The affordable care act provision to expand access to Medicaid (Medicaid expansion, or ME) increased insurance coverage among individuals with cancer. Increasing evidence suggests ME impacts cancer outcomes, yet the implication of ME on primary malignant brain tumor (PMBT) outcomes remains unknown. This study suggests ME may result in an increase in 1-year predictive overall survival (1YPS) among PMBT patients.
Individuals with PMBTs have short survival and high morbidity,1 with uninsured individuals more likely to: experience delayed care2; have greater tumor burden; receive lower levels of care; and experience greater mortality rates.3,4 The Patient Protection and Affordable Care Act expanded the Medicaid public insurance program in the United States and by 2014 25 states had opted into the program, facilitating healthcare access to 21-million poor and low-income individuals.5 In other cancer types, studies have linked ME with increased earlier stage diagnoses and improved survival.6 However, the impact of ME on individuals with PMBTs has not been examined.
Data for diagnosis years 2004–2018 were obtained from the National Cancer Database (NCDB), containing clinical oncology data from more than 70% of new cancer cases from over 1500 Commission on Cancer (CoC) accredited US facilities. PMBT histopathologies were classified per the Central Brain Tumor Registry of the United States (CBTRUS) report.1 Individuals were defined as either (1) diagnosed before 2014 in a nonexpansion state, (2) diagnosed after 2014 in a nonexpansion state, (3) diagnosed before 2014 in an expansion state, or (4) diagnosed after 2014 in an expansion state.
Demographic factors included: sex, race/ethnicity (White non-Hispanic, Black non-Hispanic, White Hispanic, Other) and age (40–64 years). Supplementary geographic location (urban, rural) was extrapolated from residence zip code. The Charlson–Deyo comorbidity index (0–3+) was included, providing the number of comorbidities at diagnosis. Individuals were excluded if any of the following were unknown: race/ethnicity, survival data, or state expansion status. The 1YPS was calculated using the pseudo-observation method.7 Difference-in-difference (DID) models were employed, stratified by each variable (except insurance status) and including all other variables (except insurance status) as confounding factors to assess the variable (eg, 1YPS) as a percentage point change for the group of interest (ME-states) after an event (ME) adjusting for the 1YPS change in the comparison group (non-ME-states).8 Statistical significance was considered at P < .05.
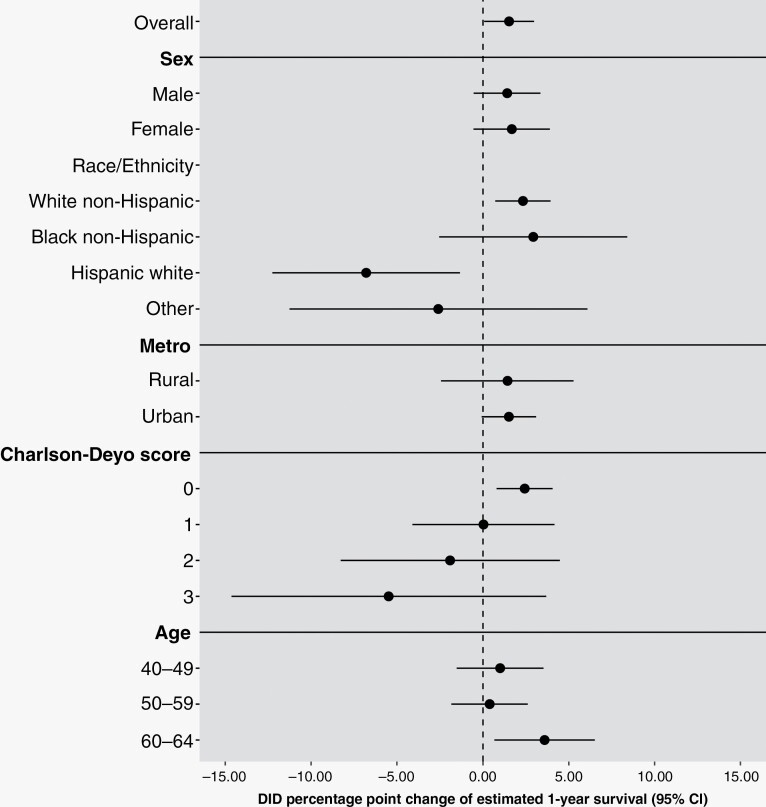
69 880 individuals with PMBTs were analyzed. Non-ME-states had 19 872 (a 28.4% share of total population) and 10 395 (14.9%) individuals diagnosed either before or after 2014, respectively. ME-states had 25 355 (36.2%) and 14 258 (20.4%) individuals diagnosed before and after 2014, respectively. Study population consisted of 40 463 (58%) males and 29 417 (42%) females. In expansion states, the 1YPS increased for individuals diagnosed after expansion (1YPS = 69.28%) compared with before expansion (1YPS = 66.08%). DID modeling showed an increase in 1YPS associated with ME (DID: 1.52%, 95% CI: 0.06–2.98) (Figure 1).
Figure 1.
Difference-in-difference (DID) results, as percentage point change of 1 year predicted survival (1YPS); before versus after the Medicaid expansion in 2014, overall, and by factors associated with overall survival for primary malignant brain tumors (PMBTs).
The impact of ME on 1YPS was observed in individuals who are White non-Hispanic (DID: 2.33%, 95% CI: 0.71 to 3.94) whereas individuals who are White Hispanics had a negative association of 1YPS (DID: −6.79%, 95% CI −12.26 to −1.32). Additionally, increases in 1YPS were shown in individuals who were either: diagnosed without comorbidities (Charlson–Deyo comorbidity score = 0; DID: 2.43%, 95% CI: 0.79–4.06) or 60–64 years old (DID: 3.59%, 95% CI: 0.66–6.52). No significant increase in 1YPS was observed for males or females.
In expansion states, the number of uninsured individuals dropped by more than half (5.2%–2.3%) after expansion, while the number of individuals with Medicaid increased (10.3%–15.1%) while in non-ME-states not-insured dropped by only 0.7% (8.6%–7.9%) and Medicaid participants increased by 0.6% (7.7%–8.3%). The ME reduced disparity gap in minority groups as the drop in uninsured and an increase in those insured in ME-states was observed through all racial/ethnical groups, in accordance with findings in other studies.9
For all demographic groups, there is an association between ME and an increase in 1YPS for individuals with PMBTs. The greatest impact of ME among ethnic and racial groups was observed in non-Hispanic Whites, the population most likely to develop PMBTs.1 The decrease in 1YPS following ME in Hispanic Whites may be the result of a decrease in care quality, or other factors beyond access to ME. This is the first finding, to our knowledge, that demonstrates a decrease in OS following ME. Other groups have either found no change in OS with Hispanic patients diagnosed with gynecological cancer.10 Interestingly, Han et al. found there was a decreased trend in 2-year OS in Hispanics newly diagnosed with cancer,6 suggesting this is an area, while beyond the scope of this study, that warrants further investigation.
Compared with other age groups, individuals diagnosed between 60 and 64 years of age had the greatest increase in 1YPS. This is likely because the risk of developing a brain tumor increases significantly with age reaching a peak at ~60 years. Similar findings were reported by Duarte et al. who found that access to insurance resulted in increased cancer detection among this near-elderly population after ME. This may be due to better and earlier tumor detection as well as improved access to treatments for insured populations resulting in improved outcomes.
It has been well established that comorbidities impact survival prognosis.11 Thus, it might be expected that ME would impact those individuals with the greatest number of comorbidities, yet this was not observed. The positive impact of ME on 1YPS was only observed in individuals with no comorbidities at the time of diagnosis. It is possible that the presence of comorbidities drives individuals to obtain insurance, and access to care, compared with those who have fewer health conditions and limited access. In this situation, the positive impact of ME may not be as easily observed in individuals with comorbidities. A limitation of NCDB data is the lack of ME status information on individuals under 40 years of age. Therefore, these individuals were excluded from this analysis. These data lack quality of life (QOL) information preventing any analysis of the impact on ME on QOL.
Taken together, these data demonstrate that ME positively impacts individuals with PMBTs as there was a significant increase in 1YPS in individuals with PMBT after the ME in 2014.
Contributor Information
Mantas Dmukauskas, Trans Divisional Research Program, Division of Cancer Epidemiology and Genetics, National Cancer Institute, Bethesda, Maryland, USA.
Gino Cioffi, Trans Divisional Research Program, Division of Cancer Epidemiology and Genetics, National Cancer Institute, Bethesda, Maryland, USA; Central Brain Tumor Registry of the United States, Hinsdale, Illinois, USA.
Corey Neff, Central Brain Tumor Registry of the United States, Hinsdale, Illinois, USA; Department of Neurosurgery, Duke University School of Medicine, Durham, North Carolina, USA.
Mackenzie Price, Central Brain Tumor Registry of the United States, Hinsdale, Illinois, USA; Department of Neurosurgery, Duke University School of Medicine, Durham, North Carolina, USA.
Kristin A Waite, Trans Divisional Research Program, Division of Cancer Epidemiology and Genetics, National Cancer Institute, Bethesda, Maryland, USA; Central Brain Tumor Registry of the United States, Hinsdale, Illinois, USA.
Carol Kruchko, Central Brain Tumor Registry of the United States, Hinsdale, Illinois, USA.
Justin M Barnes, Department of Radiation Oncology, Washington University School of Medicine in St. Louis, St. Louis, Missouri, USA.
Quinn T Ostrom, Central Brain Tumor Registry of the United States, Hinsdale, Illinois, USA; Department of Neurosurgery, Duke University School of Medicine, Durham, North Carolina, USA; The Preston Robert Tisch Brain Tumor Center, Duke University School of Medicine, Durham, North Carolina, USA; Duke Cancer Institute, Duke University Medical Center, Durham, North Carolina, USA.
Jill S Barnholtz-Sloan, Trans Divisional Research Program, Division of Cancer Epidemiology and Genetics, National Cancer Institute, Bethesda, Maryland, USA; Central Brain Tumor Registry of the United States, Hinsdale, Illinois, USA; Center for Biomedical Informatics and Information Technology, National Cancer Institute, Bethesda, Maryland, USA.
Funding
Funding for CBTRUS was provided by the Centers for Disease Control and Prevention (CDC) under Contract No. 75D30119C06056/Amendment 0002, the American Brain Tumor Association, Novocure, the Musella Foundation for Brain Tumor Research & Information, Inc., National Brain Tumor Society, the Pediatric Brain Tumor Foundation, The Sontag Foundation, the Uncle Kory Foundation, the Zelda Dorin Tetenbaum Memorial Fund, as well as private and in-kind donations. The research services of Jill S. Barnholtz-Sloan, Kristin A. Waite, and Gino Cioffi were provided by the Division of Cancer Epidemiology and Genetics (DCEG) of the National Cancer Institute (NCI).
Conflict of Interest Statement
The authors have no conflict of interest to declare. J.S.B.-S. is a full-time employee of the NIH/NCI. G.C. and K.A.W. are full-time contractors of the NIH/NCI. M.D. is a full-time postdoctoral fellow of the NIH/NCI.
Authorship Statement
Mantas Dmukauskas: investigation, methodology, formal analysis, visualization, writing original draft and editing; Gino Cioffi: data curation, investigation, methodology, formal analysis, visualization, writing original draft and editing; Corey Neff and Mackenzie Price: investigation, methodology, formal analysis, reviewing final draft; Kristin A. Waite: funding acquisition, investigation, formal analysis, writing original draft and editing, project administration, resources, supervision; Quinn T. Ostrom: data curation, conceptualization, formal analysis, investigation, methodology, visualization, reviewing final draft; Carol Kruchko: funding acquisition, investigation, project administration, resources, supervision, reviewing final draft; Jill S. Barnholtz-Sloan: conceptualization, investigation, project administration, resources, supervision, reviewing final draft.
References
- 1. Ostrom QT, Price M, Neff C, et al. CBTRUS statistical report: primary brain and other central nervous system tumors diagnosed in the United States in 2015–2019. Neuro Oncol. 2022;24(suppl 5):v1–v95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Chandra A, Rick JW, Dalle Ore C, et al. Disparities in health care determine prognosis in newly diagnosed glioblastoma. Neurosurg Focus. 2018;44(6):E16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Kolomaya A, Amin S, Lin C.. The association of health insurance with the survival of cancer patients with brain metastases at diagnosis. Tech Innov Patient Support Radiat Oncol. 2021;20:46–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Ermer T, Walters SL, Canavan ME, et al. Understanding the implications of Medicaid expansion for cancer care in the US: a review. JAMA Oncol. 2022;8(1):139–148. [DOI] [PubMed] [Google Scholar]
- 5. New Reports Show Record 35 Million People Enrolled in Coverage Related to the Affordable Care Act, with Historic 21 Million People Enrolled in Medicaid Expansion Coverage . 2022. Accessed November 2, 2022. https://www.hhs.gov/about/news/2022/04/29/new-reports-show-record-35-million-people-enrolled-in-coverage-related-to-the-affordable-care-act.html#:~:text=The%20ASPE%20findings%20build%20on,low%2Dincome%20adults%20under%2065
- 6. Han X, Zhao J, Yabroff KR, Johnson CJ, Jemal A.. Association between Medicaid expansion under the Affordable Care Act and survival among newly diagnosed cancer patients. J Natl Cancer Inst. 2022;114(8):1176–1185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Andersen PK, Perme MP.. Pseudo-observations in survival analysis. Stat Methods Med Res. 2010;19(1):71–99. [DOI] [PubMed] [Google Scholar]
- 8. Graves JA, Fry C, McWilliams JM, Hatfield LA.. Difference-in-differences for categorical outcomes. Health Serv Res. 2022;57(3):681–692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Nathan NH, Bakhsheshian J, Ding L, Mack WJ, Attenello FJ.. Evaluating Medicaid expansion benefits for patients with cancer: National Cancer Database analysis and systematic review. J Cancer Policy. 2021;29:100292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Huepenbecker SP, Fu S, Sun CC, et al. Medicaid expansion and 2-year survival in women with gynecologic cancer: a difference-in-difference analysis. Am J Obstet Gynecol. 2022;227(3):482.e1–482.e15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Carr MT, Hochheimer CJ, Rock AK, et al. Comorbid medical conditions as predictors of overall survival in glioblastoma patients. Sci Rep. 2019;9(1):20018. [DOI] [PMC free article] [PubMed] [Google Scholar]