Abstract
Purpose
While the association between intimate partner violence (IPV) and stress is well documented, the directionality of this relationship is unclear. We use an adjusted longitudinal study design to better understand if stressful life events in the home precipitate or exacerbate intimate partner violence (IPV) and if experiences of IPV, in turn, increase levels of perceived stress.
Methods
Longitudinal data were collected among married women in rural Pakistan at 12 and 24 months postpartum (N = 815). Adjusted Poisson and linear regression models were used to examine stressful life events, past year IPV and severity (number and frequency of violent acts), and perceived stress (Cohen Perceived Stress Scale).
Results
At 12 months postpartum, the prevalence of past year physical, psychological, and sexual IPV was 8.5%, 25.7%, and 25.1%, respectively, with 42.6% experiencing any IPV. After adjustment, stressful life events were associated with a subsequent increased likelihood of all IPV types and increased severity of all but physical IPV. Any past year IPV (versus none) and greater IPV severity were associated with 3.43 (95% CI 2.33–4.52) and 2.57 (95% CI 1.87–3.27) point subsequent increases in perceived stress. Physical, psychological, and sexual IPV and their respective severities were all independently associated with increased perceived stress.
Conclusions
Among postpartum women in Pakistan, stressful life events increase the likelihood of IPV and, in turn, experiences of IPV increase stress levels. Support to families undergoing stressful circumstances may be critical to reducing women’s IPV exposure and resulting elevated stress.
Keywords: Intimate partner violence, Maternal stress, Pakistan, LMIC, Postpartum
Introduction
Intimate partner violence (IPV) is defined as physical or sexual violence, stalking, or psychological aggression including coercive tactics by a current or former intimate partner [1]. Globally, approximately one in three women who have been in a relationship report being subjected to some form of violence by their intimate partner [2]. In addition to the injurious impacts of IPV, IPV is associated with many adverse outcomes such as mortality, disability, poor sexual, reproductive, and gastrointestinal health, chronic pain, poorer health behaviors, mental health conditions, and substance abuse [3–9]. IPV itself and the aforementioned consequences can be highly stressful and emotionally distressing for survivors [2, 10], as evident by many studies finding IPV to be associated with increased levels of stress or distress [11–18]. Even in circumstances where the survivor has left the relationship, stress can continue or become worse via intimidation from the abuser or emotional and financial stressors related to single parenting or court proceedings, impacting many facets of life [19]. Cumulative exposure to stress, a state of internal physiological arousal precipitated by external demands (stressors) that tax individuals’ normal adaptive capacities [20], is associated with negative health consequences. It can contribute to serious long-term health problems such as heart disease, high blood pressure, diabetes, mental health conditions, and suicide [21–23].
Stress associated with various life events may also be a precipitating factor for IPV perpetration. There are many risk factors at the individual, community, and societal level associated with IPV [24, 25]. At the community and societal levels, factors such neighborhood disadvantage [26, 27], low levels of collective efficacy [28, 29], weak community sanctions against domestic violence [30], and traditional gender norms [31] are associated with elevated risk for IPV. On an individual and relationship level, young age [32, 33], low educational attainment or socioeconomic status [34, 35], and history of family violence for the perpetrator [36–38] have been shown to be associated with IPV. These risk factors are consistent with prevailing theoretical approaches explaining the occurrence and escalation of IPV, including feminist perspectives on the role of patriarchal institutions and norms that shape power dynamics [39] and social learning theory to explain intergenerational patterns of behavior, including relationship dynamics and a propensity for abuse [40]. Other theoretical models of IPV highlight the role of situational factors such as stress in triggering IPV, usually in interaction with underlying vulnerabilities [41–45]. Consistent with these theories, extant evidence indicates that stressors such as drug or alcohol use in the family [46–48], divorce [47], unemployment [47], mortgage, foreclosure [49], and natural disasters [50] may increase the likelihood of IPV occurrence or escalation in the household. Similarly, evidence from randomized control trials shows that the removal of financial stressors (via cash transfer programs) results in a reduction of IPV [51], underscoring how financial stressors may cause and exacerbate violence. The majority of research between stress and IPV are drawn from cross-sectional and retrospective studies [12, 13, 15–17, 46–49] and given the potential bi-directionality, such well-documented associations are difficult to interpret. These studies hypothesize the directionality and cyclical nature of the relationship between IPV and stress/stressors, but they suffer from a lack of temporality and the potential for reverse causation, which limits the ability to make casual inferences about stress-related risk factors for and consequences of IPV [24, 25, 52]. There is a need for more longitudinal study designs with appropriate confounder control to better understand how stressful life events may precipitate or exacerbate IPV and how experiences of IPV may, in turn, increase levels of perceived stress, a need that has been noted in multiple formal systematic reviews [25, 52].
Also needed are robust, longitudinal studies from low- and middle- income country (LMIC) settings, where IPV is often highly prevalent and the relationships between stress and IPV may differ. A recent 2018 systematic review on risk and protective factors for IPV included 60 prospective longitudinal studies, of which only three were from LMIC settings [53]. Regional estimates from the WHO suggest that South Asia has the highest prevalence of IPV in the world at 43% overall [54], likely due in part to social norms sanctioning at least some degree of domestic violence within marriage [55]. A 2014 systematic review of IPV in Pakistan found the prevalence of IPV to range from 48 to 84% for psychological, 16 to 80% for physical, and 1 to 77% for sexual IPV, demonstrating elevated levels of gender-based violence compared to the rest of the world and, potentially, other parts of South Asia [56]. In a context of endemic IPV, the role of stressors in precipitating instances of violence is not known. Furthermore, due to the taboo nature of divorce in Pakistan, and the relative lack of socially and economically -viable options for women outside of marriage, leaving abusive relationships is extremely difficult. Remaining in abusive relationships can be highly stressful due to persistent fear of harm from the husband and in-laws, concerns about losing financial support and children’s safety, stigma, and a lack of support from family and friends [57]. However, given that IPV is so prevalent and culturally normative in Pakistan, it is also possible that the nature of the IPV–stress relationship may differ in this setting [58]. Research from other parts of South Asia has found a lack of association between relatively common, less severe IPV and depression [58], especially in communities where it is highly prevalent [59]. This research has also documented substantially elevated risk of mental health consequences associated with more severe exposure to IPV [58]. As such, studies in these regions have suggested that relying on dichotomous indicators of IPV may mask the true impact of IPV whereby notable increases in adverse mental health outcomes may only occur with more severe types of IPV [58]. It is therefore important to not only consider the occurrence of IPV, but also its frequency and severity.
We aim to fill the aforementioned literature gaps—a dearth of robust, longitudinal examination of the relationships between stressors, IPV, and stress, especially in low resources settings—by estimating the relationship between two dimensions of stress and IPV in rural Pakistan using longitudinal data and nuanced IPV measures that account for IPV subtype and frequency. More specifically, we aim to assess the impact of stressful life events reported at 12 months postpartum on experiences and severity of IPV at 24 months postpartum (Aim 1) and the impact of experiences and severity of IPV at 24 months postpartum on past month perceived stress at 24 months postpartum (Aim 2).
Methods
Data source
This paper uses longitudinal data from the Bachpan study in rural Pakistan. This study originated as a stratified, cluster-randomized controlled trial of a maternal depression intervention in 40 village clusters in Kallar Syedan, a rural subdistrict of Rawalpindi, Pakistan. Eligible participants included women aged ≥ 18 years in their third trimester of pregnancy and registered with local lady health workers (who are government-employed community health workers). Depressed women were enrolled in the trial based on Patient Health Questsionnaire-9 (PHQ-9) scores ≥ 10 and one in every three women without depression (PHQ-9 < 10) was enrolled in the observational cohort. Sampling weights create a cohort with equal numbers of women with and without prenatal depression at the beginning of data collection. A detailed description of the study design and sampling is available elsewhere [60]. Assessments were done during pregnancy and 3, 6, 12, 24, and 36 months postpartum. While the Bachpan study has baseline data for 1,154 women, the current analysis utilized data from women with data for our variables of interest (e.g., baseline control variables, stressful life events, IPV, and perceived stress) at Time 0 (pregnancy), Time 1 (12 months postpartum), and Time 2 (24 months postpartum), resulting in various sample sizes per model, to maximize the available data. An analytical sample of 815 women were represented in at least one of our adjusted models; see tables for specific sample sizes per model.
Measures
Figure 1 shows the timing of assessments and reference periods for the primary measures used in these analyses. For Aim 1, we estimated the impact of stressful life events assessed at Time 1 (12 months postpartum) on IPV assessed at Time 2 (24 months postpartum). Both measures have a reference period of the past year, so the 12- and 24-month timing of assessments allows for a lagged analysis. For Aim 2, we estimated the impact of IPV on perceived stress, with both exposure and outcome assessed at Time 2, since the reference period for the outcome (perceived stress) is only the past month. Past year stressful life events, the exposure for Aim 1, were measured using a combination of a modified version of the Life Events and Difficulties Schedule [61, 62] and a list of household economic shocks (Appendix I). Specifically, respondents were asked about whether any of the following occurred in the last year: financial problems (e.g., having debt); change in social status (e.g., engagement or marriage, separation or divorce, starting or finishing education); problems with residence; troubled relations with close relatives or friends; worries about children’s problems; quarrels/rows among family members; death of any household member; serious illness of any household member; and loss of employment. One additional stressor, problems with marital relations, was excluded from the current analysis to isolate the effect of life stressors on IPV, apart from the direct impact of marital problems. The number of stressful life events was maintained as continuous (0–9).
Fig. 1.
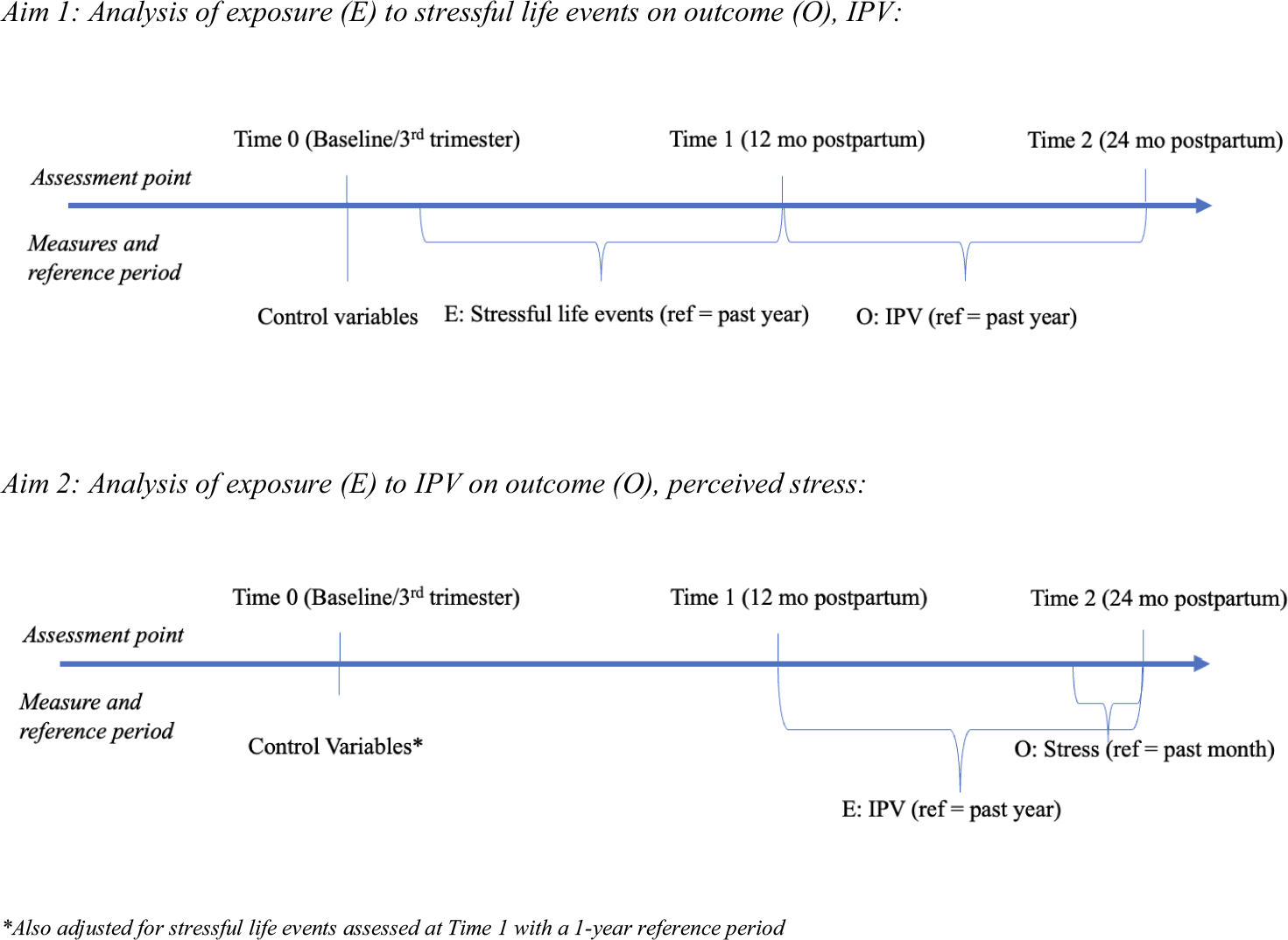
Assessment and reference periods for measures
The outcome for Aim 1 and exposure for Aim 2, IPV and IPV severity, were measured using a slightly modified version of the WHO Violence Against Women Instrument (Appendix Table) [63]. Past year psychological IPV was ascertained from nine items: husband belittled or humiliated wife; scared or intimidated on purpose; threatened to hurt; called wife ugly or said something negative about appearance; destroyed something belonging to wife; threatened to take another wife; threatened to abandon wife; threatened to divorce wife; or said wife was not able to please him sexually. Past year physical IPV was ascertained from four items: husband slapped, threw something that could hurt, pushed, or shoved; choked or burned on purpose; threatened to use a gun, knife or other weapon; or actually used a gun, knife, or other weapon. Past year sexual IPV was ascertained from three items: husband physically forced wife to have sexual intercourse when she did not want to; had sexual intercourse when she did not want to because she was afraid of what her husband might do; and husband forced her to do something sexual that she found degrading or humiliating. The women were then asked the frequency of the act in the last year (one or two times, three to five times, or more than five times). Our dichotomous measures of past year physical, psychological, and sexual IPV were based on responses of ‘yes’ to whether any of the respective behaviors occurred in the past 12 months, regardless of missing data for other items. Our measure of past year any IPV was based on responses of ‘yes’ to any of the subtypes. If respondents had missing data and only ‘no’ responses to remaining items, they were coded as missing for that subtype. If an individual had missing data on some subtypes and ‘no’ responses to remaining subtypes, they were coded as missing for any IPV. Severity was calculated by recoding frequency categories to the numeric value of the midpoint (e.g., 3–5 times was assigned a value of 4), summing the frequencies of each act, and weighting based on the number of items so that scores for all types of IPV were on the same scale of 0–10. All participants were assigned a severity score from 0 (no IPV) to 10.
Our outcome for Aim 2, perceived stress, was assessed at Time 1 and Time 2 using the total score from the 10-item Cohen Perceived Stress Scale (PSS-10), a global measure of perceived stress (Appendix Table) [64]. Participants were asked about the frequency (never, almost never, sometimes, fairly often, very often) of the following feelings or thoughts during the last month: been upset because something happened unexpectedly; unable to control the important things in life; felt nervous or stressed; felt confident about ability to handle personal problems; felt that things were going your way; found that you could not cope with all the things that you had to do; able to control irritations in your life, on top of things; angered because of things outside of control; and difficulties piling up so high that could not be overcome. Total scores were obtained by reversing the scores on the four positive items and summing all ten items with scores ranging from 0 to 40, where higher scores indicate increased stress.
Potential confounders identified via a directed acyclic graph were measured at Time 0 (pregnancy). They included trial arm, maternal age, education, whether the woman lived with just her nuclear family, and socioeconomic status measured via assets, and number of living children. Trial arm was a three-category variable depicting whether women were non-depressed, depressed and enrolled in the intervention, or depressed and in the control group. Maternal age was maintained as continuous. Maternal education was categorized into none, primary (grades 1–5), middle or secondary (grades 6–12), and tertiary (> 12 years). Assets were measured by asking about the presence of electronics, appliances, transportation, home materials, and facilities, standardized using a polychoric principal components analysis, summed, and grouped into quintiles [65, 66]. Number of living children was categorized as first pregnancy, 1–3 additional children, and 4 + additional children.
Analysis
We calculated descriptive statistics for stressful life events, past year IPV and severity, perceived stress and confounders (trial arm, maternal age, education, family structure, assets, and number of living children). Frequencies were weighted to account for the overrepresentation of women with depression in the Bachpan sample [67]. Assessment and reference periods for measures used in analyses for both aims are depicted in Fig. 1. We used Modified Poisson Generalized Estimating Equations (GEE) regression with robust standard errors [68] to estimate unadjusted and adjusted risk ratios for the effect of a 1-unit increase in stressful life events (0–9) at 12 months postpartum (Time 1) on whether IPV was reported (yes/no) at 24 months postpartum (Time 2). This GEE method was used to take into account correlation of outcomes within person over time (accounts for IPV at Time 1). Linear GEE regression with robust standard errors was used to estimate the effect of a 1-unit increase in past year stressful life events at Time 1 on the change (β) in IPV severity at Time 2.
Using linear GEE regression with robust standard errors, we then estimated the effect of the occurrence of IPV (yes/no) and a 1-unit increase in IPV severity at Time 2 on the change (β) in past month perceived stress at Time 2. GEE methods were used again to take into account correlation within person over time (accounts for perceived stress at Time 1). Because of the reference periods for past year IPV and past month stress, we used the same assessment period (Time 2) for both of these measures to ensure the appropriate lag time between exposure and outcome while still maintaining temporality (Fig. 1). In addition to aforementioned confounders, Aim 2 models also controlled for stressful life events at Time 1.
To account for potential bias from missingness at different waves of data collection, we used inverse probability weighting (IPW) in all models. Weights were the inverse probability that an observation was not missing at the 12 or 24 months based on observed characteristics. We included the marginal probability of being observed in the numerator of the IPW to stabilize weights. Baseline characteristics associated with missingness at 12 and 24 months were included in the IPW model: depressive symptoms (Patient Health Questionnaire-9), maternal disability (WHO-DAS), perceived stress (Cohen Perceived Stress Scale), total people per room in the home, clinical depression (Structured Clinical Interview for DSM-5), whether the grandmother lived in the home, and whether the husband works. The predetermined confounding factors at baseline were also included in the IPW model. All percentages, means, and standard deviations were weighted by sampling weights and all models were weighted by IPW. Analyses were conducted using SAS 9.4.
Results
Weighted descriptive statistics (and unweighted n values) are reported in Table 1. Among the sample of 815 women, at baseline (Time 0) the average age was 26.6 years (SD = 5.3) and the majority of women lived with extended family (87.5%; n = 707), completed middle or secondary education (6–12 years) (54.4%; n = 434), and had two to three living children in addition to the current pregnancy (62.7%; n = 517). The most common stressful life events reported at Time 1 were financial problems (27.3%; n = 240), changes in social status (24.1%; n = 199), and serious illness of any household member (18.8%; n = 156). The prevalence of any past year IPV was 50.6% (n = 430) at Time 2. Past year psychological IPV was the most common form of IPV (41.6%), followed by sexual IPV (27.3%), with physical IPV being the least common (9.3%), with the most common combination being psychological and sexual IPV (13.0%) and 5.9% of women reporting all three types (Fig. 2). The most common acts were husband belittled or humiliated the wife (37.3%), scared or intimidated on purpose (23.2%), and had unwanted sexual intercourse because of fear of what husband might do (19.1%; data not shown). At Time 2, the median severity (the number and frequency of IPV acts, ranging 0–10) was heavily skewed by those with values of 0 (no IPV; Table 1). Among those with each type of IPV, the median severity was highest for sexual IPV (median = 1.3; IQR = 0.7–2.7), followed by physical (median = 0.5; IQR = 0.5–1.9) and psychological IPV (median = 0.5; IQR = 0.2–0.9; Fig. 2). The average perceived stress scores (ranging 0–40) at Time 2 was 11.9 (SD = 9.9).
Table 1.
Description of outcomes and correlates of interest (n = 815)
| Correlates at baseline | N a | %a |
|---|---|---|
|
| ||
| Maternal age (mean, SD) | 26.6 (5.3) | |
| 18–24 | 555 | 32.6 |
| 25 + | 260 | 67.4 |
| Family structure | ||
| Nuclear family | 108 | 12.5 |
| Non-nuclear family | 707 | 87.5 |
| Assets quintile b | ||
| 0 | 156 | 16.3 |
| 1 | 164 | 18.9 |
| 2 | 166 | 20.6 |
| 3 | 155 | 20.4 |
| 4 | 174 | 23.8 |
| Maternal education | ||
| None | 118 | 12.9 |
| Primary (1–5) | 160 | 17.8 |
| Middle or secondary (6–12) | 434 | 54.4 |
| Tertiary | 103 | 14.9 |
| Trial arm | ||
| Depressed, intervention | 186 | 15.1 |
| Depressed, control | 200 | 16.2 |
| Non-depressed | 429 | 68.7 |
| Number of additional living children | ||
| 1st child | 237 | 30.7 |
| 1–3 additional children | 517 | 62.7 |
| 4 + additional children | 61 | 6.6 |
| Stressful life events at time 1d | ||
| Type of stressful life event | ||
| Financial problems | 240 | 27.3 |
| Change in social status | 199 | 24.1 |
| Serious illness of any household member | 156 | 18.8 |
| Death of any household member | 151 | 17.4 |
| Worried about children’s problems | 121 | 14.9 |
| Quarrels/rows with family members | 109 | 12.5 |
| Troubled relations with others | 96 | 11.1 |
| Problems with residence | 63 | 6.4 |
| Loss of employment | 24 | 2.6 |
| Number of stressful life events (mean, SD) | 1.4 (1.9) | |
| Intimate partner violence at time 2e | ||
| Any IPV | 430 | 50.6 |
| Severity of any IPV (median, IQR) | 0.0 | 0.0–0.3 |
| Physical IPV | 93 | 9.3 |
| Severity of physical IPV (median, IQR) | 0.0 | 0.0–0.0 |
| Psychological IPV | 365 | 41.6 |
| Severity of psychological IPV (median, IQR) | 0.0 | 0.0–0.3 |
| Sex-related IPV | 228 | 27.3 |
| Severity of sexual IPV (median, IQR) | 0.0 | 0.0–0.3 |
| Perceived stressf at Time 2 (mean, SD) | 11.9 (9.9) | |
Time 1 = 12 months postpartum; Time 2 = 24 months postpartum
Percentages, means, and standard deviations are weighted by sampling weights, Ns are unweighted
Summary of assets calculated using polychoric PCA and cut into quintiles
Using the Patient Health Questionnaire-9 (PHQ-9) score ≤ 9 = mild/no depression; PHQ-9 score ≥10 = moderate/severe depression
Measured using a modified version of Life Events and Difficulties Schedule and household economic shocks
Measured with the WHO Violence Against Women Instrument
Measured with the Cohen Perceived Stress Scale (0–40)
Fig. 2.
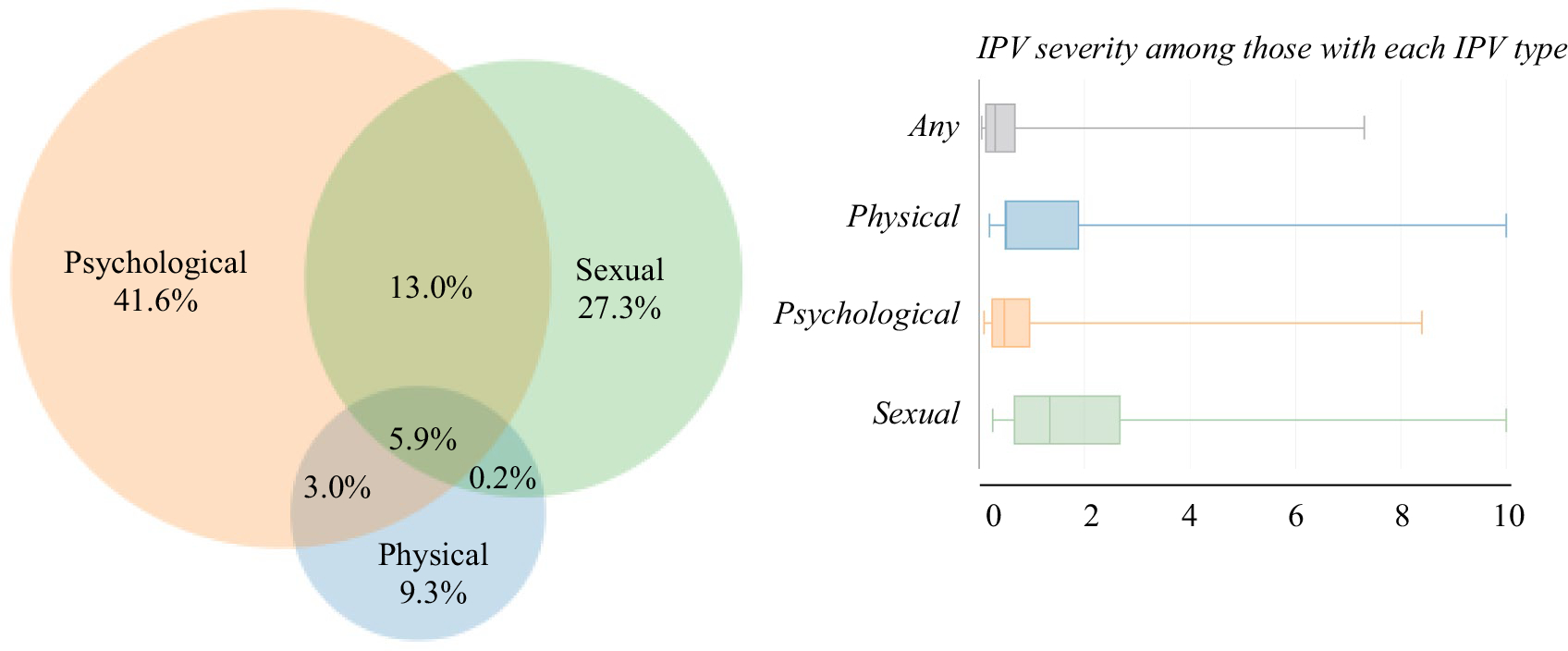
A description of intimate partner violence and severity at 24 months
Our first aim was to examine the association between stressful life events and subsequent IPV (Table 2). After adjustment, an additional stressful life event at Time 1 was associated with an increased risk, at Time 2, of past year any IPV (RR = 1.13; 95% CI = 1.09, 1.17), physical IPV (RR = 1.12; 95% CI = 1.01, 1.23), psychological IPV (RR = 1.16; 95% CI = 1.10, 1.22) and sexual IPV (RR = 1.19, 95% CI = 1.12, 1.26; Table 2). The number of stressful life events was also associated with an increased severity of any (β=0.10, 95% CI = 0.03, 0.17), psychological (β=0.14, 95% CI = 0.07, 0.22), and sexual IPV ( β=0.16, 95% CI = 0.06, 0.27; Table 3).
Table 2.
The impact of stressful life events at Time 1 on the occurrence of past year intimate partner violence (IPV)a at Time 2: Results from Modified Poisson GEE regressionb
| Exposure | Outcomes |
|||||||
|---|---|---|---|---|---|---|---|---|
| Any IPV (n = 665)c |
Physical IPV (n = 799)c |
Psychological IPV (n = 798)c |
Sexual IPV (n = 638)c |
|||||
| Unadjusted RR (95% CI) | Adjustedd RR (95% CI) | Unadjusted RR (95% CI) | Adjustedd RR (95% CI) | Unadjusted RR (95% CI) | Adjustedd RR (95% CI) | Unadjusted RR (95% CI) | Adjustedd RR (95% CI) | |
|
| ||||||||
| Stressful life events | 1.16 (1.12, 1.20) | 1.13 (1.09, 1.17) | 1.22 (1.11, 1.35) | 1.12 (1.01, 1.23) | 1.20 (1.15, 1.26) | 1.16 (1.10, 1.22) | 1.23 (1.16, 1.30) | 1.19 (1.12, 1.26) |
Time 1 = 12 months postpartum; Time 2 = 24 months postpartum
Measured with the WHO Violence Against Women Instrument
All regressions are inverse probability weighted to account for missingness
Differences in sample sizes reflect utilization of the maximum amount of data per IPV type
Adjusting for maternal age, education, assets quintile, nuclear family structure, and depressive symptoms
Table 3.
The impact of stressful life events at Time 1 on the severity of past year intimate partner violence (IPV)a at Time 2: results from linear GEE regressionb
| Exposure | Outcomes |
|||||||
|---|---|---|---|---|---|---|---|---|
| Any IPV Severity (n = 632)c |
Physical IPV Severity (n = 796)c |
Psychological IPV Severity (n = 796)c |
Sexual IPV Severity (n = 637)c |
|||||
| Unadjusted β (95% CI) | Adjustedd β (95% CI) | Unadjusted β (95% CI) | Adjustedd β (95% CI) | Unadjusted β (95% CI) | Adjustedd β (95% CI) | Unadjusted β (95% CI) | Adjustedd β (95% CI) | |
|
| ||||||||
| Stressful life events | 0.13 (0.05, 0.20) | 0.10 (0.03, 0.17) | 0.03 (0.00, 0.06) | 0.01 (−0.02, 0.03) | 0.18 (0.09, 0.26) | 0.14 (0.07, 0.22) | 0.19 (0.08, 0.31) | 1.16 (0.06, 0.27) |
Time 1 = 12 months postpartum; Time 2 = 24 months postpartum
Measured with the WHO Violence Against Women Instrument
All regressions are inverse probability weighted to account for missingness
Differences in sample sizes reflect utilization of the maximum amount of data per IPV type
Adjusting for maternal age, education, assets quintile, nuclear family structure, and depressive symptoms
Turning to Aim 2, assessing how IPV predicts perceived stress, we found that any past year IPV at Time 2 was associated with a 3.43-point (95% CI = 2.33, 4.52; Table 4) increase in past month perceived stress score at Time 2 and a 1-unit increase in severity was associated with a 2.57-point (95% CI = 1.87, 3.27; Table 5) increase in perceived stress. In terms of specific types of IPV, past year physical IPV was associated with a 4.93-point (95% CI = 3.02, 6.85; Table 4) increase in past month perceived stress score at Time 2 and a 1-unit increase in severity was associated with a 1.96-point (95% CI = 1.32, 2.60; Table 5) increase in perceived stress. Past year psychological IPV at Time 2 was associated with a 3.24-point (95% CI = 2.13, 4.35; Table 4) increase in past month perceived stress score at Time 2 and a 1-unit increase in severity was associated with a 2.17-point (95% CI = 1.58, 2.76; Table 5) increase in perceived stress. Past year sexual IPV at Time 2 as associated with a 2.78-point (95% CI = 1.51, 4.05; Table 4) increase in past month perceived stress score at Time 2 and a 1-unit increase in severity was associated with a 1.06-point (95% CI = 0.61, 1.51; Table 5) increase in perceived stress.
Table 4.
The impact of intimate partner violence (IPV)a on perceived stress at Time 2: results from linear GEE regressionb
| Exposures | Outcome: perceived stressc |
|
|---|---|---|
| Unadjusted β (95% CI) | Adjustedd β (95% CI) | |
|
| ||
| Any IPV (n = 807)e | 4.65 (3.47, 5.83) | 3.43 (2.33, 4.52) |
| Physical IPV (n = 815)e | 7.48 (5.49, 9.48) | 4.93 (3.02, 6.85) |
| Psychological IPV (n = 815)e | 4.56 (3.35, 5.76) | 3.24 (2.13, 4.35) |
| Sexual IPV (n = 800)e | 4.13 (2.72, 5.53) | 2.78 (1.51, 4.05) |
Time 2 = 24 months postpartum
Measured with the WHO Violence Against Women Instrument
All regressions are inverse probability weighted to account for missingness
Measured with the Cohen Perceived Stress Scale (0–40)
Adjusting for stressful life events at Time 1, maternal age, education, assets, nuclear family structure, and depressive symptoms
Differences in sample sizes reflect utilization of the maximum amount of data per IPV type
Table 5.
The impact of intimate partner violence (IPV)a severity on perceived stress at Time 2: results from linear GEE regressionb
| Exposures | Outcome: perceived stressc |
|
|---|---|---|
| Unadjusted β (95% CI) | Adjustedd β (95% CI) | |
|
| ||
| Any IPV severity (n = 798)e | 3.32 (2.53, 4.10) | 2.57 (1.87, 3.27) |
| Physical IPV severity (n = 813)e | 2.74 (2.06, 3.41) | 1.96 (1.32, 2.60) |
| Psychological IPV severity (n = 815)e | 2.91 (2.28, 3.54) | 2.17 (1.58, 2.76) |
| Sexual IPV severity (n = 800)e | 1.50 (0.99, 2.00) | 1.06 (0.61, 1.51) |
Time 2 = 24 months postpartum
Measured with the WHO Violence Against Women Instrument
All regressions are inverse probability weighted to account for missingness
Measured with the Cohen Perceived Stress Scale (0–40)
Adjusting for stressful life events at Time 1, maternal age, education, assets, nuclear family structure, and depressive symptoms
Differences in sample sizes reflect utilization of the maximum amount of data per IPV type
Discussion
Using a longitudinal sample of 815 postpartum women in rural Pakistan, we aimed to assess the effect of (1) life stressors on IPV occurrence and severity and (2) IPV occurrence and severity on perceived stress. For Aim 1, stressful life events reported at 12 months postpartum increased the risk of physical, psychological, and sexual IPV at 24 months postpartum by an average of 15%. Increases in these stressful events were also associated with an increase in the severity of certain subtypes of IPV, or an exacerbation of the violence. Specifically, as the number of reported stressful life events increased, we found a greater number and frequency of psychological and sexual IPV acts. For Aim 2, we found that all types of IPV were associated with significant increases in past month perceived stress, ranging from 2.78 to 4.93-point increases on a 40-point scale for sexual IPV and physical IPV, respectively. Similarly, a 1-unit increase in severity of sexual and any IPV led to increases in perceived stress ranging from 1.06- to 2.57-point increases, respectively.
The finding that stressful life events like financial, health, and conflict concerns increase the risk of IPV is consistent with previous research showing that financial constraints such as job loss or home foreclosure increase the likelihood of experiencing IPV [17, 47, 49, 50, 69]. While the events themselves do not inherently cause violent acts, they likely lead to increases in stress and conflict within the home, thereby increasing the likelihood of male perpetuation of IPV. Previous studies among men have found that economic, health, and interpersonal stressors are associated with increases in IPV perpetration [69, 70]. Some stressful life events such as changes in social status or conflict with family may not necessarily be preventable, but public health efforts to mitigate the impact of these events on marital and familial relations may help in reducing IPV. Such efforts might include increases in social or financial supports such as peer or professional support groups, affordable and accessible healthcare, and financial assistance [71].
Our second main finding that experiences and severity of IPV were associated with increases in levels of perceived stress is consistent with much of the literature [11, 13, 72, 73]. Among the subtypes, we found physical IPV to be associated with the largest increase in stress, a potentially novel finding. As previously mentioned, many of the previous studies were cross-sectional or retrospective, or took place in high- and middle-income (HMIC) settings [52]. However, findings are also consistent with one longitudinal study in pregnant and postpartum Latinas in the USA that found positive associations between IPV and perceived stress [74]. The longitudinal design and nuanced measures of IPV in the current study provide strong evidence for the causal relationship between IPV and increases in perceived stress. Many studies have attempted to use biological measures of stress (cortisol) to study this link [75, 76], but found null results, potentially a result of small sample sizes [52]. Of note, our findings conflict with one previous study in the USA that found no association between stressful life events and IPV or between IPV and perceived stress, but that study used a post-menopausal sample with high endorsement of emotional abuse and very high rates of IPV [77].
Risk factors for IPV exist at the individual, relationship, community, and societal levels [78]. Feminist and social learning theoretical frameworks can help guide our understanding of these risk factors and inform interventions to prevent and respond to IPV and its impacts. Within Pakistan, patriarchal institutions that shape power dynamics and perpetuate traditional gender attitudes exist in homes and among health service providers and decision-makers, allowing intergenerational patterns of violence to initiate and persist [39, 40, 71, 79]. Our finding that the impact of such underlying sociocultural factors associated with IPV may be exacerbated in the presence of stressors is consistent with prevailing stress-vulnerability models of IPV [42, 45]. For example, husbands who uphold patriarchal beliefs about gender roles may be more likely to respond to life stressors such as financial strain by engaging in violence against their wives than men who do not subscribe to such views, or those who do but who are less exposed to stressors. As a result, stress is appropriately characterized as “neither a necessary nor sufficient cause” for IPV perpetration [45]. However, in settings such as Pakistan, stressors as situational factors relevant to IPV have been relatively understudied and may be important targets for intervention as part of a multi-pronged approach to preventing and reducing IPV. The WHO recommends the implementation of high-quality intervention programs and policy changes that protect women, address gender-based inequalities, and reshape cultural perceptions and acceptability of violence [80]. Specifically, primary prevention efforts such as school-based programs that educate students on dating violence, gender equality training, promotion of healthy relationship and communication skills, reduction in substance use, and programmatic work that shapes cultural and social views of gender-based violence have been shown to be highly effective at preventing IPV in a different setting (South Africa) [81]. Further exploration of the efficacy of such programs in a setting such as Pakistan is needed. IPV programmatic development needs to be culturally appropriate and attend to the stigmatization survivor’s experience [82], even in settings where IPV is relatively endemic and normative, stigma itself can be an important stressor and source of ill health [83]. Secondary prevention efforts to reduce IPV and care for existing survivors may help in attenuating the link between IPV and stress. Such efforts include long-term rehabilitation to lessen trauma or reduce violence-associated disabilities. Further, local health care providers need to be educated on the intersection of gender-based violence with social and health outcomes, the proper communication and care for women experiencing IPV, local services for referral, and how to treat the physical and emotional consequences of the violence [71]. Interventions to prevent, reduce, and care for women experiencing IPV may result in reduced levels of stress during the postpartum period, a critical and vulnerable time for mothers, babies, and families. In cases where violence persists, healthcare providers may be able to alleviate the impact of stressful life events or stress through the provision of or referral to counseling.
Limitations
This study is subject to limitations. First, all data were self-reported so there may be some issues with differential recall of IPV based on stress levels. However, data are longitudinal and allow for a temporal lag, so there is a low likelihood that this impacted the current analysis with the exception of the 1-month overlap between past year IPV and past month perceived stress for the Aim 2 analysis. Second, our exposure of household stressors does not directly measure reported stressful life events as experienced by the husband, the perpetrator of IPV, which is the assumed mechanism by which stressor exposure could increase instances or exacerbation of IPV. Actual collection of these data points from the husband was not feasible given the sensitive nature of these topics. However, women’s report of stressful life events regarding their home, financial, and familial situation should serve as a reasonable proxy of stressful life events that may affect the perpetrator. Third, this study arises from a birth cohort study, so every woman in the sample has been pregnant. Thus, results may not be generalizable to nulliparous women. For this reason, it is possible that results could be attenuated compared to a more general sample. However, a few studies have concluded that IPV is not likely to statistically differ between the pregnancy and postpartum periods [84, 85]. Last, our study suffered from loss to follow-up and missing data. Specifically, our handling of missing IPV data may be biased as reasons behind non-response (e.g., women experiencing the most severe violence may be too fearful to respond) [86] may also be associated with increased stress levels, potentially resulting in estimates biased toward the null. We attempted to address this by utilizing stabilized IPW to account for missingness between the baseline sample and the sample with stress and IPV data at 12 and 24 months and utilizing the maximum available data for each IPV type. However, as a result of the slightly different analytic sample sizes, our ability to compare results across models and IPV types is somewhat limited.
Conclusions
Even in settings where IPV is highly prevalent and potentially normative, stressful life events like financial problems, changes in social status, and concerns about children may increase the risk of IPV and the severity of the violence. This violence may subsequently increase maternal stress levels, demonstrating a vicious cycle. Efforts to disrupt the cycle and better support women and their partners as they go through life changes and stressful experiences and mitigate the secondary effects of IPV may help to reduce the likelihood of IPV and increased stress in this population.
Funding
The Bachpan cohort was established by funding through the Human Development Research Foundation and leveraging the research study funded by the National Institute of Mental Health (U19MH95687) and National Institute of Child Health and Development (R01 HD075875; PI: Maselko). This analysis was supported in part by training grants from the National Institute of Child Health and Development [T32 HD52468; T32 HD091058].
Appendix
See Table 6.
Table 6.
Description of analytical measures and specific items
| Measure | Items |
|---|---|
|
| |
| Stressful Life Events “Have you or your family faced the following in the last year...” |
You or someone in your family has had any financial problem (having debt)? You or someone in your family has had a change in social status (e.g., someone’s engagement or marriage, separation or divorce, starting or finishing education)? You yourself have had any problem with your residence (e.g., change of residence or problems with neighbors)? Your relations with any of your close relatives or friends have been troubled (e.g., quarrels or falling out)? You have been worried about your children’s problems? You or other family members have had rows/quarrels among themselves? The household suffered from the death of any household member? The household suffered from any serious illness (> 10 days) of any household member? The household experienced loss of a paid employment/shrinkage of wage labor opportunity/sickness of wage earner? |
| Psychological IPV “Has your husband...” |
Insulted you or made you feel bad about yourself? Belittled or humiliated you in front of other people? Done things that scared or intimidated you on purpose, for example, by the way he looked at you, or by yelling or smashing things? Threatened to hurt you or someone you care about? Called you ugly or said something else negative about your appearance? Destroyed something belonging to you on purpose? Threatened to take another wife? Threatened to abandon you or send you back to your natal family? Threatened to divorce you? Said you were not able to please him sexually |
| Physical IPV “Has your husband...” |
Slapped you or thrown something at you that could hurt you? Pushed you or shoved you or pulled your hair? Choked or burnt you on purpose? Threatened to use a gun, knife or other Weapon against you? Actually used a gun, knife or other weapon against you? |
| Sexual IPV | Did your husband ever physically force you to have sexual intercourse when you did not want to? Did you ever have sexual intercourse when you did not want to because you were afraid of what your husband might do? Did your husband ever force you to do something sexual that you found degrading or humiliating? |
| Perceived Stress “In the last month, how often have you...” |
Been upset because of something that happened unexpectedly? Felt that you were unable to control the important things in your life? Felt nervous and “stressed”? Felt confident about your ability to handle your personal problems? Felt that things were going your way? Found that you could not cope with all the things that you had to do? Been able to control irritations in your life? Felt that you were on top of things? Been angered because of things that were outside of your control? Felt difficulties were piling up so high that you could not overcome them? |
Footnotes
Conflict of interest The authors have no relevant financial or non-financial interests to disclose.
Ethics approval This study was approved by institutional review boards at the Human Development Research Foundation, the University of North Carolina at Chapel Hill and Duke University. Written informed consent (or witnessed consent, if the participant was illiterate) was obtained from mothers before study participation.
Data availability statement
Data are available upon reasonable request from PI Maselko. Data are not publicly available due to ongoing data collection; however, data will be released when the Bachpan cohort study is completed.
References
- 1.Breiding M, Basile K, Smith S, Black M, Mahendra R (2015) Intimate partner violence surveillance uniform definitions and recommended data elements
- 2.World Health Organization (WHO) (2021) Violence against women prevalence estimates, 2018: global, regional and national prevalence estimates for intimate partner violence against women and global and regional prevalence estimates for non-partner sexual violence against women. Geneva
- 3.McLaughlin J, O’Carroll RE, O’Connor RC (2012) Intimate partner abuse and suicidality: a systematic review. Clin Psychol Rev 32:677–689. 10.1016/j.cpr.2012.08.002 [DOI] [PubMed] [Google Scholar]
- 4.Coker AL, Smith PH, Bethea L, King MR, McKeown RE (2000) Physical health consequences of physical and psychological intimate partner violence. Arch Fam Med 9:451–457. 10.1001/archfami.9.5.451 [DOI] [PubMed] [Google Scholar]
- 5.Smith S, Chen J, Basile K, Gilbert L, Merrick M, Patel N, et al. (2017) The National Intimate Partner and Sexual Violence Survey (NISVS): 2010–2012 State Report. Centers for Disease Control and Prevention; 2017 [Google Scholar]
- 6.Stöckl H, Devries K, Rotstein A, Abrahams N, Campbell J, Watts C et al. (2013) The global prevalence of intimate partner homicide: A systematic review. The Lancet 382:859–865. 10.1016/S0140-6736(13)61030-2 [DOI] [PubMed] [Google Scholar]
- 7.Coker AL, Davis KE, Arias I, Desai S, Sanderson M, Brandt HM et al. (2002) Physical and mental health effects of intimate partner violence for men and women. Am J Prev Med 23:260–268. 10.1016/S0749-3797(02)00514-7 [DOI] [PubMed] [Google Scholar]
- 8.Campbell JC (2002) Health consequences of intimate partner violence. The Lancet 359:1331–1336. 10.1016/S0140-6736(02)08336-8 [DOI] [PubMed] [Google Scholar]
- 9.Breiding MJ, Black MC, Ryan GW (2008) Chronic disease and health risk behaviors associated with intimate partner violence—18 U.S. States/Territories, 2005. Annal Epidemiol 18:538–544. 10.1016/J.ANNEPIDEM.2008.02.005 [DOI] [PubMed] [Google Scholar]
- 10.Jones L, Hughes M, Unterstaller U (2001) Post-traumatic stress disorder (PTSD) in victims of domestic violence: a review of the research. Trauma Violence Abuse 2:99–119. 10.1177/1524838001002002001 [DOI] [Google Scholar]
- 11.Agrawal A, Ickovics J, Lewis JB, Magriples U, Kershaw TS (2014) Postpartum intimate partner violence and health risks among young mothers in the United States: a prospective study. Matern Child Health J 18:1985–1992. 10.1007/s10995-014-1444-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Al-Modallal H (2012) Psychological partner violence and women’s vulnerability to depression, stress, and anxiety. Int J Ment Health Nurs 21:560–566. 10.1111/j.1447-0349.2012.00826.x [DOI] [PubMed] [Google Scholar]
- 13.Coker AL, Follingstad DR, Garcia LS, Bush HM (2017) Intimate partner violence and women’s cancer quality of life. Cancer Causes Control 28:23–39. 10.1007/s10552-016-0833-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Willie TC, Powell A, Kershaw T (2016) Stress in the City: influence of urban social stress and violence on pregnancy and postpartum quality of life among adolescent and young mothers. J Urban Health 93:19–35. 10.1007/s11524-015-0021-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Van Parys AS, Deschepper E, Michielsen K, Galle A, Roelens K, Temmerman M et al. (2015) Intimate partner violence and psychosocial health, a cross-sectional study in a pregnant population. BMC Pregnancy Childbirth. 10.1186/s12884-015-0710-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Thananowan N, Vongsirimas N (2016) Factors mediating the relationship between intimate partner violence and cervical cancer among thai women. J Interpers Violence 31:715–731. 10.1177/0886260514556108 [DOI] [PubMed] [Google Scholar]
- 17.Kingston D, Heaman M, Urquia M, O’Campo P, Janssen P, Thiessen K et al. (2016) Correlates of abuse around the time of pregnancy: results from a national survey of canadian women. Matern Child Health J 20:778–789. 10.1007/s10995-015-1908-6 [DOI] [PubMed] [Google Scholar]
- 18.Richardson R, Nandi A, Jaswal S, Harper S (2020) The effect of intimate partner violence on women’s mental distress: a prospective cohort study of 3010 rural Indian women. Soc Psychiatry Psychiatr Epidemiol 55:71–79. 10.1007/S00127-019-01735-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Anderson D, Saunders D (2003) Leaving an abusive partner: an empirical review of predictors, the process of leaving, and psychological well-being. Trauma Violence Abuse 4:163–191. 10.1177/1524838002250769 [DOI] [PubMed] [Google Scholar]
- 20.Lazarus R (1966) Psychological stress and the coping process. McGraw-Hill, New York [Google Scholar]
- 21.National Institute of Mental Health (2021) 5 things you should know about stress. US Department of Health and Human Services; n.d. https://www.nimh.nih.gov/sites/default/files/documents/health/publications/stress/19-mh-8109-5-things-stress.pdf (Accessed August 22, 2021). [Google Scholar]
- 22.Hendrix WH, Ovalle NK, Troxler RG (1985) Behavioral and physiological consequences of stress and its antecedent factors. J Appl Psychol 70:188–201. 10.1037/0021-9010.70.1.188 [DOI] [PubMed] [Google Scholar]
- 23.McFarlane AC (2010) The long-term costs of traumatic stress: intertwined physical and psychological consequences. World Psychiatry 9:3. 10.1002/J.2051-5545.2010.TB00254.X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.World Health Organization (2002) Violence by intimate partners. World Report on Violence and Health; pp. 89–121 [Google Scholar]
- 25.Capaldi DM, Knoble NB, Shortt JW, Kim HK (2012) A systematic review of risk factors for intimate partner violence. Partn Abus 3:231. 10.1891/1946-6560.3.2.231 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Benson ML, Wooldredge J, Thistlethwaite AB, Fox GL (2004) The correlation between race and domestic violence is confounded with community context. Soc Probl 51:326–342. 10.1525/SP.2004.51.3.326 [DOI] [Google Scholar]
- 27.van Wyk JA, Benson ML, Fox GL, DeMaris A (2016) Detangling individual-, partner-, and community-level correlates of partner violence. Crime Delinquency 49:412–438. 10.1177/0011128703049003004 [DOI] [Google Scholar]
- 28.Jain S, Buka S, Subramanian S, Molnar B (2010) Neighborhood predictors of dating violence victimization and perpetration in young adulthood: a multilevel study. Am J Public Health 100:1737–1744. 10.2105/AJPH.2009.169730 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Rothman E, Johnson R, Young R, Weinberg J, Azrael D, Molnar B (2011) Neighborhood-level factors associated with physical dating violence perpetration: results of a representative survey conducted in Boston. MA J Urban Health 88:201–213. 10.1007/S11524-011-9543-Z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Counts DA, Brown JK, Campbell JC (2019) Sanctions and sanctuary: Cultural perspectives on the beating of wives. Sanctions and Sanctuary: Cultural Perspectives on the Beating of Wives 1–268. 10.4324/9780429305306. [DOI] [Google Scholar]
- 31.Heise L (2016) An integrated, ecological framework. Violence Against Women 4:262–290. 10.1177/1077801298004003002 [DOI] [PubMed] [Google Scholar]
- 32.Rodriguez E, Lasch K, Chandra P, Lee J (1978) Family violence, employment status, welfare benefits, and alcohol drinking in the United States: what is the relation? J Epidemiol Commun Health 2001(55):172–178. 10.1136/JECH.55.3.172 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kim H, Laurent H, Capaldi D, Feingold A (2008) Men’s aggression toward women: A 10-year panel study. J Marriage Fam 70:1169–1187. 10.1111/J.1741-3737.2008.00558.X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Sorenson S, Upchurch D, Shen H (1996) Violence and injury in marital arguments: risk patterns and gender differences. Am J Public Health 86:35–40. 10.2105/AJPH.86.1.35 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Cunradi CB, Caetano R, Schafer J (2002) Socioeconomic predictors of intimate partner violence among white, black, and hispanic couples in the United States. J Family Violence 17:377–389. 10.1023/A:1020374617328 [DOI] [Google Scholar]
- 36.Roberts A, Gilman S, Fitzmaurice G, Decker M, Koenen K (2010) Witness of intimate partner violence in childhood and perpetration of intimate partner violence in adulthood. Epidemiology 21:809–818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Ehrensaft M, Cohen P, Brown J, Smailes E, Chen H, Johnson J (2003) Intergenerational transmission of partner violence: a 20-year prospective study. J Consult Clin Psychol 71:741–753. 10.1037/0022-006X.71.4.741 [DOI] [PubMed] [Google Scholar]
- 38.Linder J, Collins W (2005) Parent and peer predictors of physical aggression and conflict management in romantic relationships in early adulthood. J Fam Psychol 19:252–262. 10.1037/0893-3200.19.2.252 [DOI] [PubMed] [Google Scholar]
- 39.Jewkes R (2002) Intimate partner violence: causes and prevention. The Lancet 359:1423–1429. 10.1016/S0140-6736(02)08357-5 [DOI] [PubMed] [Google Scholar]
- 40.O’Leary K (1988) Physical aggression between spouses: A social learning theory perspective. Handbook of family violence, Springer, Boston, MA: pp. 31–55. 10.1007/978-1-4757-5360-8_3 [DOI] [Google Scholar]
- 41.Karney BR, Bradbury TN (1995) The longitudinal course of marital quality and stability: a review of theory, method, and research. Psychol Bull 118:3–34. 10.1037/0033-2909.118.1.3 [DOI] [PubMed] [Google Scholar]
- 42.The Oxford Handbook of Close Relationships (2013). The Oxford Handbook of Close Relationships. 10.1093/OXFORDHB/9780195398694.001.0001 [DOI]
- 43.Riggs DS, O’Leary KD (1996) Aggression between heterosexual dating partners: An examination of a causal model of courtship aggression. J Interpers Violence 11:519–540. 10.1177/088626096011004005 [DOI] [Google Scholar]
- 44.Cano A, Vivian D (2001) Life stressors and husband-to-wife violence. Aggress Violent Beh 6:459–480. 10.1016/S1359-1789(00)00017-3 [DOI] [Google Scholar]
- 45.Eckhardt CI, Parrott DJ (2017) Stress and intimate partner aggression. Curr Opin Psychol 13:153–157. 10.1016/J.COPSYC.2016.09.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Caetano R, Ramisetty-Mikler S, Vaeth PAC, Harris TR (2007) Acculturation stress, drinking, and intimate partner violence among hispanic couples in the U.S. J Interpersonal Violence 22:1431–1447. 10.1177/0886260507305568 [DOI] [PubMed] [Google Scholar]
- 47.Chu SY, Goodwin MM, D’Angelo DV (2010) Physical violence against US women around the time of pregnancy, 2004–2007. Am J Prevent Med 38:317–322. 10.1016/j.amepre.2009.11.013 [DOI] [PubMed] [Google Scholar]
- 48.Yan E, Chan KL (2012) Prevalence and correlates of intimate partner violence among older Chinese couples in Hong Kong. Int Psychogeriatr 24:1437–1446. 10.1017/S1041610212000294 [DOI] [PubMed] [Google Scholar]
- 49.Pattavina A, Socia KM, Zuber MJ (2015) Economic stress and domestic violence: examining the impact of mortgage foreclosures on incidents reported to the police. Justice Res Policy 16:147–164. 10.1177/1525107115623938 [DOI] [Google Scholar]
- 50.Schumacher JA, Coffey SF, Norris FH, Tracy M, Clements K, Galea S (2010) Intimate partner violence and Hurricane Katrina: Predictors and associated mental health outcomes. Violence Vict 25:588–603. 10.1891/0886-6708.25.5.588 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Baranov V, Cameron L, Contreras Suarez D, Thibout C (2021) Theoretical underpinnings and meta-analysis of the effects of cash transfers on intimate partner violence in low- and middle-income countries. J Develop Stud 57:1–25. 10.1080/00220388.2020.1762859 [DOI] [Google Scholar]
- 52.Yim IS, Kofman YB (2019) The psychobiology of stress and intimate partner violence. Psychoneuroendocrinology 105:9–24. 10.1016/j.psyneuen.2018.08.017 [DOI] [PubMed] [Google Scholar]
- 53.Yakubovich A, Stöckl H, Murray J, Melendez-Torres G, Steinert J, Glavin C et al. (2018) Risk and protective factors for intimate partner violence against women: systematic review and meta-analyses of prospective-longitudinal studies. Am J Public Health 108:e1–11. 10.2105/AJPH.2018.304428 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Global and regional estimates of violence against women n.d https://www.who.int/publications/i/item/9789241564625 (Accessed November 14, 2021).
- 55.Solotaroff JL, Pande RP (2014) Violence against Women and Girls: Lessons from South Asia. 10.1596/978-1-4648-0171-6 [DOI]
- 56.Ali PA, Naylor PB, Croot E, O’Cathain A (2015) Intimate partner violence in pakistan: a systematic review. Trauma Violence Abuse 16:299–315. 10.1177/1524838014526065 [DOI] [PubMed] [Google Scholar]
- 57.Andersson N, Cockcroft A, Ansari U, Omer K, Ansari NM, Khan A et al. (2010) Barriers to disclosing and reporting violence among women in Pakistan: findings from a national household survey and focus group discussions. J Interpers Violence 25:1965–1985. 10.1177/0886260509354512 [DOI] [PubMed] [Google Scholar]
- 58.Esie P, Osypuk T, Schuler S, Bates L (2019) Intimate partner violence and depression in rural Bangladesh: Accounting for violence severity in a high prevalence setting. SSM Popul Health. 10.1016/J.SSMPH.2019.100368 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Esie P, Osypuk TL, Schuler SR, Bates LM (2021) Social norms and the association between intimate partner violence and depression in rural Bangladesh-a multilevel analysis. Soc Psychiatry Psychiatr Epidemiol 56:2217–2226. 10.1007/S00127-021-02044-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Turner EL, Sikander S, Bangash O, Zaidi A, Bates L, Gallis J et al. (2016) The effectiveness of the peer-delivered Thinking Healthy PLUS (THPP+) Program for maternal depression and child socioemotional development in Pakistan: study protocol for a randomized controlled trial. Trials 17:57–79. 10.1186/S13063-016-1530-Y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Brown GW, Harris T (2021) Life events and illness. Guilford Press; 1989. https://psycnet.apa.org/record/1989-97618-000 (Accessed March 30, 2021) [Google Scholar]
- 62.Rahman A, Iqbal Z, Harrington R (2003) Life events, social support and depression in childbirth: perspectives from a rural community in the developing world. Psychol Med 33:1161–1167. 10.1017/S0033291703008286 [DOI] [PubMed] [Google Scholar]
- 63.WHO (2005) WHO multi-country study on women’s health and domestic violence against women. World Health Organization [Google Scholar]
- 64.Cohen S, Kamarck T, Mermelstein R (1983) A global measure of perceived stress. J Health Soc Behav 24:385–396. 10.2307/2136404 [DOI] [PubMed] [Google Scholar]
- 65.Maselko J, Bates L, Bhalotra S, Gallis J, O’Donnell K, Sikander S et al. (2017) Socioeconomic status indicators and common mental disorders: Evidence from a study of prenatal depression in Pakistan. SSM Popul Health 4:1–9. 10.1016/J.SSMPH.2017.10.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Kolenikov S, Angeles G (2009) Socioeconomic status measurement with discrete proxy variables: is principal component analysis a reliable answer? Rev Income Wealth 55:128–165. 10.1111/J.1475-4991.2008.00309.X [DOI] [Google Scholar]
- 67.Maselko J, Bates L, Bhalotra S, Gallis JA, O’Donnell K, Sikander S et al. (2018) Socioeconomic status indicators and common mental disorders: Evidence from a study of prenatal depression in Pakistan. SSM Popul Health 4:1–9. 10.1016/J.SSMPH.2017.10.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Zou G (2004) A modified poisson regression approach to prospective studies with binary data. Am J Epidemiol 159:702–706. 10.1093/AJE/KWH090 [DOI] [PubMed] [Google Scholar]
- 69.Schwab-Reese LM, Peek-Asa C, Parker E (2016) Associations of financial stressors and physical intimate partner violence perpetration. Injury Epidemiol. 10.1186/S40621-016-0069-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Roberts AL, McLaughlin KA, Conron KJ, Koenen KC (2011) Adulthood stressors, history of childhood adversity, and risk of perpetration of intimate partner violence. Am J Prev Med 40:128–138. 10.1016/J.AMEPRE.2010.10.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.World Health Organization (WHO) (2011) Regional Office for the Eastern Mediterranean. Rapid assessment: health sector capacity and response to gender-based violence in Pakistan. https://apps.who.int/iris/handle/10665/119948 (Accessed November 14, 2021). [Google Scholar]
- 72.Ely GE, Otis MD (2011) An examination of intimate partner violence and psychological stressors in adult abortion patients. J Interpers Violence 26:3248–3266. 10.1177/0886260510393004 [DOI] [PubMed] [Google Scholar]
- 73.Ferreira P, Loxton D, Tooth LR (2017) Intimate personal violence and caregiving: Influences on physical and mental health in middle-aged women. Maturitas 102:34–40. 10.1016/J.MATURITAS.2017.05.001 [DOI] [PubMed] [Google Scholar]
- 74.Rodríguez MA, Valentine J, Ahmed SR, Eisenman DP, Sumner LA, Heilemann MS et al. (2010) Intimate partner violence and maternal depression during the perinatal period: a longitudinal investigation of Latinas. Violence Against Women 16:543–559. 10.1177/1077801210366959 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Danielson AM, Matheson K, Anisman H (2011) Cytokine levels at a single time point following a reminder stimulus among women in abusive dating relationships: Relationship to emotional states. Psychoneuroendocrinology 36:40–50. 10.1016/J.PSYNEUEN.2010.06.003 [DOI] [PubMed] [Google Scholar]
- 76.Bernard NK, Kashy DA, Levendosky AA, Bogat GA, Lonstein JS (2017) Do different data analytic approaches generate discrepant findings when measuring mother–infant HPA axis attunement? Dev Psychobiol 59:174–184. 10.1002/DEV.21474 [DOI] [PubMed] [Google Scholar]
- 77.Newton TL, Fernandez-Botran R, Miller JJ, Lorenz DJ, Burns VE, Fleming KN (2011) Markers of inflammation in midlife women with intimate partner violence histories. J Womens Health (Larchmt) 20:1871–1880. 10.1089/JWH.2011.2788 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Hardesty JL, Ogolsky BG (2020) A socioecological perspective on intimate partner violence research: a decade in review. J Marriage Fam 82:454–477. 10.1111/JOMF.12652 [DOI] [Google Scholar]
- 79.World Health Organization, Pan American Health Organization (2012) Understanding and addressing violence against women: intimate partner violence. World Health Organization. https://apps.who.int/iris/handle/10665/77432 [Google Scholar]
- 80.World Health Organization (WHO) (2021) Violence Against Women [Google Scholar]
- 81.World Health Organization (WHO) (2010) Preventing intimate partner and sexual violence against women: taking action and generating evidence. World Health Organization. https://apps.who.int/iris/handle/0665/44350 [DOI] [PubMed] [Google Scholar]
- 82.Ali TS, Farhan R, Ayub M (2020) Intimate partner violence against women in Pakistan: a review of qualitative research. J Pak Med Assoc 70:892–903. 10.5455/JPMA.20759 [DOI] [PubMed] [Google Scholar]
- 83.Hatzenbuehler ML (2009) How does sexual minority stigma “Get under the skin”? A psychological mediation framework. Psychol Bull 135:707–730. 10.1037/A0016441 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Groves AK, McNaughton-Reyes HL, Foshee VA, Moodley D, Maman S (2014) Relationship factors and trajectories of intimate partner violence among south african women during pregnancy and the postpartum period. PLoS ONE 9:106829. 10.1371/JOURNAL.PONE.0106829 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Koenig L, Whitaker D, Royce R, Wilson T, Ethier K, Fernandez M (2006) Physical and sexual violence during pregnancy and after delivery: a prospective multistate study of women with or at risk for HIV infection. Am J Public Health 96:1052–1059. 10.2105/AJPH.2005.067744 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.McNutt L-A, Lee R (2000) Intimate partner violence prevalence estimation using telephone surveys: understanding the effect of nonresponse bias. Am J Epidemiol 152:438–441. 10.1093/AJE/152.5.438 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data are available upon reasonable request from PI Maselko. Data are not publicly available due to ongoing data collection; however, data will be released when the Bachpan cohort study is completed.


