Key Points
Question
What are the long-term health effects of involuntary displacement of people experiencing homelessness who inject drugs in US cities?
Findings
This simulation modeling study of 23 US cities projects that involuntary displacement of people experiencing homelessness may yield substantial increases in morbidity and mortality over a 10-year period. Involuntary displacement is estimated to worsen overdose and hospitalizations, decrease initiations of medications for opioid use disorder, and contribute to deaths among people experiencing homelessness who inject drugs.
Meaning
Ceasing involuntary displacement of people experiencing homelessness may mitigate some health-related harms associated with homelessness.
Abstract
Importance
At least 500 000 people in the US experience homelessness nightly. More than 30% of people experiencing homelessness also have a substance use disorder. Involuntary displacement is a common practice in responding to unsheltered people experiencing homelessness. Understanding the health implications of displacement (eg, “sweeps,” “clearings,” “cleanups”) is important, especially as they relate to key substance use disorder outcomes.
Objective
To estimate the long-term health effects of involuntary displacement of people experiencing homelessness who inject drugs in 23 US cities.
Design, Setting, and Participants
A closed cohort microsimulation model that simulates the natural history of injection drug use and health outcomes among people experiencing homelessness who inject drugs in 23 US cities. The model was populated with city-level data from the Centers for Disease Control and Prevention’s National HIV Behavioral Surveillance system and published data to make representative cohorts of people experiencing homelessness who inject drugs in those cities.
Main Outcomes and Measures
Projected outcomes included overdose mortality, serious injection–related infections and mortality related to serious injection–related infections, hospitalizations, initiations of medications for opioid use disorder, and life-years lived over a 10-year period for 2 scenarios: “no displacement” and “continual involuntary displacement.” The population-attributable fraction of continual displacement to mortality was estimated among this population.
Results
Models estimated between 974 and 2175 additional overdose deaths per 10 000 people experiencing homelessness at 10 years in scenarios in which people experiencing homelessness who inject drugs were continually involuntarily displaced compared with no displacement. Between 611 and 1360 additional people experiencing homelessness who inject drugs per 10 000 people were estimated to be hospitalized with continual involuntary displacement, and there will be an estimated 3140 to 8812 fewer initiations of medications for opioid use disorder per 10 000 people. Continual involuntary displacement may contribute to between 15.6% and 24.4% of additional deaths among unsheltered people experiencing homelessness who inject drugs over a 10-year period.
Conclusion and Relevance
Involuntary displacement of people experiencing homelessness may substantially increase drug-related morbidity and mortality. These findings have implications for the practice of involuntary displacement, as well as policies such as access to housing and supportive services, that could mitigate these harms.
This modeling study examines the potential long-term health effects of involuntary displacement among unsheltered people experiencing homelessness who inject drugs in 23 US cities.
Introduction
More than 500 000 people in the US experience homelessness nightly.1 After decreasing between 2007 and 2016, estimates of homelessness have steadily increased since 2017.2 Approximately two-thirds of people who are chronically homeless3 are unsheltered (ie, lack physical shelter).2
Although local shelters attempt to provide refuge and resources to people experiencing homelessness, shelters alone are inadequate to meet the needs of the population. Although temporary emergency shelter is a vital component of the social safety net, it is not a sufficient substitute for safe and affordable long-term housing.
Across the US, involuntary displacement that forces people experiencing homelessness to regularly relocate from one temporary location to another is common. Involuntary displacement may be operationalized or labeled differently depending on the city. Sometimes referred to as “sweeps,” “clearings,” or “cleanups,” displacement is often done without connecting people to services or housing and without regard for past trauma.4 People experiencing homelessness are often forced to disperse away from services, resulting in loss of personal belongings, medications, identification cards, and social support.5 Involuntary displacement may disproportionately impact people experiencing homelessness who use nonprescribed drugs6 because it can affect access to sterile injection equipment, naloxone, and medications for opioid use disorder (MOUD).7,8 Decreased access to support services and life-saving medications may increase overdose risk and death.9 This modeling study aimed to better understand the potential long-term health effects of involuntary displacement among unsheltered people experiencing homelessness who inject drugs in 23 US cities.
Methods
Model Description
A closed cohort microsimulation model was developed, validated, and calibrated to simulate the heterogeneous natural histories of injection drug use among people experiencing homelessness in 23 US cities. We sought to estimate the effect of involuntary displacement on overdose and serious injection-related bacterial infections (SIRIs), including infective endocarditis and severe skin and soft tissue infections, which account for substantial burden of the health effects among this population (Figure 1).10
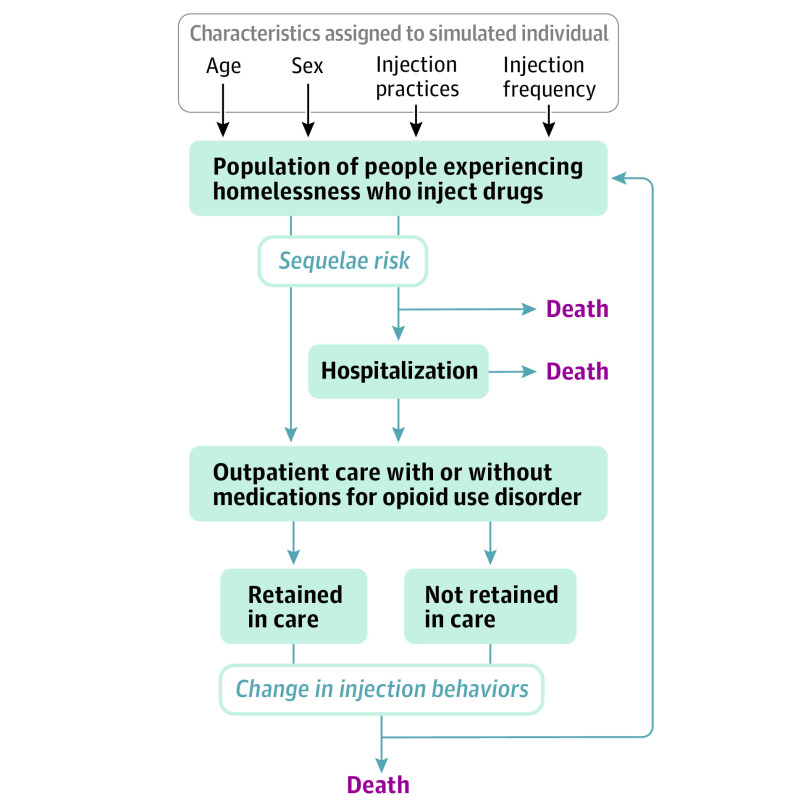
Figure 1. Model Schematic for Natural History of Injection Drug Use and Related Sequelae Among People Experiencing Homelessness.
Using the model parameters specified in the Table, a microsimulation of the heterogeneous natural history of injection drug use among people experiencing homelessness was used. The schematic demonstrates how individuals “move through” different modules in the model related to sequelae of injection drug use, health care access, behavioral changes, and mortality. A comprehensive model description is included in Supplement 1.
A simulated individual enters the model and is randomly assigned an age, sex, and history of injection drug use. Among those who have a history of any injection drug use, the model then assigns a current injection status and injection-related behaviors. Injection status and behaviors, in turn, govern risk of overdose and injection-related infections. Individuals progress on a weekly timestep through a series of modules in which they encounter probabilities of SIRI and overdose (referred to as sequelae), hospitalization, and outpatient care. An individual’s progression through these modules affects the transition probabilities among injection-related health states and the probability of death.
The model was used to simulate separate cohorts from 23 US cities because these cities participated in the 2018 cycle for the National HIV Behavioral Surveillance (NHBS), which focused on people who inject drugs (NHBS cities are listed in Supplement 1). NHBS is a comprehensive system for biobehavioral surveillance conducted since 2003 among populations with high a prevalence of HIV in annual rotating cycles. For each city, model cohorts were stratified by sex, age, and injection behavior profile (eTable 1 in Supplement 1). Only individuals with current injection drug use were at risk of sequelae. Probabilities of overdose, infective endocarditis, and severe skin and soft tissue infection risk were derived by age, sex, and injection behavior profile for each city. Individuals who developed sequelae had a probability of being hospitalized and treated. Individuals encountered probabilities of linking to outpatient care, which include MOUD with buprenorphine and methadone (eTable 2 in Supplement 1). Linkage to MOUD could happen after a hospitalization for sequelae or via a “background” mechanism. The background mechanism simulated the observation that some individuals link to outpatient addiction care spontaneously and without prior hospitalization.
In the model, individuals in each city faced a risk of death from sequelae as well as from age- and sex-related causes (ie, competing causes of death). The probability of overdose-associated mortality by age, sex, injection behavior profile (assuming intravenous opioid use), and probability of overdose was derived. Infective endocarditis and skin and soft tissue infection were both characterized as untreated, in treatment, or resolved, with mortality risk being lower when characterized as being in treatment or resolved. Probabilities of non–drug-related death from other causes by sex, age, and injection behavior profile were applied.
Model Parameterization and Calibration
A total of 23 separate cohorts were parameterized after calibration (see eTables 4-26 in Supplement 1 for city-specific calibration results); inputs were derived with city-level data wherever possible. Other inputs were derived from national estimates from primary data and published literature when city-specific data were not available. Parameter source types (eg, city-specific) are summarized in the Table, and eTable 27 in Supplement 1 includes a complete list of sources for each parameter for each city.
Table. Model Parameters, Data Type Used to Inform Parameters, and Sampling Distributions for Probabilistic Sensitivity Analyses.
| Parameters | Data typesa | PSA distributionb |
|---|---|---|
| Cohort characteristics among people experiencing homelessness who inject drugs | ||
| Background mortality | National homeless, US Census | |
| Infection prevalence based on injection frequency | National inject, primary national inject, US Census | |
| Injection frequency stratified by age | City | |
| Proportion male | City | |
| Male age (mean/SD) | City | Normal |
| Female age (mean/SD) | City | Normal |
| Minimum age (mean/SD) | US Census | Normal |
| Needle sharing prevalence | City | Uniform |
| Skin cleaning prevalence | City | Uniform |
| Sequelae of drug use parameters | ||
| Combined overdose prevalence (high) | National inject, national homeless, primary national homeless | Uniform |
| Combined overdose prevalence (low) | National injection, national homeless, primary national homeless | Uniform |
| Fatal overdose prevalence | National inject, national homeless | Uniform |
| IE prevalence | National inject | Uniform |
| Overdose history multipliers | National inject | Uniform |
| Infection history multiplier | National inject | Uniform |
| Mortality, untreated SSTI | National inject | Uniform |
| Mortality, inpatient SSTI | National inject | Uniform |
| Mortality, untreated IE | National inject | Uniform |
| Mortality, inpatient IE | National inject | Uniform |
| Mortality, inpatient overdose | National inject | Uniform |
| Inpatient parameters | ||
| Inpatient linkage (SSTI) | National inject | Uniform |
| Inpatient linkage (IE) | National inject | Uniform |
| Inpatient linkage (overdose) | National inject | Uniform |
| Discharge against medical advice | National inject | Uniform |
| Inpatient SSTI duration (mean/STD) | National inject | |
| Inpatient IE duration (mean/SD) | National inject | |
| Outpatient parameters | ||
| Linkage from inpatient to outpatient, with MOUD | National inject | Uniform |
| Background linkage to outpatient care | National inject | Uniform |
| MOUD acceptance | City, primary national homeless | Uniform |
| Unlinkage from care, with MOUD | National inject, national homeless | Uniform |
| Unlinkage from care, without MOUD | National inject, national homeless | Uniform |
| Transition probabilities | ||
| Injection frequency transition probabilities | National inject, national homeless, primary national inject | Uniform |
| Needle sharing transition probabilities | National inject, primary national homeless | Uniform |
Abbreviations: IE, infective endocarditis; MOUD, medications for opioid use disorder; SSTI, skin and soft tissue infection.
Data types were defined as follows: city, primary data from 2018 National HIV Behavioral Surveillance data on people who inject drugs and people experiencing homelessness in the last year from each of the 23 US cities being analyzed; national inject, data specific to people who inject drugs from published literature; national homeless, data specific to people experiencing homelessness from published literature; primary national inject, primary data from cohort studies, randomized clinical trials, and case-control studies about people who inject drugs processed to develop input parameters; primary national homeless, primary data from cohort studies, randomized clinical trials, case-control studies about people experiencing homelessness processed to develop input parameters; and US Census, primary data from US Census processed to develop input parameters.
Probabilistic sensitivity analysis (PSA) was performed to characterize parameter uncertainty and create credible intervals for outcome estimates. The model was programmed to utilize normal, uniform, and log-normal distributions for PSA. Parameters with empty cells in the PSA distribution column were not included in the probabilistic sensitivity analysis.
City-level data obtained from NHBS11 were used to inform the cohort characteristics. In this survey, people also provided their housing status (eg, homeless in the past 12 months) and cohorts were limited to those who reported homelessness. This meant that the entirety of the cohorts used to inform the model were people experiencing homelessness who had recent (past 12 months) injection drug use or a history of injection drug use. The individuals who reported that they had not injected drugs in the past 12 months were used to inform the “no current use” health state. Those who reported recent or active injection drug use were used to inform the “low frequency” and “high frequency” drug use health state cohorts. City-specific parameter estimates are included in eTable 27 in Supplement 1.
Both city- and national-level sources for overdose were used. We estimated the rates of fatal overdose from 2018 Centers for Disease Control and Prevention WONDER (Wide-ranging Online Data for Epidemiologic Research) data.12 A combination of nationally representative published literature and NHBS city-specific sources were used to estimate the risk of nonfatal overdose. We used published literature that was not city-specific for SIRI estimates.13,14,15,16
“Community linkage” was derived from estimates from McLaughlin et al17 and Krawczyk et al.18 Based on these previous findings, people experiencing homelessness are approximately 0.46 times as likely as housed individuals to be linked to a health care provider. An assumption was made that all clinicians could prescribe MOUD (buprenorphine), although access to MOUD in the US is likely more limited. As such, a weekly probability of 0.81% linking to a clinician was calculated. MOUD use in 2021 from NHBS city-level data was used to estimate the probability of acceptance conditional on linkage to care.
US age- and sex-adjusted mortality from the National Vital Statistics System19 was used (with overdose removed) to derive the competing risks mortality. The increased risk of death among people experiencing homelessness was accounted for by using age group–standardized mortality ratios from the study by Nicholas et al.20
The model was deterministically calibrated separately for each city to fit clinically relevant outcomes: percentage of deaths attributable to overdose, 1-year nonfatal overdose, life expectancy, and 6-month retention in MOUD treatment. Data from 2 US cities were used (Boston, MA, and Denver, CO) to develop the calibration target of 25% to 33% of deaths attributable to overdose.10,21 City-specific data from NHBS were used to develop the target for the percentage of people experiencing homelessness who experienced a nonfatal overdose in the previous year, which ranged from 15% to 51%. Several sources were used, including a systematic review, to develop a calibration target for mean life expectancy being approximately 50 to 59 years among this population.22,23,24 Finally, multiple published studies estimated that 6-month MOUD retention among people experiencing homelessness is between 18% and 30%,25,26 which is why this range was chosen as a calibration target. These data were used to estimate feasible ranges of parameter values and the model was then calibrated within those ranges to fit simulated outputs to observed targets. Simulated values were within 15% absolute error of observed targets.
Model Analyses
The model was used to generate potential health outcomes by 2028 for each city assuming, in the base case, that population was not subjected to continual involuntary displacement. Population-level health outcomes for each city were projected per 10 000 unsheltered people experiencing homelessness, including overdose mortality, SIRIs and SIRI-related mortality, hospitalizations, and initiations of MOUD. Mean per-person health outcomes, including mean number of total overdoses (fatal and nonfatal) and mean life-years lived over the 10-year period, were also projected. The population modeled was people experiencing homelessness who inject drugs or who have ever injected drugs.
A counterfactual simulation for each city was performed to assess the association of “continual involuntary displacement” on health outcomes. The policy of continual involuntary displacement was modeled as having a persistent risk of being forced to relocate with a disruption in health services. Operationally, in the model, this was simulated by a change in overdose probability, MOUD treatment initiation, and receptive syringe sharing. Because these are changes to individual probabilities, continual involuntary displacement was modeled such that everyone in the model was at risk of displacement, but the experience of an individual was unique. This did not mean that displacement happened on a weekly basis, but that probabilities were applied to individuals based on the cycle length (weekly). These changes did not abate over time. Empirical data collected from people experiencing homelessness who inject drugs in 2 cities in which data were available (Los Angeles and San Francisco, California) were used to estimate the changes to model parameters to reflect the association of outcomes with displacement (eTable 3 in Supplement 1).9,27 For example, people who reported being forcibly displaced in the past 30 days had an adjusted odds ratio (aOR) of 2.50 (95% CI, 1.28-4.90) for nonfatal overdose compared with people who had not been displaced in the past 30 days. This aOR was then applied as a multiplier to the base case overdose probabilities. Similarly, people displaced in the past 30 days were less likely to initiate MOUD than people without recent displacement (aOR, 0.62 [95% CI, 0.42-0.89]). This was applied as a multiplier to the probability of initiation of MOUD. Finally, people who were displaced in the past 30 days were at higher odds of receptive needle/syringe sharing compared with people who were not displaced (aOR, 2.26 [95% CI, 1.18-4.32]). This was applied as a multiplier to the transition probabilities that characterize needle/syringe sharing in the model. Each of these multipliers was applied to the probabilities for each city and the simulation was run for 10 years. These outcomes were compared with those of the “no continual displacement” scenario and the percent change was calculated.
To estimate the potential contribution of continual displacement to mortality, the no displacement model fits for each city were run for 10 years, from 2019 to 2028, with each being compared with the counterfactual model scenario over that period. The population-attributable fraction (PAF) of displacement was calculated by comparing the number of deaths from all causes occurring over 10 years as
| PAF = 100 − 100 × (deaths in base case/deaths in counterfactual). |
Sensitivity analyses were also performed on outcomes for a 5-year period.
Sensitivity Analyses
Because there was uncertainty regarding the empirical data used to inform the population cohorts and model parameters, particularly those related to the outcomes of displacement, probabilistic sensitivity analyses were performed to generate quantitative estimates of uncertainty in select simulated outcomes. For each probabilistic sensitivity analysis, 1000 simulations were performed on a cohort of 1000 people. Displacement parameters were included in the probabilistic sensitivity analyses. For each of the 23 cities, based on unpublished results and expert opinion, the displacement parameters varied through a range of 0.5 to 2.0 times the base case input and drew from a uniform distribution; 99.5% credible intervals (CrIs) were generated using probabilistic sensitivity analyses.
Because the OR estimates are crucial to the study findings, a number of deterministic sensitivity analyses on the displacement parameters were performed because displacement practices across the US may vary. First, for each city, scenarios were modeled in which 1 of the 3 displacement parameters—overdose risk, syringe sharing probability, or MOUD—was unchanged with displacement, while the other 2 were affected by displacement. Additionally, for each city, a 3-way deterministic sensitivity analysis was performed using the upper and lower bounds of the 95% CIs from the study by Chiang et al9 on the aORs that were used for the primary analysis. All 3 parameters were varied simultaneously for a “worst-case” and a “best-case” scenario. For the best-case scenario, lower bounds for overdose and syringe sharing parameter estimates and the upper bound for MOUD initiation were used. For the worst-case scenario, the upper bound for overdose and syringe sharing estimates and the lower bound for MOUD initiation were used.
The Consolidated Health Economic Evaluation Reporting Standards guided writing of this article (eTables 58-59 in Supplement 1).
Results
In the no displacement strategy over a 10-year period, the model predicted between 795 (99% CrI, 0-4198) and 1313 (99% CrI, 0-7433) overdose deaths per 10 000 unsheltered people experiencing homelessness who inject drugs, depending on the city. Furthermore, the model predicted 2204 (99% CrI, 637-5160) to 4220 (99% CrI, 597-5754) SIRIs and 528 (99% CrI, 70-1085) to 1647 (99% CrI, 0-2085) SIRI-related deaths per 10 000 unsheltered people experiencing homelessness who inject drugs, depending on the city. Also, per 10 000 unsheltered people experiencing homelessness who inject drugs, there was an estimated 1520 (99% CrI, 1089-3170) to 2263 (99% CrI, 826-4742) people hospitalized by city and between 7700 (99% CrI, 5319-8779) and 21 731 (99% CrI, 14 512-24 778) initiations of MOUD by city.
In the no displacement strategy over the 10-year period, the mean estimated number of total overdoses varied by city, ranging from 0.6 (99% CrI, 0.04-1.4) to 1.5 (99% CrI, 0-4.2) per person. The mean estimated nonfatal overdoses ranged from 0.52 (99% CrI, 0.05-1.1) to 1.3 (99% CrI, 0-3.5) per person. Depending on the city, individuals lived between 6.4 (99% CrI, 3.0-7.9) and 7.8 (99% CrI, 5.9-8.6) years of the possible 10 years.
At the population level, the model predicted between 1851 (99% CrI, 1163-7958) and 3379 (99% CrI, 1715-8676) overdose deaths per 10 000 unsheltered people experiencing homelessness who inject drugs across cities for the continual displacement strategy (compared with 795 to 1313 per 10 000 in the no displacement strategy). The mean number of total overdoses per person in each city ranged from 1.6 (99% CrI, 0-3.8) to 3.7 (99% CrI, 0.5-6.0). Unsheltered people experiencing homelessness who inject drugs lived a mean of 5.4 (99% CrI, 0.6-6.7) to 7.0 (99% CrI, 4.4-8.1) years of the possible 10 years in the no displacement strategy (eTables 28-50 in Supplement 1).
The ranges of outcomes for each strategy as well as the differences between the 2 strategies are shown in Figure 2. Differences delineated by city are included in eFigure 1 in Supplement 1. At the population level, the model predicted between 974 and 2175 additional overdose deaths per 10 000 people experiencing homelessness who inject drugs, depending on the city, in the continual involuntary displacement strategy compared with no displacement. In 17 of 23 cities, SIRIs and SIRI-related mortality were estimated to be higher in the continual involuntary displacement strategy compared with the no displacement strategy (eFigure 1 in Supplement 1). In those cities with decreases in SIRIs and SIRI-related mortality, the model predicted particularly large increases in overdose-related mortality, which likely account for the SIRI decreases (ie, people die before they get infections). Compared with no displacement, the number of people hospitalized in each city was predicted to be higher in the continual displacement strategy, while initiations of MOUD were lower. eTable 51 in Supplement 1 denotes the percent differences between the 2 strategies, which are relative differences calculated as follows.
Figure 2. Ten-Year Modeled Clinical Outcomes for “No Displacement” and “Continual Involuntary Displacement” Strategies.
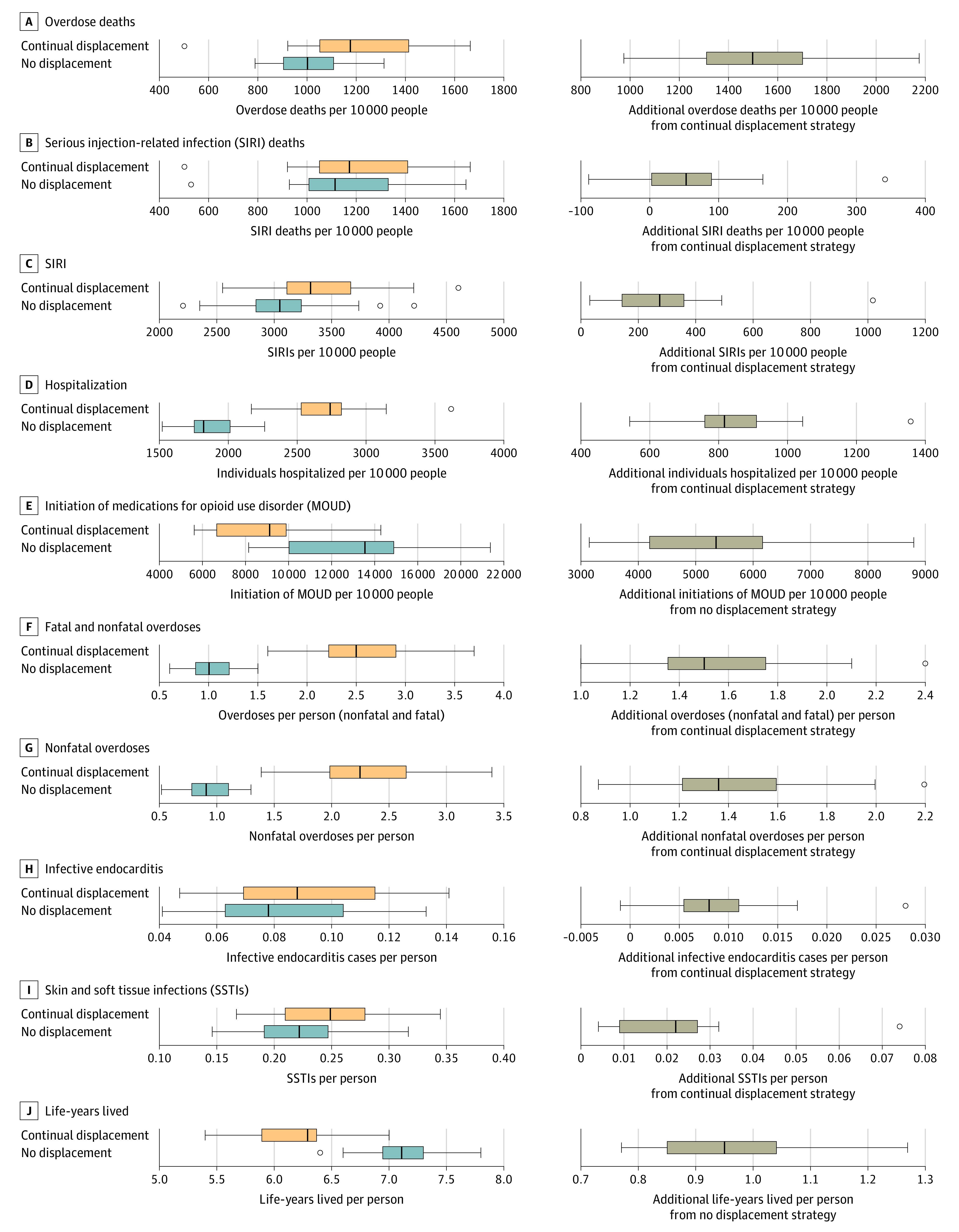
Plots on the left show the ranges of the absolute numbers for each clinical outcome for the “no displacement” and “continual involuntary displacement” strategies and plots on the right show the absolute differences for each clinical outcome between the 2 strategies (medians noted with black lines). Boxes denote first to third quartiles. Whiskers extend to extreme observed values with 1.5 × the IQR of the nearer quartile. Circles denote outside values. An individual could have more than 1 MOUD initiation.
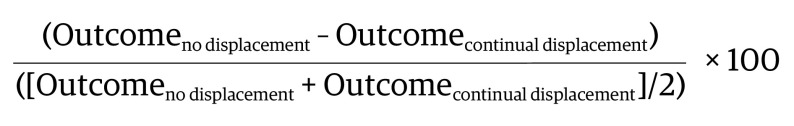 |
Using this equation, the model predicted between a 71% and 94% within-city increase in overdose mortality in the continual involuntary displacement strategy compared with no displacement.
The model estimated potential all-cause mortality PAF estimates for all 23 cities. Continual involuntary displacement could contribute up to 24.4% (99% CrI, 22.9%-27.5%) of deaths among unsheltered people experiencing homelessness who inject drugs over a 10-year period compared with no displacement (eFigure 2 in Supplement 1).
Results of the deterministic sensitivity analyses in which displacement parameters were varied did not qualitatively change the findings (eTables 52-56 and eFigures 3-7 in Supplement 1). Changing the time period to 5 years (eTable 57 and eFigure 8 in Supplement 1) worsened SIRI mortality across the cities, but did not otherwise qualitatively change outcomes. The probabilistic sensitivity analyses demonstrated wide variation in the possible results (eTables 28-50 and eFigure 2 in Supplement 1), but all in the direction of worse health outcomes predicted for displacement.
Discussion
Based on these results, continual involuntary displacement of unsheltered people experiencing homelessness who inject drugs was associated with increased overdose and SIRI-related mortality and decreased 10-year life expectancy by 2028. Overall, the PAF of continual displacement to all-cause mortality among unsheltered people experiencing homelessness who inject drugs may reach as high as 25% by 2028.
As in all modeling studies, these estimates should serve as a broad guide rather than as a predictive tool and can be used to inform policy discussions and future research to reduce harm among this vulnerable population. It was projected that continual involuntary displacement could be associated with one-fourth of all deaths among people experiencing homelessness who inject drugs by 2028. Given the limitations of the underlying data used to inform this projection, it is not possible to know the actual effect of displacement in the next 10 years given the changing sociopolitical landscape, environmental conditions, and health care system.
Displacement also comes with costs.28,29 The main cost drivers are “encampment clearance,” “encampment prevention,” “outreach and housing navigation,” labor costs, and additional health care hospitalizations, which are incurred largely by public insurance, including Medicaid. According to a 2015 analysis,30 a hospitalization for injection-related infective endocarditis in Miami may cost up to $180 000 and a hospitalization for skin and soft tissue infection may cost up to $100 000. In that same cohort of 349 people, over the course of 1 year, there were 35 cases of injection-related infective endocarditis and 170 severe skin and soft tissue infections among people experiencing homelessness who inject drugs. Using model estimates of the current study, displacement in Miami could result in an additional $1.6 million in SIRI-related hospitalization costs over the next 10 years in addition to the costs of the sweeps themselves.
Limitations
This study has several potential limitations related to data quality and availability, as well as uncertainty, inherent in modeling studies. First, there are several assumptions on which the analysis is based, each of which could introduce biases. It was assumed that some parameter inputs were city specific, whereas others were more generalizable. Also, the empirical data used to estimate the changes to displacement model parameters were derived from a small subset of cities and might not be reflective of all cities included in the model. The population from which the displacement parameters were drawn is not necessarily representative of all people experiencing homelessness who inject drugs in the US. Second, the nature of the inputs to the model make it difficult to prove causality rather than association. An attempt to address this limitation was made by performing both deterministic and probabilistic sensitivity analyses. However, available data on forced displacement are limited. Although data are imperfect and the absolute effect of displacement policies are uncertain, no feasible scenario was found in which displacement was beneficial, or even neutral, to health outcomes.
Third, some of the associated effects on overdose reflect the fact that displaced individuals were also less likely to be receiving MOUD. Both outcomes were modeled independently, which may have led to an overestimation. It was also assumed that displacement did not abate over the course of the simulation. In reality, individuals may go through periods of stability in which displacement is not a threat, either because they are temporarily housed, have received support services, or have found a stable outdoor space. In such cases, the effect of displacement may have been overestimated. The model did not capture potential health outcomes other than overdoses and SIRIs, nor did it capture costs or quality of life. The analysis may be limited in that it did not stratify outcomes by race, even though there are increasing disparities in homelessness, overdoses, and SIRIs by race.1,16,31 Future work should stratify outcomes by race, particularly because of the social and structural context in which different racial groups experience homelessness and drug use.
Fourth, this was a closed cohort simulation that assumed that individuals who were homeless at the beginning of the simulation remained homeless throughout. This is a strong assumption that may bias the results toward worse outcomes. However, this is likely balanced with the fact that the model did not account for people who became newly homeless or newly initiated drug use. A manual calibration approach was used because the model was not structured, nor did it have the computational ability, to undertake an optimized calibration approach (eg, joint distribution sampling). As such, bias may have been introduced in the analysis, but a standardized approach to the manual calibration was developed to minimize such bias (Supplement 1). Fifth, the probabilistic sensitivity analyses showed that under different assumptions about parameter values, some of the city-based outcomes had wide ranges, with estimates for some outcomes in which CrIs overlapped between the status quo and continual displacement scenarios. This draws attention to the need for better data and additional research on this vulnerable population and on how to improve health outcomes. In the absence of high-quality data, modeling studies such as this can provide information on the ranges of possible risks that can be useful to decision-makers considering such policies and potential interventions to mitigate risk.
Conclusions
Involuntary displacement of people experiencing homelessness may substantially increase drug-related morbidity and mortality. These findings have implications for the practice of involuntary displacement, as well as policies such as access to housing and supportive services that could mitigate these harms.
eAppendix
Nonauthor collaborators
Data sharing statement
References
- 1.Henry M, de Sousa T, Roddey C, Gayen S, Bednar TJ. The 2020 Annual Homeless Assessment Report (AHAR) to Congress. US Dept of Housing and Urban Development; 2021. Accessed October 31, 2022. https://www.huduser.gov/portal/sites/default/files/pdf/2020-AHAR-Part-1.pdf
- 2.State of Homelessness: 2021 Edition. National Alliance to End Homelessness ; 2021.
- 3.Homeless emergency assistance and rapid transition to housing: defining “chronically homeless”. Fed Regist. 2015;80(233):75791-75806. [Google Scholar]
- 4.After Echo Park Lake research collective . (Dis)Placement: The Fight for Housing and Community After Echo Park Lake. UCLA Luskin Institute on Inequality and Democracy; 2022. [Google Scholar]
- 5.Coalition on Homelessness Human Rights Workgroup . Punishing the Poorest: How the Criminalization of Homelessness Perpetuates Poverty in San Francisco. Coalition on Homelessness; 2015.
- 6.Stringfellow EJ, Kim TW, Gordon AJ, et al. Substance use among persons with homeless experience in primary care. Subst Abus. 2016;37(4):534-541. doi: 10.1080/08897077.2016.1145616 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Yamamoto A, Needleman J, Gelberg L, Kominski G, Shoptaw S, Tsugawa Y. Association between homelessness and opioid overdose and opioid-related hospital admissions/emergency department visits. Soc Sci Med. 2019;242:112585. doi: 10.1016/j.socscimed.2019.112585 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hotton A, Mackesy-Amiti ME, Boodram B. Trends in homelessness and injection practices among young urban and suburban people who inject drugs: 1997-2017. Drug Alcohol Depend. 2021;225:108797. doi: 10.1016/j.drugalcdep.2021.108797 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chiang JC, Bluthenthal RN, Wenger LD, Auerswald CL, Henwood BF, Kral AH. Health risk associated with residential relocation among people who inject drugs in Los Angeles and San Francisco, CA: a cross sectional study. BMC Public Health. 2022;22(1):823. doi: 10.1186/s12889-022-13227-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Fine DR, Dickins KA, Adams LD, et al. Drug overdose mortality among people experiencing homelessness, 2003 to 2018. JAMA Netw Open. 2022;5(1):e2142676. doi: 10.1001/jamanetworkopen.2021.42676 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Centers for Disease Control and Prevention . National HIV Behavioral Surveillance. Published 2022. Accessed June 14, 2022. https://www.cdc.gov/hiv/statistics/systems/nhbs/populations-projects/pwid.html
- 12.Centers for Disease Control and Prevention . Wide-ranging online data for epidemiologic research (WONDER). Accessed June 16, 2022. https://wonder.cdc.gov/
- 13.Jackson KA, Bohm MK, Brooks JT, et al. Invasive methicillin-resistant staphylococcus aureus infections among persons who inject drugs: six sites, 2005-2016. MMWR Morb Mortal Wkly Rep. 2018;67(22):625-628. doi: 10.15585/mmwr.mm6722a2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Larney S, Peacock A, Mathers BM, Hickman M, Degenhardt L. A systematic review of injecting-related injury and disease among people who inject drugs. Drug Alcohol Depend. 2017;171:39-49. doi: 10.1016/j.drugalcdep.2016.11.029 [DOI] [PubMed] [Google Scholar]
- 15.Miller AC, Polgreen PM. Many opportunities to record, diagnose, or treat injection drug-related infections are missed: a population-based cohort study of inpatient and emergency department settings. Clin Infect Dis. 2019;68(7):1166-1175. doi: 10.1093/cid/ciy632 [DOI] [PubMed] [Google Scholar]
- 16.Kadri AN, Wilner B, Hernandez AV, et al. Geographic trends, patient characteristics, and outcomes of infective endocarditis associated with drug abuse in the United States from 2002 to 2016. J Am Heart Assoc. 2019;8(19):e012969. doi: 10.1161/JAHA.119.012969 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.McLaughlin MF, Li R, Carrero ND, Bain PA, Chatterjee A. Opioid use disorder treatment for people experiencing homelessness: a scoping review. Drug Alcohol Depend. 2021;224:108717. doi: 10.1016/j.drugalcdep.2021.108717 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Krawczyk N, Fawole A, Yang J, Tofighi B. Early innovations in opioid use disorder treatment and harm reduction during the COVID-19 pandemic: a scoping review. Addict Sci Clin Pract. 2021;16(1):68. doi: 10.1186/s13722-021-00275-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Arias E. United States life tables, 2008. Natl Vital Stat Rep. 2012;61(3):1-63. [PubMed] [Google Scholar]
- 20.Nicholas W, Greenwell L, Henwood BF, Simon P. Using point-in-time homeless counts to monitor mortality trends among people experiencing homelessness in Los Angeles County, California, 2015-2019. Am J Public Health. 2021;111(12):2212-2222. doi: 10.2105/AJPH.2021.306502 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Colorado Coalition for the Homeless. We will remember 2019: homeless death review. Accessed March 28, 2022. https://www.coloradocoalition.org/sites/default/files/2020-02/Homeless%20Death%20Review_final%2012-17-19.pdf
- 22.Cawley CL, Kanzaria HK, Kushel M, Raven MC, Zevin B. Mortality among people experiencing homelessness in San Francisco 2016-2018. J Gen Intern Med. 2022;37(4):990-991. doi: 10.1007/s11606-021-06769-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Funk AM, Greene RN, Dill K, Valvassori P. The impact of homelessness on mortality of individuals living in the United States: a systematic review of the literature. J Health Care Poor Underserved. 2022;33(1):457-477. doi: 10.1353/hpu.2022.0035 [DOI] [PubMed] [Google Scholar]
- 24.Baggett TP, Hwang SW, O’Connell JJ, et al. Mortality among homeless adults in Boston: shifts in causes of death over a 15-year period. JAMA Intern Med. 2013;173(3):189-195. doi: 10.1001/jamainternmed.2013.1604 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lee CS, Liebschutz JM, Anderson BJ, Stein MD. Hospitalized opioid-dependent patients: exploring predictors of buprenorphine treatment entry and retention after discharge. Am J Addict. 2017;26(7):667-672. doi: 10.1111/ajad.12533 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ker S, Hsu J, Balani A, et al. Factors that affect patient attrition in buprenorphine treatment for opioid use disorder: a retrospective real-world study using electronic health records. Neuropsychiatr Dis Treat. 2021;17:3229-3244. doi: 10.2147/NDT.S331442 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Goldshear JCK, Huh J, Henwood B, Kral AH, Bluthenthal RN. Association between relocation and substance use outcomes among a community sample of people who inject drugs in Los Angeles, CA and Denver, CO. Presented at: 84th College on Problems of Drug Dependence Annual Scientific Meeting; June 11-15, 2022; Minneapolis, MN. [Google Scholar]
- 28.Tinoco M. LA will spend $30M this year on homeless sweeps: do they even work? LAist. April 10, 2019. Accessed June 16, 2022. https://laist.com/2019/04/10/homeless_sweeps_los_angeles_public_health.php
- 29.Dunton LKJ, Burnett K, Fiore N, Yetvin W. Exploring Homelessness Among People Living in Encampments and Associated Cost: City Approaches to Encampments and What They Cost. Office of Policy Development and Research; 2021. [Google Scholar]
- 30.Tookes H, Diaz C, Li H, Khalid R, Doblecki-Lewis S. A cost analysis of hospitalizations for infections related to injection drug use at a county safety-net hospital in Miami, Florida. PLoS One. 2015;10(6):e0129360. doi: 10.1371/journal.pone.0129360 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Larochelle MR, Slavova S, Root ED, et al. Disparities in opioid overdose death trends by race/ethnicity, 2018-2019, from the Healing Communities Study. Am J Public Health. 2021;111(10):1851-1854. doi: 10.2105/AJPH.2021.306431 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eAppendix
Nonauthor collaborators
Data sharing statement