Hidradenitis suppurativa (HS) is a chronic, recurrent, and debilitating inflammatory skin condition mostly affecting armpits, submammary folds and groins. 1 Pain, malodorous discharge, and scarring often occur, resulting in a significantly decreased quality of life. 2 Up to now, there are no recent data about deodorants use and hair removal in patients suffering from HS, even more new tools and methods have recently been introduced. An 11‐point anonymous online questionnaire on these behaviors was administered to 114 patients affected by HS; 53 males and 61 females aged between 18 and 45 years old with HS‐Physician's Global Assessment (HS‐PGA) score 3 between 1 and 3 were enrolled. The questionnaire was divided into two sections: (i) axillary deodorants and (ii) hair removal habits (Figure 1). Data were analyzed by chi‐square statistics with p < 0.05. Patients with HS suffer significant social stigma, sexual dysfunction, and low self‐esteem. 4 Up to now, the only study on deodorants and shaving in HS patients dates up to 1982 and reported no significant differences in the application of shaving, chemical depilatories, or deodorants in patients with hidradenitis in comparison with the normal controls. Furthermore, it showed that deodorants were not primarily involved in HS initiation. 5
FIGURE 1.
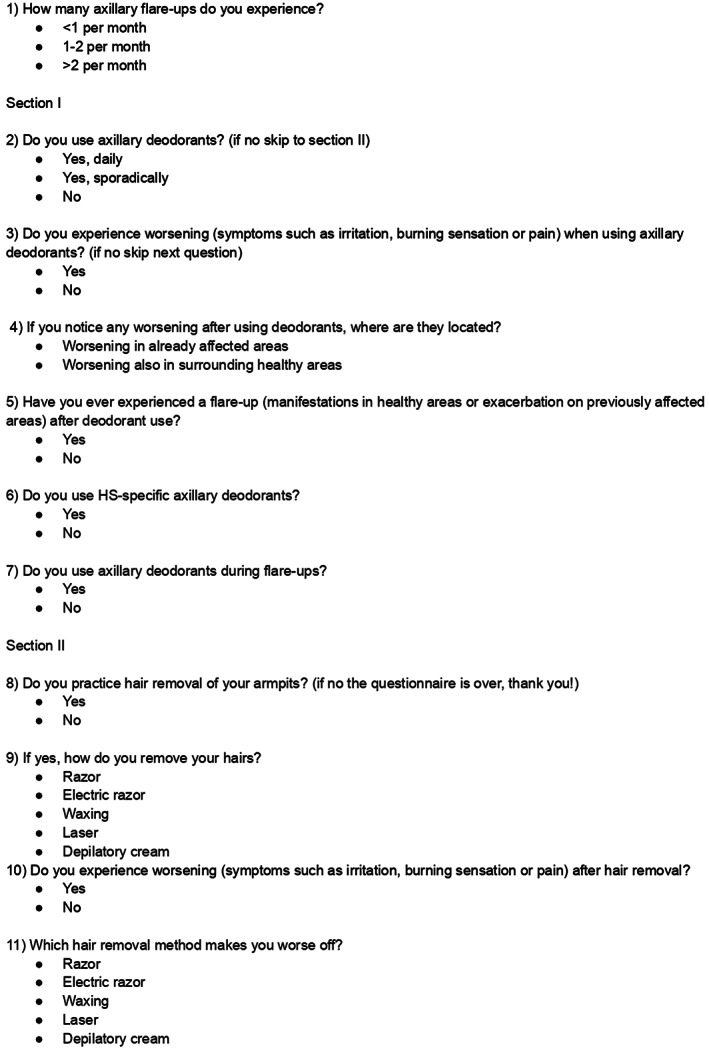
Eleven‐point anonymous online questionnaire on these behaviors administered to 114 patients enrolled, divided into two sections: (i) axillary deodorants and (ii) hair removal habits.
As shown in Figure 2, in our study population, 31% of patients were affected by minimal disease, 39% of patients were affected by mild HS and 44% were affected by moderate HS according to HS‐PGA score. 70.2% of patients affirmed to use axillary deodorants with an inverse relation between use frequency and PGA (p = 0.048). 46.2% of patients reported HS worsening (appearance of manifestations in previously healthy areas) after deodorants use; even more, 45% of patients using deodorants reported a consequent flare‐up (reappearance of manifestations in areas previously affected by the disease and then cured) even if such data were no statistically significant (p > 0.05). Almost one‐third of patients (29.8%) do not use deodorants; this could be due to both real worsening after use and patient fear of a possible worsening. Such hypotheses find additional feedback when patients are asked about deodorants use during a flare‐up; only 25% of them used deodorants in such condition, with higher PGA score related to reduced deodorants use (p = 0.037). Finally, just a few patients (11.9%) used specific deodorants, showing the need for more suited products and better patient education. 65.8% of patients reported to usually shave axillae with an inverse relation between shaving frequency and PGA score (p = 0.001). Although not statistically significant (p > 0.05), 31.7% of patients reported a worsening aftershave, while 34.2% of patients did not shave axillae at all, this could be due to personal choice, fear of flare‐ups, or previous worsening after shaving. Razor resulted in the most used shaving technique (64%) and to be the one which more frequently led to a worsening (60%). Diode laser and intense pulsed light laser, indeed, showed better outcomes than any other method, with no patients reporting worsening after laser hair removal even if it was used only by 8% of patients. Patients with higher HS‐PGA scores have more frequent flare‐ups. Deodorant use is similar and frequent in patients with minimal to mild HS, while almost half of the patients scoring HS‐PGA 3 stated to not use deodorants. Furthermore, patients with a higher HS‐PGA score showed a slightly increased susceptibility of experiencing a worsening after deodorant use, even though most patients stated to experience such worsening in already affected areas, with no significant correlation to HS‐PGA score. Consistent flare‐ups are documented in almost 50% of patients after deodorant use, with a reduced possibility of flare‐ups in patients with minimal disease; this could be explained since patients with minimal disease show less frequent flare‐ups, despite the use or not use of deodorants. It is important to note how a very small percentage of our patients declared to use an HS‐specific deodorant. No guidelines on the use of deodorants in patients suffering from HS have been drawn up, and even more, there are no recommendations on specific types of deodorants should be used.
FIGURE 2.
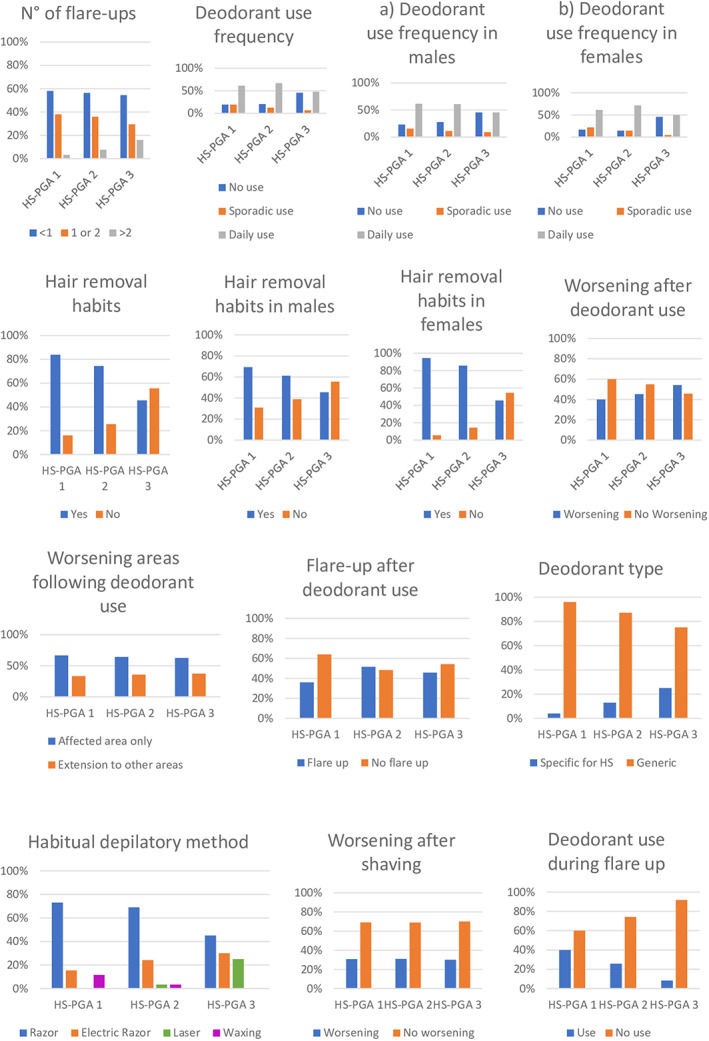
Graphical representation of the data obtained from the responses to the questionnaire.
In conclusion, bigger studies are needed to better clarify deodorants and shaving habits' impact on HS natural history, while specific and safe products for personal hygiene are promptly required; patients' education about shaving is fundamental to better their quality of life too.
AUTHOR CONTRIBUTIONS
WL contributed to the manuscript conception, performed the research, analyzed the data, and wrote the article. GC performed the research, analyzed the data, and wrote the article. GF analyzed the data and reviewed the paper for important intellectual content. CM contributed to the manuscript conception, analyzed the data, and reviewed the paper for important intellectual content.
CONFLICT OF INTEREST
None of the contributing authors has any conflict of interest, including specific financial interests or relationships and affiliation relevant to the subject matter or discussed materials in the manuscript.
ETHICAL APPROVAL
This study has been approved by the local ethics committee of A.O.U. Federico II of Naples and complies with the ethical standards of the Helsinki Declaration of 1975, as revised in 1983.
ACKNOWLEDGMENT
The patients in this manuscript have given written informed consent to the publication of their case details. Open Access Funding provided by Universita degli Studi di Napoli Federico II within the CRUI‐CARE Agreement.
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the corresponding author upon reasonable request.
REFERENCES
- 1. Goldburg SR, Strober BE, Payette MJ. Hidradenitis suppurativa: epidemiology, clinical presentation, and pathogenesis. J Am Acad Dermatol. 2020;82(5):1045‐1058. [DOI] [PubMed] [Google Scholar]
- 2. Garg A, Kirby JS, Lavian J, Lin G, Strunk A. Sex‐ and age‐adjusted population analysis of 386 prevalence estimates for hidradenitis suppurativa in the United States. JAMA Dermatol. 2017;153(8):760‐764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Zouboulis CC, Desai N, Emtestam L, et al. European S1 guideline for the treatment of hidradenitis 493 suppurativa/acne inversa. J Eur Acad Dermatol Venereol. 2015;29(4):619‐644. [DOI] [PubMed] [Google Scholar]
- 4. Kirby JS, Butt M, Esmann S, Jemec GBE. Association of resilience with depression and health‐related quality of life for patients with hidradenitis suppurativa. JAMA Dermatol. 2017;153(12):1263‐1269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Morgan WP, Leicester G. The role of depilation and deodorants in hidradenitis suppurativa. Arch Dermatol. 1982;118(2):101‐102. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.


