Abstract
This statement paper summarises and appraises the evidence on diagnosis, prevention, and treatment of common shoulder injuries in sports. We systematically searched Medline and Embase. The Grading of Recommendations Assessment, Development and Evaluation tool was applied to evaluate the overall quality of evidence.
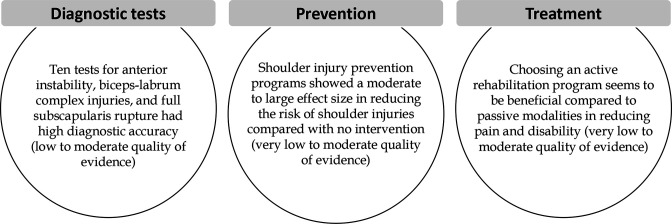
For diagnosis, we included 19 clinical tests from mixed populations. Tests for anterior instability, biceps-labrum complex injuries and full subscapularis rupture had high diagnostic accuracy (low to moderate quality of evidence).
For prevention, the Oslo Sports Trauma Research Center, the Shoulder Control, the FIFA 11+ shoulder injury prevention programmes, and a baseball-specific programme (range of motion, stretching, dynamic stability and strengthening exercises) showed moderate to large effect size in reducing the risk of shoulder injury compared with no intervention (very low to moderate quality of evidence).
For treatment, a rehabilitation programme including stretching, ice packs, electrotherapy and compression, and strengthening exercises showed a large effect size in reducing pain and disability compared with no intervention in athletes with subacromial impingement syndrome (very low to moderate quality of evidence). For the treatment of supraspinatus tendinopathy, hyperthermia treatment (heating the skin to 38°C–40°C) resulted in large effect size in reducing pain and disability compared with ultrasound or pendular swinging and stretching exercises (moderate quality of evidence). Strengthening exercise alone or in combination with stretching exercises promoted a large effect in reducing shoulder pain (cohort studies, no comparators) (very low quality of evidence). The quality of evidence for most estimates was low to moderate, indicating that future high-quality research may alter our recommendations for clinical practice.
Keywords: Athletic Injuries, Exercise, Rehabilitation, Shoulder, Sporting injuries
What is already known
Shoulder injuries are very common in overhead athletes.
The quality of evidence related to diagnosis, prevention and treatment of the most common shoulder injuries has not been investigated.
What are the new findings
High diagnostic accuracy was observed for 10 tests covering anterior instability (apprehension test (+relocation)), SLAP injuries (Biceps Load II), biceps-complex injuries (three-pack and Yergason), and rupture of the subscapularis (internal rotation lag).
Shoulder injury prevention programmes showed a moderate to large effect size in reducing the risk of shoulder injuries compared with no intervention.
Choosing an active rehabilitation programme seems to be beneficial compared with passive modalities in reducing pain and disability.
Most outcomes were graded as very low to moderate quality of evidence, indicating that future high-quality research may alter our findings.
Introduction
Shoulder injuries occur frequently in sports such as swimming, volleyball and handball, where movements are performed repeatedly over the head at high speed or in extreme positions.1–4 Athletes from these sports are often referred to as ‘overhead athletes’. It is widely accepted that these athletes are at significant risk of sustaining shoulder injuries, with several attempts made to identify risk factors and optimal management.5–8 The risk of shoulder injuries varies across sports and depends on the definition (time loss in sports, medical attention, severity etc). In swimming, 23%–38% of athletes sustain shoulder injuries within 1 year,3 4 and 23% of volleyball players experience dominant shoulder pain during the ongoing season.9 In a large study of elite handball, 44%–75% have previously had shoulder pain, 20%–52% report current shoulder pain and the prevalence of weekly shoulder pain and substantial shoulder injuries is 28% and 12%, respectively.1 These high rates of shoulder injuries are also seen in other overhead sports such as baseball10 and waterpolo11 and may vary depending on age, sex and level of competition.
Shoulder injuries may result from an instantaneous transfer of large quantities of kinetic energy (ie, acute with sudden onset), from the gradual accumulation of low-energy transfer over time (ie, repetitive with gradual onset) or a combination of both mechanisms (ie, repetitive with sudden onset).12 Although the International Olympic Committee recently provided consensus-based guidelines for recording and reporting epidemiological data on injuries in sport,12 defining and classifying mechanisms and mode of onset of shoulder injuries is challenged by the lack of consistent terminology in the existing literature.
The clinical management of shoulder injuries is of interest to a broad audience within the sports medicine community, including physiotherapists, sports physicians and orthopaedic surgeons with interest in the diagnosis, prevention and treatment of such injuries.8 Therefore, to improve the management of shoulder injuries, this statement paper, commissioned by the Danish Society of Sports Physical Therapy, aimed at providing an overview of the present literature. We graded the quality of evidence concerning the diagnostic accuracy of commonly used clinical tests and the effect of preventive and treatment strategies for the most common shoulder injuries.
Methods
This statement paper is divided into three domains: (1) diagnosis, (2) prevention and (3) treatment of five common shoulder injuries, including subacromial impingement syndrome (SIS), internal posterosuperior impingement, biceps-labrum complex injuries, rotator cuff injuries, and anterior instability, but also unspecified shoulder pain or injuries. The SIS is not well defined but includes structural damage in the subacromial space, including tendinopathies, partial rotator cuff ruptures, bursitis—without distinction to the mechanism behind it.13 Internal posterosuperior impingement is a frequent cause of pain among overhead athletes, characterised by an increased or repeated contact between the rotator cuff tendons attachment on the tuberculum majus humeri and the posterosuperior aspect of the glenoid cavity when the arm is in an maximally abducted and externally rotated position.14 Clinical studies indicate that its cause is multifactorial, and several anatomical structures are involved in the condition. Biceps-labrum injuries (including SLAP) involve the biceps' long head and its attachment to the glenoid labrum and can involve the labrum in varying degrees as an actual SLAP lesion.15 Rotator cuff injuries include tendinopathies and partial or complete tendon ruptures, most related to the supraspinatus tendon.16 Anterior shoulder instability may be caused by previous traumatic shoulder dislocation or repeated stress on the anterior structures with prolonged microtraumas and anterior subluxations.17 As such, the selected diagnoses and common shoulder injuries include athletes with any physical shoulder complaint irrespective of the need for medical attention or time loss,18 and represent the spectrum from acute, sudden onset injuries to repetitive, gradual onset injuries, including unspecified shoulder pain or injuries. However, we excluded diagnoses likely to be solely of traumatic origin (ie, dislocations and fractures) because athletes presenting with such injuries are expected to have a different clinical profile and management needs.
Search
Three systematic searches covering diagnosis, prevention, and treatment of the five selected shoulder injuries were performed in MEDLINE via PubMed and EMBASE via Ovid in April 2021 and updated August 2022, with no restrictions in the year of publication. Only publications in English were included. We searched individual text words in the title/abstract and supplemented them with Medical Subject Headings terms (MeSH). We combined anatomical region of interest (eg, 'Shoulder (MeSH)' OR 'rotator cuff' OR ’shoulder') AND the type of shoulder problem (eg, 'Athletic injury (MeSH)' OR 'injur*' OR ’strain*' OR 'impingement') AND outcome for diagnosis and prevention (eg, 'Physical examination (MeSH)' OR 'test' OR 'diagnostic*' and 'Primary prevention (MeSH)' OR 'prevent*', respectively) or intervention for treatment (eg, 'Physical therapy modalities (MeSH)' OR 'exercise' OR 'education' OR 'Shockwave'). For treatment and prevention, the search strategy also included research design (eg, 'Systematic review (MeSH)' OR 'meta-analysis' OR 'randomised controlled trial'). In addition, reference lists of the included studies were screened for potential eligible references. The complete search strategy for all searches is available in online supplemental file 1.
bjsports-2022-105674supp001.pdf (1.4MB, pdf)
Selection of studies
Two authors (BL and JRP) independently screened studies using Covidence systematic review software (Veritas Health Innovation, Melbourne, Australia). Articles were initially screened by title and abstract for eligibility. Full-text articles were then screened for inclusion. Disagreements were solved by consensus. For all domains, studies were included based on the highest level of available evidence.19 For the diagnostic domain, systematic reviews and diagnostic cohort studies were preferred as these represent the highest starting point in the Grading of Recommendations Assessment, Development and Evaluation (GRADE) tool (3). We aimed to include studies comparing clinical tests to either arthroscopy, MRI, or ultrasound as the diagnostic reference standard. For the prevention and treatment domains, systematic reviews or randomised controlled trials (RCTs) were preferred as these represent the highest starting point in the GRADE tool (3). However, observational studies were also eligible for inclusion. For the prevention domain, all shoulder problem definitions were accepted (eg, time-loss, medical attention, severity scores, patient-reported outcomes (eg, pain)). Similarly, for the treatment domain, all effect measures were accepted (eg, risk of reinjuries, time to return to sport, number of criteria passed or patient-reported outcomes (eg, pain, physical function in sport and recreational activities)).
Appraisal
Two authors (BL and JRP) independently assessed the risk of bias in the included studies. The Cochrane Risk of Bias assessment tool 2.0 was used for RCTs,20 QUADAS-2 for diagnostic studies,21 ROBINS-I for non-randomised studies of interventions,22 and ROBIS for systematic reviews.23 Details of each tool can be found in online supplemental file 2. Disagreements were solved by consensus. If a systematic review included a risk of bias assessment of individual studies using one of the aforementioned assessment tools, no additional risk of bias assessment was conducted for these individual studies. However, if these tools were not used, or there was conflicting risk of bias assessments between two or more systematic reviews, risk of bias was reassessed. Two authors (BL and JRP) evaluated the overall quality of evidence for each outcome relating to diagnosis, prevention and treatment, following the GRADE approach.24 Disagreements were solved by consensus. The quality of evidence was graded as (1) high, indicating that further research is unlikely to alter the confidence in the estimates, (2) moderate, indicating that further research is likely to have an important impact on the confidence in the estimates and may change the estimates,24 low, indicating that further research is very likely to have an important impact on the confidence in the estimates and is likely to change the estimates or (4) very low, indicating high uncertainty about the estimates. For the prevention and treatment domains, the starting quality of evidence was ‘high’ for data based on RCTs and ‘low’ for data based on observational studies. For the diagnostic domain, the starting quality of evidence was ‘high’ when based on cohort studies. Subsequently, the quality of evidence could be downgraded one or two levels for each of five domains, including study limitation (ie, serious risk of bias),25 imprecision (ie, wide CIs around estimates or few studies included),26 inconsistency (ie, heterogeneity of results cross studies if more than one study was included for a specific outcome/intervention),27 indirectness (ie, lack of generalisability of the findings to the target population)28 and publication bias (ie, results depend on the sample size).29 The quality of evidence could be upgraded due to a large magnitude of effect, dose-response gradient, and effect of plausible residual confounding. The GRADE assessments can be found in online supplemental file 3.
bjsports-2022-105674supp002.pdf (32.6KB, pdf)
bjsports-2022-105674supp003.pdf (119.6KB, pdf)
Data synthesis
Diagnostic tests
The diagnostic accuracy of clinical tests was estimated as positive (LR+) and negative (LR−) likelihood ratios and expressed the change in odds of the patient having the problem.30 An LR+ >1 increases the post-test probability of a diagnosis following a positive test, while an LR− <1 decreases the post-test probability of a diagnosis following a negative test. The diagnostic accuracy was classified based on current guidelines as: very low (LR+ 1 to 2; LR− 0.5 to 1), low (LR+ 2 to 5; LR− 0.2 to 0.5), moderate (LR+ 5 to 10; LR− 0.1 to 0.2) and large (LR+ >10; LR− <0.1).31 When available, positive predictive values (PPV) and negative predictive values (NPV) were extracted or calculated from data presented in the individual studies. The PPV expresses the probability that a patient with a positive test had the problem in question, while NPV expresses the probability that a patient with a negative test did not have the problem. The diagnostic accuracy was classified based on current guidelines as: high (≥0.85), moderate (0.70–0.84) and low (≤0.69).32
Prevention and treatment
Due to substantial clinical heterogeneity in types of shoulder injuries, and intervention and population characteristics, pooling of results were not possible and a narrative synthesis was adopted. For dichotomous prevention outcomes (ie, problem/no problem), the effect of the intervention was presented as ORs, HRs, or incidence rate ratios. For continuous prevention outcomes (eg, pain measured using patient-reported outcomes, number of pain episodes), the effect of the intervention was presented as between-group differences. For the treatment domain, the effect was presented as between-group differences or, if between-group differences were not available, as within-group changes.
Results
The main findings are summarised in figure 1.
Figure 1.
Summary of main findings about diagnostic tests, prevention and treatment of common shoulder injuries in sport.
Domain 1: diagnostic tests
A total of 1286 studies were identified in the literature search. No studies were identified on the diagnostics of the selected shoulder injuries in athletes. Data on diagnostic tests were therefore obtained from studies including both athlete and non-athlete populations. Five studies (two systematic reviews33 34 and three prospective studies35–37) were included (table 1). No meta-analysis of diagnostic accuracy was available in the literature or conducted as a part of this statement paper.
Table 1.
Diagnostic accuracy of clinical tests and grading the quality of evidence
| Clinical test | Likelihood ratio | Positive and negative predicative values | Diagnostic accuracy | ||
| High* | Moderate | Low/very low | |||
| Arthroscopy used as reference standard | |||||
| Subacromial impingement | |||||
| Composit test (combination of Hawkins-Kennedy, Neer, Painful arc, Empty can/Jobe, external rotation against resistance)33 | LR+=2.93 | Low quality of evidence | |||
| LR−=0.34 | Low quality of evidence | ||||
| Internal posterosuperior impingement | |||||
| Posterior impingement test37 | LR+=5.0 | N/A* | |||
| LR−=0.29 | N/A† | ||||
| Anterior instability | |||||
| Apprehension33 | LR+=17.21 | Moderate quality of evidence | |||
| LR−=0.39 | Low quality of evidence | ||||
| Relocation33 | LR+=5.48 | Very low quality of evidence | |||
| LR−=0.55 | Very low quality of evidence | ||||
| Surprise33 | LR+=5.42 | Very low quality of evidence | |||
| LR−=0.25 | Very low quality of evidence | ||||
| Apprehension + relocation33 | LR+=39.68 | Moderate quality of evidence | |||
| LR−=0.19 | Moderate quality of evidence | ||||
| SLAP | |||||
| Biceps load II35 ‡ | LR+=26.38 | PPV=92.1 | Moderate quality of evidence | ||
| LR−=0.11 | NPV=95.5 | Moderate quality of evidence | |||
| Biceps-Labrum complex injuries | |||||
| O’Brien’s active compression; Inside36 § | LR+=1.62 | PPV=63.2 | Low quality of evidence | ||
| LR−=0.27 | NPV=77.8 | Low quality of evidence | |||
| O’Brien’s active compression; Junctional36 § | LR+=2.48 | PPV=82.4 | Low quality of evidence | ||
| LR−=0.15 | NPV=77.8 | Low quality of evidence | |||
| O’Brien’s active compression; Bicipital tunnel36 § | LR+=2.00 | PPV=65.7 | Low quality of evidence | ||
| LR−=0.08 | NPV=92.6 | Moderate quality of evidence | |||
| Throwing test; Inside36 § | LR+=2.32 | PPV=71.2 | Low quality of evidence | ||
| LR−=0.36 | NPV=72.1 | Low quality of evidence | |||
| Throwing test; Junctional36 § | LR+=3.42 | PPV=86.5 | Moderate quality of evidence | ||
| LR−=0.35 | NPV=60.5 | Low quality of evidence | |||
| Throwing test; Bicipital tunnel36 § | LR+=2.09 | PPV=66.7 | Low quality of evidence | ||
| LR−=0.40 | NPV=72.1 | Low quality of evidence | |||
| Bicipital tunnel palpation; Inside36 § | LR+=1.92 | PPV=67.2 | Low quality of evidence | ||
| LR−=0.16 | NPV=85.7 | Moderate quality of evidence | |||
| Bicipital tunnel palpation; Junctional36 § | LR+=3.43 | PPV=86.6 | Moderate quality of evidence | ||
| LR−=0.09 | NPV=85.7 | Moderate quality of evidence | |||
| Bicipital tunnel palpation; Bicipital tunnel36 § | LR+=2.24 | PPV=68.2 | Low quality of evidence | ||
| LR−=0.04 | NPV=96.4 | Moderate quality of evidence | |||
| Yergasons test; Inside36 § | LR+=2.13 | Low quality of evidence | |||
| LR−=0.76 | Low quality of evidence | ||||
| Yergasons test; Junctional36 § | LR+=6.57 | Low quality of evidence | |||
| LR−=0.83 | Low quality of evidence | ||||
| Yergasons test; Bicipital tunnel36 § | LR+=12.43 | Moderate quality of evidence | |||
| LR−=0.75 | Low quality of evidence | ||||
| MRI or ultrasound used as reference standard | |||||
| Rotator cuff injury | |||||
| Painful Arc34 | LR+=3.70 | Low quality of evidence | |||
| LR−=0.36 | Low quality of evidence | ||||
| Gerber/Lift-off test34 | LR+=1.40–1.50 | Very low quality of evidence | |||
| LR−=0.63–0.85 | Very low quality of evidence | ||||
| External rotation against resistance34 | LR+=2.60 | Low quality of evidence | |||
| LR−=0.49 | Low quality of evidence | ||||
| Full can34 | LR+=2.40 | Low quality of evidence | |||
| LR−=0.37 | Low quality of evidence | ||||
| Empty can/Jobe34 | LR+=1.30 | Very low quality of evidence | |||
| LR−=0.64 | Very low quality of evidence | ||||
| Full rotator cuff rupture | |||||
| External rotation lag34 | LR+=7.20 | Low quality of evidence | |||
| LR−=0.57 | Low quality of evidence | ||||
| Internal rotation lag34 | LR+=5.60 | Low quality of evidence | |||
| LR−=0.04 | Moderate quality of evidence | ||||
| Drop sign34 | LR+=3.20 | Low quality of evidence | |||
| LR−=0.35 | Low quality of evidence | ||||
*Tests that are considered to highly important in the choice of treatment were only downgraded one step in accordance with the GRADE approach for diagnostic studies.
†The article by Meister et al was not obtained in full text hindering risk of bias assessment.
‡Prevalence of SLAP injury=30.7%.
§Prevalence of biceps-labrum complex injuries=70%.
GRADE, Grading of Recommendations Assessment, Development, and Evaluation; LR−, negative likelihood ratio; LR+, positive likelihood ratio; NPV, negative predictive value; PPV, positive predictive value.
Subacromial impingement syndrome
Several tests for SIS were examined in a systematic review by Hegedus et al,33 of which one test battery, the Composite test, used five of the most commonly used tests in clinical practice (Hawkins-Kennedy, Neer, Painful arc, Empty can/Jobe and external rotation against resistance) and was included in this statement paper. Based on one prospective study (n=55), the composite test showed low diagnostic accuracy, with a low agreement between clinical testing and arthroscopic examination (LR+=2.93, LR−=0.34; low quality of evidence).38 Based on one prospective study (n=69), the posterior impingement test showed low to moderate diagnostic accuracy in predicting a positive or negative arthroscopic examination (LR+=5.0, LR−=0.29; not possible to assess the quality of evidence as the full-text version of the article was not accessible).37
Anterior instability
Eight studies, including four clinical tests, were included in the systematic review by Hegedus et al.33 Based on two studies (n=409), the apprehension test showed high diagnostic accuracy when positive (LR+=17.21) and low diagnostic accuracy when negative (LR−=0.39) in predicting a positive or negative arthroscopic examination, respectively (low to moderate quality of evidence). The diagnostic accuracy of the relocation test was investigated in three studies (n=509) and showed moderate diagnostic accuracy when positive (LR+=5.48) and low diagnostic accuracy when negative (LR−=0.55) in predicting a positive and negative arthroscopic examination, respectively (very low quality of evidence). A combination of the apprehension test and relocation test showed high diagnostic accuracy (LR+=39.68, LR−=0.19) in predicting a positive and negative arthroscopic examination (one study, n=46) (moderate quality of evidence). Based on two studies (n=128), the surprise test showed moderate diagnostic accuracy when positive (LR+=5.42) and low diagnostic accuracy when negative (LR−=0.25) in predicting a positive or negative arthroscopic examination, respectively (very low quality of evidence).
Biceps labral complex injuries
Based on one study35 (n=127), the Biceps Load II test showed high diagnostic accuracy when positive (LR+=26.38) and negative (LR−=0.11) in predicting a positive and negative arthroscopic examination, respectively (moderate quality of evidence). The diagnostic accuracy of the three-pack test (active compression, throwing test and bicipital tunnel palpation) was investigated for three anatomically different locations in the shoulder joint (inside, junctional and bicipital tunnel) in 116 patients.36 Active compression in the bicipital tunnel showed high diagnostic accuracy when negative in ruling out injury on arthroscopic examination (LR−=0.08) (moderate quality of evidence). Bicipital tunnel palpation junctional showed high diagnostic accuracy when negative in ruling out injury on arthroscopic examination (LR−=0.09) (moderate quality of evidence). Bicipital tunnel palpation on the bicipital tunnel showed high diagnostic accuracy when negative in ruling out injury on arthroscopic examination (LR−=0.04) (moderate quality of evidence). For the remaining locations (inside and junctional), low to moderate diagnostic accuracy (LR+=1.62 to 3.43, LR−= 0.16 to 0.40) were observed for all tests (low to moderate quality of evidence).
Rotator cuff injury
Four studies, including five clinical tests for rotator cuff injury (painful arc, gerber/lift-off test, external rotation against resistance, full can, empty can/Jobe), were included.34 All tests showed low diagnostic accuracy when positive (LR+=1.30 to 3.70) and negative (LR−=0.36 to 0.85) in predicting positive or negative rotator cuff injury on ultrasound or MRI, respectively (very low to low quality of evidence).39–41 One study including three clinical tests for full rotator cuff rupture was included.42 External lag rotation for infraspinatus and supraspinatus showed moderate diagnostic accuracy when positive (LR+=7.2) and low diagnostic accuracy when negative (LR−=0.57) in predicting positive and negative rotator cuff rupture on ultrasound, respectively (low quality of evidence). Internal rotation lag test for subscapularis showed moderate diagnostic accuracy when positive (LR+=5.6) and high diagnostic accuracy when negative (LR−=0.04) in predicting positive and negative rotator cuff rupture on ultrasound, respectively (moderate quality of evidence). Lastly, the drop-sign for infraspinatus and supraspinatus showed low diagnostic accuracy (LR+=3.2, LR−=0.35) in predicting positive and negative rotator cuff rupture on ultrasound (low quality of evidence).
Domain 2: prevention
A total of 932 studies were identified in the literature search. No systematic reviews were identified. Eight RCTs1 43–49 and one prospective study50 were included (table 2). The highest quality of evidence for a preventative effect was observed for Oslo Sports Trauma Research Center (OSTRC) Shoulder Injury Prevention programme,1 the Shoulder Control programme,47 a throwing injury prevention programme43 and the FIFA 11+ shoulder injury prevention programme (moderate quality of evidence).44 Performing the OSTRC Shoulder Injury Prevention programme during warm-up three times per week for 7 months resulted in 28% lower odds of shoulder injuries (OR=0.72 (95% CI 0.52 to 0.98)) and 22% reduced odds of substantial shoulder injuries (OR=0.78 (95% CI 0.53 to 1.16)) as measured by the OSTRC Overuse Injury Questionnaire, which covers all shoulder injuries regardless of time-loss from sport or medical attention.1 The Shoulder Control programme focusing on shoulder and trunk strength and control, trunk mobility and handball throwing load (velocity and frequency) performed three times weekly resulted in a 56% lower shoulder injury rate compared with usual care (HRR=0.44 (95% CI 0.29 to 0.68)).47 A throwing injury prevention programme consisting of stretching, mobility exercises and balance exercises performed at least once a week during warm-up was superior to a 12-month control period in preventing shoulder injuries in young baseball players (HR=0.48 (95% CI 0.21 to 1.08)).43 Performing the FIFA 11+shoulder injury prevention programme during warm-up in all training sessions for 6 months compared with usual care resulted in a lower incidence rate of shoulder injuries among soccer goalkeepers (IRR=0.28 (95% CI 0.13 to 0.60)).44
Table 2.
Prevention of shoulder injuries: effect and grading the quality of evidence
| Outcomes | Effect size | |||
| Effect (95% CI) | Large | Moderate | Small | |
| Risk of shoulder injuries | ||||
| Oslo Sports Trauma Research Centre Shoulder Injury Prevention programme versus usual care; n=660, male/female handball1 | All shoulder injuries OR=0.72 (0.52 to 0.98) | Moderate quality of evidence | ||
| Substantial shoulder injuries OR=0.78 (0.53 to 1.16) |
Moderate quality of evidence | |||
| Risk of shoulder injury | ||||
| Throwing injury prevention programme versus usual care; n=237, male/female baseball43 | HR=0.48 (0.21 to 1.08) | Moderate quality of evidence | ||
| The Shoulder Control programme versus usual care; n=465, male/female handball47 | HRR=0.44 (0.29 to 0.68) | Moderate quality of evidence | ||
| FIFA 11+ shoulder prevention programme versus usual care; n=726, male football44 | IRR=0.28 (0.13 to 0.60) | Moderate quality of evidence | ||
| Intervention including Sleeper’s stretch versus usual care; n=46, male baseball50 | HR=0.35 (0.13 to 0.94) | Very low quality of evidence | ||
| Intervention including Sleeper’s stretch and prone shoulder external rotation exercise versus usual care; n=60, male baseball50 | HR=0.47 (0.20 to 1.10) | Very low quality of evidence | ||
| TennisReady programme, versus usual care; n=579, male/female tennis49 | OR=0.96 (p=0.93) | Low quality of evidence | ||
| Intervention including stretching and rubber band strengthening exercises versus usual care; n=579, male/female handball48 | Absolute risk reduction=−2.5%(−10.3 to 5.4) | Low quality of evidence | ||
| No of shoulder pain episodes | ||||
| Intervention including functional exercises using resistance bands or dumbbells versus usual care; n=26, male/female swimming45 | Between-group difference in no of shoulder pain episodes=2.8 (CI not reported), p=0.02 | Low quality of evidence | ||
| Patient-reported shoulder pain | ||||
| Intervention including shoulder strengthening exercises versus usual care, n=106, female handball46 | Between group difference in VAS=0.1 (CI not reported), p=0.746 | Moderate quality of evidence | ||
HR, hazard ratio; HRR, hazard rate ratio; IRR, incidence rate ratio; VAS, Visual Analogue Scale.
Domain 3: treatment
A total of 4040 studies were identified in the literature search. No systematic reviews were identified. Four RCTs51–54 and three prospective studies55–57 including athletes were included (table 3).
Table 3.
Treatment of shoulder injuries: effect and grading the quality of evidence
| Injury | Effect | Effect size | ||
| Large | Moderate | Small | ||
| Subacromial impingement | ||||
| Intervention including shoulder specific warm-up and exercises versus no intervention; n=30, male baseball51 | Within-in group baseline and follow-up scores (SD) of pain (NRS) Intervention 7.88 (1.02) to 3.56 (1.31) Control 7.71 (0.83) to 8.00 (0.88) |
Moderate quality of evidence | ||
| Intervention including strengthening exercises (no comparator group); n=47; male/female mixed sports55 | Within-in group baseline and follow-up scores (SD) of pain and function (SPADI) 29.86 (17.03) to 11.7 (13.78) |
Very low quality of evidence | ||
| Supraspinatus tendinopathy | ||||
| Interventions including hyperthermia or ultrasound versus passive stretches; n=37, male/female mixed sports54 | Within-in group baseline and follow-up scores (SD) of pain (VAS) Hyperthermia 5.96 (0.83) to 1.2 (0.63) Ultrasound 6.3 (0.86) to 5.15(0.87) Passive stretches 6.1(0.89) to 4.9(0.88) |
Moderate quality of evidence | ||
| Interventions including hyperthermia or ultrasound versus passive stretches; n=37, male/female mixed sports54 | Within-in group baseline and follow-up scores (SD) of physical function (Constant and Murley score) Hyperthermia 58.6 (3.9) to 82.0 (5.7) Ultrasound 58.9(2.8) to 61.8(4.2) Passive stretches 59.5 (2.7) to 63.3 (5.6) |
Moderate quality of evidence | ||
| Shoulder pain | ||||
| Intervention including anteroposterior mobilisation of the shoulder joint vs manual treatment versus attention; n=31, male/female overhead athletes52 | Within-group changes (95% CI) of pain (NRS) Mobilisation 0.6 (0.1 to 1.1) Manual treatment 0.0 (0.0 to 0.3) Attention 0.2 (−0.2 to 0.7) |
Moderate quality of evidence | ||
| Intervention including anteroposterior mobilisation of the shoulder joint versus manual treatment versus attention; n=31, male/female overhead athletes52 | Within-group changes (95% CI) of physical function (DASH) Mobilisation 0.3 (−2.7 to 3.4) Manual treatment 0.5 (−0.3 to 1.3) Attention 0.7 (−0.6 to 2.0) |
Moderate quality of evidence | ||
| Intervention including posture correcting exercises versus no intervention; n=28, swimming53 | Within-in group baseline and follow-up scores (SD) of physical function and pain (ASES) Intervention Right shoulder: 89.1 (11.2) to 89.3 (14.6) Left shoulder: 89.9 (11.4) to 91.1 (10.6) Control Right shoulder: 90.8 (11.7) to 86.4 (17.9) Left shoulder: 90.7 (12.4) to 86.9 (15.5) |
Low quality of evidence | ||
| Intervention include strengthening exercises (no comparator group); n=29, male/female overhead athletes56 | Within-in group baseline and follow-up scores (SD) of pain (VAS) 3 months follow-up: 7.5 (2.3) to 3.4 (1.8) 6 months follow-up: 7.5 (2.3) to 2.9 (2.1) |
Very low quality of evidence | ||
| Intervention including scapula-focused stretching and strengthening exercises (no comparator group); n=31, male/female volleyball57 | Within-in group baseline and follow-up scores (SD) of pain (VAS) 3 months follow-up: 7.2 (1.3) to 2.4 (1.8) 6 months follow-up: 7.2 (1.3) to 2.6 (1.4) |
Very low quality of evidence | ||
ASES, The American Shoulder and Elbow Surgeons Shoulder Score; DASH, Disabilities of the Arm, Shoulder, and Hand; NRS, Numeric Rating Scale; SPADI, Shoulder Pain and Disability Index; VAS, Visual Analogue Scale.
Subacromial impingement syndrome
Limited evidence was found to guide the treatment of SIS. A single RCT51 in male baseball players observed a larger within-group reduction in shoulder pain after a programme combining warm-up modalities (laser, ultrasound, cycling, and stretching), shoulder strengthening exercises, and cool down (stretching, ice packs, electrotherapy, compression) performed three times per week for 12 weeks compared with no intervention (0–10 Numeric Rating Scale (NRS) mean (SD): intervention group changed from 7.88 (1.02) to 3.56 (1.31); control group from 7.71 (0.83) to 8.00 (0.88)) (moderate quality of evidence). The between-group difference and corresponding 95% CI were not reported. A prospective study55 of 47 young athletes showed reductions in pain and disability following daily shoulder strengthening exercises (Shoulder Pain and Disability Index mean (SD): from 29.86 (17.03) to 11.70 (13.78)) (very low quality of evidence).
Supraspinatus tendinopathy
One three-arm RCT54 allocated athletes randomly to hyperthermia (434 MHz, heating the skin to 38°C–40°C), continuous ultrasound (1 MHz, intensity 2.0 w/cm2), or exercise intervention. Hyperthermia and ultrasound were performed three times per week for 30 min for 4 weeks, while the exercise intervention was performed twice daily for 4 weeks. The effect of the intervention on pain and physical function was measured at end-of-the intervention using the mean of three Visual Analogue Scale scores (VAS) (at night, at rest and with movement, respectively), and the Constant and Murley score, respectively. The group receiving hyperthermia experienced significant improvements in pain (within-group change (SD): VAS 5.96 (0.83) to 1.2 (0.63), p=0.03) and physical function (within-group change (SD): from Constant and Murley score 58.57 (3.92) to 82 (5.73). The remaining groups experienced smaller and non-significant improvements in pain and physical function (moderate quality of evidence).
Shoulder pain
Two RCTs52 53 and two prospective studies56 57 were included. The highest quality of evidence was found for an intervention of one session of anteroposterior mobilisation of the glenohumeral joint compared with massage and attention controls in improving pain and physical function in 31 athletes from different sports.52 The group receiving anteroposterior mobilisation experienced a statistically significant reduction in shoulder pain measured using an 11-point NRS (within-group change (95% CI): 0.6 (0.1 to 1.1)) at end-of-intervention (moderate quality of evidence). The remaining groups experienced smaller and non-significant reductions in shoulder pain (manual contact: 0.0 (0.0 to 0.3), attention control: 0.2 (−0.2 to 0.7)). None of the group experienced a statistically significant improvement in physical function measured using the Disabilities of the Arm, Shoulder, and Hand (mobilisation: 0.3 (-2.7 to 3.4), manual contact: 0.5 (-0.3 to 1.3), attention control: 0.7 (-0.6 to 2.0)) (moderate quality of evidence). The remaining studies provided low to very low quality of evidence for the effect of posture correcting exercises, strengthening exercises, and a combination of strengthening and stretching exercises on pain and physical function.53 56 57
Discussion
The following paragraphs discuss the statements for diagnosis, prevention, and treatment, including the limitations in the existing literature.
Diagnosis
Diagnostic accuracy was based on studies with mixed populations with heterogeneous sex, age and activity levels but with clinical presentations likely comparable with athletes with shoulder injuries. High diagnostic accuracy was observed for 10 tests covering anterior instability, SLAP injuries and biceps-complex injuries. The positive apprehension test had the largest LR+ (17.21) of the three most commonly used anterior instability tests, which means that a positive test is highly effective at ruling in anterior instability.33 Conversely, there is uncertainty about whether a negative test rebuts anterior instability in patients who do not have anterior instability verified by arthroscopy. The combination of the apprehension and relocation tests was evaluated in traumatic anterior shoulder instability and showed an even higher LR+.58 Overall, the use of the apprehension test has good clinical utility for diagnosing anterior shoulder instability. The three-pack test for biceps-labrum complex injuries has been presented with test performances related to the exact point of interest (bicipital tunnel, inside, junctional), with varying diagnostic accuracy. Regrettably, no data is available concerning the combination of the three tests, although the name could indicate that it is a test battery and intended to be used as such. However, from a clinical perspective, the data supports the relevance of the three-pack tests to rule out an injury, while we propose that a positive test must be interpreted with caution. The Biceps Load II test had a high LR+and low LR− for ruling in and out a SLAP injury in patients with shoulder pain and can be either performed alone or after a positive test in one or more of the three three-pack tests. The internal rotation lag test had a low LR− to rule out rupture of the subscapularis muscle, and moderate diagnostic accuracy was observed for the internal rotation lag and external rotation lag for supraspinatus and infraspinatus. The diagnostic tests available for subacromial impingement, internal posterosuperior impingement, and rotator cuff injury (not rupture) showed low to very low diagnostic accuracy and low quality of evidence, and their utility in correctly identifying injury is therefore questionable. Concerning subacromial impingement, the diagnosis describes the clinical entity of a painful and functionally impaired shoulder usually experienced when combining shoulder elevation and rotation. Current data do not support the use of the Composite test, and this corresponds well with the unknown pathogenesis of the injury. Diagnostic ultrasound may be a valuable supportive tool in the clinical assessment of shoulder injuries in sport to evaluate structural integrity.59
Prevention
Eight studies investigating the prevention of the selected shoulder injuries were identified, with six including overhead athletes (three handball and three baseball). Four studies had a moderate quality of evidence: (1) The OSTRC Shoulder Injury Prevention programme (moderate effect size) aims to increase internal glenohumeral rotation, external rotation strength and scapular muscle strength, as well as improve kinetic chain and thoracic mobility.1 However, the exercise programme did not affect the risk factors external rotation strength and internal rotation range of motion.60 The preventive effect of the programme must therefore be due to other factors; (2) The Shoulder Control programme was tested in 15–19 years handball-players with the aim of increasing shoulder and trunk strength and control, trunk mobility, and handball throwing load by using five principal exercises with four progressive levels performed as part of the warm-up routine.47 The absolute risk reduction was 11% (95% CI 4% to 18%). (3) The throwing injury prevention programme (large effect size) was tested in 9–11 years old baseball players and consisted of stretching, dynamic mobility and balance training during warm-up and showed a 52% injury risk reduction43; (4) The FIFA 11+shoulder prevention programme has a large effect size and was developed for goalkeepers and consisted of general warming-up exercises, exercises to improve strength and balance of the shoulder, elbow, wrist and finger muscles, and advanced exercises for core stability and muscle control.44 61 The evidence of effect of exercise in preventing sports-related shoulder injuries is evolving. Despite few identified studies of moderate evidence quality, the effect sizes are comparable to other body regions.62 Our findings provide preliminary data to support the implementation of shoulder prevention programmes—in line with the recommendations from a recent consensus statement which concluded that ‘injury prevention programmes/exercises are appropriate to prescribe for athletes of all levels to prevent shoulder injury’.8 However, three studies of low quality showed no preventative effect of exercise-based interventions, suggesting that investigations into differences in effects of exercise intervention characteristics (ie, frequency, type, dose, volume) is necessary to guide clinical practice. Further, we recognise that effective shoulder injury prevention programmes do not always directly elicit improvements in modifiable risk factors60 (eg, glenohumeral internal rotation deficit, muscular imbalances, or scapula dyskinesis),5 6 and that exercise progressions1 44 and exercises individualised to sports-specific movements throughout the whole range of motion may be preferable.1 8
Treatment
The low number of studies investigating the treatment of the selected shoulder injuries in the athletic population is detrimental and calls for action. There was very low to moderate quality of evidence for a large effect of exercise-based treatment for subacromial impingement and shoulder pain.51 55–57 There was moderate quality of evidence of a small effect with manual treatment in overhead athletes on reducing shoulder pain on short term.52 These findings, although based on little evidence, are in line with current weak recommendations for exercise-based interventions in the general population to reduce pain and increase shoulder function.63 For the treatment of supraspinatus tendinopathy, hyperthermia treatment resulted in a large effect size in reducing pain and disability compared with ultrasound or pendular swinging and stretching exercises (low quality of evidence). However, this treatment is rarely used in a clinical sports setting and cannot be recommended based on the current study.
Limitations and methodological considerations
This paper has some limitations. First, inconsistent terminology and lack of consensus on definition and classification of shoulder injuries in the existing literature challenged the selection of diagnoses relevant for inclusion in this position statement. As such, we included diagnoses with different mechanisms and presentations that may represent the spectrum from acute, sudden-onset injuries to repetitive, gradual-onset injuries, including shoulder pain. Although we were unable to identify whether shoulder injuries in the individual studies may be the result of trauma or (in)direct contact mechanisms, we excluded diagnoses likely to be solely of traumatic origin (ie, dislocations and fractures). Furthermore, we emphasise that shoulder injuries are often not restricted to single structures, but may involve multiple structures, which may confound a test specific to a single tissue or dysfunction. Chronic shoulder injuries, SIS, supraspinatus tendinopathy, and shoulder pain may be considered within the same spectrum, challenging separate categorisation.
Most studies included a majority of young male athletes. As such, our results may have limited application to female athletes and athletes above the age of 25. In addition, none of the included studies reported data on race, socioeconomic status or other social determinants, thus hindering an evaluation of the applicability of the findings according to these characteristics. Future studies should prioritise the inclusion of more diverse samples and report more detailed information on athlete characteristics.
We selected a sample of clinical tests that reflected current best practice for the included shoulder injuries. However, we acknowledge the vast number of tests available in the literature. Furthermore, as limited evidence was available to guide the diagnosis of shoulder injuries in athletes, we included diagnostic studies of non-athlete populations, but we believe it is unlikely that these tests perform very differently in athlete than in non-athlete populations.
Finally, we did not perform risk of bias assessments of the individual studies if an assessment was already available as part of a systematic review. This was chosen a priori to acknowledge the original study findings but may introduce risk of bias, and potential rating discrepancies may exist due to differences in interpretation of risk of bias domains. However, since GRADE represents an overall assessment encompassing several domains and thus does not rely only on risk of bias,24 potential discrepancies are unlikely to change the quality of evidence provided in the present statement paper. As we were unable to pool individual study results, inconsistency was not reported in the GRADE assessments. As such, the quality of evidence may change when future studies are published and compared with the current body of literature.
Conclusion
We have graded the quality of evidence concerning diagnosis, prevention and treatment of common shoulder injuries and provide a comprehensive and up-to-date summary of the best available evidence. High diagnostic accuracy was observed for 10 tests covering anterior instability, SLAP injuries and biceps-complex injuries, and these can be used confidently in a clinical setting. For prevention, based on a few high-quality studies, implementing a shoulder injury prevention programme showed a moderate to large effect size in reducing the risk of shoulder injuries compared with no intervention. For the treatment of the selected shoulder injuries, choosing an active rehabilitation programme seems to be beneficial compared with passive modalities in reducing pain and disability. However, the evidence for most estimates were graded very low to moderate, indicating that future high-quality research may alter our findings.
Acknowledgments
We would like to acknowledge the Danish Society of Sports Physical Therapy (DSSF) for supporting this project.
Footnotes
Twitter: @behnam_liaghat, @JulieKRPedersen, @Husted_RS, @Lislunped, @KThorborg, @BoghJuhl
Contributors: BL, JRP, RSH, KT, LLP and CBJ conceived the study idea. BL and JRP performed the systematic searches with input from RSH, KT, LLP and CBJ. BL and JRP conducted risk of bias assessments and GRADE assessments. BL and JRP wrote the initial draft. All authors revised the draft critically and agreed on the final version.
Funding: The Danish Society of Sports Physical Therapy initiated the project and provided financial support to authors (BL, JRP, RSH, LLP and KT).
Competing interests: KT is Deputy Editor in BJSM. KT and JRP have received grants from the Danish Society of Sports Physical Therapy unrelated to the present study.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Ethics statements
Patient consent for publication
Not applicable.
References
- 1. Andersson SH, Bahr R, Clarsen B, et al. Preventing overuse shoulder injuries among throwing athletes: a cluster-randomised controlled trial in 660 elite handball players. Br J Sports Med 2017;51:1073–80. 10.1136/bjsports-2016-096226 [DOI] [PubMed] [Google Scholar]
- 2. Seminati E, Minetti AE. Overuse in volleyball training/practice: a review on shoulder and spine-related injuries. Eur J Sport Sci 2013;13:732–43. 10.1080/17461391.2013.773090 [DOI] [PubMed] [Google Scholar]
- 3. Walker H, Gabbe B, Wajswelner H, et al. Shoulder pain in swimmers: a 12-month prospective cohort study of incidence and risk factors. Phys Ther Sport 2012;13:243–9. 10.1016/j.ptsp.2012.01.001 [DOI] [PubMed] [Google Scholar]
- 4. Chase KI, Caine DJ, Goodwin BJ, et al. A prospective study of injury affecting competitive collegiate swimmers. Res Sports Med 2013;21:111–23. 10.1080/15438627.2012.757224 [DOI] [PubMed] [Google Scholar]
- 5. Asker M, Brooke HL, Waldén M, et al. Risk factors for, and prevention of, shoulder injuries in overhead sports: a systematic review with best-evidence synthesis. Br J Sports Med 2018;52:1312–9. 10.1136/bjsports-2017-098254 [DOI] [PubMed] [Google Scholar]
- 6. Tooth C, Gofflot A, Schwartz C, et al. Risk factors of overuse shoulder injuries in overhead athletes: a systematic review. Sports Health 2020;12:478–87. 10.1177/1941738120931764 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Wright AA, Ness BM, Donaldson M, et al. Effectiveness of shoulder injury prevention programs in an overhead athletic population: a systematic review. Phys Ther Sport 2021;52:189–93. 10.1016/j.ptsp.2021.09.004 [DOI] [PubMed] [Google Scholar]
- 8. Schwank A, Blazey P, Asker M, et al. 2022 Bern consensus statement on shoulder injury prevention, rehabilitation, and return to sport for athletes at all participation levels. J Orthop Sports Phys Ther 2022;52:11–28. 10.2519/jospt.2022.10952 [DOI] [PubMed] [Google Scholar]
- 9. Forthomme B, Wieczorek V, Frisch A, et al. Shoulder pain among high-level volleyball players and preseason features. Med Sci Sports Exerc 2013;45:1852–60. 10.1249/MSS.0b013e318296128d [DOI] [PubMed] [Google Scholar]
- 10. Fares MY, Fares J, Baydoun H, et al. Prevalence and patterns of shoulder injuries in major league baseball. Phys Sportsmed 2020;48:63–7. 10.1080/00913847.2019.1629705 [DOI] [PubMed] [Google Scholar]
- 11. Miller AH, Evans K, Adams R, et al. Shoulder injury in water polo: a systematic review of incidence and intrinsic risk factors. J Sci Med Sport 2018;21:368–77. 10.1016/j.jsams.2017.08.015 [DOI] [PubMed] [Google Scholar]
- 12. Bahr R, Clarsen B, Derman W, et al. International Olympic Committee consensus statement: methods for recording and reporting of epidemiological data on injury and illness in sport 2020 (including STROBE extension for sport injury and illness surveillance (STROBE-SIIS)). Br J Sports Med 2020;54:372–89. 10.1136/bjsports-2019-101969 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Hawkins RJ, Kennedy JC. Impingement syndrome in athletes. Am J Sports Med 1980;8:151–8. 10.1177/036354658000800302 [DOI] [PubMed] [Google Scholar]
- 14. Paley KJ, Jobe FW, Pink MM, et al. Arthroscopic findings in the overhand throwing athlete: evidence for posterior internal impingement of the rotator cuff. Arthroscopy 2000;16:35–40. 10.1016/s0749-8063(00)90125-7 [DOI] [PubMed] [Google Scholar]
- 15. Andrews JR, Carson WG, McLeod WD. Glenoid labrum tears related to the long head of the biceps. Am J Sports Med 1985;13:337–41. 10.1177/036354658501300508 [DOI] [PubMed] [Google Scholar]
- 16. Carvalho CD, Cohen C, Belangero PS, et al. Partial rotator cuff injury in athletes: bursal or articular? Rev Bras Ortop 2015;50:416–21. 10.1016/j.rboe.2015.06.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Wilbur RR, Shirley MB, Nauert RF, et al. Anterior shoulder instability in throwers and overhead athletes: long-term outcomes in a geographic cohort. Am J Sports Med 2022;50:182–8. 10.1177/03635465211059195 [DOI] [PubMed] [Google Scholar]
- 18. Fuller CW, Ekstrand J, Junge A, et al. Consensus statement on injury definitions and data collection procedures in studies of football (soccer) injuries. Br J Sports Med 2006;40:193–201. 10.1136/bjsm.2005.025270 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Durieux N, Vandenput S, Pasleau F. [OCEBM levels of evidence system]. Rev Med Liege 2013;68:644–9. [PubMed] [Google Scholar]
- 20. Sterne JAC, Savović J, Page MJ, et al. Rob 2: a revised tool for assessing risk of bias in randomised trials. BMJ 2019;366:l4898. 10.1136/bmj.l4898 [DOI] [PubMed] [Google Scholar]
- 21. Whiting PF, Rutjes AWS, Westwood ME, et al. QUADAS-2: a revised tool for the quality assessment of diagnostic accuracy studies. Ann Intern Med 2011;155:529–36. 10.7326/0003-4819-155-8-201110180-00009 [DOI] [PubMed] [Google Scholar]
- 22. Sterne JA, Hernán MA, Reeves BC, et al. ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. BMJ 2016;355:i4919. 10.1136/bmj.i4919 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Whiting P, Savović J, Higgins JPT, et al. ROBIS: a new tool to assess risk of bias in systematic reviews was developed. J Clin Epidemiol 2016;69:225–34. 10.1016/j.jclinepi.2015.06.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Schünemann H, Brożek J, Guyatt G. Handbook for grading the quality of evidence and the strength of recommendations using the grade approach. Vol. 2013, 2013. [Google Scholar]
- 25. Guyatt GH, Oxman AD, Vist G, et al. GRADE guidelines: 4. Rating the quality of evidence--study limitations (risk of bias). J Clin Epidemiol 2011;64:407–15. 10.1016/j.jclinepi.2010.07.017 [DOI] [PubMed] [Google Scholar]
- 26. Guyatt GH, Oxman AD, Kunz R, et al. GRADE guidelines 6. Rating the quality of evidence--imprecision. J Clin Epidemiol 2011;64:1283–93. 10.1016/j.jclinepi.2011.01.012 [DOI] [PubMed] [Google Scholar]
- 27. Guyatt GH, Oxman AD, Kunz R, et al. GRADE guidelines: 7. Rating the quality of evidence--inconsistency. J Clin Epidemiol 2011;64:1294–302. 10.1016/j.jclinepi.2011.03.017 [DOI] [PubMed] [Google Scholar]
- 28. Guyatt GH, Oxman AD, Kunz R, et al. GRADE guidelines: 8. Rating the quality of evidence--indirectness. J Clin Epidemiol 2011;64:1303–10. 10.1016/j.jclinepi.2011.04.014 [DOI] [PubMed] [Google Scholar]
- 29. Guyatt GH, Oxman AD, Montori V, et al. GRADE guidelines: 5. Rating the quality of evidence--publication bias. J Clin Epidemiol 2011;64:1277–82. 10.1016/j.jclinepi.2011.01.011 [DOI] [PubMed] [Google Scholar]
- 30. McGee S. Simplifying likelihood ratios. J Gen Intern Med 2002;17:646–9. 10.1046/j.1525-1497.2002.10750.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Jaeschke R, Guyatt GH, Sackett DL. Users' guides to the medical literature. III. How to use an article about a diagnostic test. B. What are the results and will they help me in caring for my patients? The evidence-based medicine working group. JAMA 1994;271:703–7. 10.1001/jama.271.9.703 [DOI] [PubMed] [Google Scholar]
- 32. Thorlund JB, Juhl CB, Ingelsrud LH, et al. Risk factors, diagnosis and non-surgical treatment for meniscal tears: evidence and recommendations: a statement paper commissioned by the danish society of sports physical therapy (DSSF). Br J Sports Med 2018;52:557–65. 10.1136/bjsports-2017-098429 [DOI] [PubMed] [Google Scholar]
- 33. Hegedus EJ, Goode AP, Cook CE, et al. Which physical examination tests provide clinicians with the most value when examining the shoulder? Update of a systematic review with meta-analysis of individual tests. Br J Sports Med 2012;46:964–78. 10.1136/bjsports-2012-091066 [DOI] [PubMed] [Google Scholar]
- 34. Hermans J, Luime JJ, Meuffels DE, et al. Does this patient with shoulder pain have rotator cuff disease?: the rational clinical examination systematic review. JAMA 2013;310:837–47. 10.1001/jama.2013.276187 [DOI] [PubMed] [Google Scholar]
- 35. Kim SH, Ha KI, Ahn JH, et al. Biceps load test II: a clinical test for slap lesions of the shoulder. Arthroscopy 2001;17:160–4. 10.1053/jars.2001.20665 [DOI] [PubMed] [Google Scholar]
- 36. Taylor SA, Newman AM, Dawson C, et al. The "3-pack" examination Is critical for comprehensive evaluation of the biceps-labrum complex and the bicipital tunnel: a prospective study. Arthroscopy 2017;33:28–38. 10.1016/j.arthro.2016.05.015 [DOI] [PubMed] [Google Scholar]
- 37. Meister K, Buckley B, Batts J. The posterior impingement sign: diagnosis of rotator cuff and posterior labral tears secondary to internal impingement in overhand athletes. Am J Orthop 2004;33:412–5. [PubMed] [Google Scholar]
- 38. Michener LA, Walsworth MK, Doukas WC, et al. Reliability and diagnostic accuracy of 5 physical examination tests and combination of tests for subacromial impingement. Arch Phys Med Rehabil 2009;90:1898–903. 10.1016/j.apmr.2009.05.015 [DOI] [PubMed] [Google Scholar]
- 39. Chew K, Pua Y, Chin J. Clinical predictors for the diagnosis of supraspinatus pathology. Physiotherapy Singapore 2010;13:12–17. [Google Scholar]
- 40. Silva L, Andréu JL, Muñoz P, et al. Accuracy of physical examination in subacromial impingement syndrome. Rheumatology 2008;47:679–83. 10.1093/rheumatology/ken101 [DOI] [PubMed] [Google Scholar]
- 41. Salaffi F, Ciapetti A, Carotti M, et al. Clinical value of single versus composite provocative clinical tests in the assessment of painful shoulder. J Clin Rheumatol 2010;16:105–8. 10.1097/RHU.0b013e3181cf8392 [DOI] [PubMed] [Google Scholar]
- 42. Miller CA, Forrester GA, Lewis JS. The validity of the lag signs in diagnosing full-thickness tears of the rotator cuff: a preliminary investigation. Arch Phys Med Rehabil 2008;89:1162–8. 10.1016/j.apmr.2007.10.046 [DOI] [PubMed] [Google Scholar]
- 43. Sakata J, Nakamura E, Suzuki T, et al. Throwing injuries in youth baseball players: can a prevention program help? A randomized controlled trial. Am J Sports Med 2019;47:2709–16. 10.1177/0363546519861378 [DOI] [PubMed] [Google Scholar]
- 44. Al Attar WSA, Faude O, Bizzini M, et al. The FIFA 11+ shoulder injury prevention program was effective in reducing upper extremity injuries among soccer goalkeepers: a randomized controlled trial. Am J Sports Med 2021;49:2293–300. 10.1177/03635465211021828 [DOI] [PubMed] [Google Scholar]
- 45. Swanik KA, Swanik CB, Lephart SM, et al. The effect of functional training on the incidence of shoulder pain and strength in intercollegiate swimmers. J Sport Rehabil 2002;11:140–54. 10.1123/jsr.11.2.140 [DOI] [Google Scholar]
- 46. Sommervold M, Østerås H. What is the effect of a shoulder-strengthening program to prevent shoulder pain among junior female team handball players? Open Access J Sports Med 2017;8:61–70. 10.2147/OAJSM.S127854 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Asker M, Hägglund M, Waldén M, et al. The effect of shoulder and knee exercise programmes on the risk of shoulder and knee injuries in adolescent elite handball players: a three-armed cluster randomised controlled trial. Sports Med Open 2022;8:91. 10.1186/s40798-022-00478-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Achenbach L, Huppertz G, Zeman F, et al. Multicomponent stretching and rubber band strengthening exercises do not reduce overuse shoulder injuries: a cluster randomised controlled trial with 579 handball athletes. BMJ Open Sport Exerc Med 2022;8:e001270. 10.1136/bmjsem-2021-001270 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Pas HIMFL, Pluim BM, Kilic O, et al. Effectiveness of an e-health tennis-specific injury prevention programme: randomised controlled trial in adult recreational tennis players. Br J Sports Med 2020;54:1036–41. 10.1136/bjsports-2019-101142 [DOI] [PubMed] [Google Scholar]
- 50. Shitara H, Yamamoto A, Shimoyama D, et al. Shoulder stretching intervention reduces the incidence of shoulder and elbow injuries in high school baseball players: a time-to-event analysis. Sci Rep 2017;7:45304. 10.1038/srep45304 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Cha J-Y, Kim J-H, Hong J, et al. A 12-week rehabilitation program improves body composition, pain sensation, and internal/external torques of baseball pitchers with shoulder impingement symptom. J Exerc Rehabil 2014;10:35–44. 10.12965/jer.140087 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. E L, Pecos-Martín D, Domenech-García V, et al. Effects of an anteroposterior mobilization of the glenohumeral joint in overhead athletes with chronic shoulder pain: a randomized controlled trial. Musculoskelet Sci Pract 2018;38:91–8. 10.1016/j.msksp.2018.09.009 [DOI] [PubMed] [Google Scholar]
- 53. Lynch SS, Thigpen CA, Mihalik JP, et al. The effects of an exercise intervention on forward head and rounded shoulder postures in elite swimmers. Br J Sports Med 2010;44:376–81. 10.1136/bjsm.2009.066837 [DOI] [PubMed] [Google Scholar]
- 54. Giombini A, Di Cesare A, Safran MR, et al. Short-term effectiveness of hyperthermia for supraspinatus tendinopathy in athletes: a short-term randomized controlled study. Am J Sports Med 2006;34:1247–53. 10.1177/0363546506287827 [DOI] [PubMed] [Google Scholar]
- 55. De Mey K, Danneels L, Cagnie B, et al. Scapular muscle rehabilitation exercises in overhead athletes with impingement symptoms: effect of a 6-week training program on muscle recruitment and functional outcome. Am J Sports Med 2012;40:1906–15. 10.1177/0363546512453297 [DOI] [PubMed] [Google Scholar]
- 56. Merolla G, De Santis E, Campi F, et al. Supraspinatus and infraspinatus weakness in overhead athletes with scapular dyskinesis: strength assessment before and after restoration of scapular musculature balance. Musculoskelet Surg 2010;94:119–25. 10.1007/s12306-010-0082-7 [DOI] [PubMed] [Google Scholar]
- 57. Merolla G, De Santis E, Sperling JW, et al. Infraspinatus strength assessment before and after scapular muscles rehabilitation in professional volleyball players with scapular dyskinesis. J Shoulder Elbow Surg 2010;19:1256–64. 10.1016/j.jse.2010.01.022 [DOI] [PubMed] [Google Scholar]
- 58. Farber AJ, Castillo R, Clough M, et al. Clinical assessment of three common tests for traumatic anterior shoulder instability. J Bone Joint Surg Am 2006;88:1467–74. 10.2106/JBJS.E.00594 [DOI] [PubMed] [Google Scholar]
- 59. Liang W, Wu H, Dong F, et al. Diagnostic performance of ultrasound for rotator cuff tears: a systematic review and meta-analysis. Med Ultrason 2020;22:197–202. 10.11152/mu-2352 [DOI] [PubMed] [Google Scholar]
- 60. Fredriksen H, Cools A, Bahr R, et al. Does an effective shoulder injury prevention program affect risk factors in handball? A randomized controlled study. Scand J Med Sci Sports 2020;30:1423–33. 10.1111/sms.13674 [DOI] [PubMed] [Google Scholar]
- 61. Ejnisman B, Barbosa G, Andreoli CV, et al. Shoulder injuries in soccer goalkeepers: review and development of a FIFA 11+ shoulder injury prevention program. Open Access J Sports Med 2016;7:75–80. 10.2147/OAJSM.S97917 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Ishøi L, Krommes K, Husted RS, et al. Diagnosis, prevention and treatment of common lower extremity muscle injuries in sport - grading the evidence: a statement paper commissioned by the danish society of sports physical therapy (DSSF). Br J Sports Med 2020;54:528–37. 10.1136/bjsports-2019-101228 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Liaghat B, Ussing A, Petersen BH, et al. Supervised training compared with no training or self-training in patients with subacromial pain syndrome: a systematic review and meta-analysis. Arch Phys Med Rehabil 2021;102:2428–41. 10.1016/j.apmr.2021.03.027 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bjsports-2022-105674supp001.pdf (1.4MB, pdf)
bjsports-2022-105674supp002.pdf (32.6KB, pdf)
bjsports-2022-105674supp003.pdf (119.6KB, pdf)