Abstract
Background:
Despite the efforts of the health system to improve access to medications during the coronavirus disease of 2019 (COVID-19) pandemic, such as online consultations, encouraging generic prescriptions, and other measures to limit the storage of medication, psychotropic patients faced significant challenges in accessing their medications.
Objectives:
This study aimed (1) to compare the consumption of psychotropics before and during the pandemic, (2) to assess the association between having difficulties finding the medications and the general characteristics of the patients, and (3) to assess the predictors of these difficulties.
Design:
A case–control study was performed in which 128 patients (cases) were recruited during the pandemic (July–October 2021), and 256 patients (controls) using psychotropics before the pandemic were matched for age and sex.
Methods:
Data were collected using a uniform survey given to patients using psychotropics and filled out at their time and place preferences.
Results:
More patients used antipsychotics and anti-anxiety medications before the pandemic, while antidepressants were used more during the pandemic. Almost half of the patients reported facing difficulties finding their medications in both time frames. Before the pandemic, these difficulties were noted per increase in age and being employed and were less faced if patients had medical assistance or lived in the north of Lebanon. However, more patients reported having difficulties accessing their medication during the pandemic, with no significant differences.
Conclusion:
The consumption of psychotropic drugs was higher among cases. All patients faced challenges in accessing their medication throughout the pandemic, while older and employed patients had more limitations before the pandemic. Further investigations exploring viable solutions are recommended in order to maintain sustainable access to treatment.
Keywords: COVID-19 pandemic, psychotropic medication, patients, shortage of medication, access to medication, predictors
Introduction
The coronavirus disease of 2019 (COVID-19) pandemic has disrupted the supply chain of drugs and, as a result, negatively affected access to medications, particularly for chronic conditions. 1 Among others, access to psychotropic medications is crucial due to the impact of the pandemic itself on the mental health of patients, which can be more considerably influenced by the associated emotional responses. 2 Other challenges exacerbated patients’ mental health, such as the lack of health professionals and health facilities and increased medication storage. 3
Evidence suggests that a psychiatric epidemic is cooccurring with the COVID-19 pandemic, 4 which may necessitate attention to improving access to psychotropic drugs. Several psychopathologies, such as anxiety and depression,5,6 increased during the pandemic in addition to other conditions, including burnout 7 and post-traumatic stress disorder. 8 Eating disorders and violence rates also grew, requiring substantial management through psychotropics. 9 Uptake of hypnotic medications was 12% higher among those under 18 years of age, and anxiolytic and antipsychotic consumption significantly increased following the pandemic among the elderly. 10 Problematic use of the Internet, depressive symptoms, and suicidal ideas were also observed among younger populations, 11 in addition to alcohol abuse associated with psychological disorders following the pandemic. 12 Despite the health system’s efforts to improve access to medications during the pandemic, such as online consultations, 13 encouraging generic prescription, 14 and other measures to limit the storage of medication, 15 psychotropic patients faced significant challenges in finding their medications. 16 In response, some patients tried alternatives due to the unavailability of the prescribed medication, 17 while others relied on self-medication without referring to a specialist. 18
The healthcare system in Lebanon relies mostly on private institutions (70%), with most medical expenses being out-of-pocket. The rest are either operated by non-governmental organizations or are public hospitals. 19 Recently, the COVID-19 pandemic negatively affected the healthcare system and imposed many dilemmas such as prioritization of treatment, 20 which can aggravate the status of psychotropic patients. Healthcare workers were at higher risk for poor sleep limiting their productivity and quality of life. 21 Successive lockdowns and social isolation increased the odds of depression, anxiety, and stress symptoms. 22 Other stressors such as the Beirut port explosion, economic crisis, and political unrest, intensified both the need for support and the severity of cases. 23 Patients using psychotropic medications were mainly affected by the consequences of the pandemic since mental health stigma limited their access to care. 24 To understand what possible strategies can be applied to improve access to medications, this study aims (1) to compare the consumption of psychotropics before and during the COVID-19 pandemic, (2) to assess the association between having difficulties finding the medications and the general characteristics of the patients, and (3) to assess the predictors of these difficulties.
Method
Study design
To achieve the intended objectives, a case–control study was performed by interpreting findings from two cross-sectional studies. In the first study, data were collected before the COVID-19 pandemic over a period of 6 months (May to October 2019) while in the second one, data collection was carried out during the pandemic between July and October 2021.
Study sample
Patients using psychotropic drugs were invited to participate in the study with no preferences based on race or ethnicity. Lebanese adult patients residing in Lebanon during the interview period were included. However, those refusing to participate in the study or those with severe mental disorders making them unable to adequately answer the survey were excluded.
Overall, 283 patients were approached during the period before the pandemic and 256 (90.5%) accepted to participate in the study compared to 163 during the pandemic with a response rate of 78.5% (N = 128). Table 1 represents the general characteristics of the study participants. Before the pandemic, the sample consisted of almost 32% of males and 68% of females (p = 0.938). The mean age was 39.6 years (SD = 12.9) for the control group and 36.8 years (SD = 13.4) for the cases. Most of the sample had less than 40 years, almost 32% were between 41 and 60 years and 5.5% were older than 60 years (p = 0.997). Statistically significant differences were noted in terms of the governorate of residence with 58.7% of controls living in Beirut compared to 34.4% of cases (p < 0.001). Almost a third of the participants had a high school degree and more than 40% had a university degree or more (p = 0.293). The majority were employed at the data collection time (p = 0.140). Most of the patients had public insurance (50.4% for controls and 56.3% for cases) and 34.4% of the controls lack any type of medical coverage compared to 27.3% of the cases (p = 0.377).
Table 1.
Distribution of the general characteristics of the patients.
| Before COVID-19 (controls) |
During COVID-19 (cases) |
p-value | ||
|---|---|---|---|---|
| Frequency (%) | Frequency (%) | |||
| Sex | Male | 83 (32.4) | 41 (32.0) | 0.938 |
| Female | 173 (67.6) | 87 (68.0) | ||
| Age (years) | Mean ± SD | 39.6 ± 12.9 | 36.8 ± 13.4 | |
| 18–40 | 159 (62.1) | 80 (62.5) | ||
| 41–60 | 83 (32.4) | 41 (32.0) | 0.997 | |
| More than 60 | 14 (5.5) | 7 (5.5) | ||
| Governorate of residence | Beirut | 149 (58.7) | 44 (34.4) | |
| North | 52 (20.5) | 11 (8.6) | ||
| South | 25 (9.8) | 11 (8.6) | <0.001 | |
| Mount Lebanon | 16 (6.3) | 55 (43.0) | ||
| Bekaa | 12 (4.7) | 7 (5.5) | ||
| Marital status | Single | 83 (32.4) | 49 (38.3) | |
| Married | 124 (48.4) | 67 (52.3) | 0.044 | |
| Divorced/widowed | 49 (19.1) | 12 (9.4) | ||
| Household arrangement | With family | 55 (21.6) | 39 (30.5) | |
| Alone | 177 (69.4) | 78 (60.9) | 0.158 | |
| Medical assistance | 23 (9.0) | 11 (8.6) | ||
| Ethics approval and consent to participate | <Middle school | 63 (24.8) | 23 (18.0) | |
| High school | 83 (32.7) | 43 (33.6) | 0.293 | |
| University or more | 108 (42.5) | 62 (48.4) | ||
| Ethics approval and consent to participate | Employed | 157 (61.3) | 87 (69.0) | 0.140 |
| Unemployed | 99 (38.7) | 39 (31.0) | ||
| Type of health coverage | None | 88 (34.4) | 35 (27.3) | |
| Public insurance | 129 (50.4) | 72 (56.3) | 0.377 | |
| Private insurance | 39 (15.2) | 21 (16.4) |
Results are given in terms of frequency (percentage) or mean ± standard deviation. p-values < 0.05 are presented in bold and represent statistically significant differences.
Sample size calculation
WinPepi was used to calculate the sample size needed to test the difference between proportions in a case–control study with a power of 80% and a significance level of 5%. 25 The expected proportion of the population with a specific outcome was set at 0.65. This value was computed as an average value to represent patients with limited access to medicine (65%) based on opinions of 30 community pharmacists. To allow the detection of the impact of the COVID-19 pandemic, participants from the second study were considered cases and those from the first were the control group (allocation 1:2). This yielded a necessary sample size of 128 cases and 256 controls matched for age and sex.
Data collection
Four pharmacy students were responsible for data collection in both timeframes during their internship period (9 am–2 pm). They approached patients in community pharmacies and explained the study’s objectives. If they accepted to participate, their data were only collected if they answered with “Yes” to the question: Are you currently using psychotropic drugs? Data collection was performed through a uniform survey (Supplementary material) developed after an extensive literature review taking into consideration two experts′ opinions. The survey was initially piloted on 15 patients (only in the period before the pandemic), and questions that lacked clarity or comprehensiveness were adjusted or deleted accordingly. The survey was filled at their time and place preferences. It was available in Arabic (official language in Lebanon) and took an average of 10 min per participant to complete.
General characteristics of the participants
The survey included questions about the general characteristics of the participants (age, sex, marital status (single, married, and divorced/widowed), governorate of residence, and level of education (<middle school, high school, and university or more)). Participants were also asked about their household arrangements (alone, with family, or with medical assistance). Information about the employment status (employed or unemployed) and the type of health coverage (public, private insurance, or none) was collected as well in this part.
Lifestyle habits of the participants
This section collected information about participants’ smoking status (cigarettes or Nargileh) and whether active or passive. Nargileh is also called shisha or waterpipe and is considered a common type of smoking in Lebanon. Moreover, this part collected participants’ drinking habits (alcohol and caffeine consumption) and their physical activity status.
Medical and medication history of the participants
The presence of comorbidities such as diabetes, hypertension, dyslipidemia, cardiovascular diseases, mental disorders, cancer, peptic ulcer, and respiratory diseases was collected in this part (multiple answers were allowed). The name of the psychotropic drug (s) previously or currently taken by the participants was also collected in this part and was then classified into four types of drugs by a clinical pharmacist: (1) antipsychotics (typical or atypical), (2) antidepressants (TriCyclic Antidepressant, Selective serotonin reuptake inhibitors, Serotonin, and norepinephrine reuptake inhibitors), (3) anti-anxiety drugs (Benzodiazepines), and (4) mood stabilizers (lithium, anticonvulsants).
Difficulties in finding psychotropic drugs before and during the COVID-19 pandemic
Patients were asked if they had difficulties finding their psychotropic medication during the past 3 months. These difficulties include lack of access to pharmacies, difficulties in renewing the medical prescription, not finding the required dosage or number of boxes needed, and inability to find the medication.
Statistical analysis
Statistical analyses were performed using Statistical Package for Social Sciences (SPSS Inc, Chicago, Illinois) Version 27. 26 Based on the values of the skewness and Kurtosis of the sample, it is normally distributed and converge to the actual values. 27 The age of patients is presented using means and standard deviations while categorical variables are presented using frequencies and percentages. A bivariate analysis was conducted taking the general characteristics of the participants as independent variables and having difficulties finding the medication as the dependent variable. The aforementioned analysis was conducted before and during the COVID-19 pandemic. The Chi-square/Fisher exact test was used to compare percentages between associate categorical variables. The unpaired student t-test/Mann–Whitney test was used for the comparison of data between two different groups. A multivariate analysis using a logistic regression model was performed to assess the predictors of having difficulties finding the drug. These analyses produced odd ratios with a 95% confidence interval (CI). Independent variables were only selected if they had p-values < 0.20 in bivariate analyses. A p-value < 0.05 was considered statistically significant.
Ethical considerations
This study used a survey for data collection without any type of invasive procedures or intervention. Data were completely anonymous and non-identifiable; storage of data follow-up university general data protection regulation guidelines and written informed consent was obtained from each participant. They were also informed that they could withdraw their participation at any point during the interview. Findings were considered for research purposes only and no financial incentives were provided.
Results
Lifestyle habits of the participants
Table 2 presents the lifestyle habits of the study sample. Statistically significant differences between cases and controls were reported as regards cigarette smoking and physical activity where 141 of the controls (55.1%) were cigarette smokers compared to only 38 cases (29.7%; p < 0.001). Furthermore, more cases (41.3%) practiced physical activity compared to a significantly lower percentage of controls (24.2%; p < 0.001). Nevertheless, no differences were shown in terms of smoking shisha, passive smoking, alcohol, and caffeine consumption.
Table 2.
Lifestyle habits of the study sample before and during the COVID-19 pandemic.
| Before COVID-19 (controls) |
During COVID-19 (cases) |
p-value | |
|---|---|---|---|
| Frequency (%) | Frequency (%) | ||
| Cigarette smoking | 141 (55.1) | 38 (29.7) | < 0.001 |
| Shisha smoking | 74 (29.0) | 44 (34.4) | 0.284 |
| Passive smoking | 160 (62.7) | 78 (62.9) | 0.976 |
| Alcohol consumption | 39 (15.3) | 19 (14.8) | 0.908 |
| Caffeine consumption | 231 (90.2) | 110 (85.9) | 0.208 |
| Physical activity | 62 (24.2) | 52 (41.3) | < 0.001 |
Results are given in terms of frequency (percentage). p-values < 0.05 are presented in bold and represent statistically significant differences.
Medical and medication history of the participants
The comparison of the medical history between cases and controls is presented in Table 3 below. More than 70% of patients reported having comorbidities in both cases and controls (p = 0.523). No differences were reported between cases and controls as regards having hypertension (17.2% and 16.8%; p = 0.923), diabetes (5.5% and 7.4%; p = 0.473), dyslipidemia (12.6% and 13.7%; p = 0.771), cardiovascular diseases (7.8% of both cases and controls) and peptic ulcer disease (7.8% and 7.0%; p = 0.781). Nonetheless, more cases (49.2%) reported having a diagnosed mental disorder compared to 33.2% of controls (p = 0.002) and a higher percentage of controls (6.6%) suffered from cancer (p = 0.031).
Table 3.
Medical history of the study sample before and during the COVID-19 pandemic.
| Before COVID-19 (controls) |
During COVID-19 (cases) |
p-value | |
|---|---|---|---|
| Frequency (%) | Frequency (%) | ||
| Do you have comorbidities? | 180 (70.3) | 94 (73.4) | 0.523 |
| Hypertension | 43 (16.8) | 22 (17.2) | 0.923 |
| Diabetes | 19 (7.4) | 7 (5.5) | 0.473 |
| Dyslipidemia | 35 (13.7) | 16 (12.6) | 0.771 |
| Cardiovascular diseases | 20 (7.8) | 10 (7.8) | 1.000 |
| Mental disorders | 85 (33.2) | 63 (49.2) | 0.002 |
| Cancer | 17 (6.6) | 2 (1.6) | 0.031 |
| Peptic ulcer disease | 18 (7.0) | 10 (7.8) | 0.781 |
| Respiratory disease | 13 (5.1) | 3 (2.3) | 0.206 |
Results are given in terms of frequency (percentage). p-values < 0.05 are presented in bold and represent statistically significant differences.
Figure 1 illustrates the comparison in psychotropic medications consumption before and during the COVID-19 pandemic. No significant difference was noted in terms of mood stabilizer consumption (6.3% of controls and 8.2% of cases; p = 0.537). Nevertheless, a higher percentage of patients (36.8%) used anti-anxiety medications before the pandemic compared to 24.6% of patients during the pandemic (p = 0.012). In contrast, more patients (63.1%) used antidepressants during the pandemic in comparison to before it (52.4%; p = 0.039).
Figure 1.
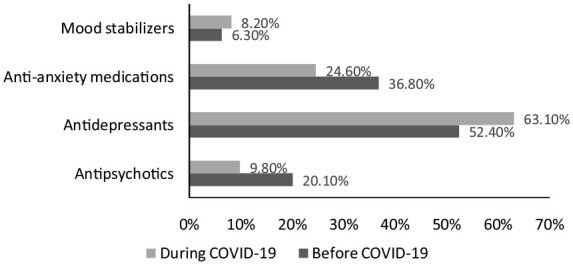
Comparison in psychotropic medications consumption before and during the COVID-19 pandemic.
Association between having difficulties finding the psychotropic medications and the general characteristics of the patients
Before the pandemic, age was significantly associated with having difficulties finding psychotropic medication with a higher percentage of those aged < 60 years (p = 0.019). During the pandemic, more patients faced difficulties finding their medication with no differences in terms of age groups (p = 0.387). Twenty-five percent of patients living in the north of Lebanon had difficulties finding their medication before the pandemic compared to 75% of those living in Mount Lebanon (p < 0.001). Almost half of the controls who live alone or with their families reported difficulties accessing their medication compared to only 26.1% of those with medical assistance (p = 0.050). Moreover, those employed reported having more difficulties accessing their psychotropic medication before the pandemic compared to unemployed patients (p = 0.050). Nevertheless, during the pandemic, no significant differences were noted as regards the place of residence, household arrangement, or employment status (p > 0.05; Table 4).
Table 4.
Association between having difficulties finding the psychotropic medications and the general characteristics of the patients.
| Having difficulties finding the psychotropic medication | |||||
|---|---|---|---|---|---|
| Before COVID-19 (controls) | p-value | During COVID-19 (cases) | p-value | ||
| Frequency (%) | Frequency (%) | ||||
| Sex | Male | 47 (56.6) | 0.142 | 14 (63.6) | 0.457 |
| Female | 81 (46.8) | 26 (54.2) | |||
| Age (years) | 18–40 | 85 (53.5) | 24 (52.2) | ||
| 41–60 | 41 (49.4) | 0.019 | 14 (70.0) | 0.387 | |
| More than 60 | 2 (14.3) | 2 (50.0) | |||
| Governorate of residence | Beirut | 81 (54.4) | 15 (55.6) | ||
| North | 13 (25.0) | 2 (40.0) | |||
| South | 12 (48.0) | <0.001 | 4 (100.0) | 0.451 | |
| Mount Lebanon | 12 (75.0) | 18 (56.3) | |||
| Bekaa | 8 (66.7) | 1 (50.0) | |||
| Marital status | Single | 39 (47.0) | 11 (47.8) | ||
| Married | 67 (54.0) | 0.445 | 24 (61.5) | 0.544 | |
| Divorced/widowed | 22 (44.9) | 5 (62.5) | |||
| Household arrangement | With family | 27 (49.1) | 15 (75.0) | ||
| Alone | 94 (53.1) | 0.050 | 21 (50.0) | 0.162 | |
| Medical assistance | 6 (26.1) | 4 (50.0) | |||
| Level of education | <Middle school | 30 (47.6) | 8 (50.0) | ||
| High school | 42 (50.6) | 0.908 | 15 (60.0) | 0.802 | |
| University or more | 55 (50.9) | 17 (58.6) | |||
| Employment status | Employed | 86 (54.8) | 0.050 | 28 (57.1) | 1.000 |
| Unemployed | 42 (42.4) | 12 (57.1) | |||
Results are given in terms of frequency (percentage). p-values < 0.05 are presented in bold and represent statistically significant differences.
Predictors of having difficulties finding psychotropic medications before the COVID-19 pandemic
The predictors of having difficulties finding psychotropic medications before the COVID-19 pandemic are presented in Table 5. It has been reported that the odds of having difficulties finding psychotropic drugs were 1.01 higher per increase of 1 year in age (OR 1.01, 95% CI = [1.00, 1.02]). Moreover, patients having medical assistance had 69% lower odds of having difficulties finding their medication compared to those living alone (OR 0.31, 95% CI = [0.12, 0.83]). Furthermore, those living in the North of Lebanon had 72% lower odds of having difficulties finding their medication compared to those in the capital Beirut (OR 0.28, 95% CI = [0.14, 0.57]). A significant correlation was also noted between being employed and having difficulties finding the medication with 1.64 higher odds compared to unemployed patients (OR 1.64, 95% CI = [1.01, 2.73]).
Table 5.
Predictors of having difficulties finding psychotropic medications before the COVID-19 pandemic.
| Crude model | ||
|---|---|---|
| OR [95% CI] | p-value | |
| Age in years (per increase of 1 year) | 1.01 [1.00, 1.02] | 0.050 |
| Female sex (male as reference) | 0.67 [0.39, 1.14] | 0.143 |
| Household arrangement (Alone as reference) | ||
| With family | 0.85 [0.46, 1.56] | 0.603 |
| With medical assistance | 0.31 [0.12, 0.83] | 0.019 |
| Governorate of residence (Beirut as reference) | ||
| Mount-Lebanon | 2.52 [0.78, 8.17] | 0.124 |
| South | 0.78 [0.33, 1.81] | 0.556 |
| North | 0.28 [0.14, 0.57] | <0.001 |
| Bekaa | 1.68 [0.48, 5.82] | 0.414 |
| Employment status (Unemployed as reference) | ||
| Employed | 1.64 [1.01, 2.73] | 0.050 |
OR: odds ratio; CI: confidence interval.
Question: Do you find difficulties finding your psychotropic medication? The baseline answer is “No.”. p-values < 0.05 are presented in bold and represent statistically significant differences.
Discussion
This study explored the impact of the COVID-19 pandemic on the consumption patterns of psychotropic medications and the factors affecting access to psychotropic drugs among patients in Lebanon. It also investigated the predictors of having difficulties accessing medication. Overall, more patients used antipsychotics and anti-anxiety medications before the pandemic while antidepressants were more used during the pandemic. Almost half of the patients reported facing difficulties finding their medications in both time frames. Nevertheless, before the pandemic, these difficulties were noted per increase in age and being employed and were less faced if patients had medical assistance or lived in the north of Lebanon. More patients reported having difficulties accessing their medication during the pandemic with no significant differences.
During the COVID-19 pandemic, a higher consumption of psychotropic drugs was noted among females. This finding was also reported in a cross-sectional survey performed in Lebanon in 2022 highlighting the impact of lockdowns and other associated stressors during the pandemic on depression and anxiety among patients. 22 Most of the sample was 40 years or less. In agreement with the distribution of the sample, a report published during the pandemic showed that females had two times higher rate of depression and younger population had higher odds of mental disorders. 28 Since controls were age-matched to cases, this result could reflect the age group with most patients using psychotropics during the pandemic. Reports revealed that during the COVID-19 pandemic, young adults had a higher risk of developing psychological problems, 29 possibly related to the fear of getting infected or infecting others, 30 job losses, 31 stress, and frailty. 32 Before the pandemic, patients who resided in the capital (Beirut) were those mostly using psychotropic drugs. Nevertheless, throughout the pandemic, those living in Mount Lebanon had the highest consumption. This finding may be associated with the fact that the highest number of COVID-19 cases were in Mount Lebanon, which has led to more strict containment measures and as a result higher risks of mental disorders. 33 Before the COVID-19 pandemic, a significantly higher percentage of psychotropic patients were smokers in comparison to the period afterward. This result is in accordance with a systematic review published in 2021 and reporting several lifestyle modifications following the pandemic including a decrease in alcohol consumption and cigarette smoking. 34 However, physical activity increased in contrast with the findings of a systematic review that was published recently and reported an increase in sedentary behaviors during the pandemic. 35 Significantly more patients had a history of cancer before the pandemic which can be related to the postponement of the screening and diagnostic tools for the different types of cancer during the pandemic, 36 and as a result, a decrease in the reported cases.
Antidepressants use increased remarkably during the COVID-19 pandemic in agreement with other studies performed in different settings.37–39 A recent study published in 2022 showed an increase in antidepressant use following the outbreak, namely among women and those aged 40 years or more. 40 Nonetheless, a significant decrease in the use of anti-anxiety medications and antipsychotics was noted during the same period. This finding can be explained by the higher preference for antidepressants for the long-term treatment of post-COVID mental disorders since their discontinuation has less severe withdrawal symptoms in comparison to anti-anxiety medications. 41 Moreover, recommendations advised limiting the prescription of benzodiazepine to treat anxiety and depression during the COVID-19 pandemic due to its association with respiratory depression which may have led to the substitution of benzodiazepines with antidepressants.42,43 More patients faced difficulties finding their medications during the COVID-19 pandemic in comparison to the period before, possibly due to the over-storage of many products including medicines, 44 and the fear of having difficulties accessing treatments which have led to a shortage of many drugs such as psychotropics. 45 However, these difficulties were not significantly varying with any of the general characteristics of the patients contrary to the period before the pandemic. In contrast, a study conducted in Bangladesh reported that patients with more comorbidities or those with multimorbidity were more likely to experience difficulties accessing their medications. 46 This incompatible result in this study can be due to the increase in the prices of medicines and the lack of access to new treatments in Lebanon during the pandemic.47,48 The odds of having difficulties finding psychotropic drugs before the pandemic were higher per increase of 1 year in age. Non-adherence to medication was reported to be higher with age, 49 which may potentially lead to skipping dosage or excess intake of medicines. 50 Moreover, patients in this study who had medical assistance had lower odds of having difficulties finding their medication compared to those living with their families or alone. Social and clinical support can improve adherence to treatments, 51 and better monitoring of the needs of patients in advance. Lower odds of having difficulties finding medications were noted among those living in the North of Lebanon compared to those in the capital. This easier access to medication may be associated with their location next to the Syrian border and consequently, the importation of unfound drugs in Lebanon from Syria. 52 Employed patients faced more challenges finding their medication compared to unemployed ones possibly due to time and work constraints or their reliance on other family members in the supply of drugs.
This study has limitations. The relatively small sample size in addition to the convenience sampling method might not have reflected the actual distribution of patients using psychotropics and, therefore, can affect the generalizability of the findings to other patients. Given that data were self-reported, recall bias might have arisen, namely, during the pandemic given the existence of other priorities. This bias was reduced since the survey was filled out at the time and place preferences of the patients. The present study has also strengths. Patients from the two-time frames were age and sex-matched which allowed a stronger detection of the impact of the pandemic itself. Furthermore, to our knowledge, this is the first study assessing access to medicines among psychotropic patients before and during the COVID-19 pandemic.
Conclusion
The COVID-19 pandemic affected the consumption patterns of psychotropics with a higher use of antidepressants and a lower use of anti-anxiety and antipsychotic drugs during the aforementioned period. Before the pandemic, patients reported facing difficulties accessing their medications which were associated with the increase in 1 year of age and being employed, and were less faced if patients had medical assistance or lived in the north of Lebanon. More patients faced these difficulties during the pandemic with no significant differences between them. Further investigation through a longitudinal study is recommended to assess the current situation in Lebanon.
Supplemental Material
Supplemental material, sj-docx-1-map-10.1177_27550834231163706 for Impact of the COVID-19 pandemic on the consumption patterns of psychotropic drugs and predictors of limited access to medication by Maya Rachidi, Georges Hatem, Melissa Hatem, Salam Zein, Samar Rachidi and Sanaa Awada in The Journal of Medicine Access
Supplemental material, sj-docx-2-map-10.1177_27550834231163706 for Impact of the COVID-19 pandemic on the consumption patterns of psychotropic drugs and predictors of limited access to medication by Maya Rachidi, Georges Hatem, Melissa Hatem, Salam Zein, Samar Rachidi and Sanaa Awada in The Journal of Medicine Access
Acknowledgments
We thank Dr Mathijs Goossens for his assistance with the analysis of data and for his comments that greatly improved the manuscript.
Footnotes
ORCID iD: Georges Hatem  https://orcid.org/0000-0003-0964-9722
https://orcid.org/0000-0003-0964-9722
Supplemental material: Supplemental material for this article is available online.
Declarations
Ethics approval and consent to participate: The study protocol, survey, and consent form were reviewed and approved by the institutional review board of the faculty of pharmacy of the Lebanese University (reference: 7/21/D). Written informed consent was obtained from every participant.
Consent for publication: Not applicable.
Author contribution(s): Maya Rachidi: Data curation; Methodology; Project administration; Writing – original draft.
Georges Hatem: Conceptualization; Data curation; Formal analysis; Validation; Writing – original draft.
Melissa Hatem: Data curation; Methodology; Writing – original draft.
Salam Zein: Conceptualization; Methodology; Validation; Writing – review & editing.
Samar Rachidi: Investigation; Methodology; Resources; Supervision; Writing – review & editing.
Sanaa Awada: Conceptualization; Methodology; Project administration; Supervision; Writing – review & editing.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Availability of data and materials: Not applicable.
References
- 1.Clement J, Jacobi M, Greenwood BN.Patient access to chronic medications during the Covid-19 pandemic: evidence from a comprehensive dataset of US insurance claims. PLoS ONE 2021; 16(4): e0249453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Yao H, Chen JH, Xu YF.Patients with mental health disorders in the COVID-19 epidemic. Lancet Psychiatry 2020; 7: E21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kumar A, Nayar KR.COVID 19 and its mental health consequences. Milton Park, Abingdon: Taylor & Francis, 2021, p. 1-2. [DOI] [PubMed] [Google Scholar]
- 4.Hossain MM, Tasnim S, Sultana A, et al. Epidemiology of mental health problems in COVID-19: a review. F1000res 2020; 9: 636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Păunescu RL, Miclu Ia IV, Verişezan OR, et al. Acute and long‑term psychiatric symptoms associated with COVID‑19. Biomed Rep 2023; 18(1): 4–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Arias Molina Y, Herrero Solano Y, Cabrera Hernández Y, et al. Manifestaciones psicológicas frente a la situación epidemiológica causada por la COVID-19. Revista Habanera De Ciencias Médicas 2020; 19: 1–13. [Google Scholar]
- 7.Chong YY, Frey E, Chien WT, et al. The role of psychological flexibility in the relationships between burnout, job satisfaction, and mental health among nurses in combatting COVID-19: a two-region survey. J Nurs Scholar. Epub ahead of print 6 Jan 2023. DOI: 10.1111/jnu.12874. [DOI] [PubMed] [Google Scholar]
- 8.Clemente-Suárez VJ, Martínez-González MB, Benitez-Agudelo JC, et al. The impact of the COVID-19 pandemic on mental disorders: a critical review. Int J Environ Res Public Health 2021; 18: 10041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Winkler P, Formanek T, Mlada K, et al. Increase in prevalence of current mental disorders in the context of COVID-19: analysis of repeated nationwide cross-sectional surveys. Epidemiol Psychiatr Sci 2020; 29: e173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Maguire A, Kent L, O'Neill S, et al. Impact of the COVID-19 pandemic on psychotropic medication uptake: time-series analysis of a population-wide cohort. Br J Psychiatry 2022; 221(6): 748–757. [DOI] [PubMed] [Google Scholar]
- 11.Villanueva-Silvestre V, Vázquez-Martínez A, Isorna-Folgar M, et al. Problematic internet use, depressive symptomatology and suicidal ideation in university students during COVID-19 confinement. Psicothema 2022; 34: 518–527. [DOI] [PubMed] [Google Scholar]
- 12.Villanueva-Blasco V, Villanueva-Silvestre V, Vázquez-Martínez A.Relationship between depression and risky alcohol consumption in women: the mediating role of coping styles and age. Int J Ment Health Addict 2022; 12: 1–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gheni AY, Yousif HA, Jusoh YY.Online medical consultation: covid-19 system using software object-oriented approach. Bull Electr Eng Inform 2021; 10: 3471–3480. [Google Scholar]
- 14.Hatem G, Navasardyan N, Lahoud E, et al. Predictors of substitution to generic drugs and physicians’ perceived exclusivity of substitution: a cross sectional survey among physicians. J Generic Med 2022; 19: 17411343221107569. [Google Scholar]
- 15.Hatem G, Lahoud E, Halwani L, et al. The unified medical prescription as a tool to promote generic prescription: a cross-sectional study addressing physicians’ perception in Lebanon. J Generic Med 2022; 18: 17411343221076963. [Google Scholar]
- 16.Marehin M-S, Hinnouo AM, Obiang P-A.Organization of psychiatric care in Gabon during the Covid-19 epidemic. Annales Medico-psychologiques 2020; 179: 137–140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Otiashvili D, Mgebrishvili T, Beselia A, et al. The impact of the COVID-19 pandemic on illicit drug supply, drug-related behaviour of people who use drugs and provision of drug related services in Georgia: results of a mixed methods prospective cohort study. Harm Reduct J 2022; 19: 1–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Shrestha AB, Aryal M, Magar JR, et al. The scenario of self-medication practices during the covid-19 pandemic; a systematic review. Ann Med Surg 2022; 82: 104482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kronfol NM.Rebuilding of the Lebanese health care system: health sector reforms. East Mediterr Health J 2006; 12(3–4): 459–473. [PubMed] [Google Scholar]
- 20.Hatem G, Goossens M.Health care system in Lebanon: a review addressing health inequalities and ethical dilemmas of frontline workers during COVID-19 pandemic. BAU J Health Wellbeing 2022; 5: A4887. [Google Scholar]
- 21.Huang Y, Zhao N.Generalized anxiety disorder, depressive symptoms and sleep quality during COVID-19 outbreak in China: a web-based cross-sectional survey. Psychiat Res 2020; 288: 112954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Khalil RB, Dagher R, Zarzour M, et al. The impact of lockdown and other stressors during the COVID-19 pandemic on depression and anxiety in a Lebanese opportunistic sample: an online cross-sectional survey. Current Psychology 2022; 10: 1742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Farran N.Mental health in Lebanon: tomorrow’s silent epidemic. Ment Health Prev 2021; 24: 200218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Abi Hana R, Arnous M, Heim E, et al. Mental health stigma at primary health care centres in Lebanon: qualitative study. Int J Mental Health Syst 2022; 16: 1–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Abramson JH.WINPEPI updated: computer programs for epidemiologists, and their teaching potential. Epidemiol Perspect Innovat 2011; 8: 1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.George D, Mallery P.IBM SPSS statistics 26 step by step: a simple guide and reference. Abingdon: Routledge, 2019. [Google Scholar]
- 27.Hatem G, Zeidan J, Goossens M, et al. Normality testing methods and the importance of skewness and kurtosis in statistical analysis. BAU J Sci Tech 2022; 3: 7. [Google Scholar]
- 28.Villanueva-Blasco VJ, Villanueva-Silvestre V, Vázquez-Martínez A, et al. Depression, suicidal ideation, and consumption of psychotropic drugs during lockdown by COVID-19 according to gender and age. Int J Mental Health Addict 2022; 2022: 1-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lee CM, Cadigan JM, Rhew IC.Increases in loneliness among young adults during the COVID-19 pandemic and association with increases in mental health problems. J Adolesc Health 2020; 67(5): 714–717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hoffart A, Johnson SU, Ebrahimi OV.The network of stress-related states and depression and anxiety symptoms during the COVID-19 lockdown. J Affect Disord 2021; 294: 671–678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Murray S, Olivares E.Job losses during the onset of the COVID-19 pandemic: stay-at-home orders, industry composition, and administrative capacity. Industry Composition, and Administrative Capacity, 2020, https://papers.ssrn.com/sol3/papers.cfm?abstract_id=3633502
- 32.Hawes MT, Szenczy AK, Klein DN, et al. Increases in depression and anxiety symptoms in adolescents and young adults during the COVID-19 pandemic. Psychol Med 2022; 52: 3222–3230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Fridman GA.Use of psychotropic drugs during the Argentine quarantine due to the COVID-19 pandemic. Pharm Pharmacol Int J 2021; 9(2): 39–43. [Google Scholar]
- 34.Sane Schepisi M, Di Napoli A, Asciutto R, et al. The 2008 financial crisis and changes in lifestyle-related behaviors in Italy, Greece, Spain, and Portugal: a systematic review. Int J Environ Res Public Health 2021; 18: 8734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Stockwell S, Trott M, Tully M, et al. Changes in physical activity and sedentary behaviours from before to during the COVID-19 pandemic lockdown: a systematic review. BMJ Open Sport Exerc Med 2021; 7(1): e000960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Fagundes TP, Albuquerque RM, Miranda DLP, et al. Dealing with cancer screening in the COVID-19 era. Rev Assoc Med Bras (1992) 2021; 67(Suppl. 1): 86–90. [DOI] [PubMed] [Google Scholar]
- 37.de Oliveira Costa J, Gillies MB, Schaffer AL, et al. Changes in antidepressant use in Australia: a nationwide analysis (2015–2021). Aust N Z J Psychiatry 2023; 57: 49–57. [DOI] [PubMed] [Google Scholar]
- 38.Rabeea SA, Merchant HA, Khan MU, et al. Surging trends in prescriptions and costs of antidepressants in England amid COVID-19. Daru 2021; 29(1): 217–221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Yavuz-Guzel E, Atasoy A, Gören İE, et al. Impact of COVID-19 pandemic on antidepressants consumptions by wastewater analysis in Turkey. Sci Total Environ 2022; 838: 155916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Leong C, Kowalec K, Eltonsy S, et al. Psychotropic medication use before and during COVID-19: a population-wide study. Front Pharmacol 2022; 13: 886652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Rohilla J, Tak P, Jhanwar S, et al. Primary care physician's approach for mental health impact of COVID-19. J Family Med Primary Care 2020; 9: 3189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Shah K, Kamrai D, Srinivas S, et al. Benzodiazepine interaction with COVID-19 drugs. Prim Care Companion CNS Disord 2021; 23: 37719. [DOI] [PubMed] [Google Scholar]
- 43.Clelland CL, Ramiah K, Steinberg L, et al. Analysis of the impact of antidepressants and other medications on COVID-19 infection risk in a chronic psychiatric in-patient cohort. Bjpsych Open 2022; 8: e6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Goodwin R, Wiwattanapantuwong J, Tuicomepee A, et al. Anxiety, perceived control and pandemic behaviour in Thailand during COVID-19: results from a national survey. J Psychiatr Res 2021; 135: 212–217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Costa M, Pavlo A, Reis G, et al. COVID-19 concerns among persons with mental illness. Psychiat Ser 2020; 71: 1188–1190. [DOI] [PubMed] [Google Scholar]
- 46.Mistry SK, Ali ARMM, Yadav UN, et al. Older adults with non-communicable chronic conditions and their health care access amid COVID-19 pandemic in Bangladesh: findings from a cross-sectional study. PLoS ONE 2021; 16(7): e0255534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Chaiban L, Benyaich A, Yaacoub S, et al. Access to primary and secondary health care services for people living with diabetes and lower-limb amputation during the COVID-19 pandemic in Lebanon: a qualitative study. BMC Health Serv Res 2022; 22: 1–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Islam Z, Gangat SA, Mohanan P, et al. Mental health impacts of Lebanon’s economic crisis on healthcare workers amidst COVID-19. Int J Health Plann Manage 2022; 37(2): 1160–1165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Stewart SL, Baiden P.An exploratory study of the factors associated with medication nonadherence among youth in adult mental health facilities in Ontario, Canada. Psychiat Res 2013; 207: 212–217. [DOI] [PubMed] [Google Scholar]
- 50.Nurminen J, Puustinen J, Piirtola M, et al. Psychotropic drugs and the risk of fractures in old age: a prospective population-based study. BMC Public Health 2010; 10: 1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Semahegn A, Torpey K, Manu A, et al. Psychotropic medication non-adherence and its associated factors among patients with major psychiatric disorders: a systematic review and meta-analysis. Syst Rev 2020; 9: 17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Institute GH.The real impact of disastrous medicine shortages in Lebanon, https://ghi.aub.edu.lb/ghiblog/the-real-impact-of-disastrous-medicine-shortages-in-lebanon/ (2022, accessed November 2022).
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-docx-1-map-10.1177_27550834231163706 for Impact of the COVID-19 pandemic on the consumption patterns of psychotropic drugs and predictors of limited access to medication by Maya Rachidi, Georges Hatem, Melissa Hatem, Salam Zein, Samar Rachidi and Sanaa Awada in The Journal of Medicine Access
Supplemental material, sj-docx-2-map-10.1177_27550834231163706 for Impact of the COVID-19 pandemic on the consumption patterns of psychotropic drugs and predictors of limited access to medication by Maya Rachidi, Georges Hatem, Melissa Hatem, Salam Zein, Samar Rachidi and Sanaa Awada in The Journal of Medicine Access


