Key Points
Question
Is change in body size associated with increased mortality risk among healthy older adults?
Findings
In this cohort study of 16 523 community-dwelling healthy participants, 1256 died over a mean (SD) of 4.4 (1.7) years of follow-up. Among men, loss of 5% to 10% of body weight and loss of more than 10% of body weight were associated with a 33% and 289% increase in mortality, respectively; among women, loss of 5% to 10% of body weight and loss of more than 10% of body weight were associated with a 26% and 114% increase in mortality, respectively.
Meaning
This study suggests that weight loss was associated with an increase in mortality, particularly among men, highlighting the need to monitor and investigate weight loss in older adults.
Abstract
Importance
The association between weight change and subsequent cause-specific mortality among older adults is not well described. The significance of changes in waist circumference (WC) has also not been compared with weight change for this purpose.
Objective
To examine the associations of changes in body weight and WC with all-cause and cause-specific mortality.
Design, Setting, and Participants
This cohort study is a post hoc analysis of data from the Aspirin in Reducing Events in the Elderly (ASPREE) randomized clinical trial, which recruited participants between March 1, 2010, and December 31, 2014. The study included community-based older adults (16 703 Australian participants aged ≥70 years and 2411 US participants aged ≥65 years) without evident cardiovascular disease (CVD), dementia, physical disability, or life-limiting chronic illness. Data analysis was performed from April to September 2022.
Exposures
Body weight and WC were measured at baseline and at annual visit 2. Analysis models were adjusted for baseline body mass index because height and weight were measured at baseline, allowing for calculation of body mass index and other variables. Both body weight and WC changes were categorized as change within 5% (stable), decrease by 5% to 10%, decrease by more than 10%, increase by 5% to 10%, and increase by more than 10%.
Main Outcomes and Measures
All-cause, cancer-specific, CVD-specific, and noncancer non-CVD–specific mortality. Mortality events were adjudicated by an expert review panel. Cox proportional hazards regression and competing risk analyses were used to calculate hazard ratios (HRs) and 95% CIs.
Results
Among 16 523 participants (mean [SD] age, 75.0 [4.3] years; 9193 women [55.6%]), 1256 deaths were observed over a mean (SD) of 4.4 (1.7) years. Compared with men with stable weight, those with a 5% to 10% weight loss had a 33% higher (HR, 1.33; 95% CI, 1.07-1.66) risk of all-cause mortality, and those with more than a 10% decrease in body weight had a 289% higher (HR, 3.89; 95% CI, 2.93-5.18) risk. Compared with women with stable weight, those with a 5% to 10% weight loss had a 26% higher (HR, 1.26; 95% CI, 1.00-1.60) risk of all-cause mortality, and those with more than a 10% decrease in body weight had a 114% higher (HR, 2.14; 95% CI, 1.58-2.91) risk. Weight loss was associated with a higher cancer-specific mortality (>10% decrease among men: HR, 3.49; 95% CI, 2.26-5.40; 5%-10% decrease among women: HR, 1.44; 95% CI, 1.46-2.04; >10% decrease among women: HR, 2.78; 95% CI, 1.82-4.26), CVD-specific mortality (>10% decrease among men: HR, 3.14; 95% CI, 1.63-6.04; >10% decrease among women: HR, 1.92; 95% CI, 1.05-3.51), and noncancer non-CVD–specific mortality (>10% decrease among men: HR, 4.98; 95% CI, 3.14-7.91). A decrease in WC was also associated with mortality.
Conclusions and Relevance
This cohort study of healthy older adults suggests that weight loss was associated with an increase in all-cause and cause-specific mortality, including an increased risk of cancer, CVD, and other life-limiting conditions. Physicians should be aware of the significance of weight loss, especially among older men.
This cohort study uses data from the Aspirin in Reducing Events in the Elderly clinical trial to examine the associations of changes in body weight and waist circumference with all-cause and cause-specific mortality.
Introduction
As individuals age, many experience a slow but progressive decrease in weight.1 In contrast, weight gain in others may accompany the adoption of a more sedentary existence.2 Physicians generally monitor weight changes in their older patients and target their advice, focusing particularly on the management of an idealized healthy weight. However, to our knowledge, the clinical significance of weight change has not been well documented in a population of relatively healthy older individuals free of diagnosed life-limiting illnesses.
One recently published systematic review of 30 studies reported that in older adults, weight loss, weight gain, or weight fluctuation was associated with increased risk of all-cause mortality.3 However, the studies included in this review differed substantially, involving varying measures of body size (mostly self-reported) and variability in the rigor with which mortality events were assessed. Most of the studies included individuals with preexisting illness, such as cancer, dementia, and cardiovascular disease (CVD). Thus, the mortality risk associated with weight loss or weight gain among apparently healthy older men and women requires further study.
Waist circumference (WC) may be a better measure than body weight to estimate all-cause mortality, CVD mortality, and premature mortality because it captures the negative outcomes of abdominal adiposity,4 which may be associated with an enhanced release of inflammatory mediators.5 However, data on the relative significance of changes in weight, WC, and cause-specific mortality have not been established in an aging population, to our knowledge.
In the Aspirin in Reducing Events in the Elderly (ASPREE) randomized clinical trial,6 body size parameters (weight and WC) were measured annually for a large population of initially healthy individuals. We used this information to investigate the associations of percentage change in body weight and WC with the risk of all-cause and cause-specific mortality in this population.
Methods
Study Design and Setting
The ASPREE trial recruited 19 114 community-dwelling adults from Australia (n = 16 703; aged ≥70 years) and the United States (n = 2411; aged ≥65 years) from March 1, 2010, to December 31, 2014. The detailed methods of the ASPREE trial have been previously reported.6 Participants were randomly assigned to receive 100 mg of aspirin daily or matching placebo.6,7 Participants were excluded if they had prior documented CVD events, dementia, physical disability, or a chronic illness expected to limit survival to less than 5 years. Ethics approval was obtained from institutional ethics review committees in Australia (the Royal Australasian College of General Practitioners Ethics Committee, the Monash Human Research Ethics Committee, the Human Research Ethics Committee [Tasmanian] Network, the Goulburn Valley Health Ethics & Research Committee, and ACT Health Human Research Ethics Committee) and the US (individual clinic sites were responsible for obtaining institutional review board approval from their respective institutions prior to study initiation). Participants provided written informed consent. This study followed the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) reporting guideline.
Standard Assessments
After randomization, ASPREE trial participants were contacted quarterly by telephone and visited in person annually. At these annual visits, body weight, height at baseline, WC, and laboratory test measurements were recorded, and other health-related data were collected.6 Frailty was defined using the modified Fried frailty phenotype, as the presence of weakness, slowness, exhaustion, low physical activity, and a body mass index (BMI; calculated as weight in kilograms divided by height in meters squared) of less than 20 (included instead of weight loss).7 Any person with 1 or 2 of these criteria was categorized as prefrail, and those with 3 or more of these criteria were categorized as frail. Prespecified ASPREE end points (ie, cancer, clinically significant bleeding, dementia, depression, hospitalization for heart failure, myocardial infarction, and stroke) and hospitalizations were recorded at 6-month intervals by in-person interview or by a 6-month telephone call. All end point data were adjudicated by expert panels.6
Assessment of Change in Body Size
We calculated percentage change in body weight from the difference in weight over the first 2 years after randomization as (weight at annual visit 2 − baseline weight) / baseline weight, expressed as a percentage. Change in WC was measured in a similar manner. The values for change in body-size indices (weight and WC) were divided into 5 categories: change within 5% (stable), decrease by 5% to 10%, decrease by more than 10%, increase by 5% to 10%, and increase by more than 10%.
Assessment of Mortality
Mortality events were identified during routine follow-up by a review of health records when participants could not be contacted or when the next of kin or a close contact notified the trial center. In Australia, the trial staff performed weekly linkage with the Ryerson Index, a community-maintained register that monitors death notices and obituaries. The names of all Australian and US participants who had withdrawn or were lost to follow-up were linked to the National Death Index. Cause of death was established by an adjudication panel determining the single disease that was most likely to have initiated the trajectory toward death. Where relevant records could not be obtained, the underlying cause of death was based on International Statistical Classification of Diseases and Related Health Problems, Tenth Revision codes recorded on the death certificate or on the results of a search of the National Death Index. The present study analyzed change in body size between study entry and annual visit 2 and mortality that occurred after annual visit 2.
Statistical Analysis
Statistical analysis was performed from April to September 2022. The characteristics of the participants were compared for continuous variables using analysis of variance and for categorical variables using χ2 tests, according to the weight change categories and WC change categories.
Cox proportional hazards regression was used to calculate the hazard ratios (HRs) and 95% CIs for all-cause mortality, and competing risk was used for cause-specific mortality. Initially, we examined the 5 weight change categories with all-cause mortality and cause-specific mortality using stable weight (within 5% change) as the reference category. Thereafter, we examined the 5 categories of WC change with mortality in a similar manner. All analyses were repeated in the same way for the individual end points of all-cause mortality, cancer-specific mortality, CVD-specific mortality, and noncancer non-CVD–specific mortality. Various analytical models were adjusted for 1 or more of the following characteristics: age, baseline BMI, baseline WC, frailty status, country of birth, smoking status, alcohol intake, educational level, hypertension, chronic kidney disease (estimated glomerular filtration rate, <60 mL/min/1.73 m2), diabetes, and interim hospitalization status.
There was a significant interaction between change in body size categories and sex that persisted in the fully adjusted models. There was no similar interaction between change in body size and age; analyses were therefore stratified by sex.
Sensitivity analyses were performed excluding the US population (predominantly comprising the US racial and ethnic minority population), excluding participants with a cognitive impairment at baseline,8 and restricting the analysis of outcomes to those occurring after annual visit 3 (to reduce the association with outcomes of illness progressing during years 1 and 2). Additional stratified analyses were performed based on baseline obesity status (nonobese BMI vs obese BMI), age category (<75 years vs ≥75 years), and the occurrence of hospitalization between baseline and annual visit 2, to account for individuals whose weight loss might have occurred during recovery after a hospitalization for an acute illness. Statistical significance was defined as a 2-sided P < .05. Stata MP, version 17 (StataCorp LLC), was used for analysis.
Results
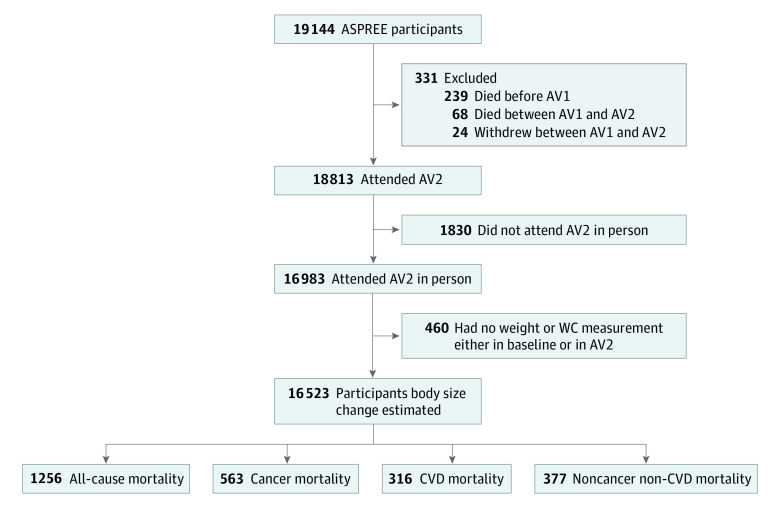
Of the 19 114 participants, 16 523 (mean [SD] age, 75.0 [4.3] years; 9193 women [55.6%] and 7330 men [44.4%]) had both weight and WC measured at baseline and annual visit 2, allowing for estimation of percentage change in body size (Figure 1). Among these participants, 1256 mortality events were recorded. The participants were followed up for a mean (SD) of 4.4 (1.7) years.
Figure 1. Percent Body Mass Index Changes and Mortality Ascertainment Timeline Among the Aspirin in Reducing Events in the Elderly (ASPREE) Trial Participants.
AV indicates annual visit; CVD, cardiovascular disease; and WC, waist circumference.
Characteristic of Participants
The body weight of 12 370 participants (74.9%) remained within 5% (stable) during the first 2 years (baseline to annual visit 2), 1299 (7.9%) had a 5% to 10% increase in weight, and 314 (1.9%) had an increase of more than 10%. Conversely, 1953 participants (11.8%) had a 5% to 10% decrease in weight, and 587 (3.6%) had a decrease of more than 10% (Table 1). Those who had a decrease in weight were mainly women, from the US, and prefrail or frail.
Table 1. Baseline Characteristics of Aspirin in Reducing Events in the Elderly Trial Participants Who Remained Free of Mortality Through the Second Annual Visit.
| Characteristic | Participants, No. (%) | P value | |||||
|---|---|---|---|---|---|---|---|
| All | Within 5% weight change or stable weight | Increase in weight | Decrease in weight | ||||
| 5%-10% | >10% | 5%-10% | >10% | ||||
| No. (%) | 16 523 (100.0) | 12 370 (74.9) | 1299 (7.9) | 314 (1.9) | 1953 (11.8) | 587 (3.6) | NA |
| Age, mean (SD), y | 75.0 (4.3) | 75.0 (4.4) | 74.6 (4.1) | 74.7 (4.5) | 75.5 (4.8) | 75.6 (4.8) | <.001 |
| Sex | |||||||
| Male | 7330 (44.4) | 5750 (46.5) | 525 (40.4) | 107 (34.1) | 765 (39.2) | 183 (31.2) | <.001 |
| Female | 9193 (55.6) | 6620 (53.5) | 774 (59.6) | 207 (65.9) | 1188 (60.8) | 404 (68.8) | |
| Country | |||||||
| Australia | 14 632 (88.6) | 10 984 (88.8) | 1170 (90.1) | 277 (88.2) | 1711 (87.6) | 490 (83.5) | <.001 |
| US | 1891 (11.4) | 1386 (11.2) | 129 (9.9) | 37 (11.8) | 242 (12.4) | 97 (16.5) | |
| Low physical activity | 1139 (6.9) | 806 (6.5) | 88 (6.8) | 23 (7.3) | 167 (8.6) | 55 (9.4) | .002 |
| Weight, mean (SD), kg | 77.1 (14.8) | 77.2 (14.6) | 75.2 (14.5) | 71.8 (14.2) | 77.3 (15.2) | 80.1 (16.9) | <.001 |
| Waist circumference, mean (SD), cm | 97.1 (12.7) | 97.1 (12.5) | 96.4 (13.2) | 95.1 (13.0) | 97.5 (13.2) | 98.9 (14.4) | <.001 |
| Current or former smoking | 7276 (44.0) | 5387 (43.5) | 594 (45.7) | 151 (48.1) | 863 (44.2) | 281 (47.9) | .08 |
| Current alcohol use | 12 806 (77.5) | 9717 (78.6) | 992 (76.4) | 231 (73.6) | 1453 (74.4) | 413 (70.4) | <.001 |
| Educational level, y | |||||||
| <12 | 9371 (56.7) | 6980 (56.4) | 795 (61.2) | 194 (61.8) | 1083 (55.5) | 319 (54.3) | .002 |
| ≥12 | 7152 (43.3) | 5390 (43.6) | 504 (38.8) | 120 (38.2) | 870 (44.5) | 268 (45.7) | |
| Hypertension | 12 222 (74.0) | 9104 (73.6) | 956 (73.6) | 225 (71.7) | 1492 (76.4) | 445 (75.8) | .07 |
| Dyslipidemia | 10 789 (65.3) | 8040 (65.0) | 846 (65.1) | 207 (65.9) | 1321 (67.6) | 375 (63.9) | .21 |
| Chronic kidney disease | 2878/16 113 (17.9) | 2099/12 067 (17.4) | 214/1265 (16.9) | 59/305 (19.3) | 384/1905 (20.2) | 122/571 (21.4) | .005 |
| Diabetes | 1721 (10.4) | 1236 (10.0) | 135 (10.4) | 41 (13.1) | 245 (12.5) | 64 (10.9) | .006 |
| Prefrail or frail | 6503 (39.4) | 4708 (38.1) | 509 (39.2) | 145 (46.2) | 861 (44.1) | 280 (47.7) | <.001 |
| ≥1 Interim hospitalization | 3403 (20.6) | 2356 (19.0) | 276 (21.2) | 80 (25.5) | 476 (24.4) | 215 (36.6) | <.001 |
| Taking trial medication (100 mg of aspirin) | 8199 (49.6) | 6125 (49.5) | 651 (50.1) | 163 (51.9) | 961 (49.2) | 299 (50.9) | .85 |
| Outcomes | |||||||
| All-cause mortality | 1256 (7.6) | 850 (6.9) | 87 (6.7) | 30 (9.6) | 183 (9.4) | 106 (18.1) | <.001 |
| Cancer mortality | 563/15 830 (3.6) | 385/11 905 (3.2) | 39/1251 (3.1) | 11/295 (3.7) | 79/1849 (4.3) | 49/530 (9.2) | <.001 |
| Cardiovascular disease mortality | 316/15 583 (2.0) | 215/11 735 (1.8) | 25/1237 (2.0) | 6/290 (2.1) | 47/1817 (2.6) | 23/504 (4.6) | <.001 |
| Noncancer non-CVD mortality | 377/15 644 (2.4) | 250/11 770 (2.1) | 23/1235 (1.9) | 13/297 (4.4) | 57/1827 (3.1) | 34/515 (6.6) | <.001 |
Abbreviations: CVD, cardiovascular disease; NA, not applicable.
The characteristics of participants according to change in WC are shown in eTable 1 in Supplement 1. Of the included participants, 10 234 (61.9%) had a stable WC (within 5% change), 295 (12.7%) had a 5% to 10% increase, and 973 (5.9%) had an increase in their WC of more than 10%. Conversely, 2309 participants (14.0%) had a decrease of 5% to 10%, and 912 (5.5%) had a decrease of more than 10% in their WC. Those with a decrease of more than 10% in WC were mainly US participants, women, prefrail or frail, and those with impaired kidney function.
Change in Body Weight and Mortality
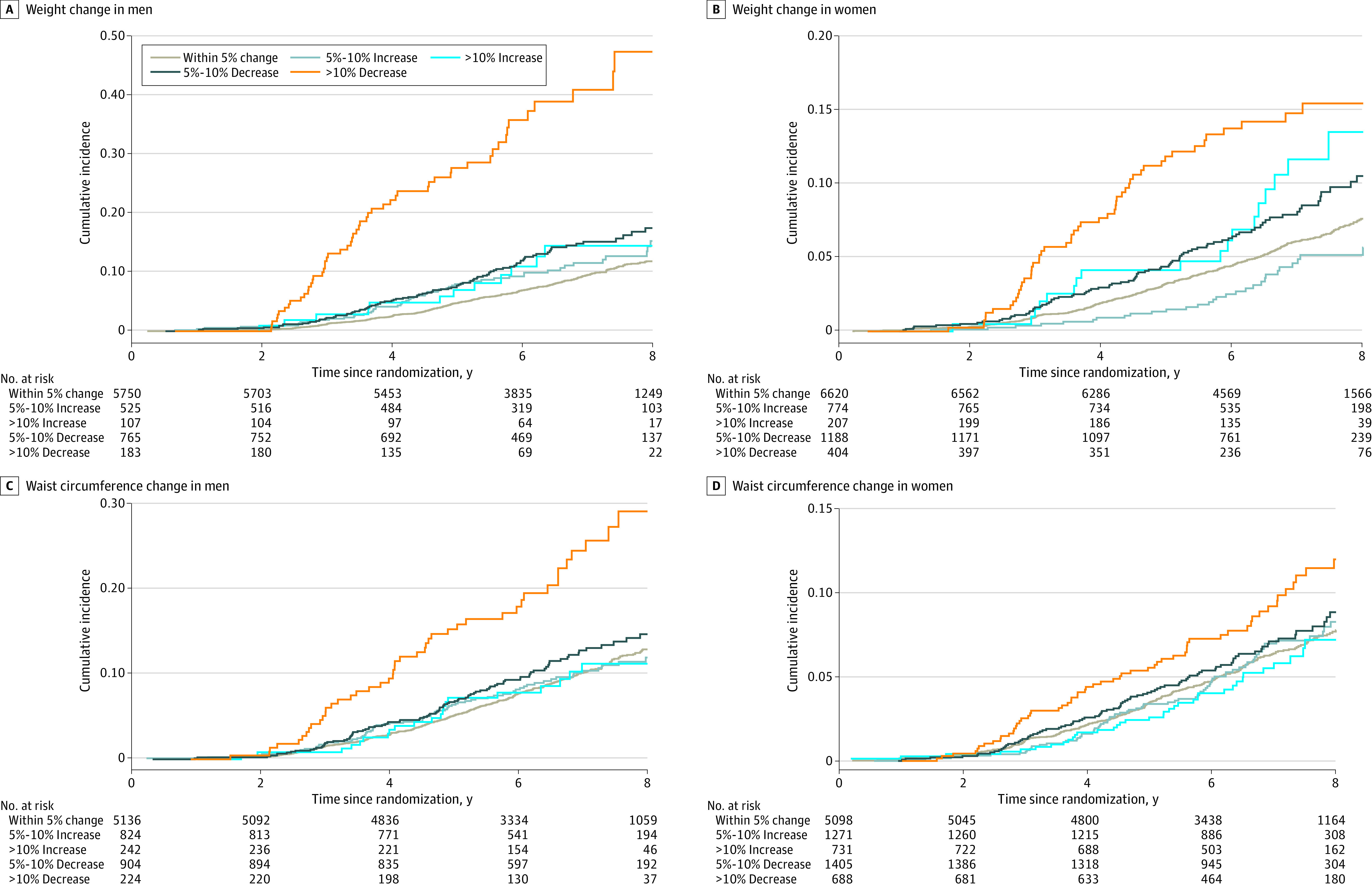
All-Cause Mortality
Table 2 shows the association between percentage change in BMI and subsequent all-cause and cause-specific mortality. The lowest risk of all-cause mortality was observed for the stable weight group (Figure 2). A total of 484 of mortality events were recorded among 5750 men with stable weight (8.4%), while 55 mortality events were recorded among 183 men with more than 10% weight loss (30.1%) (Table 2). Compared with men who had a stable weight (change within 5%), those who had a 5% to 10% decrease in weight had a 33% higher risk of all-cause mortality (HR, 1.33; 95% CI, 1.07-1.66), and those who had a more than 10% decrease in weight had a 289% higher (HR, 3.89; 95% CI, 2.93-5.18) risk. Hazard ratios were only modestly changed after adjustment for age, frailty status, country of birth, smoking status, alcohol intake, educational level, hypertension, chronic kidney disease, diabetes, and interim hospitalization. A decrease in weight was also associated with a higher mortality risk among women (5%-10% decrease: HR, 1.26; 95% CI, 1.00-1.60; >10% decrease: HR, 2.14; 95% CI, 1.58-2.91). A total of 366 mortality events were recorded among 6620 women with stable weight (5.5%), while 51 mortality events were recorded among 404 women with more than 10% weight loss (12.6%).
Table 2. Association Between Body Weight Change Categories and Risk of Mortality in Men and Womena.
| Type of mortality | Hazard ratio (95% CI) | ||||
|---|---|---|---|---|---|
| Within 5% of weight change or stable weight | Increase in weight | Decrease in weight | |||
| 5%-10% | >10% | 5%-10% | >10% | ||
| All-cause mortality | |||||
| Men | |||||
| Events, No./total No. (%) | 484/5750 (8.4) | 56/525 (10.7) | 12/107 (11.2) | 97/765 (12.7) | 55/183 (30.1) |
| Risk/10 000 person-years | 128 | 168 | 179 | 201 | 555 |
| Model 1 | 1 [Reference] | 1.44 (1.09-1.90) | 1.56 (0.88-2.75) | 1.42 (1.14-1.76) | 4.72 (3.56-6.23) |
| Model 2 | 1 [Reference] | 1.45 (1.10-1.92) | 1.59 (0.89-2.82) | 1.41 (1.13-1.75) | 4.68 (3.53-6.18) |
| Model 3 | 1 [Reference] | 1.46 (1.11-1.93) | 1.54 (0.87-2.72) | 1.38 (1.11-1.72) | 4.56 (3.44-6.03) |
| Model 4 | 1 [Reference] | 1.45 (1.09-1.91) | 1.37 (0.75-2.49) | 1.35 (1.08-1.68) | 4.23 (3.19-5.61) |
| Model 5 | 1 [Reference] | 1.45 (1.10-1.92) | 1.38 (0.76-2.52) | 1.33 (1.07-1.66) | 3.89 (2.93-5.18) |
| Women | |||||
| Events, No./total No. (%) | 366/6620 (5.5) | 31/774 (4.0) | 18/207 (8.7) | 86/1188 (7.2) | 51/404 (12.6) |
| Risk per 10 000 person-years | 83 | 60 | 137 | 112 | 204 |
| Model 1 | 1 [Reference] | 0.78 (0.54-1.13) | 1.67 (1.04-2.68) | 1.30 (1.03-1.65) | 2.46 (1.83-3.29) |
| Model 2 | 1 [Reference] | 0.79 (0.55-1.13) | 1.70 (1.06-2.73) | 1.29 (1.02-1.64) | 2.41 (1.80-3.24) |
| Model 3 | 1 [Reference] | 0.77 (0.53-1.11) | 1.61 (1.01-1.62) | 1.28 (1.01-1.63) | 2.37 (1.77-3.19) |
| Model 4 | 1 [Reference] | 0.75 (0.52-1.09) | 1.49 (0.91-2.42) | 1.27 (1.01-1.62) | 2.24 (1.66-3.03) |
| Model 5 | 1 [Reference] | 0.75 (0.52-1.09) | 1.47 (0.90-2.39) | 1.26 (1.00-1.60) | 2.14 (1.58-2.91) |
| Cancer mortality | |||||
| Men | |||||
| Events, No./total No. (%) | 227/5493 (4.1) | 25/494 (5.1) | 6/101 (5.9) | 39/707 (5.5) | 23/151 (15.2) |
| Risk per 10 000 person-years | 60 | 75 | 89 | 81 | 232 |
| Model 1 | 1 [Reference] | 1.35 (0.89-2.04) | 1.62 (0.72-3.67) | 1.26 (0.89-1.77) | 4.27 (2.78-6.56) |
| Model 2 | 1 [Reference] | 1.36 (0.91-2.07) | 1.75 (0.78-3.94) | 1.22 (0.87-1.72) | 4.07 (2.64-6.26) |
| Model 3 | 1 [Reference] | 1.36 (0.90-2.05) | 1.62 (0.72-3.64) | 1.24 (0.88-1.74) | 4.20 (2.73-6.45) |
| Model 4 | 1 [Reference] | 1.36 (0.90-2.06) | 1.58 (0.70-3.55) | 1.23 (0.87-1.73) | 3.91 (2.54-6.04) |
| Model 5 | 1 [Reference] | 1.37 (0.91-2.08) | 1.60 (0.71-3.60) | 1.20 (0.85-1.69) | 3.49 (2.26-5.40) |
| Women | |||||
| Events, No./total No. (%) | 158/6412 (2.5) | 14/757 (1.8) | 5/194 (2.6) | 40/1142 (3.5) | 26/379 (6.9) |
| Risk per 10 000 person-years | 36 | 27 | 38 | 53 | 104 |
| Model 1 | 1 [Reference] | 0.79 (0.45-1.36) | 1.07 (0.44-2.62) | 1.44 (1.02-2.03) | 2.97 (1.96-4.50) |
| Model 2 | 1 [Reference] | 0.79 (0.46-1.37) | 1.10 (0.45-2.68) | 1.42 (1.01-2.01) | 2.87 (1.89 to 4.36) |
| Model 3 | 1 [Reference] | 0.78 (0.45-1.35) | 1.06 (0.43-2.57) | 1.43 (1.01-2.02) | 2.93 (1.94-4.44) |
| Model 4 | 1 [Reference] | 0.79 (0.46-1.37) | 0.81 (0.30-2.18) | 1.46 (1.03-2.06) | 2.90 (1.90-4.44) |
| Model 5 | 1 [Reference] | 0.79 (0.46-1.36) | 0. 80 (0.30-2.15) | 1.44 (1.02-2.04) | 2.78 (1.82-4.26) |
| CVD mortality | |||||
| Men | |||||
| Events, No./total No. (%) | 115/5381 (2.1) | 15/484 (3.1) | 2/97 (2.1) | 25/693 (3.6) | 10/138 (7.2) |
| Risk per 10 000 person-years | 30 | 45 | 30 | 51 | 101 |
| Model 1 | 1 [Reference] | 1.67 (0.98-2.87) | 1.12 (0.28-4.52) | 1.49 (0.97-2.30) | 3.69 (1.93-7.04) |
| Model 2 | 1 [Reference] | 1.68 (0.98-2.88) | 1.14 (0.28-4.60) | 1.48 (0.96-2.28) | 3.64 (1.90-6.98) |
| Model 3 | 1 [Reference] | 1.70 (0.99-2.91) | 1.10 (0.27-4.47) | 1.45 (0.94-2.24) | 3.56 (1.86-6.80) |
| Model 4 | 1 [Reference] | 1.58 (0.90-2.75) | 1.10 (0.27-4.48) | 1.34 (0.86-2.10) | 3.30 (1.72-6.35) |
| Model 5 | 1 [Reference] | 1.58 (0.90-2.78) | 1.11 (0.27-4.32) | 1.38 (0.89-2.13) | 3.14 (1.63-6.04) |
| Women | |||||
| Events, No./total No. (%) | 100/6354 (1.6) | 10/753 (1.3) | 4/193 (2.1) | 22/1124 (2.0) | 13/366 (3.6) |
| Risk per 10 000 person-years | 23 | 19 | 30 | 29 | 52 |
| Model 1 | 1 [Reference] | 0.95 (0.50-1.82) | 1.37 (0.51-3.72) | 1.20 (0.76-1.91) | 2.25 (1.26-4.02) |
| Model 2 | 1 [Reference] | 0.97 (0.51-1.86) | 1.44 (0.53-3.91) | 1.18 (0.74-1.87) | 2.11 (1.18-3.77) |
| Model 3 | 1 [Reference] | 0.94 (0.49-1.79) | 1.33 (0.49-3.61) | 1.18 (0.75-1.88) | 2.19 (1.23- 3.90) |
| Model 4 | 1 [Reference] | 0.93 (0.48-1.78) | 1.32 (0.48-3.58) | 1.15 (0.72-1.84) | 2.01 (1.10-3.68) |
| Model 5 | 1 [Reference] | 0.93 (0.48-1.78) | 1.30 (0.48-3.54) | 1.14 (0.71-1.82) | 1.92 (1.05-3.51) |
| Noncancer non-CVD mortality | |||||
| Men | |||||
| Events, No./total No. (%) | 142/5408 (2.6) | 16/485 (3.3) | 4/99 (4.0) | 33/701 (4.7) | 22/150 (14.7) |
| Risk per 10 000 person-years | 38 | 48 | 59 | 69 | 222 |
| Model 1 | 1 [Reference] | 1.42 (0.85-2.38) | 1.78 (0.66-4.81) | 1.59 (1.09-2.33) | 6.21 (3.96-9.74) |
| Model 2 | 1 [Reference] | 1.41 (0.84-2.37) | 1.66 (0.61-4.51) | 1.64 (1.13-2.41) | 6.49 (4.13-10.21) |
| Model 3 | 1 [Reference] | 1.46 (0.87-2.44) | 1.75 (0.65-4.73) | 1.52 (1.04-2.23) | 5.83 (3.71-9.16) |
| Model 4 | 1 [Reference] | 1.48 (0.88-2.49) | 1.24 (0.39-3.89) | 1.53 (1.04-2.24) | 5.39 (3.41-8.52) |
| Model 5 | 1 [Reference] | 1.48 (0.88-2.50) | 1.25 (0.40-3.94) | 1.51 (1.03-2.21) | 4.98 (3.14-7.91) |
| Women | |||||
| Events, No./total No. (%) | 108/6362 (1.7) | 7/750 (0.9) | 9/198 (4.5) | 24/1126 (2.1) | 12/365 (3.3) |
| Risk per 10 000 person-years | 25 | 14 | 68 | 32 | 48 |
| Model 1 | 1 [Reference] | 0.62 (0.29-1.34) | 2.85 (1.44-5.62 | 1.21 (0.77-1.88) | 1.91 (1.05-3.46) |
| Model 2 | 1 [Reference] | 0.61 (0.28-1.31) | 2.74 (1.39-5.43) | 1.22 (0.78-1.89) | 1.98 (1.09-3.60) |
| Model 3 | 1 [Reference] | 0.60 (0.28-1.29) | 2.63 (1.34-5.20) | 1.17 (0.75-1.81) | 1.77 (0.98-3.22) |
| Model 4 | 1 [Reference] | 0.52 (0.23-1.19) | 2.60 (1.31-5.15) | 1.13 (0.72-1.78) | 1.56 (0.84-2.91) |
| Model 5 | 1 [Reference] | 0.52 (0.23-1.19) | 2.58 (1.30-5.11) | 1.12 (0.71-1.76) | 1.49 (0.80-2.79) |
Abbreviation: CVD, cardiovascular disease.
There was a significant interaction between the direction of the weight change and sex (P < .001); therefore, results are presented by sex. Models adjusted for age (model 1); model 1 plus baseline body mass index (model 2); model 1 plus frailty status (model 3); model 3 plus country of birth, smoking status, alcohol intake, educational level, hypertension, chronic kidney disease, and diabetes (model 4); and model 4 plus interim hospitalization (model 5).
Figure 2. Associations of Changes in Body Size and All-Cause Mortality in the Aspirin in Reducing Events in the Elderly Trial.
Cancer Mortality
In the fully adjusted analysis, a decrease of more than 10% in weight was associated with a 3.5-fold (HR, 3.49; 95% CI, 2.26-5.40) higher risk of cancer-specific mortality among men (Table 2). A decrease of 5% or more in weight was associated with cancer mortality among women (5%-10% decrease: HR, 1.44; 95% CI, 1.02-2.04; >10% decrease: HR, 2.78; 95% CI, 1.82-4.26). Increase in weight was not associated with cancer mortality.
CVD Mortality
A more than 10% decrease in weight was associated with higher CVD mortality for both men (HR, 3.14; 95% CI, 1.63-6.04) and women (HR, 1.92; 95% CI, 1.05-3.51) (Table 2). Increase in weight was not associated with CVD mortality.
Noncancer Non-CVD Mortality
A 10% or more decrease in weight was associated with a 5-fold higher risk of noncancer non-CVD mortality for men (HR, 4.98; 95% CI, 3.14-7.91) (Table 2). However, this association was not seen for women (HR, 1.49; 95% CI, 0.80-2.79).
Change in WC and Mortality
The associations of change in WC with all-cause and cause-specific mortality are presented in Table 3. A more than 10% decrease in WC was associated with 2.14-fold higher (HR, 2.14; 95% CI, 1.57-2.91) risk in all-cause mortality for men and a 34% higher (HR, 1.34; 95% CI, 1.02-1.78) risk in all-cause mortality for women. There was no association between a 5% to 10% decrease in WC or any increase in WC and all-cause mortality (Figure 2).
Table 3. Association Between WC Change Categories and Risk of Mortality in Men and Womena.
| Type of mortality | Hazard ratio (95% CI) | ||||
|---|---|---|---|---|---|
| Within 5% of WC change | Increase in WC | Decrease in WC | |||
| 5%-10% | >10% | 5%-10% | >10% | ||
| All-cause mortality | |||||
| Men | |||||
| Events, No./total No. (%) | 463/5136 (9.0) | 77/824 (9.3) | 21/242 (8.7) | 98/904 (10.8) | 45/224 (20.1) |
| Risk per 10 000 person-years | 139 | 142 | 135 | 168 | 324 |
| Model 1 | 1 [Reference] | 1.07 (0.85-1.36) | 0.96 (0.62-1.48) | 1.15 (0.93-1.44) | 2.24 (1.65-3.04) |
| Model 2 | 1 [Reference] | 1.12 (0.88-1.43) | 1.05 (0.67-1.62) | 1.14 (0.92-1.42) | 2.27 (1.67-3.09) |
| Model 3 | 1 [Reference] | 1.08 (0.85-1.38) | 0.94 (0.61-1.46) | 1.15 (0.92-1.43) | 2.15 (1.58-2.29) |
| Model 4 | 1 [Reference] | 1.10 (0.87-1. 40) | 0.90 (0.57-1.42) | 1.13 (0.90-1.40) | 2.18 (1.61-2.97) |
| Model 5 | 1 [Reference] | 1.11 (0.88-1.42) | 0.90 (0.57-1.42) | 1.10 (0.89-1.38) | 2.14 (1.57-2.91) |
| Women | |||||
| Events, No./total No. (%) | 286/5098 (5.6) | 77/1271 (6.1) | 37/731 (5.1) | 91/1405 (6.5) | 61/688 (8.9) |
| Risk per 10 000 person-years | 85 | 91 | 77 | 99 | 134 |
| Model 1 | 1 [Reference] | 1.06 (0.83-1.36) | 0.89 (0.64-1.26) | 1.13 (0.90-1.43) | 1.42 (1.07-1.87) |
| Model 2 | 1 [Reference] | 1.08 (0.84-1.39) | 0.96 (0.68-1.37) | 1.12 (0.88-1.42) | 1.37 (1.03-1.80) |
| Model 3 | 1 [Reference] | 1.07 (0.83-1.37) | 0.89 (0.63-1.25) | 1.14 (0.90-1.44) | 1.37 (1.04-1.81) |
| Model 4 | 1 [Reference] | 1.07 (0.83-1.39) | 0.88 (0.62-1.24) | 1.17 (0.93-1.49) | 1.35 (1.03-1.79) |
| Model 5 | 1 [Reference] | 1.07 (0.83-1.38) | 0.87 (0.62-1.24) | 1.16 (0.92-1.48) | 1.34 (1.02-1.78) |
| Cancer mortality | |||||
| Men | |||||
| Events, No./total No. (%) | 215/4888 (4.4) | 42/789 (5.3) | 9/230 (3.9) | 36/842 (4.3) | 18/197 (9.1) |
| Risk per 10 000 person-years | 65 | 77 | 58 | 61 | 130 |
| Model 1 | 1 [Reference] | 1.23 (0.88-1.71) | 0.89 (0.46-1.73) | 0.92 (0.65-1.31) | 1.98 (1.23-3.21) |
| Model 2 | 1 [Reference] | 1.33 (0.95-1.85) | 1.04 (0.53-2.03) | 0.90 (0.63-1.28) | 2.02 (1.25-3.27) |
| Model 3 | 1 [Reference] | 1.23 (0.89-1.72) | 0.88 (0.45-1.72) | 0.93 (0.64-1.31) | 1.94 (1.20-3.14) |
| Model 4 | 1 [Reference] | 1.24 (0.89-1.74) | 0.83 (0.41-1.67) | 0.90 (0.64-1.29) | 1.93 (1.20-3.13) |
| Model 5 | 1 [Reference] | 1.25 (0.89-1.75) | 0.82 (0.40-1.66) | 0.88 (0.62-1.26) | 1.87 (1.15-3.03) |
| Women | |||||
| Events, No./total No. (%) | 124/4936 (2.5) | 32/1226 (2.6) | 17/711 (2.4) | 44/1358 (3.2) | 26/653 (4.0) |
| Risk per 10 000 person-years | 37 | 38 | 35 | 48 | 57 |
| Model 1 | 1 [Reference] | 1.01 (0.69-1.50) | 0.95 (0.56-1.57) | 1.28 (0.91-1.80) | 1.44 (0.95-2.20) |
| Model 2 | 1 [Reference] | 1.05 (0.71-1.54) | 1.02 (0.61-1.69) | 1.26 (0.89-1.77) | 1.38 (0.90-2.11) |
| Model 3 | 1 [Reference] | 1.02 (0.69-1.50) | 0.94 (0.57-1.56) | 1.28 (0.91-1.81) | 1.42 (0.93-2.17) |
| Model 4 | 1 [Reference] | 1.05 (0.71-1.55) | 0.88 (0.51-1.49) | 1.33 (0.95-1.88) | 1.50 (0.98-2.29) |
| Model 5 | 1 [Reference] | 1.05 (0.71-1.54) | 0.88 (0.51-1.40) | 1.32 (0.94-1.87) | 1.49 (0.97-2.28) |
| CVD mortality | |||||
| Men | |||||
| Events, No./total No. (%) | 114/4787 (2.4) | 12/759 (1.6) | 6/227 (2.6) | 26/832 (3.1) | 9/188 (4.8) |
| Risk per 10 000 person-years | 34 | 22 | 39 | 45 | 65 |
| Model 1 | 1 [Reference] | 0.70 (0.38-1.25) | 1.10 (0.48-2.49) | 1.24 (0.81-1.90) | 1.77 (0.90-3.50) |
| Model 2 | 1 [Reference] | 0.72 (0.40-1.31) | 1.19 (0.52-2.73) | 1.23 (0.80-1.88) | 1.80 (0.91-3.56) |
| Model 3 | 1 [Reference] | 0.70 (0.40-1.27) | 1.08 (0.48-2.45) | 1.24 (0.81-1.89) | 1.71 (0.87-3.37) |
| Model 4 | 1 [Reference] | 0.71 (0.39-1.29) | 0.92 (0.38-2.25) | 1.20 (0.78-1.84) | 1.72 (0.87-3.35) |
| Model 5 | 1 [Reference] | 0.71 (0.39-1.28) | 0.92 (0.38-2.26) | 1.19 (0.77-1.82) | 1.71 (0.87-3.38) |
| Women | |||||
| Events, No./total No. (%) | 76/4888 (1.6) | 24/1218 (2.0) | 10/704 (1.4) | 23/1337 (1.7) | 16/643 (2.5) |
| Risk per 10 000 person-years | 23 | 28 | 21 | 25 | 35 |
| Model 1 | 1 [Reference] | 1.23 (0.78-1.95) | 0.91 (0.47-1.77) | 1.08 (0.67-1.72) | 1.36 (0.80-2.34) |
| Model 2 | 1 [Reference] | 1.29 (0.81-2.04) | 1.02 (0.52-1.99) | 1.05 (0.66-1.68) | 1.27 (0.73-2.18) |
| Model 3 | 1 [Reference] | 1.25 (0.79-1.97) | 0.91 (0.47-1.76) | 1.09 (0.68-1.73) | 1.33 (0.77-2.27) |
| Model 4 | 1 [Reference] | 1.32 (0.83-2.09) | 0.94 (0.49-1.82) | 1.15 (0.72-1.83) | 1.17 (0.66-2.08) |
| Model 5 | 1 [Reference] | 1.32 (0.82-2. 08) | 0.94 (0.49-1.82) | 1.13 (0.70-1.81) | 1.15 (0.65-2.05) |
| Noncancer non-CVD mortality | |||||
| Men | |||||
| Events, No./total No. (%) | 134/4807 (2.8) | 23/770 (3.0) | 6/227 (2.6) | 36/842 (4.3) | 18/197 (9.1) |
| Risk per 10 000 person-years | 40 | 42 | 39 | 62 | 130 |
| Model 1 | 1 [Reference] | 1.13 (0.73-1.76) | 0.94 (0.42-2.10) | 1.46 (1.01-2.10) | 3.03 (1.85-4.95) |
| Model 2 | 1 [Reference] | 1.12 (0.72-1.76) | 0.93 (0.41-2.14) | 1.46 (1.01-2.11) | 3.02 (1.84-4.94) |
| Model 3 | 1 [Reference] | 1.14 (0.74-1.78) | 0.92 (0.41-2.08) | 1.44 (1.00-2.09) | 2.83 (1.72-4.64) |
| Model 4 | 1 [Reference] | 1.20 (0.77-1.87) | 0.98 (0.43-2.22) | 1,42 (0.98-2.06) | 2.99 (1.82-4.91) |
| Model 5 | 1 [Reference] | 1.21 (0.77-1.89) | 0.98 (0.43-2.22) | 1.39 (0.96-2.02) | 2.93 (1.78-4.80) |
| Women | |||||
| Events, No./total No. (%) | 86/4898 (1.8) | 21/1215 (1.7) | 10/704 (1.4) | 24/1338 (1.8) | 19/646 (2.9) |
| Risk per 10 000 person-years | 26 | 25 | 20 | 26 | 42 |
| Model 1 | 1 [Reference] | 0.95 (0.59-1.53) | 0.81 (0.42-1.55) | 0.98 (0.63-1.54) | 1.44 (0.88-2.37) |
| Model 2 | 1 [Reference] | 0.95 (0.59-1.53) | 0.80 (0.41-1.56) | 0.99 (0.63-1.55) | 1.45 (0.88-2.39) |
| Model 3 | 1 [Reference] | 0.98 (0.61-1.57) | 0.80 (0.41-1.57) | 1.00 (0.64-1.57) | 1.35 (0.82-2.23) |
| Model 4 | 1 [Reference] | 0.90 (0.55-1.48) | 0.82 (0.42-1.57) | 0.99 (0.62-1.57) | 1.33 (0.81-2.20) |
| Model 5 | 1 [Reference] | 0.90 (0.54-1.48) | 0.82 (0.42-1.55) | 0.98 (0.62-1.55) | 1.32 (0.80-2.17) |
Abbreviations: CVD, cardiovascular; WC, waist circumference.
There was a significant interaction between the direction of the WC change and sex (P = .01); therefore, results are presented by sex. Models adjusted for age, (model 1); model 1 plus baseline WC (model 2); model 1 plus frailty status (model 3); model 3 plus country of birth, smoking status, alcohol intake, educational level, hypertension, chronic kidney disease, and diabetes (model 4); and model 4 plus interim hospitalization (model 5).
A more than 10% decrease in WC was associated with higher cancer mortality for men (HR, 1.87; 95% CI, 1.15-3.03) and women (HR, 1.49; 95% CI, 0.97-2.28) in fully adjusted analyses (Table 3). Change in WC was not associated with CVD mortality. A more than 10% decrease in WC was associated with higher noncancer non-CVD mortality among men (HR, 2.93; 95% CI, 1.78-4.80) only. Change in WC was not associated with noncancer non-CVD mortality among women.
Sensitivity Analyses
The associations persisted when we excluded participants from the US and participants who had any evidence of cognitive impairment at baseline and after restricting the analysis to outcomes occurring after annual visit 3 (eTables 2, 3, and 4 in Supplement 1). Similar associations of change in body weight with all-cause mortality and cause-specific mortality were observed among participants with or without obesity, as well as participants who were younger than 75 years at recruitment or those 75 years or older at recruitment (eTable 5 and eTable 6 in Supplement 1). The associations of change in BMI with all-cause and cause-specific mortality also remained similar when the analyses were stratified by interim hospitalization status (eTable 7 in Supplement 1). The associations of change in WC with all-cause mortality and cause-specific mortality remained similar to our main analyses in all the sensitivity analyses (eTables 8-13 in Supplement 1).
Discussion
The principal finding of this study was that a weight loss of more than 10% was associated with higher all-cause mortality (including increased mortality from cancer, CVD, and noncancer non-CVD) among both men and women. The association was more pronounced among men, for whom, in absolute terms, subsequent all-cause mortality was 8.4% among those maintaining consistent weight over a mean (SD) of 4.4 (1.7) years vs 30.1% among those for whom weight decreased by more than 10%; for women, the equivalent mortality rates were 5.5% and 12.6%. Lesser weight loss (between 5% and 10%) was associated with higher all-cause mortality for both sexes compared with stable weight, as well as a higher cancer mortality for women and a higher noncancer non-CVD mortality for men.
A decrease in WC was also associated with increased mortality. Weight gain, however, was not significantly associated with mortality, with the possible exception of noncancer non-CVD mortality for women. However, based on the small number of events in that category, this result should be interpreted cautiously.
Previous studies have reported an association between weight loss and subsequent mortality, but these studies included only a small number of older adults, typically with multiple comorbidities (eTable 14 in Supplement 1).3,9,10,11,12,13,14,15,16,17,18,19,20,21,22 Our study extends the previous observations by demonstrating a similar association among relatively healthy community-dwelling individuals aged 65 years or older. The results also showed that weight loss was more associated with mortality among men than women.
Two previous longitudinal studies examined the association of weight loss with CVD and cancer mortality and yielded conflicting results. The Enquête de Santé Psychologique-Risques, Incidence et Traitement (ESPRIT) study showed that weight loss was associated with higher CVD mortality but not cancer mortality.22 By contrast, the Guangzhou Biobank study showed that self-reported weight loss was associated with higher CVD mortality and cancer mortality.13 These studies differed from the present cohort by including participants with various chronic diseases and not adjusting for or excluding individuals with a recent hospitalization.13,22 Our study showed that weight loss was associated with all-cause mortality and an increase in all major causes of death, including cancer and CVD in an initially healthy population. In addition, our study showed that these results persisted even after adjustment for age, frailty status, baseline BMI, country of birth, smoking, hypertension, diabetes, and hospitalization in the previous 24 months. Adjustment for recent hospitalization is important because hospitalization is often followed by weight loss due to acute conditions.
Our study demonstrates that weight loss in older men and women is associated with an increased mortality risk irrespective of an individual’s baseline weight (ie, unanticipated weight loss even among adults with obesity is associated with increased mortality, regardless of other potential benefits of weight loss that are associated with quality of life and other morbidities). In addition, our study has clarified the lesser implications of weight gain. Compared with previous reports, the present study is based on individual measures of weight (rather than self-report) and adjudicated assessments of the cause of death. Without adjudication, deaths among older populations may be misclassified in up to 30% cases.23
The observation that weight loss was associated with mortality among men may be the result of the different body composition characteristics of men and women.24 For men, a higher proportion of body mass is constituted of muscle and bone mass, whereas for women, a higher proportion of body mass is composed of fat.24 If weight loss preceding chronic illness is predominantly loss of muscle mass and bone mass, it could explain the differences observed between men and women. Something similar might be at work to explain why weight loss, rather than decrease of WC, is more associated with mortality.
A likely explanation for these findings is that weight loss can be an early prodromal indicator of the presence of various life-shortening diseases.25,26 Although it is widely acknowledged that weight loss may precede a diagnosis of cancer, in our study, weight loss also preceded an increased mortality from CVD and other causes. The latter may include deaths from trauma, dementia, Parkinson disease, and other less common causes.27
In this age group, weight loss was largely associated with a reduction of appetite, leading to reduced food intake. Appetite is a complex process, governed by both the central nervous system and various circulating hormones. Several proposals have been put forward to explain why appetite might be suppressed in the early stages of chronic illness, ranging from increases in resistance to appetite-stimulating hormones,28 increased levels of inflammatory cytokines,29 and high levels of other mediators such as growth differentiation factor 15.30 Plasma concentrations of the latter are increased in chronic inflammatory disease, most subtypes of cancer, and cardiovascular and kidney disease, and several longitudinal studies have shown it to be independently associated with decreases in muscle mass and muscle strength.30
Strengths and Limitations
This study has some strengths. The combination of the large cohort, the focus on the population older than 70 years, and the extensive amount of hospitalization data, coupled with the regular and objective measures of body size and expert adjudication of cause of death, makes this the most comprehensive and detailed study of weight loss in this age group yet published, to our knowledge. It is coherent with but extends the findings of a meta-analysis whose component studies typically involved a broader range of ages, recall of prior weight, and/or reliance on death certificate data for cause of death.31
This study also has some limitations. The principal limitation is the inability to differentiate intended vs unintended weight loss, although bariatric surgery, the only likely intervention proven capable of intended long-term sustained weight loss,32 is rarely undertaken in this age group. Furthermore, exploring whether change in activity level and diet quality between baseline and annual visit 2 had any association with outcomes was not possible because they were not recorded in this study. Residual confounding, such as intended weight loss or change in activity or diet, cannot be excluded.
Conclusions
The clinical implication of the findings of this cohort study is that physicians should be aware of the significant association with mortality of even relatively minor weight loss (≥5%), especially among older men. The risk extends beyond an increased risk of cancer, extending to CVD and a range of other life-limiting conditions. Further research will be needed to determine more precisely the association between weight loss and the onset of fatal diseases and whether clinical or laboratory investigations can identify individuals for whom early intervention may be effective.
eTable 1. Characteristics of Aspirin in Reducing Events in the Elderly Trial Participants Overall, and by Waist Circumference (WC) Change Category From Recruitment Until Annual Visit 2
eTable 2. Association Between Weight Change Categories and Risk of Mortality (HR, 95% CI) Excluding the US Participants (6500 Men and 7704 Women)
eTable 3. Association Between Body Weight Change Categories and Risk of Mortality (HR, 95% CI) Excluding Those With Baseline Cognitive Impairment (7128 Men, 8984 Women)
eTable 4. Association Between Body Weight Change Categories and Risk of Mortality (HR, 95% CI) (Restricting the Analysis After AV3: 6161 Men, 7817 Women)
eTable 5. Association Between Body Weight Change Categories and Risk of Mortality (HR, 95% CI) Stratified by Obesity Status
eTable 6. Association Between Body Weight Change Categories and Risk of Mortality (HR, 95% CI) Stratified by Age at Recruitment
eTable 7. Association Between Body Weight Change Categories and Risk of Mortality (HR, 95% CI) Stratified by Interim Hospitalisation Status During Change in Body Size Measurement
eTable 8. Association Between Waist Circumference Change Categories and Risk of Mortality (HR, 95% CI) Excluding the US
eTable 9. Association Between Waist Circumference Change Categories and Risk of Mortality (HR, 95% CI) Excluding Those With Baseline Cognitive Impairment
eTable 10. Association Between Waist Circumference Change Categories and Risk of Mortality (HR, 95% CI) (Restricting the Analysis After AV3)
eTable 11. Association Between Waist Circumference Change Categories and Risk of Mortality (HR, 95% CI) Stratified by Obesity Status
eTable 12. Association Between Waist Circumference Change Categories and Risk of Mortality (HR, 95% CI) Stratified by Age at Recruitment
eTable 13. Association Between Waist Circumference Change Categories and Risk of Mortality (HR, 95% CI) Stratified by Interim Hospitalisation Status
eTable 14. Overview of Systematic Reviews and Cohort Studies Investigating the Association Between Weight Change in Kilogram, Body Mass Index, Waist Circumference and Mortality in Noninstitutionalized People
Data Sharing Statement
References
- 1.Vlassopoulos A, Combet E, Lean ME. Changing distributions of body size and adiposity with age. Int J Obes (Lond). 2014;38(6):857-864. doi: 10.1038/ijo.2013.216 [DOI] [PubMed] [Google Scholar]
- 2.Middelbeek L, Breda J. Obesity and sedentarism: reviewing the current situation within the WHO European region. Curr Obes Rep. 2013;2(1):42-49. doi: 10.1007/s13679-013-0054-y [DOI] [Google Scholar]
- 3.Alharbi TA, Paudel S, Gasevic D, Ryan J, Freak-Poli R, Owen AJ. The association of weight change and all-cause mortality in older adults: a systematic review and meta-analysis. Age Ageing. 2021;50(3):697-704. doi: 10.1093/ageing/afaa231 [DOI] [PubMed] [Google Scholar]
- 4.Ross R, Neeland IJ, Yamashita S, et al. Waist circumference as a vital sign in clinical practice: a consensus statement from the IAS and ICCR Working Group on Visceral Obesity. Nat Rev Endocrinol. 2020;16(3):177-189. doi: 10.1038/s41574-019-0310-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chait A, den Hartigh LJ. Adipose tissue distribution, inflammation and its metabolic consequences, including diabetes and cardiovascular disease. Front Cardiovasc Med. 2020;7:22. doi: 10.3389/fcvm.2020.00022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.ASPREE Investigator Group . Study design of ASPirin in Reducing Events in the Elderly (ASPREE): a randomized, controlled trial. Contemp Clin Trials. 2013;36(2):555-564. doi: 10.1016/j.cct.2013.09.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.McNeil JJ, Nelson MR, Woods RL, et al. ; ASPREE Investigator Group . Effect of aspirin on all-cause mortality in the healthy elderly. N Engl J Med. 2018;379(16):1519-1528. doi: 10.1056/NEJMoa1803955 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kronschnabl JM, Kneip T, Weiss LM, Bergmann M. Bodyweight change and cognitive performance in the older population. PLoS One. 2021;16(4):e0249651. doi: 10.1371/journal.pone.0249651 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Karahalios A, English DR, Simpson JA. Change in body size and mortality: a systematic review and meta-analysis. Int J Epidemiol. 2017;46(2):526-546. [DOI] [PubMed] [Google Scholar]
- 10.Okada C, Kubota Y, Eshak ES, Cui R, Tamakoshi A, Iso H; and the JACC Study Group . Weight change and mortality from cardiovascular diseases: the Japan Collaborative Cohort Study. J Atheroscler Thromb. 2021;28(1):25-33. doi: 10.5551/jat.54114 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Suh J, Cho YJ, Kim HJ, Choi SS. Age-related difference in weight change and all-cause mortality in middle-aged and older Korean populations: Korean Longitudinal Study of Aging. Korean J Fam Med. 2021;42(4):297-302. doi: 10.4082/kjfm.20.0170 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Son KY, Kwon H, Park JH, et al. Association between weight change over a period of 4 years and mortality in Korean older adults. Geriatr Gerontol Int. 2020;20(5):474-481. doi: 10.1111/ggi.13908 [DOI] [PubMed] [Google Scholar]
- 13.Huang YY, Jiang CQ, Xu L, et al. Adiposity change and mortality in middle-aged to older Chinese: an 8-year follow-up of the Guangzhou Biobank Cohort Study. BMJ Open. 2020;10(12):e039239. doi: 10.1136/bmjopen-2020-039239 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Nishida MM, Okura M, Ogita M, Aoyama T, Tsuboyama T, Arai H. Two-year weight loss but not body mass index predicts mortality and disability in an older Japanese community-dwelling population. J Am Med Dir Assoc. 2019;20(12):1654.e11-1654.e18. doi: 10.1016/j.jamda.2019.04.029 [DOI] [PubMed] [Google Scholar]
- 15.Chen C, Ye Y, Zhang Y, Pan XF, Pan A. Weight change across adulthood in relation to all cause and cause specific mortality: prospective cohort study. BMJ. 2019;367:l5584. doi: 10.1136/bmj.l5584 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Park SY, Wilkens LR, Maskarinec G, Haiman CA, Kolonel LN, Marchand LL. Weight change in older adults and mortality: the Multiethnic Cohort Study. Int J Obes (Lond). 2018;42(2):205-212. doi: 10.1038/ijo.2017.188 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mulligan AA, Lentjes MAH, Luben RN, Wareham NJ, Khaw KT. Weight change and 15 year mortality: results from the European Prospective Investigation into Cancer in Norfolk (EPIC-Norfolk) cohort study. Eur J Epidemiol. 2018;33(1):37-53. doi: 10.1007/s10654-017-0343-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Pan XF, Yuan JM, Koh WP, Pan A. Weight change in relation to mortality in middle-aged and elderly Chinese: the Singapore Chinese Health Study. Int J Obes (Lond). 2019;43(8):1590-1600 doi: 10.1038/s41366-018-0259-y [DOI] [PubMed] [Google Scholar]
- 19.Haugsgjerd TR, Dierkes J, Vollset SE, et al. ; Hordaland Health Study (HUSK) . Association between weight change and mortality in community living older people followed for up to 14 years. J Nutr Health Aging. 2017;21(8):909-917. doi: 10.1007/s12603-016-0866-z [DOI] [PubMed] [Google Scholar]
- 20.Beleigoli AM, Diniz MDFH, Boersma E, Silva JL, Lima-Costa MF, Ribeiro AL. The effects of weight and waist change on the risk of long-term mortality in older adults—the Bambuí (Brazil) Cohort Study of Aging. J Nutr Health Aging. 2017;21(8):861-866. doi: 10.1007/s12603-016-0858-z [DOI] [PubMed] [Google Scholar]
- 21.Alharbi TA, Ryan J, Freak-Poli R, et al. The association of weight loss, weight status, and abdominal obesity with all-cause mortality in older adults. Gerontology. 2022;68(12):1366-1374. doi: 10.1159/000522040 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Alharbi T, Ryan J, Freak-Poli R, et al. Objectively assessed weight change and all-cause mortality among community-dwelling older people. Nutrients. 2022;14(14):2983. doi: 10.3390/nu14142983 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Tan KS. Misclassification of the actual causes of death and its impact on analysis: a case study in non-small cell lung cancer. Lung Cancer. 2019;134:16-24. doi: 10.1016/j.lungcan.2019.05.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Srikanthan P, Horwich TB, Calfon Press M, Gornbein J, Watson KE. Sex differences in the association of body composition and cardiovascular mortality. J Am Heart Assoc. 2021;10(5):e017511. doi: 10.1161/JAHA.120.017511 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ekram ARMS, Woods RL, Britt C, Espinoza S, Ernst ME, Ryan J. The association between frailty and all-cause mortality in community-dwelling older individuals: an umbrella review. J Frailty Aging. 2021;10(4):320-326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Gaddey HL, Holder KK. Unintentional weight loss in older adults. Am Fam Physician. 2021;104(1):34-40. [PubMed] [Google Scholar]
- 27.Akushevich I, Kravchenko J, Yashkin AP, Yashin AI. Time trends in the prevalence of cancer and non-cancer diseases among older U.S. adults: Medicare-based analysis. Exp Gerontol. 2018;110:267-276. doi: 10.1016/j.exger.2018.06.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Johnson KO, Shannon OM, Matu J, Holliday A, Ispoglou T, Deighton K. Differences in circulating appetite-related hormone concentrations between younger and older adults: a systematic review and meta-analysis. Aging Clin Exp Res. 2020;32(7):1233-1244. doi: 10.1007/s40520-019-01292-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Chareh N, Kiesswetter E, Kob R, et al. Association between inflammation and appetite in healthy community-dwelling older adults—an enable study. Front Aging. 2022;3:826816. doi: 10.3389/fragi.2022.826816 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Alcazar J, Frandsen U, Prokhorova T, et al. Changes in systemic GDF15 across the adult lifespan and their impact on maximal muscle power: the Copenhagen Sarcopenia Study. J Cachexia Sarcopenia Muscle. 2021;12(6):1418-1427. doi: 10.1002/jcsm.12823 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.De Stefani FDC, Pietraroia PS, Fernandes-Silva MM, Faria-Neto J, Baena CP. Observational evidence for unintentional weight loss in all-cause mortality and major cardiovascular events: a systematic review and meta-analysis. Sci Rep. 2018;8(1):15447. doi: 10.1038/s41598-018-33563-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Maciejewski ML, Arterburn DE, Van Scoyoc L, et al. Bariatric surgery and long-term durability of weight loss. JAMA Surg. 2016;151(11):1046-1055. doi: 10.1001/jamasurg.2016.2317 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eTable 1. Characteristics of Aspirin in Reducing Events in the Elderly Trial Participants Overall, and by Waist Circumference (WC) Change Category From Recruitment Until Annual Visit 2
eTable 2. Association Between Weight Change Categories and Risk of Mortality (HR, 95% CI) Excluding the US Participants (6500 Men and 7704 Women)
eTable 3. Association Between Body Weight Change Categories and Risk of Mortality (HR, 95% CI) Excluding Those With Baseline Cognitive Impairment (7128 Men, 8984 Women)
eTable 4. Association Between Body Weight Change Categories and Risk of Mortality (HR, 95% CI) (Restricting the Analysis After AV3: 6161 Men, 7817 Women)
eTable 5. Association Between Body Weight Change Categories and Risk of Mortality (HR, 95% CI) Stratified by Obesity Status
eTable 6. Association Between Body Weight Change Categories and Risk of Mortality (HR, 95% CI) Stratified by Age at Recruitment
eTable 7. Association Between Body Weight Change Categories and Risk of Mortality (HR, 95% CI) Stratified by Interim Hospitalisation Status During Change in Body Size Measurement
eTable 8. Association Between Waist Circumference Change Categories and Risk of Mortality (HR, 95% CI) Excluding the US
eTable 9. Association Between Waist Circumference Change Categories and Risk of Mortality (HR, 95% CI) Excluding Those With Baseline Cognitive Impairment
eTable 10. Association Between Waist Circumference Change Categories and Risk of Mortality (HR, 95% CI) (Restricting the Analysis After AV3)
eTable 11. Association Between Waist Circumference Change Categories and Risk of Mortality (HR, 95% CI) Stratified by Obesity Status
eTable 12. Association Between Waist Circumference Change Categories and Risk of Mortality (HR, 95% CI) Stratified by Age at Recruitment
eTable 13. Association Between Waist Circumference Change Categories and Risk of Mortality (HR, 95% CI) Stratified by Interim Hospitalisation Status
eTable 14. Overview of Systematic Reviews and Cohort Studies Investigating the Association Between Weight Change in Kilogram, Body Mass Index, Waist Circumference and Mortality in Noninstitutionalized People
Data Sharing Statement