et al., 2020).
Randomization and blinding
After completing the baseline assessment, participants were randomized to the CSI or WLC arm. Randomization was at the family level, to ensure that caregivers from the same family were not randomized to different arms of the study. This yielded a total of 240 caregivers (120 families) per arm. A block randomization design was used, using a participatory methodology implemented successfully in our pilot RCT. At baseline assessment, after completing the questionnaires, one caregiver from each family was asked to draw a lollipop out of an opaque bag, filled with an equal number of red and green lollipops to ensure an equal number of CSI and waitlist control participants. After baseline data were completed, a coin toss determined the meaning of each color, CSI or WLC. This process resulted in an equal number of CSI and WLC families in each wave. The purpose of this procedure was to increase community buy‐in to the randomization process, by giving participants an active role in the process.
The lead investigators, trial statisticians and Research Assistants (RAs) remained blind to group assignment throughout the study. The Research Coordinator and Implementation Coordinator were not blind to group assignment, as they were involved in scheduling participants into CSI groups. Given the nature of the study, participants and group facilitators were not blind to group assignment.
Statistical analysis
For all the outcome measures, missing values were analyzed, distribution of scores were tested for normality, and the descriptive statistics for each outcome were calculated for each of the groups (CSI and WLC) at baseline, endline, and three month follow‐up. Initially, a complete case analysis was performed under a missing at random assumption (MAR) where explanatory variables could predict the missing values in the respective outcome variable. These models drop any participant without outcome data at the following time point.
For the primary outcome, Parenting total score, we compared groups at endline, adjusting for baseline score of Parenting total and accounting for hierarchical clustering of caregivers at the family level. Specifically, we fitted a two‐level random intercept linear regression model with the endline score as the dependent variable, and group allocation and baseline score as the independent variables. The scores of the caregivers were defined at level one and families at level two. For the effect of CSI versus WLC on parenting at three‐month follow‐up, we fitted a three‐level random intercept linear regression model, defining the scores at endline and three‐month follow up at level one, caregivers at level two, and families at level three. A time by group interaction was included to allow the effect to differ at each time point. Additionally, we conducted a post‐hoc equivalence test on parenting at follow‐up to inform our conclusions. The equivalence bounds were based on the smallest effect size of interest, which was defined by the expected effect size on which we had based our sample size calculation for this trial (Lakens, 2017). This calculation was based on our pilot study and we considered a difference of at least 2.1 on the mean total Parenting score between the CSI and WLC groups as meaningful.
Secondary and mediator outcomes (Parental Warmth and Responsiveness, Harsh Parenting, Parenting Knowledge, and Caregiver Distress, Caregiver Psychosocial Wellbeing, Stress, Stress Management, respectively) were assessed with a similar methodology to that used with the primary outcome, using generalized linear mixed models. Moreover, because the COVID‐19‐related lockdown led to an abbreviated implementation of the CSI in Wave 2, we fitted the same generalized linear mixed models on all the outcome data of Wave 1 and Wave 2 separately to check for possible differences in intervention effects between the waves.
As noted earlier, our newly developed parenting scale and its two subscales had demonstrated good psychometrics in our formative and pilot studies. Using the baseline data from this study, we examined the concurrent validity and factor structure of the measure (Chen et al., 2022) and re‐ran our mixed models with the validated scale and subscales in a sensitivity analysis.
For the outcomes showing a significant intervention effect a parametric multilevel linear regression approach (ml mediation package in STATA version 15.1 [StataCorp]) was used to estimate the total effect, the natural indirect effects (NIE), and natural direct effects (NDE) of the intervention, taking into account the degree of clustering of caregivers within families. To quantify the magnitude of mediation, we estimated the proportion of the mediated effect (NIE/[NDE + NIE]). All analyses were estimated using bootstrapping (500 replications) to recover the correct SEs for direct and indirect effects. All p‐values were two‐tailed and the significance level was set at α = .05.
Finally, we give descriptive statistics for participants' attendance and facilitator adherence to check the fidelity of implementation.
Results
Participants were 480 caregivers from 240 families (242 caregivers in Wave 1 and 238 caregivers in Wave 2; see Figure 2 for the participant flow chart). The mean age of the caregivers at baseline was M = 37.4 (SD = 8.9). The households consisted of an average of 3.14 adults (SD = 1.8) and 4.2 children (SD = 1.9). Table 1 shows the baseline demographics of the sample.
Figure 2.
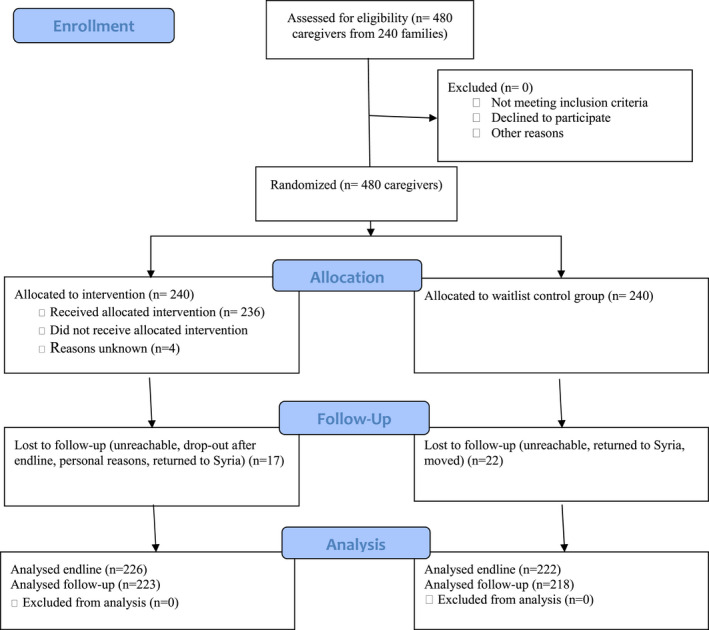
CONSORT flow diagram [Color figure can be viewed at wileyonlinelibrary.com]
Table 1.
Demographics in percentages for the total sample and per intervention group
| Total (n = 480) | WLC (n = 240) | CSI (n = 240) | ||
|---|---|---|---|---|
| Relationship IC | Mother | 48.5 | 49.2 | 47.9 |
| Father | 47.9 | 48.3 | 47.5 | |
| Grandmother | 0.8 | 0.8 | 0.8 | |
| Grandfather | 1.3 | 1.3 | 1.3 | |
| Other relative | 1.3 | 0.4 | 2.1 | |
| Non‐relative guardian | 0.2 | 0.0 | 0.4 | |
| Type home | Apartment | 37.7 | 38.8 | 36.7 |
| House | 35.4 | 36.3 | 34.6 | |
| Tented settlement | 1.9 | 1.7 | 2.1 | |
| Other | 25.0 | 23.3 | 26.7 | |
| Nationality | Syrian | 95.2 | 92.1 | 98.3 |
| Lebanese | 4.2 | 6.7 | 1.7 | |
| Palestinian | 0.6 | 1.3 | 0.0 | |
| Highest education | No schooling | 6.9 | 7.1 | 6.7 |
| Primary | 39.2 | 38.8 | 39.6 | |
| Secondary | 33.5 | 32.9 | 34.1 | |
| High school | 11.5 | 12.5 | 10.4 | |
| Vocational | 4.2 | 4.6 | 3.8 | |
| University | 4.8 | 4.1 | 5.4 | |
| Working | Yes | 22.7 | 22.9 | 22.5 |
| No | 77.3 | 77.1 | 77.5 |
Table 2 shows the means and SDs of all the outcome measures at baseline, endline and follow‐up for the CSI and WLC groups.
Table 2.
Means and standard deviations of the outcomes at the three time points
| Baseline | Endline | Follow‐up | ||
|---|---|---|---|---|
| Parenting (DPS) | WLC | 60.24 (6.92) | 60.32 (7.08) | 60.10 (8.31) |
| CSI | 60.20 (7.19) | 61.11 (7.49) | 61.14 (7.70) | |
| Parental warmth and sensitivity (DPS) | WLC | 36.18 (4.54) | 36.03 (4.59) | 35.55 (5.58) |
| CSI | 36.07 (4.86) | 36.10 (5.15) | 35.97 (5.27) | |
| Harsh parenting (DPS) | WLC | 7.57 (2.13) | 7.49 (2.23) | 7.48 (2.26) |
| CSI | 7.61 (2.20) | 7.15 (1.99) | 7.13 (2.01) | |
| Parenting knowledge (DPS) | WLC | 12.29 (1.60) | 12.67 (1.55) | 12.86 (1.46) |
| CSI | 12.11 (1.75) | 13.49 (1.38) | 13.45 (1.37) | |
| Stress (Caregiver Stress Scale) | WLC | 20.29 (3.28) | 19.91 (3.53) | 19.97 (3.67) |
| CSI | 19.89 (3.29) | 19.41 (3.82) | 20.04 (3.57) | |
| Distress (K10) | WLC | 33.10 (8.34) | 33.84 (8.11) | 33.36 (7.56) |
| CSI | 33.36 (7.59) | 31.25 (8.66) | 31.92 (8.04) | |
|
Psychosocial wellbeing WEMWBS |
WLC | 47.37 (8.22) | 46.96 (8.65) | 45.68 (8.83) |
| CSI | 47.70 (8.62) | 48.39 (8.83) | 46.12 (8.60) | |
|
Stress management Stress Management Scale |
WLC | 20.97 (2.94) | 20.38 (2.88) | 20.58 (2.90) |
| CSI | 20.59 (3.15) | 20.40 (3.07) | 20.32 (3.02) |
In the full sample, the effect of the CSI on the Parenting total score at endline was not statistically significant (see Table 3). The difference between‐group at follow‐up was larger than at endline but did not reach significance either (M diff = 1.10, 95% CI = −0.02, 2.21, p = .054, Cohen's d = 0.15). The post‐hoc equivalence test using the TOST procedure (Lakens, 2017) given the boundaries ΔL = ‐2.1 and ΔU = 2.1 was not significant, t(434.76) = −1.389, (p = .08). Examination of the results for Wave 1 and Wave 2 separately shows that the effect of the CSI at follow‐up was larger, and statistically significant in Wave 1 (those who received the full intervention) and non‐significant in Wave 2. The secondary outcome Harsh Parenting showed a significant effect at endline as well as follow‐up in the full sample. In Wave 1, this effect was only significant at endline. Parenting Knowledge also showed a significant effect both at endline and follow‐up, in the full sample and in both Waves separately. Parental Warmth and Responsiveness did not show significant changes. The putative mediator outcome Caregiver Distress showed a significant effect at both endline and follow‐up in the full sample, as it did in Wave 1, but only at endline in Wave 2. The remaining outcomes Psychosocial Wellbeing, Stress, and Stress Management did not show significant changes.
Table 3.
Mean difference and 95% confidence interval, significance, and effect size of all measures at endline and follow‐up
| Mean difference (95% CI) | Cohen's d (95% CI) | ||||
|---|---|---|---|---|---|
| Endline | Follow‐up | Endline | Follow‐up | ||
| Parenting | Full sample | 0.83 (−0.23,1.89) | 1.10 (−0.02,2.21) | 0.11 (−0.03,0.26) | 0.15 (−0.00,0.30) |
| Wave 1 | 1.31 (−0.08,2.70) | 1.76 (0.20,3.32)* | 0.20 (−0.01,0.41) | 0.25 (0.03,0.48) | |
| Wave 2 | 0.28 (−1.26,1.83) | 0.41 (−1.17,1.99) | 0.04 (−0.16,0.24) | 0.05 (−0.15,0.25) | |
| Parental warmth and responsiveness | Full sample | 0.16 (−0.58,0.91) | 0.56 (−0.24,1.35) | 0.03 (−0.12,0.19) | 0.11 (−0.05,0.27) |
| Wave 1 | 0.41 (−0.56,1.37) | 0.81 (−0.30,1.93) | 0.09 (−0.13,0.31) | 0.18 (−0.07,0.42) | |
| Wave 2 | −0.13 (−1.23,0.98) | 0.29 (−0.83,1.42) | −0.02 (−0.24,0.19) | 0.06 (−0.16,0.27) | |
| Harsh parenting | Full sample | −0.37 (−0.70,‐0.04)* | −0.42 (−0.77,‐0.07)* | −0.17 (−0.33,‐0.02) | −0.19 (−0.36,‐0.03) |
| Wave 1 | −0.49 (−0.93,‐0.06)* | −0.45 (−0.94,0.04) | −0.25 (−0.47,‐0.03) | −0.22 (−0.46,0.02) | |
| Wave 2 | −0.24 (−0.73,0.26) | −0.38 (−0.88,0.11) | −0.11 (−0.33,0.11) | −0.17 (−0.39,0.05) | |
| Parenting knowledge | Full sample | 0.92 (0.66,1.18)*** | 0.81 (0.51,1.10)*** | 0.63 (0.45,0.80) | 0.50 (0.32,0.69) |
| Wave 1 | 0.94 (0.59,1.29)*** | 1.01 (0.60,1.42)*** | 0.64 (0.40,0.87) | 0.62 (0.37,0.87) | |
| Wave 2 | 0.88 (0.52,1.24)*** | 0.60 (0.17,1.03)** | 0.61 (0.36,0.87) | 0.39 (0.11,0.66) | |
| Psychological distress | Full sample | −2.76 (−4.19,‐1.33)*** | −1.84 (−3.18,‐0.51)** | −0.33 (−0.50,‐0.16) | −0.23 (−0.39,‐0.06) |
| Wave 1 | −2.24 (−4.29,‐0.19)* | −1.98 (−3.83,‐0.13)* | −0.25 (−0.48,‐0.02) | −0.24 (−0.46,‐0.02) | |
| Wave 2 | −3.15 (−5.02,‐1.28)*** | −1.71 (−3.60,0.18) | −0.41 (−0.66,‐0.17) | −0.22 (−0.47,0.02) | |
| Psychosocial wellbeing | Full sample | 1.22 (−0.17,2.61) | 0.28 (−1.13,1.70) | 0.14 (−0.02,0.30) | 0.03 (−0.13,0.20) |
| Wave 1 | 0.93 (−0.94,2.81) | −0.52 (−2.52,1.48) | 0.11 (−0.11,0.32) | −0.06 (−0.29,0.17) | |
| Wave 2 | 1.37 (−0.53,3.26) | 1.07 (−0.89,3.04) | 0.16 (−0.06,0.39) | 0.13 (−0.11,0.36) | |
| Stress | Full sample | −0.32 (−0.93,0.29) | 0.35 (−0.23,0.93) | −0.09 (−0.25,0.08) | 0.10 (−0.06,0.26) |
| Wave 1 | −0.10 (−0.93,0.74) | 0.43 (−0.39,1.26) | −0.03 (−0.24,0.19) | 0.12 (−0.11,0.34) | |
| Wave 2 | −0.58 (−1.43,0.27) | 0.28 (−0.52,1.07) | −0.17 (−0.42,0.08) | 0.08 (−0.16,0.33) | |
| Stress management | Full sample | 0.19 (−0.35,0.73) | 0.15 (−0.44,0.75) | 0.06 (−0.12,0.24) | 0.05 (−0.15,0.25) |
| Wave 1 | 0.20 (−0.55,0.96) | −0.02 (−0.88,0.83) | 0.07 (−0.18,0.32) | −0.01 (−0.29,0.27) | |
| Wave 2 | 0.21 (−0.55,0.96) | 0.34 (−0.49,1.17) | 0.07 (−0.19,0.33) | 0.12 (−0.16,0.39) | |
*p < .05, **p < .01, ***p < .001.
The sensitivity analysis on the validated Parenting scale and subscales showed very similar results to the original measure, with a larger but non‐significant change in Parenting total score at follow‐up (M diff = 0.97, 95% CI = −0.04, 1.97, p = .059, Cohen's d = 0.14), and a significant effect on Harsh Parenting at endline (M diff = −0.50, 95% CI = −0.91, −0.09 p = .017, Cohen's d = 0.18), though not at follow‐up (M diff = −0.31, 95% CI = −0.76, 0.14, p = .172). Both effect sizes were larger in Wave 1 compared to Wave 2, and non‐significant in Wave 2.
We first tested the effect of the CSI intervention on each of the continuous multiple mediators, with the use of random intercept linear regression models taking into account that parents were clustered within families. We chose a priori a p‐value of lower than 0.15 to select the appropriate mediators to include in our final mediation analysis. We then tested independence between our multiple mediators by examining partial correlations between the mediators after accounting for treatment allocation. Two mediators emerged from this two‐step procedure who were independent from each other: Caregiver Distress (p < .001) and Caregiver Psychosocial Wellbeing (p = 0.084). Figure 3A presents the total, direct and indirect effects of the CSI on Harsh Parenting via Caregiver Distress and Figure 3B via Caregiver Psychosocial Wellbeing. All were significant (p < .05). The proportion of the effect between the CSI and Harsh Parenting mediated by Caregiver Distress was 29% and the proportion mediated by Caregiver Psychosocial Wellbeing was 7.8%.
Figure 3.
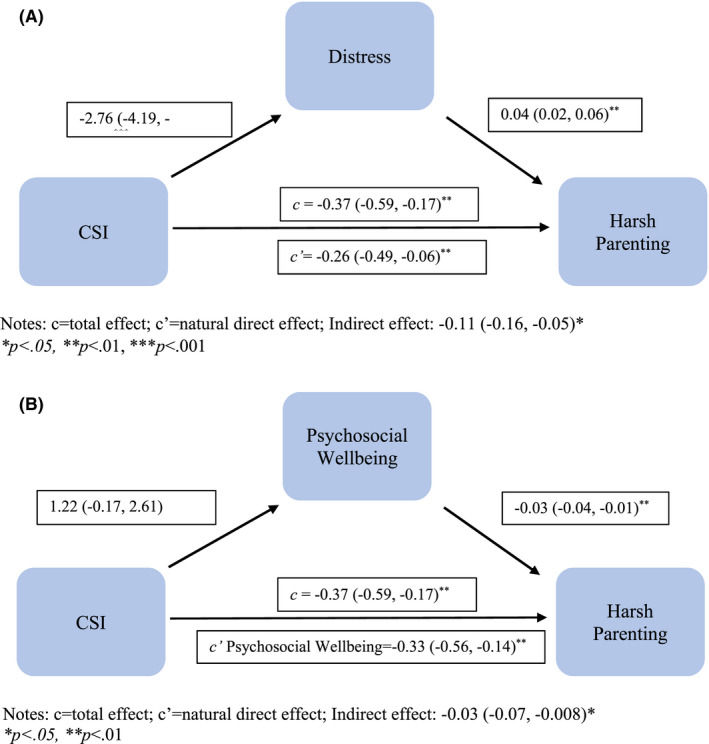
Mediating pathway of the effect of CSI intervention on harsh parenting via (A) distress, (B) psychosocial wellbeing, 95% confidence intervals in parentheses. Notes: c = total effect; c' = natural direct effect; (A) Indirect effect: −0.11 (−0.16, −0.05)*. *p < .05, **p < .01, ***p < .001. (B) Indirect effect: −0.03 (−0.07, −0.008)*. *p < .05, **p < .01 [Color figure can be viewed at wileyonlinelibrary.com]
Attendance in Wave 1 averaged 87% (n = 112), and 87% in Wave 2 (n = 111). Fidelity of implementation, measured as the percentage of planned activities that were actually implemented across all sessions, was high, averaging 98.5% (SD = 1.11%) across CSI groups (98.6% in Wave 1 and 98.4% in Wave 2).
We did not receive any reports of harm as a result of participation in this study.
Discussion
This study examined the effectiveness of the Caregiver Support Intervention among Syrian refugees in North Lebanon. In contrast to conventional parenting programs that prioritize the acquisition of knowledge and skills, the CSI has a dual emphasis on strengthening caregiver wellbeing and increasing competence in positive parenting. The CSI led to a non‐significant improvement in parenting at the three‐month follow‐up. The post‐hoc equivalence test was not significant, meaning that we cannot reject the hypothesis that in the population from which our sample was drawn, the CSI has an effect on parenting large enough to be considered meaningful. Consequently, we do not seem to have sufficient data to draw firm conclusions about the effectiveness of the CSI on parenting, possibly because the trial was conducted in a context of extreme adversity which adversely impacted the implementation of the intervention in half of the sample. The intervention did lead to significant reductions in harsh parenting and caregiver distress at endline and follow‐up, as well as for parenting at follow‐up among those that received the full intervention.
The significant reduction in caregiver distress is consistent with the findings of our pilot study, where we found an even more pronounced reduction of 20% in distress among CSI participants. Although not designed as a clinical intervention, the impact of the CSI on distress suggests that the intervention can be helpful even to highly distressed caregivers.
Consistent with the underlying theoretical model guiding the intervention, the beneficial effect of the CSI on harsh parenting was partially mediated by a reduction in caregiver distress and, to a lesser extent, an improvement in psychosocial wellbeing. This finding of partial mediation is consistent with evidence of the critical role of caregiver stress and distress in mediating compromised parenting in settings of adversity (Eltanamly et al., 2019). Our findings suggest that, as caregivers become less distressed, they become better able to act upon pre‐existing as well as newly acquired parenting knowledge and skills. In a separate paper based on focus group discussions with CSI participants from this trial, caregivers spoke consistently about how their improved wellbeing (i.e., feeling less distressed and more relaxed) allowed them to interact more warmly with their children, and to make greater use of positive, non‐violent behavior management strategies—including those they already knew and others learned during the intervention (Miller et al., unpublished data). These findings imply that parenting interventions for caregivers in humanitarian settings can maximize their effects by substantively addressing caregiver wellbeing, rather than focusing primarily on the acquisition of parenting knowledge and skills. Indeed, a shift in this direction is already underway, and can be seen in the growing number of parenting interventions that have incorporated a focus on caregiver wellbeing in their curricula (Jenson et al., 2021; Sim, Bowes, Maignant, Magber, & Gardner, 2020).
Interestingly, our findings suggest that both foci—caregiver wellbeing and positive parenting—are important. When we analyzed our findings separately by wave, we found that Wave 1 participants, who received the full intervention, showed lower psychological distress, improved overall parenting, and reduced harsh parenting. In contrast, Wave 2 participants received all the wellbeing sessions but only half of the parenting sessions; correspondingly, they showed a significant reduction in distress, but no change in parenting, or in harsh parenting specifically. Improved wellbeing appears to free caregivers up to parent more effectively, but there is a clear benefit to also learning methods of positive discipline and strategies for increasing positive parent–child interactions.
Finally, we found a significant increase in parenting knowledge that was maintained over time; however, the low test–retest reliability of our parenting knowledge subscale suggests caution when interpreting this effect. We did not find an effect of the CSI on parental warmth and responsiveness, caregiver stress, stress management, or psychosocial wellbeing.
There are several points to consider when making sense of the findings of this trial. First, this study was conducted in a context of multiple and extreme adversities, including an economic crisis that has driven Syrian refugees further into poverty; political unrest that evoked distressing memories of war, and a fear among Syrians of becoming caught up in another violent conflict; and the outbreak of the COVID‐19 pandemic, followed by a lockdown that stopped all field activities and led to half our sample receiving only part of the intervention. Stress levels were extremely high throughout the trial, and the majority of families were confined in crowded, substandard living conditions for extended periods of time.
Such conditions may explain why our effects were modest, and why the CSI did not significantly improve overall parenting, reduce stress or improve caregivers' capacity for stress management. In our pilot RCT of the CSI, which was conducted prior to the economic crisis, social unrest, and COVID‐19 pandemic, we found medium to large within‐group effects on all study outcomes in the CSI arm and no significant changes on any outcomes in the control arm (Miller, Ghalayini, et al., 2020). It seems likely that in this trial, we encountered the limits of a stand‐alone preventive psychosocial intervention in a context of extreme adversity. Our focus on stress management may simply have been inadequate in the face of the intense stressors that impacted participants throughout the trial. In conditions of extreme adversity, psychosocial interventions should clearly be coupled with other types of support that address basic needs, from nutrition and housing to economic support and healthcare, as well as clinical interventions for severely distressed individuals—a key point made by the Interagency Standing Committee in its guidelines for mental health and psychosocial support in humanitarian settings (Inter Agency Standing Committee, 2007). The finding that participants did benefit from the CSI in this highly stressful context suggests that psychosocial interventions do have an important role to play even in settings of extreme adversity. However, the marked difference in findings between our pilot RCT and this trial underscores that as adversity increases, so too does the importance of coupling psychosocial programming with interventions that address basic needs.
The successful recruitment and retention of male caregivers was a significant achievement of this trial. Panter‐Brick et al. (2014) have discussed the perils of failing to include men in parenting interventions, an unfortunately common practice. Our approach was threefold: we scheduled intervention sessions and assessments on days and at times that did not conflict with income‐generation opportunities; we revised the program content substantively based on feedback from men during the iterative process of intervention development (Miller et al., 2021), and we framed the intervention as supportive sessions for men, rather than focusing on its parenting content.
Another achievement of this trial was the development of a successful mobile phone‐based assessment methodology (Chen et al., 2020). Due to the lockdown and travel restrictions, our team was dispersed across four countries. Nonetheless, we were able to reach greater than 90% of participants during each of the three phone‐based assessments.
Finally, when we reran the primary analyses on the recently validated version of our parenting measure, our findings remained largely consistent with the results from the original measure, with the exception of an attenuation of the effect on harsh parenting at follow‐up.
Limitations
There are several limitations to the present study. Our decision to prioritize the recruitment of two‐caregiver families meant that we excluded families with a single caregiver. The latter may represent a particularly at‐risk group for caregiver stress and problematic parenting, and we recognize the importance of including single‐caregiver families in future evaluations of the CSI. Our priority in this study was to first establish whether we could successfully recruit and retain both male and female caregivers in the intervention, despite the widely held perception that men will not participate in parent‐focused interventions (Panter‐Brick et al., 2014). We hope that our successful involvement of men in this trial will help challenge this erroneous perception.
This study was adversely impacted by the COVID‐19 pandemic and subsequent lockdowns, as well as a severe economic crisis and widespread social unrest. As a result of the lockdowns, we were unable to fully implement the CSI with half of the participants randomized to the intervention arm. The stronger results from Wave 1, which received the full intervention, are underpowered, as they are based on only half the sample. This raises the possibility that they understate the actual potential of the CSI and suggests the importance of a replication study conducted under less adverse circumstances.
Our experience raises questions regarding the viability and wisdom of conducting rigorous evaluation studies in settings of extreme adversity that may adversely impact trial implementation and lead to an underestimation of an intervention's true potential. Although an in‐depth examination of this critical issue is beyond the scope of this paper, in our case we were confronted by a series of so‐called “black swan” events that began just as the trial was getting underway. Had we known that Lebanon's economic crisis would be followed by a global pandemic that would curtail implementation of the intervention in Wave 2 and cause extreme distress throughout much of the trial, we might well have chosen to delay the study. Unfortunately, the reality of working in humanitarian settings is that conditions often worsen rapidly and unpredictably, making rigorous research in such settings inherently precarious. This suggests the importance of anticipating, to the extent possible, how conditions may worsen during the course of a trial, and developing alternative methods that may allow for successful completion despite changing circumstances. In our study, for example, it would have been advantageous to have developed our phone‐based data collection methodology in advance, rather than waiting until conditions necessitated its rapid development on an extremely short timeline. We might have also explored ways of implementing the CSI remotely, something we did not have time to develop in the immediate aftermath of the lockdown that brought Wave 2 implementation to a stop. Ultimately, however, we recognize that there is simply no way to fully anticipate and prepare for the range of adverse situations that may arise in the course of trials conducted in humanitarian settings. This reality underscores the limitations of any single trial conducted in a setting of adversity, and the importance of conducting replication studies in conditions that may better allow for the identification of intervention effects.
Supporting information
Table S1. CSI sessions, modules, and stress management methods.
Table S2. Eligibility criteria for becoming a CSI facilitator.
Table S3. Sample items from the dimensions of parenting scale.
Table S4. Caregiver stress Questionnaire.
Table S5. Stress management Questionnaire.
Acknowledgements
The authors wish to thank the families who participated in this trial, the organizations with which they partnered, the group facilitators and research assistants who worked under extremely challenging circumstances, and the War Child Lebanon team. The authors also wish to thank Prof. Mark Tomlinson, Dr. Andrew Rasmussen, Dr. Felicity Brown, and Dr. Eva Smallegange for their invaluable contributions to this project. This study was funded by grants from the ELMA Creative Foundations, the Open Societies Foundation, and the Fred Foundation. The authors have declared that they have no competing or potential conflicts of interest.
Key points.
In contrast to conventional parenting interventions in humanitarian settings, which prioritize the acquisition of knowledge and skills, the Caregiver Support Intervention has a substantive focus on strengthening caregiver wellbeing, a key mediator of parenting in settings of adversity.
Despite being conducted during the COVID‐19 pandemic, a severe economic crisis, and widespread social unrest, the CSI reduced caregiver distress and harsh parenting, effects that were seen at baseline and maintained at follow‐up. Among participants receiving the full intervention (i.e. the sub‐sample not interrupted due to COVID‐19), we saw a significant 3‐month effect on overall parenting.
Changes in caregiver psychological wellbeing partially mediated the effect of the CSI on harsh parenting. This underscores the importance of addressing caregiver wellbeing as a pathway to reducing harsh parenting.
We demonstrated the feasibility of recruiting and retaining male caregivers in a parenting intervention.
Conflict of interest statement: No conflicts declared.
Contributor Information
Kenneth E. Miller, Email: ken.miller@kennethemiller.com.
Mark J.D. Jordans, Email: mark.jordans@warchild.nl.
References
- Bryant, R. , Edwards, B. , Creamer, M. , O'Donnell, M. , Forbes, D. , Felmingham, K. , … Hadzi‐Pavlovic, D. (2018). The effect of post‐traumatic stress disorder on refugees' parenting and their children's mental health: A cohort study. The Lancet Public Health, 3, e249–e258. [DOI] [PubMed] [Google Scholar]
- Chen, A. , Koppenol‐Gonzalez, G.V. , Bakolis, I. , Arnous, M. , Tossyeh, F. , Al‐Ogaily, D. , Jordans, M.J.D. , & Miller, K.E. (2022). Dimensions of Parenting Scale: a culturally grounded measure of parenting in adversity (Manuscript in preparation).
- Chen, A. , Tossyeh, F. , Arnous, M. , Saleh, A. , El Hassan, A. , Sade, J. , & Miller, K.E. (2020). Phone‐based data collection in a refugee community under COVID‐19 lockdown. The Lancet Psychiatry, 7. 10.1016/S2215-0366(20)30189-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eltanamly, H. , Leijten, P. , Jak, S. , & Overbeek, G. (2019). Parenting in times of war: A meta‐analysis and qualitative synthesis of war exposure, parenting, and child adjustment. Trauma, Violence & Abuse, 22, 147–160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fung, K. (2015). Acceptance and commitment therapy: Western adoption of Buddhist tenets? Transcultural Psychiatry, 52, 561–576. [DOI] [PubMed] [Google Scholar]
- Hayes, S.C. (2002). Buddhism and acceptance and commitment therapy. Cognitive and Behavioral Practice, 9, 58–66. [Google Scholar]
- Hubbard, B. (2021, July 5). As Lebanon's crisis deepens, lines for fuel grow, and food and medicine are scarce. New York Times. Available from: https://www.nytimes.com/2021/07/05/world/middleeast/lebanon‐economic‐crisis.html
- Inter Agency Standing Committee . (2007). IASC guidelines on mental health and psychosocial support in emergency settings. Geneva, Switzerland: World Health Organization. 10.1037/e518422011-002 [DOI] [Google Scholar]
- Ismail, K. , Wilson, C. , & Cohen‐Fournier, N. (2017). Syrian refugees in Tripoli, Lebanon. Refugees in towns case study series. Medford, MA: Feinstein International Center, Tufts University. [Google Scholar]
- Jenson, S.K.G. , Placencio‐Castro, M. , Murray, S.M. , Brennan, R. , Goshev, S. , Farrar, J. , … Betancourt, T.S. (2021). Effect of a home visiting parenting program to promote early childhood development and prevent violence: A cluster randomized trial in Rwanda. BMJ Global Health, 6, e003508. 10.1136/bmjgh-2020-003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler, R.C. , Andrews, G. , Colpe, L.J. , Hiripi, E. , Mroczek, D.K. , Normand, S.L.T. , … Zaslavsky, A.M. (2002). Short screening scales to monitor population prevalences and trends in non‐specific psychological distress. Psychological Medicine, 32, 959–976. [DOI] [PubMed] [Google Scholar]
- Knerr, W. , Gardner, F. , & Cluver, L. (2013). Improving positive parenting skills and reducing harsh and abusive parenting in low‐ and middle‐income countries: A systematic review. Prevention Science, 14, 352–363. [DOI] [PubMed] [Google Scholar]
- Lakens, D. (2017). Equivalence tests: A practical primer for t‐tests, correlations, and meta‐analyses (package ‘TOSTER’ v.0.4.0) [computer software]. The Comprehensive R Archive Network. Available from: https://cran.r‐project.org/web/packages/TOSTER/TOSTER.pdf [DOI] [PMC free article] [PubMed]
- Miller, K.E. , Arnous, M. , Saade, J. , Tossyeh, F. , Koppenol‐Gonzalez, G.V. , el Hassan, A. , & Jordans, M.J.D. (unpublished). Worlds of pain: the impact of extreme adversity on a psychosocial intervention for Syrian refugee caregivers in Lebanon. Manuscript submitted for publication.
- Miller, K.E. , Arnous, M. , Tossyeh, F. , Chen, A. , Bakolis, I. , Koppenol‐Gonzalez, G.V. , … Jordans, M.J.D. (2020). Protocol for a randomized control trial of the caregiver support intervention with Syrian refugees in Lebanon. Trials, 21, 277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller, K.E. , Ghalayini, H. , Arnous, M. , Tossyeh, F. , van den Broek, M. , Koppenol‐Gonzalez, G.V. , & Jordans, M.J.D. (2020). Strengthening parenting in conflict‐affected communities: Development of the caregiver support intervention. Global Mental Health, 7, e14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller, K.E. , & Jordans, M.J.D. (2016). Determinants of Children's mental health in war torn settings: Translating research into action. Current Psychiatry Reports, 18, 6–11. [DOI] [PubMed] [Google Scholar]
- Miller, K.E. , Jordans, M.J.D. , Tol, W.A. , & Galappatti, A. (2021). A call for greater conceptual clarity in the field of mental health and psychosocial support in humanitarian settings. Epidemiology and Psychiatric Sciences, 30, E5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller, K.E. , Koppenol‐Gonzalez, G.V. , Arnous, M. , Tossyeh, F. , Chen, A. , Nahas, N. , & Jordans, M.J.D. (2020). Supporting Syrian families displaced by armed conflict: A pilot randomized controlled trial of the caregiver support intervention. Child Abuse and Neglect, 106, 104512. [DOI] [PubMed] [Google Scholar]
- Panter‐Brick, C. , Burgess, A. , Eggerman, M. , McAllister, F. , Pruett, K. , & Leckman, J.F. (2014). Practitioner review: Engaging fathers – recommendations for a game change in parenting interventions based on a systematic review of the global evidence. Journal of Child Psychology and Psychiatry, and Allied Disciplines, 55, 1187–1212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Panter‐Brick, C. , Grimon, M.P. , & Eggerman, M. (2014). Caregiver – child mental health: A prospective study in conflict and refugee settings. Journal of Child Psychology and Psychiatry, and Allied Disciplines, 55, 313–327. [DOI] [PubMed] [Google Scholar]
- Puffer, E.S. , Annan, J. , Sim, A.L. , Salhi, C. , & Betancourt, T.S. (2017). The impact of a family skills training intervention among Burmese migrant families in Thailand: A randomized controlled trial. PLoS One, 12, e0172611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sewell, A. (2020, January 9). Lebanon's financial crisis hits Syrian refugees hard. The New Humanitarian. Available from: https://www.thenewhumanitarian.org/news‐feature/2020/1/9/Lebanon‐financial‐crisis‐Syrian‐refugees
- Sim, A. , Bowes, L. , & Gardner, F. (2018). Modeling the effects of war exposure and daily stressors on maternal mental health, parenting, and child psychosocial adjustment: A cross‐sectional study with Syrian refugees in Lebanon. Global Mental Health, 5, 1–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sim, A. , Bowes, L. , Maignant, S. , Magber, S. , & Gardner, F. (2020). Acceptability and preliminary outcomes of a parenting intervention for Syrian refugees. Research on Social Work Practice, 31, 14–25. [Google Scholar]
- Sim, A. , Fazel, M. , Bowes, L. , & Gardner, F. (2018). Pathways linking war and displacement to parenting and child adjustment: A qualitative study with Syrian refugees in Lebanon. Social Science and Medicine, 200, 19–26. [DOI] [PubMed] [Google Scholar]
- Singla, D.R. , Kumbakumba, E. , & Aboud, F.E. (2015). Effects of a parenting intervention to address maternal psychological wellbeing and child development and growth in rural Uganda: A community‐based, cluster‐randomised trial. The Lancet Global Health, 3, e458–e469. [DOI] [PubMed] [Google Scholar]
- Stewart‐Brown, S. , & Janmohamed, K. (2008). Warwick‐Edinburgh Mental Well‐being Scale: User Guide, Version 1. Available from: http://www.ocagingservicescollaborative.org/wp‐content/uploads/2014/07/WEMWBS‐User‐Guide‐Version‐1‐June‐2008.pdf
- Tol, W.A. , Augustinavicius, J. , Carswell, K. , Brown, F.L. , Adaku, A. , Leku, M.R. , … van Ommeren, M. (2018). Translation, adaptation, and pilot of a guided self‐help intervention to reduce psychological distress in south Sudanese refugees in Uganda. Global Mental Health, 5, e25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ward, C. , Sanders, M. , Garder, F. , Mikton, C. , & Dawes, A. (2016). Preventing child maltreatment in low‐ and middle‐income countries. Parent support programs have the potential to buffer the effects of poverty. Child Abuse and Neglect, 54, 97–107. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1. CSI sessions, modules, and stress management methods.
Table S2. Eligibility criteria for becoming a CSI facilitator.
Table S3. Sample items from the dimensions of parenting scale.
Table S4. Caregiver stress Questionnaire.
Table S5. Stress management Questionnaire.


