Abstract
Purpose
The purpose of this investigation was to identify a mesiodistal algorithm for multiple posterior implant placement based upon an ideal prosthetically restoration design.
Methods
One hundred one cases of posterior free‐end edentulous arches were selected for digital crown designs and measurements. Cone bean computed tomogram and digital fabricated crown were applied. DICOM files were exported to a viewer software (BlueSkyPlan4) to generate digital crown and measurement. The mesiodistal space between roots of adjacent teeth and center of the potential implant horizontally, from both cross‐section and coronal plane were measured. Comparisons were performed using t‐tests.
Results
No significant difference was found in the distances of the maxillary and mandibular posterior implants to adjacent natural teeth (p > 0.05). For interdental/implant distances, premolars are around 4.2 mm and molars are 5.4 mm, correspondently. The second premolar interimplant distance is around 7–7.4 mm. The distance of interimplant of the first molar is about 8–8.5 mm. For the maxillary second molar, the interimplant distance is 9.26 ± 0.29 mm and the mandibular second molar interimplant distance is 9.58 ± 0.19 mm, which is significantly different. No difference was found between the two different measurement methods.
Conclusion
A mesiodistal algorithm of 4–4.6 (implant to adjacent canine tooth), 7–7.4, 8–8.5, and 9–9.5 mm was recommended for interimplant/tooth distance from first premolar to second molar when placing implants with or without case‐specific prosthetic planning prior to surgery.
Keywords: CBCT, dental implants, digital dentistry, implant prosthetic design
What is known
Few studies gave evidence of the acknowledged distance for posterior implant requirement. Meanwhile, biologic width (e.g., supracrestal tissue adhesion) was often disrupted and led to multiple clinical outcomes.
What this study adds
This study showed the appropriate size and spacing of dental implants in the posterior by using digital method. We would like to provide clinician with guidance to enhance implant success, prosthesis survival and patient satisfaction.
1. INTRODUCTION
Implant dentistry is a prosthetic endeavor with a biological foundation. To attain an optimal prosthetic construct and soft tissue profile, implants should be placed according to the final prosthetic prosthesis and this should be planned before initiating implant placement. 1 , 2 For the posterior edentulous teeth, the appropriate size and spacing of dental implants in the posterior could be affected by multi factors such as the restorative space available, the anatomy of the ridge, and the ability for implant maintenance in order to achieve long‐term implant stability. The presence of a supracrestal tissue height (STH) 3 or supracrestal tissue adhesion (STA) 4 around implants has been investigated. 3 , 4 , 5 , 6 , 7 , 8 Studies have verified that a STH/STA exists around implants which determines the vertical dimension of the prosthetic crown on implant. 5 , 6 , 7 , 8 , 9 For the horizontal space between adjacent tooth‐implant, a distance of at least 1.5–2 mm from the adjacent teeth has been advocated especially for the anterior teeth. 10 In addition, implants should have 3–4 mm of space between them. 11 , 12 Nonetheless, due to the issue of emergence profile and access for proper hygiene, the minimal gap distance required for the posterior implant is often set for at least 3 mm. 12 By keeping a minimum 3 mm distance from the adjacent tooth and a distance of 3–4 mm between adjacent implants, implants can often be maintained longitudinally. 10 , 12 It is because these considerations, the interimplant/tooth algorithm of 5–5.5 (implant‐tooth), 8, 8, and 9 mm of first premolar to second molars' horizontal distance has been proposed in the lecture circuit without evidence. This formular is based upon above principles (3–4 mm of interimplant distance 2 as well as 3 mm of space that is required for establishing a nice emergency contour for implant crown as well as patient's ability to clean). 13
The size of the prosthetic tooth must be considered when placing implants. If an implant placed for a premolar restoration is placed too close to the adjacent tooth, compromised contours, loss of hard and soft tissue and inability for patients and clinicians to clean the area might occur. Placing the restoration too far from the adjacent tooth also resulted in unfavorable contours of crown as well as resulting in unfavorable cantilever type of forces on the implant. 14 The natural maxillary first and second premolars, and first molars have an average mesiodistal size of 7.1, 6.8, and 10.4 mm, respectively. 15 , 16 , 17 , 18 , 19 , 20 The average dimensions of these teeth at the cementoenamel junction (CEJ) are 4.8, 4.7, and 7.9 mm. 21 , 22 , 23 Thus, a proper implant restorations design should consider the natural tooth dimension and contour.
Therefore, the purpose of this investigation was aimed at identifying a mesiodistal algorithm for multiple posterior implant placement based upon an ideal prosthetically restoration design (e.g., ideal prosthetic contour, proper distance for maintaining the interproximal bone level, interdental papilla as well as ability to clean) using cone bean computed tomogram (CBCT) and digital fabricated prosthesis. These mesiodistal distance resulting data are promising to be used by clinicians and provide references for implant placement with or without case‐specific prosthetic planning before surgery.
2. MATERIALS AND METHODS
2.1. Study design
This investigation was performed in accordance with the STROBE guidelines, 24 approved by the University of Michigan School of Dentistry Institutional Review Board for Human Studies (HUM00210043) with exemption for obtaining the patient's consent form.
We went through the database of CBCT from the year of 2021 to 2020 and selected posterior free‐end edentulous maxillary and mandibular arches in chronological order. All images were obtained from the same CBCT machine. Two authors (W.L. and A.S.) searched and included the cases according to the inclusion and exclusion criteria. Disagreements were resolved by discussion with the third senior author.
The inclusion criteria were:
Posterior free‐end edentulous maxillary and mandibular arches.
One side or two sides of the arch with at least two to three posterior teeth lost.
No obvious malformation or pathological disease.
CBCT will be excluded if:
Edentulous area without enough space for digital crown design.
2.2. CBCT data acquisition
CBCT scans were obtained from Department of Periodontics and Oral Medicine at the University of Michigan, School of Dentistry. The DICOM files were exported to a viewer software (BlueSkyPlan4; BlueSkyBio) to generate digital crown and measurement.
2.3. Measurements and variables
Before recording measurements for each potential implant site (tooth position), the examiner oriented the image in the software, using anatomic landmarks such as the occlusal plane, adjacent teeth, and then aligned the tooth of interest with the vertical reference line. The antagonists, same‐named teeth and reported data 14 , 15 , 16 , 17 , 18 , 19 were took as reference when designing the crowns' size and morphology. The virtual crowns were depicted harmoniously with patients' occlusion relationship as well as mesiodistal and vertical space. The long axes of implants were decided on the basis of standard data and adjacent teeth. Three millimeters apical to the midfacial CEJ, the examiner horizontally measured the mesiodistal space between roots of adjacent teeth and center of the potential implant. Two authors (W.L. and A.S.) designed crowns and measured the mesiodistal distances together. Disagreements were resolved by discussion with the third senior author (H.L.W.) (Figure 1 shows the Schematic drawing while Figure 2 shows the screenshot for the cases).
FIGURE 1.
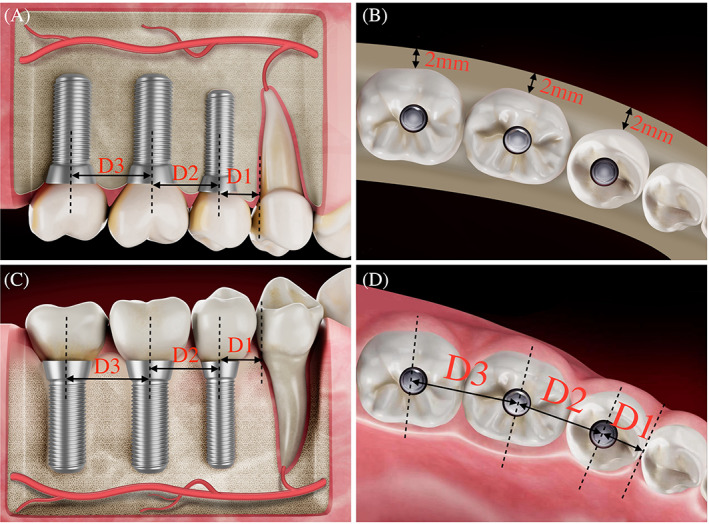
Schematic drawing of the measurement of the horizontal distance between the implant edge and an adjacent natural tooth (A, maxilla. C, mandible). Top view with (D) or without soft tissue (B). D1, distance between the implant (second premolar) to adjacent natural tooth (first premolar); D2, distance between the first molar implant to the second premolar implant; D3, distance between the second molar implant to the first molar implant.
FIGURE 2.
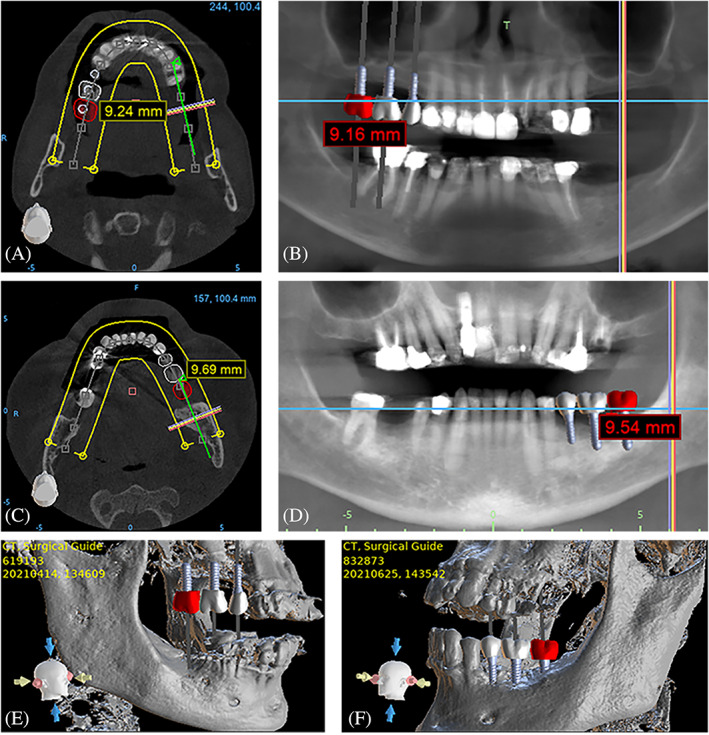
Radiographic illustration of the meausrement of horizontal distance between the implant edge and an adjacent natural tooth, measured in maxilla and mandible (A and C: cross‐section measurement. B and D: coroanl plane measurement. E and F: 3D modeling).
2.4. Statistical analysis
The average horizontal distance from cross‐section and coronal plane were analysis and expressed as a mean ± standard deviation (SD) in millimeters. Statistically significant differences (p < 0.05) were analyzed using Student t‐tests.
3. RESULTS
One hundred one cases were chosen from 635 CBCT documents (49 males, 51 females, 1 unknown; age: 64.3 ± 10.4 years). A total of 450 implants were installed in 101 cases of posterior free‐end arches. Among them, 65 were maxillary arches and the remaining 70 were mandibular arches. The mean ± SD of the distance between implant to natural teeth or between implants of the maxillary and mandibular posterior teeth were presented in Table 1 and Figures 3, 4, 5. The data were measured from cross‐section in CBCT, while data measured from coronal plane in CBCT was showed in Supporting Information S1. Data from both two planes were similar. Since the measurement from cross‐section is easy to locate the center of the implant, these data were used as the main reference in measurement.
TABLE 1.
Mean and standard deviation (SD) of the distance (mm) between implant to teeth or interimplant for each posterior tooth site and the result of t‐test
| Implant‐natural teeth | Implant‐implant | |||||
|---|---|---|---|---|---|---|
| Maxilla | Mandible | p Value | Maxilla | Mandible | p Value | |
| First premolars | 4.3 ± 0.3 | 4.2 ± 0.2 | ns | |||
| Second premolars | 4.2 ± 0.2 | 4.2 ± 0.2 | ns | 7.0 ± 0.2 | 7.1 ± 0.3 | ns |
| First molars | 5.4 ± 0.2 | 5.5 ± 0.3 | ns | 8.4 ± 0.3 | 8.5 ± 0.2 | ns |
| Second molars | 5.4 ± 0.2 | 5.4 ± 0.2 | ns | 9.3 ± 0.3 | 9.6 ± 0.2 | *** |
Note: Measured from cross‐section.
Abbreviation: ns, no significant.
p < 0.001.
FIGURE 3.
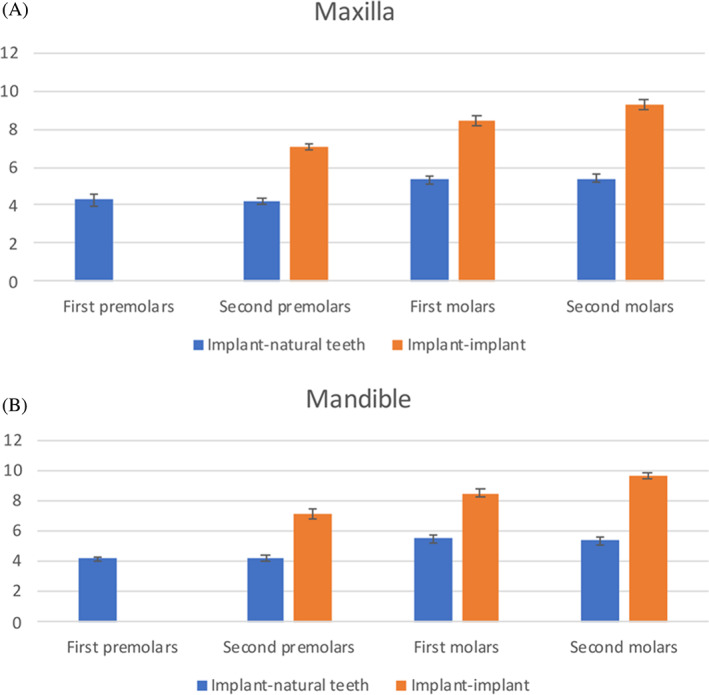
(A) Distance between implant and adjacent teeth in maxilla, measured from cross‐section. (B) Distance between implant and adjacent teeth in mandible, measured from cross‐section.
FIGURE 4.
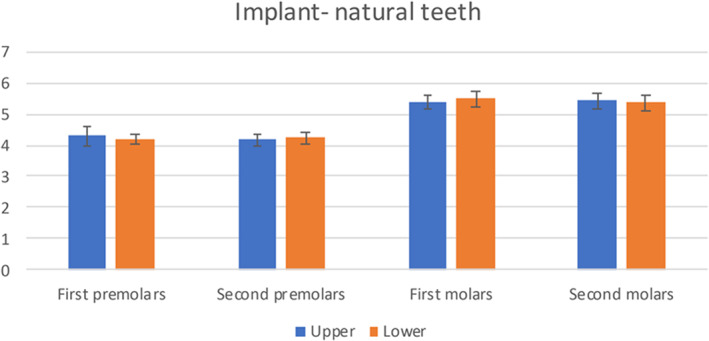
Distance between implant to natural teeth.
FIGURE 5.
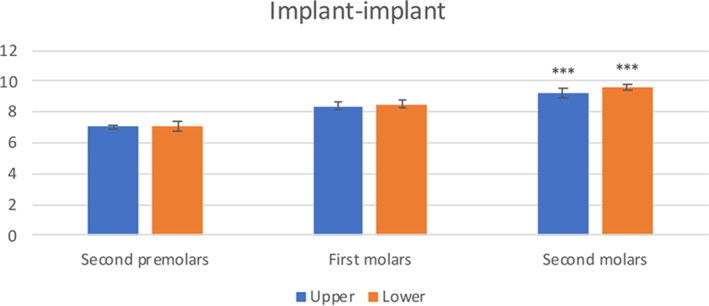
Distance between implants. ***p < 0.001.
For the first and second premolar, the distance implant to teeth distal surface is in the range of 4–4.6 mm. The second premolar interimplant distance is around 7–7.4 mm. The distance of interimplant of the first molar is about 8–8.5 mm. For the maxillary second molar, the interimplant distance is 9.3 ± 0.3 mm and the mandibular second molar interimplant distance is 9.6 ± 0.19 mm. There is significant difference between the maxillary and mandibular second molar (p < 0.001).
Comparing the distances of the maxillary and mandibular posterior implants to adjacent natural teeth, there is no significant difference in each related tooth position. Moreover, the two different measurement methods showed no significant difference.
4. DISCUSSION
Implant prosthetic factors affecting peri‐implant health such as the prosthetic crown's type, contour and the emergency profile are the potential factors which influence peri‐implant health. 25 , 26 Adequate space and bone volume are imperative for dental implant therapy. Several studies have attempted to rationalize the minimum spacing and bone volume needed for a dental implant. 27 The mesiodistal tooth sizes of the maxillary and mandibular arches should have a harmonious relationship to obtain a proper occlusion at the completion of implant restoration with adequate bone support. The inadequate restorative spacing could result in a structurally weak rehabilitation, poor physiological contours, inadequate esthetics, reduced interocclusal rest space, and decreased implant long‐term stability. 28 Studies reported a horizontal distance requires at least 2 mm space between the implant platform and the tooth. 27 Regarding the optimal buccal bone dimension required, it has been suggested to have a buccal bone plate of at least 2 mm. 29 , 30 The minimum distance required depends on implant platform depth. Because the horizontal dimension of the cone‐shaped circumferential peri‐implant bone modeling widens crestally, deeper implants require greater interimplant and implant‐to‐tooth distances. 29 Although many studies have demonstrated the implant position from the point of view of obtaining sufficient bone volume, nonetheless the fundamental requirement of implant is to provide the occlusion functions and esthetics. Thus, restorations should be functional and as close to the natural dentition as possible, to allow proper development of occlusion and embrasure forms for patient comfortable. Thus, in this study we design ideal prosthetic prosthesis to measure the mesiodistal position of the potential implants on the posterior free‐end edentulous area which could provide data reference for clinicians working with or without case‐specific prosthetic planning prior to surgery.
Results obtained from this study showed the distance from adjacent tooth to the first implant drill site position—most likely first or second premolars is 4–4.6 mm. The second implant mesiodistal distance (first molar implant position) will be 8–8.5 mm and the third implant mesiodistal distance (second molar implant position) will be 9–9.5 mm for the maxillary and mandibular, respectively. The distance coincides with the maxillary and mandible mesiodistal tooth sizes in order to obtain a harmony occlusion. 17 Slightly longer distance is needed for mandibular tooth than maxillary tooth.
Based on the measurements, if we are placing a dental implant right next a tooth, a distance of 4–4.6 mm for premolars and 5–5.5 mm for molars is recommended. When considering the distance between two implants osteotome drill location, a 7–7.4 mm for premolars, 8–8.5 mm for first molars, and 9–9.5 mm for second molars are recommended.
The presence of a STH around implants has been investigated. However, the term should be STA to better reflect the biology behind the dimension. 4 Multiple research groups have verified that a STA also exists around implants. Once an implant is uncovered, a distance of 3 mm is often needed to establish the needed implant‐abutment interface (so called STA). Literature has also reported the minimum distance between roots for two separate angular defects to be present on adjacent teeth was 3.1 mm. 31 In other words, the lateral aspect of each angular defect appears to be at least 1.0 mm on each root leaving behind of 1 mm bone peak. 31 This is in agreement with what Tarnow et al. 12 reported, in order to maintain an interproximal papilla between two adjacent implants, a minimal distance of 3 mm is needed. In our study, considering about the regular posterior implant diameter is between 4 and 5 mm. Our results of the distances between neighboring teeth and/or implants are consisted with the other researches 13 which investigated from the bone biological properties. The consistency proved that the prosthesis following natural tooth morphology and position could direct the implant position. The biological principle of the physiological position of crown and implant is therefore supported.
From the prospective prosthetic design aspect, the mesiodistal position of the gingival profile on the posterior teeth was also considered. Though esthetics is secondary in restoring the posterior areas of the oral cavity, care should be taken with implant position to allow restorations that is functional and mimics to the natural dentition as possible. 14 As posterior implant‐supported crowns serve as a guide for proper implant placement, adequate mesiodistal positioning of the implant could allow proper development of occlusal function, embrasure forms and proper establishment of interproximal hard and soft tissue dimension. The interproximal bone is predominately flat in the posterior regions of the maxilla and mandible. 32 The implant must be placed sufficiently away from the adjacent tooth or implant to allow the proper prosthetic emergence profile as well as access to hygiene. If an implant placed for a posterior restoration is placed too close to the adjacent tooth, not only can it not be cleaned but it also compromised prosthetic contours resulting in unnecessary loss of hard and soft tissue. Placing the restoration too far from the adjacent tooth also results in unfavorable contours and development of cantilever type forces on the implant which might lead to implant marginal bone loss. 14 , 27 The improper distance to the adjacent tooth or implants may lead to over‐contoured implant prosthesis which is a critical local confounder for peri‐implant mucositis 33 or peri‐implantitis. 34 Moreover, the proper distance around implant is important for the sufficient access to remove the access cement and avoid the residual cement which will lead to peri‐implant diseases. 33 , 35 In most cases, it is virtually impossible for the restorative dentist to achieve an ideal restoration if the implant is not properly placed mesiodistally by the surgeon. Therefore, the proper restorative emergence profile design is essential to maintain peri‐implant health. 36 The ideal prosthesis could provide proper self‐hygiene and mechanism properties for implant support crown and decrease the complication such as food impaction. Insufficient or excessive mesiodistal space between implant or adjacent tooth could lead to difficulty for patient to perform daily hygiene. The ease of maintenance is important for implant service life which depend, to a great extent, on the prosthesis design.
For the most distally positioned implant‐supported single crowns, study has reported the statistically significant relationship between horizontal distance and the occurrence of mechanical complications (p = 0.009). 37 Horizontal distance values in success group were 3.1 ± 0.1 mm while for complications group they were 3.8 ± 0.2 mm. The horizontal distance refers to the distal implant position which should consider the occlusal force distribution. Clinically, the optimal horizontal distance in the most distally placed implant‐supported crown is one of the key factors underlying implant success, to prevent implant failure and mechanical complications caused by an unfavorable cantilever prosthesis and bending movements. 38
This study is not without limitations. In this study, all measurements were based on the same vertical level implant. Nonetheless, some studies have reported that the deeper the implant is placed, the more the peri‐implant bone loss may occur. 29 , 39 Hence, it will be nice if we can also assess different vertical level to examine if this modification actually change the recommended mesiodistal algorithm. Furthermore, we are planning the crown dimensions based upon published data. 14 , 15 , 16 , 17 , 18 , 19 It is our goal to clinically assess the actual implant prosthesis placement and check how the above proposed mesiodistal algorithm influence the implant bone level when compared to other distances.
5. CONCLUSION
A mesiodistal algorithm of 4–4.6 (implant to adjacent tooth), 7–7.4, 8–8.5, and 9–9.5 mm was recommended for interimplant/tooth distance from first premolar to second molar for the implant‐supported reconstructed prosthesis. Abided by this algorithm could be referenced for proper implant placement in cases with or without case‐specific prosthetic planning prior to surgery.
AUTHOR CONTRIBUTIONS
Hom‐Lay Wang and Wenwen Liu conceived the concept/design. Ankita Samal and Wenwen Liu participated in the data collection. Wenwen Liu and Fangyu Zhu involved in the data analysis/interpretation. Wenwen Liu and Fangyu Zhu conducted the statistics. Wenwen Liu drafting the article. Hom‐Lay Wang critical revision of article. All authors approved of article.
CONFLICT OF INTEREST
The authors declare no conflict of interest.
Supporting information
Figure S1 Distance between implant and adjacent teeth in maxilla (a) and mandible (b), measured from coronal plane.
Figure S2 Distance between implant to natural teeth (a) and between implants (b), measured from coronal plane. ***p < 0.001.
Table S1 Mean and standard deviation (SD) of the distance (mm) between implant to teeth or inter‐implant for each posterior tooth site from coronal plane and the result of t‐test.
Liu W, Zhu F, Samal A, Wang H‐L. Suggested mesiodistal distance for multiple implant placement based on the natural tooth crown dimension with digital design. Clin Implant Dent Relat Res. 2022;24(6):801‐808. doi: 10.1111/cid.13135
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are openly available in [repository name] at [URL], reference number [reference number].
REFERENCE
- 1. Carpentieri J, Greenstein G, Cavallaro J. Hierarchy of restorative space required for different types of dental implant prostheses. J Am Dent Assoc. 2019;150(8):695‐706. [DOI] [PubMed] [Google Scholar]
- 2. Gastaldo JF, Cury PR, Sendyk WR. Effect of the vertical and horizontal distances between adjacent implants and between a tooth and an implant on the incidence of interproximal papilla. J Periodontol. 2004;75(9):1242‐1246. [DOI] [PubMed] [Google Scholar]
- 3. Avila‐Ortiz G, Gonzalez‐Martin O, Couso‐Queiruga E, Wang HL. The peri‐implant phenotype. J Periodontol. 2020;91(3):283‐288. [DOI] [PubMed] [Google Scholar]
- 4. Saleh M, Galli M, Siqueira R, Rodriguez MV, Wang H‐L. The prosthetic‐biologic connection: what is the influence of prosthetic design on peri‐implant disease? Int J Oral Maxillofac Implants. 2022;37(4):690‐699. [DOI] [PubMed] [Google Scholar]
- 5. Berglundh T, Lindhe J, Ericsson I, Marinello CP, Liljenberg B, Thomsen P. The soft tissue barrier at implants and teeth. Clin Oral Implants Res. 1991;2(2):81‐90. [DOI] [PubMed] [Google Scholar]
- 6. Abrahamsson I, Berglundh T, Lindhe J. The mucosal barrier following abutment dis/reconnection. An experimental study in dogs. J Clin Periodontol. 1997;24(8):568‐572. [DOI] [PubMed] [Google Scholar]
- 7. Buser D, Weber HP, Donath K, Fiorellini JP, Paquette DW, Williams RC. Soft tissue reactions to non‐submerged unloaded titanium implants in beagle dogs. J Periodontol. 1992;63(3):225‐235. [DOI] [PubMed] [Google Scholar]
- 8. Cochran DL, Hermann JS, Schenk RK, Higginbottom FL, Buser D. Biologic width around titanium implants. A histometric analysis of the implanto‐gingival junction around unloaded and loaded nonsubmerged implants in the canine mandible. J Periodontol. 1997;68(2):186‐198. [DOI] [PubMed] [Google Scholar]
- 9. Hermann JS, Cochran DL, Nummikoski PV, Buser D. Crestal bone changes around titanium implants. A radiographic evaluation of unloaded nonsubmerged and submerged implants in the canine mandible. J Periodontol. 1997;68(11):1117‐1130. [DOI] [PubMed] [Google Scholar]
- 10. Van Oosterwyck H, Duyck J, Vander Sloten J, et al. The influence of bone mechanical properties and implant fixation upon bone loading around oral implants. Clin Oral Implants Res. 1998;9(6):407‐418. [DOI] [PubMed] [Google Scholar]
- 11. Esposito M, Ekestubbe A, Grondahl K. Radiological evaluation of marginal bone loss at tooth surfaces facing single Branemark implants. Clin Oral Implants Res. 1993;4(3):151‐157. [DOI] [PubMed] [Google Scholar]
- 12. Tarnow DP, Cho SC, Wallace SS. The effect of inter‐implant distance on the height of inter‐implant bone crest. J Periodontol. 2000;71(4):546‐549. [DOI] [PubMed] [Google Scholar]
- 13. Su H, Gonzalez‐Martin O, Weisgold A, Lee E. Considerations of implant abutment and crown contour: critical contour and subcritical contour. Int J Periodontics Restorative Dent. 2010;30(4):335‐343. [PubMed] [Google Scholar]
- 14. Jivraj S, Chee W. Treatment planning of implants in posterior quadrants. Br Dent J. 2006;201(1):13‐23. [DOI] [PubMed] [Google Scholar]
- 15. Santoro M, Ayoub ME, Pardi VA, Cangialosi TJ. Mesiodistal crown dimensions and tooth size discrepancy of the permanent dentition of Dominican Americans. Angle Orthod. 2000;70(4):303‐307. [DOI] [PubMed] [Google Scholar]
- 16. Jain AK, Garg N, Singh J, Ansari A, Sangamesh B. Mesiodistal crown dimensions of the permanent dentition of a north Indian population. Indian J Dent. 2011;2(2):16‐20. [Google Scholar]
- 17. Malkoc S, Basciftci FA, Nur M, Catalbas B. Maxillary and mandibular mesiodistal tooth sizes among different malocclusions in a sample of the Turkish population. Eur J Orthod. 2011;33(5):592‐596. [DOI] [PubMed] [Google Scholar]
- 18. Celikoglu M, Nur M, Kilkis D, Sezgin OS, Bayram M. Mesiodistal tooth dimensions and anterior and overall Bolton ratios evaluated by cone beam computed tomography. Aust Orthod J. 2013;29(2):153‐158. [PubMed] [Google Scholar]
- 19. Ajayi EO, Ajayi YO, Oboro HO, Chukwumah NM. Mesiodistal crown dimensions of the permanent dentition in a Nigerian population. Dent Anthropol. 2010;23(2):57‐60. [Google Scholar]
- 20. Pamecha S, Dayakara HR. Comparative measurement of mesiodistal width of six anterior maxillary and mandibular teeth in Rajasthan population. J Indian Prosthodont Soc. 2012;12(2):81‐86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Scheid RC, Weiss G. Woelfel's Dental Anatomy. Lippincott Williams & Wilkins; 2010. [Google Scholar]
- 22. Misch CE. Dental Implant Prosthetics. Elsevier Mosby; 2005. [Google Scholar]
- 23. Scheid RC, Woelfel JB. Dental Anatomy: Its Relevance to Dentistry. Lippincott Williams & Wilkins; 1997. [Google Scholar]
- 24. Cuschieri S. The STROBE guidelines. Saudi J Anaesth. 2019;13(suppl 1):S31‐S34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. AlJasser RN, AlSarhan MA, Alotaibi DH, et al. Analysis of prosthetic factors affecting Peri‐implant health: an in vivo retrospective study. J Multidiscip Healthc. 2021;14:1183‐1191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Katafuchi M, Weinstein BF, Leroux BG, Chen YW, Daubert DM. Restoration contour is a risk indicator for peri‐implantitis: a cross‐sectional radiographic analysis. J Clin Periodontol. 2018;45(2):225‐232. [DOI] [PubMed] [Google Scholar]
- 27. Wilson JP, Johnson TM. Frequency of adequate mesiodistal space and faciolingual alveolar width for implant placement at anterior tooth positions. J Am Dent Assoc. 2019;150(9):779‐787. [DOI] [PubMed] [Google Scholar]
- 28. Chaimattayompol N, Arbree NS. Assessing the space limitation inside a complete denture for implant attachments. J Prosthet Dent. 2003;89(1):82‐85. [DOI] [PubMed] [Google Scholar]
- 29. Grunder U, Gracis S, Capelli M. Influence of the 3‐D bone‐to‐implant relationship on esthetics. Int J Periodontics Restorative Dent. 2005;25(2):113‐119. [PubMed] [Google Scholar]
- 30. Merheb J, Quirynen M, Teughels W. Critical buccal bone dimensions along implants. Periodontol 2000. 2014;66(1):97‐105. [DOI] [PubMed] [Google Scholar]
- 31. Tal H. Relationship between the interproximal distance of roots and the prevalence of intrabony pockets. J Periodontol. 1984;55(10):604‐607. [DOI] [PubMed] [Google Scholar]
- 32. Becker W, Ochsenbein C, Tibbetts L, Becker BE. Alveolar bone anatomic profiles as measured from dry skulls. Clinical ramifications. J Clin Periodontol. 1997;24(10):727‐731. [DOI] [PubMed] [Google Scholar]
- 33. Heitz‐Mayfield LJA, Salvi GE. Peri‐implant mucositis. J Periodontol. 2018;89(suppl 1):S257‐S266. [DOI] [PubMed] [Google Scholar]
- 34. Yi Y, Koo KT, Schwarz F, Ben Amara H, Heo SJ. Association of prosthetic features and peri‐implantitis: a cross‐sectional study. J Clin Periodontol. 2020;47(3):392‐403. [DOI] [PubMed] [Google Scholar]
- 35. Staubli N, Walter C, Schmidt JC, Weiger R, Zitzmann NU. Excess cement and the risk of peri‐implant disease—a systematic review. Clin Oral Implants Res. 2017;28(10):1278‐1290. [DOI] [PubMed] [Google Scholar]
- 36. Chu SJ, Kan JY, Lee EA, et al. Restorative emergence profile for single‐tooth implants in healthy periodontal patients: clinical guidelines and decision‐making strategies. Int J Periodontics Restorative Dent. 2019;40(1):19‐29. [DOI] [PubMed] [Google Scholar]
- 37. Lee JH, Lee JB, Park JI, Choi SH, Kim YT. Mechanical complication rates and optimal horizontal distance of the most distally positioned implant‐supported single crowns in the posterior region: a study with a mean follow‐up of 3 years. J Prosthodont. 2015;24(7):517‐524. [DOI] [PubMed] [Google Scholar]
- 38. Berglundh T, Armitage G, Araujo MG, et al. Peri‐implant diseases and conditions: consensus report of workgroup 4 of the 2017 world workshop on the classification of periodontal and peri‐implant diseases and conditions. J Periodontol. 2018;89(suppl 1):S313‐S318. [DOI] [PubMed] [Google Scholar]
- 39. Galindo‐Moreno P, Padial‐Molina M, Nilsson P, et al. The influence of the distance between narrow implants and the adjacent teeth on marginal bone levels. Clin Oral Implants Res. 2017;28(6):704‐712. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Figure S1 Distance between implant and adjacent teeth in maxilla (a) and mandible (b), measured from coronal plane.
Figure S2 Distance between implant to natural teeth (a) and between implants (b), measured from coronal plane. ***p < 0.001.
Table S1 Mean and standard deviation (SD) of the distance (mm) between implant to teeth or inter‐implant for each posterior tooth site from coronal plane and the result of t‐test.
Data Availability Statement
The data that support the findings of this study are openly available in [repository name] at [URL], reference number [reference number].


