Abstract
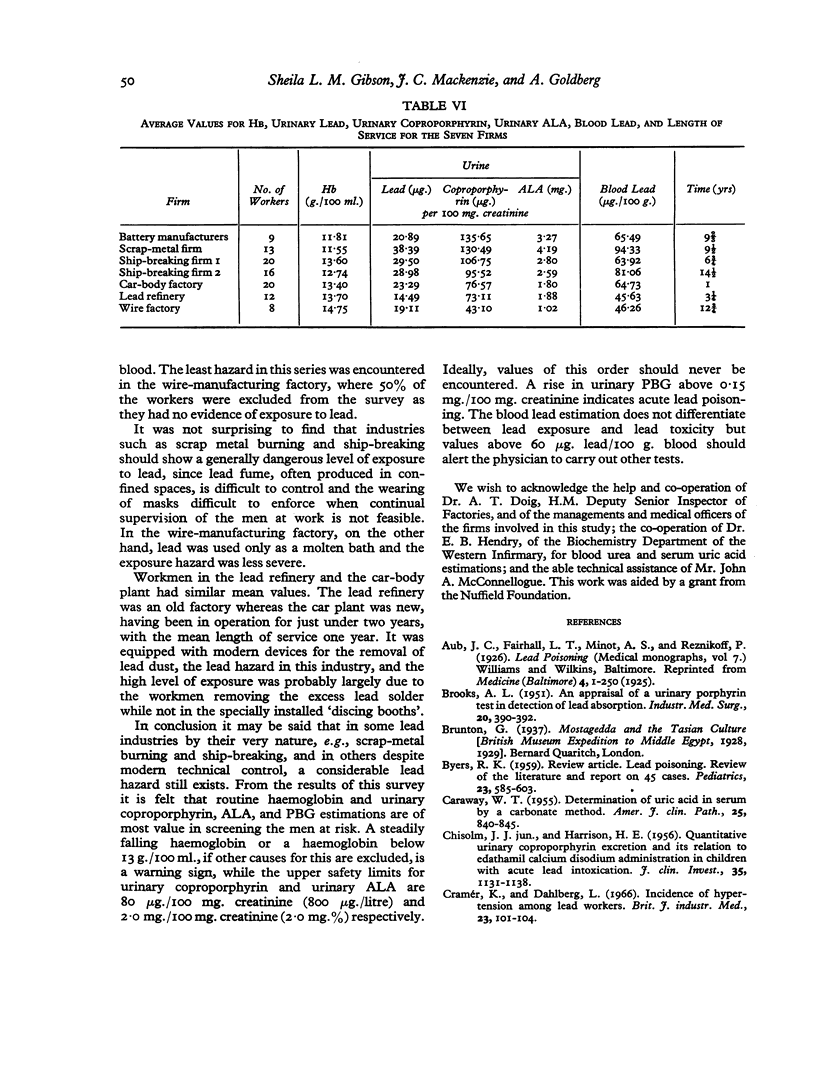
A series of 100 lead workers from different industries, 91 at work and nine admitted to hospital with lead poisoning, was studied in order to define more clearly the clinical and biochemical criteria of lead poisoning in three stages—(A) a presymptomatic state of lead exposure (37 men), (B) a state of mild symptoms or mild anaemia (45 men), and (C) frank lead poisoning with severe symptoms and signs (18 men).
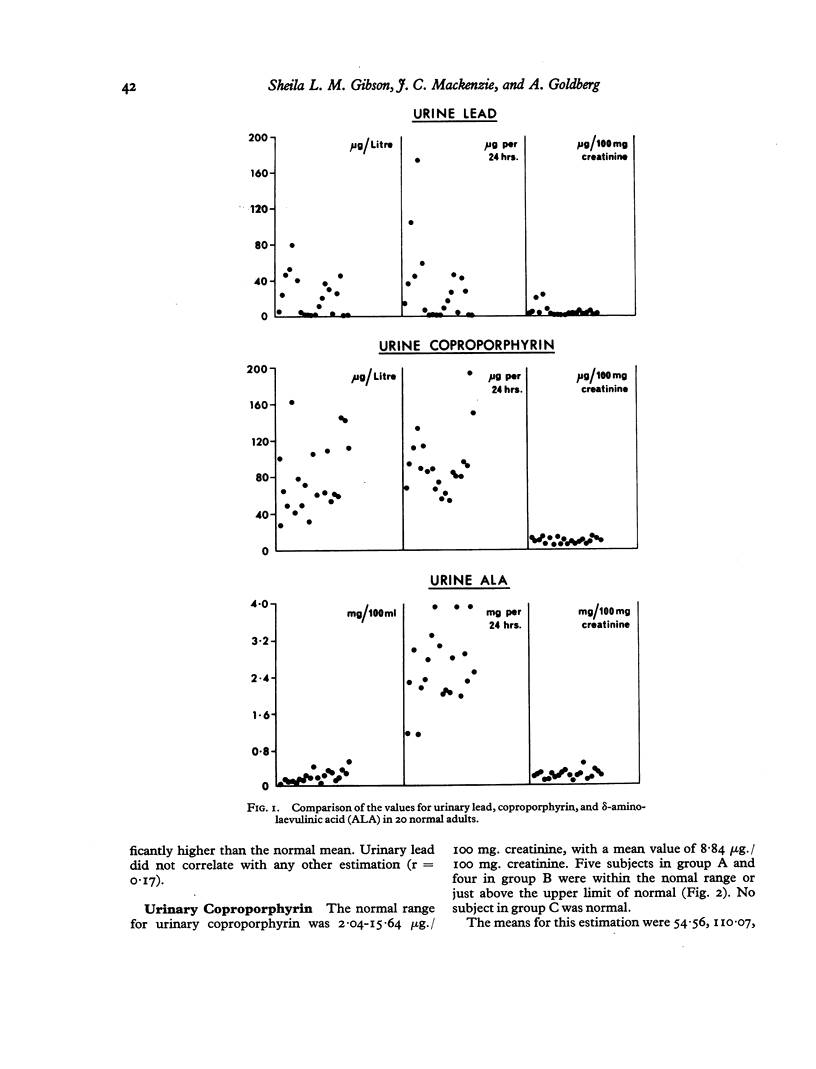
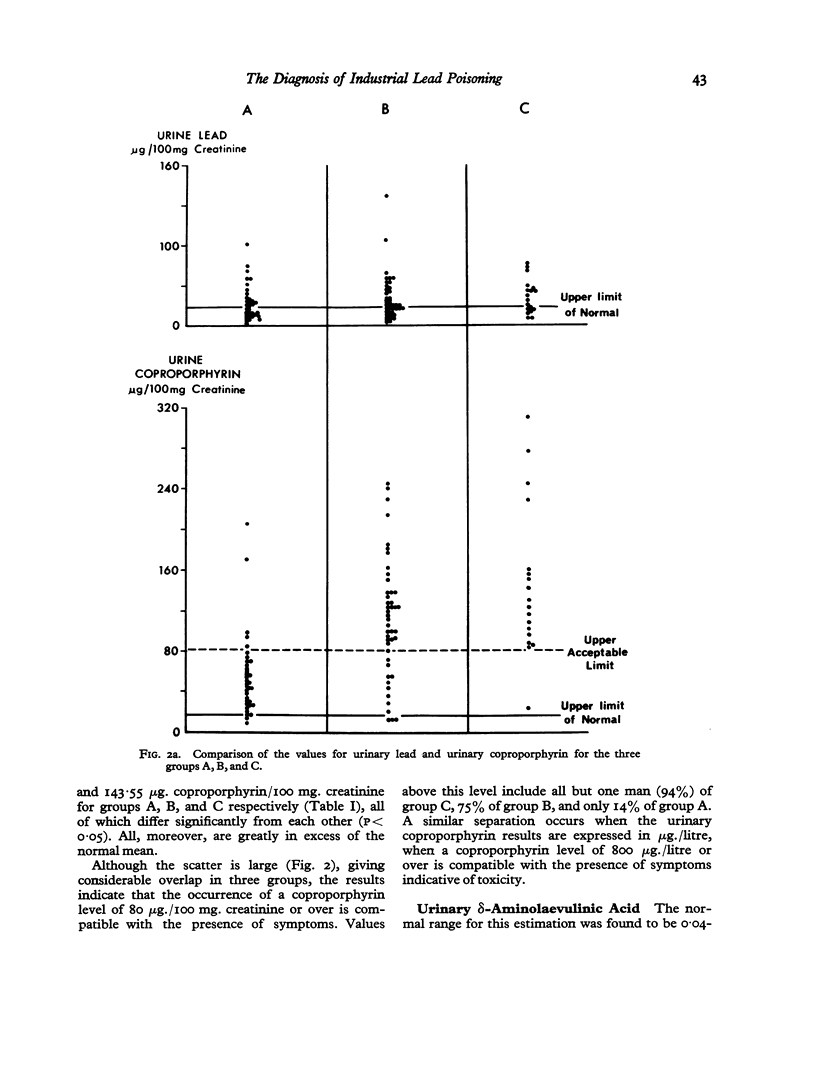
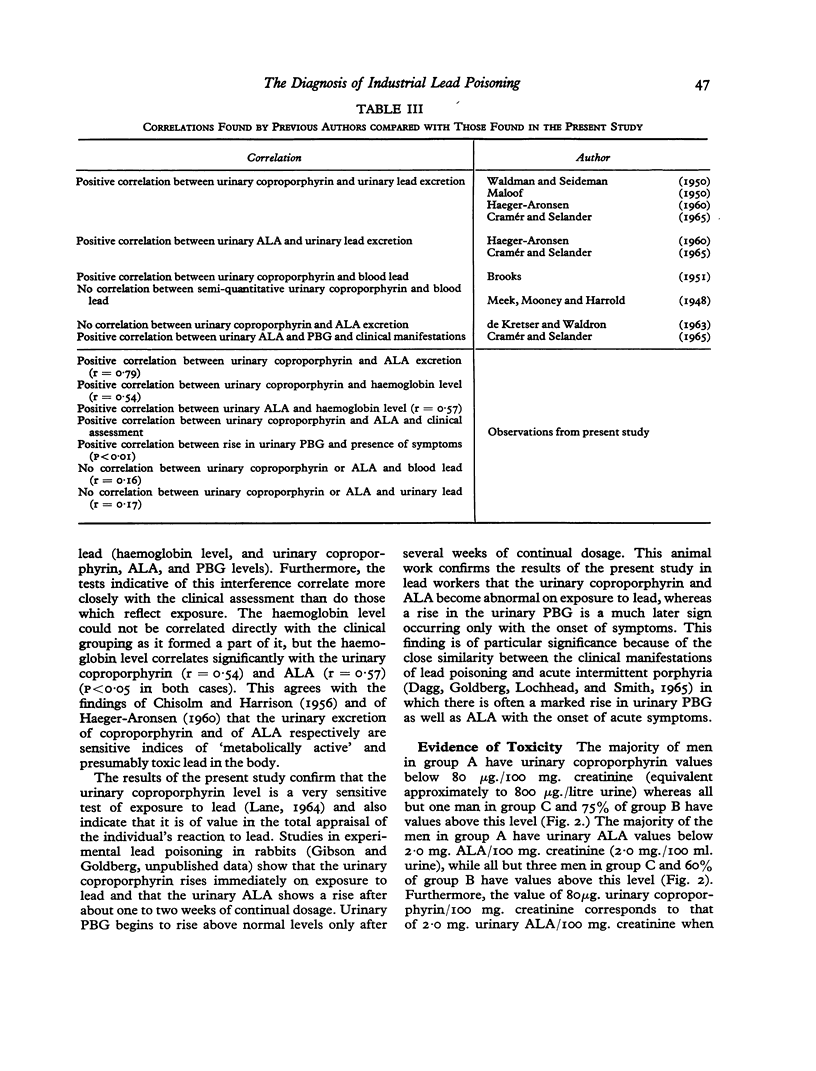
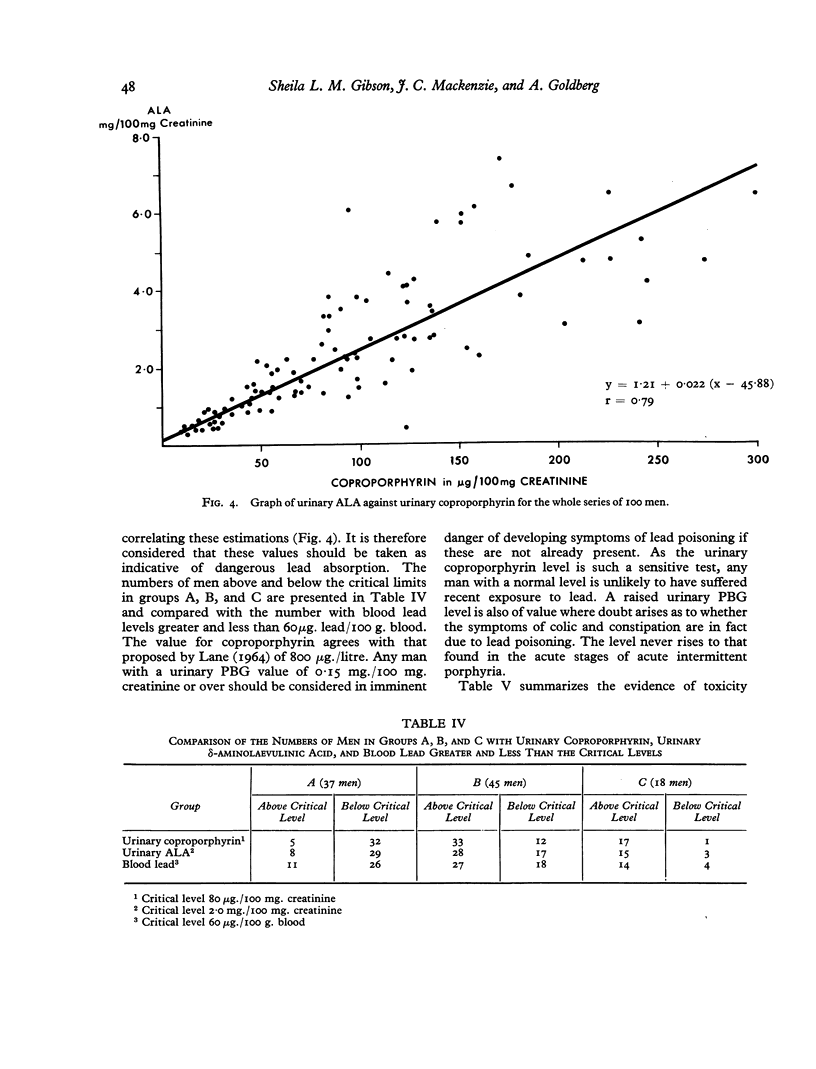
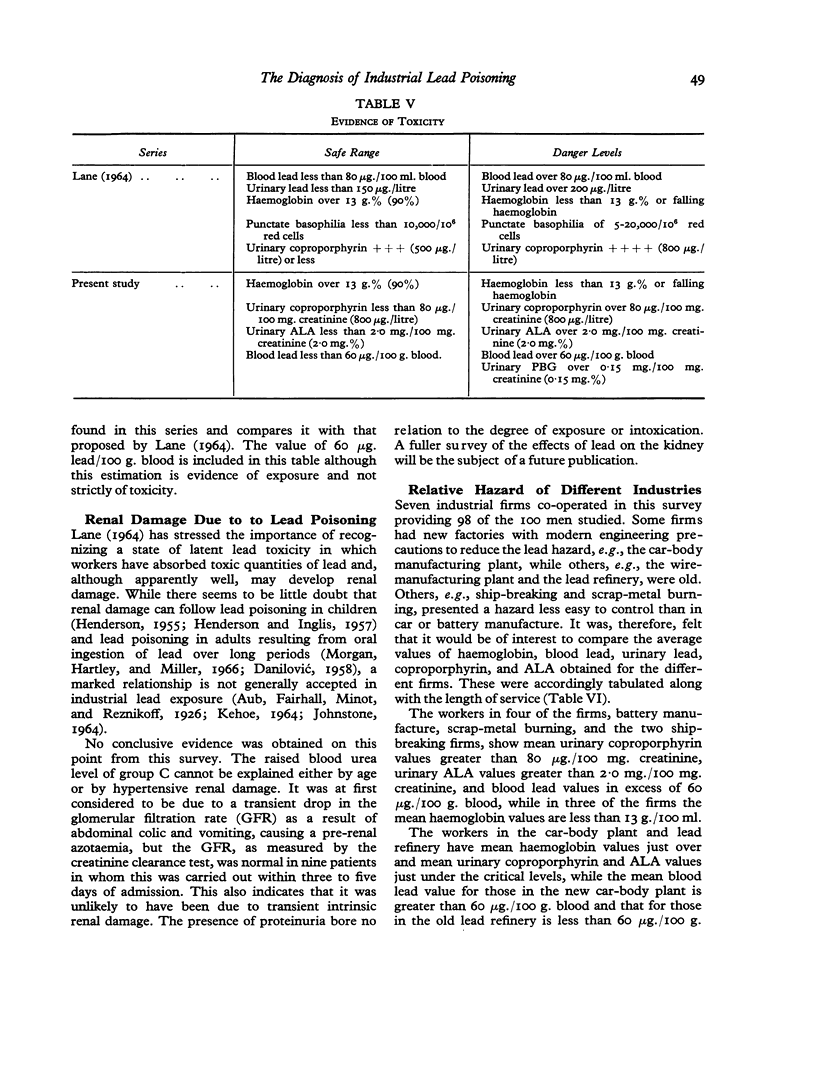
The tests used were haemoglobin, reticulocyte count, and blood lead, and urinary lead, coproporphyrin, δ-aminolaevulinic acid (ALA), and porphobilinogen (PBG) estimations. Of these, the urinary lead was similar for all three groups and the blood lead estimation was of less value for determining the clinical group of the men than the haemoglobin and urinary coproporphyrin or ALA estimations, which correlated well with the clinical assessment and with each other but showed no correlation with the urinary and blood lead levels. PBG levels became raised only with the onset of symptoms of lead poisoning.
A haemoglobin of 13 g./100 ml. (90%) or less is a cautionary sign. Urinary coproporphyrin above 80 μg./100 mg. creatinine (800 μg./litre), ALA above 2·0 mg./100 mg. creatinine (2·0 mg.%), and PBG above 0·15 mg./100 mg. creatinine (0·15 mg.%) were almost always associated with symptoms or signs and were therefore considered to be the upper safety limits. Although the blood lead level does not differentiate between lead toxicity and lead exposure, values above 60 μg. lead/100 g. blood should alert the physician to carry out other tests.
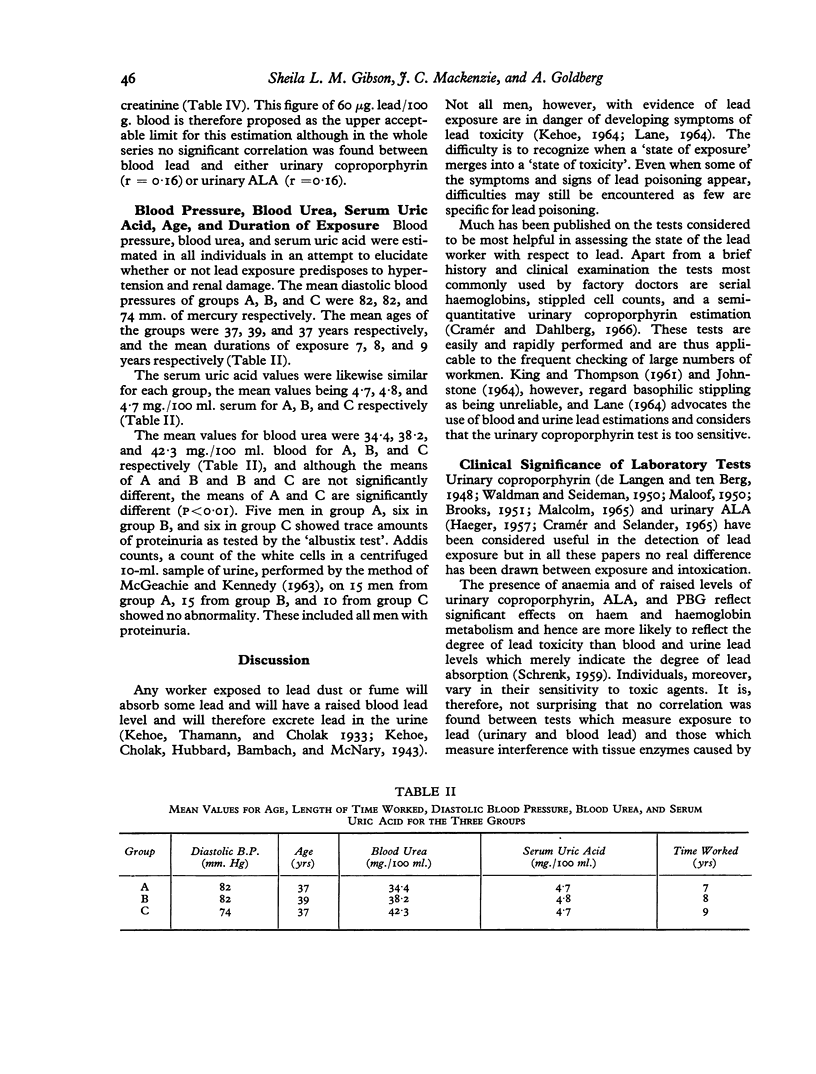
In addition to the above tests, blood pressure, blood urea, and serum uric acid estimations were performed on all the men in order to elucidate the possible role of lead in the production of renal damage. Blood pressure and serum uric acid levels were similar for all three groups but the blood urea level was raised in group C. The reason for this finding was not established.
It was found that scrap metal burning, battery manufacturing, and ship-breaking constituted the gravest lead hazards encountered in this survey whereas wire manufacture constituted the least. Workers in the most modern factory, a car-body pressing plant, gave average values just below the danger levels for the urinary coproporphyrin and ALA estimations despite apparently efficient protective measures. This finding underlines the importance of the medical supervision of lead workers.
Full text
PDF


Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- BROOKS A. L. An appraisal of a urinary porphyrin test in detection of lead absorption. Ind Med Surg. 1951 Sep;20(9):390–392. [PubMed] [Google Scholar]
- BYERS R. K. Lead poisoning; review of the literature and report on 45 cases. Pediatrics. 1959 Mar;23(3):585–603. [PubMed] [Google Scholar]
- CARAWAY W. T. Determination of uric acid in serum by a carbonate method. Am J Clin Pathol. 1955 Jul;25(7):840–845. doi: 10.1093/ajcp/25.7_ts.0840. [DOI] [PubMed] [Google Scholar]
- Cramér K., Dahlberg L. Incidence of hypertension among lead workers. A follow-up study based on regular control over 20 years. Br J Ind Med. 1966 Apr;23(2):101–104. doi: 10.1136/oem.23.2.101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DAGG J. H., GOLDBERG A., LOCHHEAD A., SMITH J. A. THE RELATIONSHIP OF LEAD POISONING TO ACUTE INTERMITTENT PORPHYRIA. Q J Med. 1965 Apr;34:163–175. [PubMed] [Google Scholar]
- DANILOVIC V. Chronic nephritis due to ingestion of lead-contaminated flour. Br Med J. 1958 Jan 4;1(5061):27–28. doi: 10.1136/bmj.1.5061.27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DE KRETSER A. J., WALDRON H. A. Urinary delta aminolaevulinic acid and porphobilinogen in lead-exposed workers. Br J Ind Med. 1963 Jan;20:35–40. doi: 10.1136/oem.20.1.35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- GOLDBERG A., SMITH J. A., LOCHHEAD A. C. Treatment of lead-poisoning with oral penicillamine. Br Med J. 1963 May 11;1(5340):1270–1275. doi: 10.1136/bmj.1.5340.1270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- HENDERSON D. A. Chronic nephritis in Queensland. Australas Ann Med. 1955 Aug;4(3):163–177. doi: 10.1111/imj.1955.4.3.163. [DOI] [PubMed] [Google Scholar]
- KEHOE R. A. METABOLISM OF LEAD UNDER ABNORMAL CONDITIONS. Arch Environ Health. 1964 Feb;8:235–243. doi: 10.1080/00039896.1964.10663661. [DOI] [PubMed] [Google Scholar]
- KING E., THOMPSON A. R. The measurement of lead absorption in industry. Ann Occup Hyg. 1961 Jun;3:247–263. [PubMed] [Google Scholar]
- MALOOF C. C. Role of porphyrins in occupational diseases; significance of coproporphyrinuria in lead workers. Arch Ind Hyg Occup Med. 1950 Mar;1(3):296–307. [PubMed] [Google Scholar]
- MAUZERALL D., GRANICK S. The occurrence and determination of delta-amino-levulinic acid and porphobilinogen in urine. J Biol Chem. 1956 Mar;219(1):435–446. [PubMed] [Google Scholar]
- SKEGGS L. T., Jr An automatic method for colorimetric analysis. Am J Clin Pathol. 1957 Sep;28(3):311–322. doi: 10.1093/ajcp/28.3_ts.311. [DOI] [PubMed] [Google Scholar]
- WALDMAN R. K., SEIDEMAN R. M. Reliability of the urinary porphyrin test for lead absorption. Arch Ind Hyg Occup Med. 1950 Mar;1(3):290–295. [PubMed] [Google Scholar]


