Abstract
Older adults with multimorbidities have the highest rate of emergency department (ED) usage. These patients are typically on numerous medications, may have underlying dementia, and often present with falls and delirium. Identifying these high-risk older adults for possible intervention is challenging in the ED setting since available screening methods are manual and resource-intensive. The objective is to study the electronic medical record (EMR) use for identifying high-risk older adults in ED. This feasibility study is conducted in an academic ED with 67 000 total and 24% geriatric (age ≥ 65 years) annual visits, American College of Emergency Physician (ACEP) accredited Level 1 Geriatric Emergency Department with an ED-based geriatric consultation program by incorporating criteria from existing manual geriatric screening instruments and the 4M framework into an automated EMR screen to identify high-risk geriatric patients. ED providers are then alerted by an EMR Best Practice Alert (BPA) if high-risk status is identified. Initial development and impact on geriatric ED consults are reported. During the study period, 7450 patient encounters occurred; 1836 (24.6%) encounters involved patients who were 65 years or older. A total of 1398 (76.1%) high-risk ED encounters resulted in BPA alerts using the EMR automated screen. BPA alerts resulted in 82 (5.9%) geriatric evaluations. We conclude that using the EMR to automate screening for older adults for high-risk geriatric conditions in the ED is feasible. An automated EMR screen with a BPA to ED providers identified a well-defined cohort of older patients appropriate for further ED geriatric evaluation.
Keywords: electronic medical record, automated screening, geriatric emergency department
INTRODUCTION
Older adults are known to have the highest rates of emergency department (ED) use in the United States.1 However, traditional ED models of care, are not always suited for the complex clinical presentation and healthcare needs of these patients.2–4 In addition to age, multiple other risk factors contribute to high ED utilization. Prior research has shown that Multi-morbidity, being on multiple Medications (polypharmacy), impaired Mobility or fall complaints, and change in Mental status (Delirium or Dementia), the 4M framework, often lead to ED visits.1,5–7 Older adults presenting to the ED with these 4M components, have worse health outcomes including iatrogenic complications, prolonged delirium, functional decline, and loss of independence,8 often resulting in high healthcare costs and uneven quality of care.2 These “hazards of hospitalization” coupled with poorer outcomes can then lead to an unfortunate cycle of subsequent repeat ED visits, hospitalization, skilled nursing home admissions, and even long-term care placement.9
Early identification of such patients, when they present to the ED, could potentially prevent this by earlier application of additional resources in the ED or hospital setting (such as early delirium detection and intervention, addressing sensory impairment and dehydration, addressing polypharmacy, or adding resources to optimize mobility). Additional interventions could include exploring alternative options for safe disposition in lieu of hospitalization, such as hospital at home, direct transition to a Skilled Nursing Facility or home rehabilitation, and enhance use of community resources.10–12
Use of geriatric screening instruments may allow early ED-based identification of geriatric patients who are at increased risk for adverse outcomes. Although most existing instruments were derived from discharged ED patients, accurate identification of high-risk patient subsets while in the ED empowers emergency clinicians to alter ED or post-ED trajectories for these vulnerable patients.13 In addition, such risk stratification would allow for more timely and efficient use of time, testing, staff, and resources for those patients most likely to benefit.13
Traditional geriatric ED patient assessment tools, such as Identification of Seniors at Risk (ISAR)14 or the Triage Risk Screening Tool (TRST)15 are often used to identify older patients at risk for adverse outcomes (return to the ED, subsequent short-term hospitalization, functional decline, institutionalization, or death) following an ED visit. These instruments could suggest additional evaluation and potential resource needs.16,17 However, such manual screening tools can be difficult to implement in a high-volume, high-acuity ED setting as they are staff-dependent and labor intensive, typically employing nursing, social work, or case management personnel to interview patients and their caregivers. In addition, these tools are only moderately sensitive in predicting the narrowly selected short-term adverse outcomes13 and were not designed to alert clinicians to the need for a more comprehensive geriatric evaluation.
With the almost universal availability and use of electronic medical records (EMRs),18 it is now possible to leverage structured EMR data elements, bypassing manual screening processes and creating more efficient workflows. In this study, we evaluate whether the risk criteria defined in these traditional screening tools could be identified by the EMR, allowing automated screening of potentially high-risk geriatric ED patients.
METHODS
This was a descriptive feasibility study of the use of EMR screening for high-risk older patients in the setting of a busy urban academic American College of Emergency Physician (ACEP)-accredited Level 1 Geriatric Emergency Department4 with an ED-based geriatric consult program, and 67 000 total annual visits, with 24% geriatric (age ≥ 65) years visits conducted from March 31, 2020 to May 31, 2020.
Subject matter experts from Emergency Medicine, Geriatric Medicine, Nursing, Pharmacy, Case Management, and Social Work used a modified Delphi method, based on review of the literature and professional judgment, to develop criteria to define high-risk geriatric characteristics which can be captured by the EMR.
Prior to EMR screening implementation, ED providers were educated on 8 geriatric domains19 using case series and CME modules and patients aged 65 years and older were screened for delirium at the time of triage using the 4AT20 delirium screen. The 4AT is a brief delirium screening tool with high sensitivity and specificity compared to established delirium tools such as the Confusion Assessment Method (CAM).21
An EMR best-practice alert (BPA) was developed to notify ED providers for high-risk geriatric characteristics defined as: age ≥80 years, fall complaint (Mobility), documented dementia history (Mentation), polypharmacy (≥10 Medications recorded),22 high ED utilization (>5 visits in 1 year), or a (+) 4AT delirium screen (Table 1). This BPA alerted the ED provider if one or more high-risk criteria were present. In addition, the BPA had an embedded link allowing ED providers to place an order for a geriatric evaluation in the ED (Supplementary Figure S1). ED providers could also request a geriatric evaluation, independent of BPA, based on professional judgment.
Table 1.
Automated EMR screening for selected high-risk geriatric characteristics (criteria for BPA trigger)
|
4AT: delirium screening tool; BPA: best practice alert; ED: emergency department.
Charlson Comorbidity Index (CCI),5 was not used as a component for the BPA but was calculated as a surrogate marker for Multi-morbidity.
Frequency of BPA notification and ED geriatric consultations (Comprehensive Geriatric Assessment, CGA) are reported. Data were abstracted from the EMR.
RESULTS
During the study period, 7450 patient encounters occurred; 1836 (24.6%) encounters were in patients 65 years or older. Additional population characteristics and high-risk criteria (excluding age over 80 years) are shown in Table 2. The mean age was 74.6 years and 49.5% were female. Delirium detection by 4AT was approximately 6% in this population. Preexisting dementia was documented in 6.6%. The average number of medications per patient was 8.4. Notably, 18% had more than 5 ED encounters in last the 12 months and the average number of ED encounters per patient during the same time period was 3.66. The average CCI was 3.82, reflective of Multi-Morbid older adults with poor prognosis.
Table 2.
Encounter level data
| Geriatric (age ≥ 65 years) encounters (N = 1836) | |
|---|---|
| Average age at ED encounter (years) | 74.6 |
| Female, n (%) | 909 (49.5) |
| Score 4AT >4 (%) | 5.8 |
| Dementia prevalence (%) | 6.6 |
| >10 medications (%) | 11.1 |
| Fall presentation (%) | 5.6 |
| 5+ encounters last 12 months (%) | 18.1 |
| Average CCI | 3.82 |
4AT: delirium screening tool; CCI: Charlson Comorbidity Index; ED: emergency department.
A total of 1398 (76.1%) geriatric ED encounters resulted in BPA alerts using the EMR automated screen. Four hundred thirty-eight (33.9%) patients did not meet high-risk criteria. BPA alerts resulted in 82 (5.9%) comprehensive geriatric assessments. Fourteen (3.2%) BPA-negative patients were also referred for CGA due to clinical judgment by ED providers. Overall, 96 (5.2%) patients had a CGA. We also examined the proportion of geriatric assessments performed in BPA-positive patients compared to the overall number of CGA obtained. In this group, 82/96 (85.4%) patients who underwent a CGA, were BPA positive.
DISCUSSION
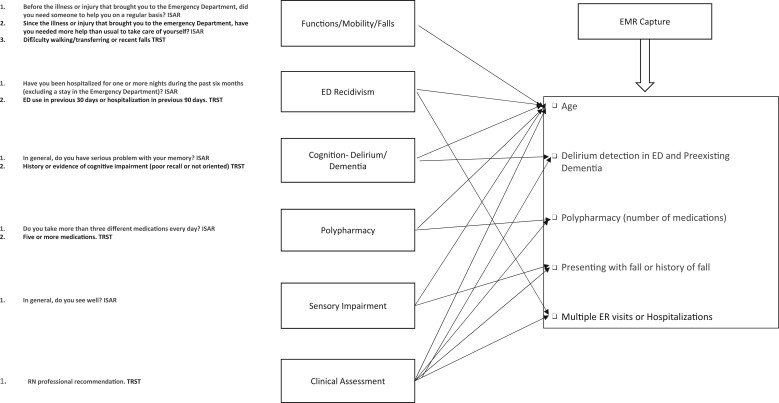
Geriatric screening tools, such as ISAR or TRST, use patient self-report and are typically administered by nursing or ancillary personnel such as case management or social workers. Individual categorical (yes/no) items are manually entered into an EMR and summed. The aim of these tools is to detect functional, cognitive, and sensory impairment, recognize polypharmacy, and document recent hospitalization or ED use. This study shows that similar risk stratification of these important geriatric syndromes,23 defined as the combination of age plus 4Ms for this study, and other health concerns can be achieved with the help of the EMR. Figure 1 illustrates alignment of the selected EMR discrete data elements with ISAR and TRST.
Figure 1.
EMR capture of high-risk geriatric domains and alignment with ISAR and TRST. ISAR: Identification of Senior at Risk; TRST: Triage Risk Screening Tool.
Although the prognostic performance of ISAR in predicting healthcare utilization is not very satisfactory,24 it has been suggested that it has utility in clinical care by risk stratifying patients for further evaluation. Various components of ISAR or TRST can also be used to alert the healthcare team to the need for additional patient evaluation or management. Screening tools, then, could best be used as a standardized adjunct to clinical decision-making.24
The use of a brief geriatric high-risk screening tool followed by a comprehensive geriatric assessment has been shown to best predict health outcomes.25 This 2-step approach has also been shown to reduce the risk of poor health outcomes in older ED patients17 and decrease the risk of hospital admission rates of older patients from the ED or a geriatric ED observation unit.26
Prior to EMR screening and BPA development, ED providers were educated about geriatric domains and delirium screening (4AT) at the time of triage was implemented. Our EMR screening used structured data including patient age, clinical diagnoses, patient problem lists, medication records, and recent healthcare system use in addition to delirium screening results to generate the high-risk BPA. As shown in Supplementary Figure S1, a positive screen resulted in an EMR-based BPA clinical decision support tool banner visible to ED providers that included an embedded link for a geriatric consult evaluation.
The EMR-automated screening process was able to efficiently screen older patients at the time of ED triage. The majority of patients who received a CGA had a positive automated screen and resulting BPA. This would suggest that the EMR screening and BPA were factors in the decision to obtain a more comprehensive geriatric assessment. This also allowed targeted evaluation of higher-risk geriatric patients and more efficient use of available geriatric medicine resources in ED. Examples include patients with polypharmacy requiring medication reconciliation; patients with delirium detection and intervention at the time of triage; patient with dementia who had goals of care discussion or alternate dispositions; patient with falls requiring mobility assessments and intervention for further fall prevention; and high ED utilizers requiring a plan of care and use of social work and case management resources.
Our experience with automated EMR screening demonstrates 2 critical findings from this descriptive study. First, it is feasible to use structured EMR data to identify older adults at risk for poor outcomes during triage, obviating the need for additional resources, such as assigning staff to perform such screening. Second, emergency medicine provider education coupled with increasingly specific EMR-driven “risk-stratified BPA” led to a much narrower and better-defined group of patients who may benefit from a more comprehensive assessment by a Geriatric Medicine provider. Both of these findings are critical for optimizing limited resources for both Emergency Medicine and Geriatric Medicine providers in the high acuity and high-volume ED environment and achievable by leveraging readily available discrete EMR data fields.
Limitations
Limitations to this single-site study include the accuracy of EMR structured data, such as the use of medication lists in assessment of polypharmacy and under-documentation of geriatric syndromes, such as dementia. Although not measured, we suspect such structured EMR data use might be superior to patient recall and self-report. Selection bias for geriatric consults due to provider bias and availability of geriatric medicine providers, and EM practice or process changes during the study period were also possible.
This study also uses the HIMSS Electronic Medical Record Adoption Model (EMRAM) Stage 7. We think that EMRAM stage 6 measures might be needed to effectively use a similar proposed algorithm to identify high-risk geriatric patients in real time.27
With the widespread adoption of EMRs, there is an increased opportunity to collect information on geriatric syndromes and frailty in the clinical setting.28 Recent research has shown potential in the development of EMR-derived frailty indexes.29 Further research efforts should be directed toward optimizing automated geriatric screening by using discrete data elements and emerging technologies such as machine learning30 and natural language processing31 to collect digital biomarkers housed within the EMR to drive geriatric evaluations and examine interventions that could improve outcomes in this vulnerable patient population.
CONCLUSIONS
This single-site study demonstrates that the EMR can be used to screen older ED patients who are at risk for poor outcomes. Using an automated EMR-driven BPA to alert ED providers to high-risk older patients, who can then be referred for further geriatric evaluation, is feasible in the ED. Compared with the labor-intensive nursing or ancillary personnel screening and documentation using patient self-report, an EMR-based automated screening tool is an efficient approach to identifying and prompting geriatric evaluations for high-risk geriatric patients in the ED setting.
Supplementary Material
Contributor Information
Saket Saxena, Center for Geriatric Medicine, Cleveland Clinic, Cleveland, Ohio, USA.
Stephen Meldon, Emergency Service Institute, Cleveland Clinic, Cleveland, Ohio, USA.
Ardeshir Z Hashmi, Center for Geriatric Medicine, Cleveland Clinic, Cleveland, Ohio, USA.
McKinsey Muir, Emergency Service Institute, Cleveland Clinic, Cleveland, Ohio, USA.
Jeffrey Ruwe, Emergency Service Institute, Cleveland Clinic, Cleveland, Ohio, USA.
FUNDING
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
AUTHOR CONTRIBUTIONS
Each author’s contribution to the paper according to the ICMJE guidelines for authorship.
ETHICS APPROVAL
This is an IRB exempted study and no ethics committee approval was needed.
SUPPLEMENTARY MATERIAL
Supplementary material is available at JAMIA Open online.
CONFLICT OF INTEREST STATEMENT
None declared.
DATA AVAILABILITY
The data underlying this article will be shared upon reasonable request to the corresponding author.
REFERENCES
- 1. Aminzadeh F, Dalziel WB.. Older adults in the emergency department: a systematic review of patterns of use, adverse outcomes, and effectiveness of interventions. Ann Emerg Med 2002; 39 (3): 238–47. [DOI] [PubMed] [Google Scholar]
- 2. Lo AX, Flood KL, Biese K, Platts-Mills TF, Donnelly JP, Carpenter CR.. Factors associated with hospital admission for older adults receiving care in U.S. emergency departments. J Gerontol A Biol Sci Med Sci 2017; 72 (8): 1105–9. [DOI] [PubMed] [Google Scholar]
- 3. Lo AX, Biese K.. Disseminating and sustaining emergency department innovations for older adults: good ideas deserve better policies. Acad Emerg Med 2018; 25 (1): 83–4. [DOI] [PubMed] [Google Scholar]
- 4. Southerland LT, Lo AX, Biese K, et al. Concepts in practice: geriatric emergency departments. Ann Emerg Med 2020; 75 (2): 162–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Charlson ME, Carrozzino D, Guidi J, Patierno C.. Charlson Comorbidity Index: a critical review of clinimetric properties. Psychother Psychosom 2022; 91 (1): 8–35. [DOI] [PubMed] [Google Scholar]
- 6. Hein C, Forgues A, Piau A, Sommet A, Nourhashémi F, Vellas B.. Impact of polypharmacy on occurrence of delirium in elderly emergency patients. J Am Med Dir Assoc 2014; 15 (11): 850.e11–850.e15. [DOI] [PubMed] [Google Scholar]
- 7. Saxena S, Hashmi AZ.. COVID-19 in older adults [published online ahead of print September 16, 2021]. Cleve Clin J Med 2021; doi: 10.3949/ccjm.88a.ccc080. [DOI] [PubMed] [Google Scholar]
- 8. Covinsky KE, Palmer RM, Fortinsky RH, et al. Loss of independence in activities of daily living in older adults hospitalized with medical illnesses: increased vulnerability with age. J Am Geriatr Soc 2003; 51 (4): 451–8. [DOI] [PubMed] [Google Scholar]
- 9. Creditor MC. Hazards of hospitalization of the elderly. Ann Intern Med 1993; 118 (3): 219–23. [DOI] [PubMed] [Google Scholar]
- 10. Gonçalves-Bradley DC, Iliffe S, Doll HA, et al. Early discharge hospital at home. Cochrane Database Syst Rev 2017; 6: CD000356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Williams S, Morrissey AM, Steed F, et al. Early supported discharge for older adults admitted to hospital with medical complaints: a systematic review and meta-analysis. BMC Geriatr 2022; 22 (1): 302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Bambach K, Southerland LT.. Applying geriatric principles to transitions of care in the emergency department. Emerg Med Clin North Am 2021; 39 (2): 429–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Carpenter CR, Shelton E, Fowler S, et al. Risk factors and screening instruments to predict adverse outcomes for undifferentiated older emergency department patients: a systematic review and meta-analysis. Acad Emerg Med 2015; 22 (1): 1–21. [DOI] [PubMed] [Google Scholar]
- 14. McCusker J, Bellavance F, Cardin S, Trépanier S, Verdon J, Ardman O.. Detection of older people at increased risk of adverse health outcomes after an emergency visit: the ISAR screening tool. J Am Geriatr Soc 1999; 47 (10): 1229–37. [DOI] [PubMed] [Google Scholar]
- 15. Meldon SW, Mion LC, Palmer RM, et al. A brief risk-stratification tool to predict repeat emergency department visits and hospitalizations in older patients discharged from the emergency department. Acad Emerg Med 2003; 10 (3): 224–32. [DOI] [PubMed] [Google Scholar]
- 16. Dendukuri N, McCusker J, Belzile E.. The identification of seniors at risk screening tool: further evidence of concurrent and predictive validity. J Am Geriatr Soc 2004; 52 (2): 290–6. [DOI] [PubMed] [Google Scholar]
- 17. McCusker J, Verdon J, Tousignant P, De Courval LP, Dendukuri N, Belzile E.. Rapid emergency department intervention for older people reduces risk of functional decline: results of a multicenter randomized trial. J Am Geriatr Soc 2001; 49 (10): 1272–81. [DOI] [PubMed] [Google Scholar]
- 18. Parasrampuria S, Henry J. Hospitals’ Use of Electronic Health Records Data, 2015-2017. https://www.healthit.gov. https://www.healthit.gov/sites/default/files/page/2019-04/AHAEHRUseDataBrief.pdf. Accessed December 19, 2022.
- 19. Hogan TM, Losman ED, Carpenter CR, et al. Development of geriatric competencies for emergency medicine residents using an expert consensus process. Acad Emerg Med 2010; 17 (3): 316–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Gagné AJ, Voyer P, Boucher V, et al. Performance of the French version of the 4AT for screening the elderly for delirium in the emergency department. Can J Emerg Med 2018; 20 (6): 903–10. [DOI] [PubMed] [Google Scholar]
- 21. Shenkin SD, Fox C, Godfrey M, et al. Delirium detection in older acute medical inpatients: a multicentre prospective comparative diagnostic test accuracy study of the 4AT and the confusion assessment method. BMC Med 2019; 17 (1): 138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Charlesworth CJ, Smit E, Lee DSH, Alramadhan F, Odden MC.. Polypharmacy among adults aged 65 years and older in the United States: 1988–2010. J Gerontol A Biol Sci Med Sci 2015; 70 (8): 989–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Inouye SK, Studenski S, Tinetti ME, Kuchel GA.. Geriatric syndromes: clinical, research, and policy implications of a core geriatric concept. J Am Geriatr Soc 2007; 55 (5): 780–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Edmans J, Bradshaw L, Gladman JRF, et al. The Identification of Seniors at Risk (ISAR) score to predict clinical outcomes and health service costs in older people discharged from UK acute medical units. Age Ageing 2013; 42 (6): 747–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Scharf AC, Gronewold J, Dahlmann C, et al. Health outcome of older hospitalized patients in internal medicine environments evaluated by Identification of Seniors at Risk (ISAR) screening and geriatric assessment. BMC Geriatr 2019; 19 (1): 221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Meldon S, Saxena S, et al. The effect of geriatric consultation on admission rates of older patients in the emergency department. Ann Emerg Med 2020; 76 (4): S140. [Google Scholar]
- 27. Electronic Medical Record Adoption Model (EMRAM) | HIMSS. https://www.himss.org/what-we-do-solutions/digital-health-transformation/maturity-models/electronic-medical-record-adoption-model-emram?gclid=Cj0KCQiA14WdBhD8ARIsANao07g30rinMGSYcj-ajcHNxMOoQlkzCJKRHgRnO1qHtLonTyaOLUH5FbMaAgzEEALw_wcB. Accessed December 20, 2022.
- 28. Rockwood K. Screening for grades of frailty using electronic health records: where do we go from here? Age Ageing 2016; 45 (3): 328–9. [DOI] [PubMed] [Google Scholar]
- 29. Clegg A, Bates C, Young J, et al. Development and validation of an electronic frailty index using routine primary care electronic health record data. Age Ageing 2016; 45 (3): 353–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Yadgir Mph SR, Engstrom C, Jacobsohn GC, et al. Machine learning-assisted screening for cognitive impairment in the emergency department. J Am Geriatr Soc 2022; 70 (3): 831–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Patra BG, Sharma MM, Vekaria V, et al. Extracting social determinants of health from electronic health records using natural language processing: a systematic review. J Am Med Inform Assoc 2021; 28 (12): 2716–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data underlying this article will be shared upon reasonable request to the corresponding author.