Abstract
Introduction:
Poor operative ergonomics can lead to muscle fatigue and injury. However, formal ergonomics education is uncommon in surgical residencies. Our study examines the prevalence of musculoskeletal (MSK) symptoms, baseline ergonomics knowledge, and the impact of an ergonomics workshop in general surgery residents.
Methods:
An anonymous voluntary presurvey and postsurvey was distributed to all general surgery residents at a single academic residency, assessing resident characteristics, MSK symptoms, and ergonomic knowledge before and after an ergonomics workshop. The workshop consisted of a lecture and a personalized posture coaching session with a physiatrist.
Result:
The presurvey received 33/35 (94%) responses. Of respondents, 100% reported some degree of MSK pain. Prevalence of muscle stiffness and fatigue decreased with increasing height. Females reported higher frequencies of MSK pain (P = 0.01) and more muscle fatigue than males (100% versus 73%, P = 0.03). All residents reported little to no ergonomics knowledge with 68% reporting that ergonomics was rarely discussed in the operating room. The postsurvey received 26/35 (74%) responses. Of respondents, 100% reported the workshop was an effective method of ergonomics education. MSK symptom severity improved in 82% of residents. Reports that ergonomics was rarely discussed in the operating room significantly decreased to 22.8% of residents (P < 0.01).
Conclusions:
Surgical resident ergonomics knowledge is poor and MSK symptoms are common. Resident characteristics are associated with different MSK symptoms. Didactic teaching and personalized posture coaching improve ergonomics knowledge and reduce MSK symptom severity. Surgical residencies should consider implementing similar interventions to improve resident wellbeing.
Keywords: Ergonomics, General surgical resident, Improvement, Knowledge, Musculoskeletal symptoms
Introduction
A career in surgery is not only mentally challenging and timeintensive but also physically demanding. Surgeons spend many hours performing repetitive motions and are required to stand for extended periods of time while contorting their bodies into awkward positions (Fig. 1). They must focus intensely on the surgical field while adjusting for a wide variety of instruments and surgical accessories such as lead aprons and surgical loupes that are part of the modern operating room (OR) environment. As a result, 74% to 87% of surgeons report symptoms or injuries that they attribute to operating.1–3 Injuries such as cervical spinal stenosis, lumbar disc herniation, rotator cuff pathology, or carpal tunnel syndrome can result in surgeons requiring operative treatment, taking an absence from work or retiring early.4 Furthermore, injuries and pain can have consequences for personal relationships, disrupt sleep and cognition, and affect how surgeons manage their patients.5,6
Fig. 1 –

Intraoperative photo demonstrating poor operative ergonomics. Surgeon in the foreground is sustaining an awkward posture while the surgeon in the background has significant neck flexion while wearing a headlight and surgical loupes.
The applied science of ergonomics is “concerned with designing and arranging the environment so that people and their surroundings interact efficiently and safely”.7 Poor surgical ergonomic practices, non-neutral postures, and forceful repetitive tasks can lead to increases in severe work-related musculoskeletal (MSK) symptoms, muscle fatigue, and decreased surgeon productivity.4 Application of surgical ergonomic principles, such as microbreaks (brief intraoperative breaks with guided exercises), have been shown to improve work-related MSK symptoms.8,9 However, less than 15% of surgeons report being aware of any ergonomic guidelines.10 Few ergonomic education programs have been designed specifically for surgeons and formal ergonomics education is rare during surgical training.11,12 Currently, it is estimated that only 1.5% of all surgical and interventional procedural training programs provide formal ergonomics education.13
As operative habits are formed during training, surgical residencies offer the ideal environment to establish proper ergonomic practices and provide formal ergonomics education. To date, only a small number of studies have sought to examine ergonomic knowledge and work-related MSK symptoms in surgical residents.9,14–16 Our study aims to characterize the prevalence of work-related MSK symptoms and the level of ergonomics knowledge among general surgical residents and determine if a formalized surgical ergonomics education can improve knowledge and symptoms.
Methods
Participants
We conducted a quality improvement initiative aimed at all 35 categorical general surgical residents at a single tertiary care academic hospital. Involvement in the surveys and participating in the intervention were voluntary. All surveys were uncompensated, anonymous, and confidential. Approval was obtained from the residency program leadership and a human subjects’ exemption was obtained from the Northwestern University Institutional Review Board. The institutional review board approved a waiver of consent.
Preworkshop survey
The survey aimed to understand work-related MSK symptoms and their impact on residents’ work and wellbeing. Questions for the survey were adapted from published surveys assessing surgeon work-related MSK symptoms and ergonomics practices.15–18 The survey asked questions regarding residents’ demographics including height (Short, <5′4″; Average, 5′5″5′8″; and Tall, > 5′9″), glove size, gender, and training level. Training level was defined as junior residents (clinical postgraduate year [PGY] 1-3) or senior residents (clinical PGY 5-4 or research residents). Questions inquiring about pre-existing injuries/medical problems were not included in the survey, as they would be sensitive personal questions that could inadvertently identify an individual resident given the small size of the general surgery residents. Our primary outcome of interest was work-related pain which included site and severity (assessed using a Likert scale from 1 to 10 with 10 being the most severe). We asked about potential symptoms of poor ergonomic principles including eye strain or discomfort, numbness or tingling, stiffness, and muscle fatigue. We then asked if the symptoms affected resident wellness (i.e., sleep and ability to perform recreational activities) and if residents had sought treatment for their symptoms. Finally, we asked what elements of the OR environment residents thought contributed to their symptoms and how often ergonomics was discussed in the OR and inquired about their baseline ergonomic knowledge and education. We distributed a 35-question Qualtrics survey (Appendix A) to all 35 categorical general surgical residents at our institution via an anonymous e-mail link. The survey was available for approximately 2 wk in December 2020 to January 2021 and three e-mail reminders were sent during that period.
Surgical ergonomics workshop
Following the closing of the pre-ergonomics workshop survey, categorical surgery residents and attending surgeons attended a one-hour didactic lecture on surgical ergonomics in the OR in January 2021. The lecture was delivered as a Department of Surgery Grand Rounds by an experienced physical medicine and rehabilitation attending at our institution (M. E. Rho, MD) who is the section chief of MSK medicine and an expert on common work-related injuries experienced by surgeons. The lecture consisted of two parts. Part 1 covered the pathophysiology of neck and back pain and described how poor ergonomics can increase MSK load and pain, including common ergonomic mistakes made by surgeons, such as significant neck flexion and sustained static posture. Part 2 included guidance on posture and microbreaks which could be performed to alleviate and prevent these symptoms. The specific microbreaks discussed included the chin tuck, scapular retractions, and standing lumbar extensions.
Following the lecture, residents could volunteer to participate in a 15-minute personalized ergonomics coaching session. These sessions were conducted by physical medicine and rehabiliation faculty and fellows. During the coaching sessions, residents received tailored feedback based upon their current symptoms and body posture. Both the lecture and coaching sessions were delivered virtually because of COVID-19-related social distancing policies.
Postworkshop survey
We allowed for a 4-month period following the surgical ergonomics interventions so residents could implement ergonomic principles learned from the lecture and coaching session. A 26-question Qualtrics postintervention survey was distributed to all categorical general surgical residents via e-mail regardless of if they attended the ergonomics workshop. This survey aimed to assess resident understanding of the didactic session and changes in work related injuries, ergonomics practices, and ergonomics knowledge (Appendix B). The survey was available online for approximately 2 wk in April 2021 and three e-mail reminders were sent during that period.
Analysis
All survey results were uploaded into Qualtrics and analysis was performed using the same software. Chi-squared tests, Mann–Whitney U-tests, pairwise Z-tests, and Fisher’s exact tests were used to compare differences in survey results between residents of different demographics and examine differences between preintervention and postintervention surveys. All statistical analyses were two-sided with a predetermined significant threshold of P < 0.05. All analyses that involved the postergonomics survey included only residents who had responded he/she attended the intervention.
Results
Preworkshop respondent demographics
In total, 33 of 35 (94%) residents completed the preintervention survey. Of the respondents, 17 (52%) identified as male and 16 (48%) identified as female; 20 (61%) were junior residents; 17 (52%) were considered tall and seven (21%) were considered short. Resident glove size ranged from 5.5 to 7.5. The median resident glove size was 7 (interquartile range [IQR] 6-7).
Preworkshop ergonomics knowledge
All residents reported knowing little to nothing about ergonomics in response to the question “Rate your knowledge on ergonomics principles”. Only one (3%) resident reported ever receiving ergonomics education. Nine (27%) residents stated that ergonomics was “occasionally to most of the time” discussed in the OR and only eight residents (24%) reported feeling comfortable speaking up about ergonomics in the OR all the time, with 19 (57%) residents stating they felt comfortable speaking up depending on the attending. Conversely, 24 residents (72%) stated that applying ergonomics principles to the OR environment would contribute to their wellbeing. When asked which format would help them learn more about incorporating surgical ergonomics, residents reported a lecture or grand rounds, workshop from physiatrists, or a short presentation during the weekly education conferences as the most useful (64%, 64%, and 61%, respectively).
Preworkshop musculoskeletal symptoms
Of respondents, 33 (100%) reported experiencing some degree of pain or discomfort during or after operating with 29 (88%) residents reporting pain or discomfort anywhere from occasionally to all the time (Table). Only four (12%) residents reported experiencing pain rarely. The most affected areas of pain were neck (79%), back (76%), and shoulder (61%) with 27 (81%) residents reporting pain at multiple sites. Neck pain was ranked the most severe site by 14 (42%) residents and back pain was ranked the most severe site by eight (24%) residents. The median severity of pain during or after operating on a scale of 1-10 was 5 (IQR 4-6) while the median pain severity more than 4 weeks on a scale of 1-10 was 3.5/10 (IQR 2.3-4.8).
Table –
Frequency of symptoms among general surgical residents at a single academic institution.
| Symptom | Frequency |
||||
|---|---|---|---|---|---|
| Never |
Rarely |
Occasionally |
Most times |
All the time |
|
| Asymptomatic | Symptomatic | ||||
| Pain/discomfort | 0 (0%) | 4 (12%) | 18 (55%) | 7 (21%) | 4 (12%) |
|
| |||||
| 4 (12%) | 29 (88%) | ||||
|
| |||||
| Eye strain/discomfort | 15 (46%) | 7 (21%) | 10 (30%) | 1 (3%) | 0 (0%) |
|
| |||||
| 22 (67%) | 11 (33%) | ||||
|
| |||||
| Numbness/tingling | 18 (55%) | 9 (27%) | 5 (15%) | 1 (3%) | 0 (0%) |
|
| |||||
| 27 (82%) | 6 (18%) | ||||
|
| |||||
| Stiffness | 6 (18%) | 4 (12%) | 16 (49%) | 6 (18%) | 1 (3%) |
|
| |||||
| 10 (30%) | 23 (70%) | ||||
|
| |||||
| Muscle fatigue | 5 (15%) | 2 (6%) | 21 (64%) | 4 (12%) | 1 (3%) |
|
| |||||
| 7 (21%) | 26 (79%) | ||||
When asked about other symptoms, 18 (55%) residents experienced eye strain related to operating, with 11 (33%) of residents reporting it occurred occasionally to most times. Numbness and tingling were reported by 15 (45%) residents with only six (18%) reporting it occurred occasionally to most times. Stiffness was reported by 27 (82%) residents, with 23 (70%) residents reporting it occurred occasionally to all the time. Muscle fatigue was common with 28 (85%) residents reporting muscle fatigue and 26 (79%) stating that it occurred occasionally to all the time. The results are summarized in Table. Few residents reported their work-related MSK symptoms affected their life outside of work, with only six (18%) residents experiencing occasional sleep disruptions and 13 (39%) residents experiencing recreational activity disruptions.
Preworkshop resident characteristics associated with musculoskeletal symptoms
Training year
Senior residents were significantly more likely to have back pain compared to junior residents (100% versus 66%, P = 0.04). There were no significant differences in existence of pain, eye strain, numbness/tingling, stiffness, or muscle fatigue between junior and senior residents.
Gender
When assessing frequency of pain experienced while or after operating, female residents reported experiencing pain more frequently compared to male residents (P = 0.01) (Fig. 2). However, their pain not only differed in frequency but also in location. Female residents were significantly more likely to have neck pain compared to male residents (100% uersus 75%, P = 0.04). Furthermore, female residents were more likely to report muscle fatigue compared to males (100% uersus 73.3%, P = 0.03).
Fig. 2 –
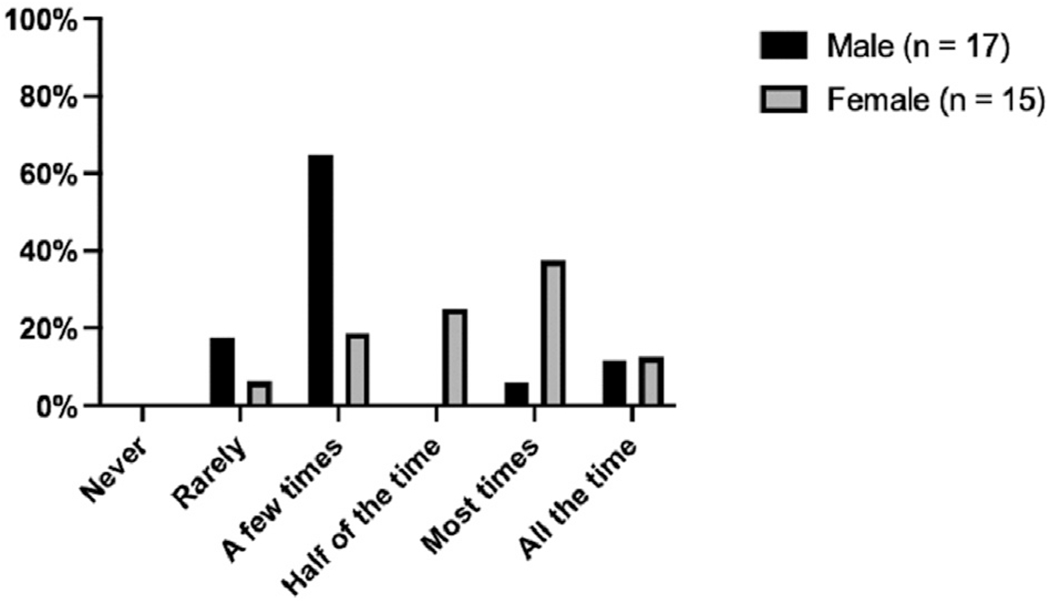
Prevalence of musculoskeletal pain related to operating among general surgical residents at a single academic institution stratified by gender. Female surgery residents report higher frequencies of musculoskeletal compared to males (P = 0.01).
Height
As resident height decreased, resident muscle stiffness and muscle fatigue increased (Fig. 3). There were no other notable differences in existence of pain, location of pain, eye strain, or numbness/tingling based on height.
Fig. 3 –
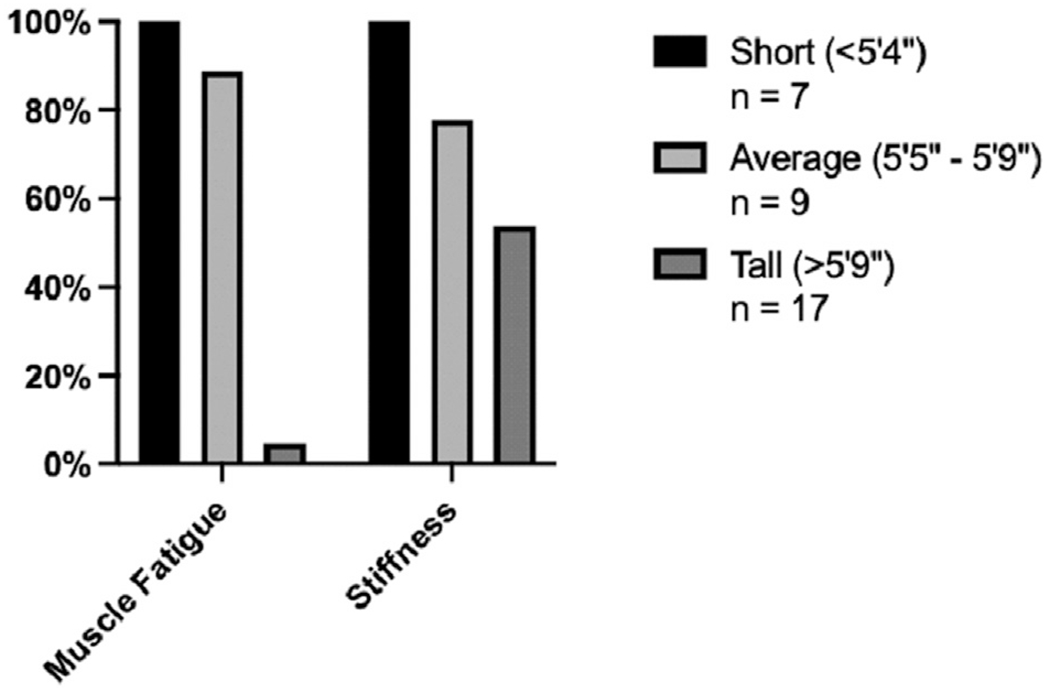
Prevalence of muscle fatigue and stiffness among general surgical residents at a single academic institution by resident height.
Glove size
There were no significant differences in existence of pain, location of pain, eye strain, numbness/tingling, stiffness, or muscle fatigue based on resident glove size.
Preworkshop factors attributing to musculoskeletal symptoms
To better assess possible solutions to operating related symptoms, residents were asked what factors contributed to their symptoms and if they sought any treatment. Residents attributed their symptoms to performing a high volume of cases, lack of breaks during long cases, table height, instrument design, same standing positions for extended time, surgical accessories (headlight, loupes, lead apron, etc.), and poor posture. The same standing position for extended time (n = 23, 70%), poor posture (n = 15, 45%), surgical accessories (n = 14, 42%), and inappropriate table height (n = 14, 42%) were reported most frequently. When asked what elements of the OR environment could be improved, residents chose surgical accessories (n = 14, 42%), surgical instruments (laparoscopic) (n = 14, 42%), and antifatigue mats (n = 12, 36%) most commonly. Six (18%) residents reported seeking treatment for their symptoms. None reported receiving any surgical treatment. Residents reported the use of exercise (n = 11, 33%), compression socks (n = 12, 36%), special shoes (n = 7, 21%), and microbreaks (n = 6, 18%) to help alleviate/prevent symptoms.
Postergonomics workshop survey demographics
Four months following the surgical ergonomics workshop, 26 of 35 (74%) residents responded to the postergonomics education survey. Twenty two of the 26 (85%) respondents reported they attended the surgical ergonomics workshop (Grand Rounds didactics lecture and personalized coaching session). The responding residents who attended the workshop had similar demographics to those who responded to the presurvey. Of the respondents who attended the workshop, 12 (55%) identified as female and 10 (45%) identified as male, 13 (59%) were junior residents, and 12 (54%) were considered tall and 5 (23%) were considered short. Resident glove size ranged from 5.5 to 8. The median resident glove size was 6.5 (IQR 6.1-7).
Postergonomics workshop musculoskeletal symptom improvement
All the following results were based on the 22 respondents who attended the surgical ergonomics workshop. When asked “Following the intervention do you feel that applying ergonomic principles to your OR environment has improved your symptom severity or frequency?” 18 (82%) residents reported an improvement in their symptom severity or frequency. Furthermore, when asked how severe the pain was in the area of the body which experienced the most severe pain, on a Likert scale from 1 (very mild) to 10 (very severe), residents reported their pain was anywhere from 1 to 7, with a median of 3 (IQR 1.5-4). On a bivariate analysis, there was significant improvement in the severity of pain when compared to before the surgical ergonomics education workshop (preintervention median 5, IQR 4-6; postintervention median of 3, IQR 1.5-4; P < 0.01). Many residents also reported improvements in eye strain, numbness/tingling, stiffness, and muscle fatigue following the surgical ergonomics workshop (50%, 45%, 73%, and 55%, respectively). There were no significant differences between reported improvements in pain severity/frequency, eye strain, numbness/tingling, stiffness, and muscle fatigue based on resident gender, training year, height, or glove size.
Postergonomics workshop implemented ergonomic practices
All residents who attended the surgical ergonomics workshop found it to be an effective method of education about ergonomics. Sixteen (73%) residents stated that applying ergonomics principles to their OR environment contributed to their overall wellbeing. Newly implemented practices by residents included adjusting the table height (73%), improved room set-up (64%), microbreaks (64%), and exercise (45%). Seventy seven percent of residents now reported that ergonomics was discussed in the OR occasionally to most times, which was a significant improvement when compared with pre-ergonomics workshop rates (P < 0.01) (Fig. 4).
Fig. 4 –
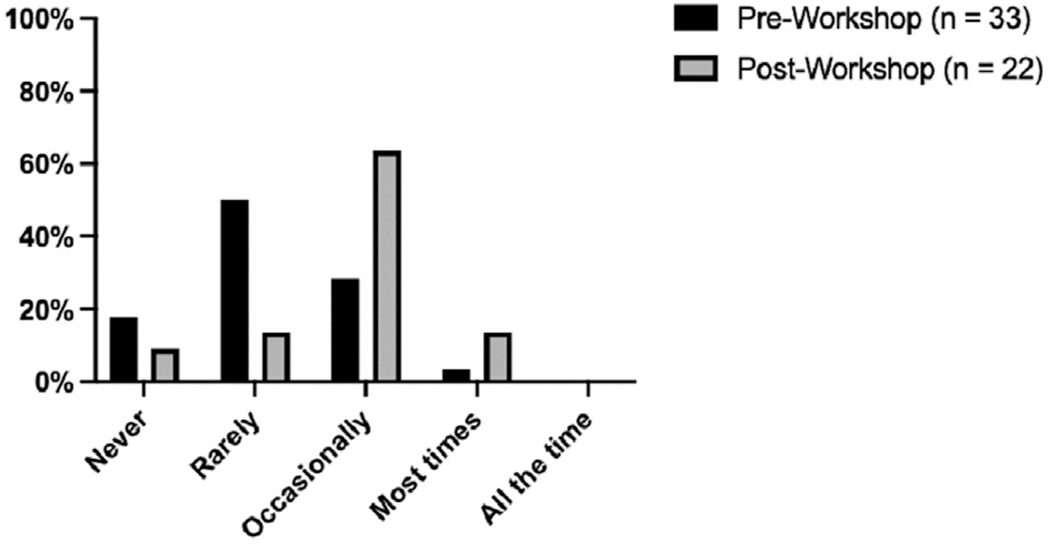
Frequency of discussion of ergonomics in the operating room before and after ergonomics workshop. The frequency to which ergonomics was discussed in the operating room following the ergonomics workshop significantly increased compared to before the workshop (P < 0.01).
Discussion
Our study demonstrates that work-related MSK symptoms are highly prevalent among general surgical residents, with all residents reporting some degree of pain or discomfort related to operating. Furthermore, symptoms including eye strain, numbness/tingling, stiffness, and muscle fatigue are common. Finally, surgical ergonomics knowledge among general surgical residents is poor with only 3% reporting formal ergonomics training and all residents reporting little to no ergonomics knowledge. These findings indicate that work-related MSK symptoms begin in training and that formalized ergonomics education coupled with the early establishment of ergonomic practices (e.g., microbreaks, body posture) has the potential to prevent future injury. Similar findings were reported by Jensen et al. at the University of Iowa, who studied the impact of two 1-h ergonomic didactic lectures on general surgical resident ergonomics knowledge. They found that MSK symptoms attributed to operating were highly prevalent, with 91% of residents reporting symptoms. However, Jensen et al. did not include personalized posture coaching and did not assess the impact of their intervention on MSK symptoms.9 Our study suggests that a surgical ergonomics workshop consisting of didactics and personalized coaching has the potential to not only improve knowledge and awareness but also to improve MSK symptoms among general surgery residents.
Musculoskeletal symptoms in surgical residents
In other surgical specialties, studies have found MSK symptoms to be highly prevalent (>90%) among residents.9,14,15 However, none have shown trainee year to be associated with worse symptoms. Kokosis et al. found that increasing trainee year had no correlation with pain.15 Our study confirmed these findings and demonstrated no significant difference in overall rates of MSK symptoms by the level of training. We did find that senior residents had more back pain specifically, which could be due to increased complexity and duration of cases. These findings suggest that MSK symptoms begin early and that preventive measures or interventions should be initiated as soon as possible in surgical training.
Without intervention, MSK symptoms in surgical residents are likely to worsen, increasing the risk of significant injury. Investigators have commented on how the altruistic nature of surgeons can further exacerbate injuries as surgeons prioritize the health and wellbeing of their patients over their own. This could explain why less than half of surgeons seek treatment for their MSK symptoms.6,19 Our results were similar with less than 20% of residents seeking treatment.
These findings highlight that in addition to teaching and practicing ergonomic principles, emphasis should be placed on the timely management of symptoms and types of treatment available.
Previous studies have sought to determine surgeon characteristics that are associated with developing MSK symptoms. Park et al. found that MSK symptoms were associated with case volume but were not associated with surgeon characteristics (e.g., height, age, gender).1 Sutton et al. found that OR designs favor taller surgeons and that female surgeons experienced more hand discomfort.20 However, both studies were limited in their generalizability as they included only minimally invasive surgery attendings and fellows. In general surgical residents, Jensen et al. found that female residents more commonly had low back pain and that lower resident height and weight was associated with symptoms of weakness.9 Similarly, Wong et al. found that female otolaryngology residents were significantly more likely to experience neck and wrist/hand symptoms.16 Our study also found differences in MSK symptoms based on gender and height. Pain frequency, stiffness, and neck pain were more common in female residents while stiffness and muscle fatigue were more common in shorter residents. These results suggest that there are operator characteristics among surgical residents that are independently associated with MSK symptoms. Identifying residents at the greatest risk of MSK symptoms may allow for targeted interventions and manipulation of the OR environment to facilitate ergonomic practice. Traditionally, surgical instruments and ORs were designed in an era where surgeons were predominantly male. The finding that MSK symptoms are more common in female surgeons may reflect the fact that instrument and OR design did not consider the needs of female or shorter surgeons. Indeed, our results found that nearly 50% of surgical residents felt that surgical accessories and instruments should be improved. As the surgical community continues to diversify, versatile OR and instrument designs that allow ergonomic use by all surgeons will be increasingly important.
Resident ergonomics knowledge
Our study demonstrated that ergonomics knowledge is lacking in general surgical residents at our institution. Only 3% of residents reported receiving any formal ergonomics education, which is similar to other published rates.13 Ergonomic knowledge among our institutions’ attending surgeons is no better, with 82% of attending surgeons reporting little to no ergonomics knowledge.21 This reflects a lack of formal ergonomics education at our institution and likely contributed to why only a minority of residents felt comfortable bringing up ergonomics in the OR prior to the workshop. Since attending surgeons are looked to as the leader of the surgical team, they have a unique opportunity to serve as advocates and role models for considering ergonomics. This OR structure highlights not only the need to raise awareness among trainees but also to provide ergonomics education to faculty.
While few general surgery residencies have formal surgical ergonomics programs, those who do have implemented various education strategies. Duke University offers a senior resident–led peer-based coaching system for the junior residents teaching appropriate posture and positioning.22 At the University of Iowa, Jensen et al. instituted didactic training sessions, which they showed to increase awareness of ergonomic principles for all residents. Following their didactic sessions, the residents in Jensen et al.’s study reported the desire to learn specific exercises to prevent and treat symptoms in future sessions.9 Our study showed that a didactic session, followed by personalized coaching sessions for residents, improves ergonomics awareness and MSK symptoms. Of the residents who participated, 82% reported an improvement in their symptom severity or frequency, with a significant reduction in maximal pain severity. Most strikingly, there was a significant improvement in how often ergonomics was discussed in the OR. This was likely due to including faculty in our didactic session, thus allowing for an open dialogue between attendings and residents regarding ergonomics while operating. Improvements remained consistent regardless of height, gender, or training year, suggesting that an ergonomics workshop is beneficial to all surgical residents.
Limitations
While this study shows clear support for incorporation of a formalized surgical ergonomics program for surgical residencies nationwide, it is not without limitations. First, this was a single institution study, and therefore our results may not be generalizable to other residents and institutions. Second, given the small sample sizes of our study, it is difficult to adjust for confounders and ascertain which resident demographic factors are independently associated with different MSK symptoms. Furthermore, our survey could not adjust for any pre-existing injuries or medical problem and handedness, which both could be confounders in this study. However, our study suggests that the prevalence of MSK symptoms in surgical residents is high and that larger multi-institutional studies may be informative. Third, research residents, who are protected from any clinical responsibilities, were included in this study and grouped with clinical PGY4–5 residents, to comprise the “senior residents”. Therefore, the impact of including research residents on the pre-ergonomics and/or postergonomics workshop surveys could not be assessed. Finally, our results are limited by potential respondent bias such as nonresponse bias, acquiescence bias, and recall bias. Regardless of these limitations, our study had high response rates to both surveys and showed that surgical residents are uniformly experiencing some degree of work-related MSK symptoms.
Further studies are needed
Our study shows resident knowledge about appropriate surgical ergonomics recommendations is minimal, although awareness and symptoms can be improved by the implementation of a didactic session with personalized coaching. Further studies are needed to characterize the prevalence of MSK symptoms and ergonomics knowledge among surgical residents and faculty nationally. Certain surgical subspecialties may be at a higher risk for certain MSK symptoms compared to others. There is additional need to include a control group to better analyze the impact of operating on the prevalence of MSK symptoms in surgical residents, of which surgical residents in their research years or internal medicine residents may be of use. The wide scale implementation of surgical ergonomic programs, educational resources, and expert coaching should be the topic of additional research. At our institution, this workshop has been incorporated into the annual residency curriculum; however, further quality improvement efforts will be needed to ensure consistent implementation of surgical ergonomics in the OR by residents and attendings. Furthermore, our institution held a similar grand rounds lecture for all OR personnel (circulating nurses, scrub technicians, etc.). However, the impact of this additional lecture was not formally assessed and will be a component of future research in surgical ergonomics.
Conclusions
Work-related MSK symptoms are extremely common among general surgery residents, with symptoms being more common in females and short (<5′4″) residents. Didactic teaching, in the form of a grand rounds lecture, and personalized posture coaching are effective in improving knowledge of ergonomic practices and reducing MSK symptom severity and frequency. Surgical residencies should consider implementing similar interventions to improve resident wellbeing and encourage residents to develop good ergonomic practices to prevent future injury.
Supplementary Material
Acknowledgments
The authors would like to thank Dr. Monia Rho for leading the Grand Rounds Ergonomics Workshop and other faculty and fellows of the Shirley Ryan Ability Lab for providing personalized posture coaching. The authors would also like to thank all general surgery residents who participated in the study.
Disclosure
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Footnotes
Supplementary Materials
Supplementary data to this article can be found online at https://doi.org/10.1016/j.jss.2022.06.014.
REFERENCES
- 1.Park A, Lee G, Seagull FJ, Meenaghan N, Dexter D. Patients benefit while surgeons suffer: an impending epidemic. J Am Coll Surg. 2010;210:306–313. [DOI] [PubMed] [Google Scholar]
- 2.Soueid A, Oudit D, Thiagarajah S, Laitung G. The pain of surgery: pain experienced by surgeons while operating. Int J Surg. 2010;8:118–120. [DOI] [PubMed] [Google Scholar]
- 3.Alleblas CCJ, de Man AM, van den Haak L, Vierhout ME, Jansen FW, Nieboer TE. Prevalence of musculoskeletal disorders among surgeons performing minimally invasive surgery: a systematic review. Ann Surg. 2017;266:905–920. [DOI] [PubMed] [Google Scholar]
- 4.Epstein S, Sparer EH, Tran BN, et al. Prevalence of work-related musculoskeletal disorders among surgeons and interventionalists: a systematic review and meta-analysis. JAMA Surg. 2018;153:e174947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hallbeck MS, Lowndes BR, Bingener J, et al. The impact of intraoperative microbreaks with exercises on surgeons: a multi-center cohort study. Appl Ergon. 2017;60:334–341. [DOI] [PubMed] [Google Scholar]
- 6.Stucky CH, Cromwell KD, Voss RK, et al. Surgeon symptoms, strain, and selections: systematic review and meta-analysis of surgical ergonomics. Ann Med Surg (Lond). 2018;27:1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Merriam Webster Online Dictionary. Copyright 2022. Available at: https://www.merriam-webster.com/ Accessed March 1, 2022.
- 8.Koshy K, Syed H, Luckiewicz A, Alsoof D, Koshy G, Harry L. Interventions to improve ergonomics in the operating theatre: a systematic review of ergonomics training and intra-operative microbreaks. Ann Med Surg. 2020;55:135–142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Jensen MJ, Liao J, Van Gorp B, et al. Incorporating surgical ergonomics education into surgical residency curriculum. J Surg Educ. 2021;78:1209–1215. [DOI] [PubMed] [Google Scholar]
- 10.Wauben LS, van Veelen MA, Gossot D, Goossens RH. Application of ergonomic guidelines during minimally invasive surgery: a questionnaire survey of 284 surgeons. Surg Endosc. 2006;20:1268–1274. [DOI] [PubMed] [Google Scholar]
- 11.Franasiak J, Craven R, Mosaly P, Gehrig PA. Feasibility and acceptance of a robotic surgery ergonomic training program. JSLS. 2014;18. e2014.00166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Aaron KA, Vaughan J, Gupta R, et al. The risk of ergonomic injury across surgical specialties. PLoS One. 2021;16:e0244868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Epstein S, Tran BN, Capone AC, et al. The current state of surgical ergonomics education in U.S. surgical training: a survey study. Ann Surg. 2019;269:778–784. [DOI] [PubMed] [Google Scholar]
- 14.McQuivey KS, Deckey DG, Christopher ZK, et al. Surgical ergonomics and musculoskeletal pain in orthopaedic surgery residents: a multicenter survey study. J Am Acad Orthop Surg Glob Res Rev. 2021;5:e20.00119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kokosis G, Dellon LA, Lidsky ME, Hollenbeck ST, Lee BT, Coon D. Prevalence of musculoskeletal symptoms and ergonomics among plastic surgery residents: results of a national survey and analysis of contributing factors. Ann Plast Surg. 2020;85:310–315. [DOI] [PubMed] [Google Scholar]
- 16.Wong K, Grundfast KM, Levi JR. Assessing work-related musculoskeletal symptoms among otolaryngology residents. Am J Otolaryngol. 2017;38:213–217. [DOI] [PubMed] [Google Scholar]
- 17.Maslach C, Jackson SE. The measurement of experienced burnout. J Organ Behav. 1981;2:99–113. [Google Scholar]
- 18.Fairbank JC, Couper J, Davies JB, O’Brien JP. The oswestry low back pain disability questionnaire. Physiotherapy. 1980;66:271–273. [PubMed] [Google Scholar]
- 19.Fisher SM, Teven CM, Song DH. Ergonomics in the operating room: the cervicospinal health of today’s surgeons. Plast Reconstr Surg. 2018;142:1380–1387. [DOI] [PubMed] [Google Scholar]
- 20.Sutton E, Irvin M, Zeigler C, Lee G, Park A. The ergonomics of women in surgery. Surg Endosc. 2014;28:1051–1055. [DOI] [PubMed] [Google Scholar]
- 21.Cerier EJ, Mills S, Hu A, Kulkarni S. Preventing surgeon injury by implementing surgical ergonomics in the operating room. J Am Coll Surg. 2020;231(Suppl 2):e198–e199. [Google Scholar]
- 22.Walker B Duke surgery introduces ergonomics program to improve surgeon health. Durham, NC: Duke University School of Medicine; 2017. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


