Abstract
Background
Since 1997, tuition has more than doubled at Ontario medical schools but has remained relatively stable in other Canadian provinces. We sought to determine whether the increasing tuition fees in Ontario affected the demographic characteristics and financial outlook of medical students in that province as compared with those of medical students in the rest of Canada.
Methods
As part of a larger Internet survey of all students at Canadian medical schools outside Quebec, conducted in January and February 2001, we compared the respondents from Ontario schools with those from the other schools (control group). Respondents were asked about their age, sex, self-reported family income (as a direct indicator of socioeconomic status), the first 3 digits of their postal code at graduation from high school (as an indirect indicator of socioeconomic status), and importance of financial considerations in choosing a specialty and location of practice. We used logistic regression models to see if temporal changes (1997 v. 2000) among Ontario medical students differed from those among medical students elsewhere in Canada apart from Quebec.
Results
Responses were obtained from 2994 (68.5%) of 4368 medical students. Across the medical schools, there was an increase in self-reported family income between 1997 and 2000 (p = 0.03). In Ontario, the proportion of respondents with a family income of less than $40 000 declined from 22.6% to 15.0%. However, compared with the control respondents, the overall rise in family income among Ontario students was not statistically significant. First-year Ontario students reported higher levels of expected debt at graduation than did graduating students (median $80 000 v. $57 000) (p < 0.001), and the proportion of students expecting to graduate with debt of at least $100 000 more than doubled. Neither of these differences was observed in the control group. First-year Ontario students were also more likely than fourth-year Ontario students to report that their financial situation was “very” or “extremely” stressful and to cite financial considerations as having a major influence on specialty choice or practice location. These differences were not observed in the control group.
Interpretation
At Canadian medical schools, there are fewer students from low-income families in general. However, Ontario medical students report a large increase in expected debt on graduation, an increased consideration of finances in deciding what or where to practise, and increasing financial stress, factors that are not observed among students in other provinces.
Since 1997 all 5 Ontario medical schools have increased tuition fees dramatically. At the University of Toronto, for example, tuition nearly tripled in 3 years, from $4844 in 1997/98 to $14 000 in 2000/01. Tuition fees at other Canadian medical schools have been relatively stable (Fig. 1).
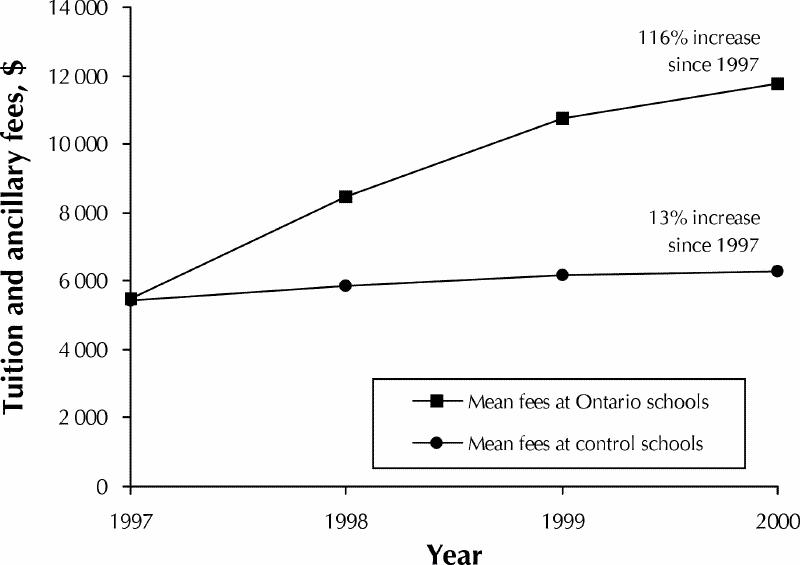
Fig. 1: Medical school tuition and ancillary fees in Ontario and elsewhere in Canada (Quebec excepted), 1997–2000. Source: Canadian Medical Education Statistics.21
The effects of increasing tuition have not been examined systematically in Canada; however, concern has been expressed that accessibility is being compromised.1,2,3 A small number of studies in the United States have investigated the effects of increasing tuition;4,5 several US commentators have also argued that high tuition may restrict access to medical education for those from low-income families, underrepresented minority groups and rural areas.6,7 Moreover, recent editorials have emphasized the advantages of a diverse, representative medical student body.8,9,10 Aside from issues of accessibility, medical student diversity may also be beneficial for pragmatic reasons. Students from underrepresented groups are more likely to treat ethnic minorities,11,12 practise in rural communities13,14 and work in socioeconomically depressed areas.15,16,17
We studied the effects of increases in tuition fees on the demographic characteristics and attitudes of medical students by comparing students in Ontario, where tuition fees increased rapidly, with students from a control group of Canadian medical schools in provinces that did not experience a rapid increase. Our main hypotheses were that the increases in fees would be associated with increases in family income and expected debt at graduation. We also hypothesized that students in Ontario who enrolled after the increase would feel more financial stress than control students and be more likely to feel that financial considerations would affect their choice of specialty or practice location.
Methods
Questionnaire design
We developed a survey to examine, among other topics, the demographic characteristics (age and sex), socioeconomic status, and financial status and related attitudes of medical students. Questions relevant to the data presented in this article are outlined below. Other aspects of this survey are described in the companion paper in this issue (page 1029).18 The survey was pretested among about 30 medical students from across the country. The pretest responses were discarded, and the pretest participants were resurveyed with the rest of the medical student population.
We used self-reported family income as a direct indicator of socioeconomic status. Since the median family income in Canada at the time of the 1996 census was $46 951,19 we used a reported family income of less than $40 000 as an indicator of low-income status. To complement the self-reported data for parental income, we also used the median income of the respondent's neighbourhood (the region defined by the first 3 digits of the postal code) in their final year of high school as an indirect indicator of socioeconomic status. We derived neighbourhood income data from responses to the 1996 census.20
Using open-ended questions, we asked students to report their debt at entry to medical school and expected debt at graduation. Students were asked to rate, on a 5-point Likert scale, the importance of financial considerations on their choice of specialty and geographic practice location (1 = not at all important, 5 = most important factor) as well as the level of stress they were experiencing as a result of their financial situation.
Survey procedure
After receiving ethics approval for the study from the Ethics Review Office at the University of Toronto, we collected email addresses from all 16 medical schools in Canada. On the basis of enrolment data from the Association of Canadian Medical Colleges,21 we estimated that we had valid email addresses for over 95% of the students enrolled at the schools under study. We then sent each student an invitation by email (with a personal identification code) to complete the questionnaire at a specific Internet site. Nonrespondents received up to 2 reminders. Student representatives at each school encouraged participation by offering draw prizes (e.g., a handheld computer) to be won by a randomly chosen respondent from each school. We conducted the survey over 7 weeks in January and February of 2001, a period chosen to avoid examinations and vacations.
Foreign students and students who did not report their year of entry to medical school were excluded from the analysis. In addition, students from the 4 medical schools in the province of Quebec were also excluded, mainly because the quality of our email address databases for the Quebec schools was poor. The databases were incomplete (e.g., we had valid email addresses for less than two-thirds of the students enrolled at the Université de Sherbrooke) and included a large number of premedical students. We discovered these problems after administering the survey but before analyzing the results. In addition, the response rates at the Quebec schools were poor (38% to 53%). Before analyzing the data, we decided to exclude Quebec students' responses because we could not be confident that the data were representative.
Analysis
Questionnaire responses were automatically compiled into a computer database. Duplicate responses and those with an invalid identification number were removed. We analyzed the data and examined frequency distributions to find evidence of irregularities in the data, which were manually recoded when possible (e.g., $50K was recoded as $50 000); nonsensical values were discarded. We used descriptive statistics to summarize responses to all questions.
We were interested in comparing changes between the 1997 and 2000 entering student groups in Ontario with corresponding changes in the control groups. To do this, we developed logistic regression models for categorical outcome variables and factorial analysis of variance for continuous outcome variables.22 We then examined the interaction term between the regional variable (Ontario v. control) and the temporal variable (1997 v. 2000) in these models to determine whether changes in Ontario were significantly different from changes observed among control students.
Results
In September 2000, 4421 medical students were enrolled at the 12 medical schools included in our study.21 Our database contained 4383 unique email addresses; 4368 of these were valid, and we received 2994 responses, for a response rate of 68.5%. After the exclusion criteria (foreign students and students who did not provide the year they matriculated) were applied, 2861 responses remained for further analysis.
Our email address database did not have information regarding when students began medical school; we relied on self-report for this information. Therefore, for each group at each school, the exact response rate could not be calculated. However, we determined lower bounds (the number of responses divided by the number of students enrolled) (Table 1). Because the denominator includes both students who received the email and those for whom we did not have a valid email address, the true response rate was slightly higher.
Table 1
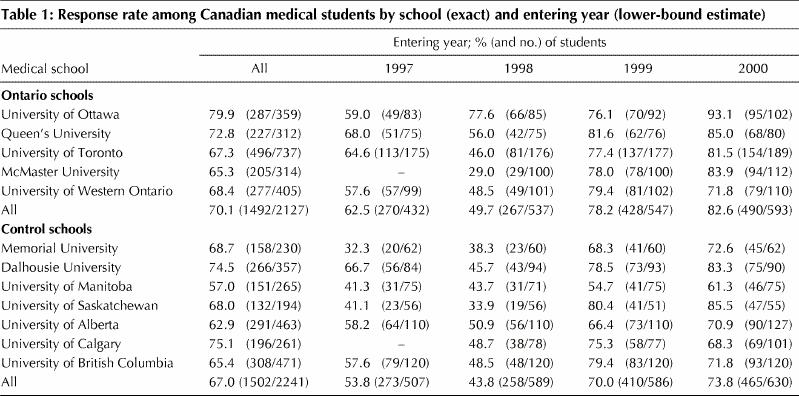
The response rates were higher for first- and second-year students than for third- and fourth-year students, and for respondents at Ontario medical schools than for respondents elsewhere (Table 1).
Demographic characteristics
The mean age (and standard deviation [SD]) at entry increased in both groups between 1997 and 2000, from 23.5 (SD 2.5) years to 24.1 (SD 2.7) years in the Ontario group and from 23.0 (SD 2.4) years to 24.0 (SD 3.0) years in the control group. The difference in the increase between the 2 groups was not significant. Slightly more respondents were female (50.6% in the Ontario group and 50.5% in the control group), but there were no temporal differences in the sex distribution.
Socioeconomic status
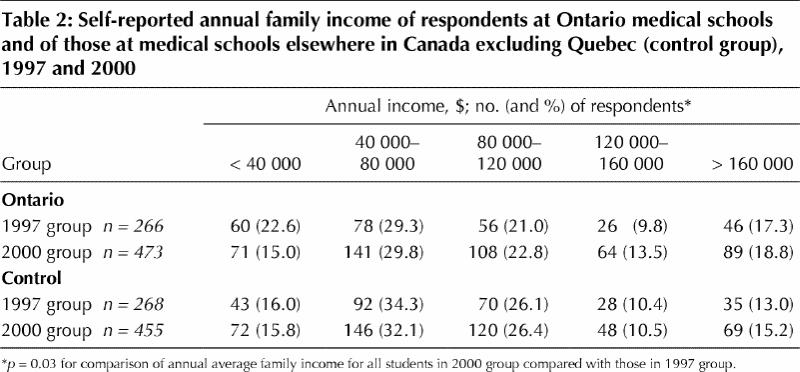
Overall, there was an increase in self-reported family income between students who entered medical school in 1997 and those who entered school in 2000 (p = 0.03). This appears to have been most true in Ontario, where, for example, the number of respondents with a family income of less than $40 000 declined from 22.6% to 15.0% (Table 2). The decline was not statistically significant (p = 0.22), which implies that the change in family income in Ontario did not differ significantly from that seen in the control group.
Table 2
The mean neighbourhood income for medical students in Ontario was significantly higher than that for the students at the control schools ($58 374 v. $52 805) (p < 0.001); there were no discernible temporal trends in either group. The correlation between neighbourhood income and self-reported family income in our sample was low (r = 0.26).
Financial status and related attitudes
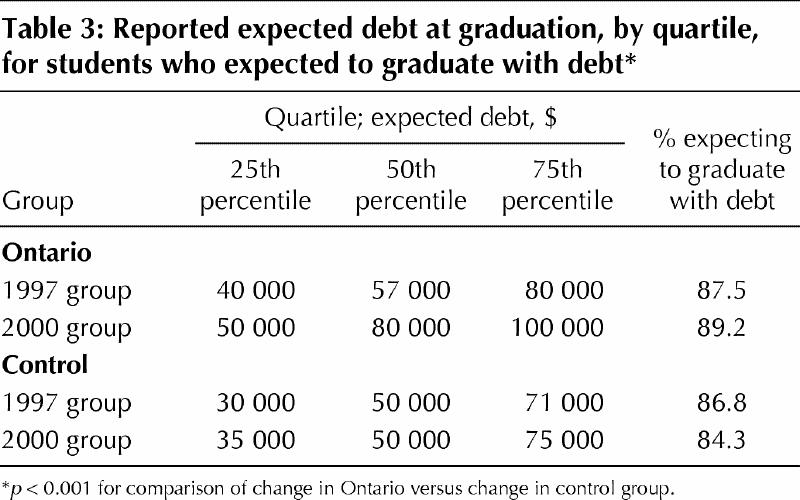
Over 85% of the medical students surveyed expected to have a debt on graduation. In Ontario, 87.5% of the students who entered medical school in 1997 expected to have a debt, as compared with 89.2% of those who entered in 2000. The reverse pattern was seen among the students at the control schools (86.8% in 1997 and 84.3% in 2000). Among those who expected to graduate with debt, the expected amount of debt was much higher for students who entered an Ontario medical school in 2000 than for those who entered in 1997 (Table 3). No increase was observed among the control students, and the interaction term was highly significant (p < 0.001), which suggests that the change in expected debt is significantly larger among the Ontario students than among the control students. Students' debt levels at entry to medical school were similar between the 2 groups for each group (data not shown).
Table 3
Almost twice as many first-year students (25.4%) as fourth-year students (13.3%) in Ontario felt that financial considerations would be a major influence on their choice of specialty (i.e., 4 or 5 on the 5-point scale); there was a difference between first- and fourth-year students in the control group, although it was not large (Table 4). The observed change among the Ontario respondents was significantly different from that observed among the control respondents (p < 0.001).
Table 4
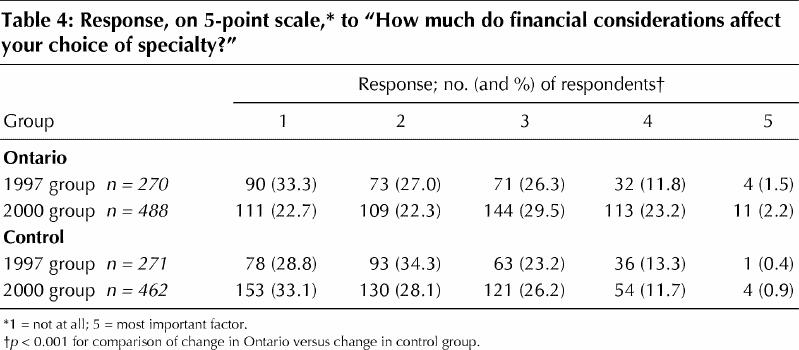
In Ontario, respondents who started medical school in 2000 were more likely than those who started in 1997 to report that financial considerations would be a major influence on chosen practice location (28.5% v. 21.2%). In contrast, in the control group, the respondents who started medical school in 2000 were less likely than those who started in 1997 to agree that financial considerations would affect their choice of practice location (21.4% v. 26.0%). The temporal changes seen for Ontario schools differed significantly from those seen for the control schools (p < 0.001).
First-year Ontario respondents were more likely than fourth-year respondents to report that their financial situation was “very” or “extremely” stressful (20.5% v. 17.5%). The opposite result was found in the control group (11.9% of first-year students v. 15.8% of fourth-year students). Again, the temporal changes seen for Ontario schools differed significantly from those seen for the control schools (p = 0.01).
Interpretation
We found that as tuition fees increased in Ontario, the proportion of students from families with incomes less than $40 000 decreased from 22.6% to 15.0%. The corresponding decrease in the control group was much smaller (from 16.0% to 15.8%). However, the change in Ontarians' family incomes was not statistically significant when compared to the change in family incomes of the control students. Our finding is in concordance with older US data, which showed that, as tuition fees rose in the 1970s and 1980s, the socioeconomic status of students enrolling in medical school increased.4,23 A 1965 study also showed that, of 4 medical schools, the school with the lowest fees attracted the greatest number of students with a low socioeconomic status.24 No published Canadian data exist for comparison. The effect associated with increased tuition fees may have been relatively small and nonsignificant for at least 2 reasons. First, our study population consisted mainly of students who had probably already decided to apply to medical school before the increases in tuition fees were announced. It is conceivable that the increasing fees did not deter them; the late effects of increasing fees may be more striking than the early effects described in this report. Second, as we have reported elsewhere,18 the number of medical students from low-income families is already strikingly low. Increases in tuition fees may have limited effects on an already affluent population.
At least 2 US studies have documented, over the last few decades, that debt on graduation has increased alongside medical school tuition.23,25 This trend is now apparent in Ontario. We found that the median expected debt at graduation and the number of students expecting very high debt ($100 000 or more) have increased in Ontario but not elsewhere in Canada (data for Quebec were excluded from analyses). This illustrates that debt at graduation is largely a function of tuition.
Several US investigators have attempted to elucidate the effects of debt on medical students' career choice. Most have found that debt is a small but significant influence away from a career in primary care,15,26,27,28 but others have reported no such effect.29,30 We found that, among Canadian medical students, financial considerations were reported to be much more important, in terms of specialty choice and practice location, for those at schools with high tuition fees than for the control subjects. The consequences of increases in tuition fees on physician resource distribution in the Canadian setting deserve further study.
An inverse relation between the number of applicants and tuition has been observed in the United States.31 In contrast, figures published by the Association of Canadian Medical Colleges21 reveal that the ratio of medical school applicants to Canadians aged 22 to 24 years32 increased nationally between 1997 and 2000, from 5.95 per 1000 to 6.17 per 1000, despite increased tuition fees at almost every school in the country. Interestingly, the proportion of applicants (adjusted for increases in the population aged 22 to 24) from Ontario increased more than the proportion of applicants from other provinces (7.1% v. 0.5%). Despite increases in tuition fees, medicine obviously remains a highly desirable career. Furthermore, the increase in applications to Ontario schools may reflect a perception that quality is proportionate to cost.
Our study has several limitations. Probably the most significant weakness is the inconsistent response rate (lower among students from the control schools and among senior students), which potentially introduces serious bias. An earlier Canadian study showed similar inconsistencies;33 it is likely that any voluntary survey of medical students would suffer similar problems. Another limitation is that we had to rely on self-report for socioeconomic data and could not independently verify the information provided. As well, student reports that financial considerations would affect their choice of specialty and practice location may not necessarily translate into different choices. Residency application data will need to be examined over the coming years to determine whether students from schools with high tuition fees make different choices than students from schools with low tuition fees. Finally, the exclusion of Quebec students from our control group limits the power of our study.
In summary, we found that the large increases in tuition fees implemented by medical schools in Ontario are associated with changes in the medical student population. At Ontario medical schools, there are now fewer students from lower-income families (but not statistically significantly fewer than in other provinces) and more students expecting to graduate with large debts. Ontario medical students also report that financial considerations have an increasing influence on their specialty choice and practice location. On the other hand, there has been an overall increase in the size of the applicant pool, particularly in Ontario. Because significant increases in tuition fees began in 1997, we were able to examine only the short-term effects of increased fees. People may decide to apply to medical school many years before they are eligible; further study is therefore needed to examine the long-term effects of increasing tuition fees.
β See related article page 1029
Footnotes
This article has been peer reviewed.
Contributors: Dr. Kwong and Mr. Dhalla were equally responsible for conceiving and coordinating the project, analyzing the data and drafting the manuscript. Dr. Johnson provided mentorship and guidance throughout the project and also participated in data analysis and manuscript preparation. Ms. Waddell helped design the questionnaire and methods. Dr. Streiner provided statistical expertise during questionnaire design and data analysis. Mr. Baddour was responsible for data collection. All of the authors contributed to revising the manuscript and approved the final draft.
Acknowledgments: We are grateful to Sharon Cushing and Valerie Panet-Raymond for providing French translations, to Anthony Hung, Lawrence Spero and Mike Mares for providing information technology support, to Paul Belletrutti, Herbert Brill and Jon Mandel for managing our finances, to Jason Kur and Antoine Groulx for providing institutional support through the Canadian Federation of Medical Students and the Fédération des associations étudiantes en médecine du Québec respectively, to Sam Bederman for providing statistical advice, to Liane Kealey and Dale Yeatman of the Association of Canadian Medical Colleges for providing us with the most recent applicant data, and to Jacalyn Duffin and David Naylor for reviewing the original proposal and providing helpful comments. We are also indebted to all the Canadian Federation of Medical Students' school representatives, without whom we would have been unable to complete this study.
This research was supported financially by the Canadian Federation of Medical Students; the Canadian Medical Association; the College of Family Physicians of Canada; the Medical Undergraduate Society of the University of British Columbia; the Professional Association of Residents of British Columbia; the Calgary Medical Students' Association; the University of Calgary Students' Union; the Alberta Medical Association; the Professional Association of Residents of Alberta; the University of Saskatchewan Student Medical Society; the Saskatchewan Medical Association; the Manitoba Medical Students' Association; the Hippocratic Council of the University of Western Ontario; the McMaster Medical Student Council; the Dean's Office, Faculty of Medicine, University of Toronto; the University of Toronto's Medical Alumni Association, Students' Administrative Council and Medical Society; the Aesculapian Society of Queen's University; the Aesculapian Society of the University of Ottawa; the Student Federation of the University of Ottawa; the Ontario Medical Association; the Professional Association of Internes and Residents of Ontario; the College of Physicians and Surgeons of New Brunswick; the Dalhousie Medical Students Society; the Medical Students' Society of Memorial University of Newfoundland; the Newfoundland and Labrador Medical Association; and the Professional Association of Residents in the Maritime Provinces.
Competing interests: None declared.
Correspondence to: Dr. Ian L. Johnson, Rm. 4017, McMurrich Building, 12 Queen's Park Cres. W, University of Toronto, Toronto ON M5S 1A8; ian.johnson@utoronto.ca
References
- 1.Sibbald B. Rising tuition fees a nightmare for many medical students. CMAJ 1998;159:553.
- 2.Theodorou M. The soaring cost of medical education in Ontario. Ont Med Rev 1996;June:50-2.
- 3.Duffin J. What goes around comes around: a history of medical tuition. CMAJ 2001;164(1):50-6. Available: www.cmaj.ca/cgi/content/full/164/1/50 [PMC free article] [PubMed]
- 4.Gordon TL. Study of US medical school applicants, 1977–78. J Med Educ 1979;54:677-702. [PubMed]
- 5.Ayers WR, Stangert AC, Dennis MJ, Henry JB. Impact of high tuition of medical school applicants and enrolees. J Med Educ 1981;56:795-802. [DOI] [PubMed]
- 6.Magnus SA, Mick SS. Medical schools, affirmative action, and the neglected role of social class. Am J Public Health 2000;90:1197-201. [DOI] [PMC free article] [PubMed]
- 7.Petersdorf RG. Financing medical education. Acad Med 1991;66:61-5. [DOI] [PubMed]
- 8.Burrow GN. Medical student diversity — Elective or required? Acad Med 1998;73:1052-3. [DOI] [PubMed]
- 9.Bergen SS. Underrepresented minorities in medicine. JAMA 2000;284:1138-9. [DOI] [PubMed]
- 10.Affirmative action [editorial]. Lancet 1999;353:1. [PubMed]
- 11.Tookenay VF. Improving the health status of aboriginal people in Canada: new directions, new responsibilities. CMAJ 1996;155(11):1581-3. [PMC free article] [PubMed]
- 12.Komaromy M, Grumbach K, Drake M, Vranizan K, Lurie N, Keane D, et al. The role of black and Hispanic physicians in providing health care for underserved populations. N Engl J Med 1996;334:1305-10. [DOI] [PubMed]
- 13.Kassebaum DG, Szenas PL. Rural sources of medical students, and graduates' choice of rural practice. Acad Med 1993;68:232-6. [DOI] [PubMed]
- 14.Easterbrook M, Godwin M, Wilson R, Hodgetts G, Brown G, Pong R, et al. Rural background and clinical rural rotations during medical training: effect on practice location. CMAJ 1999;160(8):1159-63. [PMC free article] [PubMed]
- 15.Dial TH, Elliott PR. Relationship of scholarships and indebtedness to medical students' career plans. J Med Educ 1987;62:316-24. [DOI] [PubMed]
- 16.Cantor JC, Miles EL, Baker DC, Baker LC. Physician service to the underserved. Inquiry 1996;33:167-80. [PubMed]
- 17.Rabinowitz HK, Diamond JJ, Veloski JJ, Gayle JA. The impact of multiple predictors on generalist physicians' care of underserved populations. Am J Public Health 2000;90:1225-8. [DOI] [PMC free article] [PubMed]
- 18.Dhalla IA, Kwong JC, Streiner DL, Baddour RE, Waddell AE, Johnson IL. Characteristics of first-year students in Canadian medical schools. CMAJ 2002;166(8):1029-35. Available: www.cmaj.ca/cgi/content/full/166/8/1029 [PMC free article] [PubMed]
- 19.1996 Census of Canada: profile series data: forward sortation area. Ottawa: Statistics Canada. Cat no 95F0184XDB.
- 20.1996 Census of Canada: nation series data: sources of income, earnings and total income, and family income. Ottawa: Statistics Canada. Cat no 93F0029XDB96007.
- 21.Canadian medical education statistics. Vol 23. Ottawa: Association of Canadian Medical Colleges; 2001. p. 11-2.
- 22.Tabachnick BG, Fidell LS. Using multivariate statistics. 4th ed. Toronto: Allyn and Bacon; 2001. p. 40-4, 517-81.
- 23.Kassebaum DG, Szenas PL, Schuchert MK. On rising medical student debt: in for a penny, in for a pound. Acad Med 1996;71:1124-34. [DOI] [PubMed]
- 24.Rosinski EF. Social class of medical students. A look at an untapped pool of possible medical school applicants. JAMA 1965;193:95-8. [DOI] [PubMed]
- 25.Jolly P, Jolin L, Krakower JY, Beran R. Financing medical education, 1989–1990. Acad Med 1991;66:563-76. [PubMed]
- 26.Bazzoli GJ. Medical education indebtedness: Does it affect physician specialty choice? Health Aff (Millwood) 1985;4:98-104. [DOI] [PubMed]
- 27.Colquitt WL, Zeh MC, Killian CD, Cultice JM. Effect of debt on U.S. medical school graduates' preferences for family medicine, general internal medicine, and general pediatrics. Acad Med 1996;71:399-411. [DOI] [PubMed]
- 28.Geertsma RH, Romano J. Relationship between expected indebtedness and career choice of medical students. J Med Educ 1986;61:555-9. [DOI] [PubMed]
- 29.Park R. Graduating medical students' debt and specialty choices. Acad Med 1990;65:485-6. [DOI] [PubMed]
- 30.French FD. The financial indebtedness of medical-school graduates. N Engl J Med 1981;304:563-5. [DOI] [PubMed]
- 31.Barzansky B, Jonas HS, Etzel SI. Educational programs in US medical schools, 1999–2000. JAMA 2000;284:1114-20. [DOI] [PubMed]
- 32.Annual demographic statistics, 2000. Ottawa: Statistics Canada; 2001. Cat no 91-213-XPB.
- 33.Fish DG, Farmer C, Nelson-Jones R. Some social characteristics of students in Canadian medical schools, 1965–66. CMAJ 1968;99:950-4. [PMC free article] [PubMed]


