Dear Editor,
Pityriasis versicolor is a frequent, benign, superficial fungal infection of the skin caused by Malassezia species that induces a characteristic rash of thin and scaly macules that can be hypopigmented, hyperpigmented, or erythematous. 1 Diagnosis is usually made clinically, based on characteristic skin lesions and the “evoked scale sign” (when stretching or scraping the skin makes the fine scale of lesions more apparent). 1 Diagnosis is confirmed by microscopic examination. First‐line treatment is based on the use of topical and/or systemic antifungals, depending on the extent of lesions and therapeutic response. 2 Disease recurrence is frequent, so prophylactic therapy is often indicated in the months following the resolution of skin manifestations. 2
A 23‐year‐old patient presented at the Mycology Department of the University Federico II of Naples with erythematous and dyschromic macular lesions on the dorsal and pectoral regions, which had been present for about 3 years (Figure 1A). She also reported intense itchy symptoms in the areas affected by lesions. She denied other comorbidities, stressogenic triggering events, and drug intake. During these years, she had practiced topical antifungal therapy and short cycles of systemic antihistamine therapy, always with little clinical benefit. Based on the history and clinical picture, it was decided to perform a venous blood sampling for routine hematochemical tests (normal). A Wood's lamp examination was then performed, where positive fluorescence was found (Figure 1B). The “evoked scale sign” was positive. Finally, a direct microscopic examination for mycetes was performed with 10% potassium hydroxide (KOH), where hyphae and sprouting cells (spaghetti and meatball appearance) were found (Figure 1C). All this allowed us to confirm the suspected diagnosis of pityriasis versicolor. Moreover, given the reported itchy symptoms and the appearance of pomphi during the execution of skin scale sampling for microscopic examination, the sign of dermographism was searched in correspondence with skin lesions and also of the perilesional skin, which resulted positive (Figure 1D). This sign was also searched in other areas of the body unaffected by skin manifestations, with negative results. Dermographism was positive only at the level of pityriasis versicolor lesions. A 1‐month course of therapy with oral antifungal medications (itraconazole) was prescribed, with a daily dose of 200 mg for 5 days a week, with resolution of manifestations.
FIGURE 1.
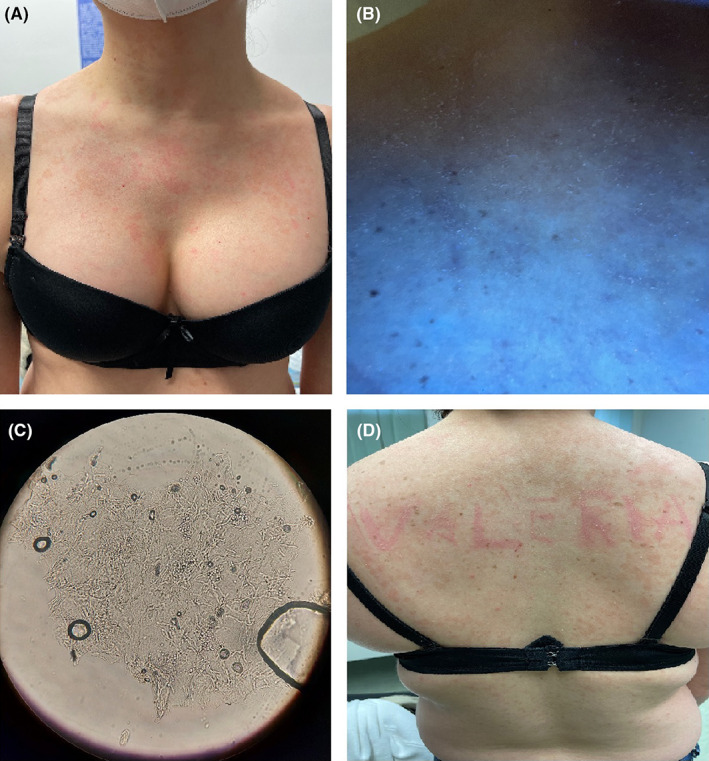
(A) Erythematous and dyschromic macular lesions on the dorsal region. (B) Positive fluorescence at Wood's lamp examination. (C) Hyphae and sprouting cells (spaghetti and meatball appearance) observed to a direct microscopic examination. (D) Positive dermographism in correspondence with pityriasis versicolor lesions
After this observation, we researched this sign in other 30 patients affected by forms of pityriasis versicolor, diagnosed clinically and with microscopic and cultural examinations, diffuse and/or resistant to conventional treatments, with an average duration of skin manifestations of 2.2 years ±0.6 standard deviation (SD). Of the 30 patients, 27 (90%) had positive dermographism at the cutaneous lesions of pityriasis versicolor (Figure 2). In addition, an interesting finding that emerged was that in the 27 patients in whom the sign was positive, Malassezia globosa was the etiologic agent found by cultural examination. In the other three patients in whom the sign was negative, Malassezia furfur was the pathogen found by cultural examination.
FIGURE 2.
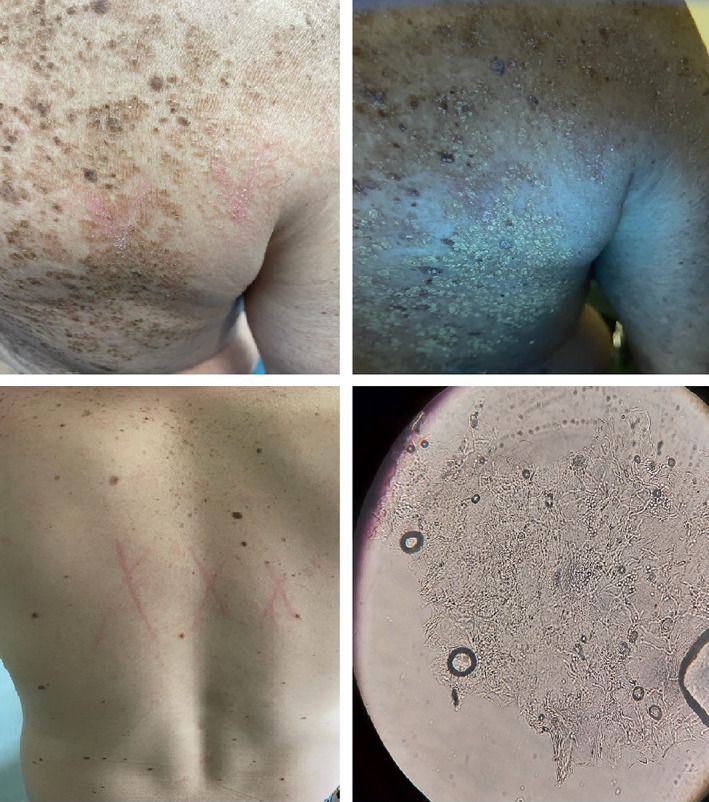
Clinical and microscopical presentation of other patients with positive “PiMa sign”
Actually, there are no cases of pityriasis versicolor in the literature in which dermographism has been shown to be positive only at the level of skin lesions of this pathology.
It is currently known that Malassezia produces MGL_1304, a major histamine‐releasing antigen. 3 MGL_1304 is produced at a size of 29 kDa by Malassezia globosa and secreted into sweat after being processed and converted into the mature form of 17 kDa. 3 , 4 , 5 This form induces significant histamine release from basophils of patients. 4 Our hypothesis is that in extensive and active forms of pityriasis versicolor, in which there is an abundant presence of Malassezia at the level of skin lesions, it is possible that through the release of MGL_1304, there is an increased propensity for histamine release from the areas of the body affected by pityriasis. This mechanism would explain the reason for the positive dermographism only at the level of skin lesions.
This particular type of dermographism, which we have called “PiMa sign,” from the initials of the fungus involved in the pathogenesis of this pathology, Malassezia (Pityrosporum), which corresponds to the initials of the authors who first observed this phenomenon (Picone V. and Martora F.), could enrich the clinical semeiotics that characterizes this pathology. To date, despite numerous evidence regarding increased histamine release caused by Malassezia globosa, 3 , 4 , 5 this phenomenon has not yet been described in the literature, not to our knowledge.
However, the limited number of cases described and the pathophysiological mechanism still not well characterized represent points to be investigated in the future. In this regard, we hope that this manuscript will encourage new, larger, and more structured work on this phenomenon, so as to test our hypothesis and better characterize it from a pathophysiological point of view.
We believe that our experience may encourage other colleagues to research this sign in forms of pityriasis versicolor extended and long‐lasting.
AUTHOR CONTRIBUTIONS
V.P. and F.M. performed the research, designed the research study, analyzed the data, and wrote the paper. V.P., F.M., L.G., and G.F. contributed essential reagents or tools.
CONFLICT OF INTEREST
None of the contributing authors has any conflict of interest, including specific financial interests or relationships and affiliation relevant to the subject matter or discussed materials in the manuscript.
ETHICAL APPROVAL
The following study was conducted in accordance with the principles of the Declaration of Helsinki.
INFORMED CONSENT
The patients in this manuscript have given written informed consent to the publication of their case details.
ACKNOWLEDGMENT
All authors equally contributed to the work. Open Access Funding provided by Universita degli Studi di Napoli Federico II within the CRUI‐CARE Agreement.
DATA AVAILABILITY STATEMENT
Data are reported in the current study.
REFERENCES
- 1. Renati S, Cukras A, Bigby M. Pityriasis versicolor. BMJ. 2015;350:h1394. doi: 10.1136/bmj.h1394 [DOI] [PubMed] [Google Scholar]
- 2. Karray M, McKinney WP. Tinea Versicolor. StatPearls. StatPearls Publishing; 2021. [PubMed] [Google Scholar]
- 3. Takahagi S, Tanaka A, Hide M. Sweat allergy. Allergol Int. 2018;67(4):435‐441. doi: 10.1016/j.alit.2018.07.002 [DOI] [PubMed] [Google Scholar]
- 4. Hiragun T, Hide M. Sweat Allergy. Curr Probl Dermatol. 2016;51:101‐108. doi: 10.1159/000446788 [DOI] [PubMed] [Google Scholar]
- 5. Hiragun T, Hiragun M, Ishii K, Kan T, Hide M. Sweat allergy: Extrinsic or intrinsic? J Dermatol Sci. 2017;87(1):3‐9. doi: 10.1016/j.jdermsci.2017.03.002 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data are reported in the current study.


