Abstract
The decline of language and communication abilities is common among people living with dementia and impacts on many areas of everyday life, including active participation in social activities and decision‐making. Despite a growing body of supporting evidence for approaches that address language and communication decline in dementia, the concept of communication rehabilitation is largely neglected in this population. This paper reports on the content validation of a novel tool, the Communication Support Needs Assessment Tool for Dementia (CoSNAT‐D). The tool has been developed to assist in the initial identification of communication difficulties and related support needs of people living with dementia. Importantly, the CoSNAT‐D is the only available tool that takes a three‐way informed approach, considering the view of the person living with dementia, their carer and an administering healthcare professional. Content validity was established between September and December 2018 using a modified Delphi approach. An international expert panel rated 32 items of a face‐validated item pool regarding their importance and relevance through an iterative feedback process. Consensus was pre‐determined at 70% of agreement for both importance and relevance of an item. Data were analysed using descriptive statistics and qualitative content analysis of comments provided in each round. Twenty‐eight experts working in dementia, language and communication participated in the Delphi survey. Qualitative analysis resulted in the addition of five items, of which three reached the required consensus in Round 3. Consensus was established for 35/37 items in three rounds. The pilot version of the CoSNAT‐D demonstrates adequate content validity and face validity. The use of the CoSNAT‐D may assist a range of healthcare professionals in the decision‐making process about appropriate next management steps, and thereby improve the care path for people with dementia and language and communication impairment. The establishment of further psychometric properties is warranted.
Keywords: assessment, communication, content validity, dementia, language
What is known about the topic and what this paper adds.
Communication abilities are affected in all forms of dementia and while interventions targeting communication rehabilitation are available, this area is frequently neglected in dementia care
Currently, there is no validated assessment tool that can be used by non‐speech specialist to assist in the identification of communication difficulties for people with dementia and the need for further (specialist) support
This paper provides new evidence regarding the development and application of a novel tool, the Communication Support Needs Assessment Tool for Dementia (CoSNAT‐D)
The content validity of the CoSNAT‐D was confirmed by an international panel with senior‐level experience in the area of language and communication in dementia
The tool offers a way to enhance multidisciplinary dementia care in the community
1. INTRODUCTION
According to national and international guidelines, principles of person‐centred care underpin the healthcare provision for people living with dementia (Guideline Adaptation Committee, 2016; National Institute for Health and Care Excellence, 2016). Effective communication is a corner stone of person‐centred care. However, impaired communication function is one of the hallmarks of dementia (Bryan & Maxim, 2006; Klimova & Kuca, 2016; Reilly et al., 2010). Communication hinges on an individual's ability to accurately process and produce language (i.e. speaking, understanding, reading and writing), and on the intact interplay of cognitive functions that enable us to focus (attention), hold the information we have received (memory) and organise and formulate our thoughts (executive function). Specific symptoms of language and communication impairment (LCI) in dementia include word finding difficulties (lexical retrieval), visual and auditory processing difficulties, motor‐planning disorders (apraxia of speech), difficulties of grammar/syntax, disorders of spelling or writing (dysgraphia) as well as the loss of meaning and coherence in conversational discourse, and difficulties adhering to social rules of communication (Graham, 2014; Harciarek & Kertesz, 2009; Klimova & Kuca, 2016; Volkmer, 2013). Changes in linguistic behaviour may serve as an early diagnostic marker in Alzheimer's dementia and mild cognitive impairment (Jokel et al., 2019) and the assessment of language plays an important role in the diagnostic process of dementia (Boschi et al., 2017).
LCI may affect social aspects of life (Ballard et al., 2001) and can place people living with dementia in a highly vulnerable and often disempowered position. LCI in dementia may also affect other aspects related to quality of life, such as relationships, psychological wellbeing and participation (Nickels & Croot, 2014). For example, communication breakdown has been reported to lead to reduced connection for the family carer, eliciting feelings of embarrassment, guilt, frustration and a loss of control, hence impacting on the quality of relationships (Beales et al., 2019; Nickels & Croot, 2014). Despite its relevance, LCI is often overlooked and its treatment frequently neglected in dementia care (Beales et al., 2019; Volkmer et al., 2018). One of the reasons for this lack of attention includes low referral rates to services that provide the above mentioned types of support, for example, speech pathology care (Krein et al., 2019).
1.1. Rehabilitation of language and communication difficulties in dementia
Aligning with the definition of the World Health Organisation (WHO, 2011), rehabilitation of language and communication abilities aims to assist the individual to ‘achieve and maintain optimum functioning in interaction with their environments’ (Clare, 2017, p. 96). Communication support may include but is not limited to: the provision of individually tailored information about the person's current cognitive‐linguistic abilities and limitations; counselling and education about the progression of LCI in dementia; developing therapy plans in conjunction with the person with dementia and their carers; and administering appropriate and evidence based therapies to maximise interpersonal engagement (Agency for Clinical Innovation, 2016; American Speech‐Language‐Hearing Association, 2020; Speech Pathology Australia, 2012). The timely identification of LCI is the first necessary step to provide such support and assist with communication rehabilitation in people living with dementia.
1.2. Assessment of communication support needs
A recent review of assessment tools available for the identification of LCI in dementia revealed that currently no tools in English exist that can assist in the identification of individual support needs for this population group (Krein et al., 2019). Assessing communication support needs of people living with dementia requires understanding the person beyond their LCI. A needs assessment can be defined as a multi‐staged process that aims to (1) identify difficulties with which the individual requires help or more help than they currently receive, (2) identify unmet need as determined by the professional but also perceived need by the individual, and (3) specify the type of help required to meet those needs (McWalter et al., 1994). It is typically conducted by a healthcare professional and should consider ‘the views of the person assessed or of their advocate’ (McWalter et al., 1994, p. 17). Currently available and commonly used tools for the assessment of support needs in dementia include the care needs assessment package for dementia (CarenapD) (McWalter et al., 1998), the Camberwell Assessment of Need for the Elderly (CANE) (Reynolds et al., 2000), and the Carer Support Needs Assessment Tool (CSNAT) (Ewing et al., 2013). Needs assessment tools can be used in a variety of settings, including in community and inpatient care. Existing tools aim to identify a wide range of unmet needs. However, none focuses on LCI specifically.
1.3. The communication support needs assessment tool for dementia (CoSNAT‐D)
The Communication Support Needs Assessment Tool for Dementia (CoSNAT‐D) was developed to address the current gap in the service delivery for communication support needs of people living with dementia. The CoSNAT‐D is a short tool for healthcare professionals who do not specialise in the management of LCI to screen for difficulties a person may have in completing everyday communication‐based tasks. The CoSNAT‐D has been designed for use in a community care context, either in a person's own home or in a residential care home. Importantly, the CoSNAT‐D is a three‐way informed tool, taking into account the perspective of the person with dementia, a carer and a healthcare professional. Healthcare professionals who are familiar with administering assessment tools may administer the tool. It can be used to inform their decision‐making regarding the next appropriate management step to best support LCI in their patients with dementia. The CoSNAT‐D helps to determine the need for (specialist) communication support through (1) assessing the likely presence of LCI and (2) identifying the level of frustration or distress the person with dementia and the caregiver experience as a result of LCI. The CoSNAT‐D aims to complement existing needs assessment tools in dementia care.
1.4. Development and face validation of the draft item pool
The development and face validation of the CoSNAT‐D involved two stages: drafting of an item pool (stage 1) and establishing the face validation of the draft items (stage 2) with the help of 22 participants of the prospective target population (seven people living with dementia and 15 family carers). Minor changes to improve clarity and the addition of one item to improve comprehensiveness resulted from consumer feedback in stage 2. Further details of development stages 1 and 2 can be found elsewhere (Krein et al., 2019; Krein et al., 2020). The establishment of the content validation of the draft items (stage 3) is the focus of this paper (see Figure 1).
FIGURE 1.
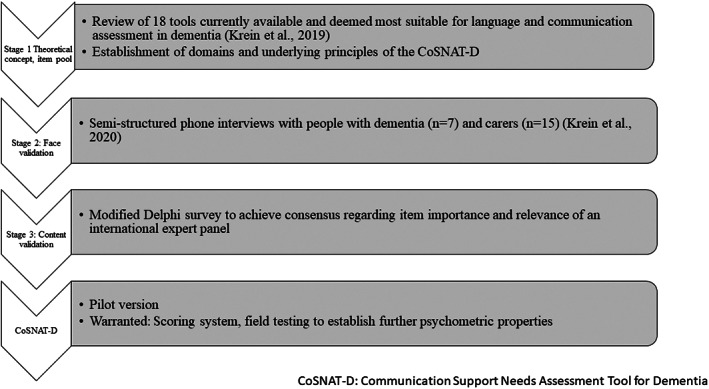
Development stages of the CoSNAT‐D pilot version.
1.5. Underlying framework and guiding principles
The underlying framework for the development of the CoSNAT‐D was informed by the WHO's International Classification of Functioning, Disability and Health (ICF) (World Health Organisation, 2001). The ICF ‘provides a standard language and framework for the description of health and health‐related states’ (World Health Organisation, 2002, p. 2) with a focus on functioning and disability. The CoSNAT‐D items are aligned to the ICF components Body functions, Activities, Participation, Environmental factors. The alignment of items with a widely used international classification system, such as the ICF, is useful in the user context of the CoSNAT‐D as this allows for clear communication among multidisciplinary health professionals, both those using the tool and those providing specialist intervention or rehabilitation services when required. The guiding principles underlying the CoSNAT‐D were established based on the limitations of existing tools. These principles were: a person‐centred assessment approach, suitability for clinician user scope of practice and a focus on the impact of LCI on the person's everyday activity and participation rather than a task‐based assessment of isolated language and cognitive function.
1.6. Description of the CoSNAT‐D items
The CoSNAT‐D addresses verbal language expression, auditory comprehension, writing, reading and functional communication. Items are organised into three sections: Section A (completed by the person with a diagnosis of dementia), Section B (completed by a ‘support person’, that is, a family carer, friend or a formal carer providing at least 7 h of emotional or physical support per week), and Section C (completed by the administering healthcare professional, who is experienced in providing dementia care but is not familiar with the assessment of speech, language and communication). Prior to administering Sections A to C, a set of baseline questions named ‘Pre‐commencement questions’ are asked to determine if the person with dementia experiences difficulties or has a health condition other than dementia which (1) may affect their ability to complete the tool or (2) may present an additional cause for the communication difficulty the person experiences. For example, a vision or hearing impairment may affect the person's ability to complete questions of Section A independently.
Items are designed to screen difficulties a person may have with completing everyday communication‐based tasks and are deliberately formulated broadly. Each item is rated on a three‐point Likert scale (1 = never or rarely, 2 = sometimes, 3 = frequently or almost always). Examples of items from each section from the original item pool including correspondence to language domains and alignment to ICF codes are presented in Table 1. A list of the face validated item set can be found in the Supplementary Material 1.
TABLE 1.
Item examples of the face‐validated CoSNAT‐D item pool, correspondence to language domains, and alignment to the international classification of function, disability and health (ICF) (World Health Organisation, 2001) codes
| CoSNAT‐D item | Language domain | ICF codes a | ||||
|---|---|---|---|---|---|---|
| Verbal expression | Auditory comprehension | Writing | Reading | Functional communication | ||
| Section A—Person with dementia | ||||||
| Do you feel you have difficulty reading any of the following: a menu at a restaurant; a text message on your phone; an email, letter or bill; newspapers, magazines or books? | X |
Body Functions: b16701 Activity & Participation: d325; d3600; d3601 |
||||
| Do you feel you have difficulty speaking fluently? | X | Body Function: b330 | ||||
| Do you feel you have difficulty understanding TV shows or radio programs? | X |
Body Functions: b16700 Activity & Participation: d3101 |
||||
| Section B—Support person | ||||||
| In your opinion, does [name] have difficulty holding or following a conversation with a group of people? | X | Activity & Participation: d3504; d330; d310 | ||||
| In your opinion, does [name] have difficulty writing any of the following: a shopping list; a text message on your phone/diary entry; an email or a letter? | X |
Body Functions: b16711 Activity & Participation: d345; d3600; d3601 |
||||
| Section C—Healthcare professional | ||||||
| Does the patient/client appear to have difficulties understanding questions, instructions or conversations? | X |
Body functions: b1700 Activity and participation: d310 Environment: e355 |
||||
| Has the patient/client required external support when talking to you? | X | |||||
ICF codes: See supplementary material 2 for a description of the here listed ICF codes.
Importantly, each item of Sections A and B includes a second part, which addresses the level of bother, or frustration related to a specific aspect of their LCI (‘Does this bother or frustrate you?’). This second part of each item in Sections A and B reflects an individualised and person‐centred assessment approach because it acknowledges that a similar impairment may affect individuals differently. For example, the inability to understand a formal letter may be experienced as very bothersome or frustrating by someone who has always managed formal affairs versus someone who has shared such tasks with their spouse. Differentiating between the presence of a LCI and its impact on the person's life allows the respondents to provide an insight into their subjective experience of the communication difficulty.
It is acknowledged that self‐completion of Section A by the person with dementia themselves may not always be possible. The person may require support to complete their section (e.g. the administrator reading out the questions or the carer supporting understanding of the questions) or may experience cognitive decline to a degree which impacts on their ability to complete Section A. In this case, or if the person with dementia declines to participate, the outcomes of Section B and C are used to determine the need for additional specialist support. Should the person with dementia live alone Section A and Section C can be used to inform adequate management pathways. The ability or capacity of the person with dementia to complete Section A should be determined based on the professional judgement of the administering healthcare professional and the knowledge of the support person. The completion of Section A is strongly encouraged but not essential for the completion of the CoSNAT‐D.
1.7. Aim
This study aimed to establish the content validity of the CoSNAT‐D tool by gaining consensus from an international expert panel regarding the importance and relevance of the CoSNAT‐D items. This study is part of a larger project that aimed to develop and establish validity of the CoSNAT‐D.
2. METHOD
2.1. Content validation design, recruitment and sampling
A modified online Delphi approach (Keeney et al., 2010a) was chosen to determine content validity of the draft item set of the CoSNAT‐D (stage 3). Ethics approval was granted by the relevant institutional Human Research Ethics Committee. Purposive sampling was performed to ensure that expert professionals with varying experiences had adequate competencies and knowledge in the areas relevant for this investigation.
Experts in this study were defined as those who (1) have been working for >5 years in either a clinical position with people with dementia or in academia with peer‐reviewed published papers or books about dementia; AND (2) have specific knowledge or experience with how dementia affects speech, language and communication, as reflected in either their recent and current research or work practice. Potential participants were identified through (1) scanning of relevant articles during the literature review that informed the development of draft items of the CoSNAT‐D, (2) the international network for healthcare professionals, ‘Contact, Help, Advice and Information Network’ (CHAIN) and (3) the authors' networks consisting of those who engage in speech, language and communication in dementia. Relevant information and contact details of potential Delphi panel members were collected from public profiles found in the World Wide Web. Recommendations in the literature regarding the optimal panel size range from less than five to several hundred participants (Habibi et al., 2014; Hsu & Sandford, 2007a). Participant retention is a common challenge in Delphi studies and, where reported, can vary greatly ranging between 19.5% and 87.1% (Hall et al., 2018; Hsu & Sandford, 2007b). To account for attrition, a total of 58 experts were approached. No further recruitment took place in between rounds.
2.2. Data collection
All data were collected and managed using REDCap electronic data capture tools (Harris et al., 2009). Panel members consented to anonymous participation by completing an initial privately linked survey, which also included questions about relevant demographic data regarding panel member's professional background, current role, country of residence and gender. Anonymous completion was chosen to reduce common societal bias of rank, gender, race or age (Colton & Hatcher, 2004) and to avoid potential analysis bias, as some panel members were known to the first and third author. Up to three email reminders were sent to consenting participants and they were given the option to save responses and return later by generating a personalised link.
In each survey round, panel members were asked to rate relevance and importance of all of the CoSNAT‐D draft items on a 4‐point Likert‐scale (1—not at all important/relevant; 2—somewhat important/relevant, 3—important/relevant, 4—highly important/relevant). In addition, space for comments was provided. If a score of 1 (not at all relevant/important) was given, experts were asked to provide a short explanation for their rating.
2.3. Data analysis
Data analysis involved the following steps for each round: First, descriptive statistics (mean, standard deviation and range of the rating for each item) were generated for panel agreement on importance and relevance for each of the items as well as for demographic data collected through participant questionnaires prior to Round 1. Second, qualitative data were collated in a table format using Microsoft Excel. Each comment was reviewed, and where possible, suggestions and recommendations were incorporated in the tool by the first author. This included re‐wording of items or adding of new items if an expert comment indicated that a modification or editing was required or that a concept was missing. Finally, outcomes of descriptive statistics and a summary of the qualitative content analysis of each round were provided to panel members for the next round.
The final content validity was determined by scores of means and standard deviation as well as lack of difference in panel response for each item. The consensus level was predetermined at 70%. Consensus was defined to be reached when at least 70% of the panel members rated each item as either ‘Important/Relevant or Highly Important/Highly Relevant’ (Keeney et al., 2010b). An item was removed if consensus of 70% on either relevance or importance was not achieved by Round 3. A two‐sampled z‐test was performed for items where consensus fluctuated between rounds to assess the precision and the degree of difference in responses between each round. This was done using the online statistics software EpiTools (AusVet, 2019).
3. RESULTS
3.1. Delphi panel characteristics
Characteristics of the final panel (n = 28) are presented in Table 2. Panellists were from Europe, Australia, and North America. The majority of respondents were female, working in academia or as speech language pathologists in clinical settings. All of the panellists have experience in working with people living with dementia and addressing LCI in their work. The mean number of years worked in dementia was 19 (SD 7.3) and the mean number of years worked in cognition, language or communication was 22.6 (SD 7.7).
TABLE 2.
Panel characteristics
| Demographic | Participants (n = 28) |
|---|---|
| Gender F/M | 23/5 |
|
Mean years worked in dementia (SD); Min‐max |
19 (SD 7.3); 5–35 |
| Mean years worked in cognition, language or communication (SD), min‐max |
22.6 (SD 7.7); 13–35 |
| Country of residence, n (%) |
UK, 10 (36) Australia, 9 (32) Canada, 5 (18) USA, 3 (11) Germany, 1 (3) |
| Occupation, n (%) |
Academic, 17 (61) Speech language pathologists, 9 (32) Psychologists, 2 (7) |
| Disciplinary background (%) |
Speech language pathology, 20 (72) Neuropsychology, 6 (21) Other, 2 (7) |
As expected, the number of participants fluctuated in each round and between sections. The highest number was 26 (Round 1) decreasing to 19 and 21 in Round 2 and 3, respectively (see Figure 2). The retention rate was 68% in Round 2 and 75% in Round 3.
FIGURE 2.

Expert participation per Delphi round.
3.2. Item importance and relevance
Table 3 shows the level of consensus achieved regarding importance and relevance of all items. For simplicity, only values for the final Round 3 are displayed. The full table of results for all rounds is provided as supplementary material 3. Table 3 displays how many of the 21 experts rated an item as ‘Important/Highly important’ and ‘Relevant/Highly relevant’. In Round 3, consensus at the predetermined agreement level of 70% regarding the importance and relevance of items was achieved for 35/37 items. More than 80% of panellists rated 91% and 94% of the final 35 items as ‘important/highly important’ and ‘relevant/highly relevant’, respectively. These ratings demonstrate overall high levels of consensus regarding the importance and relevance of the majority of the final 35 items.
TABLE 3.
Number (percentage) of panel members (n = 21) rating each item as ‘important/relevant’ or ‘highly important/relevant’ in Round 3 of the Delphi survey
| Pre‐commencement questions | Importance a | Relevance a |
|---|---|---|
| Item 01—Hearing problems | 21 (100) | 21 (100) |
| Item 02—Vision problems | 18 (85.7) | 20 (95.2) |
| Item 03—Diagnosis of depression | 16 (76.2) | 18 (85.7) |
| Item 04—Pre‐morbid language/communication difficulties | 18 (85.7) | 18 (85.7) |
| Item 05 b —Languages spoken at home | 20 (95.2) | 19 (90.5) |
| Item 06 b —Level of education | 6 (28.6) | 8 (38.1) |
| Item 07 b —Social personality (introverted vs. extroverted) | 4 (19.0) | 4 (19.0) |
| Section A—PLWD | ||
| A1—Holding a 1‐on‐1 conversation | 21 (100.0) | 21(100.0) |
| A2—Participating in a group conversation | 19 (90.5) | 20 (95.2) |
| A3—Following TV/radio programs | 18 (85.7) | 19 (90.5) |
| A4 c —Using the phone | 21 (100.0) | 21(100.0) |
| A5—Speaking fluently | 21 (100.0) | 20 (95.2) |
| A6—Writing | 20 (95.2) | 21 (100.0) |
| A7—Reading | 21 (100.0) | 21 (100.0) |
| A8—Need for help with communication | 20 (95.2) | 18 (85.7) |
| A9—Comfort/confidence with communication abilities | 15 (71.4) | 16 (76.2) |
| Part two of items A1‐A9—Level of bother/frustration in relation to communication | 20 (95.2) | 21 (100.0) |
| Section B—support person (proxy, except where indicated) | ||
| B1—Holding a 1‐on‐1 conversation | 21 (100.0) | 21 (100.0) |
| B2—Participating in a group conversation | 21 (100.0) | 21 (100.0) |
| B3—Following TV/radio programs | 20 (95.2) | 19 (90.5) |
| B4 c —Using the phone | 21 (100.0) | 21 (100.0) |
| B5—Speaking fluently | 19 (90.5) | 19 (90.5) |
| B6—Writing | 20 (95.2) | 20 (95.2) |
| B7—Reading | 20 (95.2) | 21 (100.0) |
| B8—Need for help in conversation | 21 (100.0) | 21 (100.0) |
| B9—Comfort/confidence with communication abilities | 16 (76.2) | 17 (81.0) |
| B10—Difficulties communicating with the person with dementia (support person) | 21 (100.0) | 21 (100.0) |
| Part two of items B1–B9—level of bother/frustration | 19 (90.5) | 21 (100.0) |
| Part two of item B10—level of bother/frustration (support person) | 18 (85.7) | 20 (95.2) |
| Section C—Healthcare professional | ||
| C1—Verbal comprehension | 21 (100.0) | 21 (100.0) |
| C2—Verbal expression (content) | 21 (100.0) | 21 (100.0) |
| C3—Verbal expression (speech) | 21 (100.0) | 21 (100.0) |
| C4—Maintaining conversation | 21 (100.0) | 21 (100.0) |
| C5—Writing | 17 (81.0) | 18 (85.7) |
| C6—Reading | 19 (90.5) | 19 (90.5) |
| C7—Help with communication | 20 (95.2) | 20 (95.2) |
| C8—Comfort/confidence with communication abilities (proxy) | 18 (85.7) | 19 (90.5) |
Note: Grey highlighted items (Item 06 and Item 07) did not achieve 70% consensus in Round 3 and were omitted.
Ratings included are ‘Important’ or ‘Highly important’ and ‘Relevant’ or ‘Highly relevant’.
Items were added after Round 1.
Items were added after Round 2.
The three items with the lowest acceptable level of consensus in Round 3 for importance were Item 03, Pre‐Commencement Question section (Have you been diagnosed with depression?), (76.2%); Item A9, Section A (Recently, have you felt uncomfortable when talking to others?), (71.4%); and the corresponding Item B9 in Section B (Has the person with dementia appeared to feel uncomfortable when communicating with you or others?), (76.2%). Item A9 was the only item, which reached a comparatively low level of consensus regarding relevance (76.2%). Five and respectively six panel members provided a rating of 2 (‘Somewhat important/relevant’) for the above‐named items. However, none of the experts provided a rating of 1 (‘Not important at all’). Mean ratings for the three items were also relatively high for both importance and relevance with no mean rating below 3.15 (Table 4).
TABLE 4.
Mean rating (standard deviation) and range of items with the lowest acceptable level of consensus
| Pre‐commencement questions | Round 1 (n = 26) | Round 2 (n = 19) | Round 3 (n = 21) | |||
|---|---|---|---|---|---|---|
| Importance | Relevance | Importance | Relevance | Importance | Relevance | |
| Item 03—diagnosis of depression |
3.04 (0.84) 2–4 |
3.08 (0.86) 1–4 |
3.32 (0.67) 2–4 |
3.42 (0.69) 2–4 |
3.19 (0.8) 2–4 |
3.29 (0.72) 2–4 |
| Section A—PLWD | Round 1 (n = 24) | Round 2 (n = 19) | Round 3 (n = 21) | |||
| A9—comfort/confidence with communication abilities |
3.04 (0.75) 2–4 |
3.08 (0.65) 2–4 |
3.21 (0.63) 2–4 |
3.26 (0.45) 2–4 |
3.14 (0.85) 2–4 |
3.19 (0.81) 2–4 |
| Section B—Support Person | Round 1 (n = 23) | Round 2 (n = 19) | Round 3 (n = 21) | |||
| B9—comfort/confidence with communication abilities (proxy) |
3.17 (0.78) 2–4 |
3.17 (0.78) 2–4 |
3.32 (0.75) 2–4 |
3.32 (0.75) 2–4 |
3.24 (0.83) 2–4 |
3.29 (0.78) 2–4 |
Note: 1—not at all important/relevant; 2—somewhat important/relevant, 3—important/relevant, 4—highly important/relevant.
Two items were omitted based on low levels of consensus. Both items were part of the ‘Pre‐Commencement Questions’ section and were newly introduced in Round 2 (Item 06, How old were you when you finished school? and Item 07, Would you say you are generally a more introverted or a more extroverted person?). Out of 21 panel members who participated in Round 3, six rated Item 06 as ‘important’ and eight rated Item 06 as ‘relevant’. Only four panel members determined item 07 as ‘relevant/important’ or ‘highly relevant/important’.
3.3. Participant feedback and comments
Of interest were the panel members' feedback and explanatory comments. Feedback consisted of both brief comments and constructive feedback regarding item formulation, clarity and tool content. Following each round, panel members' feedback was analysed and suggestions for change were integrated into the tool where possible. A summary of the feedback suggestions is provided in Box 1.
BOX 1. Summary of qualitative feedback provided by panel members throughout three consecutive Delphi rounds.
|
Clarify the terms ‘support’ (used in items A8, B8 and C7) and ‘recently’ (used in items A8 and A9), and the phrase ‘feeling uncomfortable’ (used in items A9, B9 and C8) Provide space after each item to record details of communication difficulties if necessary Add items to determine current languages spoken, the pre‐morbid levels of literacy and general communicative nature/character of the client Add an item related to use of the telephone (using, answering, taking a message) Review the use of ‘pre‐morbid abilities’ in section C as this is a consideration which may be more accurately determined by the caregiver, not the clinician Separate examples of items covering a broad spectrum of abilities to clarify that any one of these abilities might be impaired and to avoid potential working memory limitations of the person with dementia (A5/B5, A6/B6 and B7) Avoid clinical jargon used in questions A5/B5 |
In most cases, changes made in accordance with suggestions led to increased levels of acceptance by the panel members in subsequent rounds. For example, for the three items with the lowest acceptable level of consensus mentioned above, (Items 03, A9 and B9), the panel suggested revision of wording to reduce ambiguity, which led to higher ratings of importance and relevance in Round 3. However, not all suggested changes resulted in consensus. This was the case for two items which were subsequently omitted due to low consensus (<40%) (Items 06 and 07, see above).
A number of comments indicated the need for further explanation of the tool purpose and justification of items to the panel. This included Items A5‐7 (Item A5, Do you have difficulty speaking fluently? For example, do you have trouble finding the right words, speaking fluently or speaking clearly?; Item A6, Do you have difficulty writing ANY of the following: A shopping list, a note, a letter a text message or an email?; Item A7, Do you have difficulty reading and understanding ANY of the following: A menu at a restaurant, a letter or a bill, newspapers, magazines or books, a text message or an email?), and Items B5‐7 (items are identical to section A, but proxy versions). For instance, Items A6/B6 address writing abilities of the person with dementia. Examples included in these items explore the ability of the person with dementia to write a letter, a shopping list or a text message on the phone. It was suggested that each example should be turned into a separate item to gain more detailed information about the nature of a person's difficulty. Clarification provided to the panel in response highlighted that items were deliberately formulated broadly with the purpose of minimising administration time because the CoSNAT‐D was not intended as a comprehensive speech‐language assessment tool. This would ensure suitability for users' scope of practice for users of multidisciplinary backgrounds.
All suggestions relating to rewording in Sections A and B (particularly for revision of Items A5, A9/B9) were typically addressed in the form of additional explanatory administrator comments, rather than rewording the item itself. This is because people with dementia and caregivers confirmed the face validity of these sections in stage 2 of the development phase (Krein et al., 2020).
3.4. Consistency of responses
The majority of the final items (32/35; 91%) were consistently rated as ‘highly important/important’ or ‘highly relevant/relevant’ by more than 70% of panel members throughout the three rounds. The lowest mean score for items with the lowest acceptable level of consensus in the final 35 items was 3.14 (on a scale of 1 to 4), indicating general consensus regarding the relevance and importance of items. For two items, consensus regarding importance fluctuated and also dropped below the 70% mark in at least one round, including Pre‐commencement Item 03 (Have you been diagnosed with depression) and Item C8 (Has the person with dementia appeared to feel uncomfortable when talking to you?). The proportions of panel members who rated these item as highly important/important was compared to assess the precision and whether there was any difference between each round (see Table 5). The 95% confidence intervals around the difference for the two items passed through 0 and indicated no statistically significant difference between the proportions. Therefore, the ratings can be considered not to differ, despite fluctuation between rounds.
TABLE 5.
Difference in proportions and 95% confidence intervals between rounds of items with inconsistent importance ratings
| Item | Difference in % (95% confidence interval) | ||
|---|---|---|---|
| Round 1 − Round 2 | Round 1 − Round 3 | Round 2 − Round 3 | |
| Item 03 (diagnosis of depression)—importance | 22.0 (−3.0, 46.0) | 8.0 (−18.0, 34.0) | 13.0 (−10.0, 37.0) |
| C8 (comfort/confidence with communication abilities)—importance | 5.0 (−24.0, 34.0) | 18.0 (−8.0, 43.0) | 26.0 (−4.0, 49.0) |
4. DISCUSSION
The aim of this paper was to establish the content validity of the items of the CoSNAT‐D. Content validity of the final set of 35 items could be demonstrated through high (>70%) consensus regarding relevance and importance, overall high mean ratings as well as stability of ratings throughout the three Delphi survey rounds. The majority (32) of the final 35 items received importance and relevance ratings above 80%. Two items of the ‘Pre‐Commencement Questions’ section were omitted as a result of low consensus (<40% in Round 3).
Two items which gained sufficient consensus to be included in the final item pool but were rated at the lower end of the pre‐determined minimum percentage deserve further discussion. Interestingly, the items were companion items in Sections A (person with dementia) and B (support person) of the tool. The items addressed feelings of discomfort in social situations, which may indicate a risk of social withdrawal or social isolation. They are: Item A8 (Recently, have you felt uncomfortable when talking to others? For example, you may have felt frustrated, embarrassed, angry, sad, disappointed or helpless?); Item B9 (Has the person with dementia felt uncomfortable when talking to others? For example, he/she may have looked frustrated, embarrassed, angry or sad?). Social withdrawal or isolation is a known consequence of LCI and depression, which are frequently reported not only for people with dementia but also for people living with other neurogenic conditions, such as stroke related aphasia (Johannessen & Möller, 2013; Northcott et al., 2016). While panellists provided many affirmative comments regarding the relevance and importance of these items throughout the three rounds, suggestions for improvement were related to clarification and the need for rewording. For example, panellists found interpretation of the items ambiguous, stating that it is unclear what people with dementia are frustrated/angry about and if discomfort relates to communication problems or other reasons. It thus appears that panel members generally agreed with the relevance and importance of the items and that low ratings were related to the formulation and wording.
4.1. Clinical relevance
Healthcare professionals who are involved in the routine care of people with dementia living the community and are not familiar with speech, language and communication assessment, such as nurses, occupational therapists, physiotherapists, or social workers, can use the CoSNAT‐D in their routine care. The tool has the potential to assist these professionals in the identification of communication difficulties in dementia and provide them with guidance to undertake the next appropriate management steps. For example, the results of the CoSNAT‐D might suggest that the person with dementia is experiencing language and communication difficulties. However, a referral to specialist services may not be indicated at the time of the screening because the person with dementia and the caregiver are not worried or frustrated by the difficulties they are experiencing. In this case, rather than initiating a referral, a communication information package could be provided and a review scheduled for a later point in time.
Communication difficulties for people with dementia are widely reported in both informal and formal care settings, such in hospital settings, residential care facilities and in the community care context (Eggenberger et al., 2013; O'Halloran et al., 2017; Robinson & Cubit, 2007). Communication breakdown in formal care settings can lead to a reduction in quality of care and care recipient satisfaction (Bartlett et al., 2008; Lawthers et al., 2003). The appropriate implementation of the CoSNAT‐D is expected to lead to an enhanced identification of LCI‐associated support needs in people with dementia, which has the potential to improve timely and appropriate care provision for people with dementia, their families as well as care staff.
Speech, language and communication support in form of cognitive linguistic intervention, speech and language therapy, and communication partner training can positively affect quality of life, discourse performance and word finding abilities (Croot et al., 2015; Eggenberger et al., 2013; Haberstroh et al., 2011; Mahendra & Arkin, 2003). The use of the CoSNAT‐D is not only relevant for making decisions regarding adequate referrals to specialist services but also to facilitate the use of non‐pharmacological therapy for timely management of LCI and its impact on participation in everyday life. It is anticipated that the CoSNAT‐D can contribute to healthcare professionals' awareness of LCI and can be a source for potential management strategies. Lack of knowledge about professional available support, such as speech language pathology, has been identified as a potential reason for a gap in service delivery for people with dementia and LCI (Taylor et al., 2009; Volkmer et al., 2018, 2019).
4.2. Limitations
A limitation of this study is the anonymous nature of this survey. While complete anonymity allowed for bias‐free interpretation of results, it hindered more in‐depth analysis of items that reached comparatively low or no consensus, and the panel characteristics of each round, as the number of panel members fluctuated in each round. Due to full anonymity, it was not possible to track which of the consenting experts completed which of the Delphi rounds. Knowing if a panel member may have, for example, only participated in Round 3, but not the previous two rounds, or tracking experts' individual consistency of importance/relevance ratings may have aided analysis of panel responses. This is particularly true for items with lower or fluctuating consensus. In addition, judgement of items may differ depending on the expert's professional background. That is, a clinical professional who works directly with patients with dementia and their caregivers may rate importance and relevance differently than a researcher working purely in an academic context with this demographic group. While elimination of these limitations may have improved interpretation and analysis of results, the number of items that received relatively low or no consensus was small, and the ratings of items with lower consensus were still high. Moreover, the two items which did not gain consensus were part of the Pre‐Commencement Questions section, which provided background information, and were not part of the sections that directly addressed language and communication.
4.3. Future directions
Future development studies are needed to fully establish the CoSNAT‐D as a reliable and valid tool for use in community care settings. This includes the development of a scoring system and indications for internal consistency, interrater reliability and criterion validity. Feedback from multidisciplinary healthcare professionals administering the tool will also be sought as part of future pilot testing in the community context. A traffic light scoring system may be a viable option for the CoSNAT‐D. Traffic light scoring systems are easy and intuitive in their application and are used in other healthcare needs‐assessment tools. Colour codes (typically green, amber, red) are used to indicate the degree of urgency for a certain action, see for example, the Dutch screening tool for the early identification of undernutrition in residential care Short Nutritional Assessment Questionnaire for Residential Care (SNAQRC) (Kruizenga et al., 2010).
In conclusion, the CoSNAT‐D is the only tool for identification of communication support needs for people living with dementia. The items of this tool have been reviewed both by representatives of the target population (people living with dementia and carers) and experts in dementia and demonstrate adequate face validity and content validity. Further research is required to test the CoSNAT‐D pilot version in a community care context and to establish further relevant psychometric properties.
AUTHOR CONTRIBUTIONS
Luisa Krein is the corresponding author. She designed the study, completed the data collection, analysis and drafted the manuscript. Yun‐Hee Jeon and Amanda Miller Amberber contributed to the design of the study, critically reviewed data analysis, provided guidance and assisted in the revisions of drafts. Judith Fethney provided guidance in the writing of the manuscript with a particular focus on statistical content of this manuscript.
FUNDING INFORMATION
The corresponding author received a PhD scholarship grant from the Royal Freemasons' Benevolent Institution.
CONFLICT OF INTEREST
The authors declare no conflict of interest.
Supporting information
Supplementary material 1 Initial CoSNAT‐D item pool (items presented to panel in Delphi Survey Round 1) with corresponding language/communication domains and International Classification of Function, disability and health (ICF) (World Health Organisation, 2001) codes. Please note that additionalcomments aiding completion are not included.
Supplementary material 2 ICF code descriptions relating to codes in Supplemental material 1
Supplementary material 3 Number (percentage) of panel members rating item as either ‘important/relevant’ or ‘highly important/highly relevant’
ACKNOWLEDGEMENTS
We would like to acknowledge the Freemason's Benevolent Institution who has provided a PhD scholarship to the first author. We would like to warmly thank and acknowledge the Delphi panel who provided expert advice for the content validation of this tool. Open access publishing facilitated by The University of Sydney, as part of the Wiley ‐ The University of Sydney agreement via the Council of Australian University Librarians.
Krein, L. , Jeon, Y‐H , Miller Amberber, A. , & Fethney, J. (2022). Communication support needs assessment in dementia (CoSNAT‐D): An international content validation study. Health & Social Care in the Community, 30, e4745–e4757. 10.1111/hsc.13881
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available in the article and in the supplementary material of this article. CoSNAT‐D items are available on request from the authors due to copyright.
REFERENCES
- Agency for Clinical Innovation . (2016). Allied health professionals and you: A guide for people living with dementia and their carers. Agency for Clinical Innovation. [Google Scholar]
- American Speech‐Language‐Hearing Association . (2020). Dementia. Retrieved from https://www.asha.org/public/speech/disorders/dementia/
- AusVet . (2019). 2‐sample z‐test to compare sample proportion. http://epitools.ausvet.com.au/content.php?page=z‐test‐2
- Ballard, C. , O'Brien, J. , James, I. , Mynt, P. , Lana, M. , Potkins, D. , Reichelt, K. , Lee, L. , Swann, A. , Fossey, J. , & Fossey, J. (2001). Quality of life for people with dementia living in residential and nursing home care: The impact of performance on activities of daily living, behavioral and psychological symptoms, language skills, and psychotropic drugs. International Psychogeriatrics, 13(1), 93–106. 10.1017/S1041610201007499 [DOI] [PubMed] [Google Scholar]
- Bartlett, G. , Blais, R. , Tamblyn, R. , Clermont, R. J. , & MacGibbon, B. (2008). Impact of patient communication problems on the risk of preventable adverse events in acute care settings. Canadian Medical Association Journal, 178(12), 1555–1562. 10.1503/cmaj.070690 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beales, A. , Bates, K. , Cartwright, J. , & Whitworth, A. (2019). Lost for words: Perspectives and experiences of people with primary progressive aphasia and Alzheimer's disease and their families of participation in a lexical retrieval intervention. International Journal of Speech‐Language Pathology, 21(5), 483–492. 10.1080/17549507.2019.1625439 [DOI] [PubMed] [Google Scholar]
- Boschi, V. , Catricalà, E. , Consonni, M. , Chesi, C. , Moro, A. , & Cappa, S. F. (2017). Connected speech in neurodegenerative language disorders: A review. Frontiers in Psychology, 8(269), 1–21. 10.3389/fpsyg.2017.00269 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bryan, K. , & Maxim, J. (2006). Communication disability in the dementias. Whurr Publishers. [Google Scholar]
- Clare, L. (2017). Rehabilitation for people living with dementia: A practical framework of positive support. PLoS Medicine, 14(3), e1002245. 10.1371/journal.pmed.1002245 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Colton, S. , & Hatcher, T. (2004). The web‐based Delphi research technique as a method for content validation in HRD and adult education research. Paper presented at the Academy of Human Resource Development International Conference (AHRD), Austin, TX.
- Croot, K. , Taylor, C. , Abel, S. , Jones, K. , Krein, L. , Hameister, I. , Ruggero, L. , & Nickels, L. (2015). Measuring gains in connected speech following treatment for word retrieval: A study with two participants with primary progressive aphasia. Aphasiology, 29(11), 1265–1288. 10.1080/02687038.2014.975181 [DOI] [Google Scholar]
- Eggenberger, E. , Heimerl, K. , & Bennett, M. I. (2013). Communication skills training in dementia care: A systematic review of effectiveness, training content, and didactic methods in different care settings. International Psychogeriatrics, 25(3), 345–358. 10.1017/S1041610212001664 [DOI] [PubMed] [Google Scholar]
- Ewing, G. , Brundle, C. , Payne, S. , & Grande, G. (2013). The Carer support needs assessment tool (CSNAT) for use in palliative and end‐of‐life Care at Home: A validation study. Journal of Pain and Symptom Management, 46(3), 395–405. 10.1016/j.jpainsymman.2012.09.008 [DOI] [PubMed] [Google Scholar]
- Graham, N. L. (2014). Dysgraphia in primary progressive aphasia: Characterisation of impairments and therapy options. Aphasiology, 28(8–9), 1092–1111. 10.1080/02687038.2013.869308 [DOI] [Google Scholar]
- Guideline Adaptation Committee . (2016). Clinical practice guidelines and principles of care for people with dementia. Guideline Adaptation Committee. [Google Scholar]
- Haberstroh, J. , Neumeyer, K. , Krause, K. , Franzmann, J. , & Pantel, J. (2011). TANDEM: Communication training for informal caregivers of people with dementia. Aging & Mental Health, 15(3), 405–413. 10.1080/13607863.2010.536135 [DOI] [PubMed] [Google Scholar]
- Habibi, A. , Sarafrazi, A. , & Izadyar, S. (2014). Delphi technique theoretical framework in qualitative research. The International Journal of Engineering and Science, 3(4), 8–13. [Google Scholar]
- Hall, D. A. , Smith, H. , Heffernan, E. , & Fackrell, K. (2018). Recruiting and retaining participants in e‐Delphi surveys for core outcome set development: Evaluating the COMiT'ID study. PLoS ONE, 13(7), e0201378. 10.1371/journal.pone.0201378 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harciarek, M. , & Kertesz, A. (2009). Longitudinal study of single‐word comprehension in semantic dementia: A comparison with primary progressive aphasia and Alzheimer's disease. Aphasiology, 23(5), 606–626. 10.1080/02687030801890891 [DOI] [Google Scholar]
- Harris, P. A. , Taylor, R. , Thielke, R. , Payne, J. , Gonzalez, N. , & Conde, J. G. (2009). Research electronic data capture (REDCap)—A metadata‐driven methodology and workflow process for providing translational research informatics support. Journal of Biomedical Informatics, 42(2), 377–381. 10.1016/j.jbi.2008.08.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hsu, C.‐C. , & Sandford, B. A. (2007a). The Delphi technique: Making sense of consensus. Practical Assessment, Research & Evaluation, 12(10), 1–8. 10.7275/pdz9-th90 [DOI] [Google Scholar]
- Hsu, C.‐C. , & Sandford, B. A. (2007b). Minimizing non‐response in the Delphi process: How to respond to non‐response. Practical Assessment, Research & Evaluation, 12(17), 62–78. 10.7275/by88-4025 [DOI] [Google Scholar]
- Johannessen, A. , & Möller, A. (2013). Experiences of persons with early‐onset dementia in everyday life: A qualitative study. Dementia, 12(4), 410–424. 10.1177/1471301211430647 [DOI] [PubMed] [Google Scholar]
- Jokel, R. , Lima, B. S. , Fernandez, A. , & Murphy, K. J. (2019). Language in amnestic mild cognitive impairment and dementia of Alzheimer's type: Quantitatively or qualitatively different? Dementia and Geriatric Cognitive Disorders Extra, 9(1), 136–151. 10.1159/000496824 [DOI] [Google Scholar]
- Keeney, S. , Hasson, F. , & McKenna, H. P. (2010a). The Delphi technique. In Keeney S., Hasson F., & McKenna H.P., (Eds.), The Delphi technique in nursing and health research (pp. 1–17). Wiley‐Blackwell. [Google Scholar]
- Keeney, S. , Hasson, F. , & McKenna, H. P. (2010b). Analysing data from a Delphi and reporting results. In Keeney S., Hasson F., & McKenna H.P. (Eds.), The Delphi technique in nursing and health research (pp. 84–95). Wiley‐Blackwell. [Google Scholar]
- Klimova, B. , & Kuca, K. (2016). Speech and language impairments in dementia. Journal of Applied Biomedicine, 14, 97–103. 10.1016/j.jab.2016.02.002 [DOI] [Google Scholar]
- Krein, L. , Jeon, Y.‐H. , & Miller Amberber, A. (2020). Development of a new tool for the early identification of communication‐support needs in people living with dementia: An Australian face‐validation study. Health & Social Care in the Community, 28(2), 544–554. 10.1111/hsc.12887 [DOI] [PubMed] [Google Scholar]
- Krein, L. , Jeon, Y.‐H. , Miller Amberber, A. , & Fethney, J. (2019). The assessment of language and communication in dementia: A synthesis of evidence. The American Journal of Geriatric Psychiatry, 27(4), 363–377. 10.1016/j.jagp.2018.11.009 [DOI] [PubMed] [Google Scholar]
- Kruizenga, H. M. , De Vet, H. C. W. , Van Marissing, C. M. E. , Stassen, E. E. P. , Strijk, J. E. , Van Bokhorst‐de Van der Schueren, M. A. V. , Horman, J. C. H. , Schols, J. M. G. A. , Van Binsbergen, J. J. , Eliens, A. , Knol, D. L. , & Visser, M. (2010). The SNAQ RC, an easy traffic light system as a first step in the recognition of undernutrition in residential care. The Journal of Nutrition, Health & Aging, 14(2), 83–89. 10.1007/s12603-009-0147-1 [DOI] [PubMed] [Google Scholar]
- Lawthers, A. G. , Pransky, G. S. , Peterson, L. E. , & Himmelstein, J. H. (2003). Rethinking quality in the context of persons with disability. International Journal for Quality in Health Care, 15(4), 287–299. 10.1093/intqhc/mzg048 [DOI] [PubMed] [Google Scholar]
- Mahendra, N. , & Arkin, S. (2003). Effects of four years of exercise, language, and social interventions on Alzheimer discourse. Journal of Communication Disorders, 36(5), 395–422. 10.1016/S0021-9924(03)00048-0 [DOI] [PubMed] [Google Scholar]
- McWalter, G. , Toner, H. , Corser, A. , Eastwood, J. , Marshall, M. , & Turvey, T. (1994). Needs and needs assessment: Their components and definitions with reference to dementia. Health & Social Care in the Community, 2(4), 213–219. 10.1111/j.1365-2524.1994.tb00167.x [DOI] [Google Scholar]
- McWalter, G. , Toner, H. , McWalter, A. , Eastwood, J. , Marshall, M. , & Turvey, T. (1998). A community needs assessment: The care needs assessment pack for dementia (CarenapD)—Its development, reliability and validity. International Journal of Geriatric Psychiatry, 13(1), 16–22. [DOI] [PubMed] [Google Scholar]
- National Institute for Health and Care Excellence . (2016). Dementia: Supporting people with dementia and their carers in health and social care. In Nice guideline. National Institute for Health and Care Excellence. [Google Scholar]
- Nickels, L. , & Croot, K. (2014). Understanding and living with primary progressive aphasia: Current progress and challenges for the future. Aphasiology, 28(8–9), 885–899. 10.1080/02687038.2014.933521 [DOI] [Google Scholar]
- Northcott, S. , Moss, B. , Harrison, K. , & Hilari, K. (2016). A systematic review of the impact of stroke on social support and social networks: Associated factors and patterns of change. Clinical Rehabilitation, 30(8), 811–831. 10.1177/0269215515602136 [DOI] [PubMed] [Google Scholar]
- O'Halloran, R. , Coyle, J. , & Lamont, S. (2017). Screening patients for communication difficulty: The diagnostic accuracy of the IFCI staff questionnaire. International Journal of Speech‐Language Pathology, 19(4), 430–440. 10.1080/17549507.2016.1209560 [DOI] [PubMed] [Google Scholar]
- Reilly, J. , Rodriguez, A. D. , Lamy, M. , & Neils‐Strunjas, J. (2010). Cognition, language, and clinical pathological features of non‐Alzheimer's dementias: An overview. Journal of Communication Disorders, 43(5), 438–452. 10.1016/j.jcomdis.2010.04.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reynolds, T. , Thornicroft, G. , Abas, M. , Woods, B. , Hoe, J. , Leese, M. , & Orrell, M. (2000). Camberwell assessment of need for the elderly (CANE): Development, validity and reliability. British Journal of Psychiatry, 176(5), 444–452. 10.1192/bjp.176.5.444 [DOI] [PubMed] [Google Scholar]
- Robinson, A. , & Cubit, K. (2007). Caring for older people with dementia in residential care: Nursing students' experiences. Journal of Advanced Nursing, 59(3), 255–263. 10.1111/j.1365-2648.2007.4304.x [DOI] [PubMed] [Google Scholar]
- Speech Pathology Australia . (2012). An inquiry into dementia early diagnosis and intervention. Speech Pathology Australia. [Google Scholar]
- Taylor, C. , Kingma, R. M. , Croot, K. , & Nickels, L. (2009). Speech pathology services for primary progressive aphasia: Exploring an emerging area of practice. Aphasiology, 23(2), 161–174. 10.1080/02687030801943039 [DOI] [Google Scholar]
- Volkmer, A. (2013). Assessment and therapy for language and cognitive communication difficulties in dementia and other progressive diseases. J & R Press Ltd. [Google Scholar]
- Volkmer, A. , Spector, A. , Meitanis, V. , Warren, J. D. , & Beeke, S. (2019). Effects of functional communication interventions for people with primary progressive aphasia and their caregivers: A systematic review. Aging & Mental Health, 24(9), 1381–1393. 10.1080/13607863.2019.1617246 [DOI] [PubMed] [Google Scholar]
- Volkmer, A. , Spector, A. , Warren, J. D. , & Beeke, S. (2018). Speech and language therapy for primary progressive aphasia: Referral patterns and barriers to service provision across the UK. Dementia, 19, 1349–1363. 10.1177/1471301218797240 [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization . (2001). International classification of functioning, disability and health (ICF) .
- World Health Organization . (2002). Towards a common language for functioning, disability and health .
- World Health Organization . (2011). World report on disability .
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary material 1 Initial CoSNAT‐D item pool (items presented to panel in Delphi Survey Round 1) with corresponding language/communication domains and International Classification of Function, disability and health (ICF) (World Health Organisation, 2001) codes. Please note that additionalcomments aiding completion are not included.
Supplementary material 2 ICF code descriptions relating to codes in Supplemental material 1
Supplementary material 3 Number (percentage) of panel members rating item as either ‘important/relevant’ or ‘highly important/highly relevant’
Data Availability Statement
The data that support the findings of this study are available in the article and in the supplementary material of this article. CoSNAT‐D items are available on request from the authors due to copyright.


