Abstract
Background
With an increasing amount of small nodules being detected, segmentectomy has recently received a great deal of attention. We have previously reported the feasibility and safety of uniportal segmentectomy. This study aims to further compare the perioperative and oncological outcomes of uniportal and three-port thoracoscopic segmentectomy in lung cancer patients.
Methods
Patients undergoing thoracoscopic segmentectomy for lung cancer from January 2014 to March 2021 were enrolled. Clinical data were collected from the Western China Lung Cancer Database, a prospectively maintained database at the Department of Thoracic Surgery, West China Hospital. Propensity score matching (PSM) was used to reduce the heterogeneity in baseline characteristics. Perioperative outcomes, 1-, 3-, and 5-year overall survival (OS), and progression-free survival (PFS) were compared.
Results
Of the 10,063 lung cancer patients who underwent thoracoscopic lung resection, 2,630 patients receiving segmentectomy were selected (uniportal: 400; three-port: 2,230). After matching, similar results were found between the 2 groups (uniportal: 400; three-port: 1,200) regarding the number of lymph nodes harvested, the length of postoperative hospital stays, chest tube drainage volume, and postoperative complication rate. The mean follow-up duration was 27 months. Uniportal regimen showed similar 1- (100% vs. 99.9%, P=0.36), 3- (100% vs. 90.4%, P=0.20), 5-year OS (97.7% vs. 99.4%, P=0.78), as well as PFS, with the three-port regimen.
Conclusions
Uniportal video-assisted thoracoscopic segmentectomy is proven to be safe and feasible, and the perioperative outcomes and oncological results were similar between the uniportal and three-port regimens.
Keywords: Uniportal, three-port, segmentectomy, thoracoscopic, lung cancer, survival
Highlight box.
Key findings
• Uniportal and three-port thoracoscopic segmentectomy presented similar perioperative outcomes.
• Uniportal segmentectomy showed similar 1-, 3-, 5-year OS and PFS with three-port regimen.
What is known and what is new?
• Uniportal video-assisted thoracoscopic surgery has emerged with a series of advantages. Outcomes of uniportal segmentectomy remain unclear.
• Evidence from a large Chinese cohort proved that uniportal segmentectomy has similar perioperative and oncological outcomes compared with three-port approach.
What is the implication, and what should change now?
• Uniportal thoracoscopic segmentectomy is safe and feasible, and could be an alternative to three-port approach in treating early-stage lung cancer.
Introduction
Video-assisted thoracoscopic surgery (VATS) is now the mainstream treatment for lung cancer (1,2). With the progress of surgical techniques and instruments, VATS has evolved from a three-port or four-port method to a uniportal method (3-5). Uniportal VATS lobectomy was first reported by Diego Gonzalez in 2011 (6), and its feasibility and safety were then confirmed (7). The comparisons of perioperative outcomes between uniportal and multiportal VATS remain inconsistent. A meta-analysis, comparing the perioperative outcomes of uniportal and multiportal VATS for any type of thoracic surgery, identified less postoperative pain and blood loss, shorter drainage duration and length of hospital stay as advantages of the uniportal group (8). However, a recent meta-analysis found comparable outcomes in blood loss, drainage duration, and the length of stays between uniportal and multiport anatomic pulmonary resection (9).
Lobectomy is regarded as the standard treatment regimen for early-stage lung cancer, whereas segmentectomy has been traditionally used as a compromised treatment for the patients with poor cardiopulmonary preservation. With an increasing number of small nodules detected by widely applied low-dose computed tomography (CT) (10), segmentectomy has recently gained enthusiasm with comparable intraoperative and postoperative outcomes. Segmentectomy showed improved overall survival (OS) than lobectomy from the JCOG0802/WJOG4607L trial (11,12). Certainly, it does not mean that segmentectomy should be offered to all patients identified with small nodules. Some would opt for surveillance imaging if the malignancy probability is estimated to be low. But in those with indications for surgical resection, segmentectomy would be an alternative to lobectomy with satisfactory safety and outcomes. We previously demonstrated the feasibility and safety of three-port segmentectomy (13-16). Notably, given its high technical demands, uniportal segmentectomy was potentially associated with detrimental outcomes in inexperienced physicians. Nevertheless, we have accumulated a lot of experience in uniportal segmentectomy, especially in complex cases like basal segmentectomy (17-20).
A paucity of high-quality research identifying both the perioperative and oncological outcomes of uniportal thoracoscopic segmentectomy is present. The purpose of this study was to compare the perioperative and survival outcomes between uniportal and three-port thoracoscopic segmentectomy in patients with lung cancer. We present the study in accordance with the STROBE reporting checklist (available at https://tlcr.amegroups.com/article/view/10.21037/tlcr-22-635/rc) (21).
Methods
Data source
Clinical data were retrieved from our prospectively maintained database from September 2005, Western China Lung Cancer Database (WCLCD), which mainly included the patients from West China Hospital and Chengdu Shangjin Nanfu Hospital. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The Ethics Committee of West China Hospital of Sichuan University approved this study (No. 2021-1027) and waived the requirement of informed consent due to its retrospective nature.
Patient selection
Lung cancer patients who underwent intended thoracoscopic segmentectomy at the Department of Thoracic Surgery, West China Hospital from January 2014 to March 2021 were included.
The inclusion criteria included: (I) pathological diagnosis of lung cancer; (II) clinical stage I lung cancer according to the 8th edition of the tumor, node, and metastasis (TNM) staging system; and (III) underwent uniportal or three-port thoracoscopic intended segmentectomy. The exclusion criteria were as follows: (I) less than 18 years of age; (II) reoperation for ipsilateral lung cancer; (III) simultaneous bilateral segmentectomy; and (IV) robot-assisted thoracoscopic surgery. Patients who underwent segmentectomy combined with wedge resection were included. Patients who underwent lobectomy combined with segmentectomy were excluded. The patients were divided into a uniportal group and a three-port group.
Data collection
Clinical data collected included demographic information (age and sex), preoperative pulmonary function test [percentage of predicted forced expiratory volume in one second (FEV1%) and predicted carbon monoxide diffusing capacity (DLCO%)], tumor characteristics (tumor size, location, clinical stage, histologic subtype, and year of surgery), intraoperative findings (development of pulmonary fissures and degree of pleural adhesion), segments resected, combined with wedge resection or not. The development of pulmonary fissures was defined as well-developed (entirely separate lobes or parenchymal fusion at the base of fissure) and incomplete development (complete fusion without fissure line or visceral cleft left for part of the fissure). The pleural adhesion was classified according to the occupied fraction in the thoracoscopic view and was recorded as a binary outcome. Histological subtype was established according to the World Health Organization classification. TNM stage was determined according to the 8th edition of the TNM classification for lung cancer (22).
Outcome variables included the number of lymph nodes retrieved, the volume of intraoperative blood loss, operative time, intraoperative conversion to thoracotomy, the drainage volume within the first 3 postoperative days, the total drainage volume, the length of hospital stay, hospitalization cost, the incidence of postoperative complications (pulmonary infection, persistent air leakage, chylothorax, etc.), and survival. The blood loss was monitored by reading the scale on the collecting bottle connecting to our suction. The drainage volume in the first 3 postoperative days could reflect the recovery in the postoperative period close to surgery, which served as an addition to the total drainage volume. The pulmonary infection was diagnosed according to the following criteria: at least one of the chest radiological terms (such as new pulmonary infiltrates, consolidation, or opacity), combined with at least one of the examination terms (such as fever higher than 38 ℃ or abnormal leucocyte count less than 4×109/L or more than 12×109/L) or at least two of the symptoms (such as abnormal changes in respiratory secretions, new onset or aggravated cough). Persistent air leakage was defined as persistent air leaks lasting over 5 days.
OS was defined as the time from surgery to death. Progression-free survival (PFS) was defined as the time from surgery to any type of progression, including recurrence, metastasis, and death. The follow-up plans were scheduled for patients at discharge with CT examination every 3 or 6 months since the surgery. Clinical visits and telephone follow-ups were conducted.
Indication for segmentectomy
Indications for intended segmentectomy included: (I) peripheral nodule with a greater than or equal to 50% ground-glass appearance on preoperative CT with a diameter smaller than or equal to 2 cm; (II) solid nodule with a diameter smaller than or equal to 1 cm; (III) preoperative negative lymph nodes.
Surgical technique
All patients underwent general anesthesia and double-lumen intubation. The choice of uniportal or three-port was made based on experience and preferences of surgeons. Thoracoscopic segmentectomy was performed according to the methods previously described (13-17,19,23). After segmentectomy for major nodules, wedge resection would be performed on those additional small nodules identified in CT examination but unnecessary for segmentectomy. Lymph nodes were dissected according to NCCN guidelines (24). If unexpected circumstances occur during uniportal thoracoscopic segmentectomy, conversion to three-port VATS or thoracotomy would be considered. Postoperative analgesia, pulmonary rehabilitation, nutrition support, and drainage were routinely performed. The criteria for chest tube removal included no air leakage, drainage fluid less or equal to 300 mL/day, and complete expansion of the lungs.
Propensity score matching (PSM)
To minimize the influence of selection bias and potential confounders, PSM was performed. Propensity scores were calculated by a logistic regression model with the variables including age, sex, FEV1%, DLCO%, tumor size, clinical TNM stage, development of pulmonary fissures, degree of pleural adhesion, histology subtypes, segmentectomy types, surgeon volume, and the year of surgery. Surgeons with higher experience in segmentectomy were categorized into high-volume group, whereas those with moderate experience were categorized into low-volume group. The two groups were divided by a cut-off of 70 annual caseloads over the study period. The year of surgery was divided by 2017, after which the amount of uniportal segmentectomies in our center experienced a rapid growth (Figure S1A). Patients in the uniportal and three-port groups were matched at a ratio of 1:3 according to the propensity scores. The nearest greedy neighbor matching algorithm without replacement was used to identify PSM pairs. The balance of covariates was assessed with the standardized mean difference before and after matching. An absolute standardized mean difference less or equal to 0.1 indicated a balance in covariates between the 2 groups. The PSM was performed using the “matchit” package in R 4.0.2 (R Development Core Team, Vienna, Austria).
Statistical analysis
Data management and statistical analysis were performed using R software (version 4.1.0, R Development Core Team, Vienna, Austria). Patients’ baseline characteristics were characterized before and after matching. Appropriate descriptive statistics were used to summarize the variables. Quantitative variables were expressed as mean (standard deviation) or median [interquartile range (IQR)], and qualitative variables were expressed as numbers (ratio). For quantitative variables, the Kolmogorov-Smirnov test was used to test normal distribution. Perioperative outcomes were compared between the uniportal and three-port groups after matching. Student’s t-test was used for the quantitative variables conforming to a normal distribution, while Wilcoxon test was used for those not normally distributed. Qualitative variables were examined using Fisher’s exact test for comparisons between the two groups. The Kaplan-Meier survival curves were applied to depict the difference in OS and PFS between the two groups after matching. In addition to 1- and 3-year survival outcomes, we also preliminarily explored the long-term survival outcomes. We performed Fisher’s exact test to compare the rate of recurrence and metastasis between uniportal and three-port groups. All comparisons were two-tailed, a P value less than 0.05 was considered statistically significant.
Subgroup analyses
Subgroup analyses were performed according to prespecified segmentectomy types—simple, complex, and combined segmentectomies. Perioperative outcomes were also compared among three segmentectomy subgroups and the multiple regression analysis was performed on the association between segmentectomy subtypes and perioperative outcomes. The patients who underwent one site segmentectomy and other site segmentectomies, wedge resection, or sub-segmentectomies were classified as combined resection. The patients who only received one site segmentectomy were classified as simple and complex segmentectomy according to the complexity of the intersegmental plane (11,25,26). Simple segmentectomy was defined as segmental resection requiring a linear dissection of a single intersegmental plane, including the resection of S6, S7+8+9+10, LS1+2+3, and LS4+5. Resection of the other segments was considered a complex segmentectomy, which requires the dissection of two or more intersegmental planes.
Results
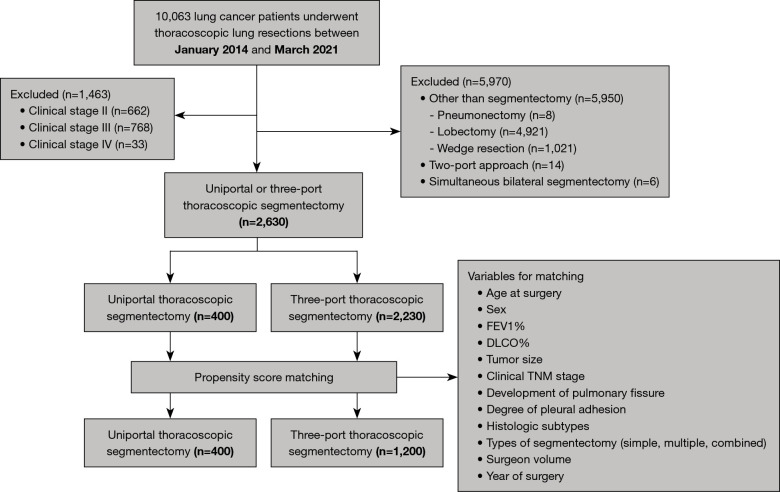
Of 10,063 lung cancer patients who underwent thoracoscopic lung resection from January 2014 to March 2021, 2,630 patients who received thoracoscopic segmentectomy were identified (uniportal: 400, three-port: 2,230). The flow chart was presented in Figures 1,2. The clinical characteristics of segmentectomy patients before and after PSM were presented in Table 1.
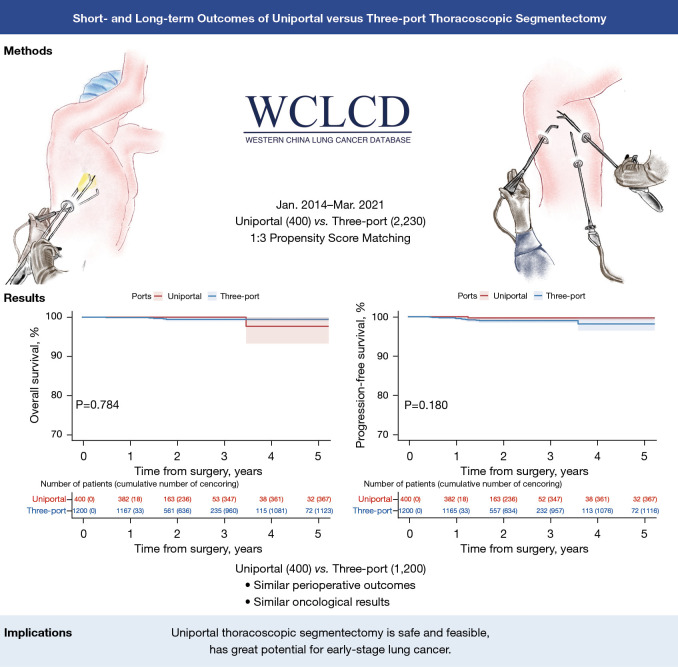
Figure 1.
Flowchart showing the methods, results, and implications of the study. Confidence limit, 95%.
Figure 2.
The flowchart summarizing the patients and propensity score matching. FEV1%, percentage of predicted FEV1 values; DLCO%, predicted diffusion capacity of carbon monoxide; TNM, tumor, node, and metastasis.
Table 1. Clinical characteristics of the included patients before and after propensity-score matching.
| Characteristics | Before PSM | After PSM | |||||
|---|---|---|---|---|---|---|---|
| Uniport (n=400) | Three-port (n=2,230) | P value | Uniport (n=400) | Three-port (n=1,200) | P value | ||
| Age at surgery (years) | <0.001 | 0.63 | |||||
| Mean (SD) | 52.40 (11.50) | 54.71 (11.33) | 52.40 (11.50) | 52.71 (11.42) | |||
| Median [IQR] | 52.00 [45.00, 60.00] | 54.00 [47.00, 63.00] | 52.00 [45.00, 60.00] | 53.00 [45.00, 60.25] | |||
| Sex | 0.12 | 0.65 | |||||
| Female | 290 (72.50) | 1527 (68.48) | 290 (72.50) | 854 (71.17) | |||
| Male | 110 (27.50) | 703 (31.52) | 110 (27.50) | 346 (28.83) | |||
| FEV1% | 0.43 | 0.85 | |||||
| Mean (SD) | 107.33 (14.87) | 106.58 (16.65) | 107.33 (14.87) | 107.51 (15.98) | |||
| Median [IQR] | 106.55 [98.10, 116.70] | 106.40 [97.10, 116.40] | 106.55 [98.10, 116.70] | 106.90 [97.80, 116.85] | |||
| DLCO% | 0.49 | 0.90 | |||||
| Mean (SD) | 101.79 (14.83) | 101.16 (15.86) | 101.79 (14.83) | 101.91 (15.39) | |||
| Median [IQR] | 99.60 [92.40, 111.70] | 100.20 [90.10, 110.60] | 99.60 [92.40, 111.70] | 100.55 [91.20, 110.60] | 0.85 | ||
| Tumor size (cm) | 0.014 | 0.95 | |||||
| Mean (SD) | 1.13 (0.49) | 1.20 (0.56) | 1.13 (0.49) | 1.13 (0.50) | |||
| Median [IQR] | 1.00 [0.80, 1.40] | 1.00 [0.80, 1.50] | 1.00 [0.80, 1.40] | 1.00 [0.80, 1.40] | |||
| Clinical stage | 0.47 | >0.99 | |||||
| IA | 398 (99.50) | 2,207 (98.97) | 398 (99.50) | 1,192 (99.33) | |||
| IB | 2 (0.50) | 23 (1.03) | 2 (0.50) | 8 (0.67) | |||
| Development of pulmonary fissure | <0.001 | >0.99 | |||||
| Well | 246 (61.81) | 914 (41.58) | 246 (61.81) | 731 (61.90) | |||
| Incomplete | 152 (38.19) | 1,284 (58.42) | 152 (38.19) | 450 (38.10) | |||
| Missing | 2 (0.50) | 32 (1.43) | 2 (0.50) | 19 (1.50) | |||
| Pleural adhesions | 0.28 | 0.28 | |||||
| No | 133 (33.42) | 675 (30.54) | 133 (33.42) | 362 (30.34) | |||
| Yes | 265 (66.58) | 1,535 (69.46) | 265 (66.58) | 831 (69.66) | |||
| Missing | 2 (0.50) | 20 (0.89) | 2 (0.50) | 7 (0.58) | |||
| Histology | 0.14 | 0.39 | |||||
| AAH | 1 (0.28) | 27 (1.39) | 1 (0.28) | 18 (1.72) | |||
| AIS | 15 (4.27) | 87 (4.47) | 15 (4.27) | 34 (3.24) | |||
| MIA | 174 (49.57) | 836 (42.94) | 174 (49.57) | 535 (51.00) | |||
| Invasive adenocarcinoma | 148 (42.17) | 894 (45.92) | 148 (42.17) | 429 (40.90) | |||
| Squamous | 0 (0.00) | 10 (0.51) | 0 (0) | 0 (0) | |||
| Others* | 2 (0.57) | 10 (0.51) | 2 (0.57) | 5 (0.48) | |||
| Missing | 11 (3.13) | 83 (4.26) | 11 (3.13) | 28 (2.67) | |||
| Type of segments resected | 0.13 | 0.68 | |||||
| Simple | 123 (30.75) | 648 (29.06) | 96 (24.00) | 264 (22.00) | |||
| Complex | 181 (45.25) | 1,124 (50.40) | 181 (45.25) | 566 (47.17) | |||
| Combined | 96 (24.00) | 458 (20.54) | 123 (30.75) | 370 (30.83) | |||
| With segmentectomy | 9 (2.25) | 113 (5.06) | 9 (2.25) | 58 (4.83) | |||
| With wedge resection | 87 (21.75) | 345 (15.47) | 87 (21.75) | 206 (17.17) | |||
| Surgeon volume | <0.001 | 0.86 | |||||
| Low | 263 (65.75) | 1,221 (54.75) | 263 (65.75) | 781 (65.08) | |||
| High | 137 (34.25) | 1,009 (45.25) | 137 (34.25) | 419 (34.92) | |||
| Year of surgery | <0.001 | 0.83 | |||||
| 2014–2017 | 48 (12.00) | 649 (29.10) | 48 (12.00) | 151 (12.58) | |||
| 2018–2021 | 352 (88.00) | 1,581 (70.90) | 352 (88.00) | 1,049 (87.42) | |||
Data were presented as mean (SD), median [IQR] or number (percentage). *, others including large cell carcinoma, undifferentiated cancers, neuroendocrine tumor, salivary gland tumor and adenosquamous carcinoma. PSM, propensity-score matching; IQR, interquartile range; FEV1%, predicted forced expiratory volume in 1 second; DLCO%, predicted carbon monoxide diffusing capacity; AAH, atypical adenomatous hyperplasia; AIS, adenocarcinoma in situ; MIA, minimally invasive adenocarcinoma.
Baseline characteristics before and after matching
Age, tumor size, development of pulmonary fissures, type of segments resected, surgeon volume, and year of surgery were significantly different between uniportal and three-port thoracoscopic segmentectomy before matching. Uniportal thoracoscopic segmentectomy group presented with smaller age than three-port group (52.40±11.50 vs. 54.71±11.33 years old, P<0.001). The proportion of patients with well-developed pulmonary fissures was higher in the uniportal group (61.81% vs. 41.58%, P<0.001). The annual number of uniportal thoracoscopic segmentectomies increased from 2014 to 2020 (Figure S1A). The proportion of uniportal thoracoscopic segmentectomy increased from 16.67% in 2014 to 42.5% in 2021.
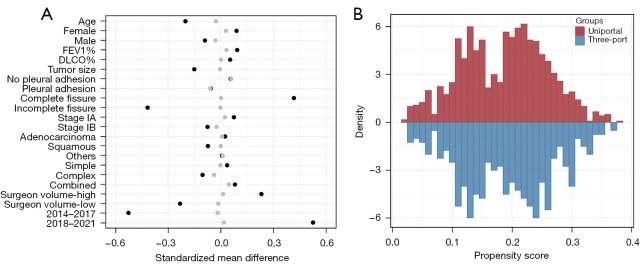
The PSM identified 1,600 patients (uniportal: 400, three-port: 1,200). The standardized mean differences were all under 0.1 and the propensity scores between two groups were balanced (Figure 3). No significant differences in baseline characteristics were identified between the two groups after matching (Table 1).
Figure 3.
(A) Standardized differences of variables between the patients who underwent uniportal and three-port thoracoscopic segmentectomy. Black circles and grey circles indicated differences before and after matching, respectively. Propensity score matching effectively minimize the difference of baseline characteristics between the 2 groups. (B) Mirror histogram of propensity score for the patients who underwent uniportal (above the horizontal line at zero) and three-port thoracoscopic segmentectomy (below the horizontal line at zero). Similar score distribution was found in the 2 matched groups. FEV1%, predicted forced expiratory volume in 1 second; DLCO%, predicted carbon monoxide diffusing capacity.
Perioperative outcomes after matching
The comparisons of the perioperative outcomes between the uniportal and three-port arms after matching were reported in Table 2.
Table 2. Perioperative outcomes between uniportal and three-port patients after matching.
| Outcomes | Uniportal (n=400) | Three-port (n=1,200) | P value |
|---|---|---|---|
| Convert to thoracotomy | 0 (0.00) | 6 (0.50) | 0.35 |
| Number of LNs harvested | 0.11 | ||
| Mean (SD) | 6.38 (2.97) | 6.70 (3.53) | |
| Median [IQR] | 6.00 [4.00, 8.00] | 6.00 [4.00, 9.00] | |
| Number of LN stations harvested | 0.02 | ||
| Mean (SD) | 4.43 (1.53) | 4.68 (1.98) | |
| Median [IQR] | 4.00 [3.00, 5.00] | 4.00 [3.00, 6.00] | |
| Intraoperative blood loss (mL) | <0.001 | ||
| Mean (SD) | 30.98 (11.88) | 43.78 (8.51) | |
| Median [IQR] | 23.38 [23.38, 48.75] | 41.48 [34.86, 56.14] | |
| Operative time (min) | <0.001 | ||
| Mean (SD) | 106.95 (32.20) | 98.47 (38.09) | |
| Median [IQR] | 105.00 [81.25, 125.00] | 90.00 [70.00, 120.00] | |
| Postoperative hospital stay (days) | 0.14 | ||
| Mean (SD) | 4.25 (2.03) | 4.17 (2.29) | |
| Median [IQR] | 4.00 [3.00, 5.00] | 4.00 [3.00, 4.00] | |
| Hospitalization cost (kUSD) | <0.001 | ||
| Mean (SD) | 7.58 (1.47) | 7.24 (1.51) | |
| Median [IQR] | 7.31 [6.67, 8.16] | 7.05 [6.31, 7.95] | |
| Chest tube drainage (mL) | |||
| Within the first 3 postoperative days | 0.45 | ||
| Mean (SD) | 352.39 (224.73) | 341.01 (268.60) | |
| Median [IQR] | 320.00 [185.00, 480.00] | 290.00 [140.00, 465.00] | |
| Total drainage | |||
| Mean (SD) | 413.18 (372.24) | 433.94 (633.61) | 0.54 |
| Median [IQR] | 330.00 [197.50, 510.00] | 300.00 [140.00, 517.50] | 0.059 |
| Postoperative complications | 17 (4.25) | 56 (4.67) | 0.84 |
| Pulmonary infection | 6 (1.50) | 12 (1.00) | 0.58 |
| Persistent air leakage | 8 (2.00) | 19 (1.58) | 0.74 |
| Chylothorax | 1 (0.25) | 8 (0.67) | 0.56 |
| Others* | 5 (1.25) | 19 (1.58) | 0.81 |
Data were presented as mean (SD), median [IQR], or number (%). *, other included atelectasis, respiratory failure, surgical site infection, subcutaneous emphysema, arrhythmia, and cerebral infarction. IQR, interquartile range; LNs, lymph nodes.
Altogether, 6 of 1,200 patients intraoperatively converted to thoracotomy were attributed to severe intraoperative bleeding in the three-port arm, whereas no patients underwent intraoperative conversion to thoracotomy or three-port VATS in the uniportal arm. No significant difference was found between the 2 groups regarding the lymph node numbers harvested (6.38±2.97 vs. 6.70±3.53, P=0.11). Fewer lymph node stations (4.43±1.53 vs. 4.68±1.98, P=0.02) were harvested in the uniportal arm than those in the three-port group. The lymph node numbers and stations harvested remained generally consistent during the past 7 years (Figure S1B,S1C).
Uniportal thoracoscopic segmentectomy was associated with less intraoperative blood loss (30.98±11.88 vs. 43.78±8.51 mL, P<0.001), longer operative time (106.95±32.2 vs. 98.47±38.09 min, P<0.001), and higher hospitalization cost (7.58±1.47 vs. 7.24±1.51 kUSD, P<0.001) (Table 2). Similar length of postoperative hospital stay was found between the 2 groups. The intraoperative blood loss of most cases in the 2 groups was less than 50 mL during the past 6 years (Figure S1D). Both uniportal and three-port thoracoscopic segmentectomy showed a decreasing trend regarding operative time and postoperative hospital stay from 2014 to 2021 (Figure S1E,S1F). No significant difference was found between the two groups in terms of chest tube drainage volume within the first 3 days and total chest tube drainage volume.
Uniportal thoracoscopic segmentectomy showed similar incidence of overall postoperative complications (4.25% vs. 4.67%, P=0.84), pulmonary infection (1.50% vs. 1%, P=0.58), persistent air leakage (2% vs. 1.58%, P=0.74), and chylothorax (0.25% vs. 0.67%, P=0.56) (Table 2, Figure S2).
Subgroup analysis for perioperative outcomes
Of 1,600 segmentectomies after matching, 493 were simple segmentectomies (uniportal:three-port =123:370), 747 were complex segmentectomies (uniportal:three-port =181:566), and 360 were combined segmentectomies (uniportal:three-port =96:264). No significant differences in most of baseline characteristics were identified between uniportal and three-port groups in each subgroup (Table S1).
In simple segmentectomy, uniportal segmentectomy showed less intraoperative blood loss (33.01±12.45 vs. 44.02±8.46 mL, P<0.001), and similar operative time, hospitalization cost and postoperative complication rate compared with three-port segmentectomy. In complex segmentectomy, uniportal segmentectomy showed less intraoperative blood loss (31.85±12.39 vs. 44.22±8.59 mL, P<0.001), longer operative time (109.25±32.62 vs. 93.32±33.54 min, P<0.001), higher hospitalization cost (7.28±1.18 vs. 6.82±1.15 kUSD, P<0.001), and similar postoperative complication rate compared with three-port segmentectomy. In combined segmentectomy, uniportal segmentectomy showed less intraoperative blood loss (26.73±8.84 vs. 42.52±8.31 mL, P<0.001), similar hospital stays, operative time, hospitalization cost, and postoperative complication rate (Table S2). We found that number of lymph node stations harvested was gradually increased from simple, complex, to combined segmentectomy (Table S3). The multivariate regression analysis on each postoperative outcome showed similar results (Figure S3).
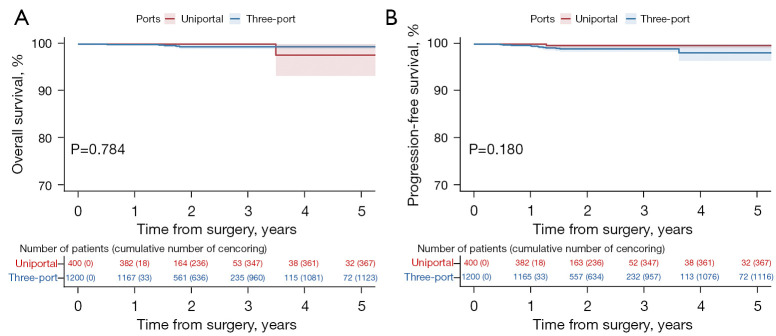
OS and PFS
The mean follow-up duration was 27 months (range, 1–101 months). Uniportal and three-port thoracoscopic segmentectomy showed similar 1-year [100% vs. 99.9% (95% CI: 99.7–100%), P=0.36], 3-year [100% vs. 90.4% (95% CI: 99.0–99.9%), P=0.20], and 5-year [97.7% (95% CI: 93.3–100%) vs. 99.4% (95% CI: 99.0–99.9%), P=0.78] OS (Figure 4A).
Figure 4.
Survival curves according to the ports. Red solid line depicted uniportal thoracoscopic segmentectomy, blue solid line depicted three-port segmentectomy. (A) Overall survival curves. The difference in 5-year overall survival is not significant (P=0.784). (B) Progression-free survival curves. The difference in 5-year progression-free survival is not significant (P=0.180). Confidence limit, 95%.
A total of 0.5% (2/400) of patients experienced recurrence in the uniportal group, and 0.41% (5/1,200) of patients experienced recurrence in the three-port group (P=0.85). Altogether 0.25% (1/400) of patients experienced metastasis in the uniportal group (brain: 1), and 0.58% (7/1,200) of patients in the three-port group (lung: 1; bone: 3; spleen: 1; brain: 1; brain and bone: 1) (P=0.68).
Uniportal and three-port thoracoscopic segmentectomy showed similar 1-year PFS [100% vs. 99.7% (95% CI: 98.4–99.6%), P=0.13], 3-year PFS [99.7% (95% CI: 99.1–100%) vs. 99.0% (95% CI: 98.4–99.6%), P=0.16], 5-year PFS [99.7% (95% CI: 99.1–100%) vs. 98.2% (95% CI: 96.5–99.9%), P=0.18] (Figure 4B).
Subgroup analysis for survival
For simple segmentectomy, the uniportal group and three-port group showed similar 5-year OS (100.0% vs. 100.0%, P>0.99) (Figure S4A). Similar OS between the 2 groups was also noticed in the complex or combined segmentectomy subgroups (Figure S4B,S4C). Similar 5-year PFS (100.0% vs. 96.8%, P=0.77) were found between the 2 groups in simple segmentectomy (Figure S4D), as well as in the patients who underwent complex or combined segmentectomy (Figures S4E,S4F).
Discussion
With the increasing focus on instruments development and surgical techniques and the increasing number of small nodules detected by CT, the question of whether less trauma leads to recovery benefits and similar oncological outcomes is currently being addressed by surgeons. Since then, uniportal VATS has been tried in clinical practice, ranging from wedge resection for pulmonary biopsy and pneumothorax, to lobectomy and segmentectomy for lung cancer resection (6,27-29). The superiority of uniportal VATS than three-port VATS in terms of perioperative outcomes was inconsistent. Two meta-analyses, which included either all thoracic surgery or the surgery for T1-3N0M0 non-small cell lung cancer, reported better perioperative outcomes in the uniportal VATS (8,30). An updated meta-analysis included lung cancer surgery identified comparable outcomes regarding to operative time, blood loss, drainage duration, and length of stays (9). Uniportal VATS is reported to be safe and feasible for more accurate pulmonary segmentectomy after complying with surgical indications (31). We also reported the feasibility of uniportal single-direction segmentectomy with a series of novel methods (17,19). In this article, we creatively evaluated the perioperative and oncological outcomes of uniportal and three-port segmentectomies. We provided first-hand information on the application of uniportal segmentectomy.
We note that OS and PFS were similar between uniportal and three-port thoracoscopic segmentectomy. The survival was better than those reported in previous studies (12,32,33). The JCOG0802 trial included NSCLC patients in stage IA with consolidation-to-tumor ratio over 0.5, and compared postoperative survival between lobectomy and segmentectomy (12). They reported that the patients who underwent segmentectomy had 5-year OS of 94.3% (12). Of note, more than 99% of the cases involved in our study were in stage IA, and more than 80% of cases were either minimally invasive adenocarcinoma or invasive adenocarcinoma. This may contribute to such a satisfactory survival. We might believe that uniportal segmentectomy could provide a similar oncological effect with the current survival results of stage I lung cancer.
We found that uniportal approach harvested fewer lymph node stations (4.43 vs. 4.68) and similar number of total lymph nodes harvested than three-port approach. However, the mean difference of lymph node stations harvested between the 2 groups was 0.25, indicating limited clinical significance. A systematic review indicated the number difference of lymph node harvested between uniportal and three-port regimen remains controversial and needs to be further identified (34). Of note, decreased lymph node retrieval may not affect survival in this population of patients with T1a disease but may be a more significant issue in more advanced stage patients.
We noticed a decrease in operative time over the past six years, indicating improved surgical techniques. We found that the uniportal group was associated with a longer operative time. This difference was of limited clinical significance for the following reasons. (I) The difference in the mean operative time was 8.48 min between the 2 groups, 8.48 min was very short, and the ratio of 8.48 to 106.95 or 98.47 was pretty small. (II) We initialized three-port VATS segmentectomy from 2005 and uniportal VATS segmentectomy from 2014. To minimize the heterogeneity over the years of recruitment, we included all patients who underwent segmentectomy from 2014 to 2021. During this period, three-port thoracoscopic segmentectomy entered a “mature stage”, while uniportal thoracoscopic segmentectomy was in an “growth stage”. Surgical instruments, operating planes, and team cooperation in uniportal thoracoscopic surgery have been gradually improved. This was followed by an increase in surgical experience and techniques. And ultimately it would translate into improvement in outcomes, including shorter operative time, less intraoperative blood loss, and less intraoperative complications like major hemorrhage (35).
We also noticed that the uniportal group was associated with less intraoperative blood loss (30.98 vs. 43.78 mL) compared with those in the three-port group. Of note, the difference of intraoperative blood loss was 12.8 mL, and the mean blood loss in both groups was far from major bleeding. Our findings were in accord with a previous meta-analysis indicating that uniportal group showed less blood loss for lung cancer (30). The benefit of less intraoperative blood loss in the uniportal regimen was also identified in the patients who underwent simple, complex, and combined segmentectomy.
At an early stage, surgeons at our center selected cases with smaller tumor sizes and fewer solid components, for whom systematic lymph node dissection was not typically required. As surgical techniques and coordination matured, we gradually recruited patients with more vascular variation in basal segment, combined lung segment and other difficult cases. There has also been an increase in the case number of our center over the past six years, indicating that surgeon experience was improving. We also included surgeon experience and year of surgery as variables in the PSM.
Although the patients who underwent uniportal thoracoscopic segmentectomy had similar postoperative hospital stays and incidence of postoperative complications, the uniportal approach was found to be more expensive than the three-port approach. The increase in cost may be related to the application of new surgical instruments (36). Indeed, as equipment became more sophisticated, instruments for a new and innovative surgical technique may be more expensive than those for previous techniques. Besides, the length of the stapler used was 45 mm in the uniportal arm and 60 mm in the three-port arm. This meant that more staplers would be needed in uniportal segmentectomy, contributing to the higher hospitalization cost. However, we cannot extract the detailed cost due to the retrospective nature. Further research is needed to determine whether the increased costs translate into better outcomes for the patients, and the pros and cons need to be balanced.
We subdivided segmentectomy into simple, complex, and combined segmentectomy according to resection sites and intersegmental plane complexity. In contrast to simple segmentectomy, complex segmentectomy needs to deal with at least two intersegmental planes. Combined segmentectomy is needed to resect two or more sites. This subgroup consisted of combined segmentectomies as well as the combination of segmentectomy and wedge resection. In some cases, we would perform wedge resection on additional small, palpable nodules after segmentectomy for major nodules. One concern is surgery safety for uniportal complex and combined segmentectomy. In each subgroup, we found less intraoperative blood loss, and similar converted thoracotomy rate and postoperative complication rate in the uniportal regimen compared with that in the three-port regimen. Another concern is oncological outcome. It is challenging to guarantee adequate lymph nodes resected and surgical margin in both uniportal complex and combined segmentectomy. Here, we found similar OS and PFS in each subgroup. This demonstrates that uniportal complex and combined segmentectomy are safe and feasible.
Some limitations of this study need to be acknowledged. First, this was a single-center retrospective study. Although we used PSM to reduce bias and ensure study cogency, there may still be unobserved confounding and selection bias between the two groups. Compared to lobectomy, segmentectomy was a newly emerged alternative and more technically challenging. Uniportal segmentectomy was even more technically demanding. The decision to apply uniportal or three-port might be affected by the complexity of the case. Although our center has accumulated experiences in uniportal segmentectomies, the presence of selection bias was unavoidable. Second, the mean follow-ups of our patients were limited to derive the results of long-term survival outcomes. Comparisons of 5-year survival outcomes from our study should be interpreted with caution. We continue to follow-up on our patients and look forward to more conclusive conclusions in further studies. Third, nearly half of the patients were minimal invasive adenocarcinoma which would lead to minimal impact on survival. This limited the power to discriminate between the uniportal and three-port approach for oncological results. Fourth, some variables, such as postoperative pain and detailed hospitalization costs, were not collected. We look forward to prospective studies that include those variables and provide a more comprehensive evaluation. Fifth, there were missing values in our baseline characteristics. But the proportion of missing values were all under 5% and mostly under 2%. The bias from missing values should be limited. Finally, we subdivided the patients into subgroups based on sites resected and complexity of segmentectomy; however, the sample size in each subgroup was limited. Further exploration of the subtypes of segmentectomy is needed. Large randomized controlled trials are also needed to provide more definitive evidence, which might contribute to the development of a uniform standard for generalizing uniportal thoracoscopic segmentectomy.
Conclusions
In conclusion, uniportal thoracoscopic segmentectomy for lung cancer resulted in less intraoperative blood loss and similar oncological outcomes. Uniportal thoracoscopic segmentectomy is a safe and feasible alternative to the three-port approach.
Supplementary
The article’s supplementary files as
Acknowledgments
We sincerely thank Xiaoqin Zhou from Center of Biostatistics, Design, Measurement and Evaluation (CBDME), Department of Clinical Research Management, West China Hospital, Sichuan University, Chengdu, Sichuan, China, for her statistical guide on our manuscript.
Funding: This work was supported by 1.3.5 Project for Disciplines of Excellence, West China Hospital, Sichuan University (No. ZYGD18021 to Dr. Lunxu Liu, No. ZYJC18009 to Dr. Jiandong Mei).
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the Ethics Committee of West China Hospital of Sichuan University (No. 2021-1027). The requirement of informed consent was waived due to retrospective nature.
Footnotes
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at https://tlcr.amegroups.com/article/view/10.21037/tlcr-22-635/rc
Data Sharing Statement: Available at https://tlcr.amegroups.com/article/view/10.21037/tlcr-22-635/dss
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://tlcr.amegroups.com/article/view/10.21037/tlcr-22-635/coif). The authors have no conflicts of interest to declare.
References
- 1.Ginsberg RJ, Rubinstein LV. Randomized trial of lobectomy versus limited resection for T1 N0 non-small cell lung cancer. Lung Cancer Study Group. Ann Thorac Surg 1995;60:615-22; discussion 622-3. 10.1016/0003-4975(95)00537-U [DOI] [PubMed] [Google Scholar]
- 2.Zhu Y, Xu GB, Lei CG, et al. Thoracic surgery: single-port video-assisted thoracoscopic lobectomy. Ann Transl Med 2015;3:143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mineo TC, Ambrogi V. A glance at the history of uniportal video-assisted thoracic surgery. J Vis Surg 2017;3:157. 10.21037/jovs.2017.10.11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Liu CC, Shih CS, Pennarun N, et al. Transition from a multiport technique to a single-port technique for lung cancer surgery: is lymph node dissection inferior using the single-port technique?†. Eur J Cardiothorac Surg 2016;49 Suppl 1:i64-72. [DOI] [PubMed] [Google Scholar]
- 5.Duan L, Jiang G, Yang Y. One hundred and fifty-six cases of anatomical pulmonary segmentectomy by uniportal video-assisted thoracic surgery: a 2-year learning experience. Eur J Cardiothorac Surg 2018;54:677-82. 10.1093/ejcts/ezy142 [DOI] [PubMed] [Google Scholar]
- 6.Gonzalez D, Paradela M, Garcia J, et al. Single-port video-assisted thoracoscopic lobectomy. Interact Cardiovasc Thorac Surg 2011;12:514-5. 10.1510/icvts.2010.256222 [DOI] [PubMed] [Google Scholar]
- 7.Gonzalez-Rivas D, Paradela M, Fieira E, et al. Single-incision video-assisted thoracoscopic lobectomy: initial results. J Thorac Cardiovasc Surg 2012;143:745-7. 10.1016/j.jtcvs.2011.07.049 [DOI] [PubMed] [Google Scholar]
- 8.Abouarab AA, Rahouma M, Kamel M, et al. Single Versus Multi-Incisional Video-Assisted Thoracic Surgery: A Systematic Review and Meta-analysis. J Laparoendosc Adv Surg Tech A 2018;28:174-85. 10.1089/lap.2017.0446 [DOI] [PubMed] [Google Scholar]
- 9.Yan Y, Huang Q, Han H, et al. Uniportal versus multiportal video-assisted thoracoscopic anatomical resection for NSCLC: a meta-analysis. J Cardiothorac Surg 2020;15:238. 10.1186/s13019-020-01280-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mazzone PJ, Silvestri GA, Patel S, et al. Screening for Lung Cancer: CHEST Guideline and Expert Panel Report. Chest 2018;153:954-85. 10.1016/j.chest.2018.01.016 [DOI] [PubMed] [Google Scholar]
- 11.Suzuki K, Saji H, Aokage K, et al. Comparison of pulmonary segmentectomy and lobectomy: Safety results of a randomized trial. J Thorac Cardiovasc Surg 2019;158:895-907. 10.1016/j.jtcvs.2019.03.090 [DOI] [PubMed] [Google Scholar]
- 12.Saji H, Okada M, Tsuboi M, et al. Segmentectomy versus lobectomy in small-sized peripheral non-small-cell lung cancer (JCOG0802/WJOG4607L): a multicentre, open-label, phase 3, randomised, controlled, non-inferiority trial. Lancet 2022;399:1607-17. 10.1016/S0140-6736(21)02333-3 [DOI] [PubMed] [Google Scholar]
- 13.Zhu Y, Mei J, Liu L. The application of a single-direction strategy in VATS segmentectomy: left S3 segmentectomy. Ann Transl Med 2018;6:410. 10.21037/atm.2018.09.64 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Pu Q, Liu C, Guo C, et al. Stem-Branch: A Novel Method for Tracking the Anatomy During Thoracoscopic S9-10 Segmentectomy. Ann Thorac Surg 2019;108:e333-5. 10.1016/j.athoracsur.2019.05.046 [DOI] [PubMed] [Google Scholar]
- 15.Zhu Y, Pu Q, Liu C, et al. Trans-Inferior-Pulmonary-Ligament Single-Direction Thoracoscopic RS9 Segmentectomy: Application of Stem-Branch Method for Tracking Anatomy. Ann Surg Oncol 2020;27:3092-3. 10.1245/s10434-020-08309-9 [DOI] [PubMed] [Google Scholar]
- 16.Liu C, Liao H, Guo C, et al. Single-direction thoracoscopic basal segmentectomy. J Thorac Cardiovasc Surg 2020;160:1586-94. 10.1016/j.jtcvs.2020.01.028 [DOI] [PubMed] [Google Scholar]
- 17.Liu C, Ma L, Guo C, et al. Non-grasping en bloc mediastinal lymph node dissection through uniportal video-assisted thoracic surgery for lung cancer surgery. J Thorac Dis 2016;8:2956-9. 10.21037/jtd.2016.10.77 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Liu C, Wang W, Mei J, et al. Uniportal Thoracoscopic Single-Direction Basal Subsegmentectomy (Left S10a+ci): Trans-Inferior-Pulmonary-Ligament Approach. Ann Surg Oncol 2022;29:1389-91. 10.1245/s10434-021-10806-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Zhu Y, Xia L, Liu C, et al. Uniportal Single-Direction Thoracoscopic Right S9 Segmentectomy: Trans-Inferior-Pulmonary-Ligament Approach. Ann Surg Oncol 2021;28:6407. 10.1245/s10434-021-10033-x [DOI] [PubMed] [Google Scholar]
- 20.Tang Y, Liu C, Guo C, et al. Uniportal video-assisted thoracic surgery basal segmentectomy: a single-center retrospective cohort study. Transl Lung Cancer Res 2022;11:2125-35. 10.21037/tlcr-22-651 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.von Elm E, Altman DG, Egger M, et al. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Lancet 2007;370:1453-7. 10.1016/S0140-6736(07)61602-X [DOI] [PubMed] [Google Scholar]
- 22.Goldstraw P, Chansky K, Crowley J, et al. The IASLC Lung Cancer Staging Project: Proposals for Revision of the TNM Stage Groupings in the Forthcoming (Eighth) Edition of the TNM Classification for Lung Cancer. J Thorac Oncol 2016;11:39-51. 10.1016/j.jtho.2015.09.009 [DOI] [PubMed] [Google Scholar]
- 23.Liu L, Che G, Pu Q, et al. A new concept of endoscopic lung cancer resection: Single-direction thoracoscopic lobectomy. Surg Oncol 2010;19:e71-7. 10.1016/j.suronc.2009.04.005 [DOI] [PubMed] [Google Scholar]
- 24.Network NCC. NCCN Clinical Practice Guidelines in Oncology. Non-Small Cell Lung Cancer, Version 5. 2021. Available online: https://www.nccn.org/professionals/physician_gls/pdf/nscl.pdf
- 25.Handa Y, Tsutani Y, Mimae T, et al. Surgical Outcomes of Complex Versus Simple Segmentectomy for Stage I Non-Small Cell Lung Cancer. Ann Thorac Surg 2019;107:1032-9. 10.1016/j.athoracsur.2018.11.018 [DOI] [PubMed] [Google Scholar]
- 26.Handa Y, Tsutani Y, Mimae T, et al. Complex segmentectomy in the treatment of stage IA non-small-cell lung cancer. Eur J Cardiothorac Surg 2020;57:114-21. 10.1093/ejcts/ezz185 [DOI] [PubMed] [Google Scholar]
- 27.Rocco G, Martin-Ucar A, Passera E. Uniportal VATS wedge pulmonary resections. Ann Thorac Surg 2004;77:726-8. 10.1016/S0003-4975(03)01219-0 [DOI] [PubMed] [Google Scholar]
- 28.Jutley RS, Khalil MW, Rocco G. Uniportal vs standard three-port VATS technique for spontaneous pneumothorax: comparison of post-operative pain and residual paraesthesia. Eur J Cardiothorac Surg 2005;28:43-6. 10.1016/j.ejcts.2005.02.039 [DOI] [PubMed] [Google Scholar]
- 29.Han KN, Kim HK, Lee HJ, et al. Single-port video-assisted thoracoscopic pulmonary segmentectomy: a report on 30 cases†. Eur J Cardiothorac Surg 2016;49 Suppl 1:i42-7. [DOI] [PubMed] [Google Scholar]
- 30.Yang X, Li M, Yang X, et al. Uniport versus multiport video-assisted thoracoscopic surgery in the perioperative treatment of patients with T1-3N0M0 non-small cell lung cancer: a systematic review and meta-analysis. J Thorac Dis 2018;10:2186-95. 10.21037/jtd.2018.03.74 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Wang C, Wu S, Zhang R, et al. Identifying Lung Cancer Patients Suitable for Segmentectomy: A Brief Review. Front Surg 2021;8:637441. 10.3389/fsurg.2021.637441 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Zhao ZR, Situ DR, Lau RWH, et al. Comparison of Segmentectomy and Lobectomy in Stage IA Adenocarcinomas. J Thorac Oncol 2017;12:890-6. 10.1016/j.jtho.2017.01.012 [DOI] [PubMed] [Google Scholar]
- 33.Xie D, Wu J, Hu X, et al. Uniportal versus multiportal video-assisted thoracoscopic surgery does not compromise the outcome of segmentectomy. Eur J Cardiothorac Surg 2021;59:650-7. 10.1093/ejcts/ezaa372 [DOI] [PubMed] [Google Scholar]
- 34.Sihoe ADL. Uniportal Lung Cancer Surgery: State of the Evidence. Ann Thorac Surg 2019;107:962-72. 10.1016/j.athoracsur.2018.08.023 [DOI] [PubMed] [Google Scholar]
- 35.Gonzalez-Rivas D, Stupnik T, Fernandez R, et al. Intraoperative bleeding control by uniportal video-assisted thoracoscopic surgery†. Eur J Cardiothorac Surg 2016;49 Suppl 1:i17-24. [DOI] [PubMed] [Google Scholar]
- 36.Ji C, Xiang Y, Pagliarulo V, et al. A multi-center retrospective study of single-port versus multi-port video-assisted thoracoscopic lobectomy and anatomic segmentectomy. J Thorac Dis 2017;9:3711-8. 10.21037/jtd.2017.09.39 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
The article’s supplementary files as