Abstract
In this subgroup analysis of the randomized, Phase 3 IKEMA study (NCT03275285), we evaluated efficacy and safety of the anti‐CD38 monoclonal antibody isatuximab (Isa) in combination with carfilzomib‐dexamethasone (Isa‐Kd) versus Kd in older (≥70 years of age, n = 86) and younger (<70 years, n = 216) patients with relapsed multiple myeloma (MM). Patients received Isa 10 mg/kg intravenously weekly for 4 weeks, then every 2 weeks in the Isa‐Kd arm, and approved schedule of carfilzomib (twice weekly) and dexamethasone in both study arms. Primary endpoint was progression‐free survival (PFS); key secondary efficacy endpoints included rates of overall response (ORR), very good partial response or better (≥VGPR), minimal residual disease negativity (MRD–), and complete response (CR). Addition of Isa to Kd resulted in improved PFS in elderly patients (hazard ratio, 0.36 [95% CI, 0.18–0.75]) consistent with the significant PFS improvement observed in the overall IKEMA population. Treatment with Isa‐Kd improved depth of response versus Kd, with higher rates of ≥VGPR (73.1% vs. 55.9%), MRD– (23.1% vs. 11.8%), and CR (38.5% vs. 23.5%). Although the incidence of grade ≥3 treatment‐emergent adverse events (TEAEs) was higher in Isa‐Kd, the incidence of serious TEAEs was similar between arms. Fewer elderly patients definitively discontinued treatment due to TEAEs in Isa‐Kd than Kd: 11.8% versus 23.5%. In conclusion, Isa‐Kd provides a consistent benefit versus Kd in elderly patients, with a manageable safety profile, and represents a new treatment option for patients with relapsed MM, independent of age.
Keywords: CD38, elderly, isatuximab, monoclonal antibody, multiple myeloma
1. INTRODUCTION
Multiple myeloma (MM) often affects older patients, as it is most frequently diagnosed in 65 to 74‐year‐old subjects, with a median age of approximately 69–70 years 1 , 2 The increase in life expectancy currently being achieved in many countries contributes to the observed increase in the global elderly population of patients with MM. 3 Older patients represent a heterogeneous population, which may present with comorbidities, a reduced functional status, and an increased risk of frailty potentially affecting therapeutic outcomes. 4 , 5 , 6
Although treatment with proteasome inhibitors (PIs) and immunomodulatory agents (IMiDs) provides benefit to MM patients, new therapeutic approaches are still needed for older as well as younger MM patients. 5 , 6 Anti‐CD38 antibody therapy with isatuximab (Isa) in combination with an IMiD or a PI and low‐dose dexamethasone represents such an option for patients with relapsed and/or refractory MM (RRMM). 7 , 8 , 9 , 10 , 11 , 12 , 13 Isa (an IgG1 monoclonal antibody) binds to a specific CD38 epitope and exerts anti‐myeloma activity through multiple mechanisms, which is enhanced by combination with IMiD and PI agents. 7 , 8 Based on the Phase 3 ICARIA‐MM study, Isa is approved in a number of countries in combination with pomalidomide and dexamethasone (Pd) for patients with RRMM (≥2 prior treatment lines). 9 , 12 , 13 Furthermore, to date, Isa in combination with carfilzomib and dexamethasone (Kd) is approved in the United States for patients with relapsed MM (≥1–3 prior lines), in the European Union for patients with MM who have received ≥1 prior therapy, and in Japan for patients with RRMM after one prior therapy, based on a prespecified interim analysis of the IKEMA study. 11 , 12 , 13 , 14
IKEMA was a randomized, multi‐national, parallel‐group, Phase 3 study that evaluated treatment with Isa in combination with Kd versus Kd in patients with relapsed MM. 11 Isa‐Kd significantly improved progression‐free survival (PFS) compared with Kd (hazard ratio [HR], 0.53; 99% confidence interval [CI], 0.32–0.89; one‐sided p = 0.0007), with clinically meaningful increases in the rates of very good partial response (VGPR) or better (72.6% vs. 56.1%), minimal residual disease negativity (MRD–, 29.6% vs. 13.0%), and complete response (CR, 39.7% vs. 27.6%), in the intent‐to‐treat (ITT) population, as well as a manageable safety profile. 11
As the median age of patients with MM is ∼70 years and survival with conventional therapies is still limited in the older adult population, 1 , 4 in this subgroup analysis of IKEMA, we evaluated efficacy and safety of treatment with Isa‐Kd versus Kd in elderly MM patients ≥70 years of age as well as in younger MM patients (<70 years of age).
2. METHODS
2.1. Study design, patients, and treatment
IKEMA (NCT03275285) was a prospective, randomized, open‐label, active‐controlled, Phase 3 study conducted in 16 countries at 69 study centers. Detailed inclusion and exclusion criteria were reported previously. 11 Briefly, eligible adults had relapsed MM following 1–3 prior treatment lines, with measurable evidence of disease (serum M‐protein ≥0.5 g/dl and/or urine M‐protein ≥200 mg/24 h). Patients with an estimated glomerular filtration rate ≥15 ml/min/1.73 m2 or prior pulmonary comorbidities (i.e., chronic obstructive pulmonary disease) were eligible. Patients were excluded if they had primary refractory MM or serum free‐light chain measurable disease only, were refractory to anti‐CD38 antibody therapy, had received prior carfilzomib therapy, or had a left ventricular ejection fraction <40%.
Patients were randomized 3:2 to receive Isa‐Kd (n = 179) or Kd (n = 123). In the Isa‐Kd arm, patients received Isa 10 mg/kg intravenously (IV) weekly (QW) for 4 weeks, then every 2 weeks (Q2W). Patients in both arms received approved schedules of Kd with carfilzomib 20/56 mg/m2, as described. 11
The study protocol was approved by the Institutional Ethics Committee or independent review board for each center; the study was conducted following the Declaration of Helsinki and IHC Guidelines for Good Clinical Practice. All patients provided written informed consent.
2.2. Study endpoints and assessments
Primary study endpoint was PFS, as determined by a blinded independent response committee (IRC), which evaluated response and disease progression according to the International Myeloma Working Group (IMWG) response criteria, 15 measured by central radiological evaluation, central laboratory M‐protein quantification, and local bone marrow aspiration when needed.
Key secondary efficacy endpoints included rates of overall response (ORR), ≥VGPR, MRD−, and CR. MRD was assessed in patients with ≥VGPR, by central laboratory next‐generation sequencing (minimum sensitivity: 1/105 nucleated cells) (Adaptive clonoSEQ Assay, Adaptive Biotechnologies, Seattle, WA). M‐protein was assessed each cycle/day 1, at end of treatment, and monthly in follow‐up of patients with no progression at end of treatment. Bone lytic disease was assessed once/year and existing baseline plasmacytoma every 12 weeks.
Adverse events (AEs) and laboratory abnormalities were monitored and graded using the NCI‐CTCAE criteria v4.03. Safety was regularly reviewed by an independent Data Monitoring Committee.
2.3. Statistical analysis
In this subgroup analysis, efficacy and safety of treatment with Isa‐Kd versus Kd were evaluated in patients from the IKEMA study who were ≥70 and <70 years of age. All efficacy analyses were conducted in the ITT population. Median PFS and 95% CIs were calculated using the Kaplan‐Meier method. HRs were estimated by subgroup (≥70 and <70 years) using a non‐stratified Cox proportional‐hazard model with terms for the factor, treatment, and their interaction. The interaction test was performed at the 10% alpha level for descriptive purpose. Treatment‐emergent AEs (TEAEs) were evaluated in the safety population. SAS 9.4 software (SAS, Cary, NC) was used for all the analyses.
3. RESULTS
3.1. Patients and treatment exposure
Baseline characteristics are presented by subgroup in Table 1. Patient age was balanced between treatment arms and it ranged from 33 to 90 years. Among the 302 randomized patients, 28.5% were elderly (≥70 years): 29.1% in Isa‐Kd, 27.6% in Kd and 71.5% were <70 years of age: 70.9% in Isa‐Kd, 72.4% in Kd. Overall, patients had received a median of 2 prior treatment lines (range, 1–4). More elderly patients were refractory to lenalidomide in the Kd (52.9%) than the Isa‐Kd (34.6%) arm, but fewer of them had renal function impairment in Kd (22.6%) than in Isa‐Kd (33.3%). Median treatment duration was longer with Isa‐Kd versus Kd for both elderly and younger patients (75.1 vs. 50.5 and 80.5 vs. 63.1 weeks, respectively) (Table 2). The median relative dose intensities for carfilzomib were comparable across treatment subgroups, and independent of age for both Isa and carfilzomib (Table 2).
TABLE 1.
Patient baseline characteristics by age group: ≥70 and <70 years, ITT population
| ≥70 Years (n = 86) | <70 Years (n = 216) | |||
|---|---|---|---|---|
| Isa‐Kd (n = 52) | Kd (n = 34) | Isa‐Kd (n = 127) | Kd (n = 89) | |
| Median age, years (range) | 73 (70–86) | 74 (70–90) | 61 (37–69) | 61 (33–69) |
| ISS stage at study entry, n (%) | ||||
| Stage I | 25 (48.1) | 16 (47.1) | 64 (50.4) | 55 (61.8) |
| Stage II | 20 (38.5) | 11 (32.4) | 43 (33.9) | 20 (22.5) |
| Stage III | 7 (13.5) | 6 (17.6) | 19 (15.0) | 14 (15.7) |
| Unknown | 0 | 1 (2.9) | 1 (0.8) | 0 |
| R‐ISS stage at study entry, n (%) | ||||
| Stage I | 14 (26.9) | 8 (23.5) | 31 (24.4) | 25 (28.1) |
| Stage II | 32 (61.5) | 22 (64.7) | 78 (61.4) | 48 (53.9) |
| Stage III | 5 (9.6) | 2 (5.9) | 11 (8.7) | 6 (6.7) |
| Not classified | 1 (1.9) | 2 (5.9) | 7 (5.5) | 10 (11.2) |
| Cytogenetic risk, a n (%) | ||||
| High risk | 11 (21.2) | 9 (26.5) | 31 (24.4) | 22 (24.7) |
| Standard risk | 33 (63.5) | 22 (64.7) | 81 (63.8) | 56 (62.9) |
| Unknown | 8 (15.4) | 3 (8.8) | 15 (11.8) | 11 (12.4) |
| Prior lines of therapy | ||||
| Median (range) | 2 (1–4) | 2 (1–4) | 2 (1–4) | 2 (1–3) |
| 1 line, n (%) | 24 (46.2) | 11 (32.4) | 55 (43.3) | 44 (49.4) |
| ≥2 lines, n (%) | 28 (53.8) | 23 (67.6) | 72 (56.7) | 45 (50.6) |
| Patients refractory to, n (%) | ||||
| Lenalidomide | 18 (34.6) | 18 (52.9) | 39 (30.7) | 24 (27.0) |
| IMiD and PI | 9 (17.3) | 10 (29.4) | 26 (20.5) | 17 (19.1) |
| Baseline eGFR, b n/n (%) | ||||
| ≥60 ml/min/1.73 m2 | 32/48 (66.7) | 24/31 (77.4) | 88/115 (76.5) | 68/79 (86.1) |
| <60 ml/min/1.73 m2 | 16/48 (33.3%) | 7/31 (22.6%) | 27/115 (23.5) | 11/79 (13.9) |
Abbreviations: d, dexamethasone; eGFR, estimated glomerular filtration rate; IMiD, immunomodulatory drug; Isa, isatuximab; ISS, International Staging System; ITT, intent‐to‐treat; K, carfilzomib; PI, proteasome inhibitor; R‐ISS, revised International Staging System.
High risk was defined as del(17p), t(4; 14), or t(14; 16) by fluorescence in situ hybridization. Cytogenetic risk was assessed by a central laboratory with a cut‐off of 50% for del(17p), and 30% for t(4; 14) and t(14; 16).
Baseline eGFR by the modification of diet in renal disease (MDRD) equation.
TABLE 2.
Overall extent of exposure by age group: ≥70 and <70 years, safety population
| ≥70 Years (n = 85) | <70 Years (n = 214) | |||
|---|---|---|---|---|
| Isa‐Kd (n = 51) | Kd (n = 34) | Isa‐Kd (n = 126) | Kd (n = 88) | |
| Median number of cycles started (range) | 19.0 (1–27) | 12.5 (1–22) | 19.5 (1–26) | 15.0 (1–28) |
| Median treatment duration, weeks (range) | 75.1 (4–111) | 50.5 (4–94) | 80.5 (1–105) | 63.1 (1–114) |
| Median relative dose intensity, % (range) | ||||
| Isatuximab | 93.41 (66.7–102.2) | N.A. | 94.51 (76.6–108.2) | N.A. |
| Carfilzomib | 90.29 (18.2–108.7) | 91.31 (41.8–103.7) | 91.49 (25.6–107.5) | 91.44 (48.5–108.6) |
| Dexamethasone | 81.25 (37.1–100.2) | 81.87 (31.2–101.6) | 86.96 (24.5–101.1) | 90.21 (27.4–101.1) |
Abbreviations: d, dexamethasone; Isa, isatuximab; K, carfilzomib; N.A., not applicable.
3.2. Efficacy
The combination of Isa with Kd resulted in improved PFS independently of age, with a HR of 0.36 (95% CI, 0.18–0.75) in elderly patients and 0.61 (95% CI, 0.38–0.97) in younger patients, which were consistent with the significant PFS improvement observed in the overall IKEMA population (Figures 1 and 2). 11
FIGURE 1.
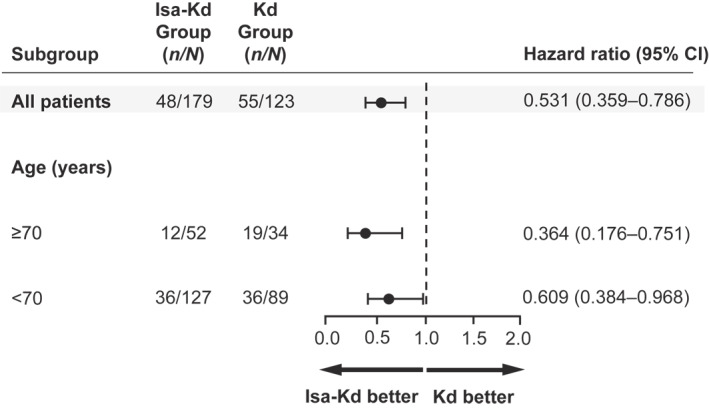
Progression‐free survival by IRC in patients ≥70 and <70 years of age, in the intent‐to‐treat population. CI, confidence interval; d, dexamethasone; IRC, Independent Response Committee; Isa, isatuximab; K, carfilzomib
FIGURE 2.
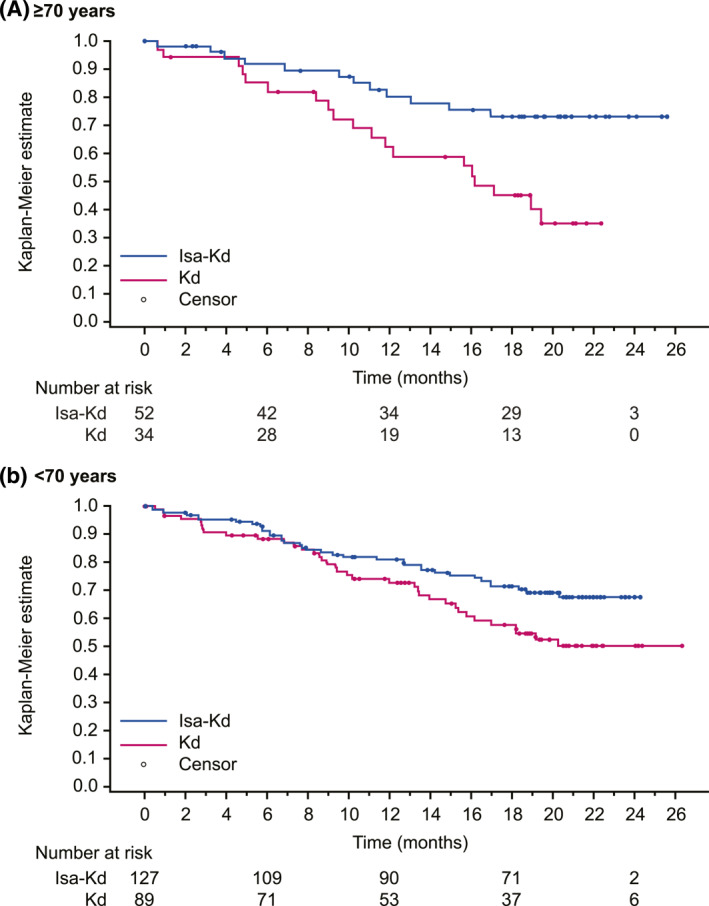
Progression‐free survival by IRC—Kaplan‐Meier estimates by age group (≥70 and <70 years), in the intent‐to‐treat population. d, dexamethasone; IRC, Independent Response Committee; Isa, isatuximab; ITT, intent‐to‐treat; K, carfilzomib; PFS, progression‐free survival
At the time of this analysis in elderly patients, median PFS with Isa‐Kd had not been reached (NR) (95% CI, NR–NR), whereas in Kd it was 16.2 months (95% CI, 10.3–NR). Median PFS had not been reached in either study arm in younger patients (95% CI, 15.8–NR in Kd).
Addition of Isa to Kd improved the depth of response, with higher rates of ≥VGPR, MRD–, and CR with Isa‐Kd versus Kd. Within the Isa‐Kd arm, ≥VGPR and CR rates were similar in elderly and younger patients (Figure 3). MRD negativity with Isa‐Kd was reached in 23.1% of older patients (vs. 11.8% with Kd) and 32.3% of younger patients (vs. 13.5% with Kd).
FIGURE 3.
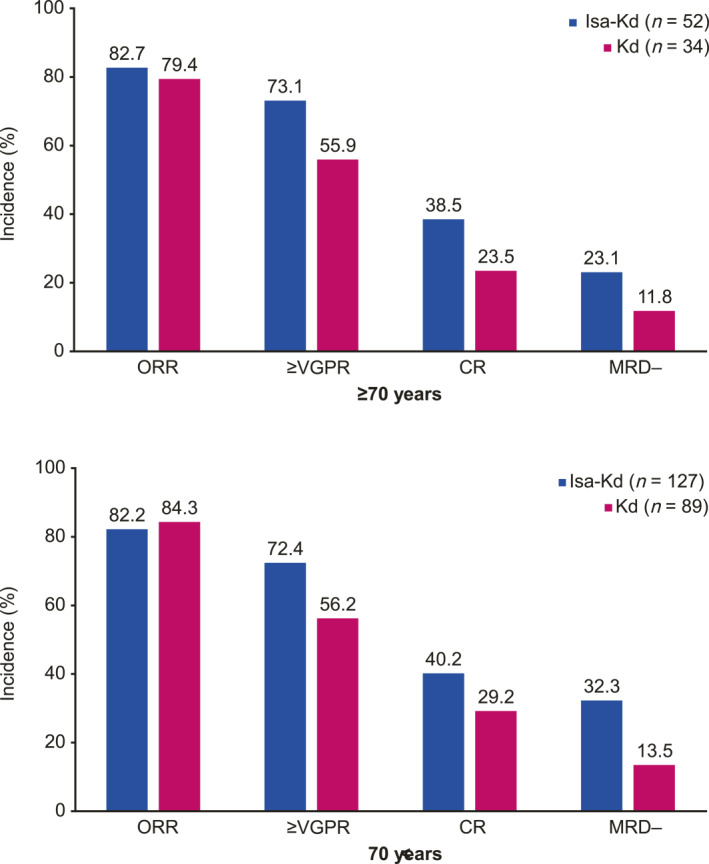
Response rates based on IRC assessment by age group: ≥70 and <70 years. CR, complete response; d, dexamethasone; IRC, Independent Response Committee; Isa, isatuximab; K, carfilzomib; MRD–, minimal residual disease negativity; ORR, overall response rate; VGPR, very good partial response
3.3. Safety
Grade ≥3 and serious TEAEs were more frequently reported in the elderly than the younger patients in both arms, as expected (Table 3).
TABLE 3.
Safety summary by age group: ≥70 and <70 years, safety population
| ≥70 Years (n = 85) | <70 Years (n = 214) | |||
|---|---|---|---|---|
| n (%) | Isa‐Kd (n = 51) | Kd (n = 34) | Isa‐Kd (n = 126) | Kd (n = 88) |
| Any grade ≥3 TEAE | 46 (90.2) | 26 (76.5) | 90 (71.4) | 56 (63.6) |
| Any serious TEAE a | 37 (72.5) | 24 (70.6) | 68 (54.0) | 46 (52.3) |
| Any grade 5 TEAE b | 3 (5.9) | 1 (2.9) | 3 (2.4) | 3 (3.4) |
| Any TEAE leading to definitive discontinuation c | 6 (11.8) | 8 (23.5) | 9 (7.1) | 9 (10.2) |
| Any TEAE leading to premature discontinuation of isatuximab | 1 (2.0) | N.A. | 0 | N.A. |
| Any TEAE leading to premature discontinuation of carfilzomib | 8 (15.7) | 0 | 18 (14.3) | 1 (1.1) |
| Any TEAE leading to premature discontinuation of dexamethasone | 3 (5.9) | 1 (2.9) | 8 (6.3) | 3 (3.4) |
Abbreviations: d, dexamethasone; Isa, isatuximab; K, carfilzomib; N.A., not applicable; TEAE, treatment‐emergent adverse event.
TEAEs with a start date before the cut‐off date and becoming serious after the cut‐off date were not counted as serious TEAE in this analysis.
TEAEs with fatal outcome during the treatment period.
Definitive discontinuation defined as definitive discontinuation of all study drugs.
For both age groups, although the incidence of grade ≥3 TEAEs was higher in the Isa‐Kd arm, the incidence of serious TEAEs was similar between arms (≥70 years: 72.5% in Isa‐Kd, 70.6% in Kd; <70 years: 54.0% in Isa‐Kd, 52.3% in Kd). In the elderly group, 3 (5.9%) patients in Isa‐Kd and 1 (2.9%) in Kd had TEAEs with fatal outcome during study treatment (Isa‐Kd: pneumonia, Kd: general health deterioration due to progressive disease). In both age groups, fewer patients definitively discontinued study treatment due to TEAEs in the Isa‐Kd than the Kd arm: 11.8% versus 23.5% (≥70 years) and 7.1% versus 10.2% (<70 years). The incidence of TEAEs leading to premature carfilzomib discontinuation in the Isa‐Kd arm was comparable between age groups (15.7% and 14.3%) (Table 3).
Any‐grade TEAEs reported in ≥20% of elderly patients are listed in Table 4, according to age group, for Isa‐Kd and the respective Kd arm. Among older patients, the most common TEAEs were diarrhea (43.1% vs. 29.4%), dyspnea (43.1% vs. 26.5%), upper respiratory tract infection (39.2% vs. 23.5%), fatigue (39.2% vs. 23.5%), and hypertension (37.3% vs. 29.4%); among younger patients, they were hypertension (36.5% vs. 31.8%), upper respiratory tract infection (34.9% vs. 23.9%), and diarrhea (33.3% vs. 28.4%). Infusion reactions occurred in 37.3% versus 5.9% of elderly patients and in 47.6% versus 2.3% of younger patients. The most common grade ≥3 TEAEs reported in ≥10% of patients in Isa‐Kd versus Kd were hypertension and pneumonia in both elderly (25.5% vs. 26.5%, 21.6% vs. 20.6%, respectively) and younger patients (18.3% vs. 17.0%, 14.3% vs. 9.1%, respectively), with similar incidence between study arms.
TABLE 4.
TEAEs by age group: ≥70 and <70 years, safety population
| ≥70 Years (n = 85) | <70 Years (n = 214) | |||
|---|---|---|---|---|
| Any‐grade TEAEs preferred term, n (%) | Isa‐Kd (n = 51) | Kd (n = 34) | Isa‐Kd (n = 126) | Kd (n = 88) |
| Most common in at least 20% of patients in one arm, ≥70 years | ||||
| Diarrhea | 22 (43.1) | 10 (29.4) | 42 (33.3) | 25 (28.4) |
| Dyspnea | 22 (43.1) | 9 (26.5) | 27 (21.4) | 17 (19.3) |
| Upper respiratory tract infection | 20 (39.2) | 8 (23.5) | 44 (34.9) | 21 (23.9) |
| Fatigue | 20 (39.2) | 8 (23.5) | 30 (23.8) | 15 (17.0) |
| Infusion reaction | 19 (37.3) | 2 (5.9) | 60 (47.6) | 2 (2.3) |
| Hypertension | 19 (37.3) | 10 (29.4) | 46 (36.5) | 28 (31.8) |
| Bronchitis | 16 (31.4) | 2 (5.9) | 24 (19.0) | 13 (14.8) |
| Pneumonia | 15 (29.4) | 9 (26.5) | 27 (21.4) | 15 (17.0) |
| Edema, peripheral | 13 (25.5) | 10 (29.4) | 10 (7.9) | 11 (12.5) |
| Insomnia | 10 (19.6) | 10 (29.4) | 32 (25.4) | 18 (20.5) |
| Asthenia | 9 (17.6) | 10 (29.4) | 23 (18.3) | 10 (11.4) |
| Pyrexia | 3 (5.9) | 9 (26.5) | 13 (10.3) | 9 (10.2) |
| Cough | 10 (19.6) | 7 (20.6) | 25 (19.8) | 10 (11.4) |
| Selected TEAEs | ||||
| Infections and infestations | 48 (94.1) | 27 (79.4) | 105 (83.3) | 71 (80.7) |
| Respiratory infection a | 47 (92.2) | 25 (73.5) | 100 (79.4) | 65 (73.9) |
| Thromboembolic events b | 9 (17.6) | 3 (8.8) | 18 (14.3) | 17 (19.3) |
| Venous c | 8 (15.7) | 3 (8.8) | 16 (12.7) | 15 (17.0) |
| Arterial | 1 (2.0) | 1 (2.9) | 2 (1.6) | 3 (3.4) |
| Cardiac failure b | 7 (13.7) | 5 (14.7) | 6 (4.8) | 3 (3.4) |
| Ischemic heart disease b | 3 (5.9) | 3 (8.8) | 5 (4.0) | 2 (2.3) |
| Second primary malignancy a | 8 (15.7) | 4 (11.8) | 5 (4.0) | 2 (2.3) |
| Solid skin malignancy | 7 (13.7) | 3 (8.8) | 2 (1.6) | 0 |
| Solid non‐skin malignancy | 2 (3.9) | 2 (5.9) | 3 (2.4) | 2 (2.3) |
| On‐treatment abnormalities | ||||
| End‐stage renal disease d eGFR <15 ml/min/1.73 m2 | 1/48 (2.1) | 2/31 (6.5) | 2/115 (1.7) | 1/79 (1.3) |
Abbreviations: d, dexamethasone; eGFR, estimated glomerular filtration rate; Isa, isatuximab; K, carfilzomib; TEAE, treatment‐emergent adverse event.
Customized MedDRA query.
MedDRA SMQ (narrow term).
In patients with venous thromboembolic events, 3/8 versus 2/3 elderly patients and 4/16 versus 3/15 younger patients, for Isa‐Kd versus Kd, had received antithrombotic prophylaxis, while 5/8 versus 1/3 elderly patients and 12/16 versus 12/15 younger patients, for Isa‐Kd versus Kd, had not received antithrombotic prophylaxis. Most events occurred in patients without a medical history of venous thromboembolism: 7/8 in Isa‐Kd and 3/3 events in Kd in elderly patients; 14/16 in Isa Kd and 14/15 events in Kd in younger patients.
On‐treatment abnormalities (eGFR <15 ml/min/1.73 m2) by the modification of diet in renal disease (MDRD) equation.
Incidences of selected TEAEs analyzed with grouping terms are presented in Table 4. In elderly patients, respiratory infections and venous thromboembolic events were more frequent in Isa‐Kd than Kd (92.2% vs. 73.5% and 15.7% vs. 8.8%), whereas cardiac failure, ischemic heart disease, and second primary malignancy were similar between arms (13.7% vs. 14.7%, 5.9% vs. 8.8%, and 15.7% vs. 11.8%, respectively). The difference between Isa‐Kd and Kd in respiratory infections was driven by upper respiratory tract infection (39.2% vs. 23.5%) and bronchitis (31.4% vs. 5.9%), with low incidence of grade ≥3 events (2.0% vs. 2.9% and 5.9% vs. 0%, respectively). Incidence of pneumonia was similar between arms (29.4% vs. 26.5%).
Among hematologic laboratory abnormalities, incidence of any‐grade anemia, thrombocytopenia, and neutropenia in elderly patients were similar to those observed in younger patients within the two arms, except for any‐grade neutropenia, which was lower in elderly than in younger patients in the Kd arm (14.7% vs. 54.5%), with comparable carfilzomib exposure (Table 5). Grade 3 neutropenia was higher in Isa‐Kd versus Kd in both age groups (≥70 years: 15.7% vs. 2.9%, <70 years: 18.3% vs. 8.0%). None of the older patients had grade 4 anemia, thrombocytopenia, or neutropenia in the Isa‐Kd arm vs. 0%, 2.9%, and 0%, respectively, in the Kd arm.
TABLE 5.
Hematologic laboratory abnormalities by age group: ≥70 and <70 years, safety population
| ≥70 Years (n = 85) | <70 Years (n = 214) | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Isa‐Kd (n = 51) | Kd (n = 34) | Isa‐Kd (n = 126) | Kd (n = 88) | |||||||||
| Grade (G) | ||||||||||||
| Laboratory parameter, n (%) | Any | G3 | G4 | Any | G3 | G4 | Any | G3 | G4 | Any | G3 | G4 |
| Anemia | 51 (100) | 9 (17.6) | 0 | 33 (97.1) | 7 (20.6) | 0 | 125 (99.2) | 30 (23.8) | 0 | 88 (100) | 17 (19.3) | 0 |
| Thrombo‐cytopenia | 48 (94.1) | 11 (21.6) | 0 | 28 (82.4) | 7 (20.6) | 1 (2.9) | 119 (94.4) | 22 (17.5) | 20 (15.9) | 79 (89.8) | 12 (13.6) | 9 (10.2) |
| Neutropenia | 28 (54.9) | 8 (15.7) | 0 | 5 (14.7) | 1 (2.9) | 0 | 69 (54.8) | 23 (18.3) | 3 (2.4) | 48 (54.5) | 7 (8.0) | 1 (1.1) |
Abbreviations: d, dexamethasone; Isa, isatuximab; K, carfilzomib.
4. DISCUSSION AND CONCLUSION
Results from this subgroup analysis of the Phase 3 IKEMA study have shown that elderly patients ≥70 years of age derived a strong PFS benefit (HR, 0.36; 95% CI, 0.18–0.75) from treatment with Isa‐Kd compared with Kd, similar to the findings previously reported with Isa‐Kd in the overall IKEMA study population. 11 PFS benefit was also observed in this analysis for younger patients (<70 years) with Isa‐Kd versus Kd (HR, 0.61; 95% CI, 0.38–0.97). The rates of ≥VGPR, MRD–, and CR were higher with Isa‐Kd compared with Kd in both elderly and younger patients. The quality of response for both age groups was consistent with the results in the overall population, 11 with high rates of CR (38.5%) and MRD– (23.1%) in elderly patients.
Prior findings reported for treatment with daratumumab in combination with Kd versus Kd in the Phase 3 CANDOR study showed that patients with relapsed MM >65 years of age had an improvement in PFS (HR, 0.76 [95% CI 0.48–1.22]) that appeared less than that observed in all randomized patients (HR, 0.63 [95% CI 0.46–0.85]) and in younger patients (≤65 years; HR, 0.57 [95% CI 0.38–0.86]) 16 , 17 Detailed subgroup analyses of daratumumab‐Kd efficacy and safety in elderly patients have yet to be reported for the CANDOR study.
In IKEMA, 11 patients ≥65 years of age derived a PFS benefit from treatment with Isa‐Kd versus Kd (HR, 0.43 [95% CI 0.25–0.74]) comparable to that observed in all patients (HR, 0.53 [95% CI 0.36–0.79]), in agreement with the efficacy findings of this latest analysis conducted for Isa‐Kd in patients ≥70 years of age. Consistently, results from subgroup analyses in older RRMM patients enrolled in the ICARIA‐MM study demonstrated improved PFS with Isa‐Pd versus Pd (≥75 years: HR, 0.48 [95% CI 0.24–0.95]; 65–74 years: HR, 0.64 [95% CI 0.39–1.06]), indicating that Isa can improve outcomes in elderly patients across different combination therapies. 9 , 10 Benefit from anti‐CD38 combination therapy in elderly RRMM patients was also reported with daratumumab plus bortezomib‐dexamethasone or lenalidomide‐dexamethasone in subgroup analyses of the Phase 3 studies CASTOR and POLLUX, respectively. 18
Elderly patients are generally more fragile patients and it is important that the increased efficacy is not obtained to the detriment of safety. Respiratory infections (by grouping analysis) and diarrhea, dyspnea, and fatigue were more frequent (at least 10% difference) in elderly versus younger patients in Isa‐Kd and higher versus Kd among the elderly. The difference observed with Isa‐Kd versus Kd in incidence of respiratory infections among elderly patients was primarily driven by upper respiratory tract infection and bronchitis, which are manageable infections, with low incidence of grade ≥3 events. Grade ≥3 diarrhea, dyspnea, and fatigue were all below 10%. The most common grade ≥3 TEAEs in both age groups were hypertension and pneumonia, with a higher incidence in elderly patients in both treatment arms, but with a similar incidence between Isa‐Kd and Kd in elderly patients (25.5% vs. 26.5% and 21.6% vs. 20.6%, respectively).
Among selected TEAEs, the incidence of cardiac failure, ischemic heart disease, and second primary malignancy, although numerically higher in older versus younger patients, were similar between Isa‐Kd and Kd in elderly patients. As previously reported in the ENDEAVOR trial, incidence of cardiac TEAEs, in particular cardiac failure, was higher in older versus younger patients treated with Kd. 19 Importantly, in the ENDEAVOR and IKEMA studies, these findings are in the context of clinical trials with specific eligibility criteria that would limit the inclusion of patients with certain, known cardiac comorbidities. Estimates of the incidence of cardiac toxicities related to carfilzomib in a real world setting are variable and depend on the terms included and the data source. 20 , 21 Importantly, age is consistently a risk factor for higher incidence of hypertension and cardiac failure. 20
Thromboembolic events were reported with similar incidence for elderly and younger patients in the Isa‐Kd arm. The majority of thromboembolic events were venous in both treatment arms and age groups. The incidence of venous thromboembolic events in Kd was surprisingly lower in elderly versus younger patients (8.8% vs. 17.0%), leading to a higher incidence in Isa‐Kd versus Kd among elderly patients. Among the patients with venous thromboembolic events, 3/8 vs. 2/3 elderly patients and 4/16 vs. 3/15 younger patients, for Isa‐Kd versus Kd, had received antithrombotic prophylaxis. Most of the observed events occurred in patients that did not receive thromboprophylaxis (5/8 vs. 1/3 elderly patients and 12/16 vs. 12/15 younger patients, for Isa‐Kd vs. Kd) and in patients that had no medical history of venous thromboembolism recorded in the database.
More serious TEAEs were reported in elderly patients, but a similar incidence of serious TEAEs was observed in the Isa‐Kd and Kd arms, within each age group, indicating that addition of Isa to Kd did not increase hospitalization of elderly patients for AE management.
Any‐grade infusion reactions occurred less frequently with Isa‐Kd in the elderly than the younger patients (37.3% and 47.6%, respectively, with similar premedication), as previously observed in RRMM patients ≥75 years (28.1%) and 65–74 years (36.4%) or <65 years (42.6%) treated with Isa‐Pd in the Phase 3 ICARIA‐MM study. 9 In contrast, findings from the CASTOR study showed that older RRMM patients (≥75 years) receiving daratumumab plus bortezomib‐dexamethasone experienced more, any‐grade infusion reactions than younger patients (65–74 years) (65.0% and 45.7%, respectively). 18
Notably, a similar incidence of elderly and younger patients within Isa‐Kd (and a lower incidence of elderly patients in Isa‐Kd vs. Kd) had TEAEs leading to definitive treatment discontinuations, suggesting tolerability of treatment with Isa‐Kd independent of age in most patients. A limitation of this study is the limited number of patients, which prevented further meaningful analyses of efficacy and safety with additional variables associated with aging (i.e., selected comorbidities). An additional limitation of this analysis is that it was conducted in the context of a clinical trial. Eligibility criteria other than age and individual investigator bias (e.g., toward ability of an individual to adhere to trial requirements) may skew the inclusion of older adults that may not represent all the patients in the community of similar age, but with additional comorbidities.
In conclusion, Isa‐Kd provides a consistent benefit versus Kd in elderly patients, with a manageable safety profile. Isa‐Kd represents a new treatment option for patients with relapsed MM, independent of age.
AUTHOR CONTRIBUTION
Thierry Facon, Philippe Moreau, Thomas G. Martin, Ivan Spicka, Albert Oriol, Youngil Koh, Andrew Lim, Michele Cavo, Kwee Yong, Marie‐Laure Risse, Sandrine Schwab, and Gracia Martinez designed the study in collaboration with the study sponsor. Marie‐Laure Risse contributed to the investigations and to the analysis, verification, and interpretation of the data for this study. Gaëlle Asset performed the formal data and statistical analyses. All authors contributed to the investigations, interpretation of the data, and drafting or critically revising the manuscript. All authors approved final version.
CONFLICT OF INTEREST
Thierry Facon: participation on a data safety monitoring board or advisory board for Amgen, Bristol Myers Squibb, Janssen, Karyopharm, Oncopeptides, Roche, and Sanofi; speakers' bureau for Bristol Myers Squibb and Janssen. Philippe Moreau: honoraria and participation on a data safety monitoring board or advisory board for AbbVie, Amgen, Bristol Myers Squibb/Celgene, Janssen, Oncopeptide, Roche, and Sanofi. Thomas G. Martin: research funding (to institution) from Sanofi; participation on a steering committee for Sanofi. Ivan Spicka: research funding, honoraria, and participation on a data safety monitoring board or advisory board for Amgen, Bristol Myers Squibb/Celgene, Janssen‐Cilag, Novartis, PharmaMar, Sanofi, and Takeda. Albert Oriol: honoraria from Amgen and Bristol Myers Squibb/Celgene; participation on a data safety monitoring board or advisory board for Amgen, Bristol Myers Squibb/Celgene, GlaxoSmithKline, Karyopharm, Oncopeptides, and Sanofi. Youngil Koh: nothing to disclose. Andrew Lim: nothing to disclose. Gabor Mikala: honoraria from AbbVie, Amgen, Celgene, Janssen, Krka Pharma, Novartis, Sandoz, and Takeda; travel support from AbbVie, Celgene, Janssen, and Takeda. Laura Rosiñol: honoraria from Amgen, Celgene, GlaxoSmithKline, Janssen, Sanofi, and Takeda; participation on a data safety monitoring board or advisory board for Amgen, Celgene, GlaxoSmithKline, Janssen, Karyopharm, Sanofi, and Takeda. Münci Yağci: nothing to disclose. Michele Cavo: honoraria from AbbVie, Adaptive Biotechnologies, Amgen, Bristol Myers Squibb/Celgene, GlaxoSmithKline, Janssen, Sanofi, and Takeda; speakers bureau for Janssen and Bristol Myers Squibb/Celgene. Kwee Yong: research funding from Bristol Myers Squibb, Janssen, and Sanofi; honoraria and travel support from Amgen, Sanofi, and Takeda; participation on an advisory board or steering committee for Janssen and Sanofi. Marie‐Laure Risse, Gaëlle Asset, and Sandrine Schwab: employed by Sanofi, may hold stock and/or stock options in the company. Gracia Martinez: nothing to disclose.
PEER REVIEW
The peer review history for this article is available at https://publons.com/publon/10.1002/hon.3038.
ETHICS STATEMENT
The study protocol was approved by the Institutional Ethics Committee or independent review board for each center; the study was conducted following the Declaration of Helsinki and IHC Guidelines for Good Clinical Practice. All patients provided written informed consent.
ACKNOWLEDGMENTS
The authors thank the participating patients and their caregivers, and the study centers and investigators for their contributions to the study. Medical writing support was provided by S. Mariani, MD, PhD of Elevate Medical Affairs, contracted by Sanofi for publication support services. This study was funded by Sanofi.
Facon T, Moreau P, Martin TG, et al. Isatuximab plus carfilzomib and dexamethasone versus carfilzomib and dexamethasone in elderly patients with relapsed multiple myeloma: IKEMA subgroup analysis. Hematol Oncol. 2022;40(5):1020‐1029. 10.1002/hon.3038
DATA AVAILABILITY STATEMENT
Qualified researchers can request access to patient‐level data and related study documents including the clinical study report, study protocol with any amendments, blank case report forms, statistical analysis plan, and dataset specifications. Patient‐level data will be anonymized, and study documents will be redacted to protect the privacy of trial participants. Further details on Sanofi's data‐sharing criteria, eligible studies, and process for requesting access are at https://vivli.org.
REFERENCES
- 1. Mina R, Bringhen S, Wildes TM, Zweegman S, Rosko AE. Approach to the older adult with multiple myeloma. Am Soc Clin Oncol Educ Book. 2019;39:500‐518. 10.1200/edbk_239067 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. SEER Cancer Statistics Review. 2017. Accessed February 4, 2022. https://seer.cancer.gov/csr/1975_2017/browse_csr.php [Google Scholar]
- 3. Cowan AJ, Allen C, Barac A, et al. Global burden of multiple myeloma: a systematic analysis for the global burden of disease study 2016. JAMA Oncol. 2018;4(9):1221‐1227. 10.1200/jco.2018.36.15_suppl.e20023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Bringhen S, Mateos MV, Zweegman S, et al. Age and organ damage correlate with poor survival in myeloma patients: meta‐analysis of 1, 435 individual patient data from 4 randomized trials. Haematologica. 2013;98(6):980‐987. 10.3324/haematol.2012.075051 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Madan S, Kumar S. Current treatment options for elderly patients with multiple myeloma: clinical impact of novel agents. Therapy. 2011;8(4):415‐429. 10.2217/thy.11.39 [DOI] [Google Scholar]
- 6. Bonello F, Boccadoro M, Larocca A. Diagnostic and therapeutic challenges in the management of intermediate and frail elderly multiple myeloma patients. Cancers (Basel). 2020;12(11):3106. 10.3390/cancers12113106 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Deckert J, Wetzel MC, Bartle LM, et al. SAR650984, a novel humanized CD38‐targeting antibody, demonstrates potent antitumor activity in models of multiple myeloma and other CD38+ hematologic malignancies. Clin Cancer Res. 2014;20(17):4574‐4578. 10.1158/1078-0432.ccr-14-0695 [DOI] [PubMed] [Google Scholar]
- 8. Martin TG, Corzo K, Chiron M, et al. Therapeutic opportunities with pharmacological inhibition of CD38 with isatuximab. Cells. 2019;8(12):1522. 10.3390/cells8121522 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Attal M, Richardson PG, Rajkumar SV, et al. ICARIA‐MM study group. Isatuximab plus pomalidomide and low‐dose dexamethasone versus pomalidomide and low‐dose dexamethasone in patients with relapsed and refractory multiple myeloma (ICARIA‐MM): a randomised, multicentre, open‐label, phase 3 study. Lancet. 2019;394(10214):2096‐2107. [DOI] [PubMed] [Google Scholar]
- 10. Schjesvold FH, Richardson PG, Facon T, et al. Isatuximab plus pomalidomide and dexamethasone in elderly patients with relapsed/refractory multiple myeloma: ICARIA‐MM subgroup analysis. Haematologica. 2021;106(4):1182‐1187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Moreau P, Dimopoulos M‐A, Mikhael J, et al. Isatuximab, carfilzomib, and dexamethasone in relapsed multiple myeloma (IKEMA): a multicentre, open‐label, randomised phase 3 trial. Lancet. 2021;397(10292):2361‐2371. [DOI] [PubMed] [Google Scholar]
- 12. SARCLISA® (Isatuximab‐irfc) Injection, for Intravenous Use. Prescribing Information. 2021. Accessed February 4, 2022. https://products.sanofi.us/Sarclisa/sarclisa.pdf [Google Scholar]
- 13. European Medicines Agency. Sarclisa, INN‐Isatuximab. Summary of Product Characteristics; 2021. Accessed February 4, 2022. https://www.ema.europa.eu/en/documents/product‐information/sarclisa‐epar‐product‐information_en.pdf [Google Scholar]
- 14. SARCLISA® (isatuximab) . Prescribing Information Nishi Shinjuku, Tokyo; 2021. Accessed February 4, 2022. https://www.pmda.go.jp/PmdaSearch/iyakuDetail/ResultDataSetPDF/780069_4291454A1021_1_02 [Google Scholar]
- 15. Kumar S, Paiva B, Anderson KC, et al. International Myeloma Working Group consensus criteria for response and minimal residual disease assessment in multiple myeloma. Lancet Oncol 2016;17(8):e328‐e346. 10.1016/s1470-2045(16)30206-6 [DOI] [PubMed] [Google Scholar]
- 16. Dimopoulos M, Quach H, Mateos MV, et al. Carfilzomib, dexamethasone, and daratumumab versus carfilzomib and dexamethasone for patients with relapsed or refractory multiple myeloma (CANDOR): results from a randomised, multicentre, open‐label, phase 3 study. Lancet. 2020;396(10245):186‐197. 10.1016/s0140-6736(20)30734-0 [DOI] [PubMed] [Google Scholar]
- 17. Silvennoinen R, Heckman CA. A candid view of CANDOR. Lancet. 2020;396(10245):147‐148. 10.1016/s0140-6736(20)30901-6 [DOI] [PubMed] [Google Scholar]
- 18. Mateos MV, Spencer A, Nooka AK, et al. Daratumumab‐based regimens are highly effective and well tolerated in relapsed or refractory multiple myeloma regardless of patient age: subgroup analysis of the phase 3 CASTOR and POLLUX studies. Haematologica. 2020;105(2):468‐477. 10.3324/haematol.2019.217448 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Ludwig H, Dimopoulos MA, Moreau P, et al. Carfilzomib and dexamethasone vs bortezomib and dexamethasone in patients with relapsed multiple myeloma: results of the phase 3 study ENDEAVOR (NCT01568866) according to age subgroup. Leuk Lymphoma. 2017;58(10):2501‐2504. 10.1080/10428194.2017.1298755 [DOI] [PubMed] [Google Scholar]
- 20. Bishnoi R, Xie Z, Shah C, et al. Real‐world experience of carfilzomib‐associated cardiovascular adverse events: SEER‐Medicare data set analysis. Cancer Med. 2021;10(1):70‐78. 10.1002/cam4.3568 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Zhai Y, Ye X, Hu F, et al. Cardiovascular toxicity of carfilzomib: the real‐world evidence based on the adverse event reporting system database of the FDA, the United States. Front Cardiovasc Med. 2021;8:735466. 10.3389/fcvm.2021.735466 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Qualified researchers can request access to patient‐level data and related study documents including the clinical study report, study protocol with any amendments, blank case report forms, statistical analysis plan, and dataset specifications. Patient‐level data will be anonymized, and study documents will be redacted to protect the privacy of trial participants. Further details on Sanofi's data‐sharing criteria, eligible studies, and process for requesting access are at https://vivli.org.


