Abstract
Aims
Commencing university presents particular challenges for young adults with diabetes. This integrative literature review aimed to synthesise the research exploring the experiences and support needs of university students with diabetes.
Methods
Medline, CINAHL, PsychInfo and EMBASE databases were searched for quantitative and qualitative studies, among undergraduate and postgraduate students with type 1 or type 2 diabetes conducted in the university setting. Two reviewers independently screened titles, abstracts and full‐text articles. Data were analysed thematically and synthesised narratively utilising the ecological model as a framework for interpreting findings and making recommendations.
Results
We identified 25 eligible papers (20 studies) utilising various methods: individual interview, focus group, survey, online forum. Four themes were identified: barriers to self‐care (e.g. lack of structure and routine); living with diabetes as a student; identity, stigma and disclosure; and strategies for managing diabetes at university. Students in the early years at university, recently diagnosed or moved away from home, reported more self‐care difficulties, yet few accessed university support services. Risky alcohol‐related behaviours, perceived stigma and reluctance to disclose diabetes inhibited optimal diabetes management.
Conclusion
Despite the heterogeneity of studies, consistent themes related to diabetes self‐care difficulties and risky behaviours were reported by young adults with diabetes transitioning to university life. No effective interventions to support students with diabetes were identified in this setting. Multilevel approaches to support students to balance the competing demands of study and diabetes self‐care are needed, particularly in the early years of university life.
Keywords: Australia, college, diabetes, review, student, university
What's new.
Young adulthood is a period of multiple life transitions.
There is a lack of information about the needs of students with diabetes at university.
This integrated review identified consistent themes in the literature. Students perceive more difficulty managing diabetes at university and may engage in risky behaviours to avoid appearing different to their peers. Multilevel intervention is needed to support students to adapt to university life.
1. INTRODUCTION
Young adulthood represents a challenging life stage for people with diabetes. Young adults are dealing with multiple transitions simultaneously, including developmental changes, increasing independence, transition to adult healthcare and university, or work, and for those who are newly diagnosed the transition from wellness to chronic illness. 1
Around 40% of school leavers in the United Kingdom and Australia start university, and others commence undergraduate or postgraduate study later. 2 , 3 The transition to university may involve independence from parents, leaving home, new relationships, experimenting with drugs and alcohol. 4 , 5 , 6 Students must learn to navigate classes and new routines, and find strategies to manage exercise, food and social activities, and for school leavers with diabetes, there is an added complexity to avoid and manage hypoglycaemia in a different environment. 1
For some young adults, managing diabetes is perceived to be harder at university than it was at school. 4 , 7 In a study from the United Kingdom, 26% of students with type 1 diabetes self‐reported a diabetes‐related hospital admission while at university, including 16% admitted for diabetic ketoacidosis (DKA) and 10% experienced severe hypoglycaemia requiring assistance. 4
Living with diabetes also impacts the social aspects of university life. A survey among first‐year college students in the United States found those with a chronic illness reported greater feelings of loneliness and lower quality of life (QoL) than their peers. 8 Most students knew no others with chronic illness, few disclosed their condition or registered with campus disability support services. Moreover, youth with chronic illnesses may be less likely to graduate from university than their peers. 9 Feeling socially isolated and unsupported may contribute to lower academic success and suboptimal health outcomes for young people with a chronic condition. 8 University support services (often referred to as disability or accessibility support) aim to minimise the impact of disability and health conditions on academic performance and outcomes, yet few students with diabetes access such support. 4
Interpersonal and self‐care concerns such as these are often reported among adolescents and young adults with diabetes. 10 , 11 However, commencing university typically coincides with new freedoms and independence, and the structures and environment may present specific barriers to self‐care. A better understanding of the unique self‐care challenges for university students with diabetes could inform appropriate strategies that enable students to achieve their health and academic goals. Primary research has explored experiences of university students with type 1 diabetes, 4 , 7 , 12 but some of these studies are small, 13 , 14 or focus on a single facet of student life. 15 , 16 Despite increasing prevalence of type 2 diabetes in young adults, few studies have considered their concerns in this setting. 15 Therefore, this literature review aimed to identify and synthesise the research to provide a comprehensive perspective of the university experience for students with diabetes and better understand their support needs while at university.
2. METHODS
An integrative literature review was undertaken to incorporate primary studies with diverse methodologies and comprehensively portray the topic, following the six‐step, systematic process described by Toronto and Remington: identify purpose and scope; systematic search using predetermined criteria; quality appraisal of selected literature; data analysis and synthesis; critical discussion; and dissemination of findings. 17
2.1. Inclusion and exclusion criteria
Included in the review were studies among undergraduate and postgraduate students diagnosed with type 1 or type 2 diabetes, reporting the student experience of living with diabetes or supportive interventions conducted in the university setting. We excluded studies not specific to diabetes, among children and adolescents, that reported only clinical outcomes or service delivery, or conducted in schools, hospitals or community settings. Limits were applied for language (English only) but not for date of publication.
2.2. Search strategy
A list of search terms was defined using a combination of subject headings, keywords and phrases and modified for each database. Following preliminary searches that included synonyms for interventions, outcomes and participant perspectives, only terms for ‘diabetes’, ‘students’ and ‘university’ were retained. For the full search strategy, see Table S1. Medline, CINAHL, Psych Info and EMBASE databases were searched 25 June 2020, and reference lists and citations of included papers checked. The Cochrane database was searched for previous reviews. The search was rerun 17 May 2022 to include the most recent publications. Search results were imported into Covidence™ database and duplicates removed. Two researchers (V.H. and T.S.) independently screened the titles and abstracts and selected full‐text articles. Discrepancies were resolved by consensus.
2.3. Quality appraisal
Study quality was appraised using the McMaster University Critical Review Forms for Quantitative Studies 18 and Qualitative Studies. 19 Two reviewers (V.H., T.S.) assessed 20% of papers independently and discussed methodological limitations. The remaining papers were assessed by one reviewer (V.H.). One author was contacted to correct data. 20
2.4. Data abstraction, analysis and synthesis
Data were extracted and recorded in an Excel spreadsheet (T.S.) which was first piloted and revised. A second reviewer (V.H.) re‐read all papers and checked data for completeness. Data were analysed and synthesised thematically, using an inductive approach described by Braun and Clark to identify patterns in the content. 21 This involved re‐reading articles, identifying initial codes, summarising and organising study results into themes and subthemes, which were re‐examined and refined iteratively. Results were reported using a narrative approach in order to present heterogeneous data in a cohesive, readable format. 17 , 21
We utilised the ecological model to guide the interpretation of results and for making recommendations to strengthen student support. 22 This model focuses on interactions between individuals and the sociocultural and physical environment, 22 and was adopted by the American College Health Association for campus health promotion. 23 We applied McLeroy et al.'s model, 24 which portrays five levels of influence on health behaviour: intrapersonal factors (e.g. demographic, psychological), interpersonal factors (e.g. family, social networks), institutional factors (e.g. rules, regulations, schedules), community factors (e.g. built environment, transport) and public policy (e.g. policies, legislation).
In this manuscript, ‘university’ includes tertiary colleges. Most studies only involved type 1, so ‘diabetes’ is used for brevity. ‘Self‐care’ encompasses health behaviours, taking responsibility for health and healthcare and managing emotions. 25
3. RESULTS
The database search located 3372 articles. No additional papers or reviews were located. After screening titles and abstracts, 137 full‐text articles were retrieved and critiqued against the inclusion and exclusion criteria. Twenty‐five articles (20 studies) were included in the review. In two cases, several papers described the same study and reported different outcomes. 12 , 26 , 27 , 28 , 29 , 30 , 31 In these instances, we nominated the earliest publications as the primary source, 12 , 30 retaining the secondary papers. The PRISMA diagram in Figure 1 shows the reasons for exclusion.
FIGURE 1.
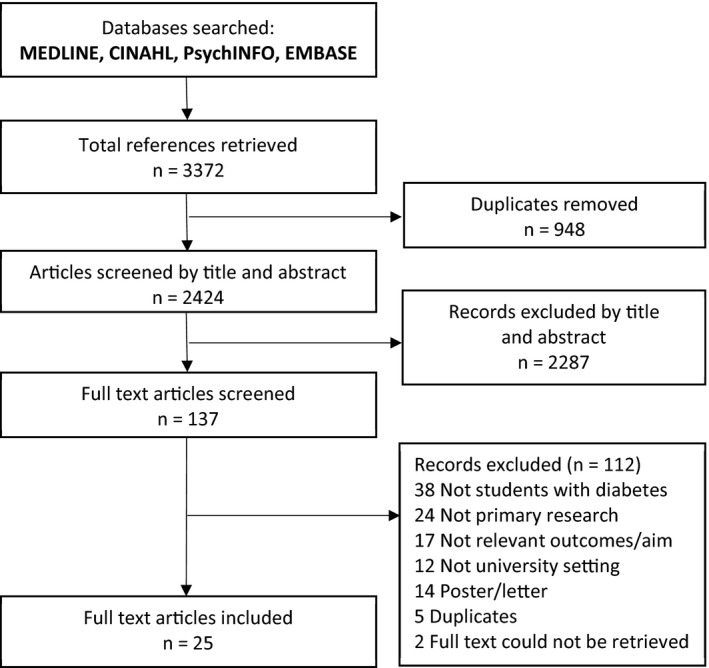
PRISMA diagram. Search results and reasons for exclusion.
3.1. Study characteristics
There were 10 qualitative studies used focus groups, 1 , 14 , 32 individual interviews 6 , 12 , 15 , 32 , 33 , 34 , 35 or online forums 36 to explore student experiences and self‐care. Nine cross‐sectional studies examined: diabetes management, 4 , 5 , 7 , 30 , 37 alcohol‐related behaviours, 16 , 30 perceived health, 20 mental health, 31 perceived stress, coping and self‐care 38 and QoL. 13 , 30 One quasi‐experimental study examined knowledge and attitudes to alcohol. 39 Fourteen studies were conducted in the United States; three in England; and one each in Ireland, Norway and Canada. Sample sizes ranged from 9 to 25 in qualitative research, and 25–584 in quantitative studies. All papers were published since 1997; 12 within the last 10 years, and seven between 10 and 25 years. Table S1 shows study details.
3.2. Recruitment
Participants were recruited through flyers or campus newsletters, 14 , 15 , 32 , 34 , 39 College Diabetes Network (CDN), 1 , 13 , 20 , 34 , 39 email 4 , 6 , 14 , 33 , 38 or mailed questionnaire, 7 medical clinics, 4 , 12 , 32 , 37 social media 39 and Diabetes UK website. 4 One study analysed publicly available online data, 36 two accessed national student health survey data 5 , 16 and one did not report recruitment method. 35
3.3. Participant characteristics
In 16 studies, participants had type 1 diabetes. 1 , 4 , 6 , 7 , 12 , 13 , 14 , 20 , 30 , 32 , 33 , 34 , 35 , 37 , 38 , 39 One included students with type 1 and type 2 diabetes 15 and the type of diabetes was unknown in three studies. 5 , 16 , 36 Most studies included undergraduate and postgraduate students, 1 , 4 , 5 , 6 , 12 , 14 , 20 , 30 , 32 , 34 , 38 , 39 ; five focused on undergraduates, 7 , 13 , 16 , 33 , 35 and in three, graduate status was not reported/unknown. 15 , 36 , 37 Participants ranged in age from 17 to 40 years, although most studies included young adults (18–30 years) and participation was typically higher among women than men. Four to 22 per cent of participants were from minority ethnic groups (where reported) (Table 1).
TABLE 1.
Table of included studies
| Author, Year | Participant characteristics | Study methods | Study aim | Themes | ||||
|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | Limitations | ||||
| Country | ||||||||
|
Balfe, 2007a; Balfe, 2007b; Balfe and Jackson, 2007; Balfe, 2009a, Balfe, 2009b England |
N = 17 T1DM 18–25 years 65% female |
Individual interviews, and 2‐week diary, follow‐up interview after 4–6 months | To explore the perceptions and practices of university students with diabetes, including alcohol, food consumption and exercise, technology use in T1DM management, body image and identity, self‐care, reasons for these practices and whether these changed over time. Data interpreted through theoretical lens of morality and discipline | x | x | x | x | Limited quotes to represent themes |
|
Bratke et al., 2020; Bratke and Sivertsen, 2021 Norway |
N = 324 T1DM 18–35 years 64% female 5% immigrants |
Cross‐sectional survey National survey university students |
To examine diabetes management and diabetes distress among university students with type 1 diabetes and compare mental and somatic health, quality of life, alcohol use and sleep disorders between students with/no diabetes | x | x | Self‐reported data representativeness | ||
|
Cockroft et al., 2019 USA |
N = 1216 students 528 with diabetes from 117 colleges 18–24 years 62% female 22% minority |
Cross‐sectional survey National college health survey data |
To compare the health behaviours of college students with diabetes to college students without diabetes |
x |
Self‐selected sample Self‐reported data Type of diabetes unknown |
|||
|
Ersig, 2019 USA |
N = 25 T1DM 18–24 years 84% female 16% minority |
Cross‐sectional survey | To explore the transition to adulthood for college students with T1D and their parents | x | x | x | Small, non‐representative sample | |
|
Fedor et al., 2017 USA |
N = 13 T1DM 18–22 years 69% female |
Individual interviews | To describe the perceptions of first‐year college students with type 1 diabetes about the effect on diabetes management of transition from living at home to living independently at college | x | x | x | x |
Limited quotes to represent themes, Transferability |
|
Fredette et al., 2016 USA |
N = 24, T1DM 18–24 years 88% female 4% minority |
Individual interviews | To (a) explore the overall QoL for emerging adults living with T1DM while attending college and (b) to identify experiences managing their condition at college that affect their quality of life | x | x | x | x |
Transferability |
|
Habenicht et al., 2021 Ireland |
N = 14, T1DM 18–28 years 50% female |
Individual interviews | To explore the concept of social support in university students and to see how this may be influenced by disclosure | x | x | x | Nil noted | |
|
Hill et al., 2013 Canada |
N = 9, T1DM >18 years 67% female |
Two focus group interviews | To examine the lived experiences of university students with T1DM to better understand the challenges of living and coping with T1DM at this life stage | x | x | x | x |
Small sample Transferability |
|
Kellett et al., 2018 England |
N = 584, T1DM 18–24 years 64% female |
Cross‐sectional survey | To investigate the experiences of university students with T1DM and to describe the impact of transition to university on diabetes care and self‐care | x | x | Self‐reported data | ||
|
Miller‐Hagan and Janas, 2002 USA |
N = 11 T1DM N = 4 T2DM 18–40 years 73% female 12% minority |
Individual interviews | To describe how college students with diabetes perceive and manage alcohol consumption | x | x | Transferability | ||
|
Ramchandani et al., 2000 USA |
N = 42, T1DM M age 21 years 64% female |
Cross‐sectional survey | To examine the self‐reported impact of different factors on overall diabetes care of college students with type 1 diabetes | x | x | x | x |
Small sample Self‐reported data Validity, reliability of survey |
|
Ravert, 2009 USA |
N = 450 Type NR 18–25 years 68% female 20% minoritiy |
Cross‐sectional survey; data from national college health survey | To examine the use of nine common alcohol management strategies among college undergraduates with diabetes to determine which strategies predicted reduced alcohol consumption and consequences | x | x | Self‐reported data | ||
|
Ravert et al., 2015 USA |
238 posts from nine social networking sites | Content analysis of online diabetes forums | To examine the experiences encountered by students with diabetes transitioning into and through college | x | x | x |
Transferability Participant characteristics unknown |
|
|
Saylor et al., 2018 USA |
N = 371, T1DM 18–30 years, Sex NR 66% general, 34% affiliated CDN members |
Cross‐sectional online survey | To examine the characteristics and health outcomes of college students with T1DM as it relates to membership involvement in a local university‐based diabetes student organisation | x |
Validity, reliability of survey Selection bias Self‐reported data Potential recall bias Error in data table (corrected) |
|||
|
Saylor et al., 2019 USA |
N = 12, T1DM <5 years 19–26 years 58% female |
Focus group CDN member event | To understand the experience of emerging adults with a relatively new T1DM diagnosis who are assimilating to college life | x | x | x | x | Transferability |
|
Thomas et al., 2021 USA |
N = 61, T1DM 74% <25 years 54% female 10% minority |
Cross‐sectional study | To examine the relationship between perceived stress, coping and self‐care | x |
Self‐reported data Small sample size Representativeness |
|||
|
Wdowik et al., 1997 USA |
N = 25 T1DM 18–35 years 68% female |
Focus groups and individual phone interviews | To identify factors that affect the ability and motivation of college students to engage in appropriate self‐care behaviours for successful management of diabetes | x | x | x | x | Limited quotes to represent themes. |
|
Wdowik et al., 2001 USA |
N = 83, T1DM M age 25 years 57% female 17% minority |
Cross‐sectional study | To develop the Diabetes College Scale (DCS) to identify predictors of diabetes self‐care | x |
Small sample Self‐reported data Missing data Limited data reported Representativeness |
|||
|
Wilson, 2010 England |
N = 23, T1DM 17–19 years 52% female |
Semi‐structured phone interviews | To explore the experiences of young people managing their type 1 diabetes at college or university | x | x | x |
No ethics approval Methods unclear |
|
|
Wisk et al., 2021 USA |
N = 122, T1DM 17–25 years 80% female 16% minority |
Pilot trial of two versions of intervention | To investigate the acceptability of a digital health intervention to reduce alcohol use risk among college students with T1D and preference for peer or medical narrator | x | x |
Unvalidated questionnaires No control group Thematic text analysis not described |
||
Note: Minority (populations): Non‐European/White. Theme 1: Barriers to self‐care at university; 2: Living with diabetes as a university student; 3: Identity, stigma and disclosure; 4: Strategies for managing diabetes at university.
Abbreviations: CDN, College Diabetes Network; NR: not reported; T1DM, type 1 diabetes; T2DM, type 2 diabetes.
3.4. Quality assessment
Among quantitative studies, potential sources of bias were representativeness, 7 , 13 , 16 , 20 , 36 , 37 , 38 small sample size (<50 participants), 7 , 13 the use of unvalidated questionnaires 20 , 39 and self‐reported data. 4 , 5 , 7 , 16 , 20 , 30 , 37 , 38 , 39 Transferability may be limited for some qualitative studies, 1 , 12 , 14 , 15 , 33 , 34 , 35 , 36 and one had fewer than 10 participants. 14 Data analysis was not well explained in two studies. 32 , 35 Refer to Table 1 for details of study limitations.
3.5. Study themes
Four major themes were identified: barriers to self‐care at university; living with diabetes as a university student; identity, stigma and disclosure; and strategies for managing diabetes at university. Table 2 lists the major themes and 18 subthemes. Figure 2 represents themes according to the Ecological model.
TABLE 2.
Study themes
| Theme/subtheme | References |
|---|---|
| Barriers to self‐care at university | |
| Lack of structure and routine | 1, 4, 7, 13, 14, 27, 29, 32, 33, 34, 35, 36 |
| Food and eating | 1, 4, 13, 14, 32, 33, 36 |
| Self‐care support | 4, 7, 14, 27, 33, 34, 35 |
| Fear of hypoglycaemia | 7, 14, 32, 35 |
| Other barriers | 1, 4, 7, 14, 30, 31, 32, 34, 37, 38 |
| Living with diabetes as a university student | |
| Alcohol and risky drinking | 5, 7, 15, 16, 26, 31, 33, 35, 39 |
| Body image | 5, 12, 26, 27, 28, 29, 30 |
| Impact on academic performance | 5, 14, 33, 34 |
| Autonomy and growth | 1, 6, 7, 34, 36 |
| Lack of diabetes awareness | 1, 6, 14, 33, 36 |
| Worry about the future | 13, 32, 34, 36 |
| Identity, stigma and disclosure | |
| Student identity | 1, 12, 14, 26, 35 |
| Diabetes stigma and telling others | 1, 6, 14, 15, 29, 32, 34 |
| Strategies for managing diabetes at university | |
| Preparing for university | 1, 4, 33, 34, 36 |
| Forward planning | 1, 14, 34, 35 |
| Obtaining support | 1, 4, 6, 7, 13, 14, 20, 32, 33, 34, 35, 36 |
| Using technology | 15, 29 |
| Alcohol management strategies | 1, 15, 16, 26, 32, 36 |
FIGURE 2.
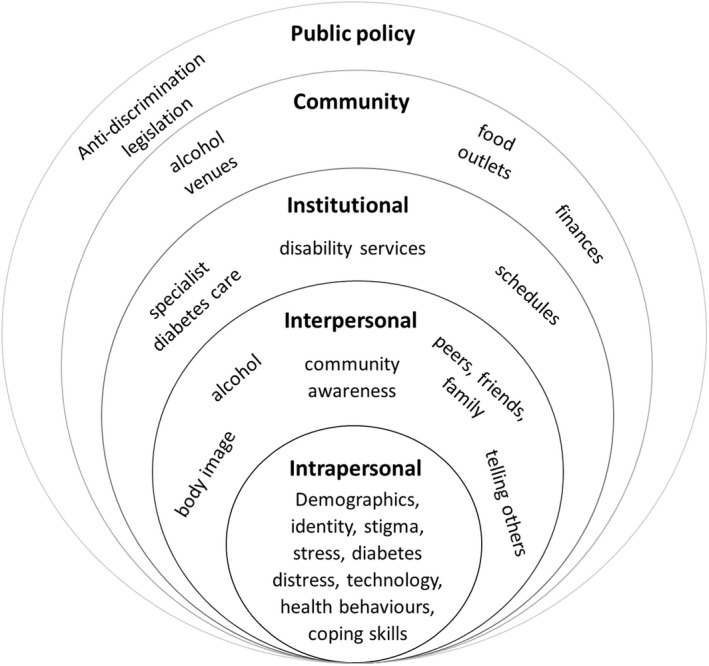
Ecological model. Adapted from McLeroy et al. 24 Factors influencing health behaviours for university students living with diabetes.
3.5.1. Barriers to self‐care at university
Managing diabetes was perceived to be more difficult at university than high school. 4 , 7 The first few months may present the greatest challenges, as students adapt to university life. 33 , 36 However, among UK students with type 1 diabetes, difficulties were not limited to younger students and women perceived more problems with diabetes self‐care than men. 4 Female students reported higher HbA1c 4 , 30 and diabetes distress than males, 31 and diabetes distress was higher among older than younger students. 31 For recently diagnosed students, learning to manage diabetes made the transition to student life more complex. 1 , 4 , 27
Lack of structure and routine
Uncertainty and lack of control over situations at university frustrated students' efforts to manage their blood glucose levels optimally. In contrast to the school environment, the lack of structure and routine, such as irregular class timetables and mealtimes, interfered with maintaining a self‐care routine. 1 , 4 , 7 , 13 , 27 , 32 , 36 Insufficient time to check blood glucose and eat between classes 35 and difficulty balancing study and diabetes resulted in some students skipping classes or blood glucose checks 34 or not testing at all. 29 Self‐care routines of first‐year students often ‘slipped’ due to staying up late, partying and studying. 27 Living in student accommodation provided some structure but moving off‐campus could be problematic for students who lacked the necessary self‐care skills. 27 Balancing study, social life and blood glucose levels was described as a constant concern, 13 , 14 , 33 with students feeling guilty when their routine and diabetes management were affected. 27 Students learnt to adapt as they progressed through university, but experienced ‘glitches’ at different times, for example, during periods of stress or exams. 27 Recently diagnosed students experienced more difficulty establishing self‐care routines in the university environment than those diagnosed at an earlier age, 1 , 4 , 27 and adapted by structuring their lives or disregarding self‐care. 27 In Kellett et al.’s study, 13% of participants were diagnosed while at university. 4 These students had more difficulty managing mealtimes, food and exercise than those diagnosed prior to university.
Food and eating
Several food‐related factors were perceived to affect self‐care. Eating patterns were altered 7 and appropriate food choices were limited on campus. 1 , 4 , 14 , 32 , 33 , 36 Nutrition information about carbohydrate content was unavailable for food in the cafeteria, limiting accurate estimation of insulin doses. 13 , 14 , 36 Take‐away food and eating out was a normal part of student life but impacted glycaemia. 36 Needing to carry food and eat in class was inconvenient. 32 Food was prohibited in some areas on campus, for example, the library, examination or laboratory rooms, resulting in students missing or leaving class to manage hypoglycaemia. 1 , 14 While some students would approach the lecturer to explain their needs, others were reluctant to draw attention to their diabetes. 14
Self‐care support
Students reported feeling less supported to care for their diabetes at university than at school. 14 They had more autonomy but lacked guidance and support from their parents, 4 , 7 , 33 , 34 particularly when living away from home. 4 , 27 Students remained with their usual diabetes care team more often than transferring to local healthcare, even when moving away from home. 4 , 33 However, being unable to travel home and clashes with university timetables were barriers to attending clinic appointments. 4 , 33 , 35 Kellett et al. found that students who transferred their medical care reported higher HbA1c, more frequent hypoglycaemia, hospital admissions and DKA than those who remained with their home specialist team. 4 Among this group, diabetes management was more likely to be impacted by alcohol, exercise and weight‐related issues. 4
Fear of hypoglycaemia
Fear of hypoglycaemia was a barrier to optimal diabetes management in four studies. 7 , 14 , 32 , 35 Hypoglycaemia or checking blood glucose might draw attention, so some students reported intentionally maintaining elevated blood glucose, 14 , 35 for example, by taking less insulin. 35
Other barriers
In four studies, students reported academic‐related stress (e.g. assessment, performance) negatively affected glycaemia. 4 , 14 , 32 , 34 Perceived general stress was associated with less frequent health behaviours (healthy eating, footcare), but positive coping skills (e.g. positive reframing, planning) predicted more frequent self‐care in one study. 38 Disturbed sleep from attending to diabetes or being woken by pump or glucose monitor alarms also impacted blood glucose levels. 1 Using a scale developed to measure attitudes and behaviours associated with diabetes self‐care at university, Widowik demonstrated that situational factors, such as social events, peers, competing priorities, stress and negative emotions, were negatively associated with self‐care. 37 Other barriers cited were finances, use of drugs and alcohol, peer pressure, disordered eating and skipping insulin. 7 Financial difficulties were also associated with high HbA1c. 30
3.5.2. Living with diabetes as a university student
Alcohol and risky drinking
Alcohol was a normal part of university life for young people and students drank at bars, clubs and parties. 15 , 26 Drinking alcohol was considered one of the main social activities at university and there was strong peer pressure to drink. 15 , 33 However, diabetes was perceived a barrier to socialising at university. The pressure to drink alcohol caused some students to avoid going out of an evening whereas others might forget diabetes and enjoy themselves. 35 Drinking alcohol enabled young people to develop their student identity and to appear ‘normal’, and when their condition was known, to appear capable and in‐control and not limited by diabetes. 26 Some students experimented with alcohol, testing the effect and their own limits. 15 Others limited drinking to maintain control of themselves, their diabetes or body weight and to avoid hypoglycaemia. 15
In three studies, students with diabetes described consuming alcohol at the same risky level as their peers without diabetes. 5 , 16 , 26 Cockroft et al. found that 70% of all students exceeded the recommended alcohol limits for age and gender and 42% engaged in binge drinking. 5 However, the students with diabetes used fewer protective strategies and were more likely to drive when drinking, and experience academic problems due to alcohol. Additionally, more students with diabetes reported treatment for substance use than those without diabetes. 5 In another study, 42% of students with diabetes reported drinking at excessive levels (≥5 in one sitting), and 37% (mostly younger students) reported one or more consequences of alcohol in the past year including injuring themselves, later regretting behaviour and forgetting what happened. 16 In contrast, fewer students with diabetes reported alcohol problems and harmful alcohol use than students without diabetes in a Norwegian cohort. 31 Students were aware that alcohol was a risk to their diabetes management, 7 , 26 , 39 future health and ability to work. 26 In one study, students had high self‐reported knowledge, but moderate concerns about the impact of alcohol on diabetes. 39
Alcohol‐induced hypoglycaemia threatened a ‘normal’ student identity and their independence if it occurred in public, but students were less anxious about hypoglycaemia occurring at home, believing they could deal with it themselves or be looked after by friends. 26 Older students transitioned to less risky drinking as their adult identities and social networks were more established and they were more cognisant of the risks to their health. 16 , 26
Body image
Students associated managing diabetes well with having a healthy body 34 and better self‐esteem. 28 In a UK study, students with type 1 diabetes perceived social pressure to maintain a slim and healthy body and control their condition through disciplined eating and exercise. 12 , 26 , 27 , 28 , 29 Men identified the desire to feel fit and healthy through sport and well‐controlled blood glucose, whereas women were concerned with body image but felt their attempts to lose weight by exercising were thwarted by hypoglycaemia. 12 Lower body weight satisfaction and unsafe weight loss strategies were more likely to be reported by students with diabetes than those without the condition. 5 Norwegian students with diabetes reported higher body mass index, 30 and lower QoL than students without diabetes, 31 but no difference in physical activity, 30 mental health, loneliness, sleep and health symptoms. 31 Some students reported adopting more healthy eating behaviours after learning about the consequences of disease in their course. 26
Impact of diabetes on academic performance
Fluctuations in blood glucose could cause fatigue and poor concentration in class, 14 difficulties completing assignments and exams and affect vision and driving. 33 , 34 Hypoglycaemia necessitated consuming food or drink to prevent or treat an episode, sometimes causing students to be late or miss classes. 33 , 34 A national college health survey in the United States found that students with diabetes had a lower grade point average (GPA) than those without diabetes and were more likely to perceive that sleep problems, disordered eating and alcohol affected their academic performance. 5
Lack of diabetes awareness
Students commented on the lack of understanding about diabetes in the community, among peers, lecturers and the media. 6 , 14 Others found peers and the public overly intrusive and offered unwelcome advice, particularly around food. 1 Some students reported neglecting self‐care in public to avoid constantly explaining their diabetes to others, 14 whereas others believed they had a responsibility to use these interactions to educate the community about diabetes. 1 University staff, including health staff, were perceived to lack knowledge about diabetes and students' needs. 33 , 36 Students felt unconfident about receiving emergency assistance for severe hypoglycaemia at university and felt less safe than at school where pupils with diabetes were well known and resources available. 14
Autonomy and growth
In six studies, students reported the positive aspects of living with diabetes. Diabetes was not perceived to deter achievement 34 and was frequently reported as a challenge that led to personal growth and maturity. 6 , 7 , 14 , 34 , 36 Going to university was an opportunity to develop independence and master diabetes self‐care, 36 and assume self‐responsibility for health. 1 In two studies, students reported optimism, enjoying life and relationships with their peers with diabetes. 1 , 34 Compassion for others was identified as an attribute of living with diabetes, 1 and some students were motivated by their condition to choose a health‐related career. 34
Worry about the future
Concerns were expressed about the impact of the student lifestyle on diabetes management and future complications. 13 , 34 , 36 As students considered life after university, they worried about gaining employment and finding a life partner that could deal with diabetes. 13 Students in the United States identified concerns about insurance and the cost of diabetes care. 13 , 32 , 36
3.5.3. Identity, stigma and disclosure
Student identity
Students described not wanting to be different to their peers or defined by diabetes. 1 , 12 , 26 They behaved in a number of ways to maintain a ‘normal’ student identity on campus, including participating in exercise, not limiting food intake, risky drinking of alcohol, 12 , 26 staying up late and partying. 1 Checking blood glucose or treating hypoglycaemia in class could be embarrassing or invite criticism. 14 Some students reported maintaining an elevated blood glucose level to avoid these situations which would draw attention to having diabetes. 14 , 26 , 35
Diabetes stigma and telling others about diabetes
Common misunderstandings and stereotypes, for example, attributing diabetes to unhealthy lifestyles, was a constant source of stress and frustration for students with type 1 diabetes, 6 , 14 and they perceived these misconceptions reduced the level of emotional support they received within social relationships. 6 Students avoided disclosing their diabetes if they anticipated a negative reaction, such as rejection or discrimination, were made to feel different, explain diabetes or receive unsolicited advice. 6 , 14 , 29 , 32 Some female students perceived stigma around using needles. 29 Older students, particularly men, were less concerned about diabetes‐related stigma and conforming to a student identity and stated they felt comfortable testing and injecting in public. 29 Habenicht et al. also found the reasons for disclosing diabetes varied by gender. 6 Despite claiming openness, some men avoided disclosure because it may elicit pity, making them feel ‘weak’, whereas women told others about their diabetes to build trusted relationships and to be responsible.
Students usually felt comfortable disclosing diabetes for safety reasons, for example, to elicit support when needed or going out, 6 , 34 and might tell others to avoid pressure to drink alcohol. 15 For some students, performing self‐care in front of others was a mean to passively disclose diabetes, which might initiate a casual conversation about the condition. 6 Sharing their diagnosis was seen as a way to educate people about diabetes. 34 Over time, most students learnt to advocate for themselves and their health in the face of peer pressure and for adjustments to manage their diabetes and study. 1
3.5.4. Strategies for managing diabetes at university
Preparing for university
Concerns for students preparing for university included access and storage of supplies, 33 , 34 , 36 health insurance, avoiding hazardous situations, dealing with hypoglycaemia and finding new health professionals. 36 Both young people and parents expressed concerns about students moving away from home and being without parental support, 1 , 4 , 36 which influenced university choices for participants in one study. 1 Students indicated they sought a supportive roommate, for example, one who could tolerate disturbed sleep and provide support with hypoglycaemia. 1 Most students in one study indicated they received information about diabetes management when preparing for university, but relevant resources, such as sexual health, mental health or substance use, how to access medical and disability support and flexible insulin adjustment were not regularly provided. 4
Forward planning
Students learnt to adapt their diabetes self‐care to the flexible university environment, which could involve long days and irregular schedules. 1 They recognised the need to plan ahead to manage blood glucose levels during classes, exams, exercise and social activities, deal with the effect of stress and avoid running out of diabetes supplies. 34 One risky forward planning strategy sometimes used, involved taking less insulin to maintain elevated blood glucose and avoid hypoglycaemia. 14 , 35
Obtaining support
Despite the diabetes management difficulties experienced by students, Kellett et al. found that few (9%) contacted university support services for advice or support. 4 Reported barriers to accessing support include lack of diabetes knowledge and understanding among campus staff 33 , 35 and failure of staff to make appropriate allowances for diabetes. 35 Participants in one study stated they did not feel disabled or want special privileges to succeed, 14 although in another study, students preferred to register for learning support than to individually approach lecturers for allowances. 1
Friends, particularly friends with diabetes were an important source of peer and diabetes self‐care support 6 , 20 , 32 , 33 , 34 and lessened feelings of isolation, 20 , 33 , 34 depression and anxiety. 20 Around half of students in one study wanted to meet other students with diabetes or join a peer support group. 32 Peers with diabetes understood the lived experience, 6 , 34 and such support was accessed via online forums, social media and the CDN. The CDN is a USA‐based national advocacy organisation providing events, online diabetes information and newsletters about preparing for, living and studying at university. 20 , 40 On occasion, the CDN assisted with emergency diabetes supplies. 34 A survey found that CDN members were more likely to access disability allowances than non‐members. 20
Students relied on friends and roommates to assist them during emergencies, teaching them what to do, such as administer glucagon or call emergency services in the event of severe hypoglycaemia, 1 , 6 , 13 although some had no supports in place for dealing with hypoglycaemia. 7 Being surrounded by people without knowledge of their diabetes afforded privacy and autonomy, but no ‘safety‐net’, challenging young adults to become more independent. 14 Parents were usually the main source of diabetes self‐care support and their ongoing involvement was valued, 4 , 6 , 34 , 36 although parental support was less accessible after moving away from home, which could lead students to paying their diabetes less attention. 6 For students who perceived their parents were over‐involved in their diabetes, going to university was an opportunity to achieve independence. 34
Using technology
Diabetes technology such as insulin pumps and glucose monitoring enabled greater flexibility with the social aspects of student life, dealing with stress and the unstructured university environment. 29 Students using an insulin pump found alcohol easier to manage. 15 , 29
Using technology allowed some students to feel and appear ‘normal’. 29 In contrast, others felt technology made their diabetes visible, so avoided checking blood glucose or injecting insulin in public. 26 These concerns were expressed more often by younger and female students due to perceived diabetes stigma and the effect of wearing technology on appearance. 29
Alcohol management strategies
In online posts, students reported incidents of severe hypoglycaemia due to alcohol but not knowing how to manage their diabetes when drinking. 36 Drinking habits may not be regularly discussed with healthcare professionals. 15 , 39 Students used a variety of methods to moderate the risks of alcohol and having strategies in place predicted less drinking and fewer consequences. 16 Strategies included eating before and/or after drinking, 15 , 16 , 26 , 32 avoiding parties and bars, 15 socialising but not drinking alcohol, 1 , 15 , 16 , 26 having personal rules about the type and amount of alcohol they can safely consume, 15 , 39 avoiding drinking games, pacing or keeping track of drinks, 15 , 16 choosing drinks with sugar or sugar‐free, 26 taking insulin to cover alcohol, 15 , 32 monitoring blood glucose 15 , 26 , 39 and drinking with friends. 39 Friends were helpful by either not pressuring them to drink or by assisting in an emergency. 15 Short‐term improvements in binge drinking, knowledge, attitudes, concerns and intentions were reported after alcohol and diabetes education. 39
4. DISCUSSION
This first integrated literature review about students with diabetes at university identified consistent patterns in the concerns and challenges for young adults and highlighted features of the university environment that present barriers to self‐care. These themes will be discussed according to the ecological model, including implications for future research and practice, and recommendations for multilevel support that can be adopted by health professionals and tertiary education institutions.
4.1. Intrapersonal factors
Managing diabetes may not be easier for students as they get older. Diabetes distress was higher among students aged 24–29 than 18–23 years, 31 a trend also found in the DAWN2 study, with the older group feeling more overwhelmed and less supported. 41 Diabetes distress characterises many of the concerns and feelings expressed by students, and affects around one‐third of young adults with diabetes. 42 It is encouraging that mental health problems were not more prevalent and students with diabetes were as physically active as their counterparts without diabetes, but QoL was lower, most likely related to the specific burden of diabetes. 43 , 44 Women perceived more difficulties and distress than men, which is a consistent finding from adolescence onwards. 45
Students perceived diabetes affected them academically. One study reported slightly lower GPA, 5 which could influence future socioeconomic and health status. However, a small study among school leavers found no difference in workforce participation, higher education or GPA with or without diabetes. 43 Acute glycaemic excursions can impair cognitive performance, 46 and elevated HbA1c is associated with lower academic achievement among adolescents. 46 , 47 While academic stress may cause short‐term fluctuations in glycaemia, students with prolonged suboptimal glycaemia are also more likely to experience diabetes distress and mental health problems 31 and students with mental health‐related, 48 or more than one disability, are less likely to graduate than other students. 49 For those from disadvantaged backgrounds, financial pressures to work or stress may further affect self‐care 30 and attention to study, while already confronting psychological and material barriers to success at university. 50 Students experiencing prolonged stress and distress could benefit from ongoing academic, financial and psychological support. Students diagnosed shortly before or while at university also need support to develop problem‐solving skills usually acquired in adolescence. 51
4.2. Interpersonal factors
Students experienced social concerns reported by young adults with diabetes elsewhere, namely, body image and unwillingness to disclose diabetes due to perceived stigma and unwanted attention. 41 , 44 , 52 These mindsets diminish with age but can intensify during transitions to new environments and with new social groups and present a barrier to self‐care in these situations. 44 Better community awareness may help to lessen the negative consequences of diabetes stigma, which disproportionately affects women. 53
Similar rates of binge drinking of alcohol are reported among youth with and without diabetes, 5 , 16 , 26 , 43 although student culture and peer pressure encourage underage, and risky drinking in the university setting. 15 , 33 , 54 Without parental surveillance, alcohol and drugs present a greater risk for students with diabetes living out of home. In a study of underage drinking at university, alcohol marketing, rewards (e.g. relaxation, getting drunk) and education predicted higher alcohol intake, 54 whereas, enforcing alcohol control policies, 55 skills‐based and motivational interventions may reduce alcohol consumption. 54 Psychoeducation interventions focused on harm reduction among students are likely to be more influential than general awareness of alcohol and diabetes. 39
As young adults transition to university or work, parental monitoring and involvement decreases and often HbA1c increases, but this may be mitigated by developing problem‐solving skills, 51 and ongoing parental support. 56 Friends and partners may take over providing emotional and practical support. The CDN has over 140 Chapters in the United States, offering peer support and information tailored to students with diabetes. 40 Although CDN resources are accessible, they are tailored to the USA context.
4.3. Institutional factors
Students with diabetes are entitled to reasonable adjustments to accommodate diabetes, for example, access to food and extra time for exams. Accessing support is associated with higher odds of graduating for students with disabilities. 48 However, few students with diabetes take advantage of this support, and institutional barriers to accessing services include staff attitudes, appropriateness of accommodations and communication about disability services. 57 Students relied on friends and roommates in emergencies, yet institutions have responsibilities to ensure students living on campus are safe and should have policies in place. 58 Students living independently need to consider strategies for checking their well‐being, in contrast to school or the workplace where attendance is monitored.
4.4. Community factors and public policy
The community level includes campus facilities, such as cafes, meal services and alcohol outlets. Adapting to these factors requires preparation and planning skills that emerge with maturity. At the policy level, anti‐discrimination legislation obliges universities to provide adjustments to enable students to fully participate in their education. 59
4.5. Limitations and strengths
There are several limitations to this research. We restricted publications to the English language which could have omitted relevant studies. In most studies, participants had type 1 diabetes, were aged under 30 years and more likely to be female, so the results may not be generalisable. We included type 2 diabetes in our search but located only one paper and none in students over the age of 40. Several studies recruited through the CDN so likely to represent more socially connected students. There were no studies that could demonstrate effective interventions to support students and few studies considered socioeconomic or racial background; factors likely to increase disparities for students with diabetes. We were unable to synthesise the data quantitatively due to the heterogeneity of studies. Nevertheless, the review was rigorously conducted following Toronto and Remington's methodology, 17 and we were able to incorporate the available evidence from different study designs, the findings of which were highly consistent. Most studies were conducted in the United States where students typically leave home to attend university and the legal drinking age is high compared to other countries (21 years). 54 These two factors may influence alcohol‐related and self‐care behaviours, so some findings may not be transferable to all settings.
4.6. Future research
There are gaps in the literature about students with type 2 diabetes, older adults and those from ethnic minorities or attending technical colleges who may experience socio‐economic disadvantage. The needs of students with complications should be explored. Further understanding is needed of the barriers to accessing disability services and student preferences for support and whether such support improves outcomes, as are evidence‐based interventions to minimise alcohol risk for students with diabetes. Outcome evaluation of support programmes such as CDN could help to advocate for establishing such programmes elsewhere.
4.7. Implications for policy and practice
Most student concerns identified in this review are experienced by young adults with type 1 diabetes. However, problems are exacerbated during life transitions and interactions with the university environment. Support could be enhanced at multiple levels.
4.7.1. Intrapersonal
Female students, students with mental health problems or those from ethnic minority or disadvantaged populations, are likely to have more problems dealing with their diabetes and to benefit from disability, academic and psychological support while at university.
4.7.2. Interpersonal
Institutions could improve understanding of diabetes in their community to minimise stigma.
4.7.3. Institutional
Institutions could monitor academic outcomes and ensure disability services are accessible and tailored for diverse students, living on‐ and off‐campus and different types of diabetes, and promote engagement. Health professionals and universities could provide evidence‐based practical information about alcohol and drug safety.
4.7.4. Community and policy
Organisations such as CDN could advocate and provide information tailored to the student experience at a campus, state or national level.
5. CONCLUSIONS
This integrated review of published studies identified consistent themes about diabetes self‐care difficulties and risky behaviours were reported by young adults with diabetes after moving from school to the less structured university setting. Some students need support to manage their diabetes in this environment and self‐care resources tailored to university lifestyles, paying particular attention to the early years at university, those leaving home or recently diagnosed with diabetes. These findings provide a foundation for the development of resources and interventions tailored to the needs of this priority population. Further research into the experiences and support needs of older students, those from diverse backgrounds and type 2 diabetes would address gaps in the literature.
AUTHOR CONTRIBUTIONS
Virginia Hagger designed the study, conducted the review and drafted the first version of the manuscript. Tarveen Singh assisted with searching, appraisal and data extraction. Bodil Rasmussen, Amelia J. Lake, Peter S. Hamblin contributed to the review design, search strategy and critical revisions to the manuscript.
CONFLICT OF INTEREST
The authors declare no conflicts of interest.
Supporting information
Table S1
ACKNOWLEDGEMENT
This project was supported by funding from the Australian Diabetes Educator's Association Diabetes Research Foundation. Open access publishing facilitated by Deakin University, as part of the Wiley ‐ Deakin University agreement via the Council of Australian University Librarians.
Hagger V, Lake AJ, Singh T, Hamblin PS, Rasmussen B. The experiences and support needs of students with diabetes at university: An integrative literature review. Diabet Med. 2023;40:e14943. doi: 10.1111/dme.14943
REFERENCES
- 1. Saylor J, Hanna KM, Calamaro CJ. Experiences of college students who are newly diagnosed with type 1 diabetes mellitus. J Pediatr Nurs. 2019;44:74‐80. doi: 10.1016/j.pedn.2018.10.020 [DOI] [PubMed] [Google Scholar]
- 2. Edwards D, van der Brugge E. Higher education students in Australia. What the census data tell us. Aust Council Educ Res. 2012;2(3):1‐14. Accessed December 9, 2021. https://research.acer.edu.au/ [Google Scholar]
- 3. Government UK . Participation rates in higher education: 2006 to 2018. Accessed June 6, 2022. https://www.gov.uk/government/statistics/participation‐rates‐in‐higher‐education‐2006‐to‐2018
- 4. Kellett J, Sampson M, Swords F, et al. Young people's experiences of managing type 1 diabetes at university: a national study of UK university students. Diabet Med. 2018;35(8):1063‐1071. doi: 10.1111/dme.13656 [DOI] [PubMed] [Google Scholar]
- 5. Cockroft MC, Bartlett TR, Wallace DC. Sleep, nutrition, disordered eating, problematic tobacco and alcohol use, and exercise in college students with and without diabetes. J Psychosoc Nurs Ment Health Serv. 2019;57(12):23‐32. [DOI] [PubMed] [Google Scholar]
- 6. Habenicht AE, Gallagher S, O'Keeffe M‐C, Creaven A‐M. Making the leap and finding your feet: a qualitative study of disclosure and social support in university students with type 1 diabetes. J Health Psychol. 2021;26(2):260‐269. [DOI] [PubMed] [Google Scholar]
- 7. Ramchandani N, Cantey‐Kiser JM, Alter CA, et al. Self‐reported factors that affect glycemic control in college students with type 1 diabetes. Diabetes Educ. 2000;26(4):656‐666. [DOI] [PubMed] [Google Scholar]
- 8. Herts K, Wallis E, Maslow G. College freshmen with chronic illness: a comparison with healthy first‐year students. J Coll Stud Dev. 2014;55(5):475‐480. [Google Scholar]
- 9. Maslow GR, Haydon A, McRee A‐L, Ford CA, Halpern CT. Growing up with a chronic illness: social success, educational/vocational distress. J Adolesc Health. 2011;49(2):206‐212. doi: 10.1016/j.jadohealth.2010.12.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Montali L, Zulato E, Cornara M, Ausili D, Luciani M. Barriers and facilitators of type 1 diabetes self‐care in adolescents and young adults. J Pediatr Nurs. 2022;62:136‐143. doi: 10.1016/j.pedn.2021.09.014 [DOI] [PubMed] [Google Scholar]
- 11. Rasmussen B, Ward G, Jenkins A, King SJ, Dunning T. Young adults' management of type 1 diabetes during life transitions. J Clin Nurs. 2011;20(13‐14):1981‐1992. doi: 10.1111/j.1365-2702.2010.03657.x [DOI] [PubMed] [Google Scholar]
- 12. Balfe M. Diets and discipline: the narratives of practice of university students with type 1 diabetes. Sociol Health Illn. 2007;29(1):136‐153. [DOI] [PubMed] [Google Scholar]
- 13. Ersig AL. An exploratory study: transition to adulthood for college students with type 1 diabetes and their parents. J Pediatr Nurs. 2019;46:12‐17. doi: 10.1016/j.pedn.2019.01.008 [DOI] [PubMed] [Google Scholar]
- 14. Hill S, Gingras J, Gucciardi E. The lived experience of Canadian university students with type 1 diabetes mellitus. Can J Diabetes. 2013;37(4):237‐242. [DOI] [PubMed] [Google Scholar]
- 15. Miller‐Hagan RS, Janas BG. Drinking perceptions and management strategies of college students with diabetes. Diabetes Educ. 2002;28(2):233‐244. [DOI] [PubMed] [Google Scholar]
- 16. Ravert RD. Alcohol management strategies of college students with diabetes. Patient Educ Couns. 2009;77(1):97‐102. [DOI] [PubMed] [Google Scholar]
- 17. Toronto C, Remington R. A Step‐By‐Step Guide to Conducting an Integrative Review. Springer Nature; 2020. doi: 10.1007/978-3-030-37504-1_1 [DOI] [Google Scholar]
- 18. Law M, Stewart D, Pollock N, Letts L, Bosch J, Westmorland M. Critical Review Form ‐ Quantitative Studies. McMaster University; 2007. [Google Scholar]
- 19. Letts L, Wilkins S, Law M, Stewart D, Bosch J, Westmorland M. Critical Review Form ‐ Qualitative Studies (Version 2.0). McMaster University; 2007. [Google Scholar]
- 20. Saylor J, Lee S, Ness M, et al. Positive health benefits of peer support and connections for college students with type 1 diabetes mellitus. Diabetes Educ. 2018;44(4):340‐347. doi: 10.1177/0145721718765947 [DOI] [PubMed] [Google Scholar]
- 21. Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol. 2006;32(2):77‐101. doi: 10.1191/1478088706qp063oa [DOI] [Google Scholar]
- 22. Sallis J, Owen N. Ecological models of health behavior. In: Glanz K, Rimer BK, Viswanath K, eds. Health Behavior: Theory, Research, and Practice. 5th ed. Wiley; 2014. [Google Scholar]
- 23. American College Health Association . Healthy campus: ecological model. Accessed May 31, 2022. https://www.acha.org/HealthyCampus/Ecological_Model
- 24. McLeroy KR, Bibeau D, Steckler A, Glanz K. An ecological perspective on health promotion programs. Health Educ Q. 1988;15(4):351‐377. doi: 10.1177/109019818801500401 [DOI] [PubMed] [Google Scholar]
- 25. Jones MC, MacGillivray S, Kroll T, Zohoor AR, Connaghan J. A thematic analysis of the conceptualisation of self‐care, self‐management and self‐management support in the long‐term conditions management literature. J Nurs Healthc Chronic Illn. 2011;3(3):174‐185. doi: 10.1111/j.1752-9824.2011.01096.x [DOI] [Google Scholar]
- 26. Balfe M. Alcohol, diabetes and the student body. Health Risk Soc. 2007;9(3):241‐257. [Google Scholar]
- 27. Balfe M. Healthcare routines of university students with type 1 diabetes. J Adv Nurs. 2009;65(11):2367‐2375. [DOI] [PubMed] [Google Scholar]
- 28. Balfe M. The body projects of university students with type 1 diabetes. Qual Health Res. 2009;19(1):128‐139. [DOI] [PubMed] [Google Scholar]
- 29. Balfe M, Jackson P. Technologies, diabetes and the student body. Health Place. 2007;13(4):775‐787. [DOI] [PubMed] [Google Scholar]
- 30. Bratke H, Lønning KJ, Sivertsen B. DiaSHoT18: a cross‐sectional national health and well‐being survey of university students with type 1 diabetes. Pediatr Diabetes. 2020;21(8):1583‐1592. doi: 10.1111/pedi.13119 [DOI] [PubMed] [Google Scholar]
- 31. Bratke H, Sivertsen B. Mental and somatic health in university students with type 1 diabetes: new results from DiaSHoT18, a cross sectional national health and well‐being survey. J Pediatr Endocrinol Metab. 2021;34(6):697‐705. doi: 10.1515/jpem-2021-0041 [DOI] [PubMed] [Google Scholar]
- 32. Wdowik MJ, Kendall PA, Harris MA. College students with diabetes: using focus groups and interviews to determine psychosocial issues and barriers to control. Diabetes Educ. 1997;23(5):558‐562. [DOI] [PubMed] [Google Scholar]
- 33. Fedor A, Schumacher JR, Banning J, McKinnis R, Wilson M. Perceptions of how the transition from home life to college life affects type 1 diabetes management. Diabetes Spectr. 2017;30(4):315‐319. doi: 10.2337/ds17-0019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Fredette J, Mawn B, Hood K, Fain J. Quality of life of college students living with type 1 diabetes: a qualitative view. West J Nurs Res. 2016;38(12):1595‐1610. [DOI] [PubMed] [Google Scholar]
- 35. Wilson V. Students' experiences of managing type 1 diabetes. Nurs Child Young People. 2010;22(10):25‐28. doi: 10.7748/paed2010.12.22.10.25.c8134 [DOI] [PubMed] [Google Scholar]
- 36. Ravert RD, Boren SA, Wiebke E. Transitioning through college with diabetes: themes found in online forums. J Am Coll Health. 2015;63(4):258‐267. [DOI] [PubMed] [Google Scholar]
- 37. Wdowik MJ, Kendall PA, Harris MA, Auld G. Expanded health belief model predicts diabetes self‐management in college students. J Nutr Educ. 2001;33(1):17‐23. [DOI] [PubMed] [Google Scholar]
- 38. Thomas JJ, Moring J, Bowen A, Rings JA, Emerson T, Lindt A. The influence of stress and coping on diabetes self‐care activities among college students. J Am Coll Health. 2021;1‐6:1‐6. doi: 10.1080/07448481.2021.1928142 [DOI] [PubMed] [Google Scholar]
- 39. Wisk LE, Magane KM, Nelson EB, Tsevat RK, Levy S, Weitzman ER. Psychoeducational messaging to reduce alcohol use for college students with type 1 diabetes: internet‐delivered pilot trial. J Med Internet Res. 2021;23(9):e26418. doi: 10.2196/26418 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. College Diabetes Network . CDN chapters. Accessed December 9, 2021. https://collegediabetesnetwork.org/
- 41. Vallis M, Willaing I, Holt RIG. Emerging adulthood and type 1 diabetes: insights from the DAWN2 study. Diabet Med. 2018;35(2):203‐213. doi: 10.1111/dme.13554 [DOI] [PubMed] [Google Scholar]
- 42. Morrissey EC, Casey B, Dinneen SF, Lowry M, Byrne M. Diabetes distress in adolescents and young adults living with type 1 diabetes. Can J Diabet. 2020;44(6):537‐540. doi: 10.1016/j.jcjd.2020.03.001 [DOI] [PubMed] [Google Scholar]
- 43. Palladino DK, Helgeson VS, Reynolds KA, Becker DJ, Siminerio LM, Escobar O. Emerging adults with type 1 diabetes: a comparison to peers without diabetes. J Pediatr Psychol. 2013;38(5):506‐517. doi: 10.1093/jpepsy/jst002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Balfe M, Doyle F, Smith D, et al. What's distressing about having type 1 diabetes? A qualitative study of young adults' perspectives. BMC Endocr Disord. 2013;13(1):25. doi: 10.1186/1472-6823-13-25 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Fisher L, Polonsky WH, Hessler DM, et al. Understanding the sources of diabetes distress in adults with type 1 diabetes. J Diabetes Complications. 2015;29(4):572‐577. doi: 10.1016/j.jdiacomp.2015.01.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Knight M, Perfect M. Glycemic control influences on academic performance in youth with type 1 diabetes. Sch Psychol. 2019;34(6):646‐655. doi: 10.1037/spq0000320 [DOI] [PubMed] [Google Scholar]
- 47. Winnick JB, Berg CA, Wiebe DJ, Schaefer BA, Lei P‐W, Butner JE. Metabolic control and academic achievement over time among adolescents with type 1 diabetes. Sch Psychol Q. 2017;32(1):105‐117. doi: 10.1037/spq0000190 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Pingry O'Neill LN, Markward MJ, French JP. Predictors of graduation among college students with disabilities. J Postsecond Educ Disabil. 2012;25(1):21‐36. [Google Scholar]
- 49. Herbert JT, Hong BS, Byun S‐y, Welsh W, Kurz CA, Atkinson HA. Persistence and graduation of college students seeking disability support services. J Rehabil. 2014;80(1):22‐32. [Google Scholar]
- 50. Jury M, Smeding A, Stephens NM, Nelson JE, Aelenei C, Darnon C. The experience of low‐SES students in higher education: psychological barriers to success and interventions to reduce social‐class inequality. J Soc Issues. 2017;73(1):23‐41. doi: 10.1111/josi.12202 [DOI] [Google Scholar]
- 51. Majumder E, Cogen FR, Monaghan M. Self‐management strategies in emerging adults with type 1 diabetes. J Pediatr Health Care. 2017;31(1):29‐36. doi: 10.1016/j.pedhc.2016.01.0035 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Wentzell K, Vessey JA, Laffel LMB. How do the challenges of emerging adulthood inform our understanding of diabetes distress? An integrative review. Curr Diab Rep. 2020;20(6):21. doi: 10.1007/s11892-020-01301-3 [DOI] [PubMed] [Google Scholar]
- 53. Liu NF, Brown AS, Folias AE, et al. Stigma in people with type 1 or type 2 diabetes. Clin Diabetes. 2017;35(1):27‐34. doi: 10.2337/cd16-0020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Paek H‐J, Hove T. Determinants of underage college student drinking: implications for four major alcohol reduction strategies. J Health Commun. 2012;17(6):659‐676. doi: 10.1080/10810730.2011.635765 [DOI] [PubMed] [Google Scholar]
- 55. Wechsler H, Lee JE, Nelson TF, Kuo M. Underage college students' drinking behavior, access to alcohol, and the influence of deterrence policies: findings from the harvard school of public health college alcohol study. J Am Coll Health. 2002;50(5):223‐236. doi: 10.1080/07448480209595714 [DOI] [PubMed] [Google Scholar]
- 56. Berg CA, Wiebe DJ, Tracy EL, et al. Parental involvement and executive function in emerging adults with type 1 diabetes. J Pediatr Psychol. 2019;44(8):970‐979. doi: 10.1093/jpepsy/jsz025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Marshak L, Van Wieren T, Ferrell DR, Swiss L, Dugan C. Exploring barriers to college student use of disability services and accommodations. J Postsecond Educ D isabil. 2010;22(3):151‐165. [Google Scholar]
- 58. Strachan M, MacCuish A, Frier B. The care of students with insulin‐treated diabetes mellitus living in university accommodation: scope for improvement? Diabet Med. 2000;17(1):70‐73. [DOI] [PubMed] [Google Scholar]
- 59. Australian Government . Disability Discrimination Act 1992. No. 135. Australian Government; 2018. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1


