Abstract
STXBP1 variants are one of the most common genetic causes of neurodevelopmental disorders and epilepsy, wherein STXBP1-related disorders are characterized by neurodevelopmental abnormalities in 95% and seizures in 89% of affected patients. However, the spectrums of both genotype and phenotype are quite wide and diverse, with a high baseline variability even for recurrent STXBP1 variants. Until now, no clear genotype–phenotype correlations have been established and multiple disease mechanisms have been proposed for STXBP1-related disorders. Without an ascertained disease cause for many cases of STXBP1 variants, it is challenging to manage this disease in an effective manner and current symptom-based treatments are focused on seizure control only, which has a minimal impact on global development. A novel STXBP1 canonical splice variant, NM_001032221.4:c.578+2T>C, was reported in this study, together with detailed documentation of disease manifestations and treatment management. Further RNA expression analysis revealed abnormal intron retention and possible production of truncated STXBP1 proteins as a likely pathogenic mechanism. More importantly, the landscape of previously understudied STXBP1 splice variants and functional investigations was assessed for the first time to provide a context for the discussion of the complicated genotype–phenotype relationship of STXBP1-related disorders. Future cases of this disorder and a deeper mechanism-based understanding of its pathogenic cause are required for precision medicine and better disease management.
Keywords: STXBP1-related disorder, Ohtahara syndrome, epilepsy, splice variant, functional study, RT-PCR, intron retention, genotype-phenotype relationship
Introduction
Disease-relevant STXBP1 variants are one of the most common genetic causes of neurodevelopmental disorders and epilepsy, wherein STXBP1-related disorders are characterized by neurodevelopmental abnormalities in 95% and seizures in 89% of affected patients (1, 2). However, the overall phenotypic spectrum of STXBP1-related disorders is quite broad. According to one recent comprehensive profiling, the patients could be grouped into several categories, which were early onset epileptic encephalopathy (EOEE), Ohtahara syndrome (OS), West syndrome (WS), other developmental and epileptic encephalopathies (other DEE), neurodevelopmental disorders (NDD), and atypical Rett syndrome (2). The group of EOEE included patients with a seizure onset within 3 months of age and clinical manifestations of developmental and epileptic encephalopathy. However, a more specific category of EOEE (such as OS or WS) would be assigned if possible. The OS group had tonic seizures and suppression-burst electroencephalogram (EEG) in addition to EOEE, whereas the WS group presented with infantile spasms as the first seizure presentation. The group of other DEEs showed DEE which was not categorized as EOEE, OS, or WS. However, if patients showed developmental abnormalities, seizures (if any) could be controlled with medicine and there were no signs of epileptic encephalopathy (significant EEG findings), they would be classified as NDD. In addition, the group with atypical Rett syndrome had developmental abnormalities and Rett-like features.
STXBP1 encodes the syntaxin-binding protein 1 (STXBP1, also known as Sec1/Munc18-1), which is well characterized in its interaction with syntaxin-1 and regulation of synaptic vesicle and neurotransmitter release (1, 3). In addition, STXBP1 also binds other protein partners and involves in non-synaptic processes (such as Golgi transport and intracellular trafficking), suggesting a broad involvement in cellular activities and thus providing a possible explanation for the diverse phenotypes of STXBP1-related disorders (4). Disease-related STXBP1 variants include missense, nonsense, splice-site, frameshift, deletion, and other variants, spanning the full spectrum of genetic mutations (1, 2, 4). Multiple pathogenic mechanisms have been proposed for STXBP1-related disorders, such as haploinsufficiency, dominant negative effects, and gain-of-function molecular consequences (3, 5, 6). However, due to a high baseline variability, no significant phenotypic similarity or discrete phenotypic subgroups emerged for recurrent STXBP1 variants and mutation hotspots (2). In addition, no clear genotype–phenotype correlations have been identified so far from several large-scale analyses (2, 4, 7).
In this study, we identified a novel heterozygous STXBP1 splice variant from a patient with OS and assessed the splicing defect with ex vivo RNA expression analysis of patient blood samples. We discussed the genotype–phenotype relationship within the context of previously reported STXBP1 splice variants and functional investigations. Future cases of this disorder and a deeper mechanism-based understanding of its genotype–phenotype relationship are required for precision medicine and better disease management.
Case presentation
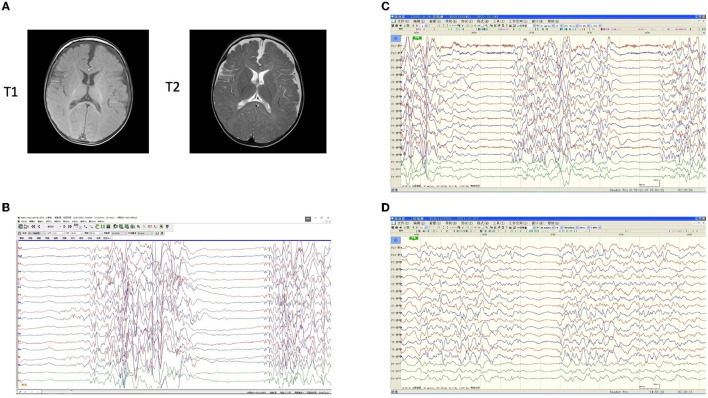
One 15-month-old male patient presented with neonatal-onset, repeated seizures, and progressing developmental delay (Table 1 and Supplementary Table 1). At 2 months of age, the patient was admitted to the hospital and a clinical diagnosis of OS was made based on the burst-suppression EEG result (Figure 1B). With the administration of adrenocorticotropic hormone (ACTH), topiramate, and valproic acid, the intensity of the burst period was weakened, but the burst-inhibition pattern was still obvious, and their durations remained relatively long by EEG (Figure 1C). At 3 months of age, with a treatment of prednisone, topiramate, levetiracetam, and midazolam, EEG showed very few burst periods, reduced inhibition periods, and significantly shorter durations (Figure 1D). During follow-ups at 4 months (18 weeks) and 6 months (26 weeks), the epileptic seizures were under control, and EEG findings significantly improved, but the development remained markedly behind (Table 1 and Supplementary Table 1). Brain magnetic resonance imaging (MRI) showed no obvious abnormality at the age of 6.5 months (Figure 1A).
Table 1.
Disease timeline and therapeutic interventions/outcomes.
| Age | Clinical descriptions |
|---|---|
| At birth | The patient was born at 40 weeks by natural delivery, with a weight of 3320 g and height of 50 cm, passing newborn screenings of foot blood and hearing. The mother of the patient had hypothyroidism and was treated with oral Eucalyptus during pregnancy. The patient was breastfed for 1 month after birth, and then on artificial feeding. Immunization was performed according to local regulations, without any noted adverse reactions. His parents were healthy and there was no family history of epilepsy or other genetic disorders. |
| Shortly after birth | Clustered seizures like nodding and hugging multiple times a day, more than 10 at a time and each lasting 1–2 min. |
| 1.5 months | Bilateral or unilateral limb tonic seizures or tonic-clonic seizures occurred, more than 10 times a day and each time lasting 2–10 s. |
| 2 months | Hospital admission and diagnosis of Ohtahara syndrome based on burst-suppression electroencephalogram (EEG). Physical examination at admission revealed consciousness, poor response, ability to suck, inability to eye-track or to hold the head up. Eye examinations revealed slight esotropia, pupils on both sides of equal size and circle, diameters at about 2 mm, and with light reflex. Further tests showed stable breathing, inspiratory depression in the suprasternal fossa, normal heart and lung auscultation, soft abdomen, and no palpable enlargement of the liver or spleen under the ribs. Besides, the neck was soft, the muscle strength and muscle tone of the limbs were low, the bilateral Babinski sign was negative, and there was a livedo about 2 cm*2 cm on the back. Blood biochemical examinations and genetic metabolism screening also revealed nothing remarkable in lactate, blood ammonia, ceruloplasmin, thyroid function, blood liver and kidney function, electrolytes, and blood sugar. Treatment with oral Adrenocorticotropic Hormone (ACTH), topiramate, and valproic acid. |
| 2 months and 3 weeks | Poor outcome (EEG) and severe pulmonary infection resulted in admission to the Pediatric Intensive Care Unit; ACTH ended and prednisone acetate tablets added; topiramate and valproic acid continued. |
| One STXBP1 variant identified through genetic testing; oral levetiracetam and midazolam micropump added, prednisone acetate and topiramate continued, valproic acid reduced and withdrawn. | |
| 3 months | Seizures under control (EEG) and reduced to 1–3 times a day; midazolam withdrawn and oral clonazepam tablets added (both midazolam and clonazepam are benzodiazepines). |
| Discharge from hospital with prednisone acetate tablets, topiramate, levetiracetam oral liquid, and clonazepam tablets; seizures under control. | |
| 4 months | Seizure attacks were in the form of binocular staring, with or without rigidity of both upper limbs, 3–4 times a day. |
| 5 months | The symptoms were similar to those at 4 months, with reduced seizure attacks at once every 2–3 days and improved EEG; prednisone acetate tablets withdrawn and topiramate gradually reduced, whereas oral levetiracetam liquid and clonazepam continued. |
| 6 months | Seizures were under control and occurred once every 10 days. EEG findings significantly improved, but the development was still markedly behind. The muscle strength and muscle tone of the limbs were low. |
Figure 1.
Imaging examinations of the patient. Brain magnetic resonance imaging (MRI) showed no obvious abnormality at the age of 6.5 months (A). T1-weighted and T2-weighted images were consistent. Electroencephalogram (EEG) results before and after antiepileptic medications (B–D). (B) A burst-inhibition pattern was observed before any medication at 2 months. (C) With a treatment of oral adrenocorticotropic hormone (ACTH), topiramate, and valproic acid, the intensity of the burst period was significantly weakened, but the burst-inhibition pattern was still obvious, and their durations remained relatively long. In addition, a small amount of bilateral discharge and an extremely asymmetric background were observed. (D) After treatment of prednisone, topiramate, levetiracetam, and midazolam, there were very few burst periods and reduced inhibition periods, with significantly shorter durations at 3 months. A small amount of 4–6c/sθ activity was visible and distributed. Distinguishable focal discharges in the background, apparent asymmetry, and a tendency for a high degree of arrhythmia were also observed.
Genetic diagnosis
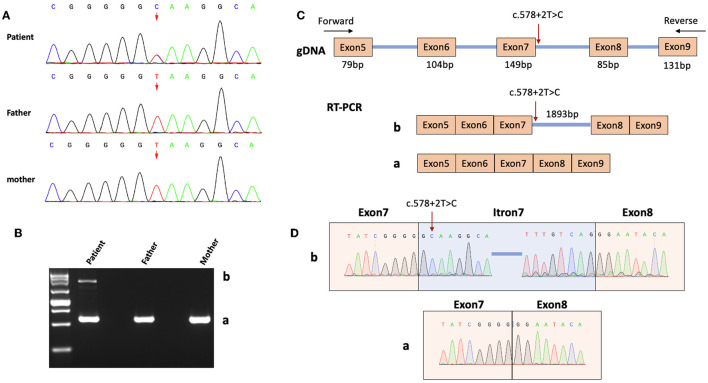
A pathogenic heterozygous variant, NM_001032221.4:c.578+2T>C, was identified in the STXBP1 gene from the patient through whole genome sequencing. This variant is located at a canonical splice donor site and is predicted to result in abnormal splicing of STXBP1 mRNA. To date, this novel variant has no minimum allele frequency documented in the Reference Population Gene Frequency Database (gnomAD) and has not been reported in the Clinvar database. By Sanger sequencing analysis, this mutation was not identified in the patient's father or mother (Figure 2A). According to the American College of Medical Genetics and Genomics (ACMG) guidelines, this novel de novo variant is classified as pathogenic. Together with the clinical findings described earlier, a final diagnosis of STXBP1 encephalopathy with OS was made.
Figure 2.
Genetic diagnosis and RNA analysis. (A) Sanger sequencing results of the patient and his parents. The arrow indicates the genomic location (according to the human genome assembly GRCh37 / hg19) of the heterozygous variant NM_001032221.4:c.578+2T>C. (B) RT-PCR product analysis by agarose gel electrophoresis. A normal band (Band a) was observed in both the male patient and controls (his parents), whereas an extra band (Band b) was observed in the patient only. (C) A diagram showed the design of PCR primers for cDNA amplification and the contents of the two bands in B (Bands a and b). Red arrow indicates the variant site. (D) Sanger sequencing revealed the sequences of Bands a and b.
RNA analysis for splicing defect of our STXBP1 variant
STXBP1 c.578+2T>C is one canonical splice variant, which usually leads to exon skipping, intron retention, and/or the activation of an alternative cryptic splice site (8). RNA expression analysis was carried out on patient blood samples using a method published earlier (9). Briefly, RNA was first extracted from blood samples collected from the patient and his parents as controls. Complementary DNA was then obtained and one pair of primers was designed to amplify regions of interest, which were separated by agarose gel electrophoresis. Bands of interest were gel extracted and sequenced.
As shown in Figures 2B, C, the normally spliced mRNAs from both parents generated a PCR product of 570bp (Band a) that contains 4-bp at the 3' end of Exon4, 79-bp Exon5, 104-bp Exon6, 149-bp Exon7, 85-bp Exon8, 131-bp Exon9, and 18-bp at the 5' end of Exon10. However, samples from the patient with heterozygous STXBP1 c.578+2T>C showed two PCR products, of which the normal one was Band a and an abnormal one (2463bp, Band b) contains the additional 1893-bp Intron7. Moreover, sequencing results of Band b showed that the second nucleotide of the retained Intron7 is the variant T, rather than the normal C, indicating that the abnormally spliced transcript was from the variant allele as a result of the splicing defect (Figures 2C, D). The translation of the abnormal transcript would lead to a premature termination codon within the retained Intron7 and therefore a truncated STXBP1 protein.
The overall profile of STXBP1 canonical splice variants
Our identified variant, STXBP1 NM_001032221.4:c.578+2T>C, is located at a canonical splice site and leads to abnormal splicing. In general, canonical splice variants, within 2bp of exon–intron junction, are widely annotated as “loss of function” (LoF) variants and are known to be strong diagnostic candidates in LoF disorders (10). For example, +2T>C variants have been frequently reported to cause human genetic disease and are routinely scored as pathogenic splicing mutations. However, it was recently demonstrated that diverse molecular outcomes exist and such +2T>C variants in human disease genes may not invariably be pathogenic (11, 12).
To obtain a comprehensive understanding of the genotype–phenotype relationship for STXBP1 splice variants, we compiled a list of 54 canonical and 203 non-canonical splice variants (Supplementary Table 2) from the Clinvar database. We evaluated those variants through spliceAI, a deep neural network that accurately predicts splice sites based on pre-mRNA sequence, which proves to be a highly accurate and informative prediction tool for potential splicing changes (10, 12, 13). Most canonical splice variants (44 out of 54) cause frameshift insertion or deletion and thus disruptive changes in STXBP1 expression. Out of the 44 frameshift splice variants, 12 are associated with early infantile epileptic encephalopathy with suppression bursts, 16 are associated with developmental and epileptic encephalopathy, whereas the rest do not have specified clinical conditions.
Because many of the variants reported by Clinvar do not have a phenotypic description available for in-depth assessment (only general disease category provided), clinical information from the comprehensive list of 534 individuals with STXBP1-related disorders published in 2022 (2) was referenced for phenotype analysis. A brief survey of multiple canonical splice variants spanning the full length of STXBP1 pre-mRNA (Supplementary Table 3) showed that the majority of them correlated with severe phenotypes and early disease onset in the patients (12 at more than 2 months and only one at 14 months), suggesting that STXBP1 is highly sensitive to decreased amount of expression, consistent with its high probability of loss-of-function intolerance and predicted probability of haploinsufficiency (14).
For the ten canonical splice variants of STXBP1 that were predicted to result in in-frame splicing changes, it is reasonable to speculate that their consequent less disruptive changes would lead to less severe phenotypes in general than those with frameshift changes. Previously published data (2) were utilized for this analysis (Table 2). It seems that smaller deletion (one case of c.795-2A>T, 12bp deletion, and moderate delay with seizure onset at 2.5 months) causes phenotypes less severe than larger deletion (two cases of c.795-2A>G, 108bp deletion, severe delay with seizure onset at 0.5 or 0.35 month). Different changes at the same splice site (c.795-2A>T/G) could cause different molecular consequences enough for significant clinical differences, supporting a previous notion that the functional effect of splicing variants is on a continuum rather than binary (10). Similarly, c.1030-1G > A is predicted to result in skipping of the whole 81-bp Exon13, compared to a deletion of only 27bp caused by c.1030-1G>T. More drastic differences likely exist between c.1462-2A>G (12bp in-frame deletion) and c.1462-2A>T (86bp frameshift deletion), but unfortunately, no clinical data are available to assess the genotype–phenotype relationship. More well-documented cases and experimental characterizations of the exact molecular defect are needed to draw a more convincing conclusion since only a small number of splice variants were currently available with experimental characterization and SpliceAI predictions were used as a proxy for functional evaluation.
Table 2.
Canonical splice variants of STXBP1.
| Variant | Patient ID | Disease categories | Disease onset/month | SpliceAI prediction |
|---|---|---|---|---|
| c.578+1G>A | STX_32139178_Patient_Infantile22 | EOEE | 3 | Frame-shift |
| c.578+1dupG | STX_CHCO_01 | EOEE | 0.1 | Frame-shift |
| c.578+2T>C | This study | OS (EOEE) | 0 | Frame-shift |
| c.169+2T>C | STX_31344879_Patient3 | Atypical Rett Syndrome | 2 | Frame-shift |
| c.1249+2T>C | STX_HSJD_Patient_9 | EOEE | 0.13 | Frame-shift |
| STX_25631041_case_report | OS | 0.49 | ||
| c.1359+1G>A | STX_P_28 | EOEE | 72 | Frame-shift |
| STX_HSJD_Patient_7 | EOEE | 1 | ||
| STX_26865513_Patient_13 | EOEE | 4 | ||
| c.1702+1G>A | STX_31344879_Patient5 | Atypical Rett Syndrome | 0.5 | Frame-shift |
| STX_EG1074P | WS | 0.26 | ||
| STX_P_22 | NDD | 0.1 | ||
| STX_Syrbe_21 | WS | 3 | ||
| c.795-2A>G | STX_25951140_Case_32 | EOEE | 0.5 | In-frame 108bp deletion |
| STX_26514728_Patient_4 | EOEE | 0.35 | ||
| c.795-2A>T | STX_26865513_Patient_22 | EOEE | 2.5 | In-frame 12bp deletion |
| c.1030-1G>A | STX_29896790_P2 | EOEE | 0 | In-frame 81bp deletion |
The overall profile of STXBP1 non-canonical splice variants
For non-canonical splice variants with a broader range of functional consequences and thus a wider phenotypic spectrum, their contribution to disease is more difficult to establish. Functional characterization is not practical for all of them, so accurate prediction tools (such as SpliceAI) serve as a good approximate proxy. In total, 203 STXBP1 non-canonical splice variants (synonymous variants close to splice sites and deeper intronic variants) from Clinvar were grouped based on their respective clinical significance. By SpliceAI, 13 out of the 15 pathogenic or likely pathogenic variants (87%), eight out of the 18 variants of uncertain significance (44%), and one out of the four variants with conflicting interpretations of pathogenicity (25%) were predicted with splicing changes that are likely functionally relevant, consistent with the designated clinical significance of each group. From the remaining benign or likely benign variants, we randomly picked 20 for SpliceAI prediction, and only two showed a positive indication for likely significant splicing changes (10%). No detailed clinical data were available from Clinvar for more in-depth phenotypic evaluation. Ultimately, experimental functional characterization is required for confirmation, but prediction tools are quite useful to prioritize a large number of candidate splice variants.
To complement the analysis of data from Clinvar, which is a database for disease-associated variants, 6824 STXBP1 variants (including deep intronic regions) from gnomAD (15) and the Genome Aggregation Database from population genetic studies were evaluated, and none of the canonical splice variants showed up. In addition, 23 of the 24 non-canonical splice variants that have likely significant splicing changes were absent from the gnomAD database, and only one was reported with one allele out of 2,51,470 (a frequency of 3.98e-06). In contrast, many of the variants with no predicted splicing changes have a high allele frequency in gnomAD.
STXBP1 c.578+2T>C and related splice variants
STXBP1 c.578+2T>C and two splice variants nearby (c.578+1G>A and c.578+1dupG) shared severe splicing defects as predicted by SpliceAI and early onset EOEE in respective patients (Table 2). Similarly, two other +2T>C variants (c.169+2T>C and c.1249+2T>C) were predicted to cause a frameshift, and patients with those variants showed early onset STXBP1-related disorders. Previous studies suggested that +2T>C variants typically lead to exon skipping (rather than intron retention) and/or activation of the cryptic splice site (8). However, the RNA analysis of our patient with c.578+2T>C revealed intron retention as the functional consequence. Future investigations on more STXBP1 +2T>C variants will help clarify a general pattern in terms of their effect on splicing.
Most of the splice variants were reported in only one patient, but there are several associated with multiple patients, such as c.1249+2T>C, c.1359+1G>A, c.1702+1G>A, and c.795-2A>G (Table 2). For those recurrent splice variants, the associated disease categories could be diverse, but the age of disease onset was generally consistent, except for c.1359+1G>A, with which one patient had much later disease onset than the other two patients (72 months compared to 1 and 4 months).
Discussion
Genotype–phenotype relationship of STXBP1-related disorders
As illustrated in one recent comprehensive profiling of STXBP1 variants, no significant phenotypic similarity or discrete phenotypic subgroups emerged for recurrent STXBP1 variants and mutation hotspots due to a high baseline variability (2). Until now, no clear genotype–phenotype correlations for STXBP1-related disorders have been identified despite several large-scale efforts (2, 4, 7). However, the majority of patients with STXBP1-related disorders present with neurodevelopmental abnormalities (developmental delay and intellectual disability) and seizures (mostly onset in the first year of life) across the whole spectrum of many different types of genetic variants (missense, nonsense, frameshift, and splice variants, small intragenic deletions and duplications, and whole-gene deletions) (1, 2, 4), suggesting an overall genotype–phenotype correlation and shared overarching disease mechanisms that are consistent with the molecular function of STXBP1 protein during synaptic transmission. In addition, monozygotic twins with the same STXBP1 splice variant presented with similar phenotypes and disease course (7), and two sisters with identical STXBP1 missense variants showed highly similar clinical symptoms, whereas their heterozygous mother and siblings are asymptomatic (6), indicating the consistent role of genetic factors in STXBP1-related disease. Therefore, focusing on the overall profile or key phenotypic indicators, rather than individual phenotypic features, maybe a more productive approach to assessing its genotype–phenotype relationship.
Another recent study showed that despite no clear genotype–phenotype correlation, age at the seizure onset correlated with the severity of the developmental outcome, with an earlier seizure onset related to worse developmental achievement (7). Therefore, we focused on the general categories of disease (EOEE, WS, OS, other DEE, or NDD) and the age of seizure onset as key indicators and reassessed several recurrent missense variants reported previously (2). Moreover, different variants at the same site were analyzed separately rather than being grouped as in previous studies (2, 7), with the reasoning that different substitutions at the same position would present with different degrees of functional perturbation due to the varying biochemical properties of different amino acid residues.
Disease categories and ages of seizure onset were analyzed for the top seven missense variants, and a summary is given in Supplementary Table 4. As expected, diverse phenotypes of each variant spanned different categories of STXBP1-related disorders, but the ages of seizure onset were all below 1 year with no more than two exceptions for each variant (2/19 for Arg406His, 2/19 for Arg406Cys, 2/18 for Arg292His, 1/10 for Arg292Cys, 2/18 for Arg551Cys, 1/12 for Pro139Leu, and 1/11 for Arg190Trp).
For typical genotype–phenotype analysis beyond recurrent variants, certain types of variants, such as non-sense, splice-site, frameshift, and whole/partial deletion variants, were grouped together as protein-truncating variants due to their presumed similarity in their functional consequences (2). However, this heterogenous group of variants can lead to drastically different outcomes in terms of functional changes that are sufficient to warrant different phenotypes. One recent study of two protein-truncating STXBP1 variants showed that one deletion variant caused non-sense-mediated decay (NMD) and likely no production of truncated proteins, whereas NMD was not observed with the other non-sense variant, and truncated proteins were possibly produced (9). This different molecular outcome may explain the different disease phenotypes associated with the two variants (seizure-free compared to early onset epileptic spasms). Therefore, more precise classification of variants should not be based on gross groups but instead on efficient and feasible functional assays, which are not always available currently.
On the contrary, different types of variants can lead to similar clinical phenotypes. For example, homozygous STXBP1 missense variants (p.Leu446Phe) lead to refractory Lennox-Gastaut syndrome and severe intellectual disability (ID) (6), which could also result from a small intragenic deletion of one amino acid residue in another case (p.Lys21del) (2). In comparison, a different small in-frame deletion near p.Lys21 (c.57_59del:p.19_20del) identified in three unrelated patients showed consistent NDD with only mild ID and similar ages of seizure onset (2), arguing for the importance of exact locations even for the same type of variants that are close to each other. The pathogenicity of these variants, as well as the recurrent missense variants described earlier and other examples not listed here, should all be traced back to the biochemical function of respective sites, but only a rather limited number of them have been functionally characterized, such as p.Leu446Phe and p.39dup (6, 16).
With respect to STXBP1 splice variants, the vast majority of canonical ones correlated well with severe phenotypes and early seizure onset in the patients (Table 2 and Supplementary Table 3). In contrast, non-canonical splice variants form a much larger and more diverse group in terms of their functional consequences and associations with disease (Supplementary Table 2). Despite limited experimental assessments of those variants, accurate in silico tools such as SpliceAI, could be utilized for preliminary evaluation and prioritization to facilitate genetic diagnosis. Hopefully, increasing the application of genomic sequencing as the first-line diagnosis tool will enable the identification of more disease-related STXBP1 variants and together with better reliable predictive and experimental tools to characterize the actual functional consequences, a genotype–phenotype correlation may emerge (4).
Treatment of STXBP1-related disorders
Due to the limited understanding of the disease mechanism and diverse spectrum of both genotypes and phenotypes for STXBP1-related disorders, current treatments are focused on seizure control, wherein usually multiple antiepileptic drugs were prescribed, but a significant portion of the patients still had frequent seizures (1, 2, 7). Different drugs showed significantly different efficacies, depending on seizure type and age, but in general, ACTH and phenobarbital were effective in initially decreasing seizure frequency in infantile spasms and focal seizures, whereas the ketogenic diet was the most effective treatment to maintain seizure freedom (2). In our case, ACTH was first used with poor outcomes and concurrent severe pulmonary infections, while benzodiazepines (midazolam and clonazepam) showed good efficacy in seizure control and maintenance, suggesting that individual differences should be taken into consideration for disease management.
Symptom-based seizure control was able to improve behavioral and interactive skills, while additional physical and occupational therapies could relieve locomotor problems and maximize developmental potential (1, 7). However, the currently available multidisciplinary treatments had a minimal impact on global development (7). As illustrated in our patient, the mental and motor development was markedly behind children of the same age and significant intellectual disability persisted despite good seizure control with medication (Table 1 and Supplementary Table 1). A future mechanism-based targeted approach may benefit both seizure and developmental outcomes (1). For example, several chemical chaperons demonstrated a good rescue effect on functional deficits caused by STXBP1 variants with decreased stability and increased aggregation in multiple in vitro and in vivo models (5).
Conclusion
Ohtahara syndrome is an early-onset epileptic encephalopathy with severe psychomotor development delay, characterized by frequent and uncontrollable tonic-spasmodic seizures and periodic burst-inhibition patterns in the EEG of both waking and sleeping phases. For infants with neonatal-onset OS who have neither history of hypoxic-ischemic encephalopathy nor obvious abnormal brain MRI, genetic factors such as STXBP1 variants should be considered. The identified novel STXBP1 splice variant in our patient (NM_001032221.4:c.578+2T>C) and the detailed documentation of clinical phenotypes and disease management would enrich the spectrum of genotypes and phenotypes of STXBP1-related disorders. A review of STXBP1 splice variants was also provided to facilitate the understanding of the disease genotype–phenotype relationship.
Data availability statement
The datasets presented in this article are not readily available because of ethical and privacy restrictions. Requests to access the datasets should be directed to the corresponding authors.
Ethics statement
This study was approved and carried out under the ethical guidelines for clinical investigation of our institution. Informed consent was obtained and available upon request. Written informed consent was obtained from the participant/patient(s) for the publication of this case report.
Author contributions
HW and MH: preparing the original draft. HW, MH, and ZZ: reviewing, editing, supervision, and conceptualization. HW, XL, and MH: genetic data analysis. HW, XC, ZL, CC, and ZZ: clinical data acquisition. All authors contributed to the article and approved the submitted version.
Acknowledgments
We would like to thank the patient and his parents for their trust and cooperation.
Funding Statement
This study was supported by the Hangzhou Municipal Health Bureau Science and Technology Program and the Zhejiang Provincial Medical and Health Science and Technology Program.
Conflict of interest
XL and MH are employed by the Aegicare Technology Co., Ltd. The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fneur.2023.1146875/full#supplementary-material
References
- 1.Stamberger H, Nikanorova M, Willemsen MH, Accorsi P, Angriman M, Baier H, et al. STXBP1 encephalopathy: a neurodevelopmental disorder including epilepsy. Neurology. (2016) 86:954–62. 10.1212/WNL.0000000000002457 [DOI] [PubMed] [Google Scholar]
- 2.Xian J, Parthasarathy S, Ruggiero SM, Balagura G, Fitch E, Helbig K, et al. Assessing the landscape of STXBP1-related disorders in 534 individuals. Brain. (2022) 145:1668–83. 10.1093/brain/awab327 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kovacevic J, Maroteaux G, Schut D, Loos M, Dubey M, Pitsch J, et al. Protein instability, haploinsufficiency, and cortical hyper-excitability underlie STXBP1 encephalopathy. Brain. (2018) 141:1350–74. 10.1093/brain/awy046 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Abramov D, Guiberson NGL, Burre J. STXBP1 encephalopathies: clinical spectrum, disease mechanisms, and therapeutic strategies. J Neurochem. (2021) 157:165–78. 10.1111/jnc.15120 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Guiberson NGL, Pineda A, Abramov D, Kharel P, Carnazza KE, Wragg RT, et al. Mechanism-based rescue of Munc18-1 dysfunction in varied encephalopathies by chemical chaperones. Nat Commun. (2018) 9:3986. 10.1038/s41467-018-06507-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lammertse HCA, van Berkel AA, Iacomino M, Toonen RF, Striano P, Gambardella A, et al. Homozygous STXBP1 variant causes encephalopathy and gain-of-function in synaptic transmission. Brain. (2020) 143:441–51. 10.1093/brain/awz391 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Balagura G, Xian J, Riva A, Marchese F, Ben Zeev B, Rios L, et al. Epilepsy course and developmental trajectories in STXBP1-DEE. Neurol Genet. (2022) 8:e676. 10.1212/NXG.0000000000000676 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lin JH, Tang XY, Boulling A, Zou WB, Masson E, Fichou Y, et al. First estimate of the scale of canonical 5' splice site GT>GC variants capable of generating wild-type transcripts. Hum Mutat. (2019) 40:1856–73. 10.1002/humu.23821 [DOI] [PubMed] [Google Scholar]
- 9.Yang P, Broadbent R, Prasad C, Levin S, Goobie S, Knoll JH, et al. De novo STXBP1 mutations in two patients with developmental delay with or without epileptic seizures. Front Neurol. (2021) 12:804078. 10.3389/fneur.2021.804078 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Blakes AJM, Wai HA, Davies I, Moledina HE, Ruiz A, Thomas T, et al. A systematic analysis of splicing variants identifies new diagnoses in the 100,000 Genomes Project. Genome Med. (2022) 14:79. 10.1186/s13073-022-01087-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Joynt AT, Evans TA, Pellicore MJ, Davis-Marcisak EF, Aksit MA, Eastman AC, et al. Evaluation of both exonic and intronic variants for effects on RNA splicing allows for accurate assessment of the effectiveness of precision therapies. PLoS Genet. (2020) 16:e1009100. 10.1371/journal.pgen.1009100 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chen JM, Lin JH, Masson E, Liao Z, Ferec C, Cooper DN, et al. The experimentally obtained functional impact assessments of 5' splice site GT'GC variants differ markedly from those predicted. Curr Genomics. (2020) 21:56–66. 10.2174/1389202921666200210141701 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Jaganathan K, Kyriazopoulou Panagiotopoulou S, McRae JF, Darbandi SF, Knowles D, Li YI, et al. Predicting splicing from primary sequence with deep learning. Cell. (2019) 176:535–48. 10.1016/j.cell.2018.12.015 [DOI] [PubMed] [Google Scholar]
- 14.Firth HV, Richards SM, Bevan AP, Clayton S, Corpas M, Rajan D, et al. DECIPHER: Database of chromosomal imbalance and phenotype in humans using ensembl resources. Am J Hum Genet. (2009) 84:524–33. 10.1016/j.ajhg.2009.03.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Karczewski KJ, Francioli LC, Tiao G, Cummings BB, Alfoldi J, Wang Q, et al. Author correction: the mutational constraint spectrum quantified from variation in 141,456 humans. Nature. (2021) 590:E53. 10.1530/ey.17.14.3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Banne E, Falik-Zaccai T, Brielle E, Kalfon L, Ladany H, Klinger D, et al. De novo STXBP1 mutation in a child with developmental delay and spasticity reveals a major structural alteration in the interface with syntaxin 1A. Am J Med Genet B Neuropsychiatr Genet. (2020) 183:412–22. 10.1002/ajmg.b.32816 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets presented in this article are not readily available because of ethical and privacy restrictions. Requests to access the datasets should be directed to the corresponding authors.