Abstract
Background:
Patients experiencing homelessness have higher rates of substance use and related mortality, often driven by opioid overdose. Conversely, opioid use disorder (OUD) is a leading risk factor for homelessness. Our goal was to test the efficacy of an electronic health record (EHR) screen in identifying this vulnerable population during hospitalization and to assess the feasibility of a bundled intervention in improving opioid safety.
Methods:
We assessed patients’ housing status, substance use, previous MOUD treatment, barriers to MOUD treatment and readiness to take MOUD in and out of the hospital. For each post discharge follow up call, patients were asked about their MOUD status, barriers accessing treatment, current substance use, and housing status. We also assessed team members perceptions and experiences of the study.
Results:
We enrolled 32 patients with housing insecurity and OUD. The mean age was 44, the majority self-identified as male (78%), and mostly as White (56%) or Black (38%). At each follow up within the 6-months post-discharge, reach rates were low: 40% of enrollees answered at least 1 call and the highest reach rate (31% of patients) occurred at week 4. At the third and sixth-month follow ups, >50% of subjects still taking MOUD were also using opioids.
Conclusion:
Our clinician augmented EHR screen accurately identified inpatients experiencing OUD and PEH. This intervention showed high rates of attrition among enrolled patients, even after providing cellphones. The majority of patients who were reached remained adherent to MOUD though they reported significant barriers.
Keywords: opioid use disorder, medication for opioid use disorder, bundled intervention, OUD, MOUD
Background
Patients experiencing homelessness with concurrent substance use disorders are among the most vulnerable people treated by clinicians. Deaths from the opioid epidemic have accelerated in recent years. Since April 2021, U.S. accidental drug overdose deaths topped 100 000 for the preceding 12-month period. 1 In San Francisco, concurrent with the COVID-19 pandemic, there was a record number of opioid-related overdose deaths in 2020. 2 Specifically, while COVID-related deaths in San Francisco through 2021 totaled 693, drug overdose deaths were nearly double at 1347. Of all overdose deaths, 27% (in 2020) and 23% (in 2021) occurred in persons without a fixed address. 3
People experiencing homelessness (PEH) demonstrate higher rates of substance use, related mortality, and comorbid diseases, with opioid use also contributing to homelessness.4,5 Patients experiencing homelessness face significant barriers accessing care and following treatment recommendations for OUD. 6 These barriers often include lack of financial resources, lack of stable housing, stigma, racism, comorbid medical conditions, mistrust, and abstinence-only based housing services.7-10 PEH are often discharged from the hospital during the waiting period for residential substance use treatment, presenting a treatment gap that poses high risk for adverse events, including overdoses and readmissions. 6 Bundled interventions that combine medications for OUD (MOUD) such as buprenorphine and follow up services such as counseling, educational groups, or connections to housing have shown to increase adherence to buprenorphine.11,12 Additionally, some of the most important factors for improving treatment retention are housing assistance, consistent access to a telephone, and mental health services. 13
Hospitalizations for patients with PEH and OUD present a unique opportunity to optimize treatment. However, identification of these patients is key. Our study team recognized a lack of standardized inpatient processes to identify PEH using the electronic health record (EHR) and admission screening. Additionally, typical of US healthcare, our system of care does not provide comprehensive, wrap-around psycho-social services for patients who need them at hospital discharge. Thus, our team sought to implement some more feasible practices for PEH with OUD with the goal of reducing opioid-related harms. Our study had 2 main objectives to assess the feasibility of a focused intervention implemented within the current structure of our health system. First, we developed, tested, and explored automated EHR screens to identify hospitalized PEH with OUD with a goal of initiating MOUD following screening and referral to inpatient addiction clinicians and social work. Second, we sought to determine the feasibility and acceptability of a bundled intervention to improve opioid safety among PEH, comprised of integrated behavioral treatment and MOUD, with streamlined connection to ongoing outpatient MOUD treatment and 6 months of telephone follow-up from our study team. To determine the acceptability of the bundled intervention within clinical workflows, we qualitatively measured intervention satisfaction among clinicians and study staff.
Methods
Study population and data sources
We identified all hospitalized adults (aged ⩾18 years) from November 2020 through June 2021 admitted to all services at the University of California, San Francisco (UCSF) Helen Diller Medical Center at Parnassus Heights, a 785-bed urban academic teaching hospital. Post-discharge data was collected through September 2021. All EHR data were collected from the hospital’s Epic based platform (Epic 2017, Epic Systems Corporation, Verona, Wisconsin) with additional data elements extracted from Clarity, the relational database that stores Epic inpatient data. Informed consent was obtained from all study participants and this project was approved by the UCSF Institutional Review Board. To assess feasibility of the study, we measured our ability to recruit our target population, patient retention, and adherence to the prescribed treatment protocol. We defined clinical intervention acceptability as a qualitative assessment of clinician and study personnel’s satisfaction.
Screening methods
We developed an automated search query within Epic that searched the text of medical notes for free text entries indicating potential OUD. We used this approach, as opposed to ICD-10 codes, because we wanted to broadly identify participants during hospitalization and free-text searches within notes is more sensitive (Supplemental Appendix A). For the housing insecurity screen, the EHR tool utilized address confirmation, nursing admission screening, and clinical documentation of social determinants of health by providers, over the last year. Patients identified via the OUD screening method were assessed via chart review by the study team nurse who confirmed or ruled-out housing insecurity. Those patients identified as experiencing homelessness from the housing screen were chart reviewed for markers of OUD. Functionally, this process started with an automated weekday morning email sent to the study team with potential cases. Monday’s email included any weekend admissions.
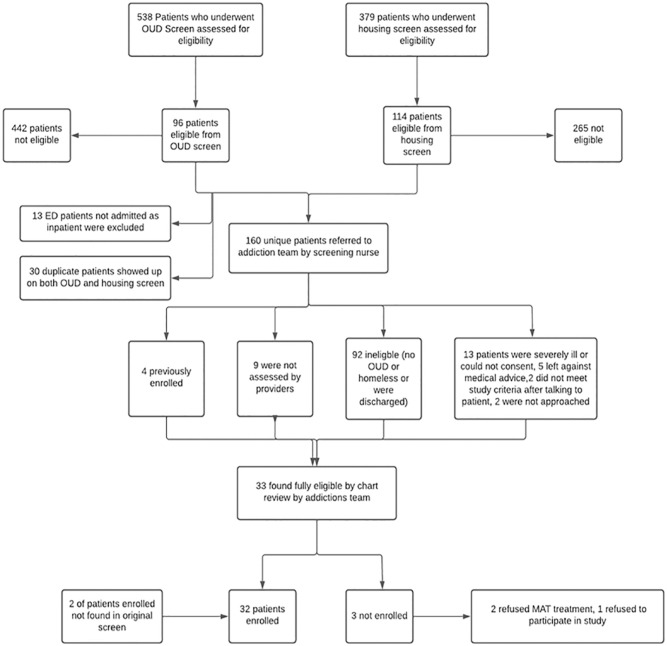
Patients identified by the screening nurse as “likely to have OUD and housing insecurity” were then assessed by an addiction specialty clinician for final confirmation of these traits which qualified for study. Identified eligible subjects were then approached for clinical evaluation and official study enrollment including initiation of MOUD treatment or optimization of already in-place MOUD treatment. Patients were subsequently enrolled by our research analyst and evaluated clinically by the addiction clinician (Figure 1). Patients who did not meet the OUD or housing screen, were in the emergency department, or who were already on MOUD treatment were excluded.
Figure 1.
Screening procedures for OUD and PEH screenings All individuals ⩾18 years of age who were admitted to the University of California, San Francisco (UCSF) Helen Diller Medical Center between November 2012 and December June 2021, were included in the source population. We excluded those who did not meet the criteria for OUD and PEH.
Bundled intervention
Once a patient was deemed eligible, they were consented by the research analyst for study participation and an intake questionnaire was conducted via video or phone call (due to COVID-19 restrictions) or in person by an addiction clinician. A licensed clinical social worker (LCSW) subsequently performed a brief psychosocial intervention (Supplemental Appendix B) and provided the patient with resources for outpatient connections. The psychosocial intervention focused on assessing current opioid use, including negative consequences and readiness for treatment, and exploring a plan to quit. Each participant was given a pre-paid cell phone that was activated for up to 6 months of follow-up and provided a nominal incentive gift card. Our institution has existing relationships with 2 residential drug treatment facilities to refer patients for ongoing MOUD management and a network of outpatient clinics for continuity of MOUD. Prior to discharge, a social worker provided a warm handoff to the identified outpatient facility, however, with limited availability and COVID restrictions, referring patients to residential facilities was not always possible. Our research analyst performed follow-up phone call questionnaires to track changes from the initial intake questionnaire at 2, 4, and 6 weeks, 3 and 6 months after discharge and provided a second gift card after final follow-up. Patients were reached at the provided cell phone, and phone calls were attempted up to 3 times per follow up period.
Outcomes
We collected 3 domains of data for patients who were enrolled (Figure 2). First, we obtained data relating to study feasibility including the enrollment rate (# patients approached for enrollment/number enrolled), retention rate, and MOUD adherence at each follow up call. These measures were used to analyze whether we were able to recruit our target population.
Figure 2.
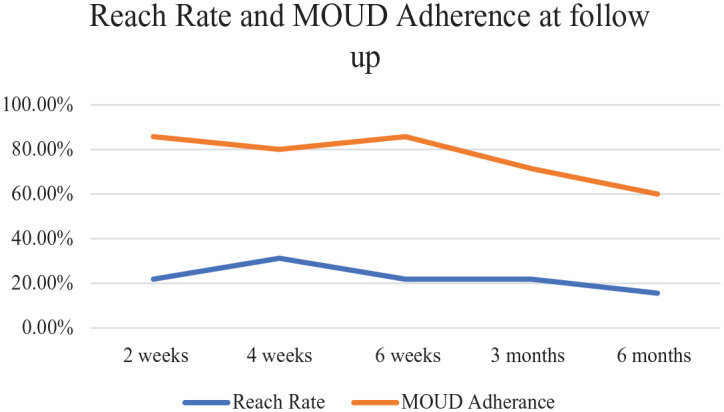
Feasibility Outcomes Feasibility outcomes, including reach rate and MOUD adherence after 6 months of follow up.
The second domain included participant responses to the intake questionnaire, including questions on current housing status, substance use, previous MOUD treatment, barriers to continued MOUD treatment, and feelings of readiness to take MOUD in and out of the hospital (Table 1). For each post discharge follow-up call, we recorded participants’ current MOUD treatment status, barriers in accessing treatment, current substance use, and housing status. We also report additional patient centered outcomes including MOUD adherence (the number of patients with self-reported adherence at a given time point/total patients on MOUD enrolled in study who answered questionnaires at each timepoint), change in housing status over the course of the study, a comparison of patients lost to follow-up versus patients who stayed in the study, 7 and 30-day readmission rates, length of stay, and utilization, defined as the total ED visits and readmissions during 6 months of follow-up, identified using our EHR at our medical system or any medical center that shared records.
Table 1.
Selected demographic and patient data from intake questionnaire of enrolled patients.
| Variable | n (%) or mean (SD) |
|---|---|
| Demographics | |
| Age (mean, SD) | 44 (14) |
| Gender | Male: 25 (78) |
| Female: 7 (22) | |
| Race/ethnicity | White: 18 (56) |
| Black: 12 (38) | |
| Other/Unknown: 2 (6) | |
| Insurance | Medicaid: 26 (81) |
| Medicare: 6 (19) | |
| Uninsured: 0 (0) | |
| Length of stay in days (mean, SD) | 10.3 (10.6) |
| Post discharge n (%) | 7-day ED visit: 1 (3) |
| 7-day readmission: 3 (9) | |
| 30-day readmission: 1 (3) | |
| Hospital service n (%) | Hospital medicine: 22 (69) |
| Cardiology: 4 (13) | |
| Surgery*: 5 (16) | |
| Malignant hematology: 1 (3) | |
| Most common discharging diagnoses n (%) | SSTI: 10 (31) |
| Osteomyelitis/discitis: 4 (13) | |
| CHF exacerbation: 4 (13) | |
| Questionnaire results | |
| Housing insecurity in the last year? Last 2 months? On admission? N = 32 | Last year: 100 |
| Last 2 months: 78.1 | |
| On admission: 68.8 | |
| Self-reported substances: | Alcohol use: 43.8 |
| Tobacco use: 84.4 | |
| Prescription drugs: 34.4 | |
| Illegal or illicit drugs: 96.9 | |
| Past month how often did you use opioids? | 1-2 monthly: 12.5 |
| Several times monthly: 0 | |
| Weekly: 6.3 | |
| Almost daily: 75 | |
| Don’t know: 6.3 | |
| Past month, how often have you had a strong desire to use opioids? | Once: 0 |
| Not often: 16.7 | |
| Sometimes: 3.3 | |
| Often: 16.7 | |
| Very often: 63.3 | |
| Past month, how often has use led to health, social, legal, or financial problems? | Once: 0 |
| Not often: 23.3 | |
| Sometimes: 20 | |
| Often: 23.3 | |
| very often: 33.3 | |
| Have you ever tried to control, cut down, or stop using opioids? | Yes: 83.9 |
| No: 16.1 | |
| Have you experienced withdrawal when you stopped opioids? | Yes: 90.6 |
| No: 9.4 | |
| Have you ever overdosed on opioids? If so, how many times? | Yes: 59.4 |
| Mean OD (SD): 3.5 (3.9) | |
| Have you ever required administration of naloxone after OD? If so, how many times? | Yes: 44 |
| Mean Naloxone (SD): 2.45 (2.1) | |
| Have you ever taken methadone or buprenorphine? | Yes: 90.6 |
| Have you ever received psychological treatment for addiction? (%) | Yes: 31.3 |
| Top 3 biggest barriers to staying in medication or psychological treatment (n = 10) | Using opioids again or had relapse and never went back to clinic: 90 |
| Visit frequency intolerable: 60 | |
| Clinic not conveniently located: 70 | |
| How ready do you feel to start treatment for OUD in the hospital? (0-10) (mean, SD) | 8.5 (2.6) |
| How ready are you to continue treatment in the community? (Scale 0-10) (mean, SD) | 8.6 (2.3) |
| Gained housing during follow-up n (%) | 9 (28.1) |
| Percent still using opioids at each time point n (%) | Week 2:0/7 (0) |
| Week 4:3/10 (30) | |
| Week 6: 2/7 (29) | |
| Month 3: 4/7 (57) | |
| Month 6: 4/5 (80) | |
| Percent still using opioids on MOUD at each time point n (%) | Week 2:0/6 (0) |
| Week 4: 2/8 (25) | |
| Week 6: 1/6 (17) | |
| Month 3: 3/5 (60) | |
| Month 6: 2/3 (67) | |
| Likeliness to continue MOUD at last check-in (1 being extremely unready 10 being extremely ready)? (Mean, SD) | 10 (0) |
| Satisfaction in treatment at week 4 (1 being extremely dissatisfied 10 being extremely satisfied) (Mean, SD) | Week 2: 9.33 (1.0) |
| Week 4: 7.38 (3.1) | |
| Week 6: 9.6 (0.9) | |
| Month 3: 8.33 (2.1) | |
| Month 6: 9.5 (0.9) | |
Includes orthopedic surgery, general surgery, vascular surgery.
The third domain involved 2 external reviewers who used semi-structured interviews to explore research team members’ perceptions of the study design, implementation, and impact. Research team members were asked open-ended questions about their experiences with the study and were given time for reflections (Table 3).
Table 3.
Dominant themes of qualitative interviews among study personnel.
| Tension between science and service |
| “Sometimes grant restrictions prevent you from doing what you would really like to do or what you feel you should do.” |
| “In some ways, sometimes I feel we should just kind of forget the science and just give people the resources they need.” |
| “From a utilitarian perspective, I wish we could have used our grant funding to achieve proper science and also help people.” |
| Challenges to retaining study subjects |
| “It frustrated me that we weren’t more proactive in thinking about once you discharge a patient with a phone, thinking about of the potential challenges there could be. I felt bad and sad for patients; [I was] kicking myself in terms of what we could have done better to retain patients once they were enrolled in the project and discharged [from the hospital].” |
| “I think we were all a little surprised that we didn’t have more participants than we had. We came in with a baseline understanding that there were so many patients with opioid use disorder and homelessness, but we had a pretty small sample.” |
| COVID-19 pandemic-related challenges to study implementation |
| “We are thinking that a lot of patients were not presenting to the ED because they were just staying in. It is hard to separate our low enrollment numbers from being in the midst of COVID.” |
| “Talking [to study participants] on Zoom on an iPad felt impersonal especially when we were discussing things like substance use, and a lot of times participants were in withdrawal and weren’t comfortable. It might have been different if I had been there in person. The biggest logistical hurdle was COVID.” |
| “We had weekly team meetings but were never in a room together. It’s kind of weird to think about working together for 14 months on a study without having a team in a room together. Would [being able to be together] have led to better brainstorming? There has to have been an effect on that.” |
Statistical analysis
Transcripts of the acceptability by study analysis were analyzed independently by 2 reviewers using inductive content analysis. Initially, the reviewers independently reviewed the same 3 transcripts to identify themes, then met via a video call for an in-depth discussion of the themes identified in the 3 transcripts, reconciling differences in perceptions of these themes, and developing a codebook for use in the analysis of subsequent transcripts. The reviewers felt after reviewing the initial transcripts that thematic saturation had been reached. Next, the remainder of the 8 interview transcripts were analyzed independently by 2 reviewers using Dedoose software to capture each initially identified theme, and to add others that surfaced. The reviewers then compared their findings; any differences with regards to themes were resolved via discussion.
Results
Enrollment process and study feasibility
Between November 2020 to June 2021 our concurrent OUD and housing insecurity screens identified a total of 887 unique patients (Figure 1). Of those, 160 patients were referred to the addictions team by our screening nurse and 32 were found to be fully eligible, having both concurrent OUD and housing insecurity within the last year.
Participant demographics and questionnaire results
We enrolled a total of 32 patients who met study criteria. The mean age was 44 years old, the majority self-identified as male (78%), and self-identified mostly as White (56%) or Black (38%). All subjects had either Medi-Cal (81%), California’s version of Medicaid, or Medicare (19%). The most common discharging service was hospital medicine (60%), and the most common diagnoses were skin and soft tissue infection (SSTI) (31%), osteomyelitis or discitis (13%), and congestive heart failure (CHF) exacerbation (13%) (Table 1).
All 32 subjects were administered our intake questionnaire with key results in Table 1. A large proportion of subjects had concurrent alcohol or tobacco use (44% and 84%, respectively) and utilized opioids daily (75%). Subjects also expressed a strong urge to use opioids and reported that their use of opioids had led to health, social, legal, or financial problems in the past month. Most participants (59%) had overdosed on opioids at least once (mean 3.5, SD 3.9) and almost half had been administered naloxone for an overdose at least once (mean 2.5, SD 2.1). Almost all subjects (84%) reported that they had attempted to cut down or stop using opioids at some point, with 90% having been on methadone or buprenorphine in the past. Few subjects had received prior psychological treatment for addiction (31.3%). Of subjects with any past treatment for addiction, the biggest barriers in staying in treatment were relapse (90%), intolerably frequent clinic visit requirements (60%), and inconvenient locations of methadone clinics (70%). At enrollment, subjects had endorsed high levels of readiness to start MOUD treatment in the hospital and to continue treatment after discharge in the community (mean 8.5, SD 2.6 and mean 8.6, SD 2.3, respectively) (scale 1-10).
At each follow up within the 6-month period after discharge, reach rates were low: 40% of enrollees answered at least 1 follow up call and the highest reach rate (31% of enrolled patients) occurred at the week 4 follow up (Figure 2). During the full follow up period, only 28% of enrolled subjects gained housing. Among subjects who answered at each time point, MOUD adherence was high but decreased after each follow up (Figure 2). At the highest outreach period (week 4), participants reported an average satisfaction rate of 7.4 (scale 1-10) with MOUD treatment. The most common barrier to MOUD treatment mentioned by participants was lack of transportation to get to the clinic every day, specifically among subjects who had health issues that limited mobility. The proportion of subjects using opioids, other than treatment opioids, at each check-in increased with time, including 0% using opioids at the 2 weeks follow up assessment, and 80% of subjects using opioids at 6 months follow up. At the third and 6 months follow ups, more than half of the subjects still taking MOUD were also concurrently using opioids. Based on chi-squared and ANOVA testing, demographic and clinical variables were not significantly different among the groups of patients who had different reach rates throughout the 6 months follow up period (all P-values >.05) (Table 2).
Table 2.
Demographic and clinical characteristics by number of completed follow up calls.
| Variable | High rate of follow-up (4-5 follow up calls completed) | Low rate of follow-up (1-3 follow up calls completed) | No follow-up |
|---|---|---|---|
| N = 5 | N = 7 | N = 20 | |
| Age (Mean, SD) | 46.8 (10.8) | 49.1 (11.5) | 42.1 (15.4) |
| Gender | Male: 4 (80%) | Male: 5 (71%) | Male: 16 (80%) |
| Female: 1 (20%) | Female: 2 (29%) | ||
| Race | African American: 2 (40%) | African American: 2 (29%) | African American: 8 (40%) |
| White: 2 (40%) | White: 5 (71%) | White: 11 (55%) | |
| Unknown: 1(20%) | Other: 1 (5%) | ||
| Length of stay in days (Mean, SD) | 6.2(5.0) | 5.3(2.1) | 11.9(11.7) |
| Insurance status | Medicaid: 4 (80%) | Medicaid: 6 (86%) | Medicaid: 16 (80%) |
| Medicare: 1(20%) | Medicare: 1(14%) | Medicare: 4(20%) | |
| MOUD adherence at last follow up | Yes: 3 (60%) | Yes: 6 (86%) | NA |
| No: 2 (40%) | No: 1 (14%) | ||
| Concurrent opioid use at last follow up | Yes: 3 (60%) | Yes: 2 (29%) | NA |
| No: 2 (40%) | No: 5 (71%) | ||
| Readmission | |||
| 30-day ED visit | 0 (0%) | 0 (0%) | 1 (5%) |
| 7-day readmission | 0 (0%) | 0 (0%) | 3 (15%) |
| 30-day readmission | 0 (0%) | 1 (14%) | 0 (0%) |
| Previous MOUD treatment | 5 (100%) | 7 (100%) | 17 (85%) |
| Readiness to continue MOUD treatment after discharge (scale 1-10) Mean (SD) | 9.6 (0.89) | 7.86 (2.67) | 8.6 (2.39) |
Our participants had an average length of stay of 10.3 days in the hospital; 3% had an ED visit within 7 days of discharge, 9% had a 7-day readmission, and 3% had a 30-day readmission. In comparison, adult patients at our institution for fiscal year 2021 had an average length of stay of 6.5 days and a 30-day readmission rate of 10%. Subjects who had been contacted at least once had a utilization average of 0.92 and subjects who were unable to be reached at any point during follow up had a utilization average of 2.35 within the 6 months of follow up.
Acceptability by study clinicians and personnel
Among the 8 study personnel that were interviewed, 3 major themes were identified among responses to perceptions, implementation, and impact of the study. These themes included the tension between scientifically sound inquiry and the desire to provide maximal services to a vulnerable population, challenges to retaining study subjects, and challenges to study implementation due to the COVID-19 pandemic (Table 3). Many study team members discussed the tension they felt between following a predetermined research protocol and adapting the study to best serve the largest number of people in need of the resources provided to study participants, such as gift cards and cellphones. This created moral distress among some team members, and some reflected during the interview on the disappointment they felt with regards to the resources that could have been disseminated to severely impoverished people in the community with substance use disorder who did not qualify for the study. These same interviewees discussed the obstacles that physical distancing during COVID-19 posed with regards to making a therapeutic connection with study participants or reaching patients before they left against medical advice.
Discussion
In a prospective longitudinal study, we screened 887 unique patients admitted to our hospital and enrolled 32 subjects with opioid use disorder and homelessness who initiated or optimized MOUD. Subjects underwent a brief psychosocial intervention, and up to 6 months of treatment follow-up after hospital discharge. We found that subjects who are PEH with OUD are motivated to initiate MOUD in the hospital. Subjects reached at any follow up expressed high likeliness to continue MOUD, high satisfaction with MOUD treatment, and initially high, though progressively decreasing, MOUD adherence. Due to the significant study attrition rate of subjects, we cannot generalize these findings to the rest of the enrolled subjects.
We were able to detail important characteristics of this patient population, notably including high rates of concurrent alcohol and tobacco use, and high rates of prior overdose and attempts at starting MOUD. These baseline findings indicate broader health risks beyond opioid overdose and indicate areas for potential targeted interventions in the future. We found high rates of loss to follow up after hospital discharge, even after providing participants with a pre-paid cellphone. Barriers to continued MOUD included difficulty in getting to a methadone clinic daily due to poor access to appropriate transportation, not having stable housing, long wait times at clinics, and exposure to settings with high levels of drug use. Of the subjects that we reached on follow up, many expressed difficulties in getting additional medical resources, housing, and continuing MOUD treatment. Among subjects who continued MOUD, there were high rates of concurrent opioid use. While continued MOUD is important in the treatment of OUD, a chronic illness associated with considerable morbidity and mortality for PEH, competing world factors associated with homelessness interfere with the ability to adhere to daily treatment, including lack of access to transportation and medical resources.
There were also high rates of study attrition and loss to follow up which may have been due to a few reasons. The first follow up call was at 2 weeks after discharge. However, a study has shown that transitional care resources are most beneficial within 7 days of discharge and 2 weeks may have been too long of a delay to establish a connection with our study population. 14 Additionally, patients who were lost to follow up often had calls go straight to voicemail, indicating that the phone may not have been actively used or was not fully charged. Our patients experiencing homelessness may not have had a consistent place to charge their cellphones after discharge and there may have been a technological literacy barrier for some patients in how to consistently operate a cell phone. 9
Our study was developed based on the hypothesis that there are many high-risk patients who are not being identified for MOUD treatment. This study involved an extensive screening process that required daily chart review by our nurse, research analysts, and addiction clinicians, who all performed this work on top of existing duties. Despite a 97% enrollment rate, only 3.7% of screened patients were ultimately eligible for enrollment. Comparing this approach to the existing pathway is challenging, given secular trends in EHR identification and practice patterns during the pandemic, but this intensive approach may not be worthwhile or effective in identifying patients in need. This is a challenge that many health systems may encounter when using electronic health record screens, that lack specificity, in identifying vulnerable patient groups. We hope that in the future, automated EHR screens would be both sensitive and specific enough to properly identify PEH with OUD. This would protect the time for addiction clinicians to provide clinical care and devote resources to address larger systemic issues identified by the research team, including bedside counseling, treatment of concurrent substance use disorders, discharge planning, housing, and patient education such as harm reduction strategies. We already know that housing assistance, access to communication/telephone, and durable outpatient and inpatient mental health services are essential to treatment retention.5,13 From the qualitative interviews, our study staff identified the moral distress of having access to grant funding and resources and feeling that direct financial assistance offered to patients would be of greater benefit. Our results underlie the known challenges of remaining on MOUD considering the extreme systemic barriers faced by these patients.
We had many limitations in this study. This was a single center study that focused on recruitment in 1 tertiary hospital in San Francisco that focuses on subspecialty care and has limited dedicated clinical addiction services. The high rates of loss to follow up at each period made it difficult to assess the needs of this vulnerable population after discharge. Studies show that few patients with opioid use disorder receive MOUD post discharge. 15 While our reached patients had high rates of MOUD adherence, there may be selection bias to those individuals who answered our follow up calls. 15 This entire study was performed early during the COVID-19 pandemic in San Francisco. With lockdowns in place and with available local novel housing resources, including hotels for PEH, presentations to the hospital may have been reduced, decreasing the pool of potential enrollees.16,17 Additionally, due to COVID restrictions on study personnel, we were unable to enroll patients who entered and were discharged from the emergency department, limiting our prospective participant pool. Finally, we recognize that there are additional aspects to a bundled intervention that could have enhanced the prospects of recovery in this population, but we were limited by pilot funding for this project, and the constraints of our health system during the COVID pandemic, including staffing, available outpatient linkages, and scheduling.
With the pandemic forcing hospitals and clinics to focus on treating patients with COVID-19, people with OUD and other substance use disorders, who have already experienced marginalization and stigmatization by healthcare systems, have encountered additional barriers to treatment. 18 Although the San Francisco area was not significantly impacted by overwhelmed hospitals early in the pandemic, our study team found physical distancing a significant barrier in making meaningful connections with patients in need of multiple resources. During this intervention, our addiction specialists provided their study related services on top of their existing clinical and administrative obligations, highlighting the importance of health systems hiring and funding dedicated addiction specialists. While screening for and enrolling patients in the inpatient setting can form part of a multipronged intervention, our results demonstrate that it is insufficient in retaining patients longitudinally.
Despite these significant limitations, our study points to the importance of holistic approaches to address opioid-related risks for this vulnerable population. Approaches include the importance of delivering evidence-based MOUD, and also include the access to psycho-social needs that support MOUD treatment for PEH, such as reliable transportation and housing. It has recently been argued that in order to transform the current system of addiction and mental health services, the health care system has to meet these patients by addressing the specific socioeconomic circumstances that exacerbate the health concerns of this population. 19 Overcoming scarcity of time and resources for social workers and case management, and ensuring reliable linkage to outpatient follow-up care and social services, including housing, are other ways to potentially improve care for this vulnerable patient population.
Conclusions
While our extensive screening process accurately identified at risk patients who were experiencing OUD and homelessness, similar interventions can be made more effective through ongoing improvement in EHR diagnostic and demographic classification to efficiently identify vulnerable patients. Post-discharge outreach for the 6 months of follow up showed high rates of attrition even after providing patients with cell phones. Of the patients who were able to be reached, the majority remained adherent to MOUD, though barriers such as lack of transportation and unstable housing were often identified as challenges to long term MOUD adherence. Resource limitation was a major theme for this intervention. Health systems, supported by regional and federal health policy, should ensure that patients with substance use disorder and homelessness are well-supported through social services, affordable and accessible transportation, stable housing, and reliable access to outpatient care. Without these larger extra-medical supports and resources for vulnerable patients, the ever-increasing morbidity and mortality from opioid use seems likely to continue.
Supplemental Material
Supplemental material, sj-docx-1-sat-10.1177_11782218231166382 for A Focused Screening and Clinical Intervention with Streamlined Outpatient Linkage for Hospitalized Patients with Opioid Use Disorder Experiencing Homelessness by Sandra Oreper, Allison Bond, Marilyn Bazinski, Matthew Tierney, Margaret Fang, Sujatha Sankaran and Aksharananda Rambachan in Substance Abuse: Research and Treatment
Supplemental material, sj-docx-2-sat-10.1177_11782218231166382 for A Focused Screening and Clinical Intervention with Streamlined Outpatient Linkage for Hospitalized Patients with Opioid Use Disorder Experiencing Homelessness by Sandra Oreper, Allison Bond, Marilyn Bazinski, Matthew Tierney, Margaret Fang, Sujatha Sankaran and Aksharananda Rambachan in Substance Abuse: Research and Treatment
Acknowledgments
We are incredibly grateful to Meher Singh, our social workers and addiction providers for their invaluable assistance with this project. We thank Yumiko Abe-Jones and the UCSF Data Core for their assistance in developing our EHR screen.
Footnotes
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This publication was supported by the National Center for Advancing Translational Sciences, National Institutes of Health, through UCSF-CTSI Grant Number #UL1 TR001872. Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the NIH. Dr. Fang’s institution received funding from the National Heart, Lung, and Blood Institute (NHLBI) K24HL141354.
The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: Mrs. Sandra Oreper reports personal fees from EpiExcellence, LLC outside the submitted work.
Author contributions: AR, SS, MT, MB, and MF developed the intervention and study methodology. MB, MT, SS, and AR, SO, enrolled patients in the study. SO conducted all follow up calls with enrolled patients. AB conducted the qualitative interview and analyses for the acceptability by study team section of the study. SO and AR wrote the manuscript with support from all of the other authors. All authors contributed and provided critical feedback to the research, analyses and final version of the manuscript.
Supplemental material: Supplemental material for this article is available online.
References
- 1.Ahmad FB, Cisewski JA, Rossen LM, Sutton P. Provisional drug overdose death counts. National Center for Health Statistics. Accessed May 9, 2022. https://www.cdc.gov/nchs/nvss/vsrr/drug-overdose-data.htm
- 2.Jung Y. Tracking San Francisco’s drug overdose epidemic. Accessed May 9, 2022. https://www.sfchronicle.com/projects/2021/san-francisco-drug-overdoses-map/
- 3.COVID-19 cases and deaths | San Francisco. Accessed May 9, 2022. https://sf.gov/data/covid-19-cases-and-deaths#total-cases-and-deaths
- 4.Baggett TP, Chang Y, Singer DE, et al. Tobacco-, alcohol-, and drug-attributable deaths and their contribution to mortality disparities in a cohort of homeless adults in Boston. Am J Public Health. 2015;105:1189-1197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Pfefferle SG, Karon SS, Wyant B. Choice Matters: Housing Models that May Promote Recovery for Individuals and Families Facing Opioid Use Disorder. ASPE. Accessed May 5, 2022. https://aspe.hhs.gov/reports/choice-matters-housing-models-may-promote-recovery-individuals-families-facing-opioid-use-disorder-0 [Google Scholar]
- 6.McLaughlin MF, Li R, Carrero ND, Bain PA, Chatterjee A.Opioid use disorder treatment for people experiencing homelessness: a scoping review. Drug Alcohol Depend. 2021;224:108717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Carter J, Zevin B, Lum PJ.Low barrier buprenorphine treatment for persons experiencing homelessness and injecting heroin in San Francisco. Addict Sci Clin Pract. 2019;14:20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Slesnick N, Chavez L, Bunger A, et al. Housing, opportunities, motivation and engagement (HOME) for homeless youth at-risk for opioid use disorder: study protocol for a randomized controlled trial. Addict Sci Clin Pract. 2021;16:30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Godersky ME, Saxon AJ, Merrill JO, Samet JH, Simoni JM, Tsui JI.Provider and patient perspectives on barriers to buprenorphine adherence and the acceptability of video directly observed therapy to enhance adherence. Addict Sci Clin Pract. 2019;14:11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.O’Gurek DT, Jatres J, Gibbs J, Latham I, Udegbe B, Reeves K.Expanding buprenorphine treatment to people experiencing homelessness through a mobile, multidisciplinary program in an urban, underserved setting. J Subst Abuse Treat. 2021;127:108342. [DOI] [PubMed] [Google Scholar]
- 11.Langabeer J, Champagne-Langabeer T, Luber SD, et al. Outreach to people who survive opioid overdose: linkage and retention in treatment. J Subst Abuse Treat. 2020;111:11-15. [DOI] [PubMed] [Google Scholar]
- 12.Weinstein LC, Iqbal Q, Cunningham A, et al. Retention of patients with multiple vulnerabilities in a federally Qualified Health Center buprenorphine Program: Pennsylvania, 2017–2018. Am J Public Health. 2020;110:580-586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Simpson SA, Hordes M, Blum J, Rinehart D, Al-Tayyib A.Barriers to engagement in opioid use disorder treatment after buprenorphine induction. J Addict Med. 2022;16:479-482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Jackson C, Shahsahebi M, Wedlake T, DuBard CA.Timeliness of outpatient follow-up: an evidence-based approach for planning after hospital discharge. Ann Fam Med. 2015;13:115-122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Naeger S, Mutter R, Ali MM, Mark T, Hughey L.Post-discharge treatment engagement among patients with an opioid-use disorder. J Subst Abuse Treat. 2016;69:64-71. [DOI] [PubMed] [Google Scholar]
- 16.Fuchs JD, Carter HC, Evans J, et al. Assessment of a hotel-based COVID-19 isolation and quarantine strategy for persons experiencing homelessness. JAMA Netw Open. 2021;4:e210490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Grunau B, Helmer J, Lee S, et al. Decrease in emergency medical services utilization during early stages of the COVID-19 pandemic in British Columbia. Can J Emerg Med. 2021;23:237-241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Khatri UG, Perrone J.Opioid use disorder and COVID-19: crashing of the crises. J Addict Med. 2020;14:e6-e7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Alegría M, Frank RG, Hansen HB, Sharfstein JM, Shim RS, Tierney M.Transforming mental health and addiction services: commentary describes steps to improve outcomes for people with mental illness and addiction in the United States. Health Aff. 2021;40:226-234. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-docx-1-sat-10.1177_11782218231166382 for A Focused Screening and Clinical Intervention with Streamlined Outpatient Linkage for Hospitalized Patients with Opioid Use Disorder Experiencing Homelessness by Sandra Oreper, Allison Bond, Marilyn Bazinski, Matthew Tierney, Margaret Fang, Sujatha Sankaran and Aksharananda Rambachan in Substance Abuse: Research and Treatment
Supplemental material, sj-docx-2-sat-10.1177_11782218231166382 for A Focused Screening and Clinical Intervention with Streamlined Outpatient Linkage for Hospitalized Patients with Opioid Use Disorder Experiencing Homelessness by Sandra Oreper, Allison Bond, Marilyn Bazinski, Matthew Tierney, Margaret Fang, Sujatha Sankaran and Aksharananda Rambachan in Substance Abuse: Research and Treatment