Abstract
Background:
Low-income racially and ethnically diverse children are at higher risk for obesity compared with their counterparts; yet, few studies have assessed their diet quality.
Objective:
To evaluate the diet quality of a racially and ethnically diverse cohort of 2-year-olds using the Healthy Eating Index (HEI)-2010.
Methods:
We used 24-hour dietary recall data from caregivers of toddlers (24–34 months) at 4 pediatric resident clinics that participated in the Greenlight Study to calculate compliance with the Dietary Guidelines for Americans (DGA) using total HEI score (range 0–100) and 12 component scores.
Results:
Participants (n=231) were mostly Hispanic (57%) or non-Hispanic black (27%) and from low-income families. Mean HEI-2010 score was 62.8 (SD 10.5). Though not significant, Hispanics had the highest HEI score. Toddlers of caregivers without obesity, older than 35 years and born outside the U.S. had higher HEI scores. Most had high HEI component scores for dairy, fruit, and protein foods, but few achieved maximum scores, particularly for whole grains (13%), vegetables (10%), and fatty acid ratio (7%).
Conclusion:
Despite scores reflective of DGA recommendations for fruit, dairy and protein foods, toddlers in this diverse sample had low quality diets as measured by the HEI, driven largely by low component scores for whole grains, vegetables and ratio of unsaturated to saturated fatty acids.
Keywords: Childhood Obesity, Child Nutrition, Dietary Patterns, Dietary Guidelines, Diet Quality`
Introduction
National data document an increase in the prevalence of obesity (BMI≥95th percentile) among 2- to 5-year-olds with 13.7% considered obese in 2015–2016 compared with 9.3% in 2013–2014.1 We continue to see disparities among children with obesity, with higher rates among non-Hispanic black and Hispanic children compared with non-Hispanic white and non-Hispanic Asian children. These children with obesity are at increased risk of developing chronic conditions during childhood, having poorer quality of life, remaining obese as adults, and having more severe forms of chronic conditions during adulthood.2–4
Dietary intake drives diet quality, and dietary habits associated with obesity, such as low intakes of fruits and vegetables and high intakes of sugar-sweetened beverages, are emerging during the first two years of life.5–7 Many toddlers consume some type of dessert, sweet/savory snack or sugar-sweetened beverage at least once in a day, while a substantial proportion do not consume any fruit or vegetable in a given day.8 This is concerning because early established food preferences and eating behaviors track through childhood, potentially setting the stage for poor diet quality and increased risk for obesity.9,10
While consuming certain foods, such as a variety of fruits and vegetables,11 and limiting others, such as sugar-sweetened beverages,12 is important, evaluating the quality of children’s diets as a whole remains critical. Recommendations for optimal diet quality to help achieve and maintain a healthy weight, promote health, and prevent disease for healthy Americans aged 2 years and older exist through the Dietary Guidelines for Americans (DGAs).13 However, few studies examine diet quality in toddlers and the extent to which their diet aligns with recommendations outlined in the DGAs, and none do so in a diverse, low-income sample.14,15
Given the impact consumption of obesogenic foods can have on later intake, a need for studies examining diet quality during early childhood exists, particularly for those at highest risk for obesity. The objective of this study was to evaluate the diet quality of a racially and ethnically diverse sample of 2-year-olds using data from 24-hour dietary recalls to calculate a Healthy Eating Index (HEI)-2010 score; the HEI is a tool used to assess the extent to which diets are consistent with the DGAs.16
Methods
Participants
Data for this cohort come from caregiver-toddler dyads who participated in the Greenlight Intervention Study (Greenlight), a cluster randomized obesity prevention trial conducted during the first 2 years of life at 4 U.S. pediatric resident clinics (NC, FL, CA and NY). Detailed design and methods of Greenlight have been described elsewhere.17 Beginning September 2012 through August 2014 caregiver-toddler dyads who were enrolled in the original Greenlight intervention study17 were recruited to participate in two 24-hour multi-pass dietary recalls. Caregiver-child dyads were approached by phone or in-person from all four participating clinics to consent to participate. Participants received $10 compensation for each recall completed. For this study, only children between 24 and 34 months of age who were not receiving breast milk were included (n=231) to reflect the target population of the DGAs. Currently, the DGAs do not include children receiving breast milk or those aged 0–2 years. All protocols were approved by IRBs at all the sites and all caregivers provided written informed consent.
Dietary intake
To assess the diet, we relied on caregivers as proxy reporters.18 Toddler dietary intakes were assessed via telephone by trained, bilingual study personnel using computerized 24-hour dietary recalls (24HDR) and the Nutrition Data System for Research (NDSR™) (version 2012; Nutrition Coordinating Center, University of Minnesota, Minneapolis, MN). Caregivers were provided example food charts in English or Spanish, and detailed instructions on how to use the food log in the event the child was attending child/day care or otherwise spending portions of their day away from the caregiver responding. Caregivers were also provided measurement aids to estimate portion size. The 24HDRs were performed on random nonconsecutive days that included one week day and one weekend day. Most 81% (n=188) completed two 24HDRs; however, 17% (n=40) completed only one while 1% (n=3) completed a third recall when assessments were deemed incomplete or implausible (i.e. participant was unable to complete the entire recall at one time).
Diet Quality
To assess diet quality, we used the Healthy Eating Index-2010 (HEI-2010), a tool developed by the U.S. Department of Agriculture and the National Cancer Institute to determine conformance with the 2010 DGAs, which were current at the time of data collection.16 Data from the 24HDR were averaged and used to calculate HEI-2010 component and total scores. The HEI score consists of 12 components19, 9 of which assess adequacy of the diet, including 1) total fruit; 2) whole fruit; 3) total vegetables; 4) greens and beans (dark green vegetables and legumes not already counted as protein foods); 5) whole grains; 6) dairy; 7) total protein foods; 8) seafood and plant proteins; and 9) fatty acids, which is a ratio of unsaturated versus saturated fatty acids. The remaining three assess dietary components recommended to consume in moderation: 10) refined grains; 11) sodium; and 12) empty calories (i.e., energy from solid fats, alcohol, and added sugars). For all components, higher scores reflect better diet quality as moderation components are reverse scored. Each component is scored on a density basis, either as a percentage of calories or per 1000 calories allowing use of the HEI for a range of ages and populations - based on quality vs. quantity, i.e. a standard serving size. Summed scores of the 12 components yield a possible total score of 100, with a higher score reflecting greater compliance with the 2010 DGAs.20
Covariates
Socioeconomic and demographic characteristics were measured during participation in Greenlight. Covariates were selected a priori and drawn from the literature to include factors previously associated with child diet: caregiver education, age, income, marital status and obesity (BMI ≥30.0), and toddler BMI percentile, race/ethnicity, and sex.21–24 Caregiver height and weight were collected at baseline (2 months) and toddler height and weight were measured at the 24-month well-child visit; these data are missing for 9% of toddlers (n=21) who participated in the 24HDR data collection by phone, but were no longer patients at study clinics where anthropometric measurements were completed. We explored specific predictors of diet quality in our analyses, including participation in the Special Supplemental Nutrition Program for Women, Infants, and Children (WIC) and household food security status, which was assessed using the 2-item screen derived from the U.S. Department of Agriculture 18-item Household Food Security Survey.25 Given the diversity of our sample, we also included whether caregivers were born in the U.S.
Statistical analysis
Characteristics are summarized as frequencies (%) for categorical variables and means and standard deviations (SD) for continuous variables. HEI-2010 scores were calculated using NDSR output to estimate each component with guidance from the Nutrition Coordinating Center.26 With guidance from the National Cancer Institute, the mean ratio approach was applied to calculate total HEI and HEI component scores, summarized as means and standard deviation (SD).27 We also present the percent of maximum score achieved [(mean score/maximum score) x 100%], since maximum scores differed for various components and ranged from 5–20. Component scores are reported as medians with interquartile range (IQR) given skewness. A one sample t-test was applied to determine if total HEI scores were significantly different from the maximum score of 100 and Wilcoxon signed-rank test for component scores and their respective maximum scores. Polychoric correlation matrices tested for collinearity among socioeconomic and demographic predictors. No predictors were significantly correlated. We assessed the relationship of each socioeconomic and demographic predictor with HEI score using linear regression, while controlling for participating site. Since this was a cluster randomized trial, by controlling for site, we implicitly control for the intervention received. Percentages of toddlers meeting the maximum score for each HEI-2010 component were calculated. P values <0.05 were regarded as significant. All analyses were conducted using Stata 14 (StataCorp, College Station, TX).
Results
Most toddlers were Hispanic (57%) and non-Hispanic black (27%), from households earning less than $20,000 per year (64%), and receiving WIC benefits (87%) (Table 1). Although most toddlers (73%) had a healthy weight, 14% had overweight (BMI 85th to <95th percentile) and 7% had obesity (BMI >=95th percentile). One third of caregivers had obesity (BMI >=30), and the majority (70%) had completed high school. HEI-2010 scores ranged from 37.9 to 93.6; the mean score was 62.8 (SD 10.5) and was significantly lower than the optimal recommended score of 100 (P<.001) (Table 2).
Table 1.
Sociodemographic characteristics for toddlers (24–34 months) with 24-hour dietary recall data and mean Healthy Eating Index (HEI)-2010 score, who participated in the Greenlight Study (n=231).
| Characteristics | N (%) | HEI score,1 mean (sd) | |
|---|---|---|---|
| Sex | Female | 128 (55) | 63.2 (10.9) |
| Male | 103 (45) | 62.3 (10.1) | |
| Race/ethnicity | Hispanic | 131 (57) | 64.1 (9.6) |
| Non-Hispanic white | 29 (13) | 60.1 (11.6) | |
| Non-Hispanic black | 63 (27) | 61.3 (11.6) | |
| Non-Hispanic other | 8 (3) | 63.1 (11.2) | |
| Household income2,3 | <$19,999 | 141 (64) | 62.9 (10.3) |
| ≥$20,000 | 81 (36) | 62.8 (11.2) | |
| Child BMI percentile4 | Underweight (<5th percentile) | 12 (6) | 58.9 (11.0) |
| Healthy weight (5th to <85th) | 153 (73) | 62.8 (10.7) | |
| Overweight (85th to <95th percentile) | 30 (14) | 64.7 (8.5) | |
| Obese (≥95th percentile) | 15 (7) | 62.2 (11.9) | |
| Received WIC benefits2,5 | Yes | 200 (87) | 62.8 (10.5) |
| No | 30 (13) | 63.4 (10.4) | |
| Food insecure2,5 | Yes | 117 (51) | 62.8 (10.9) |
| No | 113 (49) | 62.7 (10.1) | |
| Caregiver characteristics | |||
| Education5 | Less than high school | 68 (30) | 61.7 (11.3) |
| High school graduate | 68 (30) | 63.2 (9.2) | |
| Some college | 54 (23) | 62.5 (10.9) | |
| College graduate | 40 (17) | 64.2 (10.9) | |
| Age | <30 years | 123 (53) | 61.1 (10.7)* |
| 30 –34 years | 66 (29) | 64.0 (9.36) | |
| ≥35 years | 42 (18) | 66.1 (11.1)* | |
| Obesity (BMI≥30.0)2,6 | Yes | 72 (35) | 60.0 (10.2)* |
| No | 131 (65) | 64.6 (10.6) | |
| Born in the U.S. | Yes | 101 (44) | 60.1 (10.3)* |
| No | 130 (56) | 64.9 (10.3) | |
| Married2,4 | Yes | 142 (68) | 64.2 (10.0)* |
| No | 68 (32) | 59.8 (10.8) | |
Healthy Eating Index, maximum score is 100
Measured at baseline at the 2-month well-child visit
Missing 9
Missing 21
Missing 1
Missing 28
p<.05
Table 2.
Mean and standard deviation for Healthy Eating Index-2010 component and total scores with median and interquartile range for toddlers participating in Greenlight (24–34 months) (n=231).
| Dietary Component1 (Max Score) | Mean | SD | Median | IQR | Percent of toddlers who achieved max score |
|---|---|---|---|---|---|
| Adequacy (higher scores indicate higher consumption) | |||||
| Total Fruit (5) | 4.1 | 1.5 | 5.0 | 3.4–5.0 | 65 |
| Whole Fruit (5) | 3.8 | 1.9 | 5.0 | 2.8–5.0 | 63 |
| Total Vegetables (5) | 2.2 | 1.4 | 1.9 | 1.1–3.1 | 10 |
| Greens and Beans (5) | 1.4 | 1.9 | 0.0 | 0.0–3.0 | 16 |
| Whole Grains (10) | 4.1 | 3.5 | 3.7 | 0.7–7.1 | 13 |
| Dairy (10) | 9.0 | 2.4 | 10.0 | 10.0–10.0 | 79 |
| Total Protein Foods (5) | 3.9 | 1.5 | 4.8 | 2.9–5.0 | 53 |
| Seafood and Plant Proteins (5) | 1.5 | 2.0 | 0.0 | 0.0–3.0 | 18 |
| Fatty Acid Ratio (10) | 2.3 | 3.1 | 0.9 | 0.0–3.5 | 7 |
| Moderation (higher scores indicates lower consumption) | |||||
| Refined Grains (10) | 7.7 | 2.9 | 9.0 | 5.9–10.0 | 45 |
| Sodium (10) | 5.3 | 3.4 | 5.4 | 2.4–8.5 | 19 |
| Empty Calories (20) | 17.8 | 3.1 | 19.1 | 16.2–20.0 | 45 |
| Total HEI-2010 Score (100) | 62.8 | 10.5 | 64.0 | 55.4–70.4 | 0 |
A higher number signifies a healthier amount of intake
Toddlers of caregivers with obesity had lower HEI scores in contrast to those without obesity (60.0 (SD 10.2) vs. 64.6 (SD 10.6), P=.009) (Table 1). Toddlers from caregivers born outside the U.S. had higher HEI scores compared to those born in the U.S. (64.9 (SD 10.3) vs. 60.1 (SD 10.3), P=.007). Toddlers from caregivers who were married or living with their partner had higher HEI scores in contrast to those who were single, separated/divorced or widowed (64.2 (SD 10.0) vs. 59.8 (SD 10.8), P=.005). Though not significant, Hispanic toddlers had higher HEI scores compared with non-Hispanic white, non-Hispanic black, and non-Hispanic other toddlers (64.1 (SD 9.6) vs. 60.1 (SD 11.6), P=.305; 61.3 (SD 11.6), P=.485; and 63.1 (SD 11.2), P=.850, respectively) (Table 1).
All HEI-2010 component scores were significantly lower than their respective maximum scores (P<.001) (higher scores reflect better diet quality for all components, as moderation components are reverse scored) (Table 2). Figure 1 is a radar graph to simultaneously show the percent of the maximum score achieved for each component; a perfect HEI-2010 total score (100% for each component) would be displayed as a line around the border of the radar graph. As demonstrated, the largest contributors to the HEI score were dairy, empty calories and total fruit, followed by total protein, refined grains and whole fruit. Toddlers consumed higher amounts of dairy and total fruit and lower amounts of empty calories and refined grains. However, toddlers consumed lower amounts of unsaturated fatty acids (i.e. fatty acid ratio), greens and beans and seafood and plant proteins and higher amounts of sodium. HEI-2010 component scores varied by race/ethnicity. In contrast to non-Hispanic white children, Hispanic and non-Hispanic black children had poorer whole fruit scores (4.3 (SD 1.4) vs. 3.8 (SD 1.9), P=.037 and 3.3 (SD 2.1), P=.010, respectively), and Hispanic children had better refined grain component scores (8.3 (SD 2.7) vs 6.4 (SD 2.9), P=.005). No other components varied by race/ethnicity.
Figure 1.
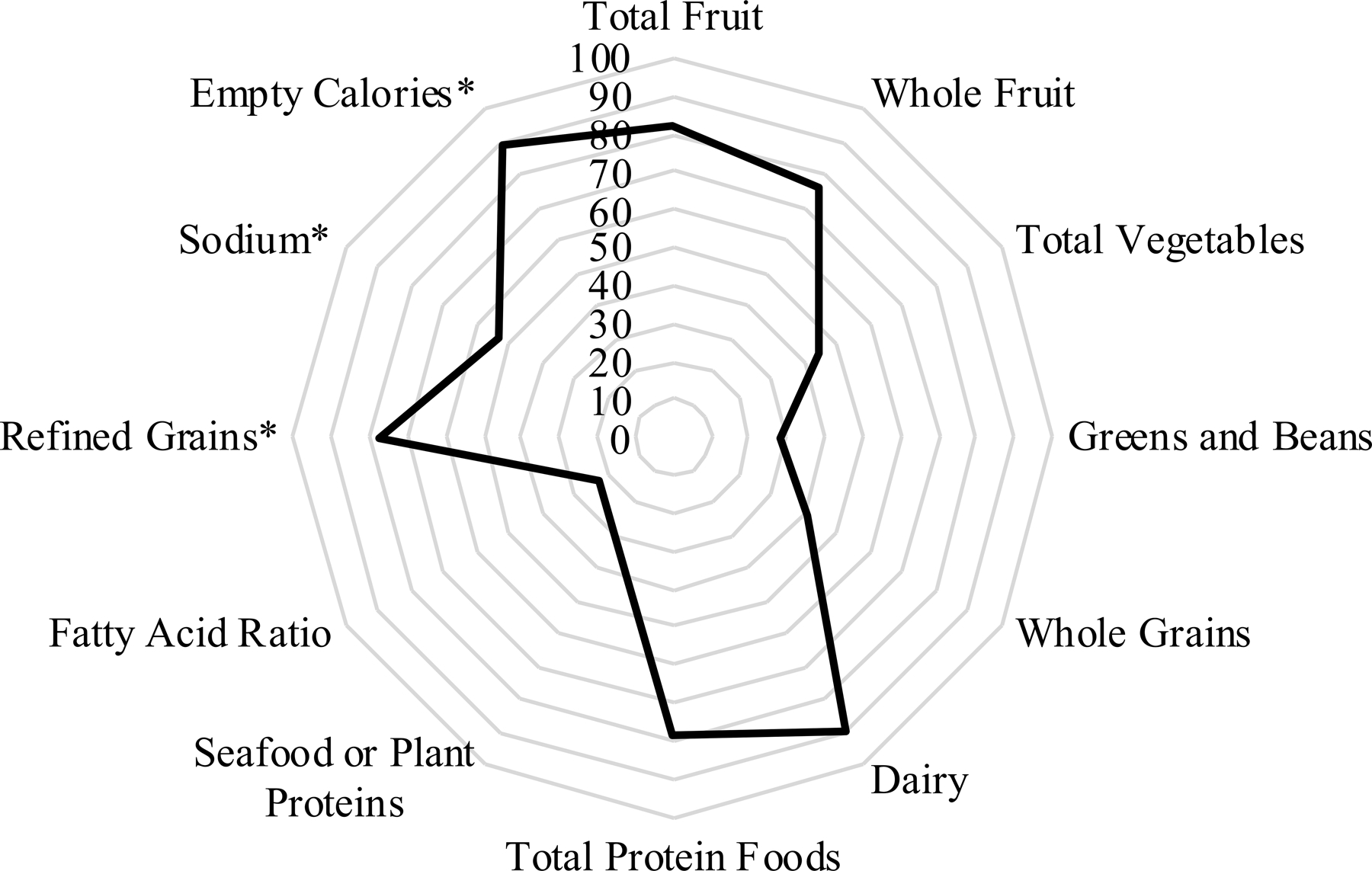
Radar plot showing the Healthy Eating Index (HEI)-2010 scores for toddlers participating in Greenlight (n=231). For each component, the plot is showing the percentage of total points received.
*Moderation components – higher score indicates lower consumption.
No children achieved the maximum score of 100 for total HEI score (Table 2). Most toddlers (79%) consumed the recommended amount of dairy. Many (65%) consumed the recommended amount of total fruit and whole fruit (63%) and nearly half (53%) of protein foods. Less than a quarter of children consumed the recommended amount of seafood and plant proteins (18%) and greens and beans (16%) and very few for whole grains (13%), total vegetables (10%) and unsaturated fatty acids (7%). Over half (55%) of toddlers consumed more than recommended amount of refined grains and empty calories and 81% consumed too much sodium. In contrast to non-Hispanic white children, Hispanic children were more likely to consume the recommended amount of refined grains (54% vs. 38%, P=.007).
Discussion
A significant finding of the present study is that overall diet quality is poor, particularly among diverse, low-income toddlers and can vary by race/ethnicity. Although many toddlers were consuming adequate amounts of fruit, dairy and foods high in protein, diets were generally lacking in other foods important not only for the prevention of obesity and chronic disease, but also for optimal growth and development, such as seafood and plant proteins. 28,29 Toddlers were falling short in their intake of vegetables, whole grains and greens and beans, while consuming too much sodium and saturated fatty acids. Among the few studies that have evaluated individual HEI-2010 dietary components among young children in the U.S., results are similar in that scores were highest for dairy, fruit, and protein foods, while most had suboptimal scores for seafood and plant proteins and greens and beans.15,30–32 These studies, together with previous studies examining consumption patterns of young children,5,33 suggest diets of children need improvement early on.
Among the few studies that have examined diet quality using HEI-2010, most are among older groups of less diverse children and show that as children age HEI-2010 scores decrease.14,15,31,34 Comparatively, we found slightly higher HEI scores in our younger, more diverse sample. In addition to the young age of our sample, receiving WIC benefits could explain the higher scores. In our sample, 87% of families were receiving WIC benefits, and those who were not receiving WIC benefits were more likely to have higher income levels, perhaps protecting their diet quality. Studies show diet quality is often better among children receiving WIC compared to children of similar economic status not receiving WIC;35,36 especially since the WIC food package was updated in 2009 to include more fruits and vegetables and a switch to low fat milk.37–39 Young children from WIC participating households demonstrate better diet quality, driven largely by increases in greens and beans, whole grains and unsaturated fatty acids and decreases in 100% juice.30,38,40,41 Together, these results suggest receiving WIC benefits could explain the higher HEI scores observed among this population and the importance of this program on diet quality of low-income children.
Over half of our sample included caregivers born outside the U.S., mostly (59%) from Mexico. Children from these caregivers demonstrated higher HEI-2010 scores. Other studies have demonstrated children from immigrant families, particularly among those of Mexican descent, have better diet quality.14,42,43 However, more time spent in the U.S. often results in poorer diet,44 which is likely due to adherence to the typical U.S. diet high in refined grains and added sugars compared to the more healthy foods found in traditional Mexican diets, including vegetables, legumes and whole grains.45 In fact, Hispanic children in our sample had higher HEI scores and consumed less refined grains. These results highlight the importance of encouraging immigrant Hispanic families to maintain components of their traditional diet while trying to adjust to U.S. dietary patterns.
We found that toddlers from caregivers with obesity had lower HEI scores. Possible explanations include the shared food environment at home or role modeling of poor eating behaviors.46 Additionally, toddlers from caregivers who were married or living with their partner had better diet quality. Studies show that diet quality differs among single vs. married mothers, marked by lower intakes of fruits and vegetables and higher intake of energy dense foods.47,48
Our results for the fatty acid ratio and the greens and beans HEI component scores differed slightly compared to published literature. Mean component scores for the fatty acid ratio were lower compared to scores reported in other studies.15,30–32 One reason for this could be the high prevalence of milk consumption, typical of 2-year olds.6,49 Most (93%) were consuming milk, and of those 40% were consuming whole milk. Milk is a top contributor to both energy and saturated fat intake among young children.6 The mean component score for greens and beans was comparatively higher. As described earlier, studies show legumes are commonly consumed among Latino populations and 57% of our population was Hispanic.50,51 This presents an opportunity to offer targeted interventions promoting the use of nuts and beans that are often found in traditional Hispanic and Latino dishes to increase diet quality.
Our study has several limitations. The use of a parent/caregiver proxy may have led to incomplete recalls, particularly if a child spends part of their day in a different environment. However, proxies are successfully used in many national surveys and are considered accurate to assess young children's diets.52 It is possible that caregivers, because of desirability bias, reported intakes that were more favorable than accurate. Nevertheless, study findings show very low intake of vegetables and whole grains and a lower than desirable HEI. Also, while the HEI has been updated beyond the 2010 version, we use the 2010 version because of the match with the standards at the time. The strengths of this study include the diverse racial and economic background of the sample and the developmental life stage that was targeted. Importantly, the age group targeted in this study is considered high risk for obesity in today’s food environment.
Understanding diet quality at this young age is important since nutrition plays an essential role in growth, development, and health. Our findings can be used to influence nutrition education and policy aimed at improving diet quality and provide nutrition education to parents and caregivers, specifically around increasing intake of whole grains, vegetables and unsaturated fats. Healthcare providers can play an active role in helping parents and caregivers understand the importance of healthy eating from an early age. A unique aspect of the WIC program is the requirement to provide nutrition education, which, given our results, could play an influential role in improving diet quality; the program dedicates considerable resources to developing and conducting high-quality, participant-centered learning. Additionally, the American Academy of Pediatrics and the Centers for Disease Control and Prevention have resources for parents, caregivers, and providers that support adopting a healthy dietary pattern.53 Our results may be useful to the U.S. Department of Agriculture and Department of Health and Human Services as they work to extend the Dietary Guidelines for Americans to children under the age of 2 years for the first time. The project, informally called the “B-24 project," aims to develop information and guidance on feeding and nutrition to achieve optimal growth and development for infants and toddlers.54 The findings from this study provide evidence that diet quality could be improved by increasing intake of vegetables, especially dark-green vegetables and peas and beans; substituting whole-grain for refined-grain products and seafood for some meat and poultry; choosing more nutrient-dense forms of foods, that is, foods low in solid fats and free of added sugars. Such changes would potentially reduce the risk for obesity by encouraging consumption of foods associated with a healthy weight.
Conclusions
Overall, diet quality in this cohort of low-income, diverse 2-year olds was poor. This study informs future directions for research because it prompts us to think through modifiable factors of toddler diet such as caregiver modeling, home environment and the importance of nutrition support programs, such as WIC. It also highlights the need for culturally tailored interventions. Thinking through methods to provide parental support for all race/ethnicities to support healthy eating may ultimately create improved toddler dietary intake which may have broad ranging clinical implications. Future research efforts could target interventions to test increasing consumption of fish, legumes, whole grains and unsaturated fatty acids and decreasing sodium intake to allow children to grow up with healthier dietary habits. Future research efforts should also examine racial and ethnic disparities in the relationship of toddler dietary patterns to later obesity.
What is Known
Early childhood nutrition is critical for optimal growth and development
Patterns of dietary intakes during early childhood influence later healthy eating habits
Racially and ethnically diverse children are at higher risk for obesity
What is New
In a diverse, low-income cohort of toddlers, many are consuming low quality diets as measured by the Healthy Eating Index (HEI)
Toddlers are consuming inadequate amounts of whole grains, vegetables and unsaturated fatty acids
Acknowledgements
NH/NICHD R01 HD059794 (PIs: Perrin, Yin, Rothman, Sanders, Delamater). The UNC-CH, NORC – Diet, Physical Activity and Body Composition Core with a grant from the NIH (DK56350). Thank you to the Greenlight Study Team and the research dietitians of the Vanderbilt Diet, Body Composition and Human Metabolism Core.
Funding sources:
This research was supported by the National Institutes of Health (NIH)/Eunice Kennedy Shriver National Institute of Child Health and Human Development grant R01HD059794 with Centers for Disease Control and Prevention supplements 04S1 and 04S2; NIH grant UL1TR001111; NIH/National Center for Advancing Translational Sciences grant UL1TR000445; NIH/National Center for Research Resources grants U54RR023499, UL1RR025747, and UL1TR000038; Robert Wood Johnson Foundation Physician Faculty Scholars program (Dr Yin); the Duke Center for Research to Advance Healthcare Equity, which is supported by NIMHD U54MD012530, and Health Resources and Services Administration grant T32HP014001; and the UNC-CH, NORC – Diet, Physical Activity and Body Composition Core with a grant from the NIH (DK56350). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. Special thanks to the Vanderbilt Diet, Body Composition, and Human Metabolism Core Research Dietitians and the Greenlight Study Team.
Footnotes
Conflict of Interest: Dr. Rothman reports personal fees from Abbott and Edlogics, outside the submitted work.
ClinicalTrials.gov Identifier: NCT01040897
References:
- 1.Skinner AC, Ravanbakht SN, Skelton JA, Perrin EM, Armstrong SC. Prevalence of Obesity and Severe Obesity in US Children, 1999–2016. In: Pediatrics United States: 2018 by the American Academy of Pediatrics.; 2018. [DOI] [PMC free article] [PubMed]
- 2.Baird J, Fisher D, Lucas P, Kleijnen J, Roberts H, Law C. Being big or growing fast: systematic review of size and growth in infancy and later obesity. BMJ (Clinical researched) 2005;331(7522):929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Reilly JJ, Armstrong J, Dorosty AR, Emmett PM, Ness A, Rogers I, Steer C, Sherriff A, Avon Longitudinal Study of P, Children Study T. Early life risk factors for obesity in childhood: cohort study. BMJ (Clinical research ed) 2005;330(7504):1357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Taveras EM, Rifas-Shiman SL, Sherry B, Oken E, Haines J, Kleinman K, Rich-Edwards JW, Gillman MW. Crossing growth percentiles in infancy and risk of obesity in childhood. Archives of Pediatrics & Adolescent Medicine 2011;165(11):993–998. [DOI] [PubMed] [Google Scholar]
- 5.Roess A, Jacquier E, Catellier D, Carvalho R, Lutes A, Anater A, Dietz W. Food consumption patterns of Infants and Toddlers with Racial/Ethnic Differences: Findings from The Feeding Infants and Toddlers study (FITS) 2016 2018. [DOI] [PMC free article] [PubMed]
- 6.Kay M, Welker E, Jacquier E, Story M. Beverage Consumption Patterns among Infants and Young Children (0–47.9 Months): Data from the Feeding Infants and Toddlers Study, 2016. Nutrients 2018;10(7):825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hamner HC, Perrine CG, Gupta PM, Herrick KA, Cogswell ME. Food Consumption Patterns among U.S. Children from Birth to 23 Months of Age, 2009–2014. Nutrients 2017;9(9). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Welker E, Jacquier E,DC, Anater A, Story M. Food consumption patterns of young children aged 2 to 4 years: Findings from the Feeding Infants and Toddlers study (FITS) 2016. Journal of Nutrition 2018. [DOI] [PMC free article] [PubMed]
- 9.Park S, Pan L, Sherry B, Li R. The association of sugar-sweetened beverage intake during infancy with sugar-sweetened beverage intake at 6 years of age. Pediatrics 2014;134 Suppl 1:S56–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Grimm KA, Kim SA, Yaroch AL, Scanlon KS. Fruit and vegetable intake during infancy and early childhood. Pediatrics 2014;134 Suppl 1:S63–69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ramsay SA, Shriver LH, Taylor CA. Variety of fruit and vegetables is related to preschoolers' overall diet quality. Prev Med Rep 2017;5:112–117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bleich SN, Vercammen KA. The negative impact of sugar-sweetened beverages on children's health: an update of the literature. BMC Obes. 2018;5:6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Department of Health US and Human Services D US Department of Agriculture U. 2015–2020 Dietary Guidelines for Americans 8th Edition. 2015;Available at http://health.gov/dietaryguidelines/2015/guidelines/(Journal,Electronic). Accessed November 11, 2016. [Google Scholar]
- 14.Gu X, Tucker KL. Dietary quality of the US child and adolescent population: trends from 1999 to 2012 and associations with the use of federal nutrition assistance programs. In: Am J Clin Nutr Vol 105. United States: 2017 American Society for Nutrition.; 2017:194–202. [DOI] [PubMed] [Google Scholar]
- 15.Ford CN, Poti JM, Ng SW, Popkin BM. SSB taxes and diet quality in US preschoolers: estimated changes in the 2010 Healthy Eating Index. Pediatr Obes 2017;12(2):146–154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Guenther PM, Casavale KO, Reedy J, Kirkpatrick SI, Hiza HA, Kuczynski KJ, Kahle LL, Krebs-Smith SM. Update of the Healthy Eating Index: HEI-2010. J Acad Nutr Diet 2013;113(4):569–580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sanders LM, Perrin EM, Yin HS, Bronaugh A, Rothman RL. "Greenlight study": a controlled trial of low-literacy, early childhood obesity prevention. Pediatrics 2014;133(6):e1724–1737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Tran KM, Johnson RK, Soultanakis RP, Matthews DE. In-person vs telephone-administered multiple-pass 24-hour recalls in women: validation with doubly labeled water. In: J Am Diet Assoc Vol 100. United States: 2000:777–783. [DOI] [PubMed] [Google Scholar]
- 19.National Cancer Institute. Developing the Healthy Eating Index 2020; https://epi.grants.cancer.gov/hei/developing.html. Accessed May 5, 2020.
- 20.Guenther PM, Kirkpatrick SI, Reedy J, Krebs-Smith SM, Buckman DW, Dodd KW, Casavale KO, Carroll RJ. The Healthy Eating Index-2010 is a valid and reliable measure of diet quality according to the 2010 Dietary Guidelines for Americans. J Nutr 2014;144(3):399–407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hendricks K, Briefel R, Novak T, Ziegler P. Maternal and child characteristics associated with infant and toddler feeding practices. Journal of the American Dietetic Association 2006;106(1 Suppl 1):S135–148. [DOI] [PubMed] [Google Scholar]
- 22.Smithers LG, Brazionis L, Golley RK, Mittinty MN, Northstone K, Emmett P, McNaughton SA, Campbell KJ, Lynch JW. Associations between dietary patterns at 6 and 15 months of age and sociodemographic factors. European journal of clinical nutrition 2012;66(6):658–666. [DOI] [PubMed] [Google Scholar]
- 23.Lazarou C, Newby PK. Use of dietary indexes among children in developed countries. Adv Nutr 2011;2(4):295–303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Russell CG, Haszard JJ, Taylor RW, Heath AM, Taylor B, Campbell KJ. Parental feeding practices associated with children's eating and weight: What are parents of toddlers and preschool children doing? Appetite 2018;128:120–128. [DOI] [PubMed] [Google Scholar]
- 25.Hager ER, Quigg AM, Black MM, Coleman SM, Heeren T, Rose-Jacobs R, Cook JT, Ettinger de Cuba SA, Casey PH, Chilton M, Cutts DB, Meyers AF, Frank DA. Development and validity of a 2-item screen to identify families at risk for food insecurity. In: Pediatrics Vol 126. United States 2010:e26–32. [DOI] [PubMed] [Google Scholar]
- 26.Nutrition Coordinating Center. Guide to Creating Variables Needed to Calculate Scores for Each Component of the Healthy Eating Index-2010 (HEI-2010) 2014; https://drive.google.com/file/d/0B4snm2Q3-ffQQTVHUWE1NGNxUnc/view. Accessed 35 July 2, 2019. [Google Scholar]
- 27.National Cancer Institute. The Healthy Eating Index – Mean Ratio Method 2017; https://epi.grants.cancer.gov/hei/population-ratio-method.html. Accessed January 8, 2020.
- 28.Nyaradi A, Li J, Foster JK, Hickling S, Jacques A, O'Sullivan TA, Oddy WH. Good-quality diet in the early years may have a positive effect on academic achievement. Acta Paediatr 2016;105(5):e209–218. [DOI] [PubMed] [Google Scholar]
- 29.Kim JL, Winkvist A, Aberg MA, Aberg N, Sundberg R, Toren K, Brisman J. Fish consumption and school grades in Swedish adolescents: a study of the large general population. In: Acta Paediatr. Vol 99. Norway: 2010:72–77. [DOI] [PubMed] [Google Scholar]
- 30.Tester JM, Leung CW, Crawford PB. Revised WIC Food Package and Children's Diet Quality. Pediatrics 2016;137(5). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Banfield EC, Liu Y, Davis JS, Chang S, Frazier-Wood AC. Poor Adherence to US Dietary Guidelines for Children and Adolescents in the National Health and Nutrition Examination Survey Population. J Acad Nutr Diet 2016;116(1):21–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kong A, Schiffer L, Antonic M, Braunschweig C, Odoms-Young A, Fitzgibbon M. The relationship between home- and individual-level diet quality among African American and Hispanic/Latino households with young children. Int J Behav Nutr Phys Act 2018;15(1):5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Welker EB, Jacquier EF, Catellier DJ, Anater AS, Story MT. Room for Improvement Remains in Food Consumption Patterns of Young Children Aged 2–4 Years. In: J Nutr. United States 2018. [DOI] [PMC free article] [PubMed]
- 34.Leung CW, DiMatteo SG, Gosliner WA, Ritchie LD. Sugar-Sweetened Beverage and Water Intake in Relation to Diet Quality in U.S. Children. Am J Prev Med 2018;54(3):394–402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Siega-Riz AM, Kranz S, Blanchette D, Haines PS, Guilkey DK, Popkin BM. The effect of participation in the WIC program on preschoolers' diets. In: J Pediatr Vol 144. United States 2004:229–234. [DOI] [PubMed] [Google Scholar]
- 36.Cole N, Fox MK. Diet Quality of American Young Children by WIC Participation Status: Data from the National Health and Nutrition Examination Survey, 1999–2004 Washington, DC2008. [Google Scholar]
- 37.Morshed AB, Davis SM, Greig EA, Myers OB, Cruz TH. Effect of WIC Food Package Changes on Dietary Intake of Preschool Children in New Mexico. Health Behav Policy Rev 2015;2(1):3–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Andreyeva T, Luedicke J, Henderson KE, Schwartz MB. The positive effects of the revised milk and cheese allowances in the special supplemental nutrition program for women, infants, and children. In: J Acad Nutr Diet Vol 114. United States: 2014 Academy of Nutrition and Dietetics. Published by Elsevier Inc; 2014:622–630. [DOI] [PubMed] [Google Scholar]
- 39.Odoms-Young AM, Kong A, Schiffer LA, Porter SJ, Blumstein L, Bess S, Berbaum ML, Fitzgibbon ML. Evaluating the initial impact of the revised Special Supplemental Nutrition Program for Women, Infants, and Children (WIC) food packages on dietary intake and home food availability in African-American and Hispanic families. Public Health Nutr 2014;17(1):83–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Andreyeva T, Luedicke J. Federal food package revisions: effects on purchases of whole-grain products. In: Am J Prev Med Vol 45. Netherlands: 2013 American Journal of Preventive Medicine.; 2013:422–429. [DOI] [PubMed] [Google Scholar]
- 41.Andreyeva T, Luedicke J, Tripp AS, Henderson KE. Effects of reduced juice allowances in food packages for the women, infants, and children program. Pediatrics 2013;131(5):919–927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.de Hoog ML, Kleinman KP, Gillman MW, Vrijkotte TG, van Eijsden M, Taveras EM. Racial/ethnic and immigrant differences in early childhood diet quality. Public Health Nutr 2014;17(6):1308–1317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Kranz S, Findeis JL, Shrestha SS. Use of the Revised Children's Diet Quality Index to assess preschooler's diet quality, its sociodemographic predictors, and its association with body weight status. J Pediatr (Rio J) 2008;84(1):26–34. [DOI] [PubMed] [Google Scholar]
- 44.Batis C, Hernandez-Barrera L, Barquera S, Rivera JA, Popkin BM. Food acculturation drives dietary differences among Mexicans, Mexican Americans, and Non-Hispanic Whites. J Nutr 2011;141(10):1898–1906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Santiago-Torres M, Kratz M, Lampe JW, Tapsoba Jde D, Breymeyer KL, Levy L, Villasenor A, Wang CY, Song X, Neuhouser ML. Metabolic responses to a traditional Mexican diet compared with a commonly consumed US diet in women of Mexican descent: a randomized crossover feeding trial. Am J Clin Nutr 2016;103(2):366–374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Larsen JK, Hermans RC, Sleddens EF, Engels RC, Fisher JO, Kremers SP. How parental dietary behavior and food parenting practices affect children's dietary behavior. Interacting sources of influence? In: Appetite Vol 89. England: 2015 Elsevier Ltd; 2015:246–257. [DOI] [PubMed] [Google Scholar]
- 47.Elfhag K, Rasmussen F. Food consumption, eating behaviour and self-esteem among single v. married and cohabiting mothers and their 12-year-old children. In: Public Health Nutr Vol 11. England 2008:934–939. [DOI] [PubMed] [Google Scholar]
- 48.Potocka A, Jacukowicz A. Differences in nutritional status of preschool children in the context of the maternal social characteristics. Int J Occup Med Environ Health 2017;30(5):811–821. [DOI] [PubMed] [Google Scholar]
- 49.Grimes CA, Szymlek-Gay EA, Nicklas TA. Beverage Consumption among U.S. Children Aged 0–24 Months: National Health and Nutrition Examination Survey (NHANES). Nutrients 2017;9(3). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Mattei J, Sotres-Alvarez D, Daviglus ML, Gallo LC, Gellman M, Hu FB, Tucker KL, Willett WC, Siega-Riz AM, Van Horn L, Kaplan RC. Diet Quality and Its Association with Cardiometabolic Risk Factors Vary by Hispanic and Latino Ethnic Background in the Hispanic Community Health Study/Study of Latinos. J Nutr 2016;146(10):2035–2044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Mitchell DC, Lawrence FR, Hartman TJ, Curran JM. Consumption of dry beans, peas, and lentils could improve diet quality in the US population. In: J Am Diet Assoc Vol 109. United States 2009:909–913. [DOI] [PubMed] [Google Scholar]
- 52.Anater AS, Catellier DJ, Levine BA, Krotki KP, Jacquier EF, Eldridge AL, Bronstein KE, Harnack LJ, Lorenzana Peasley JM, Lutes AC. The Feeding Infants and Toddlers Study (FITS) 2016: Study Design and Methods. In: J Nutr United States 2018. [DOI] [PMC free article] [PubMed]
- 53.American Academy of Pediatrics, Institute for Healthy Childhood Weight. Building a Foundation for Healthy Active Living https://ihcw.aap.org/Pages/default.aspx. Accessed May 12, 2020.
- 54.Food and Nutrition Service USDoA. Pregnancy and Birth to 24. 2019; https://www.fns.usda.gov/resource/pregnancy-and-birth-24-months. Accessed May 12, 2020.


