Abstract
Objectives
To identify and examine the reported effectiveness of education programs for health professionals on frailty.
Methods
A systematic review was conducted of articles published up to June 2021, examining the evaluation of frailty training or education programs targeting health professionals/students. The participant demographics, program content and structure, effectiveness assessment methodology and outcomes, as well as participant feedback, were recorded with narrative synthesis of results.
Results
There were nine programs that have evaluated training of health professionals in frailty. These programs varied with respect to intensity, duration, and delivery modality, and targeted a range of health professionals and students. The programs were well‐received and found to be effective in increasing frailty knowledge and self‐perceived competence in frailty assessment. Common features of successful programs included having multidisciplinary participants, delivering a clinically tailored program and using flexible teaching modalities. Of note, many programs assessed self‐perceived efficacy rather than objective changes in patient outcomes.
Conclusions
Despite increasing attention on frailty in clinical practice, this systematic review found that there continues to be limited reporting of frailty training programs.
Keywords: curriculum, education, frailty, interprofessional education, medical, teaching
Policy Impact.
This study has found that frailty training programs are feasible and perceived by healthcare professionals to be effective in building knowledge and skills.
1. INTRODUCTION
Frailty is highly prevalent in both community and hospital settings and associated with significant financial and resource costs. 1 , 2 , 3 Frailty prevention and intervention programs have demonstrated improved quality of life, reduced hospitalization, and decreased mortality rates. 4 , 5 The World Health Organization's ‘Global strategy and action plan on ageing and health’ states that all healthcare professionals should receive training to ensure that the needs of the population are being met. 6 Yet many health care professionals are still unaware of the concept of frailty or do not routinely use it in their clinical practice. 7 , 8 , 9 , 10 , 11 , 12 Studies recruiting a wide range of health care professionals demonstrate difficulties defining frailty 12 , 13 and poor awareness of frailty screening tools. 14 Misconceptions, such as believing that frailty equates to ageing or is not modifiable, are common. 10 , 12 Consequently, frailty assessment and management are often neglected in clinical practice. 10 , 11 Current research highlights that healthcare professionals not only need but also want further training in frailty. 7 , 8 , 9 , 12
Universities and healthcare organizations have responded to the call for improved knowledge at the clinical frontline by developing and implementing frailty training programs, workshops, and other educational activities. 15 A systematic review of the academic and grey literature conducted in 2017 did not find any studies reporting on the effectiveness of these frailty training programs, 16 however, many were identified as being developed. Here, 5 years later, we aimed to examine the effectiveness of frailty training programs for healthcare professionals and to detail the positive and negative participant feedback from these programs.
2. METHODS
This systematic review was conducted in accordance with the preferred reporting items for systematic reviews and meta‐analyses (PRISMA) statement recommendations; however, there was no review protocol generated and it was not preregistered. 17 PubMed, Embase, PsycINFO, and CINAHL were searched from inception to 30 June 2021 using the terms: “frailty” and “education” or “training” or “teaching” or “program” and “healthcare” or “health professional” or “clinician” or “nursing” or “medical” or “physician” or “allied health” or “dietetics” or “occupational therapy” or “physiotherapy” or “social work”. Search and screening at title, abstract, and full text was performed independently by two authors (NW, EP) and references of selected articles were searched for additional studies. Any divergence was resolved between all authors.
Broad inclusion criteria were used to maximize the number of studies from which data could be extracted. Studies of any type published in English that reported on an education program, workshop or module that named frailty as a primary focus, directed at any type of health professional/student working in any setting and which carried out an evaluation of that program/workshop/module, were included. Studies were excluded if the program only focussed on ageing/geriatric care or geriatric assessment and did not specifically address frailty. Studies reporting on programs directed at consumers or carers were excluded. Articles describing programs/workshops/modules without any assessment of their quality or efficacy were excluded (noted in Table 1).
TABLE 1.
Frailty education programs for health care professionals (gray literature search)
| United Kingdom | |
| Frailty Hub, British Geriatric Society | https://www.bgs.org.uk/resources/frailty‐hub‐education‐and‐training |
| Frailty360 | https://www.frailtytoolkit.org/frailty360/ |
| FACET | https://waru.org.uk/cms/projects/facet/facet‐mooc/ |
| NICE | https://stpsupport.nice.org.uk/frailty/index.html |
| Europe | |
| European innovation partnership on active and healthy ageing—training program on frailty for physicians | https://ec.europa.eu/eip/ageing/commitments‐tracker/a3/training‐program‐health‐care‐professionals‐detecting‐pre‐frailty‐and_en.html |
| Frailty Education Program—Ireland | https://tilda.tcd.ie/ppi/frailty‐education/ |
| Canada | |
| Canadian Frailty Network | http://cfn‐nce.ca |
| McMaster University—geriatric certificate program, frailty e‐module | http://geriatriccp.ca |
| Discipline specific | |
| Physiotherapy—Physioplus | https://members.physio‐pedia.com/learn/introduction‐to‐frailty/ |
Two authors (NW, EP) independently performed quality assessment of the studies and extracted data, with discussion between all authors if there was a disagreement about that data. The Joanna Briggs Institute critical appraisal (cross sectional and qualitative research) tools were utilised, which detail design, conduct, and analysis of the methodological quality of studies and allow comparison and interpretation by providing a score (the maximum score indicating well‐conducted research). 18 Data variables included participant demographics, program content, structure and location, effectiveness assessment methodology and outcomes, and participant feedback. When frailty education was included within broader geriatric training, only data relating to frailty was noted. Narrative synthesis of the data was performed, with no meta‐analysis planned due to likely heterogeneous outcome measures.
3. RESULTS
Database searches yielded 1277 nonduplicated studies. Following title and abstract screening and full‐text review, 10 studies, all published between 2018 to 2021, were included (Figure 1). These studies reported on the effectiveness of nine frailty training programs (Table 2) conducted in five Western countries. 19 , 20 , 21 , 22 , 23 , 24 , 25 , 26 , 27 Quality assessment was moderate with a mean of 5.9/8 for cross‐sectional studies and 8/11 for qualitative studies (Table 3).
FIGURE 1.
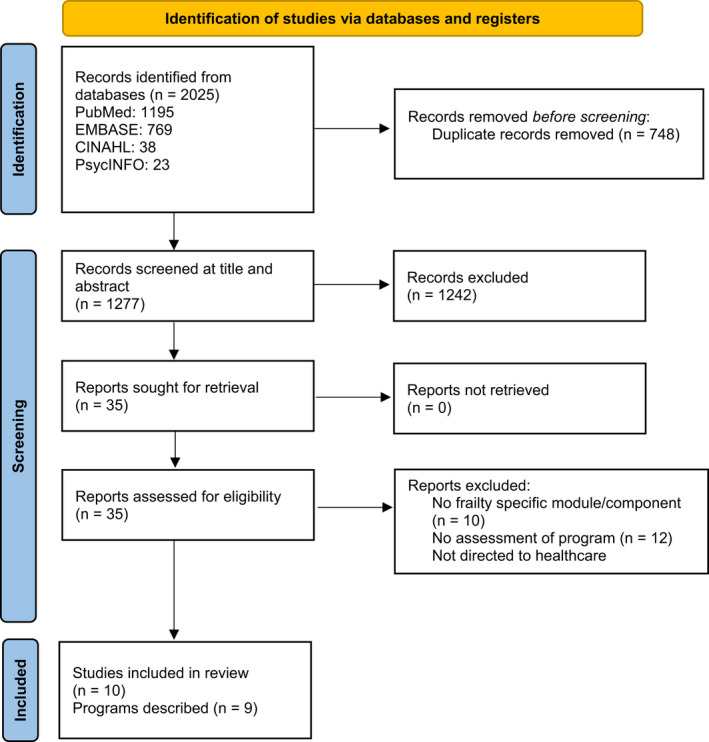
PRISMA flow chart: Frailty education programs for health care professionals
TABLE 2.
Evaluation of frailty education programs
| Author, date | Location | Participants | Frailty training program | Assessment of effectiveness | ||
|---|---|---|---|---|---|---|
| Structure | Content | Methodology | Results | |||
| Aijaz et al. 2018 26 | Emergency Departments, UK | “all staff groups” | Frailty education session | Frailty identification and assessment | Review of clinical documentation looking for frailty documentation and use of CGA and CFS | Frailty identification improved from 40% to 80% |
| Nimmons et al. 2018 24 | Medical School, University of Manchester, UK |
21 medical students: 10 received education week; 11 did not |
Frailty e‐modules, small group teaching session and clinical experience in a geriatric training week | Concept of frailty and assessment tools/processes | Semi‐structured interviews comparing students receiving education with those who did not | Improved attitude toward frailty, ability to define it and knowledge of assessment in those who received this education |
| Reico‐Saucedo et al. 2018 19 | 4 ‘Frailty Units’, UK | “staff working in frailty units” | Training program for frailty units including shadowing, case discussion and online modules | Concept and assessment of frailty, CGA training |
Focus groups Phone interviews Observation of training |
Strongest view was that training improved understanding of definition/complexity of frailty and directly improved care of patients/carers. |
| McKelvie et al. 2019 20 | Oxford Health, UK | 30 allied health professionals and nurses | 10‐day classroom teaching, 76 hrs supervised practice | Concept of frailty, CGA training |
Focus group Survey |
Valued learning skills in multidisciplinary environment Barriers: service provision needs, time pressure |
| Arakawa et al. 2020 18 | Medical School, University of Adelaide, Australia | 61 fifth‐year medical students | Lectures as part of a 4.5‐week geriatric medicine course | Assessment, diagnosis and management of frailty | 26 item survey on self‐perceived competence | Increased perceived importance of defining frailty, communicating with patient/family, providing nutritional/exercise advice. Overall improved perceived competence in assessment, diagnosis and management. |
| Donoghue et al. 2020 22 | Trinity College, Dublin, Ireland | 141 staff: medical, nursing, physiotherapy, dietetics, social work, occupational therapy, speech therapy, pharmacy and administration | Interactive workshop and training day | Understanding and recognising frailty, overview of TILDA study, frailty assessment tools | Pre‐ and post‐education survey on perceived competence | 94%: excellent/very good program; 74%: improved frailty knowledge; 73%: could easily define frailty; 75%: improved frailty assessment knowledge |
| Hesselink et al. 2020 21 | Canisius Wilhelmina Hospital, Netherlands | 21 Emergency physicians | Online module as part of a 6‐week training and eight interactive lectures including case studies | Frailty and frail older patients |
Pre‐ and post‐education multiple choice exam Qualitative survey of perceived knowledge and attitudes Pre‐ and post‐analysis of 100 medical records |
Self‐perceived improvement in ability to define and recognise frailty, more holistic view of patient's condition and needs, better understanding of implications of caring for frail older person |
| Dowell et al. 2021 25 | Emergency Department, UK | “nursing staff” | Two education sessions | Frailty and CFS | Review of medical records | Frailty screening increased from 60% to >80%, increased reliability of CFS |
| Kotsani et al. 2021 23 | Aristotle University of Thessaloniki Primary Research Network, Greece | 31 Primary health care professionals: 17 physicians, 12 nurses, 2 health visitors | One‐day training course, take‐home self‐education material | Definition and current frailty theories, assessment tools, management of frailty | Survey before, on completion, and 3 months after education | 90% rating workshop as good/very good; 80% improved familiarisation of concept; 76% found workshop still useful 3 months' later; improved perception of knowledge and skills for recognition and management; 70% likely to modify current clinical practice; 52% increased use of frailty tools |
Abbreviations: CFS, clinical frailty scale; CGA, comprehensive geriatric assessment; TILDA, the Irish Longitudinal Study on Ageing.
TABLE 3.
Quality assessment of studies
| Author, date | Country | Article type | Study analysis | JBI Quality Assessment |
|---|---|---|---|---|
| Aijaz et al. 2018 27 | UK | Poster abstract | Cross‐sectional | 5/8 |
| Nimmons et al. 2018 25 | UK | Article | Qualitative | 8/10 |
| Reico‐Saucedo et al. 2018 20 | UK | Published report | Qualitative | 8/10 |
| McKelvie et al. 2019 21 | UK | Poster abstract | Cross‐sectional | 5/8 |
| Arakawa et al. 2020 19 | Australia | Article | Cross‐sectional | 7/8 |
| Donoghue et al. 2020 23 | Ireland | Article | Cross‐sectional | 6/8 |
| Hesselink et al. 2020 22 | Netherlands | Article |
Qualitative Cross‐sectional |
6/10 8/8 |
| Dowell et al. 2021 26 | UK | Poster abstract | Cross‐sectional | 4/8 |
| Kotsani et al. 2021 24 | Greece | Article | Cross‐sectional | 6/8 |
Note: Scoring: Cross‐sectional critical appraisal checklist: minimum score of 1, maximum score of 8 indicating well‐conducted cross‐sectional study. Qualitative research critical appraisal checklist: minimum score 1, maximum score of 10 indicating well‐conducted qualitative research.
Abbreviations: JBI, Johanna Briggs Institute; UK, United Kingdom.
3.1. Program location and participants
Participant numbers varied (from 10 to 356 participants, median 30.5) and was not clearly defined in two studies. The largest program, described by Donoghue et al., was completed by 356 participants, although fewer than half (approximately 40%) were involved in the assessment of the program. Two studies reported on training programs for medical students. 19 , 25 Three trained Emergency Department staff 22 , 26 , 27 and one reported on primary health care professional education. 24 The remaining three programs were for multidisciplinary staff working or planning to work with older patients. 20 , 21 , 23
3.2. Program structure and content
Most frailty training was embedded in broader geriatric training programs, with only three studies describing programs that solely addressed frailty. 20 , 23 , 24 The majority of the programs were short in duration, delivered as either individual modules or single‐day workshops. Only the frailty unit training program described by Recio‐Saucedo et al. 20 involved extended training, shadowing of expert clinicians and case discussions. A period of supervised practice was also included in the program described by McKelvie et al. 21 and both programs which targeted medical students included concurrent clinical exposure to frailty cases. 19 , 25 Most of the programs were delivered as in‐person lectures or workshops. Online modules formed the basis of three programs. 20 , 22 , 25
All programs covered theoretical knowledge around the concept of frailty. These included definitions of frailty, its prevalence and addressed misconceptions associated with it. Directions on how to conduct an assessment of frailty was also commonly covered. 23 , 24 , 25 , 26 , 27 In comparison, frailty interventions were not discussed by most programs, although Kostani et al. 24 included some frailty management training and Arakawa et al. 19 did focus on exercise prescriptions for frail older people.
Most programs included aspects of active learning and use of clinical information to engage participants. Kostani et al. 24 and Donoghue et al. 23 discussed using focus groups to assess educational needs prior to commencing more didactic learning, as well as interactive workshops allowing practical training on frailty assessment. Three other studies noted dedicated training on specific frailty assessment tools, such as the clinical frailty scale 26 or a comprehensive geriatric assessment tool. 21 , 27 Many programs included case studies or discussion of participants' practical experience 19 , 22 , 25 . Individualized feedback on performance was provided in two programs 25 , 27 and McKelvie et al. 21 discussed using an electronic competency framework to allow immediate tracking of learning progression.
3.3. Evaluation of program effectiveness
Assessments of program effectiveness included quantitative and qualitative methodologies, including semi‐structured interviews, focus groups, surveys, multiple choice examination of knowledge, and review of medical records. All studies reported improvement in participant awareness of frailty following the training program, with many describing an improvement in the ability to define frailty 19 , 20 , 21 , 22 , 23 , 24 , 25 , 26 , 27 and understand it as a complex and multifactorial concept. 20 , 24 , 25 For example, Aijaz et al. 27 and Dowell et al. 26 reported a 40% and 20% increase, respectively, in Emergency Department clinician ability to identify frailty, through review of clinical documentation pre‐ and post‐intervention. Donoghue et al 23 noted that there was a 74% improvement in perceived frailty knowledge and 73% subjective improvement in multidisciplinary clinicians' ability to define frailty. 23 When delivering frailty education to medical students, Arakawa et al. reported the greatest increase in self‐perceived knowledge in those with no or limited prior exposure to geriatrics (54% of cohort). 19 Both Kotsani et al. and Nimmons et al. reported benefits in reducing frailty misconceptions, with a reduction in attitudes such as ‘frailty is an inevitable consequence of aging’. 24 , 25
Hesselink et al. demonstrated a statistically significant improvement in performance on a multiple‐choice examination by staff who participated in both e‐modules and interactive lectures. 22 All staff, regardless of the teaching received, described an increase in self‐perceived knowledge. Hesselink et al. also reviewed patient records pre‐ and post‐frailty training and identified a 22% increase in documentation of patient social circumstances, functional abilities and sensory capacity in assessments of older people in the Emergency Department. 22
Five studies noted an improvement in participant knowledge around frailty assessments 23 , 24 , 25 , 26 , 27 with Donoghue et al. reporting a 75% improvement in perceived frailty assessment knowledge. 23 Dowell et al. reported an increase in completed frailty assessments of older people presenting at Emergency Departments from 60% to over 80%, reflecting knowledge transfer to clinical practice. 26 Kotsani et al. also assessed completed frailty screening, describing an increase in frailty screening (52% increased use) that was sustained at 3 months. 24
Only two training programs specifically discussed the impact of education on frailty management. Kotsani et al. noted an initial increase in the self‐perceived ability to manage frailty, but this was not sustained over 3 months, with a drop from 70% to 32% of participants stating that they applied this knowledge to daily practice. 24 Arakawa et al also reported increased medical student perception of competence in frailty management, but there was no assessment of this perceived competence. 19
3.4. Participant feedback
Seven studies documented participant perception and experience of the frailty education program. 19 , 20 , 21 , 22 , 23 , 24 , 25 Characteristics of the programs regarded as beneficial included being multidisciplinary in nature, 20 , 21 promoting group learning, 20 use of case studies, 20 having enthusiastic and visible leaders running the programs 20 and building on prior knowledge and experiences 23 (Table 4). Nimmons et al. 25 highlighted the benefit of having clinical exposure to people with frailty at the same time as didactic education. The Emergency Department clinicians in Hesselink et al. 22 mentioned appreciating the flexibility of e‐learning but cautioned overuse of this modality given concerns for lack of interaction. The most common feedback was to recommend the teaching of skills and practical aspects of frailty assessment and management rather than a purely theoretical approach. 19 , 20 , 21 , 22 Additionally, the importance of having protected time to complete training was noted. 20
TABLE 4.
Frailty training program recommendations
| Structure |
| Multidisciplinary participants and facilitators |
| Hybrid teaching modalities (e.g., online and in‐person teaching, if possible, or interactive virtual experiences) to promote engagement, interaction between participants and flexibility in the context of other commitments |
| Allow for scalability (in duration/intensity) for differing levels of expertise/knowledge needs |
| Embed review of program and assessment of effectiveness to enable quality improvement |
| Content |
| Content tailored to specific health professionals, teams (e.g., medical/surgical disciplines), or setting |
| Assess prior knowledge and experience |
| Mix of theoretical knowledge and practical skills |
| Address frailty myths and misconceptions |
| Consider ongoing learning resources: handouts, online material, link with mentor, clinical placement |
| Implementation |
| Embed in course/curriculum |
| Dedicated time concurrent with relevant clinical experience |
4. DISCUSSION
Despite the increasing attention on frailty in clinical practice, this systematic review found that there continues to be limited reporting and evaluation of frailty training programs for health professionals, with reports identified on only nine programs. Training programs differed with respect to target audience, intensity, duration, and delivery modality, but had overall positive evaluations and were effective in increasing frailty knowledge and self‐perceived competence in frailty assessment. Studies that assessed translation of this knowledge into clinical practice consistently reported significant improvements in the completion of standardized frailty assessments and consideration of frailty‐related principles during routine health care. Some common features of successful programs included having multidisciplinary participants and/or facilitators and delivering a clinically tailored program, using flexible teaching modalities.
The majority of programs' content focused on introducing frailty and increasing frailty awareness, which is important, but likely to only be part of the solution of bridging the knowledge‐practice gap for optimising the management of frailty. Barriers related to the system (time, staffing), patient perceptions (fear of stigma), and teams (poor collaboration) contributed strongly, and could form part of an interactive discussion in frailty education programs. 12 , 28 , 29 Another key concern is that there is currently no consensus as to a standardized tool for frailty measurement with 89 different measures utilized in the acute care setting alone, as described in a 2018 scoping review. 30 While some health systems will advocate for specific tools (e.g., the electronic frailty index is automatically generated for all adults aged 65 years and over who attend a GP for primary care in the UK 31 ), other frailty training program developers will need to identify the tool(s) most appropriate or relevant to the program participants and setting.
Teaching focussing specifically on frailty management strategies was barely covered in the majority of programs. Positive outcomes on frailty improvement have been noted for interventions such as nutritional supplementation, prescription of physical activity, health education, cognitive training, and hormone therapy; however, overall, the certainty of evidence remains low with further confirmation studies required. 32 Yet, there may be benefits to including a balanced discussion of emerging management strategies in frailty education programs, especially for addressing misconceptions such as the inevitability and permanence of frailty. This discussion may be enhanced by highlighting consensus guidelines recommendations (e.g., WHO guideline for Integrative Care for Older People and NICE guideline for multimorbidity). 33 , 34
Program participant feedback highlighted the desire for active learning strategies, such as facilitating practical clinical skills over theoretical knowledge. Although shown to result in increased knowledge, critical thinking and participant engagement in medical education, active learning activities may require greater time for preparation, and increased presenter training or exposure to current medical education pedagogical practice. 35 , 36 , 37 , 38 Use of cases studies was noted in many of the education programs, which cannot only be used to demonstrate assessment of frailty but also to model decision‐making and professional behaviour, which are key to addressing internalised misconceptions and the stigma of frailty. 36 , 39 Protected teaching time was highlighted as a potential challenge, which needs to be considered prior to implementation of future programs, but may be assisted by strategies such as initial identification of learning goals to target teaching and embedding teaching into specific clinical areas. Additionally, especially in the era of COVID‐19, training programs need to adapt to the requirements of the health service and careful consideration must be given to the cost of virtual and hybrid training programs. 40 , 41
It is important to consider the results of the study in the context of its limitations. Despite broad inclusion criteria, a small number of studies were ultimately included in this review. A lack of publication may not necessarily mean a lack of frailty education, and, similar to previous review, many other frailty education programs can be found in a search of gray literature (Table 1). The breadth of medical and surgical disciplines and healthcare settings were not captured by the included studies, and given known differences in patient case‐mix, clinician roles and responsibilities, and logistical considerations (e.g., time constraints), the results may not apply to all potential participants and training programs. Many studies provided limited detail on the content and education processes, and may have been improved by following criteria for evaluating education interventions in health care. 42 Only one study assessed whether participant changes were maintained for a prolonged period (3 months). 24 Additionally, the majority of programs assessed perceived efficacy rather than objective changes in patient care or patient outcomes.
Only a third of the programs solely addressed frailty, with the majority including frailty in general education on older people's healthcare. Potentially, this may cloud results with the broader education facilitating transfer of frailty knowledge. It should be noted that the frailty‐specific programs accounted for the majority of participants, and demonstrated some of the strongest evidence for program efficacy. 20 , 23 , 24 In 2013, a consensus group consisting of delegates from six major international, European, and US societies proposed a call to action for frailty screening, assessment and management. 43 The National Institute for Health and Care Excellence and the National Health Service England responded to the call by supporting and then mandating routine frailty assessment in primary care. 33 , 44 Multiple other health care bodies have similarly implemented guidelines and recommendations to include frailty assessment and management as best practice. 45 , 46 , 47 To promote and facilitatethe uptake of these best practice guidelines, it is imperative that a wide range of health care professionals be taught about frailty and this is possible to achieve as a specific teaching goal, outside of geriatric education.
5. CONCLUSIONS
The results of this review should reassure local and national education and healthcare bodies that frailty training programs are feasible, flexible, and perceived by healthcare professionals to be effective in building knowledge and skills. There are opportunities for frailty training programs to be systematically incorporated into education for health professionals at universities and in the work‐place, with content focus not only on awareness of frailty and its assessment tools but also on its prevention and management. This should occur in combination with continued and longitudinal evaluation, not only for the adoption of frailty clinical skills but also for improving patient outcomes following the introduction of education programs.
CONFLICTS OF INTEREST
NW has received speaker fees from Otsuka, Lundbeck and Janssen. DS is funded in part by NHMRC Emerging Leadership Fellowship GNT1194635. CEB is an associate editor of the Australasian Journal on Ageing. NR is funded in part by the Metro South Research Support Scheme.
ACKNOWLEDGEMENT
Open access publishing facilitated by The University of Queensland, as part of the Wiley ‐ The University of Queensland agreement via the Council of Australian University Librarians.
Warren N, Gordon E, Pearson E, et al. A systematic review of frailty education programs for health care professionals. Australas J Ageing. 2022;41:e310‐e319. doi: 10.1111/ajag.13096
Funding information
None.
DATA AVAILABILITY STATEMENT
Data sharing is not applicable to this article as no new data were created or analyzed in this study.
REFERENCES
- 1. Han L, Clegg A, Doran T, Fraser L. The impact of frailty on healthcare resource use: a longitudinal analysis using the clinical practice research datalink in England. Age Ageing. 2019;48(5):665‐671. doi: 10.1093/ageing/afz088 [DOI] [PubMed] [Google Scholar]
- 2. Bock J‐O, König H‐H, Brenner H, et al. Associations of frailty with health care costs – results of the ESTHER cohort study. BMC Health Serv Res. 2016;16(1):128. doi: 10.1186/s12913-016-1360-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Comans TA, Peel NM, Hubbard RE, Mulligan AD, Gray LC, Scuffham PA. The increase in healthcare costs associated with frailty in older people discharged to a post‐acute transition care program. Age Ageing. 2016;45(2):317‐320. doi: 10.1093/ageing/afv196 [DOI] [PubMed] [Google Scholar]
- 4. Apóstolo J, Cooke R, Bobrowicz‐Campos E, et al. Effectiveness of interventions to prevent pre‐frailty and frailty progression in older adults: a systematic review. JBI Database System Rev Implement Rep. 2018;16(1):140‐232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Cunha AIL, Veronese N, de Melo BS, Ricci NA. Frailty as a predictor of adverse outcomes in hospitalized older adults: a systematic review and meta‐analysis. Ageing Res Rev. 2019;56:100960. doi: 10.1016/j.arr.2019.100960 [DOI] [PubMed] [Google Scholar]
- 6. World Health O . Global Strategy and Action Plan on Ageing and Health. World Health Organization; 2017. [Google Scholar]
- 7. Papadopoulou C, Barrie J, Andrew M, et al. Perceptions, practices and educational needs of community nurses to manage frailty. Br J Community Nurs. 2021;26(3):136‐142. 10.12968/bjcn.2021.26.3.136 [DOI] [PubMed] [Google Scholar]
- 8. Britton H. What are community nurses' experiences of assessing frailty and assisting in planning subsequent interventions? Br J Community Nurs. 2017;22(9):440‐445. doi: 10.12968/bjcn.2017.22.9.440 [DOI] [PubMed] [Google Scholar]
- 9. Coker JF, Martin ME, Simpson RM, Lafortune L. Frailty: an in‐depth qualitative study exploring the views of community care staff. BMC Geriatr. 2019;19(1):47. doi: 10.1186/s12877-019-1069-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Obbia P, Graham C, Duffy FR, Gobbens RJ. Preventing frailty in older people: an exploration of primary care professionals' experiences. Int J Older People Nurs. 2020;15(2):e12297. doi: 10.1111/opn.12297 [DOI] [PubMed] [Google Scholar]
- 11. Ambagtsheer RMC, Archibald M, Lawless M, Mills D, Yu S, Beilby J. GP perceptions and experiences of frailty and frailty screening. Aust J General Pract. 2019;48:426‐433. doi: 10.31128/AJGP-11-18-4757 [DOI] [PubMed] [Google Scholar]
- 12. Avgerinou C, Kotsani M, Gavana M, et al. Perceptions, attitudes and training needs of primary healthcare professionals in identifying and managing frailty: a qualitative study. Eur Geriat Med. 2021;12(2):321‐332. doi: 10.1007/s41999-020-00420-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Korenvain C, Famiyeh I‐M, Dunn S, Whitehead CR, Rochon PA, McCarthy LM. Identifying frailty in primary care: a qualitative description of family physicians' gestalt impressions of their older adult patients. BMC Fam Pract. 2018;19(1):61. doi: 10.1186/s12875-018-0743-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. D'Avanzo B, Shaw R, Riva S, et al. Stakeholders' views and experiences of care and interventions for addressing frailty and pre‐frailty: a meta‐synthesis of qualitative evidence. PloS One. 2017;12(7):e0180127. doi: 10.1371/journal.pone.0191763 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Society BG . Frailty Hub. https://www.bgs.org.uk/resources/resource‐series/frailty‐hub. Accessed 19 September 2021
- 16. Windhaber T, Koula ML, Ntzani E, et al. Educational strategies to train health care professionals across the education continuum on the process of frailty prevention and frailty management: a systematic review. Aging Clin Exp Res. 2018;30(12):1409‐1415. doi: 10.1007/s40520-018-0918-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Moher D, Shamseer L, Clarke M, et al. Preferred reporting items for systematic review and meta‐analysis protocols (PRISMA‐P) 2015 statement. Syst Rev. 2015;4(1):1. doi: 10.1186/2046-4053-4-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Moola S MZ, Tufanaru C, Aromataris E, Sears K, Sfetcu R, Currie M, Qureshi R, Mattis P, Lisy K, Mu P‐F. Chapter 7: systematic reviews of etiology and risk. In Aromataris E, Munn Z (Editors). JBI Manual for Evidence Synthesis JBI. 2020.
- 19. Arakawa Martins B, Jadczak AD, Dollard J, et al. Fifth‐year medical students' perceptions of the importance of frailty and competence in assessing, diagnosing and managing frailty before and after a geriatric medicine course. Australas J Ageing. 2020;39(3):e472‐e477. doi: 10.1111/ajag.12412 [DOI] [PubMed] [Google Scholar]
- 20. Recio‐Saucedo A. Health Education England Wessex Workforce and Education Initiative to support the delivery of better care to patients living with frailty. 2018. https://clahrc‐wessex.nihr.ac.uk/img/publications/HEE_Frailty_pathways__DraftReport[.pdf Accessed 30 June 2021.
- 21. McKelvie S, Broad A, Matthew H, Bolton S. Preparing the workforce for frailty, an education intervention for allied health professionals and community nurses in primary and community healthcare. Physiotherapy. 2019;105:e170‐e171. doi: 10.1016/j.physio.2018.11.176 [DOI] [Google Scholar]
- 22. Hesselink G, Sir Ö, Öztürk E, Heiwegen N, Olde Rikkert M, Schoon Y. Effects of a geriatric education program for emergency physicians: a mixed‐methods study. Health Education Research Jun 1. 2020;35(3):216‐227. doi: 10.1093/her/cyaa007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Donoghue OA, O'Shea M, McGarrigle CA, et al. Translating frailty assessment methodologies and research‐based evidence to clinical education and practice. J Aging Soc Policy. 2020;1‐15:1‐15. doi: 10.1080/08959420.2020.1777825 [DOI] [PubMed] [Google Scholar]
- 24. Kotsani M, Avgerinou C, Haidich A‐B, et al. Feasibility and impact of a short training course on frailty destined for primary health care professionals. Eur Geriat Med. 2021;12(2):333‐346. doi: 10.1007/s41999-021-00467-7 [DOI] [PubMed] [Google Scholar]
- 25. Nimmons D, Pattison T, O'Neill P. Medical student attitudes and concepts of frailty and delirium. Eur Geriat Med. 2018;9(1):45‐50. doi: 10.1007/s41999-017-0018-y [DOI] [PubMed] [Google Scholar]
- 26. Dowell H, Mallinson R, Cartmell D, Mellstrom K, Pettigrew G, Spice C. 107 improving frailty screening and accuracy in the emergency department (ed) of a Busy District general hospital. Age and Ageing. 2021;50(Suppl 1):i12‐i42. 10.1093/ageing/afab030.68 [DOI] [Google Scholar]
- 27. Aijaz F, Conroy S, Banerjee J. 59 embedding the clinical frailty scale in the emergency department and its impact on patient care. Age and Ageing. 2018;47(suppl_3):ii20‐iii23. 10.1093/ageing/afy127.08 [DOI] [Google Scholar]
- 28. Taylor JK, Fox J, Shah P, Ali A, Hanley M, Hyatt R. Barriers to the identification of frailty in hospital: a survey of UKclinicians. Future Healthc J. 2017;4(3):207‐212. doi: 10.7861/futurehosp.4-3-207 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Gwyther H, Shaw R, Jaime Dauden E‐A, et al. Understanding frailty: a qualitative study of European healthcare policy‐makers' approaches to frailty screening and management. BMJ Open. 2018;8(1):e018653. doi: 10.1136/bmjopen-2017-018653 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Theou O, Squires E, Mallery K, et al. What do we know about frailty in the acute care setting? A scoping review. BMC Geriatr. 2018;18(1):139. doi: 10.1186/s12877-018-0823-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Clegg A, Bates C, Young J, et al. Development and validation of an electronic frailty index using routine primary care electronic health record data. Age Ageing. 2016;45(3):353‐360. doi: 10.1093/ageing/afw039 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Dent E, Martin FC, Bergman H, Woo J, Romero‐Ortuno R, Walston JD. Management of frailty: opportunities, challenges, and future directions. The Lancet. 2019;394(10206):1376‐1386. doi: 10.1016/S0140-6736(19)31785-4 [DOI] [PubMed] [Google Scholar]
- 33. NICE . National Institute for Health and Care Excellence, Multimorbidity: clinical assessment and management (NICE). 2016. https://www.nice.org.uk/guidance/ng56/resources/multimorbidity‐clinical‐assessment‐and‐management‐pdf‐1837516654789. Accessed 30 June 2021
- 34. Organization WH . Integrated care for older people: guidelines on community‐level interventions to manage declines in intrinsic capacity. 2017. https://apps.who.int/iris/handle/10665/258981. Accessed 30 June 2021 [PubMed]
- 35. McMahon GT. What do I need to learn today?‐‐the evolution of CME. N Engl J Med. 2016;374(15):1403‐1406. doi: 10.1056/NEJMp1515202 [DOI] [PubMed] [Google Scholar]
- 36. Graffam B. Active learning in medical education: strategies for beginning implementation. Med Teach. 2007;29(1):38‐42. doi: 10.1080/01421590601176398 [DOI] [PubMed] [Google Scholar]
- 37. Bucklin BA, Asdigian NL, Hawkins JL, Klein U. Making it stick: use of active learning strategies in continuing medical education. BMC Med Educ. 2021;21(1):1‐9. doi: 10.1186/s12909-020-02447-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Anderson WL, Mitchell SM, Osgood MP. Comparison of student performance in cooperative learning and traditional lecture‐based biochemistry classes. Biochem Mol Biol Educ. 2005;33(6):387‐393. doi: 10.1002/bmb.2005.49403306387 [DOI] [PubMed] [Google Scholar]
- 39. Kojima G, Liljas AE, Iliffe S. Frailty syndrome: implications and challenges for health care policy. Risk Manag Healthcare Policy. 2019;12:23‐30. doi: 10.2147/RMHP.S168750 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Papapanou M, Routsi E, Tsamakis K, et al. Medical education challenges and innovations during COVID‐19 pandemic. Postgrad Med J. 2021;98:321‐327. doi: 10.1136/postgradmedj-2021-140032 [DOI] [PubMed] [Google Scholar]
- 41. Crossman M, Papanagnou D, Sullivan T, Zhang XC. Virtual grand rounds in COVID‐19: a financial analysis. Acad Emerg Med. 2021;28(4):480‐482. doi: 10.1111/acem.14224 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Van Hecke A, Duprez V, Pype P, Beeckman D, Verhaeghe S. Criteria for describing and evaluating training interventions in healthcare professions – CRe‐DEPTH. Nurse Educ Today. 2020;84:104254. doi: 10.1016/j.nedt.2019.104254 [DOI] [PubMed] [Google Scholar]
- 43. Morley JE, Vellas B, van Kan GA, et al. Frailty consensus: a call to action. J Am Med Dir Assoc. 2013;14(6):392‐397. doi: 10.1016/j.jamda.2013.03.022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. NHS England . Supporting routine frailty identification and frailty through the GP Contract 2017/2018 (NHS). 2021. https://www.england.nhs.uk/publication/supporting‐routine‐frailty‐identification‐and‐frailty‐through‐the‐gp‐contract‐20172018/. Accessed 30 June 2017.
- 45. The Royal Australian College of General Practitioners (RACGP) . RACGP Aged care clinical guide (silver book), 5th ed. East Melbourne, Vic: RACGP; 2019‐2020. [Google Scholar]
- 46. Afilalo J, Alexander KP, Mack MJ, et al. Frailty assessment in the cardiovascular care of older adults. J Am Coll Cardiol. 2014;63(8):747‐762. doi: 10.1016/j.jacc.2013.09.070 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Hoogendijk EO, Afilalo J, Ensrud KE, Kowal P, Onder G, Fried LP. Frailty: implications for clinical practice and public health. The Lancet. 2019;394(10206):1365‐1375. doi: 10.1016/S0140-6736(19)31786-6 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data sharing is not applicable to this article as no new data were created or analyzed in this study.


