Abstract
Backgroud
In recent years the pre‐auricular area is increasingly used for filler injections.
Aims
Assessment of depth of the subcutaneous fat and the process of realtime filler injection.
Materials & Methods
Ultrasonographic data of two cases and a video are studied.
Results
These show how filler injections may very easily be delivered inside the parotid gland. This may go unnoticed by injector and client.
Discussion
This study and data from literature prove that filler injections in the pre‐auricular area may end up inside or in the vicinity of the parotid gland, and this can lead to an inflammatory response.
Conclusion
It is recommended to be careful with filler injections in this area. Prior sonographic assessment of the subcutaneous depth in this area is advised.
Keywords: complications, duplex ultrasound, filler, parotid gland
1. INTRODUCTION
The pre‐auricular (parotid‐masseteric) area is a region that for many years has largely been ignored in filler augmentation. However in particular for increasing lateral facial width in males and enhance the mandibular angle prominence filler treatment has been advised 1 , 2 and is now been performed on a regular basis. Recently, we encountered two patients with complications. Their cases are presented in conjunction with a video of an event we experienced ourselves in this area. We feel that lessons can be learned about the challenges this region poses in filler injection therapy.
2. DESCRIPTION OF CASES
2.1. Case 1
A 50‐year‐old female patient was treated with 2 × 1 ml hyaluronic acid filler (Volux®, Allergan) in the jawline and pre‐auricular area. Six months later, being one month after a Covid infection, the patient noticed an increasing swelling, pain, and other signs of inflammation on the left side of her jaw (Figure 1). At the moment of presentation, the right side of her jaw seemed to start swelling also. Clinical examination revealed a 1x1 cm open wound with underlying abscess on the left side of the jaw 2 cm caudal from the temporomandibular joint. On the right side of the face, a non‐fluctuant swelling was observed in the pre‐auricular region. Duplex ultrasound imaging displayed multiple anechoic pockets in the parotid gland on both sides of the face (Figures 2A,B). On the left side, an abscess was found to connect with a tunnel to the filler material inside the parotid gland (Figure 2B). Hyaluronidase 3× 150 units (Hyason®, Organon) was injected under ultrasound guidance into the pockets. Oral antibiotic medication was given, that is, amoxicillin/clavulanic acid (500/125 mg) for 10 days in addition to prednisone in tapering dosage for 7 days. At follow‐up after 4 days, the swelling had diminished on both sides of the face. Duplex ultrasound displayed only a few residual pockets mainly on the right side. An additional 150 units of hyaluronidase were injected into the remaining pockets. One week later, pain and abscess were gone.
FIGURE 1.

Left side of the face of patient in case 1: remnant of abscess
FIGURE 2.
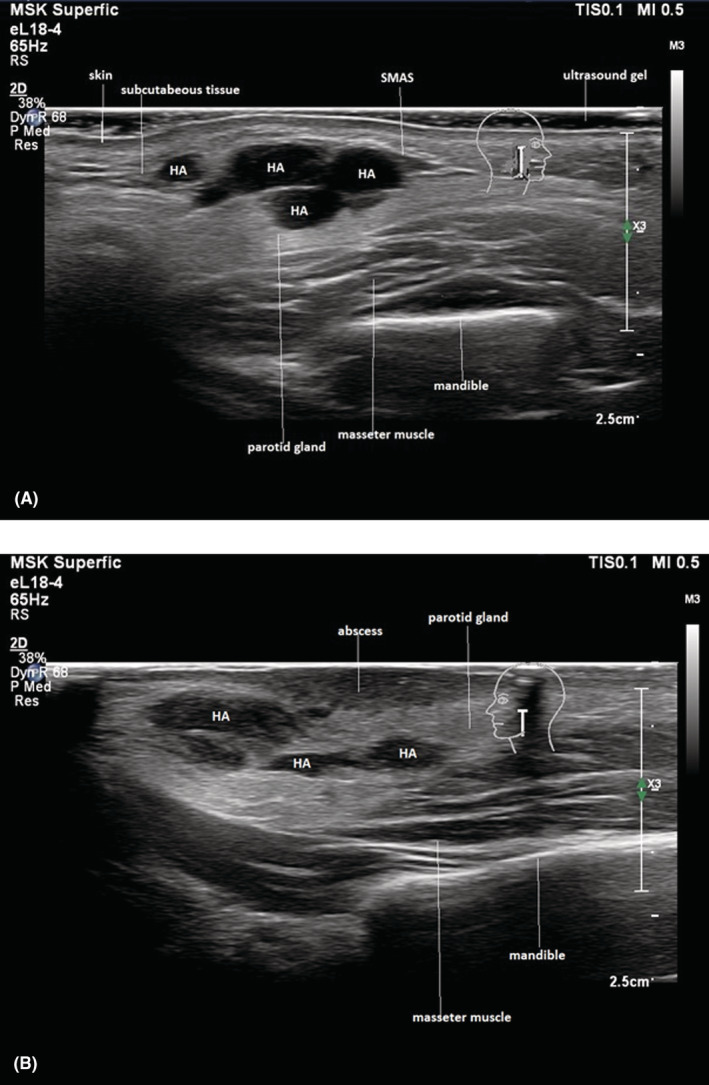
(A) Right side of the patient in case 1: hyaluronic acid deposits (HA) injected into the subcutaneous layer, SMAS, and parotid gland. (B) Left side of the patient in case 1: hyaluronic acid deposits (HA) injected into the parotid gland. Abscess formation visible coming from HA deposit into the skin
2.2. Case 2
A 33‐year‐old male patient presented at our clinic with a hardened asymmetric thickening of the parotid‐masseteric region on both sides of his face.
The patient had a history of a hyaluronic acid filler injections (Restylane®, Galderma) in the zygomatic arch and pre‐auricular area 1 year prior to presentation. The treatment was performed by a board‐certified dermatologist. Soon after the augmentation, edema and tenderness appeared in the parotid‐masseteric region. The patient received multiple treatments with antibiotics and two different physicians tried to remove the product without success before he was referred to us.
On physical examination, the patient showed no swelling of the parotid‐masseteric region. Ultrasound images (Philips Affiniti 70, 18 MHz linear probe) displayed multiple anechoic pockets in the parotid gland on both sides of the face, matching with nodules seen with chronic parotitis (Figure 3). Two pockets of hyaluronic acid fillers were seen in the parotid gland with ultrasound. The patient was treated with hyaluronidase intralesional injections (150 units divided over the two pockets) under ultrasound guidance. At follow‐up 4 weeks later, swelling and tenderness had disappeared.
FIGURE 3.
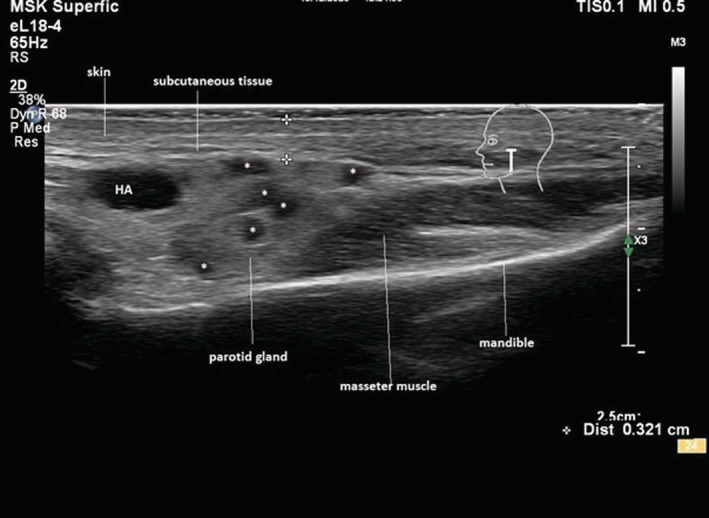
Hyaluronic acid deposits (HA) visible in the parotid gland. Nodules (*) visible seen by chronic parotid inflammation. The total distance from skin to SMAS including the subcutaneous layer is 3.21 mm
2.3. Video
During an ultrasound training session, we introduced under ultrasound guidance a 25G canula subcutaneously in the pre‐auricular area through an 21G needle opening made at the mandibular angle. The cannula was moved cranially without much resistance until at one point it started to course inside the parotid gland (Video S1; see https://vimeo.com/698981131/f8408bfd96).
Remarkably, the injector felt no differences in resistance, and the patient did not experience any pain during this incident.
3. DISCUSSION
Our cases make clear that HA filler material injected in the parotid gland can cause inflammation. It can manifests itself with edema, pain in the whole area, tender nodules, and even abscess formation. In a study of 63 frequent users of common types of cosmetic fillers, Wortsman et al. reported 55 individuals exhibit subclinical sonographic signs of inflammation in the parotid gland. 3 Sonography displayed abnormalities in the echo structures of the parenchyma and hypervascularity of the parotid gland with all kinds of fillers including hyaluronic acid. This study did not detect sonographic deposits of fillers within the parotid gland. Seemingly, filler injections can cause signs of inflammation in the parotid gland that continues even after the filler material has been resorbed. In our case no. 1, both sided were affected, but only one side gave symptoms. Apparently filler injections in the parotid gland may go unnoticed. Our video makes it clear that entering the parotid gland with a canula can happen easily without resistance felt by the physician or pain by the patient.
Anatomical layers in pre‐auricular region from superficial to deep are as follows: skin (epidermis/dermis), subcutaneous fat (superficial fatty tissue), superficial musculoaponeurotic system (SMAS), parotid fascia, parotid gland, parotideo‐masseteric fascia, masseter muscle, and mandibular bone (Figure 4) It is also obvious that in this region the only feasible layer for a filler, being the subcutaneous space, is thin. As a consequence, the space to inject into is limited. Routinely, we measure a width of 2–4 millimeters with sometimes subcutaneous layers being less than one millimeter thick. Ours and Wortsman's findings indicate that filler injections in the pre‐auricular area may deliver material inside the gland. This may go by direct penetration of the gland and be unperceived by both physician and patient. Another potential pathway for filler to enter the gland is via the pre‐auricular ligament. This very dense structure may be difficult for fillers to infiltrate, and these may migrate to the deeper layers and hence the parotid. Wortsman's study makes clear that filler injected into the parotids gland is not a rare finding and apparently causes minor degrees of inflammation that go unnoticed by the patient. Prevention by means of ultrasound imaging prior to treatment in order to establish the width of the subcutis can help to prevent these problems. Also, the placement of a canula after insertion can be checked in this manner.
FIGURE 4.
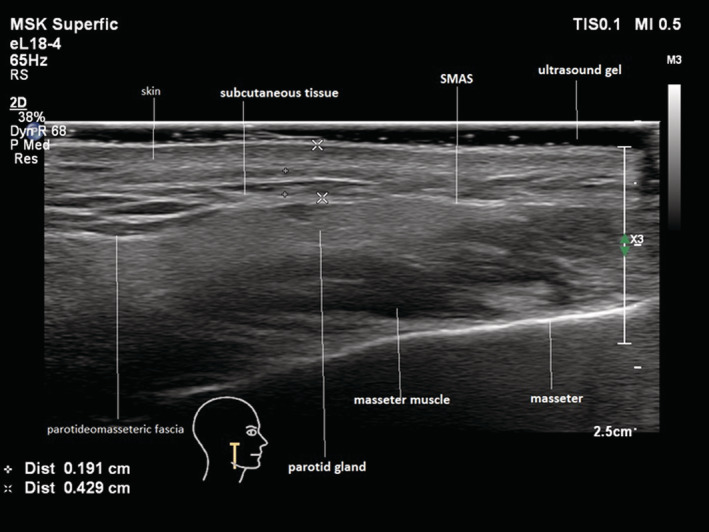
Normal anatomy of the vertical jawline. Note the thickness of the subcutaneous tissue of 1.91 mm (+ between markers +). Terminology is not standardized. The parotideo‐masseteric fascia also named parotid fascia envelops the parotid gland between its superficial and deep layers. The superficial layer is commonly referred to as parotideo‐masseteric fascia instead of the deep layer
CONFLICT OF INTEREST
The authors have no conflicts of interest regarding the present study.
ETHICS STATEMENT
This research has been conducted according to Helsinki declaration. The patients depicted granted permission for the use of data and photographs.
Supporting information
Video S1
ACKNOWLEDGMENTS
The authors gratefully acknowledge the help of Drs. A. Onderdijk and M. Hamer in discussing the patients.
Schelke L, Schoonen T, Velthuis PJ. Filler injections in the pre‐auricular space: Be aware of the parotid gland. J Cosmet Dermatol. 2023;22:173‐176. doi: 10.1111/jocd.15319
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are not openly available due to reasons of privacy.
REFERENCES
- 1. Braz A, Eduardo C. Reshaping the lower face using injectable fillers. Indian J Plast Surg. 2020;53(02):207‐218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Wortsman X, Moll‐Manzur C, Ramírez‐Cornejo C, et al. Ultrasonographic subclinical signs of inflammation of the lacrimal, parotid, and submandibular glands in users of cosmetic fillers. J Ultrasound Med. 2021;40(11):2377‐2389. [DOI] [PubMed] [Google Scholar]
- 3. Vazirnia A, Braz A, Fabi S. Nonsurgical jawline rejuvenation using injectable fillers. J Cosmet Dermatol. 2019;19(8):1940‐1947. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Video S1
Data Availability Statement
The data that support the findings of this study are not openly available due to reasons of privacy.


