Abstract
Background:
Immediate postoperative pain relief following arthroscopic partial meniscectomy remains a critical contributor to improved patient experience, early recovery of range of motion, and enhanced rehabilitation.
Purpose:
To evaluate the effect of intra-articular versus extra-articular bupivacaine on pain intensity and analgesic intake after arthroscopic partial meniscectomy.
Study Design:
Randomized controlled trial; Level of evidence, 1.
Methods:
This was a prospective double-blind, randomized clinical trial. All patients included underwent arthroscopic partial meniscectomy under general anesthesia. Patients were randomized into 2 groups, with 20 patients in each group. At the conclusion of the arthroscopic procedure, the intra-articular group received 10 mL 0.5% bupivacaine introduced intra-articularly and 10 mL isotonic saline 0.9% infiltrated subcutaneously around the portals. The extra-articular group received the isotonic saline intra-articularly and the bupivacaine around the portals. The primary outcome was the visual analog scale (VAS) for pain. Assessments were performed 0 to 0.5, 1 to 2, 2 to 4, and at 24 and 48 hours postoperatively. In addition, analgesic and narcotic consumption was monitored.
Results:
There were no differences between the groups in terms of patient demographics. VAS scores for the intra-articular group were 6, 8, 3.25, 4.3, and 4.5 at 0 to 0.5, 1 to 2, 2 to 4, 24, and 48 hours postoperatively, respectively. VAS scores for the extra-articular group were 3.8, 5, 2.9, 5.2, and 5.25, respectively. No statistically significant differences were observed between the 2 groups regarding pain intensity at all time points. There was also no statistically significant difference in analgesic consumption. Dipyrone was the preferred drug by patients from the intra-articular group, while the extra-articular group preferred to use opioids and nonsteroidal anti-inflammatory drugs.
Conclusion:
There were no differences in pain severity and analgesic intake between intra- or extra-articular bupivacaine administration after arthroscopic partial meniscectomy.
Keywords: arthroscopy, bupivacaine, extra-articular, intra-articular, local anesthesia, meniscectomy
Approximately two-thirds of patients undergoing knee arthroscopy have pain after the procedure.3,4 While pain mechanisms are complex and multifactorial, evidence suggests postoperative pain stems from peripheral sensitization of afferent nociceptive neurons, as well as central sensitization of spinal neurons upon the surgical trauma. 6 Postoperative pain can also cause various indirect complications and can lead to increased hospitalization duration, resulting in increased cost of treatment.11,29
Optimal pain control and relief is necessary to achieve recovery of the knee range of motion, function, and effective postoperative rehabilitation.5,6 Postoperative pain relief methods include regional nerve blocks, continuous epidural analgesia, and patient controlled oral analgesia.2,19,24,31 Preemptive direct application of local anesthetics can also provide analgesia through several mechanisms, such as blocking transmission of pain from nociceptive afferents from the wound surface, inhibition of local inflammatory responses to the injury, reduction in the formation of free oxygen radicals, and reduction of local edema.15,18
The administration of various local anesthetic drugs into the joint space, either by a single injection or by a continuous infusion, to ameliorate postoperative pain following knee arthroscopy had been investigated, with some studies showing a beneficial effect while other studies did not.26,30,34
Bupivacaine is commonly used for intra-articular analgesia because of its extended duration of action. The peak plasma concentrations of the drug upon intra-articular injection were found to be low, rendering systemic toxicity extremely unlikely. 33 However, there is evidence demonstrating that bupivacaine could induce a process of cartilage breakdown–-chondrolysis. 33 Moreover, several studies have demonstrated a link between chondrocyte damage and the development of osteoarthritis. 17 Nevertheless, it should be taken into consideration that it may take several years between the insult to the cartilage and the onset of the osteoarthritis. 17 In addition, there is some risk in the intra-articular injection itself since it involves not only the soft tissues of the knee but also the posterior capsule of the knee.
An additional method to relief postoperative pain following knee arthroscopy is the extra-articular/periarticular administration of anesthetics. The conventional periarticular method usually contains antalgic agents, nonsteroidal anti-inflammatory drugs (NSAIDS), steroid hormones, and local anesthetics of amide derivative bupivacaine. 20 Although this technique has been extensively studied in patients who underwent knee arthroplasty, there is a lack of data regarding its affects in knee arthroscopy. Previous researchers have demonstrated that the use of different anesthetic agents’ mixtures (such as ketorolac, ropivacaine, bupivacaine, morphine sulfate, epimorphine, methylprednisolone, cefuroxime, and epinephrine) by extra-articular infiltration induces a beneficial effect on postoperative pain relief as well as on functional recovery after surgery. 25
The potential damage to the articular cartilage by using intra-articular analgesia in knee arthroscopy raises concern. This, in addition to the absence of information about the use of extra-articular analgesia after knee arthroscopy, emphasizes the need to investigate the effect of an extra-articular drug injection compared with an intra-articular injection on pain relief after knee arthroscopy. The purpose of this study was to evaluate the effect of intra-articular bupivacaine in comparison with extra-articular bupivacaine administration on pain intensity and analgesic intake after arthroscopic partial meniscectomy. We hypothesized that there would be no differences in terms of postoperative pain and analgesia intake between the groups.
Methods
Study Design
The study was a prospective double-blind, randomized, controlled clinical trial. The study protocol was approved by the institutional review board. Inclusion criteria were the following: patients undergoing knee arthroscopy of the knee with partial meniscectomy due to a meniscal tear under general anesthesia, American Society of Anesthesiologists physical status of I to II, and age >18 years. Patients with a history of adverse reactions or allergy to the medication used in the study, radiological evidence of osteoarthritis, chondral and ligamentous injuries, concomitant procedures with weightbearing limitations, and patients who did not want to participate or sign an informed consent form were excluded from the study. Patients who underwent meniscal repair were also excluded. Written informed consent was obtained on the day of surgery, after the patients had read the information and had a thorough discussion with their surgeon regarding study participation and potential risks and benefits. Between 2014 and 2019, a total of 40 patients were enrolled.
Patients were randomized into 2 groups without stratification (n = 20 patients in each group). At the conclusion of the knee arthroscopy, patients in group 1 received 10 mL 0.5% bupivacaine introduced intra-articularly and 10 mL isotonic saline 0.9% infiltrated subcutaneously around the portals (intra-articular group). Patients in group 2 received 10 mL intra-articular isotonic saline 0.9% and 10 mL 0.5% bupivacaine infiltrated subcutaneously around the portals (extra-articular group). Randomization was performed by a blinded research assistant who randomly picked a closed opaque envelope containing a treatment regimen on the day of each surgery. The allocated sealed envelope was opened at the operating room by a nonblinded circulating operating room nurse.
Knee arthroscopy was performed under a standard general anesthetic protocol during the procedure. Intravenous 200 µg fentanyl and 1 g paracetamol was administered by the anesthesiologist. No additional long-acting analgesic agents or regional nerve blocks were administered. A nonsterile pneumatic thigh tourniquet was used at a pressure of 300 mmHg. Knee arthroscopy was performed in a standard fashion using anterolateral and anteromedial parapatellar portals by a group of fellowship-trained sports medicine orthopaedic surgeons. On completion of anesthesia, patients were transferred to the postanesthesia care unit.
The standard “pain-contingent” postoperative pain control protocol was as follows:
visual analog scale (VAS) 1 to 3: oral dipyrone 1 g (Optalgin; Teva Pharmaceutical Industries), oral ibuprofen 400 mg, or oral codeine phosphate 15 mg/paracetamol 500 mg/caffeine 50 mg (Rokacet Plus; Taro Pharmaceutical Industries)
VAS 4 to 6: oral oxycodone 10 mg, intramuscular diclofenac 75 mg, or 2 caplets of oral codeine phosphate 15 mg/paracetamol 500 mg/caffeine 50 mg (Rokacet Plus)
VAS 7 to 10: oral oxycodone/paracetamol 2 tablets (Percocet; Endo Pharmaceuticals) 5 mg or intramuscular/intravenous tramadol 100 mg plus metoclopramide 10 mg.
After a VAS assessment, the patient was offered analgesic medications from the protocol. The patients would then decide whether to take the analgesic according to their need for pain alleviation.
The primary outcome measure was the VAS for pain, using a 10-cm linear scale where 0 represented no pain and 10 the most severe pain. This scale is used commonly in clinical orthopaedic practice and is a reliable and valid outcome measure for pain. The VAS monitoring was conducted by a blinded member of the recovery staff in the postanesthesia care unit.
Assessments were performed at 0 to 0.5, 1 to 2, 2 to 4, and at 24 and 48 hours postoperatively. Patients were discharged on the same day once they were oriented to time and place, had stable vital signs, had minimal or no pain, with no experience of nausea, vomiting, or other side effects, and were ambulating with or without the assistance of crutches. In addition, pain levels were followed via a telephone call at 24 and 48 hours postoperatively. Use of additional analgesia and narcotic intake was also recorded. Assessments were performed by nurses in the postanesthesia care unit and by research assistants once the patients left the recovery area and were discharged. All assessors were blinded to the patients’ allocation to treatment groups.
Statistical Analysis
Sample size power analysis calculation for this study was based on VAS for pain. A clinically relevant difference between the treatment groups was defined as 1 point. With an assumed SD of 2 points and a P value of .05, 20 patients in each group were required to obtain a power of 80%.7,9,10,22,23 Analysis was performed with PASW SPSS 24.0 software (IBM Corp). Normality of the data was checked using the Kolmogorov-Smirnov tests. For parametric statistics, t test or analysis of variance test was used. Nonparametric Mann-Whitney or Kruskal-Wallis test was used only if parametric assumptions could not be satisfied. In the case of a nominal variable, the chi-square and the Fisher exact test were used. Data were summarized using frequency tables, summary statistics, confidence intervals, and P values. Statistical significance was determined at a P value of <.05.
Results
Patient Characteristics
All 40 patients completed the study; there were no dropouts or patients lost to follow-up. There were no significant differences between the intra-articular and extra-articular bupivacaine groups regarding patient demographics (Table 1).
Table 1.
Comparison of Demographic and Clinical Characteristics Between Study Groups a
| All Patients (N = 40) |
Intra-articular (n = 20) |
Extra-articular (n = 20) |
P | |
|---|---|---|---|---|
| Age at surgery, y, mean ± SD (range) | 45 ± 14.4 (19-74) | 45.05 ± 14.7 (19-66) | 44.95 ± 14.5 (21-74) | .983 |
| Sex | .339 | |||
| Male | 25 (62.5) | 11 (55) | 14 (70) | |
| Female | 15 (37.5) | 9 (45) | 6 (30) | |
| Body mass index | 26.5 ± 5.2 | 26.8 ± 4.7 | 26.3 ± 5.9 | .855 |
| Laterality | .349 | |||
| Right | 23 (57.5) | 13 (65) | 10 (50) | |
| Left | 17 (42.5) | 7 (35) | 10 (50) | |
| Procedure | ||||
| Medial meniscectomy | 22 (55) | 11 (55) | 11 (55) | >.999 |
| Lateral meniscectomy | 10 (25) | 4 (20) | 6 (30) | .474 |
| Medial and lateral meniscectomy | 8 (20) | 5 (25) | 3 (15) | .439 |
a Data are reported as mean ± SD or n (%) unless otherwise indicated.
There were no significant differences between the 2 groups in terms of pain intensity as assessed by VAS at all time points (Table 2 and Figure 1). The pain level increased in both groups during the first 2 hours after surgery. At 0 to 30 minutes after the operation the VAS score was 6, increasing to 8 at 1 to 2 hours postsurgery in the group that had an intra-articular treatment, whereas in the extra-articular group the VAS score was 3.8 at 0 to 30 minutes after the operation, increasing to 5 at 1 to 2 hours postoperatively. At 2 to 4 hours after surgery the pain level decreased in both groups. The pain intensity recorded 24 hours and 48 hours after the operation rose compared with that reported 2 to 4 hours postoperatively and remained stable.
Table 2.
Comparison of VAS Pain Scores Between Groups by Postoperative Time Point a
| VAS Pain Score | ||||
|---|---|---|---|---|
| Postoperative Time Point | Mean ± SD | Range | 95% CI | P |
| 0-30 minutes | .3443 | |||
| Intra-articular | 6.000 ± 2.828 | 0.0-10.0 | 3.64 to 8.36 | |
| Extra-articular | 3.750 ± 3.500 | 0.0-8.0 | -1.82 to 9.32 | |
| 1-2 hours | >.9999 | |||
| Intra-articular | 8.000 ± 1.414 | 7.0-9.0 | -4.71 to 20.71 | |
| Extra-articular | 5.000 ± 7.071 | 0.0-10.0 | -58.53 to 68.53 | |
| 2-4 hours | .6004 | |||
| Intra-articular | 3.250 ± 3.279 | 0.0-10.0 | 1.17 to 5.33 | |
| Extra-articular | 2.938 ± 3.415 | 0.0-10.0 | 1.12 to 4.76 | |
| 24 hours | .3339 | |||
| Intra-articular | 4.333 ± 2.267 | 0.0-7.5 | 2.81 to 5.86 | |
| Extra-articular | 5.211 ± 1.537 | 2.0-7.0 | 4.36 to 6.06 | |
| 48 hours | .4509 | |||
| Intra-articular | 4.500 ± 1.871 | 2.0-7.0 | 2.18 to 6.82 | |
| Extra-articular | 5.250 ± 1.389 | 3.0-7.0 | 4.09 to 6.41 | |
a VAS, visual analog scale (0 = no pain, 10 = most severe pain).
Figure 1.
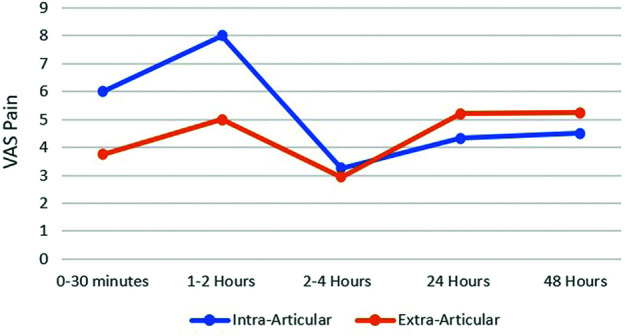
Mean visual analog scale (VAS) pain scores over time between patients in the intra-articular versus extra-articular bupivacaine groups.
Pain relief medications were consumed by 25%, 7.5%, 22.5%, 42.5%, and 22.5% of all patients at 0 to 0.5, 1 to 2, 2 to 4, and at 24 and 48 hours postoperatively, respectively. However, no significant differences between the 2 groups regarding pain relief medication consumption were observed. Data are presented in Table 3 and Figure 2.
Table 3.
Pain Relief Medication Consumption Between Groups by Postoperative Time Point a
| Postoperative Time Point | Took Medication | No Medication | P |
|---|---|---|---|
| 0-30 minutes | .160 | ||
| Intra-articular | 7 (35) | 13 (65) | |
| Extra-articular | 3 (15) | 17 (85) | |
| Total | 10 (25) | 30 (75) | |
| 1-2 hours | .555 | ||
| Intra-articular | 2 (10) | 18 (90) | |
| Extra-articular | 1 (5) | 19 (95) | |
| Total | 3 (7.5) | 37 (92.5) | |
| 2-4 hours | .709 | ||
| Intra-articular | 4 (20) | 16 (80) | |
| Extra-articular | 5 (25) | 15 (75) | |
| Total | 9 (22.5) | 31 (77.5) | |
| 24-48 hours | .126 | ||
| Intra-articular | 6 (30) | 14 (70) | |
| Extra-articular | 11 (55) | 9 (45) | |
| Total | 17 (42.5) | 23 (57.5) | |
| >48 hours | .074 | ||
| Intra-articular | 2 (10) | 18 (90) | |
| Extra-articular | 7 (35) | 13 (65) | |
| Total | 9 (22.5) | 31 (77.5) |
a Data are reported as n (%).
Figure 2.
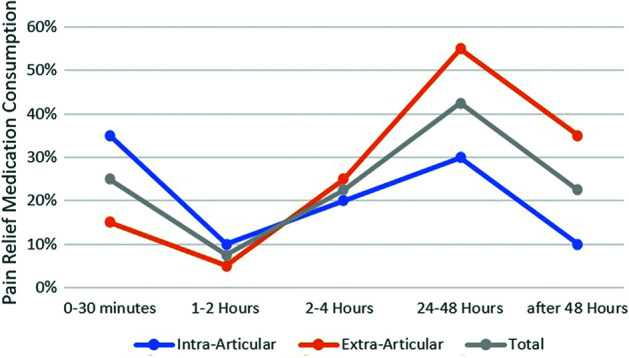
Percentage of patients who took pain relief medication at each time point, overall and by group.
The drug of choice was dipyrone, especially for patients from the intra-articular group compared with the extra-articular group. Interestingly, opioids (such as oxycodone and codeine phosphate) as well as NSAIDs (etoricoxib and ibuprofen) were preferred by patients from the extra-articular group in comparison with the intra-articular group.
Discussion
The main finding of this randomized clinical trial is that there were no differences in pain relief and analgetic medication consumption after arthroscopic partial meniscectomy between patients who were treated with intra-articular or extra-articular bupivacaine.
Literature reporting on the effect of intraoperative intra-articular administration of various local anesthetics drugs following knee arthroscopy has yielded conflicting results. Some of the published studies demonstrated that these treatments indeed reduced the requirements for postoperative pain relief medication and led to an earlier discharge from the hospital. For example, in a study that included 60 patients who underwent an arthroscopic knee surgery, intra-articular levobupivacaine combined with morphine and adrenaline or only bupivacaine decreased the postoperative duration of analgesic use and accelerated knee mobility. 26 On the other hand, some studies did not reveal any significant benefit to the different intra-articular anesthetic treatments. Solheim et al 30 compared the analgesic effect of intra-articular administration of saline or 5 mg morphine and found that there were no differences in pain intensity or pain relief at any time during the 48-hour observation period between morphine or saline. In another study, Zou et al 34 screened 28 studies involving 2564 participants to evaluate the effects on pain relief of intra-articular morphine compared with placebo. No statistical difference was found between 1 mg morphine and placebo administered intra-articularly with regard to pain intensity at 0 to 2, 2 to 6, or 30 hours after knee arthroscopy.
An important consideration when administering intra-articular injections is the potential for chondrotoxicity. Suggested mechanisms of the toxicity of local anesthetics toward the cartilage include damage to the mitochondrial DNA and mitochondrial protein synthesis. 13 Preclinical studies showed that even short-term exposure to local anesthetics led to dose- and time-dependent chondrocyte death. The traditional agents, lidocaine and bupivacaine, were more harmful than the newer agents such as mepivacaine and ropivacaine. However, these findings were not reproduced by other studies showing no influence of a traditional agent such as lidocaine on cell viability, morphology, and cultivation potential of chondrocytes. 28 Moreover, Piper et al 27 reported significant risk with continuous bupivacaine infusion but found the effects of a single injection of bupivacaine unclear. A series of 27 postarthroscopic glenohumeral chondrolysis has been published in the literature; 25 of these cases received postoperative continuous intra-articular analgesia with bupivacaine.12,16,21 A review that summarized clinical and laboratory data from 41 published studies demonstrated that bupivacaine, lidocaine, ropivacaine, and levobupivacaine were toxic to cartilage. Importantly, intra-articular infusions were found to result in a greater toxicity to cartilage than single injections. 14
Our findings are consistent with the results of another study in which pain and analgesia consumption after surgery was the same in patients who received either extra-articular or intra-articular treatment of anesthetic drugs. Townshend et al 32 randomized 137 patients who received bupivacaine introduced either intra-articularly or extra-articularly following arthroscopy. The effect on pain relief 1 hour postoperatively was slightly higher in the extra-articularly treated group versus the intra-articularly treated group but this difference was not statistically significant. However, this study assessed VAS only 1 hour following knee arthroscopy and is limited to that time period. Given the elimination half-life of bupivacaine is 3.1 hours in adults, we sought in this study to follow up with patients for a longer duration of time to fully comprehend the analgesic effect of intra- and extra-articular bupivacaine. A survey of the literature, conducted to locate studies that demonstrated the superiority of one technique over the other in patients who underwent knee arthroscopy, did not yield further contributory results. Nevertheless, there are a few studies demonstrating the superiority of one technique over the other in knee arthroplasty. For example, 50 patients who had arthrotomy surgery were divided randomly into a group that was treated with combination of intra-articular morphine and ketamine compound at the end of surgery and into a group that was treated with a combination of extra-articular morphine and ketamine compound. The pain severity 2, 4, 6, 12, and 24 hours after surgery was significantly lower among the intra-articular injection group than in the extra-articular injection group. In addition, postoperative morphine consumption in the intra-articular injection group was significantly less than in the extra-articular injection group. 1 On the other hand, Cheng et al 8 recently published data from a randomized controlled trial with patients who had simultaneous bilateral total knee arthroplasty. The patients were assigned randomly to be treated with either an extra-articular injection or with an intra-articular injection in 1 side. Cheng et al reported administering a cocktail that contained 200 mg ropivacaine, 100 µg fentanyl, 0.25 mg adrenaline, 50 mg flurbiprofen axetil, and 1 mg diprospan, diluted with normal saline. Patients who were administered an extra-articular injection had lower pain scores than patients with the knee receiving an intra-articular injection during the first 48 hours after surgery, both in rest and during activity. In addition, the extra-articular group demonstrated better results in passive and in active range of motion in the first 3 days after surgery compared with the intra-articular group. 8
Limitations
This study is not without limitations. The main limitation of the present study was the small number of patients, although a priori power analysis did confirm this sample size is adequate. We also included patients undergoing lateral, medial and lateral, and medial meniscectomies, who may differ in their postoperative pain levels. However, this randomized clinical trial still represents a very homogeneous population with strict inclusion and exclusion criteria. Furthermore, there were no significant differences between the groups in terms of patients’ demographics. Last, different analgesic medication consumption may have a variable effect on the reported VAS scores. However, all patients were given the same postoperative S.O.S. (per patient request) pain medication protocol, which is based on postoperative VAS as well as patient’s preference within the protocol limits.
Conclusion
To summarize, we believe pain management strategies are critical after knee arthroscopy and investigated 2 techniques, extra- or intra-articular administration of various analgesic drugs, to relieve pain and reduce narcotic medication consumption after the procedure. Our data demonstrated that there was no difference in pain severity and medication requirement after treatment with bupivacaine via intra- or extra-articular administration. However, previous evidence had suggested that intra-articular anesthetic injection might injure the articular cartilage and this should be a major consideration in the treatment of every patient undergoing knee arthroscopy.
Acknowledgment
The authors acknowledge Carni Barak for her dedication and hard work in coordinating this randomized clinical trial.
Footnotes
Final revision submitted October 1, 2022; accepted October 11, 2022.
The authors declared that there are no conflicts of interest in the authorship and publication of this contribution. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval for this study was obtained from Shamir Medical Center (ref No. 9/14).
References
- 1.Akhondzade R, Pipelzade MR, Gousheh MR, Sarrafan N, Mahmoodi K. Comparison of the analgesic effect of intra-articular and extra-articular injection of morphine and ketamine compound in arthrotomy lower limb surgery under spinal anesthesia. Pak J Med Sci. 2014;30(5):942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Allen GC, St. Amand MA, Lui AC, Johnson DH, Lindsay MP. Postarthroscopy analgesia with intraarticular bupivacaine/morphine: a randomized clinical trial. J Am Soc Anesthesiol. 1993;79(3):475–480. [DOI] [PubMed] [Google Scholar]
- 3.Beattie WS, Warriner CB, Etches R, et al. The addition of continuous intravenous infusion of ketorolac to a patient-controlled analgetic morphine regime reduced postoperative myocardial ischemia in patients undergoing elective total hip or knee arthroplasty. Anesth Analg. 1997;84(4):715–722. [DOI] [PubMed] [Google Scholar]
- 4.Bonica JJ. Management of pain with regional analgesia. Postgrad Med J. 1984;60(710):897–904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Browne C, Copp S, Reden L, Pulido P, Colwell C, Jr. Bupivacaine bolus injection versus placebo for pain management following total knee arthroplasty. J Arthroplasty. 2004;19(3):377–380. [DOI] [PubMed] [Google Scholar]
- 6.Busch CA, Shore BJ, Bhandari R, et al. Efficacy of periarticular multimodal drug injection in total knee arthroplasty: a randomized trial. J Bone Joint Surg Am. 2006;88(5):959–963. [DOI] [PubMed] [Google Scholar]
- 7.Calmet J, Esteve C, Boada S, Gine J. Analgesic effect of intra-articular ketorolac in knee arthroscopy: comparison of morphine and bupivacaine. Knee Surg Sports Traumatol Arthrosc. 2004;12(6):552–555. [DOI] [PubMed] [Google Scholar]
- 8.Cheng K-Y, Feng B, Peng H-M, et al. The analgesic efficacy and safety of peri-articular injection versus intra-articular injection in one-stage bilateral total knee arthroplasty: a randomized controlled trial. BMC Anesthesiology. 2020;20(1):2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Dal D, Tetik O, Altunkaya H, Tetik Ö, Doral MN. The efficacy of intra-articular ketamine for postoperative analgesia in outpatient arthroscopic surgery. Arthroscopy. 2004;20(3):300–305. [DOI] [PubMed] [Google Scholar]
- 10.Eroglu A, Saracoglu S, Erturk E, Kosucu M, Kerimoglu S. A comparison of intraarticular morphine and bupivacaine for pain control and outpatient status after an arthroscopic knee surgery under a low dose of spinal anaesthesia. Knee Surg Sports Traumatol Arthrosc. 2010;18(11):1487–1495. [DOI] [PubMed] [Google Scholar]
- 11.Ferasatkish R, Dabbagh A, Alavi M, et al. Effect of magnesium sulfate on extubation time and acute pain in coronary artery bypass surgery. Acta Anaesthesiol Scand. 2008;52(10):1348–1352. [DOI] [PubMed] [Google Scholar]
- 12.Greis PE, LeGrand A, Burks RT. Bilateral shoulder chondrolysis following arthroscopy: a report of two cases. J Bone Joint Surg Am. 2008;90(6):1338–1344. [DOI] [PubMed] [Google Scholar]
- 13.Grishko V, Xu M, Wilson G, Pearsall AW IV. Apoptosis and mitochondrial dysfunction in human chondrocytes following exposure to lidocaine, bupivacaine, and ropivacaine. J Bone Joint Surg Am. 2010;92(3):609–618. [DOI] [PubMed] [Google Scholar]
- 14.Gulihar A, Robati S, Twaij H, Salih A, Taylor GJ. Articular cartilage and local anaesthetic: a systematic review of the current literature. J Orthop. 2015;12:S200–S210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hahnenkamp K, Theilmeier G, Van Aken HK, Hoenemann CW. The effects of local anesthetics on perioperative coagulation, inflammation, and microcirculation. Anesth Analg. 2002;94(6):1441–1447. [DOI] [PubMed] [Google Scholar]
- 16.Hansen BP, Beck CL, Beck EP, Townsley RW. Postarthroscopic glenohumeral chondrolysis. Am J Sports Med. 2007;35(10):1628–1634. [DOI] [PubMed] [Google Scholar]
- 17.Hashimoto S, Ochs RL, Komiya S, Lotz M. Linkage of chondrocyte apoptosis and cartilage degradation in human osteoarthritis. Arthritis Rheum. 1998;41(9):1632–1638. [DOI] [PubMed] [Google Scholar]
- 18.Hollmann MW, Durieux ME, Fisher DM. Local anesthetics and the inflammatory response: a new therapeutic indication? J Am Soc Anesthesiol. 2000;93(3):858–875. [DOI] [PubMed] [Google Scholar]
- 19.Klasen J, Opitz S, Melzer C, Thiel A, Hempelmann G. Intraarticular, epidural, and intravenous analgesia after total knee arthroplasty. Acta Anaesthesiol Scand. 1999;43(10):1021–1026. [DOI] [PubMed] [Google Scholar]
- 20.Kuang M-J, Du Y, Ma J-X, et al. The efficacy of liposomal bupivacaine using periarticular injection in total knee arthroplasty: a systematic review and meta-analysis. J Arthroplasty. 2017;32(4):1395–1402. [DOI] [PubMed] [Google Scholar]
- 21.Levy JC, Virani NA, Frankle MA, et al. Young patients with shoulder chondrolysis following arthroscopic shoulder surgery treated with total shoulder arthroplasty. J Shoulder Elbow Surg. 2008;17(3):380–388. [DOI] [PubMed] [Google Scholar]
- 22.Marret E, Gentili M, Bonnet MP, Bonnet F. Intra-articular ropivacaine 0.75% and bupivacaine 0.50% for analgesia after arthroscopic knee surgery: a randomized prospective study. Arthroscopy. 2005;21(3):313–316. [DOI] [PubMed] [Google Scholar]
- 23.Milligan K, Mowbray M, Mulrooney L, Standen P. Intra-articular bupivacaine for pain relief after arthroscopic surgery of the knee joint in daycase patients. Anaesthesia. 1988;43(7):563–564. [DOI] [PubMed] [Google Scholar]
- 24.Mulroy MF, Larkin KL, Batra MS, Hodgson PS, Owens BD. Femoral nerve block with 0.25% or 0.5% bupivacaine improves postoperative analgesia following outpatient arthroscopic anterior cruciate ligament repair. Reg Anesth Pain Med. 2001;26(1):24–29. [DOI] [PubMed] [Google Scholar]
- 25.Nair VS, Radhamony NG, Rajendra R, Mishra R. Effectiveness of intraoperative periarticular cocktail injection for pain control and knee motion recovery after total knee replacement. Arthroplast Today. 2019;5(3):320–324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ozdemir N, Kaya FN, Gurbet A, et al. Comparison of intraarticular bupivacaine and levobupivacaine with morphine and epinephrine for knee arthroscopy. Eurasian J Med. 2013;45(2):77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Piper SL, Kramer JD, Kim HT, Feeley BT. Effects of local anesthetics on articular cartilage. Am J Sports Med. 2011;39(10):2245–2253. [DOI] [PubMed] [Google Scholar]
- 28.Ravnihar K, Barlič A, Drobnič M. Effect of intra-articular local anesthesia on articular cartilage in the knee. Arthroscopy. 2014;30(5):607–612. [DOI] [PubMed] [Google Scholar]
- 29.Schouten JW. Neuroprotection in traumatic brain injury: a complex struggle against the biology of nature. Curr Opin Crit Care. 2007;13(2):134–142. [DOI] [PubMed] [Google Scholar]
- 30.Solheim N, Rosseland LA, Stubhaug A. Intra-articular morphine 5 mg after knee arthroscopy does not produce significant pain relief when administered to patients with moderate to severe pain via an intra-articular catheter. Reg Anesth Pain Med. 2006;31(6):506–513. [DOI] [PubMed] [Google Scholar]
- 31.Tetzlaff JE, Andrish J, O’Hara J, Jr, Dilger J, Yoon HJ. Effectiveness of bupivacaine administered via femoral nerve catheter for pain control after anterior cruciate ligament repair. J Clin Anesth. 1997;9(7):542–545. [DOI] [PubMed] [Google Scholar]
- 32.Townshend D, Emmerson K, Jones S, Partington P, Muller S. Intra-articular injection versus portal infiltration of 0.5% bupivacaine following arthroscopy of the knee: a prospective, randomised double-blinded trial. J Bone Joint Surg Br. 2009;91(5):601–603. [DOI] [PubMed] [Google Scholar]
- 33.Webb ST, Ghosh S. Intra-articular bupivacaine: potentially chondrotoxic? Br J Anaesth. 2009;102(4):439–441. [DOI] [PubMed] [Google Scholar]
- 34.Zou Z, An MM, Xie Q, et al. Single dose intra-articular morphine for pain control after knee arthroscopy. Cochrane Database Syst Rev. 2016;5:CD008918. [DOI] [PMC free article] [PubMed] [Google Scholar]


