Abstract
Isometric handgrip or (wall) squat exercise performed three times per week produces reductions in systolic blood pressure (SBP) in adults with hypertension. We aimed to compare these interventions and the potential to retain benefits with one exercise session per week. We compared blood pressure changes following handgrip and squat isometric training interventions with controls in a randomized controlled multicentre trial in 77 unmedicated hypertensive (SBP ≥ 130 mmHg) adults. Exercise sessions were performed in the workplace and consisted of four repetitions—three sessions per week for the first 12 weeks (phase 1), and one session per week for the subsequent 12 weeks (phase 2). Office blood pressure (BP) was measured at baseline, post‐phase 1 and post‐phase 2. Post‐phase 1, mean reductions in SBP were significantly greater in handgrip (–11.2 mmHg, n = 28) and squat (–12.9 mmHg, n = 27) groups than in controls (–.4 mmHg; n = 22) but changes in DBP were not. There were no significant within‐group changes during phase 2 but SBP was 3.8 mmHg lower in the wall squat than the handgrip group—a small magnitude but clinically important difference. While both interventions produced significant SBP reductions, the wall squat appears to be more effective in maintaining benefits with a minimal training dose. The low time investment to achieve and retain clinically significant SBP reductions—42 and 12 min, respectively—and minimal cost, particularly of the wall squat, make it a promising intervention for delivery in public health settings.
Keywords: exercise/hypertension, handgrip, isometric, wall squat
1. INTRODUCTION
Hypertension (HTN) affects 1.39 billion individuals worldwide. 1 It is one of the most significant modifiable risk factors for cardiovascular diseases (e.g., coronary artery disease, stroke, and heart failure), the leading cause of death worldwide, and the third leading cause of disability‐adjusted life years lost. 2 Guidelines for the management of elevated BP recommend non‐pharmacologic lifestyle modifications as the first line of treatment, with physical activity levels as a key component. 3
As a lack of time is cited as one of the major barriers to participation in physical activity/exercise, 4 low time‐cost exercise, effective in reducing BP is of interest from a compliance/adherence perspective. Evidence has accumulated demonstrating that low intensity isometric resistance training (IRT) involving a total time investment of up to 14 min per session, performed three times per week can produce clinically and statistically significant reductions in systolic blood pressure (SBP) and diastolic blood pressure (DBP) in people with hypertension. 5 , 6 These interventions, identified in a meta‐analysis as being superior to aerobic exercise or dynamic resistance training in reducing BP have mainly been implemented using a handgrip dynamometer or resistance device, 7 with three to four repetitions (reps) of 2‐min isometric contractions at 30% of the individual's maximum handgrip strength completed. 6 , 7 , 8
While the majority of IRT interventions in people with hypertension have examined handgrip exercise, several studies have examined the effect of instead using the wall squat, a lower equipment cost, lower body, alternative. 9 Remarkably, a wall squat intervention 10 using the same 4 × 2 min, three session per week protocol for only 4‐weeks showed BP reductions of similar magnitude as that reported following handgrip interventions of longer duration. However, the efficacy of handgrip training has not been compared with that of wall squat training within a sample of adults with hypertension. This comparison is important because on the one hand, the lower cost associated with implementing wall squat training makes it more feasible to scale and make accessible to large numbers of people with hypertension. On the other hand, the far larger body of evidence demonstrating the efficacy of handgrip exercise might favor its prescription. 5 , 6 , 8 , 9 Another aspect of the IRT program that has yet to be examined is a change in training frequency—all wall squat and handgrip studies to date involve at least three sessions per week. If BP reductions achieved with this frequency could be maintained with a lower frequency (and therefore lower time investment), as has been demonstrated with respect to other adaptations to exercise, 11 this might enhance long‐term compliance.
Therefore, the principal aims of this randomized controlled trial delivered within the workplace during the working day to adults with hypertension, were as follows: (1) to compare the effects of handgrip and wall squat training on office measured BP after a 12‐week 3 sessions per week training protocol (phase 1); and (2) to examine BP changes following a subsequent 12‐week, once per week “maintenance” protocol (phase 2).
2. METHODOLOGY
2.1. Study design
The study was a parallel randomized controlled multi‐centre clinical trial. Adults were recruited across seven businesses and clinics in the cities of Bucaramanga and Barranquilla, Colombia. The inclusion criteria for the present analysis, were as follows: aged between 35 and 65 years, individuals with a SBP of >130 mmHg (the 2017 American College of Cardiology/American Heart Association cut‐point for HTN), 3 but had not been prescribed medication for the condition. The sample therefore included individuals who were not aware that they were hypertensive. Inclusion and exclusion criteria are shown in Figure 1. All participants were provided with, and signed informed consent and were told that they were free to withdraw at any time. Power analysis determined that with the inclusion of 144 individuals across the control and two intervention groups, with a type I error (α) of 5%, power (1‐β) of 90%, a mean difference of 6 mmHg (±9 mmHg) SBP between control and intervention groups. Based on the final sample size of the 77 non‐medicated hypertensive participants, the study had an α of 5% and a power of 99%.
FIGURE 1.
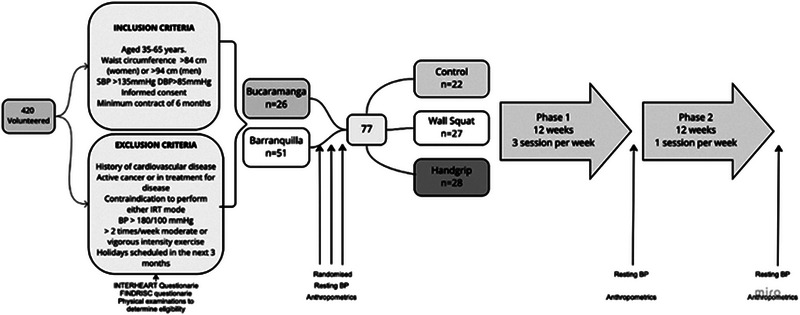
Study flow diagram summarizing recruitment, inclusion/exclusion criteria, randomization, and timing of measurements.
2.2. Measurements
All potential participants were interviewed at their workplace to obtain their medical history and sociodemographic data. Using an automatic device (OMRON HEM 705 CP, Tokyo, Japan) BP was measured following the recommendations of the British Hypertension Society and repeated after sitting for a further 5–10 min with the mean used as day 1 BP. Day 2 BP was taken when this procedure was repeated 2 to 3 days later when body composition was also assessed, with bioimpedance analysis (Ironman, BC‐554, Hawaii, USA), and waist circumference. Maximal isometric handgrip strength was then assessed with a handgrip dynamometer (JAMAR, Model J00105, Lafayette Instrument Company, USA) in a seated position.
For most participants, the mean of day 1 and day 2 BP measurements was used to determine inclusion and as the baseline value for those randomized. However, if day 1 and day 2 values differed by >10 mmHg, a third‐day measure was taken (on the first day of the intervention but prior to the training session), and a mean of these 3 days was used instead. Participants with SBP values >160 mmHg were encouraged to seek a medical appointment for treatment, whereas those with between 130 and 160 mmHg SBP were directed to the 4 × 4 recommendation, 12 a national strategy based on WHO guidelines for lifestyle intervention and includes video and written material in Spanish.
Wall squat performance was then evaluated with the participant in a squat position with their back against the wall, arms crossed on the chest (Figure 2A) and feet at shoulder width, 95° of knee flexion (measured using a goniometer at the level of the knee joint). 13
FIGURE 2.

(A) Position for initial wall squat evaluation (B) Wall squat training @95° (C) Handgrip training.
The participant was asked to try and maintain this position for 2 min. If they could not do so the time (seconds) at which participants voluntarily ended the test was recorded. At end of the test, participants were asked to provide a rating of perceived effort using the modified Borg scale.
3. INTERVENTION
During phase 1, individuals in both intervention groups performed their exercise supervised by qualified physiotherapists who contacted the participants and met them in their office (Figure 2B,C) or work area at scheduled times.
3.1. Handgrip group (n = 28)
Participants randomized to the handgrip group performed four reps of a 2‐min isometric contraction with 2 min of rest between each rep. For the 2‐min duration of each rep, participants produced and sustained a force value of 30% of handgrip strength. For the first 4 weeks this value was calculated using the maximum value they had achieved in the initial baseline measurement. After the first 4 weeks and then every 4 weeks thereafter, maximal isometric handgrip strength was re‐evaluated using the protocol described above, and the 30% value used in the exercise training session adjusted if this value changed. This training was performed using a digital hand dynamometer (Zhongshan Camry Electronic Co. Ltd. Zhongshan Guangdong, China), with real‐time feedback of force (kg) being applied and displayed on an LCD screen allowing the physiotherapist to ensure that the target value was being maintained.
3.2. Wall squat group (n = 27)
This group also performed four reps of 2 min with 2 min rest between each rep but instead, this consisted of maintaining a squat position with their back against the wall as described above for the initial wall squat test. The knee joint angle was set using a fixed goniometer fastened with Velcro to the thigh and leg (Figure 2A). Between each set participants were given 2 min of rest while seated.
We assigned wall squat group participants to one of two standardized program progressions based on an initial assessment of their ability to sustain the wall squat position at a knee joint angle of 95° for 2 min, or not. Those that were able to do so performed the exercise at 125° for the first 3 weeks of the intervention, 115° for weeks 4–6, 105° for weeks 7–9, and 95° for weeks 10–12. Those that were unable to do so performed the exercise at 135° for weeks 1–2 of the intervention, 125° for weeks 3–4, 115° for weeks 5–6, 105° for weeks 7–9, and 95° for weeks 10–12. As there is a curvilinear relationship between these joint angles and heart rate response (greater knee flexion is associated with a higher HR) 13 wall squat intensity progressively increased during phase 1 for all participants. In phase 2, during the single weekly session, all participants performed the exercise at 95°.
3.3. Control group (C) (n = 22)
The control group was involved in the same pre‐ and post‐study 3‐month BP, anthropometric, body composition, handgrip, and wall squat assessments but did not undertake any isometric training. They were however provided via e‐mail with a link to the 4 × 4 recommendations for healthy lifestyles referred to above.
3.4. Statistical analysis
An ANCOVA was used to evaluate potential intergroup differences in BP (adjusted for baseline values) between baseline and end of phase 1 and between baseline and the end of phase 2, respectively. Partial eta squared (η2), was used to quantify magnitude of effect size differences in this analysis with a small effect indicated by η2 = .01; a medium effect=; η2 = .06 and η2 = .14 a large effect. We also assessed the significance and magnitude of within‐group changes in BP using paired samples t‐tests. The magnitude of between and within group change was quantified using Cohen d’s effect size, 14 with values classified as follows: <.2 trivial, .2–.5 small, .5–.8 moderate, .8–1.2 large, >1.2 very large.
4. RESULTS
The 77 non medicated people with hypertension who were recruited, randomized and assessed at baseline all completed both phases of the intervention and completed all training sessions, with no adverse events reported. The mean age of the sample was 44.9 (±9.6) and 67% were male. Anthropometric measures and lean body mass are shown in supplemental material/appendix. Mean SBP and DBP at baseline, post‐phase 1 and post‐phase 2 are shown in Table 1 and Figure 3.
TABLE 1.
Blood pressure at baseline, post phase 1 and post phase 2.
| CONTROL (n = 22) | HANDGRIP (n = 28) | WALL SQUAT (n = 27) | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Pre | Post P1 | p ES | Post P2 | p ES | Pre | Post P1 | p ES | Post P2 | p ES | Pre | Post P1 | p ES | Post P2 | p ES | |
| SBP |
138.9 (6.4) |
138.5 (12.6) |
.86 .04 |
139.4 (13.9) |
.69 0.06 |
140.0 (7.4) |
128.8 (12.5) |
<0.001 1.09 |
129.3 (13.5) |
.74 .03 |
141.2 (7.4) |
128.3 (10.0) |
<0.001 1.46 |
126.5 (9.2) |
.34 .19 |
| DBP |
86.0 (4.6) |
85.1 (6.5) |
.52 .15 |
85.0 (7.6) |
.95 .01 |
86.7 (4.6) |
82.7 (8.2) |
<0.001 .60 |
81.6 (8.8) |
.38 .12 |
87.0 (4.7) |
82.9 (9.1) |
.03 0.56 |
80.4 (9.1) |
.09 .27 |
Note: P1, Phase 1; P2, Phase 2. p and effect size are based on within‐group changes between baseline and end of P1, and P1 and between end of P1 and end of P2, respectively.
Bold script indicates a significant within group change.
FIGURE 3.
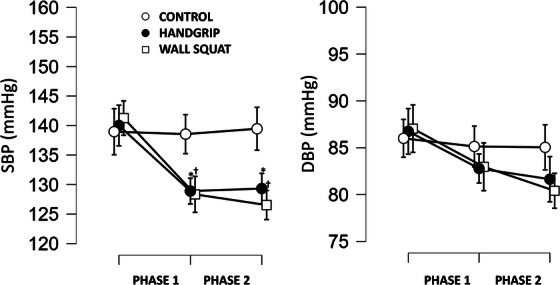
Systolic blood pressure (SBP) and diastolic blood pressure (DBP) mean and 95% confidence intervals by group at baseline, post phase 1 and post phase 2. Mean and 95% confidence intervals by group pre intervention, post phase 1 and post phase 2 for systolic blood pressure (SBP) and diastolic blood pressure (DBP). * Indicates significant difference between pre intervention and post phase one. † Indicates significant difference between pre intervention and post phase 2.
There were significant large and very large magnitude decreases in SBP between baseline and post phase 1, in the handgrip and wall squat groups respectively and significant moderate magnitude decreases in DBP in both intervention groups.
Comparing BP between groups at baseline versus post phase 1 (ANCOVA adjusted for baseline values), there were significant, large magnitude differences between groups in SBP (p < .001, F = 7.9, η2 = .156) and small magnitude, non‐significant differences in DBP (p = .366, F = 1.019, η2 = .024). Post hoc analysis (Table 2) revealed large magnitude, significant differences in SBP between the handgrip and control groups and very large magnitude, significant differences between the wall squat and the control.
TABLE 2.
Between group differences in blood pressure after phase 1 and phase 2
| PHASE 1 | PHASE 2 | |||||||
|---|---|---|---|---|---|---|---|---|
| SBP Mean (95% CI) | p/ES | DBP Mean (95% CI) | p/ES | SBP Mean (95% CI) | p/ES | DBP Mean (95% CI) | p/ES | |
| CONTROL vs. HANDGRIP |
10.3 (2.8 to 17.8) |
.004 * .819 |
2.8 (–2.5 to 8.1) |
.418 .369 |
10.9 (3.3 to 18.5) |
.003 * .797 |
3.9 (–1.7 to 9.5) |
.224 .466 |
| CONTROL vs. WALL SQUAT |
11.7 (4.1 to 19.3) |
<.001 † 1.03 |
2.8 (–2.5 to 8.1) |
.427 .345 |
14.7 (6.8 to 22.4) |
<.001 † 1.26 |
5.3 (–.32 to 11.) |
.068 .622 |
| HANDGRIP vs. WALL SQUAT |
1.4 (–5.7 to 8.4) |
.89 .119 |
–.01 (–5.0 to 5.0) |
1 0.001 |
3.75 (–3.5 to 11.0) |
.432 .323 |
1.4 (–3.8 to 6.7) |
.795 .158 |
Abbreviations: SBP, systolic blood pressure; DBP, diastolic blood pressure; ES, effect size.
* = p < .01; † = p < .001 for difference between groups at end of phase compared to baseline (ANCOVA adjusted for baseline values).
Bold script indicates a significant within group change.
There were no significant changes within any group (Table 1) between post phase 1 and phase 2. Comparing post‐phase 2 with baseline, there were significant differences between groups in SBP (p = <.001, F = 10.9, η2 = .194). Post‐hoc analysis (Table 2) showed significant differences of moderate magnitude between handgrip and controls and of very large magnitude between wall squat and control groups. There was also a small magnitude, non‐significant difference between handgrip and wall squat groups post phase 2. Table 2 also shows between group differences in DBP were of moderate magnitude, but non‐significant (p = .076, F = 2.67, η2 = 0.06) with post hoc analysis showing a moderate magnitude difference between wall squat and control and a small magnitude difference between handgrip and control groups.
There were no significant within group changes or between group differences in body weight, BMI, waist circumference or lean body mass (Table: supplementary material)
5. DISCUSSION
The present study confirms previous findings demonstrating significant 11.2–12.9 mmHg reductions in SBP in adults with hypertension following three times per week isometric resistance training, changes which compare favorably with the average SBP reduction (9.1 mmHg SBP) with a single, standard dose antihypertensive drug. 15 , 16 We also present some important novel findings. This is the first study to compare the BP reducing effects of isometric handgrip and wall squat exercise training. Following the initial 12‐week training phase, the two modes of IRT led to similar, clinically and statistically significant reductions in office‐measured SBP. However, after phase 2, during which training frequency was reduced to 1 session per week, in the handgrip group SBP increased by .5 mmHg, while there was a further 1.8 mmHg decline in the wall squat group, representing a small magnitude but clinically relevant 3.8 mmHg greater SBP reduction in the wall squat group over the whole intervention–which aligns with the estimated >3 mmHg difference favoring wall squat over handgrip training in a recent meta‐analysis. 17
The present study is the first to examine whether reductions achieved with the standard three times per week intervention can be retained with a reduced training frequency or “maintenance dose.” While a weekly single session of wall squat exercise not only maintains, but potentially continues to promote SBP reductions, handgrip exercise begins to show a reversal of gains and may require a higher frequency to sustain the benefits achieved. The larger muscle mass recruited and therefore area of vascular occlusion during the wall squat exercise 17 might explain its ability to maintain adaptations at a lower frequency of training.
5.1. Blood pressure changes‐phase 1
We observed reductions in SBP of lower magnitude to that reported in medicated participants following a 12‐week handgrip intervention using the same protocol, 18 but higher than determined by meta‐analyses which also included non‐supervised and shorter intervention durations—both associated with smaller BP reductions. 5 , 6 , 8 There are few wall‐squat intervention studies relative to the substantial literature examining isometric handgrip training. During phase 1, reductions in SBP were of larger magnitude (although not significantly) in the wall squat group than in the handgrip group and of similar magnitude as the only previous study of wall squat in unmedicated adults with hypertension. 10 That study found office measured SBP and DBP reductions of 12.4 and 6.2 mmHg, respectively, after 4‐weeks of three exercise sessions/week.
While SBP benefits were large and robust in both IRT groups and despite significant, moderate magnitude reductions within both intervention group during phase 1, maintained during phase 2, DBP reductions were not significantly different from that of the controls at the end of either phase. However, significant DBP reductions are not a consistent finding of handgrip studies, 6 , 18 and it is SBP control that is critical to cardiovascular health outcomes/mortality with reductions associated with reduced cardiovascular mortality. 10
5.2. Blood pressure changes‐Phase 2
The present study is the first to evaluate whether an IRT “maintenance dose” can be used to maintain BP reductions obtained with a three sessions per week protocol. Taylor et al. 10 demonstrated that BP reductions achieved during a 4‐week, three session per week wall squat intervention in adults with hypertension had returned to pre intervention values after a 3‐week “washout” (training cessation) period. We found that clinically and statistically significant SBP reductions achieved in phase 1 were largely retained with only a single session per week, a time commitment even easier to adhere to, likely to enhance long term compliance. Although our study involved supervised sessions within the workplace, and partly took place during the difficult conditions associated with the COVID‐19 pandemic, no participant dropped out with 100% compliance to the 3 sessions, and then 1 session per week program.
While our phase 2 findings show maintenance of adaptations, they do not indicate that significant reductions in BP could be achieved with a single weekly session of IRT. However, a single weekly session of dynamic resistance training can stimulate strength development 20 and epidemiological evidence suggests that significant diabetes and cardiovascular risk reduction is achieved with participation in once‐a‐week training strength training. 21 The only previous study examining dose‐response of IRT compared 3 versus 5 handgrip training sessions per week, finding no significant difference in SBP reduction. 22 Future research should examine the degree to which lower frequency IRT (1‐2 sessions per week) can promote BP reduction.
The minimal equipment requirement and associated cost of wall squat training make it a more scalable and widely applicable prescription for unsupervised home and/or work‐based training IRT than handgrip exercise. We used a relatively economic dynamometer (approximately $50), purchasing several devices which were shared within each workplace. While affordable to an institution, in a public health setting it may still be a prohibitively expensive to provide patients with dynamometers, particularly within the budget constraints of low‐middle income country (LMIC's). This is an important consideration as the burden of hypertension and other cardiometabolic disease is larger in LMIC than in high income countries. 2 Based on our findings and other recent evidence, 10 , 17 the wall squat appears to therefore provide the best cost‐benefit in BP in hypertensives and is well tolerated, well adhered to and with no reports of adverse events in the present or previous wall squat interventions. Indeed, no dropouts and a 77% compliance with exercise sessions was reported in a recent year‐long‐wall squat intervention. 23 Nonetheless, handgrip exercise may be an important alternative for individuals with knee pain or pathologies.
A limitation of our study is the office rather than ambulatory blood pressure measures, the latter considered the gold standard. 24 However, Taylor et al. 10 reported very similar reductions in 24‐h ambulatory and office BP measures, and of similar magnitude as observed in the present study, indirectly validating our office BP observations. Another potential limitation of the wall squat arm of our study was the use of a pragmatic approach to reduce the time cost of stratifying participants, whereby according to their performance in a 95° wall squat test, participants began the program at either of the two easiest joint angles, with intensity (angle) progressed every 2–3 weeks during phase 1. This provided a crude stratification of baseline ability to perform the exercise. It also meant that for a number of participants, it was likely that during the early weeks of the intervention the intensity was below that necessary to stimulate adaptations. In contrast, Wiles and colleagues incremental wall squat test identifies the baseline training angle associated with 95% HR peak in each participant with HR measured during the last 30 s of 2‐min tests at progressively greater knee flexion angles, starting at 135°. 13 , 25 This individualized approach to identify the training angle used throughout a 4‐week intervention 10 also ensures that each participant is physiologically challenged from the start of the program. It is also time‐consuming when delivered to a large sample. Our pragmatic stratification was conceived as a less time‐consuming practical alternative that also implemented standardized progressive loading across phase 1 to compensate for the built in underloading during the initial weeks of the intervention. This early underloading may explain why Taylor et al. 10 achieved a similar magnitude SBP reduction in 4 weeks of wall squat as we observed in 12 weeks. Nonetheless, our approach, allowing participants a period of accommodation to this novel exercise before challenging them, may be beneficial from a self‐efficacy and comfort perspective. Lastly, the greater attention/contact that the intervention groups received may also have contributed to the beneficial trends of IRT, although a previous study which compared wall squat with a sham wall squat (inadequate intensity) only demonstrated BP reductions in the “true” intervention group suggesting that the effects are specific to the exercise itself. 26
While we did not evaluate physiological parameters which might explain the SBP reductions observed, a recent meta‐analysis concluded that the principal driver of IRT induced BP reduction is reduced total peripheral resistance, potentially mediated through enhanced autonomic vasomotor control. Changes in cardiovascular function including significantly decreased heart rate and increased stroke volume (with stable cardiac output) are also consistently reported. 17
Importantly, from an adherence perspective, IRT overcomes one of the most cited barriers to exercise participation—lack of time—and reduces barriers to implementation associated with equipment costs. It can be performed with limited space, at home or in the workplace, without even requiring a change of clothes. IRT also represents an alternative to aerobic exercise for those who are unable to adopt that form of exercise or an adjunct to it. 27
The feasibility of scaling of the wall squat intervention in a public health setting has begun to be examined in the United Kingdom, 28 and such scaling should also be examined in other LMIC regions with lower healthcare budgets. Finally, longitudinal studies of sufficient duration are needed to examine the ability of IRT to impact on HTA progression and cardiovascular events in people with hypertension.
6. CONCLUSION
Our study is the first to compare the BP reducing effects of the two most well researched and potentially applicable IRT protocols, in adults with hypertension. The large decreases in SBP we observed aligns with previous studies and provides further evidence to support the prescription of IRT to hypertensive individuals. Three sessions per week of wall squat and handgrip produce comparable SBP reductions. We also showed that SBP reductions are largely maintained after 3 months of single session per week training, but the wall squat appears to better retain benefits with this minimal dose of training—with important implications for longer term adherence. The effectiveness of this dose—12 min of time investment—should be confirmed in future longer duration studies and in unsupervised interventions. Future research should also determine whether initial benefits can also be achieved with lower frequency training interventions involving 1 or 2 sessions per week, to better define the minimum effective dose.
AUTHOR CONTRIBUTIONS
Daniel Dylan Cohen: Concept and design of study, preparation of manuscript. Gustavo Aroca Martinez: Leader of Barranquilla site delivery, review of manuscript. Javier Carreño‐Robayo: Operational leader of Bucaramanga intervention delivery, study design, review of manuscript. Alvaro Castañeda‐Hernández: Operations Bucaramanga intervention. Yaneth Herazo Beltran: Operations Barranquilla intervention. Paul Camacho‐López: Assistance with study design and operations Bucaramanga intervention. Johanna Otero: Assistance with study design and statistics. Daniel Martinez‐Bello: Statistical expertise. Jose P. Lopez‐Lopez: Review of manuscript. Patricio Lopez‐Jaramillo: Study design and lab director Bucaramanga, review of manuscript.
CONFLICT OF INTEREST
The authors report no conflict of interest.
PATIENT CONSENT STATEMENT
All participants provided written consent.
Supporting information
Supporting Information
ACKNOWLEDGMENT
The study was funded by the Ministerio de ciencia tecnología e innovación. Colciencias (the Colombian Ministry of Science). Grant number: 807–18, contract number: 759–18.
Cohen DD, Aroca‐Martinez G, Carreño‐Robayo J, et al. Reductions in systolic blood pressure achieved by hypertensives with three isometric training sessions per week are maintained with a single session per week. J Clin Hypertens. 2023;25:380–387. 10.1111/jch.14621
Clinical trial registration: Unique Protocol ID: 129980764353
REFERENCES
- 1. Forouzanfar MH, Liu P, Roth GA, et al. Global burden of hypertension and systolic blood pressure of at least 110 to 115 mm Hg, 1990–2015. JAMA. 2017;317(2):165‐182. [DOI] [PubMed] [Google Scholar]
- 2. Yusuf S, Joseph P, Rangarajan S, et al. Modifiable risk factors, cardiovascular disease, and mortality in 155 722 individuals from 21 high‐income, middle‐income, and low‐income countries (PURE): a prospective cohort study. Lancet. 2019;395(10226):795–808. pii: S0140‐6736(19)32008‐32002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Whelton PK, Carey RM, Aronow WS, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American College of Cardiology/American Heart Association Task Force on clinical practice guidelines. J Am Coll Cardiol. 2018;71:e127‐e248. [DOI] [PubMed] [Google Scholar]
- 4. Gee ME, Bienek A, Campbell NR, et al. Prevalence of, and barriers to, preventive lifestyle behaviors in hypertension (from a national survey of Canadians with hypertension). Am J Cardiol. 2012;109(4):570‐575. [DOI] [PubMed] [Google Scholar]
- 5. Bentley DC, Nguyen CH, Thomas SG. Resting blood pressure reductions following handgrip exercise training and the impact of age and sex: a systematic review and narrative synthesis. Syst Rev. 2018;7(1):229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Loaiza‐Betancur AF, Chulvi‐Medrano I. Is low‐intensity isometric handgrip exercise an efficient alternative in lifestyle blood pressure management? A systematic review. Sports Health. 2020;12(5):470‐477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Cornelissen VA, Smart NA. Exercise training for blood pressure: a systematic review and meta‐analysis. J Am Heart Assoc. 2013;2(1):e004473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Smart NA, Way D, Carlson D, et al. Effects of isometric resistance training on resting blood pressure: individual participant data meta‐analysis. J Hypertens. 2019;37(10):1927‐1938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Wiles JD, Goldring N, Coleman D. Home‐based isometric exercise training induced reductions resting blood pressure. Eur J Appl Physiol. 2017;117(1):83‐93. [DOI] [PubMed] [Google Scholar]
- 10. Taylor KA, Wiles JD, Coleman DA, et al. Neurohumoral and ambulatory haemodynamic adaptations following isometric exercise training in unmedicated hypertensive patients. J Hypertens. 2019;37(4):827‐836. [DOI] [PubMed] [Google Scholar]
- 11. Rønnestad BR, Nymark BS, Raastad T. Effects of in‐season strength maintenance training frequency in professional soccer players. J Strength Cond Res. 2011;25(10):2653‐6015. [DOI] [PubMed] [Google Scholar]
- 12. Normatividad ‐ Ministerio de Educación Nacional de Colombia [Internet]. Accessed Sept 19th 2019, available: https://www.mineducacion.gov.co/1759/w3‐propertyvalue‐51455.html
- 13. Wiles JD, Allum SR, Coleman DA, Swaine IL. The relationships between exercise intensity, heart rate, and blood pressure during an incremental isometric exercise test. J Sports Sci. 2008;26(2):155‐162. [DOI] [PubMed] [Google Scholar]
- 14. Cohen J. Statistical power analysis for the behavioral sciences. Routledge Academic; 1988. [Google Scholar]
- 15. Law MR, Morris JK, Wald NJ. Use of blood pressure lowering drugs in the prevention of cardiovascular disease: meta‐analysis of 147 randomised trials in the context of expectations from prospective epidemiological studies. BMJ. 2009;338:b1665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Zanchetti A. Randomized controlled trials of blood pressure lowering in hypertension: a critical reappraisal. Circ Res. 2015;116(6):1058‐1073. [DOI] [PubMed] [Google Scholar]
- 17. Edwards JJ, Wiles J, O'Driscoll J. Mechanisms for blood pressure reduction following isometric exercise training: a systematic review and meta‐analysis. J Hypertens. 2022;40(11):2299‐2306. [DOI] [PubMed] [Google Scholar]
- 18. Palmeira AC, Farah BQ, Silva GOD, et al. Effects of isometric handgrip training on blood pressure among hypertensive patients seen within public primary healthcare: a randomized controlled trial. Sao Paulo Med J. 2021;139(6):648‐656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Lonn EM, Bosch J, López‐Jaramillo P, et al. Blood‐Pressure lowering in intermediate‐risk persons without cardiovascular disease. N Engl J Med. 2016;374(21):2009‐2009‐2010. [DOI] [PubMed] [Google Scholar]
- 20. Ralston GW, Kilgore L, Wyatt FB, Buchan D, Baker JS. Weekly training frequency effects on strength gain: a meta‐analysis. Sports Med Open. 2018;4(1):36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Shiroma EJ, Cook NR, Manson JE, et al. Strength training and the risk of type 2 diabetes and cardiovascular disease. Med Sci Sports Exerc. 2017;49(1):40‐46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Badrov MB, Bartol CL, DiBartolomeo MA, et al. Effects of isometric handgrip training dose on resting blood pressure and resistance vessel endothelial function in normotensive women. Eur J Appl Physiol. 2013;113(8):2091‐2091‐2100. [DOI] [PubMed] [Google Scholar]
- 23. O'Driscoll JM, Edwards JJ, Coleman DA, et al. One year of isometric exercise training for blood pressure management in men: a prospective randomized controlled study. J Hypertens. 2022;40(12):2406‐2412. [DOI] [PubMed] [Google Scholar]
- 24. Sega R, Facchetti R, Bombelli M, et al. Prognostic value of ambulatory and home blood pressures compared with office blood pressure in the general population: follow‐up results from the Pressioni Arteriose Monitorate e Loro Associazioni (PAMELA) study. Circulation. 2005;111:1777‐1783. [DOI] [PubMed] [Google Scholar]
- 25. Wiles JD, Taylor K, Coleman D, Sharma R, O'Driscoll JM. The safety of isometric exercise: rethinking the exercise prescription paradigm for those with stage 1 hypertension. Medicine (Baltimore). 2018;97(10):e0105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Decaux A, Edwards JJ, Swift HT, et al. Blood pressure and cardiac autonomic adaptations to isometric exercise training: a randomized sham‐controlled study. Physiol Rep. 2022;10(2):e15112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Smart NA, Gow J, Bleile B, Van der Touw T, Pearson MJ. An evidence‐based analysis of managing hypertension with isometric resistance exercise‐are the guidelines current? Hypertens Res. 2020;43(4):249‐254. [DOI] [PubMed] [Google Scholar]
- 28. Wiles J, Rees‐Roberts M, O'Driscoll JM, et al. Feasibility study to assess the delivery of a novel isometric exercise intervention for people with stage 1 hypertension in the NHS: protocol for the IsoFIT‐BP study including amendments to mitigate the risk of COVID‐19. Pilot Feasibility Stud. 2021;7(1):192. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supporting Information


