Abstract
Objective
To conduct a meta-analysis to evaluate the effect of endovascular therapy (EVT) in mild acute ischemic stroke (AIS) due to proximal versus distal occlusions.
Methods
We searched PubMed, Embase, the Cochrane Library, and clinicaltrials.gov from January 2000 to September 2021 to identify studies comparing EVT versus best medical management (BMM) in AIS with National Institutes of Health Stroke Scale (NIHSS) scores ≤5 due to proximal internal carotid artery (ICA) or M1 versus distal M2 occlusions. We included studies that reported the number of patients with proximal or distal occlusions separately and reported the number of patients with freedom of disability (modified Rankin Scale (mRS) score 0–1) or functional independence (mRS score 0–2) at 90 days in proximal or M2 occlusions, respectively. OR with 95% CI was used.
Results
We identified six studies with 653 proximal ICA and M1 occlusion patients and 666 distal M2 occlusion patients. Pooled results showed EVT versus BMM was associated with a higher rate of being disability-free in patients with proximal occlusions (OR 1.58, 95% CI 1.09 to 2.30), but was associated with a lower rate of being disability-free in patients with M2 occlusions (OR 0.70, 95% CI 0.49 to 0.99). Effect of EVT in proximal versus distal occlusions was substantially different (P for interaction=0.002). A similar pattern was seen for functional independence (P for interaction=0.05).
Conclusions
For patients with mild AIS, observational data suggest that EVT may be beneficial for proximal ICA or M1 but not for distal M2 occlusions. Randomized trials are needed to confirm these findings.
PROSPERO registration number
CRD42021281034.
Keywords: Thrombectomy, Stroke, Thrombolysis
Introduction
Among patients with mild acute ischemic stroke (AIS) in the anterior circulation, nearly one-third harbor occlusions in the internal carotid artery (ICA), M1 middle cerebral artery (MCA), or M2 MCA when imaged with CT angiography or MR angiography within 6 hours of symptom onset.1 A substantial proportion of patients presenting with a low National Institutes of Health Stroke Scale (NIHSS) score have unfavorable functional outcomes when an ICA or M1 occlusion is present.2–4 Endovascular therapy (EVT) works well at reperfusing occluded large, proximal cerebral vessels and has become the standard reperfusion therapy for AIS due to ICA and M1 occlusions in the anterior circulation with NIHSS scores >5.5 However, only 14 of the 1916 randomized patients in the pivotal EVT trials had NIHSS scores ≤56; therefore it is unknown whether EVT is superior to best medical management (BMM) in strokes with NIHSS scores ≤5 due to large vessel occlusions (LVOs). Even less randomized data are available regarding mild deficit patients with more distal M2 MCA occlusions, as several of the pivotal trials excluded M2 MCA patients. M2 MCA occlusions can occur in vessel segments that are large (LVO ≥2 mm in diameter) or medium (medium vessel occlusion (MVO) 0.75–1.9 mm in diameter).7 While M2 segment occlusions may be LVOs or MVOs, all are distal vessel occlusions (DVOs) occurring in vessels that can be reached only by further and more tortuous endovascular navigation.
There are potential reasons that, among patients with mild ischemic stroke, EVT may be of greater benefit over BMM for proximal ICA or M1 than distal M2 occlusions. Mild deficit proximal occlusion patients fare worse than distal occlusion patients when treated with medical management, showing higher frequencies of early neurologic deterioration.8 9 Conversely, mild deficit distal occlusion patients may fare worse when treated with EVT, showing more frequent symptomatic hemorrhagic transformation.10 We therefore performed a systematic review and meta-analysis to evaluate the effect of EVT in AIS with NIHSS scores ≤5 and proximal ICA or M1 versus distal M2 occlusions.
Methods
This study was performed in accordance with the recommendations of the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA statement).10 This study was a systematic review and meta-analysis and did not need institutional review board or ethics committee approval.
Data sources and searches
We searched PubMed, Embase, the Cochrane Library, and the clinical trial registry maintained at clinicaltrials.gov from January 1, 2000 to September 30, 2021 with the terms: ‘stroke or cerebrovascular accident’ or ‘brain vascular accident’ or ‘cerebral infarct or intracranial vascular disease’ or ‘cerebrovascular disease or brain vascular disorder’ or ‘cerebrovascular occlusion’ or ‘cerebrovascular insufficiency’ AND ‘mild or minor or low NIHSS’ or ‘low National Institutes of Health Stroke Scale’ AND ‘large vessel occlusions’ or ‘internal carotid artery occlusion’ or ‘middle cerebral artery occlusion’ or ‘M1 occlusion’ or ‘M2 occlusion’ AND ‘endovascular thrombectomy’ or ‘endovascular therapy’ or ‘mechanic thrombectomy’ or ‘intra-arterial therapy’. We limited search results to humans. We also reviewed the introduction and discussion sections of retrieved studies and of prior meta-analyses to identify additional studies.11 12
Study selection and data extraction
Criteria for inclusion of a study were as follows: (1) the study design was a randomized controlled trial or cohort study; (2) patients with AIS and NIHSS scores ≤5; (3) the active treatment group consisted of EVT (with or without intravenous thrombolysis (IVT)); (4) the control group consisted of BMM (with IVT if suitable); (5) reported number of patients with proximal ICA or M1, M1, or distal M2 occlusion separately; (6) reported number of patients with freedom of disability, defined as modified Rankin Scale (mRS) score 0 to 1 or functional independence (mRS score 0 to 2), at 90 days, in proximal ICA or M1 or distal M2 occlusions separately. Exclusion criteria were: (1) studies with some patients having NIHSS scores >5; (2) rescue EVT used after early neurological deterioration in either the active or control arm. One investigator extracted the data and another investigator reviewed the extracted data. Any discrepant judgments were resolved by joint discussion.
Study quality
We assessed the quality of eligible studies. Assessment was based on guidelines developed by the US Preventive Task Force as well as the modified checklist used in previous studies.13 14 We assessed four characteristics: prospective study design, comparable group available, adjustment of potential confounders (ie, age, sex, and baseline NIHSS scores), and documented loss of follow-up rate.
Statistical analyses
The primary outcome was freedom of disability (mRS 0–1) at 90 days. For randomized controlled trials of AIS, investigators usually chose an appropriate primary outcome according to the baseline NIHSS scores to differentiate the effect of treatment. For example, mRS 0–1 was used as the primary outcome for trials of IVT (median NIHSS score 9)15 and dual antiplatelet therapies (median NIHSS score 2) in AIS,16 mRS 0–2 for a trial of EVT in AIS due to LVO (median NIHSS score 17),17 and mRS 0–3 for a trial of EVT in AIS due to LVO with a large ischemic region (median NIHSS score 22).18 Because this meta-analysis only included studies with patients having NIHSS scores ≤5, we chose mRS 0–1 as the primary outcome. The secondary outcomes were functional independence (mRS 0–2), symptomatic intracranial hemorrhage (ICH), any ICH, and all-cause mortality. The Cochrane Collaboration’s Review Manager Software Package (RevMan 5.4.1) was used for the meta-analysis. Odds ratio (OR) with 95% confidence interval (95% CI) was used as a measure of the association between EVT and outcomes. All reported p values were two-sided, with significance set at <0.05. Heterogeneity was assessed by the p value of χ2 statistics and I2. We regarded an I2 value <40% as ‘heterogeneity might not be important’ and >75% as ‘considerable heterogeneity’ based on the suggestion of the Cochrane Handbook for Systematic Reviews of Interventions.19 20 We pooled data across studies by using the fixed-effects model based on an inverse variance method and compared the results with those obtained from a random-effects model. We also performed sensitivity tests to further explore the robustness of our results for the primary outcome (mRS 0–1). We evaluated the effect of EVT in M1 versus M2 occlusion. We compared EVT with IVT by excluding studies with some patients in the control arm not receiving IVT. Since devices and techniques of EVT evolve over time, and to make the results compatible with current EVT practice, we restricted analysis to studies with all patients enrolled after 2011, considering the earliest EVT beneficial-proven trial (MR CLEAN: a Multicenter Randomized CLinical trial of Endovascular treatment for Acute ischemic stroke in the Netherlands) started enrolling patients from December 2010.21 Also, we tried to identify the percentage of included patients who were treated after 2015 because modern devices might more effectively remove distal lesions and might affect outcomes.
Results
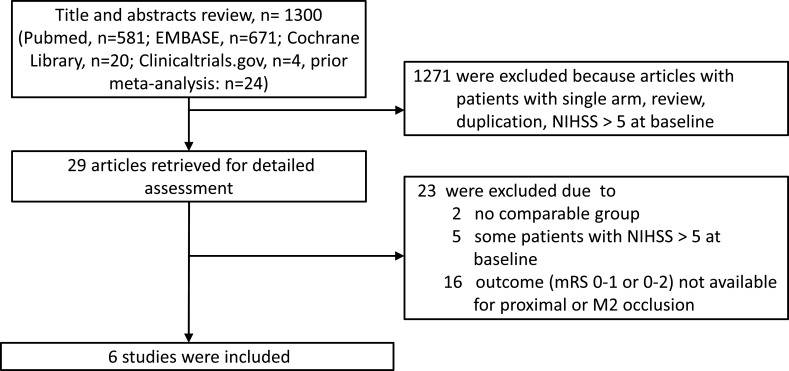
Of the 29 studies retrieved for detailed assessment, two were excluded due to no comparable group in two studies, some patients having NIHSS scores >5 at baseline in five studies, or not reporting number of patients with freedom of disability or functional independence at 90 days in proximal ICA or M1 versus distal M2 occlusions separately in 16 studies (figure 1). Our final analysis included six studies,10 12 22–25 comprising 653 patients with proximal ICA or M1 occlusions and 666 patients with distal M2 occlusions, respectively, and NIHSS scores ≤5. Among patients with proximal ICA or M1 occlusions, 360 patients received EVT and 293 patients received BMM. Among patients with distal M2 occlusions, 236 patients received EVT and 430 patients received BMM. The study design, quality, and baseline characteristics of these included studies are shown in table 1. Mean age, percentage of men or women, comorbidity (eg, atrial fibrillation), and median NIHSS score were not available because almost all of the included studies were not designed to explore the effect of EVT on specific vessel occlusion sites and we only retrieved the subset of data from these studies for the purpose of this meta-analysis. Only one study provided the percentage of patients who were treated after 2015 and this study showed that 111 out of 169 patients (65.7%) were treated after 2015, and mRS 0–1 at 3 months was not significantly different between the EVT versus IVT groups in mild ischemic stroke due to distal M2 occlusions.24
Figure 1.
Flow of study selection. mRS, modified Rankin Scale; M2, second segment of middle cerebral artery; NIHSS, National Institutes of Health Stroke Scale.
Table 1.
Characteristics of included studies
| Dobrocky et al 24 | Goyal et al 12 | Messer et al 25 | Saito et al 22 | Sarraj et al 23 | Seners et al 10 | |
| Countries | Switzerland, Germany | North America, Europe, Asia |
Germany | Japan | USA, Spain | France |
| Study duration (dates) | 2005–2020 | 2013–2017 | 1998–2015 | 2014–2016 | 2012–2017 | 2006–2018 |
| NIHSS score | ≤5 | ≤5 | ≤5 | ≤5 | ≤5 | ≤5 |
| Active group | EVT±IVT | EVT±IVT | EVT±IVT | EVT±IVT | EVT±IVT | EVT±IVT |
| Comparator group | IVT | BMM (including IVT) | IVT | IVT | BMM (including IVT) | IVT |
| Outcome available in vessel occlusion sites | M2 | Proximal ICA or M1 and M2 | Proximal ICA or M1 | Proximal ICA or M1 | Proximal ICA or M1, M1, and M2 | M1 and M2 |
| ICA or M1 occlusions | 0 | 172 | 26 | 81 | 122 | 252 |
| M2 occlusions | 164 | 79 | 0 | NA | 77 | 346 |
| Prospective study design | No | No | No | No | No | Yes |
| Comparable group available | Yes | Yes | Yes | Yes | Yes | Yes |
| Adjustment of confounders | No | No | No | No | No | No |
| Documented loss of follow-up rate | No | No | No | No | No | No |
BMM, best medical management; EVT, endovascular therapy; ICA, internal carotid artery; IVT, intravenous thrombolysis; M1, first segment of middle cerebral artery; M2, second segment of middle cerebral artery; NA, not available.
Primary outcome
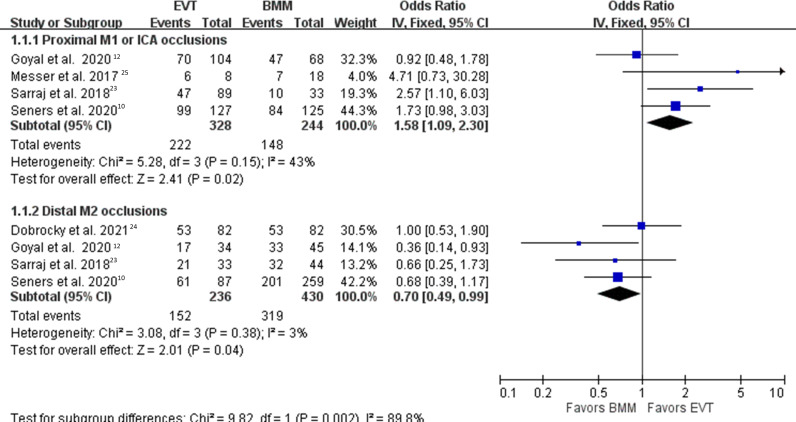
For AIS patients with NIHSS scores ≤5, pooled results from the fixed-effect model showed that EVT compared with BMM was associated with a higher rate of being disability-free in patients with proximal ICA or M1 occlusions (67.6% vs 60.6%; OR 1.58, 95% CI 1.09 to 2.30, p=0.02),10 12 23 25 but was associated with a lower rate of being disability-free in patients with distal M2 occlusions (64.4% vs 74.1%; OR 0.70, 95% CI 0.49 to 0.99, p=0.04),10 12 23 24 and the effect of EVT in the proximal ICA or M1 versus distal M2 occlusions was substantially different (P for interaction=0.002, I2=90%) (figure 2).
Figure 2.
Freedom of disability. Forest plot comparing EVT versus BMM for freedom of disability (modified Rankin Scale 0–1) in proximal ICA or M1 versus distal M2 occlusions. BMM, best medical management; EVT, endovascular therapy; ICA, internal carotid artery; M1, first segment of middle cerebral artery; M2, second segment of middle cerebral artery.
The analysis using the random-effects model obtained similar results (proximal ICA or M1 occlusions: OR 1.68, 95% CI 0.98 to 2.88 vs distal M2 occlusions: OR 0.69, 95% CI 0.48 to 1.00; P for interaction=0.008, I2=86%) (online supplemental eFigure 1).
neurintsurg-2022-018662supp001.pdf (713.9KB, pdf)
Secondary outcomes
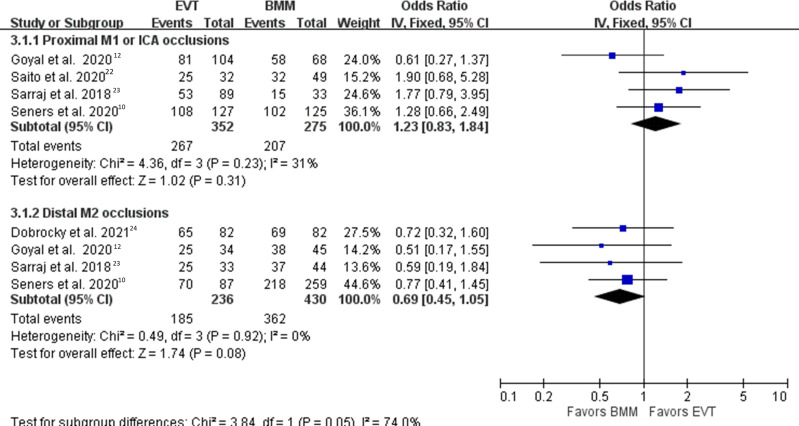
For AIS patients with NIHSS scores ≤5, pooled results from the fixed-effect model showed that EVT compared with BMM was associated with a non-significantly higher rate of functional independence in patients with proximal ICA or M1 occlusions (75.8% vs 75.2%; OR 1.23, 95% CI 0.83 to 1.84),10 12 22 23 but was associated with a non-significantly lower rate of functional independence in patients with distal M2 occlusions (78.3% vs 84.1%; OR 0.69, 95% CI 0.45 to 1.05),10 12 23 24 and the effect of EVT in the proximal ICA or M1 versus distal M2 occlusions was borderline different (P for interaction=0.05, I2=74%) (figure 3).
Figure 3.
Functional independence. Forest plot comparing EVT versus BMM for functional independence (modified Rankin Scale 0–2) in proximal ICA or M1 versus distal M2 occlusions. BMM, best medical management; EVT, endovascular therapy; ICA, internal carotid artery; M1, first segment of middle cerebral artery; M2, second segment of middle cerebral artery.
Pooled results showed that EVT compared with BMM was not associated with a significantly higher rate of symptomatic ICH in proximal ICA or M1 occlusions (5.1% vs 3.1%; OR 1.71, 95% CI 0.61 to 4.81),10 12 but was associated with a higher rate of symptomatic ICH in distal M2 occlusions (6.8% vs 2.3%; OR 3.44, 95% CI 1.42 to 8.32),10 12 24 and the effect of EVT in the proximal ICA or M1 versus distal M2 occlusions was not significantly different (P for interaction=0.31, I2=18%) (online supplemental eFigure 2).
Pooled results showed that EVT compared with BMM was associated with higher rates of any ICH both in the proximal ICA or M1 occlusions (20.3% vs 8.2%; OR 2.79, 95% CI 1.51 to 5.16)10 12 and in the distal M2 occlusions (21.4% vs 8.1%; OR 3.20, 95% CI 1.72 to 5.96),10 12 and the effect of EVT in the proximal ICA or M1 versus distal M2 occlusions was not significantly different (P for interaction=0.76, I2=0%) (online supplemental eFigure 3).
There was no difference in all-cause mortality between EVT and BMM in the proximal ICA or M1 occlusions (8.2% vs 4.9%; OR 1.56, 95% CI 0.53 to 4.63)12 23 and in the distal M2 occlusions (7.3% vs 4.0%; OR 1.87, 95% CI 0.71 to 4.94),12 23 24 and the effect of EVT in the proximal ICA or M1 versus distal M2 occlusions was not significantly different (P for interaction=0.81, I2=0%) (online supplemental eFigure 4).
Sensitivity tests
When we restricted analysis in studies with proximal M1 versus distal M2 occlusions, pooled results showed that EVT compared with BMM was associated with a higher rate of being disability-free in patients with proximal M1 occlusions (69.2% vs 61.0%; OR 2.00, 95% CI 1.21 to 3.31),10 23 but was associated with a lower rate of being disability-free in patients with distal M2 occlusions (64.4% vs 74.2%; OR 0.70, 95% CI 0.49 to 0.99),10 12 23 24 and the effect of EVT in proximal M1 versus distal M2 occlusions was substantially different (P for interaction=0.0007, I2=91%) (online supplemental eFigure 5).
When we restricted analysis in studies with EVT versus IVT, pooled results showed that EVT compared with IVT was associated with a higher rate of being disability-free in patients with proximal ICA or M1 occlusions (77.8% vs 63.6%; OR 1.88, 95% CI 1.10 to 3.21),10 25 but was associated with a non-significant lower rate of being disability-free in patients with distal M2 occlusions (67.5% vs 74.5%; OR 0.80, 95% CI 0.53 to 1.21),10 24 and the effect of EVT compared with IVT in the proximal ICA or M1 versus distal M2 occlusions was substantially different (P for interaction=0.01, I2=84%) (online supplemental eFigure 6).
When we restricted analysis to studies with all patients enrolled after 2011, pooled results showed that EVT compared with BMM was associated with a non-significantly higher rate of being disability-free in patients with proximal ICA or M1 occlusions (60.6% vs 56.4%; OR 1.35, 95% CI 0.80 to 2.27),12 23 but was associated with a lower rate of being disability-free in patients with distal M2 occlusions (56.7% vs 73.0%; OR 0.48, 95% CI 0.25 to 0.95),12 23 and the effect of EVT in proximal ICA or M1 versus distal M2 occlusions was substantially different (P for interaction=0.02, I2=82%) (online supplemental eFigure 7).
Discussion
In this meta-analysis, which compared mild severity AIS patients with proximal ICA or M1 occlusions versus those with distal M2 occlusions, we found that, compared with BMM, EVT was associated with a higher rate of being disability-free in those with proximal ICA or M1 occlusions, but with a lower rate of being disability-free in those with distal M2 occlusions. Similar effects of EVT were found with the outcome of functional independence in proximal ICA or M1 versus distal M2 occlusions. Also, EVT was associated with a higher rate of symptomatic ICH in distal M2 occlusions. Taken together, for AIS with NIHSS scores ≤5 due to vessel occlusions in the anterior circulation, EVT may be beneficial in proximal ICA or M1 occlusions, but the benefit–risk profile may be more in favor of BMM in distal M2 occlusions. Still, these observational data should only be seen as a suggestive rather than a definitive evidence-based guide for clinical practice.
In US national practice, more than one-half of AIS hospitalizations have mild deficits (NIHSS scores ≤5), accounting for one of every 10 EVT treatments.26 However, the effect of EVT versus no EVT is not known as administrative databases do not capture information regarding the presence or absence of vessel occlusions.26 Prior meta-analyses generally show neutral results between EVT and BMM in mild stroke due to vessel occlusions in the anterior circulation, but none of them explored proximal ICA or M1 and distal M2 occlusions separately.12 27 As EVT is likely to be beneficial in mild strokes due to proximal ICA or M1 occlusions, but possibly harmful in those due to distal M2 occlusions as noted in this meta-analysis, it is conceivable that the effect of EVT versus BMM would be neutral if patients with proximal or distal occlusions are pooled together. There are two ongoing randomized trials—Endovascular Therapy for Low NIHSS Ischemic Strokes (ENDOLOW), and Minor Stroke Therapy Evaluation (MOSTE)—which are exploring the efficacy of EVT in AIS due to LVO with NIHSS scores ≤ 5.28 29 The ENDOLOW trial enrolled stroke patients with ICA, M1, or M1-like M2 occlusions, while the MOSTE trial enrolled stroke patients with ICA, M1, or M1-M2 occlusions.28 29 The study design of these two ongoing trials for not enrolling mild stroke patients with pure distal M2 occlusions may be based on the assumption that EVT is not likely to be beneficial in these patients, which was confirmed by the current meta-analysis. The criteria of specific vessel occlusion sites used in these two randomized trials are similar to the proximal ICA or M1 occlusions in the current meta-analysis. The findings of these two trials will provide robust evidence to support or rebut our results suggesting EVT is beneficial in mild ischemic stroke with proximal ICA or M1 occlusions.
In the SITS International Stroke Thrombolysis Register involving 2553 patients with IVT-treated minor stroke (NIHSS scores ≤5), non-hemorrhagic early neurological deterioration was more frequently seen in proximal ICA or M1 occlusions than no occlusion, whereas non-hemorrhagic early neurological deterioration rate was not significantly different between distal M2 occlusions and no occlusions.4 In the MINOR-STROKE collaboration on 729 stroke patients with NIHSS scores ≤5 due to vessel occlusions and treated with IVT, a more proximal occlusion site was independently associated with early neurological deterioration.9 Another study showed that 44% of proximal ICA or M1 occlusions versus 32% of distal M2 occlusions had early neurological deterioration in AIS with NIHSS scores ≤5 not treated with EVT.8 Since there is a high rate of early neurological deterioration in mild stroke patients with proximal ICA or M1 occlusions, and early neurological deterioration is strongly associated with poor functional outcome,9 the natural course of mild stroke with proximal ICA or M1 occlusions should probably not be regarded as benign. Although data on reperfusion rates in each group were not provided by the included studies, it is conceivable that EVT compared with BMM would further increase excellent reperfusion in some patients. Also, the current meta-analysis found that EVT compared with BMM was not significantly associated with a higher rate of symptomatic ICH in proximal ICA or M1 occlusions. Taken together, EVT is likely to provide additional benefits in mild stroke with proximal ICA or M1 occlusions.
The STRATIS Registry showed that distal M2 occlusions (NIHSS score 15.7±5.0) compared with proximal M1 occlusions achieved similar rates of successful reperfusion and good functional outcome, although increased rates of symptomatic ICH were demonstrated.30 The HERMES collaboration showed that EVT compared with BMM was associated with functional independence and successful reperfusion in distal M2 occlusions (NIHSS score 14.4±5.1).31 However, none of these studies addressed lower NIHSS scores with distal M2 occlusions. Perforations and symptomatic ICH were most commonly found at distal M2 occlusions during EVT due to difficulty traversing the occlusion with a microcatheter or microwire, or while withdrawing the stent retriever,32 which may hamper the potential beneficial effect of EVT especially in patients with low NIHSS scores. On the other hand, IVT increases rates of freedom of disability5 and does not increase symptomatic ICH in mild stroke patients.33 34 Furthermore, a positive correlation between successful early reperfusion and clinical outcome could not be demonstrated for patients with distal M2 occlusions.35 In this meta-analysis, freedom of disability was most frequently found in patients with distal M2 occlusions receiving BMM (74.1%), followed by patients with proximal ICA or M1 (67.6%) and distal M2 (64.4%) occlusions receiving EVT; patients with proximal ICA or M1 occlusions not receiving EVT had the lowest rate (60.6%) for freedom of disability.
For patients with mild stroke and M2 occlusions, it may be interesting to conduct a subgroup analysis to compare patients who received EVT versus patients who did not receive any reperfusion therapy, including IVT; this is because a randomized controlled trial showed that among patients with minor non-disabling AIS (NIHSS score 0–5), treatment with IVT versus aspirin did not increase the likelihood of favorable functional outcome at 90 days.36 Also, it may be interesting to conduct a subgroup analysis to explore the limits of symptom severity that may still induce the benefit of EVT in proximal versus distal occlusions among patients presenting with NIHSS scores 0–3 versus 4–5. However, no relevant data were provided by included studies and further analyses could not be conducted.
Limitations
Limitations of this meta-analysis must be considered. First, all included studies were observational studies and selection bias is inevitable. Also, we pooled results by using raw data rather than adjusted ORs with 95% CI because most included studies did not provide such information. Since adjusted ORs with 95% CI were only reported in one study,10 pooled analysis based on adjusted results could not be done. Second, patients enrolled in the included studies from 1998 to 2020, and the devices used in EVT treatment varied during this period of time. A sensitivity test including only studies enrolling patients after 2011 obtained similar results. However, major advances have been made in the design of devices specifically created to treat distal occlusions in the past 10 years. Only one study reported subgroup analysis for patients treated after 2015 and found that mRS 0–1 at 3 months was not significantly different between EVT versus IVT groups in mild ischemic stroke due to distal M2 occlusions. Third, information on the size of infarct core and penumbra, and collateral status, was not provided by included studies and further analysis was not possible. Finally, some studies reported results based on proximal ICA or M1 occlusions while other studies reported results based on proximal M1 occlusions. Also, some studies reported IVT in the control arm while other studies reported BMM in the control arm. Still, sensitivity tests exploring these factors obtained similar results.
Conclusions
This meta-analysis highlights the importance of knowledge about specific vessel occlusion sites in decision-making for AIS with NIHSS scores ≤5 due to vessel occlusions in the anterior circulation. EVT compared with BMM was associated with a higher rate of being disability-free after mild AIS due to proximal ICA or M1 occlusions. Pending evidence from ongoing randomized trials, such findings should only be seen as a suggestive rather than an evidence-based guide for clinical practice. On the other hand, EVT compared with BMM was associated with a lower rate of being disability-free after mild AIS due to distal M2 occlusions, and therefore it may be imprudent to use EVT in these patients.
neurintsurg-2022-018662supp002.pdf (316.3KB, pdf)
Footnotes
Contributors: C-HL: acquisition of data, analysis and interpretation of data, wrote the first draft. JS: study supervision, critical revision of manuscript for intellectual content. BO: critical revision of manuscript for intellectual content. S-CT: analysis and interpretation of data. ML; study concept and design, acquisition of data, analysis and interpretation of data, critical revision of manuscript for intellectual content. DSL: critical revision of manuscript for intellectual content. ML is the guarantor.
Funding: This work was supported by Ministry of Science and Technology, Taiwan, grant number: MOST 108–2314-B-182–017, 109–2314-B-182–033 and Chang Gung Memorial Hospital, Taiwan, grant number: CMRPG6H0441, CORPG6G0191, CORPG6G0192, CORPG6G0193.
Disclaimer: The sponsors played no role in the study design, data collection and analysis, or decision to submit the article for publication.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
Data are available in a public, open access repository. Not applicable.
Ethics statements
Patient consent for publication
Not applicable.
Ethics approval
This study does not involve human participants.
References
- 1. Heldner MR, Zubler C, Mattle HP, et al. National Institutes of Health Stroke Scale score and vessel occlusion in 2152 patients with acute ischemic stroke. Stroke 2013;44:1153–7. 10.1161/STROKEAHA.111.000604 [DOI] [PubMed] [Google Scholar]
- 2. Zhu W, Churilov L, Campbell BCV, et al. Does large vessel occlusion affect clinical outcome in stroke with mild neurologic deficits after intravenous thrombolysis? J Stroke Cerebrovasc Dis 2014;23:2888–93. 10.1016/j.jstrokecerebrovasdis.2014.07.018 [DOI] [PubMed] [Google Scholar]
- 3. Nedeltchev K, Schwegler B, Haefeli T, et al. Outcome of stroke with mild or rapidly improving symptoms. Stroke 2007;38:2531–5. 10.1161/STROKEAHA.107.482554 [DOI] [PubMed] [Google Scholar]
- 4. Mazya MV, Cooray C, Lees KR, et al. Minor stroke due to large artery occlusion. When is intravenous thrombolysis not enough? Results from the SITS international stroke thrombolysis register. Eur Stroke J 2018;3:29–38. 10.1177/2396987317746003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Powers WJ, Rabinstein AA, Ackerson T, et al. Guidelines for the early management of patients with acute ischemic stroke: 2019 update to the 2018 guidelines for the early management of acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 2019;50:e344–418. 10.1161/STR.0000000000000211 [DOI] [PubMed] [Google Scholar]
- 6. Turc G, Bhogal P, Fischer U, et al. European Stroke Organisation (ESO)- European Society for Minimally Invasive Neurological Therapy (ESMINT) guidelines on mechanical thrombectomy in acute ischemic stroke. J Neurointerv Surg 2019;11:535–8. 10.1136/neurintsurg-2018-014568 [DOI] [PubMed] [Google Scholar]
- 7. Saver JL, Chapot R, Agid R, et al. Thrombectomy for distal, medium vessel occlusions: a consensus statement on present knowledge and promising directions. Stroke 2020;51:2872–84. 10.1161/STROKEAHA.120.028956 [DOI] [PubMed] [Google Scholar]
- 8. Gwak D-S, Kwon J-A, Shim D-H, et al. Perfusion and diffusion variables predict early neurological deterioration in minor stroke and large vessel occlusion. J Stroke 2021;23:61–8. 10.5853/jos.2020.01466 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Seners P, Ben Hassen W, Lapergue B, et al. Prediction of early neurological deterioration in individuals with minor stroke and large vessel occlusion intended for intravenous thrombolysis alone. JAMA Neurol 2021;78:321–8. 10.1001/jamaneurol.2020.4557 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Seners P, Perrin C, Lapergue B, et al. Bridging therapy or IV thrombolysis in minor stroke with large vessel occlusion. Ann Neurol 2020;88:160–9. 10.1002/ana.25756 [DOI] [PubMed] [Google Scholar]
- 11. McCarthy DJ, Tonetti DA, Stone J, et al. More expansive horizons: a review of endovascular therapy for patients with low NIHSS scores. J Neurointerv Surg 2021;13:146–51. 10.1136/neurintsurg-2020-016583 [DOI] [PubMed] [Google Scholar]
- 12. Goyal N, Tsivgoulis G, Malhotra K, et al. Medical management vs mechanical thrombectomy for mild strokes: an international multicenter study and systematic review and meta-analysis. JAMA Neurol 2020;77:16–24. 10.1001/jamaneurol.2019.3112 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Harris RP, Helfand M, Woolf SH, et al. Current methods of the US Preventive Services Task Force: a review of the process. Am J Prev Med 2001;20:21–35. 10.1016/s0749-3797(01)00261-6 [DOI] [PubMed] [Google Scholar]
- 14. Lin M-H, Kamel H, Singer DE, et al. Perioperative/postoperative atrial fibrillation and risk of subsequent stroke and/or mortality. Stroke 2019;50:1364–71. 10.1161/STROKEAHA.118.023921 [DOI] [PubMed] [Google Scholar]
- 15. Hacke W, Kaste M, Bluhmki E, et al. Thrombolysis with alteplase 3 to 4.5 hours after acute ischemic stroke. N Engl J Med 2008;359:1317–29. 10.1056/NEJMoa0804656 [DOI] [PubMed] [Google Scholar]
- 16. Johnston SC, Easton JD, Farrant M, et al. Clopidogrel and aspirin in acute ischemic stroke and high-risk TIA. N Engl J Med 2018;379:215–25. 10.1056/NEJMoa1800410 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Nogueira RG, Jadhav AP, Haussen DC, et al. Thrombectomy 6 to 24 hours after stroke with a mismatch between deficit and infarct. N Engl J Med 2018;378:11–21. 10.1056/NEJMoa1706442 [DOI] [PubMed] [Google Scholar]
- 18. Yoshimura S, Sakai N, Yamagami H, et al. Endovascular therapy for acute stroke with a large ischemic region. N Engl J Med 2022. 10.1056/NEJMoa2118191. [Epub ahead of print: 09 Feb 2022]. [DOI] [PubMed] [Google Scholar]
- 19. Higgins JPT, Thompson SG, Deeks JJ, et al. Measuring inconsistency in meta-analyses. BMJ 2003;327:557–60. 10.1136/bmj.327.7414.557 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Higgins JPT. Cochrane handbook for systematic reviews of interventions version 5.1.0 [updated march 2011]. The Cochrane Collaboration, 2011. [Google Scholar]
- 21. Berkhemer OA, Fransen PSS, Beumer D, et al. A randomized trial of intraarterial treatment for acute ischemic stroke. N Engl J Med 2015;372:11–20. 10.1056/NEJMoa1411587 [DOI] [PubMed] [Google Scholar]
- 22. Saito T, Itabashi R, Yazawa Y, et al. Clinical outcome of patients with large vessel occlusion and low National Institutes of Health Stroke Scale scores: subanalysis of the RESCUE-Japan Registry 2. Stroke 2020;51:1458–63. 10.1161/STROKEAHA.119.028562 [DOI] [PubMed] [Google Scholar]
- 23. Sarraj A, Hassan A, Savitz SI, et al. Endovascular thrombectomy for mild strokes: how low should we go? Stroke 2018;49:2398–405. 10.1161/STROKEAHA.118.022114 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Dobrocky T, Piechowiak EI, Volbers B, et al. Treatment and outcome in stroke patients with acute M2 occlusion and minor neurological deficits. Stroke 2021;52:802–10. 10.1161/STROKEAHA.120.031672 [DOI] [PubMed] [Google Scholar]
- 25. Messer MP, Schönenberger S, Möhlenbruch MA, et al. Minor stroke syndromes in large-vessel occlusions: mechanical thrombectomy or thrombolysis only? AJNR Am J Neuroradiol 2017;38:1177–9. 10.3174/ajnr.A5164 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Saber H, Khatibi K, Szeder V, et al. Reperfusion therapy frequency and outcomes in mild ischemic stroke in the United States. Stroke 2020;51:3241–9. 10.1161/STROKEAHA.120.030898 [DOI] [PubMed] [Google Scholar]
- 27. Zhao Y, Song Y, Guo Y, et al. Endovascular thrombectomy vs. medical treatment for mild stroke patients: a systematic review and meta-analysis. J Stroke Cerebrovasc Dis 2020;29:105258. 10.1016/j.jstrokecerebrovasdis.2020.105258 [DOI] [PubMed] [Google Scholar]
- 28.et alNagel SKP, Demchuk A, Nogueira R. Endovascular therapy for low NIHSS ischemic strokes (ENDOLOW). Available: https://clinicaltrials.gov/ct2/show/NCT04167527 [Accessed 15 Oct 2021].
- 29. Minor Stroke Therapy Evaluation (MOSTE). Available: https://clinicaltrials.gov/ct2/show/NCT03796468 [Accessed 15 Oct 2021].
- 30. Jumaa MA, Castonguay AC, Salahuddin H, et al. Middle cerebral artery M2 thrombectomy in the STRATIS registry. Stroke 2021;52:3490–6. 10.1161/STROKEAHA.120.033951 [DOI] [PubMed] [Google Scholar]
- 31. Goyal M, Menon BK, van Zwam WH, et al. Endovascular thrombectomy after large-vessel ischaemic stroke: a meta-analysis of individual patient data from five randomised trials. Lancet 2016;387:1723–31. 10.1016/S0140-6736(16)00163-X [DOI] [PubMed] [Google Scholar]
- 32. Mokin M, Fargen KM, Primiani CT, et al. Vessel perforation during stent retriever thrombectomy for acute ischemic stroke: technical details and clinical outcomes. J Neurointerv Surg 2017;9:922–8. 10.1136/neurintsurg-2016-012707 [DOI] [PubMed] [Google Scholar]
- 33. Ahmed N, Wahlgren N, Grond M, et al. Implementation and outcome of thrombolysis with alteplase 3-4.5 h after an acute stroke: an updated analysis from SITS-ISTR. Lancet Neurol 2010;9:866–74. 10.1016/S1474-4422(10)70165-4 [DOI] [PubMed] [Google Scholar]
- 34. Romano JG, Smith EE, Liang L, et al. Outcomes in mild acute ischemic stroke treated with intravenous thrombolysis: a retrospective analysis of the Get With The Guidelines-Stroke registry. JAMA Neurol 2015;72:423–31. 10.1001/jamaneurol.2014.4354 [DOI] [PubMed] [Google Scholar]
- 35. Rahme R, Yeatts SD, Abruzzo TA, et al. Early reperfusion and clinical outcomes in patients with M2 occlusion: pooled analysis of the PROACT II, IMS, and IMS II studies. J Neurosurg 2014;121:1354–8. 10.3171/2014.7.JNS131430 [DOI] [PubMed] [Google Scholar]
- 36. Khatri P, Kleindorfer DO, Devlin T, et al. Effect of alteplase vs aspirin on functional outcome for patients with acute ischemic stroke and minor nondisabling neurologic deficits: the PRISMS randomized clinical trial. JAMA 2018;320:156–66. 10.1001/jama.2018.8496 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
neurintsurg-2022-018662supp001.pdf (713.9KB, pdf)
neurintsurg-2022-018662supp002.pdf (316.3KB, pdf)
Data Availability Statement
Data are available in a public, open access repository. Not applicable.