Abstract
Aim
To compare the effectiveness of practitioner versus digitally delivered interventions for reducing hazardous and harmful alcohol consumption.
Design
Systematic review and network meta‐analysis comprising comprehensive search for randomised controlled trials, robust screening and selection methods and appraisal with the Cochrane Risk of Bias tool. Network meta‐analyses were conducted in Stata using random effects, frequentist models. The confidence in network meta‐analysis (CINeMA) tool was used to assess confidence in effect sizes.
Setting
Online or community or health settings where the intervention was immediately accessible without referral.
Participants
Non treatment‐seeking hazardous or harmful drinkers.
Measurements
Primary outcome was mean difference in alcohol consumption (g/wk); secondary outcome was number of single high intensity drinking episodes. Baseline consumption was analysed as a covariate.
Findings
Of 201 included trials (94 753 participants), 152 reported a consumption outcome that could be converted to grams/week; 104 reported number of single high intensity drinking episodes. At 1 and 6 months, practitioner delivered interventions reduced consumption more than digitally delivered interventions (1 month: −23 g/wk (95% CI, −43 to −2); 6 months: −14 g/wk [95% CI, −25 to −3]). At 12 months there was no evidence of difference between practitioner and digitally delivered interventions (−6 g/wk [95% CI, −24 to 12]). There was no evidence of a difference in single high intensity drinking episodes between practitioner and digitally delivered interventions at any time point. Effect sizes were small, but could impact across a population with relatively high prevalence of hazardous and harmful drinking. Heterogeneity was a concern. Some inconsistency was indicated at 1 and 6 months, but little evidence was apparent at 12 months.
Conclusion
Practitioner delivered interventions for reducing hazardous and harmful alcohol consumption are more effective than digitally delivered interventions up to 6 months; at 12 months there is no evidence of a difference.
Keywords: Alcohol drinking, Alcohol‐related disorders, Binge drinking, Brief alcohol interventions, Digital alcohol interventions, Hazardous alcohol consumption
INTRODUCTION
Background
Alcohol use is a prominent risk factor for population health, with well evidenced impacts on maternal and child health, infectious and noncommunicable diseases, mental health, injuries and poisonings [1]. Alcohol use disorders are among the top 20 leading causes of global disability‐adjusted life years (DALYs) for people age 25 to 49 [2]. Problems associated with alcohol use also cause social and economic losses; often lower socioeconomic groups disproportionately experience detrimental impact.
Brief interventions helping people recognise and cut down hazardous and harmful drinking are effective [3, 4, 5], widely accepted as best practice and recommended in many guidelines [6]. Practitioner delivered brief interventions usually provide one or more of the following, either in person or via telephone: personalised feedback on consumption, often compared with population norms; information and guidance about reducing consumption; or counselling techniques to explore what drinking means to them and how to reduce it. The potential for delivering similar interventions digitally through computers or mobile devices has been explored [7, 8]. However, despite the large volume of trials testing practitioner and digitally delivered interventions, and previous systematic reviews demonstrating the effectiveness of both practitioner and digitally delivered interventions compared to no or minimal intervention [3, 4, 5, 8, 9, 10, 11], few trials have compared them directly. To our knowledge, three previous systematic reviews have analysed practitioner versus digitally delivered interventions [5, 12, 13]. One review reported no evidence of any difference in consumption between interventions [5], and two reviews reported in favour of practitioner‐delivered interventions for quantity of drinking after 4 months [13], and for peak blood alcohol concentration (BAC), drinking frequency and alcohol‐related problems [12]. All noted that few trials directly compared these interventions, and this review aims to mitigate this using network meta‐analysis (NMA). Where direct evidence is lacking, indirect comparison or NMA can be used to estimate comparative effectiveness of interventions [14]. NMA allows the simultaneous comparison of more than two interventions by including effectiveness estimates from trials that directly compare them (i.e. practitioner delivered versus digitally delivered) and also from trials that do not (e.g. practitioner delivered vs control) [14]. NMA allows a more precise estimate of the comparison between interventions where trials that compare them directly are sparse. In an NMA, it is important that all participants could plausibly be eligible for any intervention in the network; this is the case for this analysis because the populations recruited across all eligible trials were screened as hazardous or harmful drinkers.
In existing trials of brief alcohol interventions, control group content varies substantially, from assessment only, through health promotion leaflets about hazardous consumption, to general advice and health education (sometimes called ‘attention controls’) [15]. Therefore, as well as exploring the difference in effectiveness between practitioner and digitally delivered interventions using NMA, we explored potential differences based on what was provided as ‘treatment as usual’ for control groups [16]. Control groups were categorised as ‘attention control’ (containing no alcohol‐specific information) and ‘minimal alcohol information’.
Aim of the review
Our aim was to compare the effectiveness of practitioner and digitally delivered interventions for reducing hazardous and harmful alcohol consumption in people not seeking alcohol treatment. This work takes a public health perspective, seeking to be generalizable to those living in the community with unrecognised hazardous consumption.
METHODS
Protocol and registration
The protocol was registered with Prospero (CRD42018089609) in July 2018. Patient and public involvement (PPI) in the form of a workshop was used to aid protocol development. Two PPI colleagues helped with interpretation and dissemination of study findings. This work follows standard systematic review procedures and is reported according to the Preferred Reporting Items for Systematic Reviews and Meta‐Analyses (PRISMA) extension for NMA [17].
Eligibility criteria for the systematic review
Randomised controlled trials were included if they recruited people living in the community who were screened as hazardous or harmful drinkers and compared a freely available practitioner or digitally delivered intervention to a comparator or a control group (Supplement 1.1). ‘Practitioner delivered’ included all interventions delivered with a conversation in real time. ‘Digitally delivered’ included all interventions delivered via a device, including text messages or other non‐synchronous interaction. All interventions had to provide personalised feedback. Control arms provided assessment only, an attention control not involving information about alcohol consumption, and/or a control condition providing brief verbal or written advice about hazardous consumption (Supplement 1.1). Trials had to report a measure of consumption and report follow‐up after at least 1 month. No restriction by language, date of publication or location was applied.
Identification of included studies and extraction of data
Published systematic reviews were used as the initial source of trials [4, 5, 7, 18, 19, 20]. Update searches using 11 databases were conducted from January 2016 to April 2020 to identify more recent trials (see Figure 1, Supplement 1.2, Supporting information Tables S1, S2 and S3). For all reviews, included and excluded studies lists were checked for potentially eligible studies.
FIGURE 1.
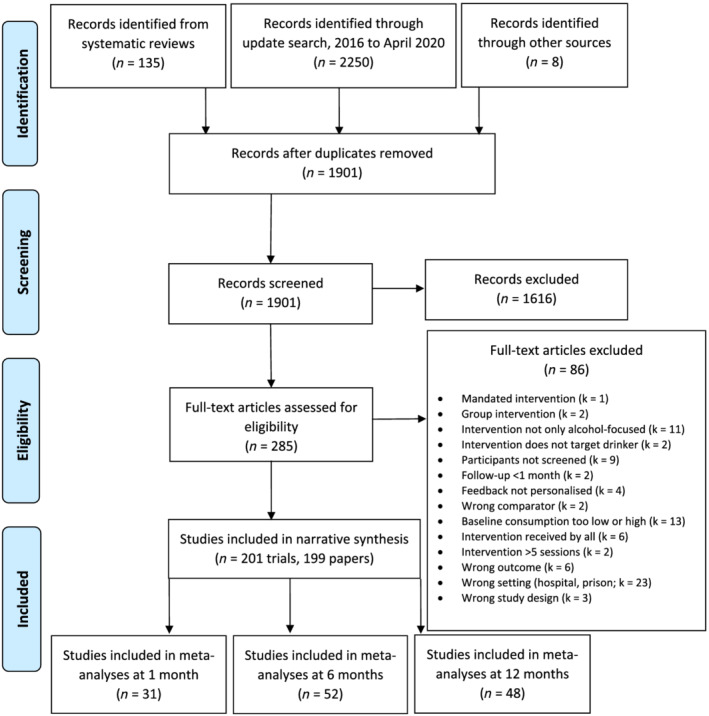
PRISMA 2009 flow diagram
Two reviewers (of F.R.B., R.P.W.K., E.J. and C.G.) independently screened all titles and abstracts from the digitally delivered update search in Rayyan [21]. Discrepancies were discussed; records where disagreement or uncertainty remained were put through to the next stage. One reviewer (F.R.B.) screened titles and abstracts from the practitioner delivered update search in Rayyan. Full texts of all potentially eligible records were assessed independently by two reviewers (of F.R.B., R.P.W.K., E.J. and C.G.) and uncertainties resolved in team meetings.
Data regarding participant and intervention characteristics, outcome, setting and methodological characteristics were extracted independently by two reviewers (Supplement 1.3). Missing data was requested from authors.
Risk of bias within individual studies
The Cochrane Risk of Bias tool was used to assess risk of bias within individual studies (see Supplement 1.5). For each domain, an assessment of high, unclear or low risk of bias was allocated. These assessments were displayed using the Robvis tool [22] and informed the sensitivity analyses.
Summary effect measures
The primary outcome measure was mean difference in alcohol consumption in grams per week, with the corresponding SD (Supplement 1.6). The secondary outcome was the number of single high intensity drinking episodes per month (referred to throughout as binge drinking episodes) with heavy drinking defined by the studies (usually five or more drinks in a single occasion for men, or four for women). Primary and secondary outcomes were analysed separately at 1, 6 and 12 months because previous work suggests evidence of treatment effect decay over a year [4, 5]. This provided six networks for analysis (three time points each for grams/week and binge drinking episodes respectively).
Planned methods of analysis
We conducted an NMA using the mvmeta package in Stata. The null hypothesis was that there was no difference in effectiveness between practitioner and digitally delivered interventions; we excluded trial arms from the analysis that blended practitioner and digitally delivered content. We assumed a common heterogeneity variance across all comparisons. For cluster‐randomised trials, we used an external estimate of the intra‐cluster coefficient to estimate the effect [23]. The between‐study variance (Tau2) and I2 statistic were estimated to measure statistical heterogeneity and tabulated alongside the effect estimates. We used the ranking function to assess the probability of each intervention being most effective.
We carried out a meta‐regression analysis to explore differences in the estimated effect size according to participants' baseline consumption.
Network connectedness was assessed visually. Four intervention nodes (categories) were formed: interventions that provided practitioner delivered content; interventions that provided digitally delivered content; interventions that provided minimal alcohol‐related content; and baseline assessment only (Supplement 1.4). Assessment only and attention control groups were combined in one node to uncover any effect of alcohol‐related material, whereas attention control and minimal alcohol information groups were combined to uncover a placebo effect from the assessment‐only group. Based on extracted data, one reviewer (F.R.B.) categorised all interventions. Where there was uncertainty, categorisation was discussed with a second reviewer (E.F.S.K., E.J., C.G. and R.P.W.K.). Interventions were categorised without reference to study authors' labelling to ensure consistency of definitions in the network. The reference category for analysis was assessment only, where participants received baseline assessment, but no other information or intervention.
Sensitivity analysis was conducted to assess the effects of omitting studies at high risk of bias.
Assessment of inconsistency
NMA assumes consistency between the direct, pairwise estimate for the comparison between any two nodes and the estimate from the corresponding indirect treatment comparison. Details of the pairwise meta‐analyses methods are reported in Supplement 1.7. We evaluated this consistency across the whole network using a design‐by‐treatment interaction [24, 25], a loop‐specific method (focusing on individual loops in the network), and side‐split methods (where direct evidence for a comparison was compared to the whole network (Supplement 1.8) [26]. Although conventional statistical significance is set at 0.05, tests for detecting inconsistency have been shown to be underpowered [14]. As such, although we report the specific P‐value, we do not rely solely on it to draw conclusions.
Credibility of evidence
We used the confidence in network meta‐analysis (CINeMA) web‐based application to assess confidence in the effect sizes and ranking [27]. We captured the maximum amount of data from all analyses using data from longest follow‐up point of all studies reporting up to 12 months.
RESULTS
Study selection
Searches of the included and excluded studies in the six systematic reviews produced 135 eligible trials. The update search yielded a further 66 trials, making a total of 201 included trials reported across 199 papers, with 94 753 participants (Figure 1). Reasons for exclusion are presented in Supporting information Table S5.
In total, 118 trials provided one or more practitioner delivered interventions and 89 provided one or more digitally delivered interventions (some provided both). Assessment only control was provided in 104 arms, attention control (non‐interventional input unrelated to alcohol additional to assessment) in 39 arms and minimal alcohol information in 78 arms. The network maps at each time point were well connected for both primary and secondary outcomes (Figure 2).
FIGURE 2.
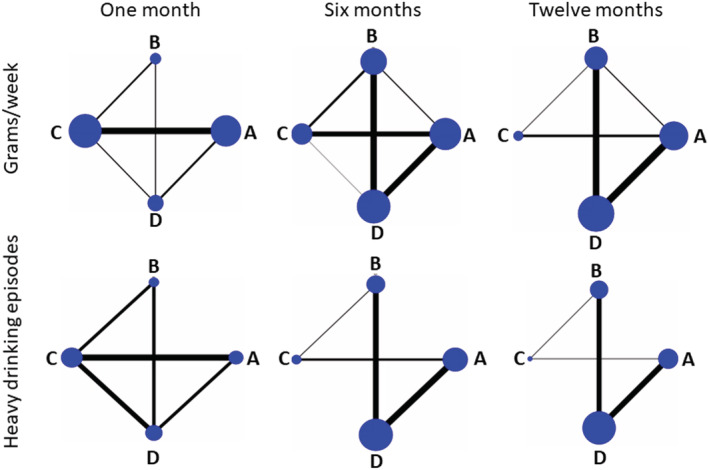
Network maps for grams/week and number of binge drinking episodes at 1, 6 and 12 months. Randomised comparisons between conditions are depicted by lines between nodes. Size of circular nodes is proportional to the number of arms providing data; thickness of the connections is proportional to the number of comparisons available from the included trials. (a) Assessment only (reference node); (b) minimal alcohol information; (c) digitally delivered intervention; (d) practitioner‐delivered intervention
Study characteristics
Trials took place in the United States (US) (n = 105), Canada (n = 5), both the United States and Canada (n = 1), United Kingdom (UK) (n = 21), Europe (n = 42), Australasia (n = 13), Asia (n = 6), Africa (n = 5), South America (n = 2) and Russia (n = 1). Study dates ranged from 1987 to 2020 (Table 1 for summary; Supporting information Table S4 for full characteristics of included studies, Supporting information Figure S3). Digitally delivered interventions were available via mobile phone or tablet (n = 66, of which three used SMS and five used an app), or desktop or fixed computer (n = 21). Practitioner delivered interventions used structured advice, motivational interviewing or cognitive behavioural approaches. Three trials involved stepped care. Few studies reported information about adverse effects as an outcome measure.
TABLE 1.
Summary characteristics of studies included in the review
| Target population | Comorbidity | Setting (recruitment) | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| General | Students/younger | Older people | Men only | Women only | None | Mental health | Physical health | Workplace | Emergency care | Primary care | Pharmacy | Community | Uni/college | Online | |
| D vs P | 6 | 9 | 0 | 1 | 0 | 12 | 0 | 1 | 1 | 3 | 3 | 0 | 1 | 6 | 1 |
| D vs As | 20 | 41 | 0 | 3 | 1 | 60 | 2 | 0 | 2 | 5 | 4 | 0 | 7 | 30 | 12 |
| D vs Al | 12 | 15 | 0 | 2 | 1 | 26 | 1 | 0 | 2 | 3 | 4 | 0 | 3 | 8 | 6 |
| P vs As | 38 | 20 | 2 | 5 | 5 | 58 | 1 | 2 | 4 | 12 | 32 | 0 | 2 | 11 | 0 |
| P vs Al | 35 | 13 | 1 | 6 | 0 | 45 | 2 | 3 | 2 | 15 | 23 | 1 | 3 | 5 | 0 |
| Total | 111 | 98 | 3 | 17 | 7 | 201 | 6 | 6 | 11 | 38 | 66 | 1 | 16 | 60 | 19 |
Al: minimal alcohol information, As: assessment only control, D: digitally delivered, P: practitioner delivered.
Risk of bias within studies
Two main sources of bias were noted in this body of trials (Figure 3, Supporting information Table S6). Performance bias was because of difficulty in blinding participants and people delivering interventions. In trials where interventions were delivered online, provider blinding was judged to be low because there were no personnel involved. These trials tended to report high levels of attrition, particularly where they were conducted purely online, involving no interaction with people. A smaller proportion of trials included in the analyses were at high risk of bias overall compared to the proportion of trials overall (46% vs 51%, respectively) (Supplement 2.2).
FIGURE 3.
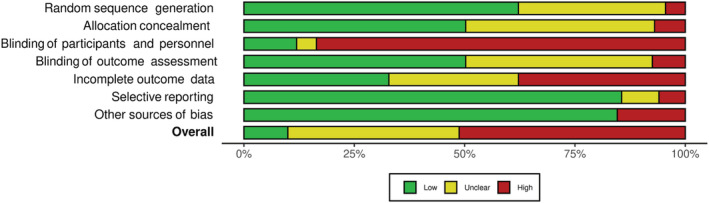
Risk of bias assessments. Figure created using robvis [22]
Results of individual studies
A total of 152 trials (76%) reported a consumption outcome that could be converted to grams per week (g/wk), of which 35 (23%) reported at 1 month, 65 (43%) at 6 months and 53 (35%) at 12 months. A further 43 trials (21%) reported frequency (number of drinking days) or intensity (drinks/drinking day) rather than a measure that could be converted to g/wk (i.e. amount/unit of time). In total, 104 studies reported a measure of high intensity drinking at 1 (n = 20, 19%), 6 (n = 45, 43%) or 12 months (n = 44, 42%) (some reported at more than one time point). We contacted one author to request raw data and had previously contacted seven authors during completion of the Cochrane reviews [4, 5].
Synthesis of results
A total of 106 trials (53%) reported evidence of a reduction in consumption in the intervention group compared to control across different time points, measured by quantity consumed (convertible to drinks/week), frequency (convertible to drinking days/week), intensity (drinks/occasion), AUDIT score, or risk group status. Another 82 trials (41%) reported some reduction in consumption, but no evidence of a difference between intervention and control arms. In 13 trials (6%), there was either no evidence of change or average consumption in an intervention arm increased compared to control. There was no apparent pattern across studies reporting no evidence or an increase; they contained a mix of mean ages, trials targeting younger people versus all adults, settings and intervention types.
Because of the volume of results and because most trials reported a reduction in intervention arms, we focus here on the findings from studies included in the NMA; findings from all included trials are shown in characteristics tables (Tables 1 and Supporting information Table S4).
Direct evidence to inform the effectiveness estimate for practitioner versus digitally delivered interventions was reported in nine trials (4%). Practitioner and digitally delivered trials had different follow‐up profiles: whereas the latter tended to report between 1 and 6 months, the former tended to report at 6 months and over. Figure 4 presents the evidence for practitioner versus digitally delivered interventions, of which nine trials compared them directly, from pairwise and network analyses at all time points. There was no evidence at any time point of a difference in consumption between participants in assessment only control groups compared to those in minimal alcohol information groups.
FIGURE 4.
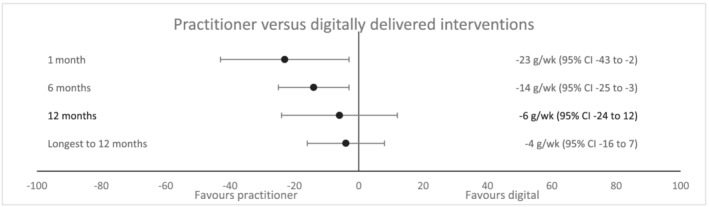
Effect estimates from network meta‐analyses for practitioner versus digitally delivered interventions, g/wk at all time points
Outcomes at 1 month
Forty‐four trials reported g/wk at 1 month, of which 31 reported sufficient data to be included in the NMA. Both practitioner delivered and digitally delivered interventions were effective at 1 month compared to assessment only control; results were consistent between network and pairwise analyses (Tables 2, Supporting information Table S7). The NMA showed that participants receiving practitioner delivered interventions reduced their consumption by 23 g/wk (2.9 UK/1.6 US units) more than those receiving digitally delivered interventions. Although the point estimate differed considerably from that of the corresponding pairwise analysis, the 95% CI from the network estimate fell within that of the pairwise estimate, which was from only three studies that reported g/wk and was very imprecise. Only one of nine trials directly comparing practitioner to digitally delivered interventions favoured digitally delivered interventions. Practitioner delivered interventions showed 98.6% probability of being ranked best and digitally delivered interventions a 93.6% probability of being ranked second best. Participants receiving a practitioner delivered intervention reduced their consumption on average by 46 g/wk (5.8 UK/3.3 US units) compared to those in assessment only arms. The corresponding reduction compared to assessment only for those receiving a digitally delivered intervention was 24 g/wk (3.0 UK/1.7 US units). When compared to control groups containing alcohol‐related information, practitioner delivered interventions showed strong evidence of reduction by 40 g/wk, whereas digital interventions showed weaker evidence of a smaller reduction (18 g/wk).
TABLE 2.
Effect estimates from pairwise and network meta‐analyses for g/wk at 1 month
| Comparison | Direct estimate (95% CI) [no. of studies] randomised participants | I 2 | Tau 2 | Network estimate [31 studies] 13 239 participants |
|---|---|---|---|---|
| Practitioner delivered vs digitally delivered |
−4 g/wk (−45 to 37) [3 studies] 321 participants |
32.9 | 473 | −23 (−43 to −2) |
| Practitioner delivered vs control (minimal alcohol information) |
−62 (−93 to −33) [3 studies] 702 participants |
0.0% | 0.0 | −40 (−65 to −16) |
| Practitioner delivered vs control (assessment only) |
−44 (−62 to −28) [6 studies] 865 participants |
0.0% | 0.0 | −46 (−66 to −27) |
| Digitally delivered vs control (minimal alcohol information) |
−10 (−23 to 4) [5 studies] 763 participants |
0.0% | 0.0 | −18 (−38 to 3) |
| Digitally delivered vs control (assessment only) |
−26 (−38 to −14) [18 studies] 11 082 participants |
72.8% | 367 | −24 (−35 to −13) |
| Control (minimal alcohol information) vs control (assessment only) | [No studies] | – | – | −6 (−28 to 16) |
Twenty‐one trials reported number of binge drinking episodes at 1 month, of which 11 contributed data to the NMA (Tables 3, Supporting information Table S8). There was no evidence of difference in number of binge drinking episodes between practitioner and digitally delivered interventions, with participants receiving practitioner delivered interventions reporting about three fewer binge drinking episodes every 2 months when compared to assessment only control participants. Digitally delivered interventions showed a statistically significant reduction when compared to assessment only control, but not to minimal alcohol information (Tables 3, Supporting information Table S8).
TABLE 3.
Effect estimates from pairwise and network meta‐analyses for number of binge drinking episodes per month at 1 month
| Comparison | Direct estimate (95% CI) [no. of studies] randomised participants | I 2 | Tau 2 | Network estimate [11 studies] 2859 participants |
|---|---|---|---|---|
| Practitioner delivered vs digitally delivered |
−0.1 (−1.0 to 0.7) [3 studies] 321 participants |
7.7% | 0.0416 | −0.5 (−1.3 to 0.3) |
| Practitioner delivered vs control (minimal alcohol information) |
−2.3 (−4.3 to −0.3) [2 studies] carriage return immediately 447 participants |
0.0% | 0.0000 | −1.2 (−2.4 to 0.0) |
| Practitioner delivered vs control (assessment only) |
−1.5 (−2.5 to −0.5) [2 studies] 280 participants |
6.7% | 0.0362 | −1.4 (−2.3 to −0.5) |
| Digitally delivered vs control (minimal alcohol information) |
−0.4 (−1.2 to 0.5) [2 studies] 358 participants |
0.0% | 0.0000 | −0.7 (−1.7 to 0.3) |
| Digitally delivered vs control (assessment only) |
−1.0 (−2.0 to −0.1) [4 studies] 1681 participants |
74.7% | 0.6542 | −0.9 (−1.6 to −0.3) |
| Control (minimal alcohol information) vs control (assessment only) | [No studies] | – | – | −0.2 (−1.4 to 0.9) |
Outcomes at 6 months
At 6 months, 65 trials reported g/wk, of which 52 contributed to the NMA. Participants receiving practitioner delivered interventions reduced their consumption on average by 14 g/wk (1.8 UK/1.0 US units) more than those who received digitally delivered interventions at 6 months (Tables 4, Supporting Table S9). Practitioner delivered interventions showed 99% probability of being ranked best and digitally delivered interventions 98.3% probability of being ranked second best. Participants receiving practitioner delivered interventions reported reducing their weekly consumption by approximately 28 g/wk (3.5 UK/2.0 US units) compared to both assessment only and minimal alcohol information participants (Table 4). Digitally delivered interventions reduced participants' consumption by approximately 14 g/wk (1.8 UK/1.0 US units) compared to both types of control.
TABLE 4.
Effect estimates from pairwise and network meta‐analyses for g/wk at 6 months
| Comparison | Direct estimate (95% CI) [no. of studies] randomised participants | I 2 | Tau 2 | Network estimate [52 studies] 26 777 participants |
|---|---|---|---|---|
| Practitioner delivered vs digitally delivered |
−7 (−64 to 51) [1 study] 279 participants |
– | – | −14 (−25 to −3) |
| Practitioner delivered vs control (minimal alcohol information) |
−23 (−32 to −15) [18 studies] carriage return immediately 6641 participants |
5.8% | 20.34 | −29 (−39 to −19) |
| Practitioner delivered vs control (assessment only) |
−33 (−45 to −21) [17 studies] 7018 participants |
44.5% | 223.41 | −28 (−37 to −18) |
| Digitally delivered vs control (minimal alcohol information) |
−31 (−47 to −15) [7 studies] 1692 participants |
0.5% | 2.59 | −15 (−28 to −3) |
| Digitally delivered vs control (assessment only) |
−10 (−18 to −3) [14 studies] 12 488 participants |
43.9% | 76.82 | −14 (−22 to −6) |
| Control (minimal alcohol information) v control (assessment only) |
−9 (−62 to 44) [3 studies] 783 participants |
21.5% | 512.39 | 1 (−10 to 13) |
The number of binge drinking episodes at 6 months was reported by 45 trials, of which 19 contributed to the NMA. There was no evidence of a difference between practitioner and digitally delivered interventions and the two types of control. Those receiving practitioner delivered interventions reduced heavy drinking compared to both types of control by the equivalent of 4 binge drinking episodes over 5 months (Tables 5, Supporting information Table S10). No statistically significant difference was found for digital interventions compared to both control groups.
TABLE 5.
Effect estimates from pairwise and network meta‐analyses for number of binge drinking episodes per month at 6 months
| Comparison | Direct estimate (95% CI) [no. of studies] randomised participants | I 2 | Tau 2 | Network estimate [19 studies] 7300 participants |
|---|---|---|---|---|
| Practitioner delivered vs digitally delivered | [No studies] | – | – | −0.6 (−1.3 to 0.1) |
| Practitioner delivered vs control (minimal alcohol information) |
−0.6 (−1.2 to −0.1) [7 studies] 2065 participants |
0.0% | 0.00 | −0.8 (−1.4 to −0.1) |
| Practitioner delivered vs control (assessment only) |
−1.0 (−1.4 to −0.6) [8 studies] carriage return immediately 3505 participants |
33.3% | 0.12 | −0.9 (−1.4 to −0.5) |
| Digitally delivered vs control (minimal alcohol information) |
−1.4 (−3.3 to 0.6) [1 study] 208 participants |
– | – | −0.1 (−1.0 to 0.8) |
| Digitally delivered vs control (assessment only) |
−0.2 (−0.9 to 0.5) [3 studies] 1522 participants |
60.7% | 0.24 | −0.3 (−0.9 to 0.3) |
| Control (minimal alcohol information) vs control (assessment only) | [No studies] | – | – | −0.2 (−0.9 to 0.5) |
Outcomes at 12 months
At 12 months, 45 trials contributed to the NMA out of 54 reporting a measure of consumption (Tables 6, Supporting information Table S11). Little evidence of a difference was found in consumption between those receiving practitioner versus digitally delivered interventions. At 12 months the ranking of best treatment between practitioner and digitally delivered interventions was more equivocal (73.9% and 26.1%, respectively). Practitioner delivered interventions reduced consumption by 19 g/wk and 21 g/wk compared to minimal alcohol information and assessment only respectively (~2.5 UK/1.4 US units). There was weaker evidence that digitally delivered interventions reduced consumption by 16 g/wk and 14 g/wk compared to assessment only and minimal alcohol information (nearly two UK/1 US unit[s]).
TABLE 6.
Effect estimates from pairwise and network meta‐analyses for g/wk at 12 months
| Comparison | Direct estimate (95% CI) [no. of studies] randomised participants | I 2 | Tau 2 | Network estimate [45 studies] 25 288 participants |
|---|---|---|---|---|
| Practitioner delivered vs digitally delivered | [No studies] | – | – | −6 (−24 to 12) |
| Practitioner delivered vs control (minimal alcohol information) |
−19 (−30 to −7) [18 studies] 6482 participants |
31.7% | 172.75 | −19 (−32 to −7) |
| Practitioner delivered vs control (assessment only) |
−22 (−33 to −10) [19 studies] 10 671 participants |
75.9% | 439.87 | −21 (−31 to −11) |
| Digitally delivered vs control (minimal alcohol information) |
−14 (−33 to 5) [2 studies] 3228 participants |
0.0% | 0.00 | −14 (−33 to 5) |
| Digitally delivered vs control (assessment only) |
−15 (−32 to 2) [7 studies] 5045 participants |
46.6% | 216.13 | −16 (−32 to 1) |
| Control (minimal alcohol information) vs control (assessment only) |
−8 (−37 to 22) [3 studies] 1220 participants |
0.0% | 0.00 | −1 (−16 to 13) |
Number of binge drinking episodes after 12 months
Of 44 trials reporting number of binge drinking episodes at 12 months, 19 contributed to the NMA. There was no evidence of a difference between practitioner and digitally delivered interventions. Participants who received practitioner delivered interventions reported the equivalent of about one less binge drinking episode every 3 months, but this was only statistically significant when compared to assessment only control (Tables 7, Supporting Information Table S12). Digitally delivered interventions resulted in slightly larger estimates of reduction, but were not statistically significant.
TABLE 7.
Effect estimates from pairwise and network meta‐analyses for number of binge drinking episodes per month at 12 months
| Comparison | Direct estimate (95% CI) [no. of studies] randomised participants | I 2 | Tau 2 | Network estimate [19 studies] 11 636 participants |
|---|---|---|---|---|
| Practitioner delivered vs digitally delivered | [No studies] | – | – | 0.1 (−0.5 to 0.8) |
| Practitioner delivered vs control (minimal alcohol information) |
−0.3 (−0.8 to 0.2) [8 studies] 2295 participants |
0.0% | 0.00 | −0.3 (−0.7 to 0.1) |
| Practitioner delivered v control (assessment only) |
−0.5 (−0.8 to −0.1) [9 studies] 6117 participants |
46.6% | 0.11 | −0.4 (−0.6 to −0.3) |
| Digitally delivered vs control (minimal alcohol information) |
−0.4 (−1.6 to 0.7) [1 study] 2652 participants |
– | – | −0.4 (−1.2 to 0.3) |
| Digitally delivered vs control (assessment only) |
−0.6 (−1.3 to 0.1) [1 study] 572 participants |
– | – | −0.6 (−1.2 to 0.0) |
| Control (minimal alcohol information) vs control (assessment only) | [No studies] | – | – | −0.2 (−0.6 to 0.3) |
Inconsistency
In the 1‐month analysis of grams/week, the overall P‐value for inconsistency of the network was 0.16 and P‐values from the side split ranged from 0.12 to 0.72. In the binge drinking analysis, the overall P‐value for inconsistency of the network was 0.13 and P‐values from the side split ranged from 0.2 to 0.81. In both analyses, there was less evidence of inconsistency between the direct and indirect evidence for practitioner versus assessment control.
In the 6‐month analysis of grams/week, the overall P‐value for inconsistency of the network was 0.34 and P‐values from the side split ranged from 0.02 to 0. 80. The lower P‐value showed strong evidence of inconsistency around much of the network, except in the comparison between assessment only and minimal alcohol information, and between practitioner and digitally delivered interventions. The binge drinking analysis at 6 months showed less evidence of inconsistency (overall and all side split values of P = 0.2).
At 12 months, all P‐values for both grams/week and binge drinking were >0.8, indicating no evidence of inconsistency.
Network meta‐regression—baseline consumption
In our protocol, we planned meta‐regression and sensitivity analyses for the main NMA analyses only. The network meta‐regression suggested that, at 1 month and 6 months, there was a correlation between baseline consumption and effect for the digitally delivered intervention, such that for every unit increase in baseline consumption the grams/week reduced. As such, people with heavier baseline consumption would benefit more from the intervention. At 12 months this effect was apparent only for practitioner delivered interventions, but not when the oldest trials (that tended to higher baseline consumption) were omitted. These results are not robust because there were few trials of digitally delivered interventions reporting at 12 months and few trials of practitioner delivered interventions reporting at 1 month.
Sensitivity analysis
The results for all studies in the analysis (n = 100 in longest follow‐up to 12 months) were compared to results with studies at high risk of bias omitted (n = 53). There was little change in the results for practitioner versus digitally delivered interventions. The effect estimate for the comparison of practitioner delivered intervention versus assessment‐only control was larger in the sensitivity analysis (−32 g/wk, 95% CI, −43 to −21, compared to −25 g/wk, 95% CI, −34 to −16 including all studies). The effect estimate for digitally delivered interventions versus assessment only control was similar, but against minimal alcohol information group the effect was reduced (−13 g/wk, 95% CI, −28 to 2, compared to −22 g/wk, 95% CI, −33 to −11 including all studies).
Strength of evidence
One of the major concerns across this evidence is heterogeneity; all comparisons were downgraded to account for this within the CINeMA tool. The comparison of digitally delivered intervention versus minimal alcohol information was additionally downgraded because more than half of the individual studies were at overall high risk of bias. The evidence presented here is graded ‘moderate’ for all comparisons except digitally delivered interventions versus minimal alcohol information, which is graded ‘low’. The evidence surrounding practitioner delivered interventions compared to assessment only or minimal alcohol information is stronger than for digitally delivered interventions.
DISCUSSION
Summary of evidence
This review provides the first combined synthesis using NMA of trials of practitioner versus digitally delivered brief alcohol interventions aiming to help people reduce hazardous or harmful alcohol consumption. The findings suggest that, on average, practitioner delivered interventions reduced weekly consumption more than digitally delivered interventions 1 and 6 months after the intervention was received, with less evidence of a difference after 1 year. Further, practitioner delivered interventions provided a stronger effect to at least 6 months and were most effective at early follow‐up, whereas the effect of digitally delivered interventions appeared more consistent over time, but evidence for an intervention effect was weaker. By 12 months there was little evidence of difference between practitioner and digitally delivered interventions. However, relatively few practitioner trials reported at 1 month, whereas relatively few digital trials reported at 12 months. Effect sizes were small compared to the baseline consumption of some participants, but given the prevalence of hazardous or harmful drinking (20%–33% in the United Kingdom), even small individual reductions in alcohol consumption could have a large, positive effect at a population level.
These trials provided no evidence of difference in the number of binge drinking episodes between practitioner and digitally delivered interventions, nor of a difference in consumption between control group participants who received alcohol‐related information compared to assessment only.
The trials synthesised in this review recruited over 94 000 participants in 24 mainly high‐income countries. Over time, trials have been more likely to take place in lower‐ and middle‐income countries; all of these showed different strengths of evidence of a reduction in consumption in the intervention group compared to control. More recent trials have been more likely to target students, younger people and women. Whereas older trials were more likely to be delivered in healthcare settings, they are now more likely in occupational, college and community‐based settings.
Most trials (94%) demonstrated a within‐group reduction in consumption in intervention groups (albeit not always statistically significant compared to control groups). Often the reduction in consumption took place in both arms, meaning there was no evidence of difference in consumption between groups. One possible explanation for this is assessment reactivity, where the act of focusing on alcohol consumption at baseline assessment changes it regardless of intervention. Another is regression to the mean, where more extreme measures of behaviour tend to become less extreme over time. The screening cut‐off in these trials means that higher baseline consumption will likely be observed to reduce, but those with lower baseline consumption who would likely have increased to their mean value will have been screened out of the trial. However, over time baseline consumption cut‐off values have decreased, so older trials reporting higher average baseline consumption are more likely to subject to regression to the mean than recent ones.
The findings of this NMA are similar to those of two previous systematic reviews that compared practitioner versus digitally delivered interventions through pair‐wise meta‐analysis [12, 13]. One concluded that ‘face‐to‐face interventions’ were favoured over computer delivered interventions in college students where trials compared them directly, and the effects of face‐to‐face interventions on quantity consumed lasted for at least a year [12]. The other included interventions providing personalised feedback and reported that although there were no short term differences in any outcome, after 4 months ‘in‐person feedback interventions’ were more effective at reducing drinking quantity [13].
This review did not consider blended (guided) interventions, which comprise a computer delivered intervention with integrated human support. The aim of this review was to provide a comparative assessment of practitioner versus computer delivered interventions; the evaluation of a single intervention comprising both cannot answer this question. However, published evidence suggests that blended interventions may be more effective than ‘self‐help’ computer delivered interventions [28, 29].
Few included trials have reported since the coronavirus disease (COVID)‐19 pandemic began, but digital and remote delivery of healthcare has become more common to allow people to maintain distance. Digitally delivered alcohol interventions save person‐time compared to practitioner delivered, which is extremely advantageous as health services work to reduce backlogs of ‘normal’ care built up during the pandemic. However, although some have embraced remote health care and use the internet more, others have not, and organisations have called for non‐digital options to remain available for those who wish to use them [30, 31].
Strengths and limitations
This review followed robust review methods and was reported according to PRISMA‐NMA [14, 17]. The updated searches were completed in April 2020. Using four published systematic reviews that assessed alcohol interventions across settings to identify eligible studies published before 2016 may have missed studies. However, given the largely consistent direction of effect in the 201 included studies in this review, further work should focus on exploring components of interventions to inform who might benefit most in which contexts, rather than adding more trials to this analysis.
This review suffered from common limitations of trials of behaviour change interventions. Outcomes comprising self‐reported alcohol consumption can be susceptible to ‘social desirability’ bias, where people are likely to under‐report their consumption to a more ‘acceptable’ level. However, this may affect both arms of trials and may be less critical for reporting alcohol consumption than other behaviours [32] and is less likely to be an issue for digitally delivered interventions because there is often no human contact. It is difficult to blind either participants or (practitioner) providers to a behaviour change intervention, although provider blinding is unlikely to cause bias when trials of digital interventions are conducted online. Finally, it was expected at the beginning of the project that there would be a large amount of heterogeneity in the interventions [4, 5], but including them in a single analysis for an overall comparison is necessary to inform policy. All studies recruited non‐treatment seeking individuals living in the community with hazardous or harmful consumption, and all trials targeted consumption. Nevertheless, there were a range of population characteristics and interventions, which changed over the 35 years since the first included trial with shifting views about alcohol‐related harm and what constitutes hazardous drinking. No statistically significant inconsistency between direct and indirect evidence was found at 1 and 12 months, although the test may be underpowered. Inconsistency was found across much of the 6‐month analysis (although not in the practitioner delivered vs digitally delivered comparison).
The large variety in consumption outcomes meant that only 50% of studies could contribute to the NMA. The core outcome set developed in the ORBITAL project should be used in future trials to aid synthesis [33, 34].
Implications for policy and practice
The results of this review suggest that practitioner delivered alcohol interventions are most effective to reduce weekly consumption, particularly for the first 6 months after intervention. Digitally delivered interventions are also effective compared to alcohol‐related advice or assessment only, and by 12 months following treatment, they show a similar impact on consumption to practitioner delivered interventions (although omitting studies at higher risk of bias suggests less of an effect for digitally delivered interventions). Where it is impossible to provide a practitioner delivered intervention, or a person expresses a preference for a digitally delivered intervention, this work suggests that digitally delivered interventions could be offered as standard. They could be used to deliver input for many people simultaneously (e.g. in the workplace) or may ‘top up’ a practitioner delivered intervention. They could also provide one element of a social prescribing offer, where people can be referred to a link worker addressing their needs in a holistic way [35]. Further work should explore the active components of interventions and whether there are differences according to participant characteristics or their context.
DECLARATION OF INTERESTS
F.R.B., R.P.W.K., E.J., D.M.C., S.R., J.S., C.A., D.C. and M.H. declare no conflicts of interest.
C.G. and S.M. were involved with developing and evaluating the Drink Less app. E.F.S.K. was involved with developing and evaluating the AESOPS, SIPS and Lock trials.
AUTHOR CONTRIBUTIONS
Fiona R. Beyer: Conceptualization, data curation, formal analysis, funding acquisition, investigation, methodology, project administration, software, validation, visualization. Ryan P. W. Kenny: Formal analysis, investigation, methodology, software, validation. Eugenie Johnson: Investigation; project administration; validation. Debora Caldwell: Conceptualization, formal analysis, funding acquisition, methodology, supervision. Claire Garnett: Investigation; methodology. Stephen Rice: Conceptualization; formal analysis; funding acquisition; methodology; supervision. Julija Simpson: Investigation. Colin Angus: Conceptualization; funding acquisition; methodology; supervision. Dawn Craig: Conceptualization; formal analysis; funding acquisition; methodology; supervision. Matt Hickman: Conceptualization, funding acquisition, methodology, supervision, writing original draft, writing review and editing. Susan Michie: Conceptualization; funding acquisition; methodology; supervision. Eileen F. S. Kaner: Conceptualization, funding acquisition, investigation, methodology, supervision.
Supporting information
Figure S1 Simplified network diagram demonstrating a loop of evidence
Figure S2 Loop specific approach to assessing inconsistency
Figure S3 Characteristics of participants and settings over time
Table S1 Sources of eligible studies
Table S2 Search strategy for practitioner delivered review on MEDLINE (OVID)
Table S3 Search strategy for digitally delivered review on MEDLINE (OVID)
Table S4 Characteristics of included studies
Table S5 Reasons for excluding studies
Table S6 Risk of bias assessments for individual included studies
Table S7 Effect estimates from pairwise and network meta‐analyses for grams/week at 1 month
Table S8 Effect estimates from pairwise and network meta‐analyses for number of binge drinking episodes/month at 1 month
Table S9 Effect estimates from pairwise and network meta‐analyses for grams/week at 6 months
Table S10 Effect estimates from pairwise and network meta‐analyses for binge drinking episodes/month at 6 months
Table S11 Effect estimates from pairwise and network meta‐analyses for grams/week at 12 months
Table S12 Effect estimates from pairwise and network meta‐analyses for binge drinking episodes/month at 12 months
ACKNOWLEDGEMENTS
This work was funded by the National Institute for Health and Care Research (NIHR) School for Public Health Research (project reference SPHR‐FUS‐PH105‐ENG).
C.G. is supported by NIHR and Cancer Research UK (CRUK).
E.F.S.K. is supported by an NIHR Senior Investigator award and is director of the NIHR ARC North East and North Cumbria.
The authors acknowledge the following: Clive Henn and Don Lavoie provided useful advice and discussion from a policy perspective; Phyllis Nwadike helped with screening of results; James Faraday checked some of the data extraction; PPI colleagues Sandy Harvey and Lois Neal helped to develop the protocol and with interpretation and dissemination and Janice Armstrong provided valuable administrative support.
Beyer FR, Kenny RPW, Johnson E, Caldwell DM, Garnett C, Rice S, et al. Practitioner and digitally delivered interventions for reducing hazardous and harmful alcohol consumption in people not seeking alcohol treatment: a systematic review and network meta‐analysis. Addiction. 2023;118(1):17–29. 10.1111/add.15999
Funding information NIHR School for Public Health Research, Grant/Award Number: SPHR‐FUS‐PH105‐ENG
REFERENCES
- 1. World Health Organization . Global status report on alcohol and health 2018 World Health Organization; 2019. [Google Scholar]
- 2. Vos T, Lim SS, Abbafati C, Abbas KM, Abbasi M, Abbasifard M, et al. Global burden of 369 diseases and injuries in 204 countries and territories, 1990‐2019: A systematic analysis for the global burden of disease study 2019. Lancet. 2020;396(10258):1204–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. O'Donnell A, Anderson P, Newbury‐Birch D, Schulte B, Schmidt C, Reimer J, et al. The impact of brief alcohol interventions in primary healthcare: A systematic review of reviews. Alcohol Alcohol. 2014;49(1):66–78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Kaner EFS, Beyer FR, Muirhead C, Campbell F, Pienaar ED, Bertholet N, et al. Effectiveness of brief alcohol interventions in primary care populations. Cochrane Database Syst Rev. 2018;(2):CD004148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Kaner EFS, Beyer FR, Garnett C, Crane D, Brown J, Muirhead C, et al. Personalised digital interventions for reducing hazardous and harmful alcohol consumption in community‐dwelling populations. Cochrane Database Syst Rev. 2017;(9):CD011479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Zhang D‐X, Li ST‐S, Lee QK‐Y, Chan KH‐S, Kim JH, Yip BH‐K, et al. Systematic review of guidelines on managing patients with harmful use of alcohol in primary healthcare settings. Alcohol Alcohol. 2017;52(5):595–609. [DOI] [PubMed] [Google Scholar]
- 7. Field M, Campbell F, Hock E, Wong R. Digital interventions to reduce alcohol‐related harm: a rapid horizon scanning review. 2019.
- 8. Smedslund G, Nilsen W, Wollscheid S, Steiro A, Fang L, Larun L. Effects of computerized interventions on risky alcohol use among youth: Systematic review. Res Soc Work Pract. 2019;29(7):731–40. [Google Scholar]
- 9. Barata IA, Shandro JR, Montgomery M, Polansky R, Sachs CJ, Duber HC, et al. Effectiveness of SBIRT for alcohol use disorders in the emergency department: A systematic review. West J Emerg Med. 2017;18(6):1143–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Joseph J, Basu D. Efficacy of brief interventions in reducing hazardous or harmful alcohol use in middle‐income countries: Systematic review of randomized controlled trials. Alcohol Alcohol. 2017;52(1):56–64. [DOI] [PubMed] [Google Scholar]
- 11. Sundström C, Blankers M, Khadjesari Z. Computer‐based interventions for problematic alcohol use: A review of systematic reviews. Int J Behav Med. 2017;24(5):646–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Carey KB, Scott‐Sheldon LAJ, Elliott JC, Garey L, Carey MP. Face‐to‐face versus computer‐delivered alcohol interventions for college drinkers: A meta‐analytic review, 1998 to 2010. Clin Psychol Rev. 2012;32(8):690–703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Cadigan JM, Haeny AM, Martens MP, Weaver CC, Takamatsu SK, Arterberry BJ. Personalized drinking feedback: A meta‐analysis of in‐person versus computer‐delivered interventions. J Consult Clin Psychol. 2015;83(2):430–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Chaimani A, Caldwell DM, Li T, Higgins JPT, Salanti G. Chapter 11: Undertaking network meta‐analyses. In: Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, et al., editorsCochrane Handbook for Systematic Reviews of Interventions version 62 (updated February 2021) Cochrane; 2021. [Google Scholar]
- 15. Aycock DM, Hayat MJ, Helvig A, Dunbar SB, Clark PC. Essential considerations in developing attention control groups in behavioral research. Res Nurs Health. 2018;41(3):320–8. [DOI] [PubMed] [Google Scholar]
- 16. Caldwell DM, Davies SR, Hetrick SE, Palmer JC, Caro P, López‐López JA, et al. School‐based interventions to prevent anxiety and depression in children and young people: A systematic review and network meta‐analysis. Lancet Psychiatry. 2019;6(12):1011–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Hutton B, Salanti G, Caldwell DM, Chaimani A, Schmid CH, Cameron C, et al. The PRISMA extension statement for reporting of systematic reviews incorporating network meta‐analyses of health care interventions: Checklist and explanations. Ann Intern Med. 2015;162(11):777–84. [DOI] [PubMed] [Google Scholar]
- 18. Plotnikoff RC, Costigan SA, Kennedy SG, Robards SL, Germov J, Wild C. Efficacy of interventions targeting alcohol, drug and smoking behaviors in university and college students: A review of randomized controlled trials. J am Coll Health. 2019;67(1):68–84. [DOI] [PubMed] [Google Scholar]
- 19. Hennessy EA, Tanner‐Smith EE, Mavridis D, Grant SP. Comparative effectiveness of brief alcohol interventions for college students: Results from a network meta‐analysis. Prev Sci. 2019;20(5):715–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Yuvaraj K, Eliyas SK, Gokul S, Manikandanesan S. Effectiveness of workplace intervention for reducing alcohol consumption: A systematic review and meta‐analysis. Alcohol Alcohol. 2019;54(3):264–71. [DOI] [PubMed] [Google Scholar]
- 21. Ouzzani M, Hammady H, Fedorowicz Z, Elmagarmid A. Rayyan—A web and mobile app for systematic reviews. Syst Rev. 2016;5(1):1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. McGuinness LA, Higgins JPT. Risk‐of‐bias VISualization (robvis): An R package and shiny web app for visualizing risk‐of‐bias assessments. Res Synth Methods. 2020;12(1):55–61. [DOI] [PubMed] [Google Scholar]
- 23. Lock CA, Kaner E, Heather N, Doughty J, Crawshaw A, McNamee P, et al. Effectiveness of nurse‐led brief alcohol intervention: A cluster randomized controlled trial. J Adv Nurs. 2006;54:426–39. [DOI] [PubMed] [Google Scholar]
- 24. Dias S, Welton NJ, Caldwell DM, Ades AE. Checking consistency in mixed treatment comparison meta‐analysis. Stat Med. 2010;29(7–8):932–44. [DOI] [PubMed] [Google Scholar]
- 25. Higgins JPT, Jackson D, Barrett JK, Lu G, Ades AE, White IR. Consistency and inconsistency in network meta‐analysis: Concepts and models for multi‐arm studies. Res Synth Methods. 2012;3(2):98–110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. White IR. Network meta‐analysis. Stata J. 2015;15(4):951–85. [Google Scholar]
- 27. Nikolakopoulou A, Higgins JPT, Papakonstantinou T, Chaimani A, Del Giovane C, Egger M, et al. CINeMA: An approach for assessing confidence in the results of a network meta‐analysis. PLoS Med. 2020;17(4):e1003082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Riper H, Blankers M, Hadiwijaya H, Cunningham J, Clarke S, Wiers R, et al. Effectiveness of guided and unguided low‐intensity internet interventions for adult alcohol misuse: A Meta‐analysis. PLoS ONE. 2014;9(6):e99912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Riper H, Hoogendoorn A, Cuijpers P, Karyotaki E, Boumparis N, Mira A, et al. Effectiveness and treatment moderators of internet interventions for adult problem drinking: An individual patient data meta‐analysis of 19 randomised controlled trials. PLoS Med. 2018;15(12):e1002714‐e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Age UK. Digital inclusion and older people – how have things changed in a Covid‐19 world? London; 2021.
- 31. Healthwatch . Locked out: Digitally excluded people's experiences of remote GP appointments. Newcastle upon Tyne; 2021.
- 32. Kypri K, Wilson A, Attia J, Sheeran P, Miller P, McCambridge J. Social desirability bias in the reporting of alcohol consumption: A randomized trial. J Stud Alcohol Drugs. 2016;77(3):526–31. [DOI] [PubMed] [Google Scholar]
- 33. Shorter GW, Bray JW, Giles EL, O'Donnell AJ, Berman AH, Holloway A, et al. The variability of outcomes used in efficacy and effectiveness trials of alcohol brief interventions: A systematic review. J Stud Alcohol Drugs. 2019;80(3):286–98. [PubMed] [Google Scholar]
- 34. Shorter GW, Bray JW, Heather N, Berman AH, Giles EL, Clarke M, et al. The “outcome reporting in brief intervention trials: Alcohol” (ORBITAL) core outcome set: International consensus on outcomes to measure in efficacy and effectiveness trials of alcohol brief interventions. J Stud Alcohol Drugs. 2021;82(5):638–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. NHS England . Social prescribing and community‐based support: Summary guide London: NHS England; 2019. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Figure S1 Simplified network diagram demonstrating a loop of evidence
Figure S2 Loop specific approach to assessing inconsistency
Figure S3 Characteristics of participants and settings over time
Table S1 Sources of eligible studies
Table S2 Search strategy for practitioner delivered review on MEDLINE (OVID)
Table S3 Search strategy for digitally delivered review on MEDLINE (OVID)
Table S4 Characteristics of included studies
Table S5 Reasons for excluding studies
Table S6 Risk of bias assessments for individual included studies
Table S7 Effect estimates from pairwise and network meta‐analyses for grams/week at 1 month
Table S8 Effect estimates from pairwise and network meta‐analyses for number of binge drinking episodes/month at 1 month
Table S9 Effect estimates from pairwise and network meta‐analyses for grams/week at 6 months
Table S10 Effect estimates from pairwise and network meta‐analyses for binge drinking episodes/month at 6 months
Table S11 Effect estimates from pairwise and network meta‐analyses for grams/week at 12 months
Table S12 Effect estimates from pairwise and network meta‐analyses for binge drinking episodes/month at 12 months


