Abstract
Objective: To probe the effect of graded cardiac rehabilitation care on clinical efficacy and quality of life in patients with severe coronary heart disease (CHD) after treatment with off-pump coronary artery bypass (OPCAB). Methods: Data of 100 patients with severe CHD treated by OPCAB from February 2020 to August 2021 in Tongji Hospital, Tongji Medical College, Huazhong University of Science and Technology were retrospectively collected. Based on the nursing methods, 52 patients who receiving graded cardiac rehabilitation care were divided to an observation group, and 48 patients receiving conventional cardiac rehabilitation care were divided to a control group. Clinical efficacy, cardiac and pulmonary functions, exercise endurance, quality of life, and adverse cardiovascular events were assessed after 6 months of rehabilitation. According to the prognosis, the patients were divided into a poor prognosis group and a good prognosis group. The risk factors of adverse cardiovascular events affecting the prognosis of the patients were analyzed by logistic regression. Results: The total effective rate of rehabilitation in the observation group was higher than that in the control group (80.77% vs. 58.33%, P<0.05). After 6 months of rehabilitation, the improvement of cardiac function and pulmonary function in the observation group was better than that in the control group (P<0.05). In addition, the exercise endurance, quality of life and health status in the observation group were better than those in the control group (P<0.05). After six months of follow-up, it was found that the incidence of adverse cardiovascular events in the observation group was lower than that in the control group (P<0.05). Unconditional classification logistic regression analysis showed that diabetes, left ventricular ejection fraction (%) ≤50, left main artery disease, and type C disease are risk factors for adverse cardiovascular events after OPCAB in patients with severe CHD (P<0.05). Conclusion: After OPCAB treatment for severe CHD, graded cardiac rehabilitation care can improve nursing efficacy, promote the recovery of cardiopulmonary function, improve exercise endurance, quality of life and health status, and reduce the incidence of adverse cardiovascular events in patients. Diabetes, left ventricular ejection fraction, left main artery disease, and type C disease were independent risk factors for adverse cardiovascular events.
Keywords: Severe coronary heart disease, grading of cardiac rehabilitation, OPCAB, quality of life, cardiac function, lung function
Introduction
Health Care Commission reported in 2021 that cardiovascular disease caused many deaths in China, with an increase in patients with severe coronary heart disease (CHD) due to advanced age, comorbidities, organ function etc. [1]. With the development of medical technology, the prognosis of CHD treatment has improved significantly, and the mortality has declined. However, the average age of onset of CHD is becoming younger, with a sharp increase in incidence and an increased survival rate, which has led to a loss of family and social labor force as well as economic pressures [2]. Therefore, helping patients return to normal life and work as well as improve their quality of life is currently a topic of concern in clinical practice [3]. For the treatment of CHD, surgery is mainly used to correct the abnormal cardiac structure to restore cardiac function, but in fact, it is difficult to achieve the expected purpose of restoring cardiac function only by correcting the abnormal cardiac structure, and systematic postoperative cardiac rehabilitation care is particularly important [4].
Off-pump coronary artery bypass grafting (OPCAB) is an effective treatment for severe CAH, while cardiac rehabilitation is a secondary strategy to improve the cardiac function, exercise tolerance and quality of life of the patients [5]. A clinical multicenter study reported a great need for cardiac rehabilitation related to inpatients with CHD [6]. Studies have reported that early cardiac rehabilitation interventions can reduce the incidence of postoperative acute myocardial infarction and arrhythmias in patients with CAH [7]. In recent years, there have been more cardiac rehabilitation programs for postoperative CHD, but they did not grade the interventions for patients with different levels of risk, and there is a lack of uniform standards for the content and processes of cardiac rehabilitation care.
Here, we designed a protocol to investigate the impact of graded cardiac rehabilitation care on the clinical efficacy and quality of life in patients with severe CHD after OPCAB, and to verify the effectiveness and safety of this care program. Our innovation is to verify the effectiveness and safety of graded cardiac rehabilitation care for patients with severe CHD after OPCAB through real clinical data. This could provide a theoretical basis for the promotion of this nursing method in clinical practice.
Materials and methods
General data
Data of 100 patients with severe CHD who underwent OPCAB treatment from February 2020 to August 2021 in Tongji Hospital, Tongji Medical College, Huazhong University of Science and Technology were collected retrospectively. Based on the nursing methods, the patients were divided into an observation group (n = 52) and a control group (n = 48).
This study was approved by the Ethics Committee of Tongji Hospital, Tongji Medical College, Huazhong University of Science and Technology.
Inclusion criteria: (1) patients who met the diagnostic criteria for severe CHD [8]; (2) patients whose diagnosis was confirmed by imaging techniques; (3) patients who underwent OPCAB treatment and with stable vital signs after surgery; (4) patients with NYHA classification III-IV by the New York Heart Association [9].
Exclusion criteria: (1) patients with a history of mental consciousness disorder, organ failure or cancer; (2) patients with a history of cerebral infarction or cerebral hemorrhage; (3) patients who underwent emergency surgery or repeat cardiac surgery; (4) patients with severe heart failure or arrhythmia; (5) patients with drug or alcohol addiction; (6) patients with pectoris who showed unstable angina pectoris within the most recent month.
Methods
Conventional cardiac rehabilitation care was used in the control group. Firstly, patients were briefly introduced to the environment, including explanation of the help buttons in the ward and were given health education on the disease and OPCAB treatment upon admission to reduce patients’ fear of unknown treatment options. Secondly, when the patient’s vital signs were stable after OPCAB treatment, passive exercises for the shoulders, elbows and knees were performed, and supplemented with additional rehabilitation such as assisted indoor walking, corridor side walking, aerobic exercise and so on as the condition improved.
The observation group received graded cardiac rehabilitation care:
(1) Firstly, A special group for graded cardiac rehabilitation was established. The group consisted of two doctors, one head nurse and three nurses from the coronary intensive care unit. The nurses also provided health education on postural management, dietary guidance and discharge guidance.
(2) The cardiac rehabilitation grading assessment criteria were as follows. According to the American Association for Cardiopulmonary Rehabilitation Guidelines for Cardiac Rehabilitation, 6th Edition [10], the grading indices of rehabilitation risk were evaluated, grade I risk: 6-minute walking distance (6MWT) [11] <150 m, blood SpO2 90%-91%, in walking HRmax = 220 × 80% - age, increase in systolic blood pressure >40 mmHg; grade II risk: 6MWT <150-450 m, blood SpO2 92%-94%, HRmax = 220 × 70% - age, increase in systolic blood pressure 10-20 mmHg during walking; grade III risk: 6MWT >450 m, blood SpO2≥95%, during walking HRmax = 220 × 60% - age, increase of 5-10 mmHg in systolic blood pressure.
(3) The specific graded cardiac rehabilitation care measures were as follows: ① Grade I risk patients: patients without compression activity or bleeding risk could freely change position in bed, prone or semi-prone, and conduct early activities including nursing assisted passive or active extremity joint activity, sitting-in-bed passive or active powerless bicycle, and breathing control or prone breathing exercises. Patients were instructed to control water intake according to the cardiac function status. In terms of living skills, the patients performed their washing in bed and ate meals on their own. ② Grade II risk patients did the same as grade I risk patients based on the content listed above, with additional early activities, such as bedside sitting and standing training 1 h per day, active joint activities, active power bicycle in bed in a sitting position, lower limb strength training, breathing exercises in standing position to improve lung function rehabilitation. The diet for patients was still low salt and low fat. ③ Grade III risk patients did the same as grade I and II risk patients, with additional bedside or ward walking training (50 m each time, 3 times a day, then gradually increasing to 200-500 m walking activity), active joint activity, lower limb strength training, respiratory exercises and standing Baduanjin for pulmonary rehabilitation. Patients were physically allowed to complete their own washing or toileting.
All subjects were required to cooperate in monitoring cardiac changes during the whole rehabilitation process and to be prepared for first aid to avoid accidents. Immediate suspension of rehabilitation was required if the patient has the following conditions: ① Chest tightness, shortness of breath, chest pain; ② Dizziness, blackness, poor standing stability; ③ Pale and sweating profusely; ④ Heart rate and pulse exceeded the normal range by 15%; ⑤ Serious arrhythmia.
Observation indicators
Clinical efficacy was assess after 6 months of rehabilitation according to the relevant standards from JSC guidelines [12]. Significantly effective: ST-T rebounded over 0.15 mV, and T-wave inversion changed by more than 50%, >450 m; effective: ST-T segment showed significant rebound, 6MWT <150-450 m; ineffective: ST-T segment showed no significant change, 6MWT <150 m.
Cardiac and pulmonary functions were evaluated using cardiac ultrasound before and after 6 months of rehabilitation. The peak power (PP) and left ventricular ejection fraction (LVEF) were recorded. The force spirometry (FVC) and force expiratory volume in 1 second (FEV1) were measured, and FEV1/FVC values were calculated.
Exercise endurance: A 6MWT test was performed before and 6 months after rehabilitation, and the distance during the test was recorded. Patients were then assessed with the aid of a professional for exercise respiratory exchange rate >1.05, and anaerobic valve (AT) and maximal oxygen uptake (VO2) were recorded.
Quality of life was assessed using the Minnesota living with heart failure questionnaire (MLHFQ) [13] before and after 6 months of rehabilitation. The questionnaire included four dimensions: disease symptoms, physical limitation, family relationships and psycho-emotional state, each of which was scored out of 21 points, with a total score of 84 points.
Health status was evaluated using the MOS 36-item short form health survey (SF-36) [14] before and after 6 months of rehabilitation. Five dimensions (physical function, social function, physiological function, mental health and overall health) were selected for the evaluation, with a single score of 0-100 points. The score is directly proportional to the quality of life.
Adverse cardiovascular events such as malignant arrhythmia, myocardial infarction, heart failure and cardiogenic death that occurred within 6 months of rehabilitation were recorded.
To analyzed the risk factors of adverse prognosis, patients with cardiovascular events were divided into a poor prognosis group, and patients without cardiovascular events were divided into a good prognosis group. Clinical data of patients were collected from electronic medical records of patients, including age, sex, duration of CHD, length of hospital stay, smoking, drinking, diabetes, hypertension, hyperlipidemia, LVEF, NYHA classification (III/IV), left main artery disease, type C disease and so on. The above data were uniformly registered in SPSS 21.0 software, and those with statistically significant differences were further analyzed by unconditional binary logistic regression.
Statistical methods
SPSS 21.0 was applied to perform data calculation. Count data were described using the frequency (n/%), and chi-square test was performed when comparing the count data between groups. Measurement data were showed using mean ± SEM, and the independent sample t-test was carried out to compare the values between groups. For comparison within the same group before and after treatment, the paired t-test was performed. Logistics regression was used to analyze the risk factors of poor prognosis. When P<0.05, the difference was statistically significant.
Results
Comparison of the general data
As shown in Table 1, there was no difference in the sex, age, duration of CAH, the length of hospitalization, and NYHA classification between two groups (P>0.05).
Table 1.
Comparison of general information
| Group | Male/Female (cases) | Age (years) | Duration of coronary heart disease (years) | Length of hospitalization (d) | NYHA classification (III/IV) |
|---|---|---|---|---|---|
| Observation group (n = 52) | 31/21 | 67.56±4.58 | 8.38±2.43 | 18.73±2.29 | 28/24 |
| Control group (n = 48) | 30/18 | 66.90±6.14 | 8.50±2.05 | 19.15±2.24 | 25/23 |
| χ2/t | 0.087 | 0.612 | 0.266 | 0.926 | 0.552 |
| P | 0.768 | 0.542 | 0.791 | 0.357 | 0.759 |
Comparison of clinical efficacy
The number of patients with significantly effective, effective and ineffective responses in the observation group was 11, 31 and 10, respectively. The number of patients with significantly effective, effective and ineffective responses in the control group was 3, 25 and 20, respectively. The observation group showed a better total effective rate of rehabilitation than the control group (80.77% vs. 58.33%, P<0.05). See Table 2.
Table 2.
Comparison of clinical efficacy
| Group | Significantly effective | Effective | Ineffective | Total effective rate |
|---|---|---|---|---|
| Observation group (n = 52) | 11 (21.15) | 31 (59.62) | 10 (19.23) | 42 (80.77) |
| Control group (n = 48) | 3 (6.25) | 25 (52.08) | 20 (41.67) | 28 (58.33) |
| χ2 | - | 5.983 | ||
| P | - | 0.014 | ||
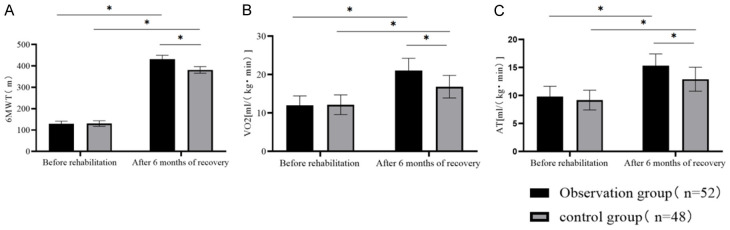
Comparison of cardiac function and pulmonary function
After 6 months of rehabilitation, LVEF, PP, FVC and FEV1/FVC in both groups were improved (P<0.05), but the improvements were more significant in the observation group than in the control group (P<0.05). See Figure 1.
Figure 1.
Comparison of cardiac and pulmonary functions (Note: *P<0.05). A. Left ventricular ejection fraction (LVEF); B. Peak power (PP); C. Force spirometry (FVC); D. Force expiratory volume in 1 second/force spirometry (FEV1/FVC).
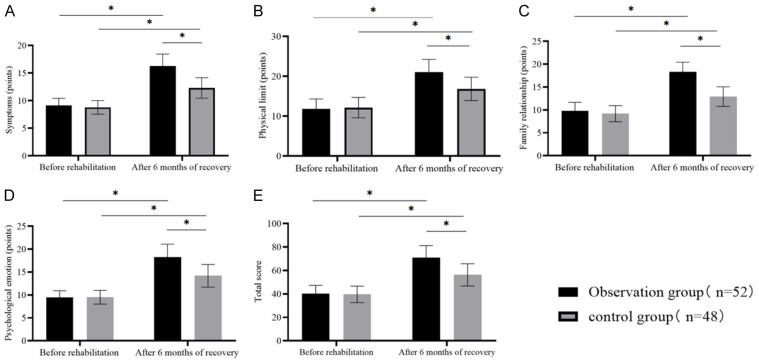
Comparison of exercise endurance
After 6 months of rehabilitation, 6MWT, peak value of VO2 and AT in both groups increased compared with those before rehabilitation (P<0.05), and the increases were more obvious in the observation group than in the control group (P<0.05), Figure 2.
Figure 2.
Comparison of exercise endurance (Note: *P<0.05). A. 6-minute walking distance (6MWT); B. Maximal oxygen uptake (VO2); C. Anaerobic valve (AT).
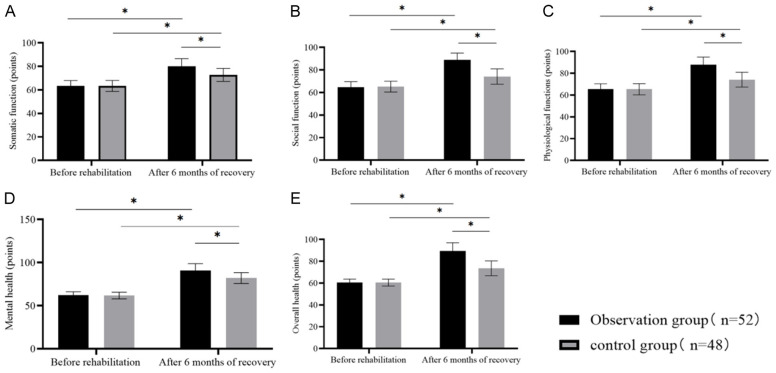
Comparison of patients’ quality of life
Before rehabilitation, the scores of quality of life in the two groups were similar (P>0.05). After 6 months of rehabilitation, the score of quality of life was obviously higher in the observation group than in the control group (P<0.05). See Figure 3.
Figure 3.
Comparison of quality of life (Note: *P<0.05). A. Disease symptoms; B. Physical limitation; C. Family relationships; D. Psycho-emotion; E. Total score.
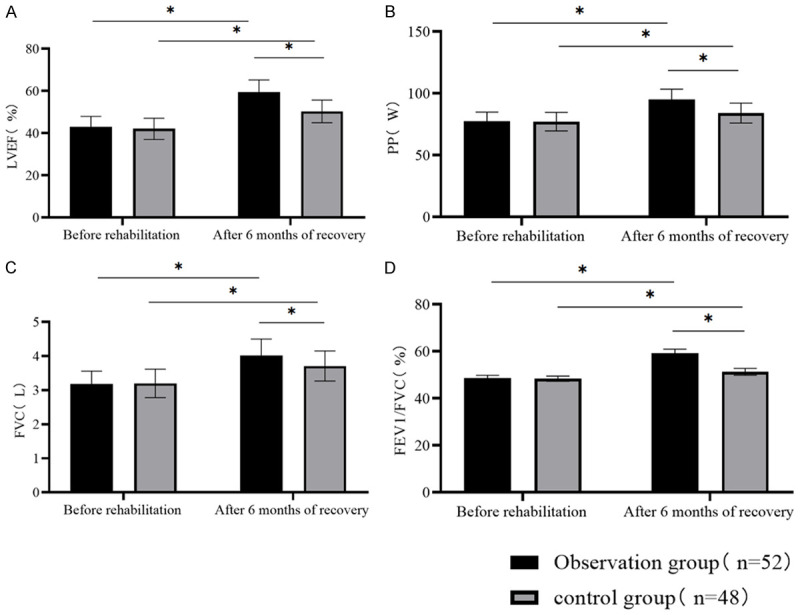
Comparison of patients’ health status
Before rehabilitation, the scores of physical function, social function, physiological function, mental health and overall health in the two groups were similar (P>0.05). After 6 months of rehabilitation, the scores of all the above 5 dimensions were improved in both groups (P<0.05), and these scores were better in the observation group (P<0.05). See Figure 4.
Figure 4.
Comparison of health status (Note: *P<0.05). A. Physical function; B. Social function; C. Physiological function; D. Mental health; E. Overall health.
Comparison of cardiovascular adverse events
After 6-month follow-up, it was found that the incidence of adverse cardiovascular events in the observation group was lower than that in the control group (17.31% vs. 41.67%, P<0.05), as shown in Table 3.
Table 3.
Comparison of cardiovascular adverse events
| Group | Arrhythmia | Myocardial infarction | Heart failure | Apoplexy | Revascularization | Total incidence |
|---|---|---|---|---|---|---|
| Observation group (n = 52) | 1 (1.92) | 2 (3.85) | 1 (1.92) | 2 (3.85) | 3 (5.77) | 9 (17.31) |
| Control group (n = 48) | 2 (2.08) | 3 (6.25) | 9 (18.75) | 3 (6.25) | 4 (8.33) | 20 (41.67) |
| χ2 | - | 7.193 | ||||
| P | - | 0.007 |
Univariate analysis of risk factors for adverse cardiovascular events
There were statistically significant differences between the two groups in diabetes, LVEF, left trunk disease and type C disease (P<0.05), while there was no statistically significant difference in other parameters (P>0.05), as shown in Table 4.
Table 4.
Univariate analysis of risk factors for adverse cardiovascular events
| Index | Poor prognosis group (n = 29) | Good prognosis group (n = 71) | χ2/t | P |
|---|---|---|---|---|
| Age/year | 68.42±5.82 | 67.39±5.49 | 0.837 | 0.202 |
| Male/female | 18/11 | 42/39 | 0.073 | 0.787 |
| Course of CHD (year) | 9.18±1.07 | 9.21±1.10 | 0.125 | 0.901 |
| Smoke | 15 (51.72) | 32 (45.07) | 0.366 | 0.545 |
| Drink | 17 (58.62) | 30 (42.25) | 2.214 | 0.137 |
| Diabetes | 19 (65.52) | 26 (36.62) | 6.947 | 0.008 |
| Hypertension | 11 (37.93) | 22 (30.99) | 0.449 | 0.503 |
| Hyperlipidemia | 15 (51.72) | 28 (39.44) | 1.268 | 0.260 |
| NYHA grade | 0.085 | 0.770 | ||
| III | 14 (48.28) | 32 (45.07) | ||
| IV | 15 (51.72) | 39 (54.93) | ||
| LVEF (%) | 7.615 | 0.006 | ||
| ≤50 | 23 (79.31) | 35 (49.30) | ||
| ≥51% | 6 (20.69) | 36 (50.70) | ||
| Left main trunk disease | 22 (75.86) | 34 (47.89) | 6.540 | 0.011 |
| Type C lesions | 21 (72.41) | 26 (36.62) | 5.654 | 0.017 |
| Postoperative medication | ||||
| Aspirin | 28 (96.55) | 71 (100.00) | 2.473 | 0.116 |
| Clopidogrel | 27 (93.10) | 70 (98.59) | 2.131 | 0.144 |
| Statins | 26 (89.66) | 69 (97.18) | 3.456 | 0.117 |
| ACEI/ARB | 24 (82.76) | 65 (82.79) | 1.625 | 0.202 |
Note: coronary heart disease (CHD); left ventricular ejection fraction (LVEF); angiotensin converting enzyme inhibitor (ACEI); angiotensin receptor blockers (ARB).
Multivariate analysis of risk factors for adverse cardiovascular events
With the occurrence of adverse cardiovascular events as the dependent variable (occurrence of adverse cardiovascular events = 1, absence of adverse cardiovascular events = 0), and with diabetes (none = 0, presence = 1), LVEF (%) (≥51 = 1, ≤50 = 0), left main artery disease (none = 0, presence = 1), and type C disease (none = 0, presence = 1) as the independent variables, we conducted unconditional classification logistic regression analysis. The results showed that diabetes (OR = 1.260, 95% CI: 1.069-1.485), LVEF (%) ≤50 (OR = 1.379, 95% CI: 1.209-1.920), left trunk disease (OR = 1.523, 95% CI: 1.209-1.920), and type C disease (OR = 1.528, 95% CI: 1.301-1.794) were independent risk factors (P<0.05) that affected the occurrence of adverse cardiovascular events in patients with severe CHD after OPCAB. See Table 5.
Table 5.
Multivariate analysis of risk factors for adverse cardiovascular events
| Factor | β | SE | Wald χ2 | P | OR | 95% CI |
|---|---|---|---|---|---|---|
| Diabetes | 0.231 | 0.084 | 7.563 | 0.006 | 1.260 | 1.069-1.485 |
| LVEF (%) ≤50 | 0.321 | 0.102 | 9.904 | 0.002 | 1.379 | 1.129-1.684 |
| Left main trunk disease | 0.421 | 0.118 | 12.729 | 0.000 | 1.523 | 1.209-1.920 |
| Type C lesions | 0.424 | 0.082 | 26.736 | 0.000 | 1.528 | 1.301-1.794 |
Discussion
The focus of clinical attention in regard to CHD is not only on treatment and resuscitation in the acute phase, but also on post-treatment rehabilitation, because patients are prone to recurrence and readmission [15]. Cardiac rehabilitation can improve the condition of patients with CAH and reduce mortality from myocardial infarction. Therefore, when implementing cardiac rehabilitation care for patients with severe CAH, it is important to carry out rehabilitation risk assessment and classification, so as to improve the effectiveness and safety of cardiac rehabilitation.
Studies have reported that prolonged adherence with exercise training can reduce cardiovascular disease recurrence, prolong survival time and improve cardiac function, and also, exercise relaxation can regulate the negative mindset of patients when facing disease [16,17]. However, exercise can increase myocardial oxygen consumption, reduce coronary perfusion, and increase arrhythmias, as well as cardiac arrest and myocardial infarction in patients with CAH [18]. Oldridge et al. [19] reported that a risk stratification assessment should be performed for cardiac rehabilitation in patients with CAH to inform the development of specific clinical cardiac rehabilitation components. Therefore, when implementing cardiac rehabilitation care, the patient’s risk should be monitored and dynamically assessed throughout the whole process, and care measures need to be implemented in a graded manner. The present results found that the observation group had a higher total effective rate of rehabilitation (80.77% vs. 58.33%), and better LVEF, PP, FVC, FEV1/FVC, 6MWT, peak VO2 and AT. It is suggested that graded cardiac rehabilitation care can improve patients’ clinical symptoms, cardiopulmonary function and exercise tolerance. FVC and FEV1/FVC were used as predictors to assess cardiopulmonary function, and their improvement suggests that patients’ comprehensive cardiopulmonary function will slowly recover [20,21]. 6MWT is a preferred method to assess exercise endurance, and peak VO2 and AT, as predictors of patients’ aerobic capacity, are positively correlated with exercise endurance [22]. Cardiac rehabilitation graded care was graded as I, II and III according to the patient’s conditions, with each grade matched to the appropriate exercise modality, time and intensity. The progressively increasing intensity allows the patient’s cardiopulmonary function and cardiorespiratory reserve capacity to slowly improve. The mechanism of action may be that with increased cardiopulmonary function, stagnant blood flow in the body is relieved, and the oxygen uptake capacity of skeletal muscle is improved, creating a good peripheral effect and also further increasing exercise endurance.
The current study also revealed that the observation group performed better in quality of life and the incidence of cardiovascular adverse events (5.77% vs. 20.83%). The follow-up within 6 months after rehabilitation showed that the incidence of adverse cardiovascular events in the observation group was lower than that in the control group (17.31% vs. 41.67%, P<0.05). These results indicated that graded cardiac rehabilitation care can improve patients’ quality of life, reduce the incidence of adverse cardiovascular events and improve prognosis. It has been clinically reported that some patients with severe CAH are less susceptible to increased incidence of adverse postoperative cardiovascular events due to timely consultation, timely relief of clinical symptoms and good self-perceived recovery after surgery [23]. However, some patients with severe CAH may experience negative emotions and excessive restriction of activities postoperatively due to the impact of adverse cardiovascular events, which require nursing-assisted rehabilitation guidance [24]. In this study, cardiac rehabilitation was graded according to the patient’s post-OPCAB status, and appropriate rehabilitation protocols were used according to levels I, II and III risk to improve patient’s perception of their conditions as well as improve compliance [25]. Therefore, the implementation of graded cardiac rehabilitation care is more advantageous than traditional cardiac rehabilitation. Firstly, exercise rehabilitation remains the core component, but it is supplemented with daily activity and self-care training to meet the rules and characteristics of cardiac rehabilitation, which increases self-participation and helps build confidence in overcoming the disease, thereby improving the quality of life. Secondly, the graded cardiac rehabilitation care can adjust the care content according to the patient’s individual conditions and provide a reference for standardizing the steps of cardiac rehabilitation care for CHD.
This study also analyzed the risk factors of adverse cardiovascular events after OPCAB. The results showed that diabetes, LVEF (%) ≤50, left main artery disease, and type C disease were independent risk factors. (1) Diabetes: A study found that about 80% of diabetes patients died due to cardiovascular events [26]. Pathological and physiological changes such as abnormal glucose and lipid metabolism, proliferation and migration of smooth muscle cells, imbalance of the fibrinolytic system and platelet aggregation in diabetes patients increase the progression of atherosclerosis and the risk of cardiovascular and cerebrovascular adverse events. Similar studies also found that diabetes is associated with CHD and stroke [27]. (2) LVEF: Many studies have found that LVEF is closely related to the myocardial systolic function of patients. The decrease of ejection fraction indicates that the myocardial systolic function of patients is impaired, and the myocardial oxygen uptake is increased, thus adverse cardiovascular events occur [28]. (3) Left main coronary artery disease and type C disease: Generally, the incidence of left main coronary artery disease is low, but it is serious once it occurs. The effect of drug or interventional surgery is not ideal, and the incidence of adverse cardiovascular events after OPCAB treatment is high [29]. Coronary artery disease type C is an independent risk factor for inducing adverse cardiovascular events after intervention [30]. The results of this study also found that the adverse cardiovascular events in patients with severe CHD after surgery and nursing rehabilitation were closely related to the degree of disease.
Conclusions
In conclusion, graded cardiac rehabilitation care was clinically effective in improving patients’ cardiopulmonary function, exercise endurance and quality of life as well as benefiting their prognosis. However, this study is a single-center small-sample study, so the findings still need to be further verified by follow-up multi-center and larger-sample studies.
Disclosure of conflict of interest
None.
References
- 1.Li P, Chen J, Ke Z, Han J, Shen L, Zhou N. Comparison of antiangina therapies in patients with coronary heart disease in China: study protocol for a multicentre, retrospective, hospital system-based study. BMJ Open. 2021;11:e036954. doi: 10.1136/bmjopen-2020-036954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Akyuz A. Exercise and coronary heart disease. Adv Exp Med Biol. 2020;1228:169–179. doi: 10.1007/978-981-15-1792-1_11. [DOI] [PubMed] [Google Scholar]
- 3.Remmele J, Pringsheim M, Nagdyman N, Oberhoffer-Fritz R, Ewert P. Cognitive function in adults with Fontan palliation versus acyanotic CHD patients and association with health-related quality of life. Cardiol Young. 2022:1–6. doi: 10.1017/S1047951122003390. [DOI] [PubMed] [Google Scholar]
- 4.Luo WY, Ni P, Chen L, Pan QQ, Zhang H, Zhang YQ. Development of the ICF-CY set for cardiac rehabilitation after pediatric congenital heart surgery. Front Pediatr. 2022;10:790431. doi: 10.3389/fped.2022.790431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sheikhy A, Fallahzadeh A, Sadeghian S, Forouzannia K, Bagheri J, Salehi-Omran A, Tajdini M, Jalali A, Pashang M, Hosseini K. Mid-term outcomes of off-pump versus on-pump coronary artery bypass graft surgery; statistical challenges in comparison. BMC Cardiovasc Disord. 2021;21:412. doi: 10.1186/s12872-021-02213-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Pogosova N, Saner H, Pedersen SS, Cupples ME, Mc Gee H, Hofer S, Doyle F, Schmid J VON Kanel On Behalf Of The Cardiac Rehabilitation Section Of The European Association Of Cardiovascular Prevention And Rehabilitation Of The European Society Of Cardiology R. Psychosocial aspects in cardiac rehabilitation: from theory to practice. A position paper from the Cardiac Rehabilitation Section of the European Association of Cardiovascular Prevention and Rehabilitation of the European Society of Cardiology. Kardiologiia. 2015;55:96–108. doi: 10.18565/cardio.2015.10.96-108. [DOI] [PubMed] [Google Scholar]
- 7.Callaghan S, Morrison ML, McKeown PP, Tennyson C, Sands AJ, McCrossan B, Grant B, Craig BG, Casey FA. Exercise prescription improves exercise tolerance in young children with CHD: a randomised clinical trial. Open Heart. 2021;8:e001599. doi: 10.1136/openhrt-2021-001599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Fihn SD, Gardin JM, Abrams J, Berra K, Blankenship JC, Dallas AP, Douglas PS, Foody JM, Gerber TC, Hinderliter AL, King SB 3rd, Kligfield PD, Krumholz HM, Kwong RY, Lim MJ, Linderbaum JA, Mack MJ, Munger MA, Prager RL, Sabik JF, Shaw LJ, Sikkema JD, Smith CR Jr, Smith SC Jr, Spertus JA, Williams SV, Anderson JL American College of Cardiology Foundation/American Heart Association Task Force. 2012 ACCF/AHA/ACP/AATS/PCNA/SCAI/STS guideline for the diagnosis and management of patients with stable ischemic heart disease: a report of the American College of Cardiology Foundation/American Heart Association task force on practice guidelines, and the American College of Physicians, American Association for Thoracic Surgery, Preventive Cardiovascular Nurses Association, Society for Cardiovascular Angiography and Interventions, and Society of Thoracic Surgeons. Circulation. 2012;126:e354–471. doi: 10.1161/CIR.0b013e318277d6a0. [DOI] [PubMed] [Google Scholar]
- 9.Greene SJ, Butler J, Spertus JA, Hellkamp AS, Vaduganathan M, DeVore AD, Albert NM, Duffy CI, Patterson JH, Thomas L, Williams FB, Hernandez AF, Fonarow GC. Comparison of New York Heart Association class and patient-reported outcomes for heart failure with reduced ejection fraction. JAMA Cardiol. 2021;6:522–531. doi: 10.1001/jamacardio.2021.0372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Aziz K, Lee CHC, Escobedo MB, Hoover AV, Kamath-Rayne BD, Kapadia VS, Magid DJ, Niermeyer S, Schmölzer GM, Szyld E, Weiner GM, Wyckoff MH, Yamada NK, Zaichkin J. Part 5: neonatal resuscitation 2020 American Heart Association guidelines for cardiopulmonary resuscitation and emergency cardiovascular care. Pediatrics. 2021;147(Suppl 1):e2020038505E. doi: 10.1542/peds.2020-038505E. [DOI] [PubMed] [Google Scholar]
- 11.Agarwala P, Salzman SH. Six-minute walk test: clinical role, technique, coding, and reimbursement. Chest. 2020;157:603–611. doi: 10.1016/j.chest.2019.10.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.JCS Joint Working Group. Guidelines for rehabilitation in patients with cardiovascular disease (JCS 2012) Circ J. 2014;78:2022–2093. doi: 10.1253/circj.cj-66-0094. [DOI] [PubMed] [Google Scholar]
- 13.Mogle J, Buck H, Zambroski C, Alvaro R, Vellone E. Cross-validation of the minnesota living with heart failure questionnaire. J Nurs Scholarsh. 2017;49:513–520. doi: 10.1111/jnu.12318. [DOI] [PubMed] [Google Scholar]
- 14.Li ZC, Hou YF, Zhou ZW, Jiang L, Zhang S, Lin JH. Patient factors influencing preoperative expectations of patients undergoing total knee arthroplasty. Beijing Da Xue Xue Bao Yi Xue Ban. 2022;54:170–176. doi: 10.19723/j.issn.1671-167X.2022.01.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ramachandran HJ, Jiang Y, Tam WWS, Yeo TJ, Wang W. Effectiveness of home-based cardiac telerehabilitation as an alternative to phase 2 cardiac rehabilitation of coronary heart disease: a systematic review and meta-analysis. Eur J Prev Cardiol. 2022;29:1017–1043. doi: 10.1093/eurjpc/zwab106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Liu T, Chan AWK, Chair SY. Group- plus home-based Tai Chi program improves functional health among patients with coronary heart disease: a randomized controlled trial. Eur J Cardiovasc Nurs. 2022;21:597–611. doi: 10.1093/eurjcn/zvab126. [DOI] [PubMed] [Google Scholar]
- 17.Zhang X, Zheng Y, Geng C, Guan J, Wang L, Zhang X, Cheng Y, Li J, Lu X. Isometric exercise promotes arteriogenesis in rats after myocardial infarction. J Biomed Res. 2021;35:436–447. doi: 10.7555/JBR.35.20210062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Noack F, Schwaab B, Voeller H, Eckrich K, Guha M, Bongarth C, Heinze V, Schlitt A. The current LDL-C target < 1.4 mmol/l of the ESC is achieved in less than 16% of patients with coronary heart disease despite effective lipid-lowering therapy: data from the LLT-R registry. Eur Heart J. 2020:41. [Google Scholar]
- 19.Oldridge N, Taylor RS. Cost-effectiveness of exercise therapy in patients with coronary heart disease, chronic heart failure and associated risk factors: a systematic review of economic evaluations of randomized clinical trials. Eur J Prev Cardiol. 2020;27:1045–1055. doi: 10.1177/2047487319881839. [DOI] [PubMed] [Google Scholar]
- 20.Cheng YJ, Chen ZG, Li ZY, Mei WY, Bi WT, Luo DL. Longitudinal change in lung function and subsequent risks of cardiovascular events: evidence from four prospective cohort studies. BMC Med. 2021;19:153. doi: 10.1186/s12916-021-02023-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Masood IR, Detterich J, Cerrone D, Lewinter K, Shah P, Kato R, Sabati A. Reduced forced vital capacity and the number of chest wall surgeries are associated with decreased exercise capacity in children with congenital heart disease. Pediatr Cardiol. 2022;43:54–61. doi: 10.1007/s00246-021-02692-0. [DOI] [PubMed] [Google Scholar]
- 22.Ritti-Dias RM, Sant’anna FDS, Braghieri HA, Wolosker N, Puech-Leao P, Lanza FC, Cucato GG, Dal Corso S, Correia MA. Expanding the use of six-minute walking test in patients with intermittent claudication. Ann Vasc Surg. 2021;70:258–262. doi: 10.1016/j.avsg.2020.07.047. [DOI] [PubMed] [Google Scholar]
- 23.Li XX, Fan ZJ, Cui J, Lin Q, Zhuang R, Liu RP, Wu Y. Cardiac rehabilitation of Baduanjin exercise in coronary heart disease after PCI: a protocol for systematic review and meta-analysis of randomized controlled trials. Medicine (Baltimore) 2021;100:e25501. doi: 10.1097/MD.0000000000025501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hohls JK, Beer K, Arolt V, Haverkamp W, Kuhlmann SL, Martus P, Waltenberger J, Rieckmann N, Müller-Nordhorn J, Ströhle A. Association between heart-focused anxiety, depressive symptoms, health behaviors and healthcare utilization in patients with coronary heart disease. J Psychosom Res. 2020;131:109958. doi: 10.1016/j.jpsychores.2020.109958. [DOI] [PubMed] [Google Scholar]
- 25.Anderson L, Thompson DR, Oldridge N, Zwisler AD, Rees K, Martin N, Taylor RS. Exercise-based cardiac rehabilitation for coronary heart disease. Cochrane Database Syst Rev. 2016;2016:CD001800. doi: 10.1002/14651858.CD001800.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kristensen SL, Rørth R, Jhund PS, Docherty KF, Sattar N, Preiss D, Køber L, Petrie MC, McMurray JJV. Cardiovascular, mortality, and kidney outcomes with GLP-1 receptor agonists in patients with type 2 diabetes: a systematic review and meta-analysis of cardiovascular outcome trials. Lancet Diabetes Endocrinol. 2019;7:776–785. doi: 10.1016/S2213-8587(19)30249-9. [DOI] [PubMed] [Google Scholar]
- 27.Sattar N, Lee MMY, Kristensen SL, Branch KRH, Del Prato S, Khurmi NS, Lam CSP, Lopes RD, McMurray JJV, Pratley RE, Rosenstock J, Gerstein HC. Cardiovascular, mortality, and kidney outcomes with GLP-1 receptor agonists in patients with type 2 diabetes: a systematic review and meta-analysis of randomised trials. Lancet Diabetes Endocrinol. 2021;9:653–662. doi: 10.1016/S2213-8587(21)00203-5. [DOI] [PubMed] [Google Scholar]
- 28.Heitner SB, Jacoby D, Lester SJ, Owens A, Wang A, Zhang D, Lambing J, Lee J, Semigran M, Sehnert AJ. Mavacamten treatment for obstructive hypertrophic cardiomyopathy: a clinical trial. Ann Intern Med. 2019;170:741–748. doi: 10.7326/M18-3016. [DOI] [PubMed] [Google Scholar]
- 29.Yaroslavskaya EI, Kuznetsov VA, Gorbatenko EA, Marinskikh LV. Association of atrial fibrillation with coronary lesion in ischemic heart disease patients. Kardiologiia. 2019;59:5–12. doi: 10.18087/cardio.2019.9.2641. [DOI] [PubMed] [Google Scholar]
- 30.Wang J, Xu HB, Zhang HP, Chen JL, Qiao SB, Hu FH, Yang WX, Yuan JS, Liu R, Cui JG, Guo C, Duan X, Gao LJ. Impact of type 2 diabetes mellitus on the progression and revascularization of coronary non-target lesions in patients with coronary heart disease. Zhonghua Xin Xue Guan Bing Za Zhi. 2020;48:393–400. doi: 10.3760/cma.j.cn112148-20190425-00204. [DOI] [PubMed] [Google Scholar]