Abstract
Background
Shenzhen has made great efforts to address the tobacco epidemic in the past decade. This study aims to evaluate the current status of the tobacco epidemic among adolescent in Shenzhen, China.
Methods
The multi-stage random cluster sampling method was used in the school-based cross-sectional study in 2019 and a total of 7,423 junior and high school (both senior and vocational) students were recruited. Information on cigarette use was collected by the electronic questionnaire. Logistic regression analysis was used to examine the associations between current cigarette use and associated factors. ORs with their 95% CIs were reported.
Results
The prevalence of current cigarette use among adolescents was 2.3%, with boys (3.4%) significantly higher than girls (1.0%). Smoking rates in junior high schools, senior high schools, and vocational senior high schools were 1.0%, 2.7%, and 4.1%, respectively. The results of multivariate logistic regression analysis indicated that gender, age, parental smoking, teachers smoking in schools, friends smoking, exposure to tobacco marketing, and misconceptions about cigarette use were associated factors for adolescent smoking behaviour.
Conclusions
The prevalence of current smoking was relatively low among adolescent in Shenzhen, China. Personal characteristics, family, and school were associated with current adolescent smokers.
Keywords: Adolescents, Smoking, Prevalence, Associated factors
Background
Tobacco use is one of the most serious public health problems in the world [1, 2]. Smoking was the second largest global disease burden in 2019 and is related to chronic obstructive pulmonary disease, cardiovascular disease, and cancer [2–4]. There are 1.14 billion smokers worldwide in 2019, and approximately 306 million adult smokers in China, with the largest smoking population worldwide [5, 6]. Most adult smokers initiate smoking before the age of 18, which increases their susceptibility to nicotine addiction and therefore makes it difficult to quit, leading to severe cumulative health risks and a reduced life expectancy [7–9]. The high smoking rate among adolescents in recent decades has raised public attention [10, 11].A meta-analysis among Chinese adolescents showed that the prevalence of smoking among Chinese adolescents increased rapidly from 1996 to 2010 [12]. The 2019 Global Youth Tobacco Survey (GYTS) in China showed that the adolescent smoking rate was 4.7%, and the prevalence of smoking among adolescents in different cities and regions in China vary greatly [13]. For example, in 2019, the current prevalence of tobacco among adolescents in Shandong Province was 2.1%, compared to 6.9% in Hebei Province [14, 15].
From 2012 to 2013, Shenzhen carried out the construction of smoke-free schools in the city and finally achieved full smoke-free in all schools. Meanwhile, a survey of smoking-related behaviors was conducted for secondary school students, and the prevalence of former smokers and current smokers was 12.65% and 2.83%, respectively [16]. Furthermore, in 2014, the Shenzhen government passed legislation to implement a city-wide ban on smoking in a wide range of places, including public places, workplaces, and public transportation [17]. Notably, Shenzhen revised its tobacco control regulations in 2019, which was described as one of the most stringent tobacco control regulations in China, including regulating e-cigarettes for the first time, banning the sale of tobacco products to minors, and completely prohibiting tobacco advertising, promotion, and sponsorship as core elements of tobacco control.
Evaluating smoking prevalence and examining the associated factors among adolescents is essential to develop more targeted and effective adolescent tobacco control policies and achieve smoke-free Shenzhen. Previous studies have shown that the factors influencing adolescent smoking behavior are complex and multiple such as sex, friends smoking, parental and teachers smoking etc [14, 15]. In 2021, the U.S. National Youth Tobacco Survey (NYTS) showed that adolescent current smoking rate was 1.5%, and found that tobacco accessibility contributed to tobacco use among adolescent [18]. In addition, a tobacco survey from Hong Kong in 2017 for adolescents showed that the prevalence of tobacco among adolescents was 2.5%, and concluded that economic inequality, misconceptions about the dangers of tobacco and positive attitudes towards smoking behaviors play a positive role in adolescent smoking [19].
About 8.7 million deaths worldwide in 2019 were linked to tobacco use, with nearly a third of these occurring in China, and without effective tobacco control measures, tobacco will cause about 3 million deaths per year in China after 2050 [2, 20]. It is of concern that approximately 100 million of the 300 million Chinese smokers currently under the age of 30 will eventually die as a result of tobacco [21]. In addition to health, smoking causes huge socio-economic costs in China such as medical costs, lost productivity and tobacco-related poverty. In 2014, the total economic cost of tobacco use in China was $57 billion, including the cost of treating tobacco-related diseases, the economic loss from reduced productivity and labour force, and the loss of millions of Chinese families to poverty due to tobacco-related diseases and premature deaths [22].
Although some research regarding adult smoking has been conducted in Shenzhen, studies on the prevalence of adolescent smoking and associated factors are still lacking [23–25]. Hence, this study is the first to evaluate the prevalence of smoking among adolescent students in Shenzhen after the implementation of smoke-free legislation and explore the associated factors of adolescent smoking.
Methods
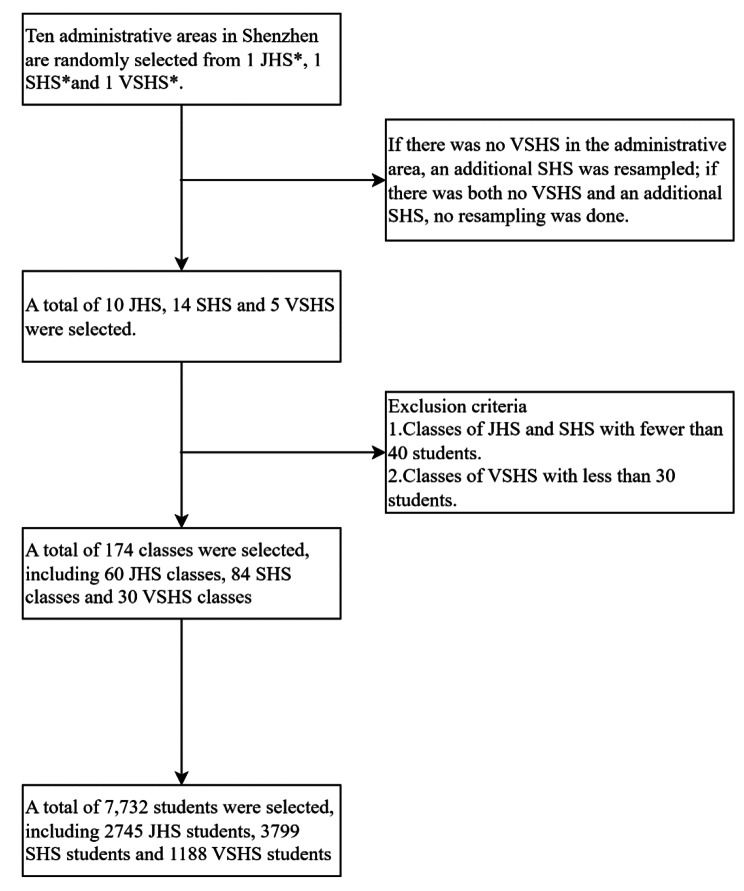
ParticipantsThe present school-based cross-sectional study was conducted in Shenzhen in 2019. Participants are students from junior high school (JHS), senior high school (SHS), and vocational senior high school (VSHS) recruited from 10 administrative districts in Shenzhen by using the multi-stage random cluster sampling method. The ten administrative districts of Shenzhen are Luohu, Futian, Nanshan, Baoan, Longgang, Longhua, Guangming, Dapeng, Yantian and Pingshan. The schools used for the sampling include all public and private schools with junior and high school grades. In the first stage of sampling, Probability Proportionate to Size method Sampling (PPS) was used in each administrative district to select one JHS, one SHS, and one VSHS. If there was no VSHS in the administrative district, we choose another SHS instead. In particular, we have selected only 1 JHS and 1 SHS in the district as there is no VSHS and another SHS in Dapeng District. In the second stage, 2 classes were randomly selected from each grade of each school, for a total sample of 174 classes at all levels of school type (60 JHS classes, 84 SHS classes and 30 VSHS classes), and all students in the selected classes were eligible to participate. Classes of JHS and SHS with fewer than 40 students, and of VSHS fewer than 30 students were excluded from the sampling frame. All stages of sampling were completed by the Tobacco Control Office of the China Center for Disease Control and Prevention. The details were showed in Fig. 1.
Fig. 1.
Sampling process chart
JHS: Junior high school
SHS: Senior high school
VSHS: Vocational senior high school
Data collection
A self-administered questionnaire, developed based on the Chinese version of the GYTS, was used to collect information on primary information (school, grade, class, and individuals), tobacco use, cessation, e-cigarette use, second-hand smoke exposure, tobacco advertisements and promotions, smoking perceptions and attitudes, and anti-tobacco information. The questionnaire was reviewed, checked, approved by experts, and revised after a pilot study. Before the survey, the investigators communicated with the schools in advance and determined the investigation time. Before the survey, we sent written letters to parents to obtain their consent for this study. On the day of the survey, participants were organized to go to multimedia classrooms provided by schools and use computers to complete the questionnaire. In particular, to ensure the accuracy of the study results, all students completed the questionnaire independently with no teachers present. All researchers were strictly trained to protect students’ privacy and ensure the confidentiality of personal data. Additionally, ethics approval (reference number: No. SZCCC-2019-028-01) was obtained from the Ethical Review Committee of the Shenzhen Center for Chronic Disease Control, and all steps and methods in the investigation process were carried out in accordance with the documents approved by the Committee. Informed consent was obtained in writing from the parents or guardians of all participants for this survey.
Measurements
The smoking behaviours of the participants were evaluated in the questionnaire by the following items: (1) Have you ever tried or experimented with cigarette smoking, even one or two puffs? (yes, no); (2) During the past 30 days, on how many days did you smoke cigarettes? (0, 1–2, 3–5, 6–9, 10–19, 20–29, 30 days). Ever smokers were identified if participants answered that they had ever tried more than one puff of cigarettes. Current smokers were identified if participants answered that they had smoked at least 1 day during the past 30 days.
Explanatory variables that are taken into consideration include age(≤ 13, 14 ~ 16, > 16 years), gender (girls, boys), school level (JHS, SHS and VSHS), parental education level (< middle school graduate, middle school graduate, >middle school graduate), family economic status (average, wealth), whether have only one child (yes, no), whether studying in boarding in school (yes, no), a number of parent smokers (no, one parent, both), frequency of noticing teachers’ smoking in schools (never, sometimes, almost every day, indifferent), friends smoking (yes, no), ever exposure to tobacco product marketing in last 30 days(yes, no), have received health education on the dangers of tobacco in class (yes, no, indifferent), considered smoking more attractive (yes, no, indifferent) and perceived comfortable smoking in social occasions (yes, no, indifferent).
Statistical analysis
Descriptive analysis was performed to estimate the prevalence of current and ever-smokers among middle and high school students. To explore the associated factors of adolescent smoking, univariate logistic regression analyses were performed to preliminarily determine the potential factors (in Tables 1 and 2) that are associated with current smoking among adolescents. Baseline variables that were considered to be associated with adolescent smoking or that showed a univariate relationship with the outcome were entered into a multivariate logistic regression model. Given the number of events available, the variables included were carefully selected to ensure parsimony of the final model. Additionally, likelihood ratio test was applied to evaluate probability of models with less predictors compared with the full model (all p < 0.05). The results proved that the full model could fit better in the dataset. The effect values were reported by odd ratios (OR) with a 95% confidence interval (95%CI). All analyzes were performed using R 3.6.1 software.
Table 1.
Univariate analysis of the associations between demographic characteristics and the risk of adolescent current smoking
| Variables | Total(N = 7423) | Smokers (N = 170, %) | OR | 95%CI | P value |
|---|---|---|---|---|---|
| Gender | |||||
| Girls | 3490 | 35(1.0) | 1.000 | ||
| Boys | 3933 | 135(3.4) | 3.509 | 2.442–5.178 | < 0.001 |
| Age | |||||
| ≤ 13 | 1447 | 10(0.7) | 1.000 | ||
| 14–16 | 4070 | 71(1.7) | 2.551 | 1.312–4.960 | 0.006 |
| > 16 | 1906 | 89(4.7) | 7.039 | 3.647–13.582 | < 0.001 |
| School level | |||||
| JHSa | 2663 | 27(1.0) | 1.000 | ||
| SHSb | 3629 | 97(2.7) | 2.681 | 1.772–4.197 | < 0.001 |
| VSHSc | 1131 | 46(4.1) | 4.139 | 2.579–6.772 | < 0.001 |
| Father’s education level | |||||
| <Middle school graduate | 466 | 18(3.9) | 1.000 | ||
| Middle school graduate | 1788 | 43(2.4) | 0.613 | 0.356–1.099 | 0.087 |
| >Middle school graduate | 5169 | 109(2.1) | 0.536 | 0.331–0.920 | 0.016 |
| Mother’s education level | |||||
| <Middle school graduate | 840 | 21(2.5) | 1.000 | ||
| Middle school graduate | 1989 | 40(2.0) | 0.800 | 0.474–1.390 | 0.414 |
| >Middle school graduate | 4594 | 109(2.4) | 0.947 | 0.489–1.347 | 0.824 |
| Family economic status | |||||
| Average | 3452 | 76(2.2) | 1.000 | ||
| Rich | 3971 | 94(2.4) | 1.077 | 0.794–1.465 | 0.634 |
| Only child | |||||
| No | 5291 | 118(2.2) | 1.000 | ||
| Yes | 2132 | 52(2.4) | 1.096 | 0.782–1.516 | 0.586 |
| Boarding in school | |||||
| No | 3726 | 73(2.0) | 1.000 | ||
| Yes | 3697 | 97(2.6) | 1.348 | 0.993–1.838 | 0.057 |
JHSa: Junior high school
SHSb: Senior high school
VSHSc: Vocational senior high school
Table 2.
Univariate analysis of the associations between related factors and the risk of adolescent current smoking
| Variables | Total(N = 7423) | Smokers (N = 170, %) | OR | 95%CI | P value |
|---|---|---|---|---|---|
| Parents smoking | |||||
| No | 3999 | 64(1.6) | 1.000 | ||
| One parent | 3205 | 84(2.6) | 1.655 | 1.193–2.306 | 0.003 |
| Both | 82 | 11(13.4) | 9.526 | 4.591–18.169 | < 0.001 |
| Unknown | 137 | 11(8.0) | 5.368 | 2.725–10.030 | < 0.001 |
| Frequency of teachers smoking in schools | |||||
| Never | 3912 | 36(0.9) | 1.000 | ||
| sometimes | 1792 | 65(3.6) | 4.052 | 2.703–6.170 | < 0.001 |
| Almost every day | 444 | 50(11.3) | 13.663 | 8.822–21.367 | < 0.001 |
| Unknown | 1275 | 19(1.5) | 1.629 | 0.913–2.815 | 0.0874 |
| Friends smoking | |||||
| No | 5005 | 14(0.3) | 1.000 | ||
| Yes | 2418 | 156(6.5) | 24.586 | 14.739–44.572 | < 0.001 |
| Exposure to tobacco product marketing | |||||
| No | 5752 | 69(1.2) | 1.000 | ||
| Yes | 1671 | 101(6.0) | 5.298 | 3.890–7.257 | < 0.001 |
| Have received health education on the dangers of tobacco in class | |||||
| No | 4255 | 76(1.8) | 1.000 | ||
| Yes | 2054 | 66(3.2) | 1.825 | 1.305–2.548 | < 0.001 |
| Unknown | 1114 | 28(2.5) | 1.417 | 0.900-2.171 | 0.119 |
| Considered smoking more attractive | |||||
| Indifferent | 2371 | 79(3.3) | 1.000 | ||
| Yes | 413 | 49(11.9) | 3.906 | 2.675–5.652 | < 0.001 |
| No | 4639 | 42(0.9) | 0.265 | 0.180–0.384 | < 0.001 |
| Perceived comfortable smoking in social occasions | |||||
| Indifferent | 863 | 53(6.1) | 1.000 | ||
| Yes | 286 | 73(25.5) | 5.238 | 3.574–7.724 | < 0.001 |
| No | 6274 | 44(0.7) | 0.108 | 0.072–0.162 | < 0.001 |
Results
Demographic characteristics
Among the 7,732 completed questionnaires, 309 samples with logical errors were excluded from the analysis, and the response rate of the questionnaire was 96.0%. In total, this study included 7423 students recruited from 10 administrative districts in Shenzhen, China. The median age of the sample was 15 years. There were 3,490 (52.98%) girls and 3,933 (47.02%) boys, and 2,263 (35.87%) were JHS students, 3,629 (48.89%) were in SHS students and 1,131(15.24%) were VSHS students.
Associated factors for current smoking among adolescents
In this study, 2.3% of students reported they were current smokers (CS) (Table 1), with the largest number being boys (3.4%) and then girls (1.0%). The prevalence rate of CS varied by age, with 4.7%, 1.7%, and 0.7% in older than 16 years old, 14–16 years, and in the younger than or equal to 13 years age group, respectively. Among them, we observed that the current smoking rate was highest in VSHS students (4.1%), and then SHS (2.7%), and lowest in JHS students (1.0%). Those students who had fathers with a high school education or higher (2.1%) had lower current smoking rate than those with fathers below a high school education (3.9%). Students whose parents smoked were more likely to be CS than those with neither parent smoking, 13.4% versus 1.6%. In addition, 11.3% and 3.6% of high school students with current smoking status indicated that they saw their teachers smoking on campus almost every day or sometimes, while only 0.9% among those who had never seen them. Those students with smoking friends had higher current smoking rates than those without such friends, 6.5% vs. 0.3%. Approximately 6.0% of CS reported that they had been exposed to tobacco product marketing, and 1.2% of them reported they had not. Furthermore, more students were educated about the dangers of tobacco than those who were not, 3.2% vs. 1.8%. Regarding the relationship between smoking and personal attractiveness, 11.9% of CS believe that smoking makes people more attractive, 0.9% hold the opposite view, and 3.3% believe that there is no relationship. Among current smoking students, 25.5% believe that smoking in social settings makes people feel more comfortable, but 0.7% disagree with this idea and 6.1% think that it makes no difference. The details were showed in Table 2.
The factors with statistically significant differences in Tables 1 and 2 were selected and multivariate logistic regression models were used to explore associated factors of currently smoking adolescents. As shown in Table 3, gender, age, parents smoking, frequency of teachers smoking in schools, friends smoking, exposure to tobacco product marketing, considered smoking more attractive, and perceived comfortable smoking at social occasions were significant independent factors of current smoking adolescents. Compared to girls, the OR of boys was 1.557 (95% CI: 1.004–2.415). Older than 16 years old (OR = 2.623, 95%CI = 1.205–5.709), friends smoking (OR = 10.991, 95%CI:6.126–19.717), exposed to tobacco marketing (OR = 4.352, 95%CI:2.996–6.321), consider smoking more attractive (OR = 2.094, 95%CI:1.266–3.464) and almost every day teachers are seen smoking at school (OR = 2.893, 95%CI:1.669–5.013) were also strongly independent factors of smoking currently adolescents. Regarding parents smoking, the OR was 1.634 (95% CI 1.099–2.428) for adolescents with one parent smoking, 5.348 (95% CI 2.092–3.672) for both parents smoking, and 4.078 (1.834–9.066) for those without knowledge of parental smoking status. Additionally, the OR of current smokers for perceived more comfortable smoking in social situations was 4.140 (95%CI:2.583–6.633), and those who felt uncomfortable was 0.201 (95%CI:0.127–0.317).
Table 3.
Multivariate analysis of the associations between related factors and the risk of adolescent current smoking
| Variables | B | SE | OR (95% CI) | P value |
|---|---|---|---|---|
| Gender | ||||
| Girls | 1.000 | |||
| Boys | 0.443 | 0.224 | 1.557(1.004–2.415) | 0.048 |
| Age | ||||
| ≤ 13 | 1.000 | |||
| 14–16 | 0.706 | 0.394 | 2.026(0.936–4.385) | 0.073 |
| > 16 | 0.964 | 0.397 | 2.623(1.205–5.709) | 0.015 |
| Parents smoking | ||||
| No | 1.000 | |||
| One parent | 0.491 | 0.202 | 1.634(1.099–2.428) | 0.015 |
| Both | 1.677 | 0.479 | 5.348(2.092–13.672) | < 0.001 |
| Unknown | 1.406 | 0.408 | 4.078(1.834–9.066) | 0.001 |
| Frequency of teachers smoking in schools | ||||
| Never | 1.000 | |||
| sometimes | 0.399 | 0.240 | 1.490(0.932–2.385) | 0.096 |
| Almost every day | 1.062 | 0.281 | 2.893(1.669–5.013) | < 0.001 |
| Unknown | -0.004 | 0.317 | 0.996(0.535–1.853) | 0.990 |
| Friends smoking | ||||
| No | 1.000 | |||
| Yes | 2.397 | 0.298 | 10.991(6.126–19.717) | < 0.001 |
| Exposed to tobacco marketing | ||||
| No | 1.000 | |||
| Yes | 1.466 | 0.190 | 4.352(2.996–6.321) | < 0.001 |
| Considered smoking more attractive | ||||
| No difference | 1.000 | |||
| Yes | 0.739 | 0.257 | 2.094(1.266–3.464) | 0.004 |
| No | -0.298 | 0.226 | 0.742(0.476–1.156) | 0.187 |
| Perceived comfortable smoking in social occasions | ||||
| No difference | 1.000 | |||
| Yes | 1.421 | 0.241 | 4.140(2.583–6.633) | < 0.001 |
| No | -1.605 | 0.233 | 0.201(0.127–0.317) | < 0.001 |
Discussion
This is the first article published on the status of youth smoking since the implementation of smoke-free legislation in Shenzhen. In the past, Shenzhen’s tobacco control efforts were primarily aimed at addressing the adult tobacco epidemic, on the basis of which numerous studies have been conducted [17, 23]. Developing sustained and well-established monitoring strategies can contribute to creating effective policies and measures for adolescents that can significantly reduce adolescent smoking rates.
According to our study, the overall current smoking rate among adolescents was 2.3% in Shenzhen, with boys (3.4%) significantly higher than girls (1.0%). There was a positive correlation between adolescent current smoking and their age, with the lowest rates in groups younger than or equal to age 13 (0.7%) and the highest rates in groups older than age 16 (4.7%). The current smoking rate also varies greatly by school type, with the highest in VSHS at 4.1%, the lowest in JSH at 1.0%, and SHS at 2.7%. The overall current smoking rate was virtually unchanged from the 2012 Shenzhen Youth Tobacco Survey, 2.8% compared to 2.3% [16]. Compared with the 2019 GYTS China survey, the overall prevalence of the current smoking rate of adolescents in 2019 was significantly decreased, (2.3% vs. 5.9%), with similar patterns in boys currently smoking rates (3.4% vs. 9.6%), but little change in current smoking rates among girls (1.0% vs. 1.9%) [13]. This indicates the need to develop gender-specific tobacco control strategies to prevent female adolescents from smoke initiation, and to assist cessation of smoking female adolescents in the future. And then, our results showed that current smoking rates were both lower in JHS, SHS, and VSHS than in the China GYTS 2019 survey, 1.0% vs. 3.9%, 2.7% vs. 5.6% and 4.1% vs. 14.7%, respectively [13]. Moreover, the current smoking rate is lower than in other studies conducted in countries and cities in China. For example, the 2021 National Youth Tobacco Survey (NYTS) showed that 1.5% of boys and 1.5% of girls smoked in the last 30 days, and a cross-sectional survey conducted by Lin zhu et al. suggested that the current smoking rate among adolescents was 4.26% in Fujian Province in 2019 [18, 26]. This may be related to the implementation of Shenzhen’s 2019 comprehensive smoking control regulations, which is considered to be one of the strictest related laws in China.
In this study, we determined the associated factors of current adolescent smoking. Adolescents who were boys or older than aged 16 years were more likely to present smoking status, which is consistent with the findings of Meng Wang et al. for middle and high school students in Zhejiang Province in 2012 [27]. Additionally, misconceptions about smoking were positively associated with the risk of smoking among adolescents [28, 29]. Adolescents who perceived smoking as more attractive (OR = 2.094, 95%CI:1.266–3.464) and comfortable in social environments (OR = 4.140, 95%CI:2.583–6.633) were at higher risk of using cigarettes and easier to accept e-cigarettes or other tobacco products [30, 31]. In particular, parents, teachers, and peers contribute strongly to adolescent smoking [32]. Parental smoking behaviour and tolerant attitudes towards tobacco use are critical to initiating and maintaining smoking among adolescents [33, 34]. Either one (OR = 1.634, 95%CI:1.099–2.428) or both parents smoked (OR = 5.348, 95%CI:2.092–13.672) made adolescents more likely to continue smoking. We did not further analyze the respective roles of fathers and mothers on adolescent smoking, but previous studies indicated that adolescents were more likely to smoke when their mothers smoked [35] and that maternal smoking had a greater effect on girls than boys [35, 36]. In addition, parental divorce or separation, and living with other family members who smoked but not parents were all more likely to lead to adolescent smoking [27, 35]. Notably, a survey of 33,408 adolescents showed that current smoking was strongly negatively associated with maternal care and control, but positively associated with paternal control [37]. In this context, the traditional Chinese parenting style (strict father and loving mother) may lead to rebellious behavior in adolescents, such as smoking. Therefore, a comprehensive review of the combined effects of family on adolescent smoking behavior is necessary in the future.
Similar to previous studies [38, 39], adolescents surrounded by smoking friends were more likely to smoke at present [38, 39]. Our study also showed that the association between current student smoking and teacher smoking depended on the extent to which teachers’ smoking behaviour was seen. There was no relationship between students smoking and occasionally seeing teachers smoking on campus; this risk was only significant when students noticed teachers smoking almost daily or daily. Teachers can play an essential role in shaping the behaviour of young people, as they spend most of their time at school, so Shenzhen implemented a city-wide smoke-free school strategy in 2013, which prohibited teachers from smoking in schools [40]. However, smoking teachers undermines or diminishes the authority of smoke-free regulations. Students observing teachers’ smoking behaviour may believe no restrictions exist or that existing regulations are more lenient, eventually inducing and sustaining smoking. A longitudinal study from the USA showed that tobacco advertising and promotion converts non-smoking adolescents into regular smokers and the more intense the tobacco marketing, the more likely adolescents are to smoke [41, 42]. Despite a complete ban on the promotion and sponsorship of tobacco advertising and the sale of tobacco products through vending devices in Shenzhen in 2019, we still found this link in our research. Therefore, there is a need to strengthen the enforcement of this regulation in the future to ensure that young people are protected from tobacco industry marketing.
The most notable strength of this study is its focus on the specific group of adolescents, including the description of tobacco use among adolescents and associated factors, which will help the government and health authorities to tailor anti-tobacco policies and measures for adolescents. However, this study also has some limitations. First, the cross-sectional study cannot provide causality, and further longitudinal research is needed. Second, the current smoking status among adolescents was a self-reported result without biological validation. Meanwhile, adolescent smoking is often perceived as a “bad boy” due to socio-cultural norms, so that the adolescent tended to report not smoking, which may result in underestimating the prevalence of smoking.
This study provides valuable insights into adolescent smoking behaviour and associated factors. Perennial and comprehensive surveillance strategies are important for understanding the smoking status and smoking-related factors among adolescent, which is the key to addressing youth smoking. future tobacco control policies should be more specific and customized, taking into consideration gender and smoking-related factors to provide effective cessation services. Additionally, this study demonstrates that the existing tobacco control strategies and measures in Shenzhen are insufficiently effective in discouraging female students from smoking. Future qualitative interviews with female adolescents may be needed to understand the particularities of this group in the area of tobacco control to implement effective and tailored measures. Targeting parents who smoke and developing school-based cessation or prevention programs in the context of smoke-free schools to decrease the number of adolescent smokers in schools, thus significantly reducing the number of smokers based on peer interaction, could be one of the effective ways to address the adolescent tobacco epidemic in the future.
Conclusions
Smoking prevalence was relatively low among Chinese adolescents in Shenzhen. Personal characteristics contributed to the influence of smoking behaviour among adolescents. In addition, environmental factors related to tobacco exposure, including family, school, and tobacco marketing, were also associated with adolescent smoking behaviour. Developing a family-school-community trinity model for tobacco control, and conducting school-based anti-tobacco information and cessation interventions to reduce adolescent smoking rates, especially those with the above associated factors.
Acknowledgements
This study was supported by research grants from the Sanming Project of Medicine in Shenzhen, SZSM201811093; Shenzhen Science and Technology program (KCXFZ20201221173400002) and the Shenzhen Medical Key Discipline Construction Fund. We also would like to thank the Chronic Disease Control Institutes in all districts of Shenzhen and those who participated in the survey and collected data.
Abbreviations
- GYTS
Global Youth Tobacco Survey
- JHS
Junior high school
- SHS
Senior high school
- VSHS
Vocational senior high school
- PPS
Proportionate to Size Sampling
- CS
Current smokers
- OR
Odds ratios
- CI
Confidence intervals
- NYTS
National Youth Tobacco Survey
Author contribution
LBL and LX performed statistical analysis, interpretation of the data and draft the manuscript. LWL, WXB, LYY, ZZY, FRY and ZLG contributed to data collection and provided training. XJF provided suggestions as well as participated in drafting the manuscript. All authors read and approved the final manuscript.
Funding
This study was supported in part by grants from “Shenzhen Science and Technology program (KCXFZ20201221173400002)” and “Sanming Project of Medicine in Shenzhen (No. SZSM201811093)” and “Shenzhen Medical Key Discipline Construction Fund”.
Data Availability
All data relevant to the study are included in the article or uploaded as online supplemental information.
Declarations
Ethics approval and consent to participate
This study was approved by the Institution Ethic Review Committee of the Shenzhen Center for Chronic Disease Control (reference number: No. SZCCC-2019-028-01), and informed consent was obtained in writing from the parents or guardians of all participants for this survey. All research methods were carried out in accordance with relevant guidelines and regulations.
Consent for publication
Not applicable.
Competing interests
All authors declare no competing interests.
Footnotes
This article has been updated to correct an affiliation and the acknowledgement.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Organization WH. WHO global report on trends in prevalence of tobacco smoking 2000–2025. World Health Organization; 2018.
- 2.Murray CJL, Aravkin AY, Zheng P, Abbafati C, Abbas KM, Abbasi-Kangevari M, Abd-Allah F, Abdelalim A, Abdollahi M, Abdollahpour I, et al. Global burden of 87 risk factors in 204 countries and territories, 1990–2019: a systematic analysis for the global burden of Disease Study 2019. The Lancet. 2020;396(10258):1223–49. doi: 10.1016/S0140-6736(20)30752-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Postma DS, Bush A, van den Berge M. Risk factors and early origins of chronic obstructive pulmonary disease. The Lancet. 2015;385(9971):899–909. doi: 10.1016/S0140-6736(14)60446-3. [DOI] [PubMed] [Google Scholar]
- 4.Koene RJ, Prizment AE, Blaes A, Konety SH. Shared Risk factors in Cardiovascular Disease and Cancer. Circulation. 2016;133(11):1104–14. doi: 10.1161/CIRCULATIONAHA.115.020406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Reitsma MB, Kendrick PJ, Ababneh E, Abbafati C, Abbasi-Kangevari M, Abdoli A, Abedi A, Abhilash E, Abila DB, Aboyans V. Spatial, temporal, and demographic patterns in prevalence of smoking tobacco use and attributable disease burden in 204 countries and territories, 1990–2019: a systematic analysis from the global burden of Disease Study 2019. The Lancet. 2021;397(10292):2337–60. doi: 10.1016/S0140-6736(21)01169-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chinese Center for Disease Control and Prevention . The results of Chinese adult Tobacco Survey in 2018 [R] Beijing: Chinese Center for Disease Control and Prevention; 2020. [Google Scholar]
- 7.Human ServicesAtlanta, editor. Preventing tobacco use among youth and young adults: a report of the Surgeon General. GA: US Department of Health and Human Services, Centers for Disease Control and Prevention, Office on Smoking and Health; 2012. [PubMed] [Google Scholar]
- 8.Breslau N, Peterson EL. Smoking cessation in young adults: age at initiation of cigarette smoking and other suspected influences. Am J Public Health. 1996;86(2):214–20. doi: 10.2105/AJPH.86.2.214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.US Department of Health and Human Services. The health consequences of smoking: a report of the Surgeon General. In.: US Department of Health and Human Services, Centers for Disease Control and Prevention, Office on Smoking and Health; 2004.
- 10.Reitsma MB, Fullman N, Ng M, Salama JS, Abajobir A, Abate KH, Abbafati C, Abera SF, Abraham B, Abyu GY, et al. Smoking prevalence and attributable disease burden in 195 countries and territories, 1990–2015: a systematic analysis from the global burden of Disease Study 2015. The Lancet. 2017;389(10082):1885–906. doi: 10.1016/S0140-6736(17)30819-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Organization WH. Youth and tobacco in the Western Pacific Region: global youth tobacco survey 2005–2014. 2016.
- 12.Han J, Chen X. A Meta-analysis of cigarette smoking prevalence among adolescents in China: 1981–2010. Int J Environ Res Public Health. 2015;12(5):4617–30. doi: 10.3390/ijerph120504617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Liu S, Xiao L, Zeng X, Di X, Li X. Tobacco use and exposure among secondary school students—China, 2019. China CDC Weekly. 2020;2(22):385–93. doi: 10.46234/ccdcw2020.100. [DOI] [Google Scholar]
- 14.Zhou PJ, Hu Y, Liu T, Wei X, Hou JX. Analysis on tobacco use and its associated factors among adolescents in Shandong Province in 2019 [J] Chin J Health Educ. 2021;37(11):970–4. [Google Scholar]
- 15.He L, Guo XL, Zhang HR, Yu F, Wen BQ, Li XT, Cheng AJ. Status of current Tobacco use and its influencing factors among adolescents in Hebei Province in 2019 [J] J Prev Med Inform. 2021;37(08):1082–9. [Google Scholar]
- 16.Xiong JF, Yang H, Luo NC, Zhu PL, Ruan JM. Smoking behavior and its relative factors among adolescents in Shenzhen. Chin J Health Educ. 2015;000(009):833–6. [Google Scholar]
- 17.Xiong JF, Xie W, Liu XL, Yang YZ. Characteristics of Shenzhen tobacco control regulation and the process of law enforcement.J Tuberc Lung Health2014(4):4.
- 18.Wang TW, Gentzke AS, Creamer MR, Cullen KA, Holder-Hayes E, Sawdey MD, Anic GM, Portnoy DB, Hu S, Homa DM: Tobacco product use and associated factors among middle and high school students—United States, 2019. 2019, 68(12):1. Gentzke AS, Wang TW, Cornelius M,. Tobacco Product Use and Associated Factors Among Middle and High School Students - National Youth Tobacco Survey, United States, 2021. MMWR Surveill Summ. 2022;71(5):1–29.
- 19.Ho SY, Chen J, Leung LT, Mok HY, Wang L, Wang MP, Lam TH. Adolescent smoking in Hong Kong: Prevalence, Psychosocial correlates, and Prevention. J Adolesc Health. 2019;64(6S):19–S27. doi: 10.1016/j.jadohealth.2019.01.003. [DOI] [PubMed] [Google Scholar]
- 20.Chen Z, Peto R, Zhou M, Iona A, Smith M, Yang L, Guo Y, Chen Y, Bian Z, Lancaster G, et al. Contrasting male and female trends in tobacco-attributed mortality in China: evidence from successive nationwide prospective cohort studies. Lancet. 2015;386(10002):1447–56. doi: 10.1016/S0140-6736(15)00340-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Liu BQ, Peto R, Chen ZM, et al. Emerging tobacco hazards in China: 1. Retrospective proportional mortality study of one million deaths. BMJ. 1998;317(7170):1411–22. doi: 10.1136/bmj.317.7170.1411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Manila P. World Health Organization Western Pacific Regional Office. The unbearable cost to China: The health, economic and social costs of the tobacco epidemic in China.
- 23.Xie W, Xiong JF, Yu WY, Feng TJ. Analysis of smoking status and influencing factors of Shenzhen residents aged 15–70 years. Chin J Prev Control Chronic Dis. 2017;25(8):3. [Google Scholar]
- 24.Han TG, Chen KY, Zhuang RS, Zhang Y, Cao L, Wu ZH. Survey of the Tobacco Epidemic in Shenzhen City in 2012.Health Education and Health Promotion2016(3):3.
- 25.Liu YH, Deng YZ, Huang Y, Huang L, Yan RL, Zhang L. Status of tobacco epidemic and factors influencing smoking and willingnessof smoking cessation among residents in Bao’an District of Shenzhen City. Practical Prev Med. 2021;28(09):1040–4. [Google Scholar]
- 26.Lin Z, Chen ML, Chen JH. Investigation and analysis on smoking behaviors of teenagers in Fujian Province in 2019. Chin J Health Educatio. 2021;37(11):975–8. [Google Scholar]
- 27.Wang M, Zhong JM, Fang L, Wang H. Prevalence and associated factors of smoking in middle and high school students: a school-based cross-sectional study in Zhejiang Province, China. BMJ Open. 2016;6(1):e010379. doi: 10.1136/bmjopen-2015-010379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Pierce JP, Choi WS, Gilpin EA, Farkas AJ, Berry CC. Tobacco industry promotion of cigarettes and adolescent smoking. JAMA. 1998;279(7):511–5. doi: 10.1001/jama.279.7.511. [DOI] [PubMed] [Google Scholar]
- 29.Biener L, Siegel M. Tobacco marketing and adolescent smoking: more support for a causal inference. Am J Public Health. 2000;90(3):407. doi: 10.2105/AJPH.90.3.407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Fadus MC, Smith TT, Squeglia LM. The rise of e-cigarettes, pod mod devices, and JUUL among youth: factors influencing use, health implications, and downstream effects. Drug Alcohol Depend. 2019;201:85–93. doi: 10.1016/j.drugalcdep.2019.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Zhao Z, Zhang M, Wu J, Xu X, Yin P, Huang Z, Zhang X, Zhou Y, Zhang X, Li C. E-cigarette use among adults in China: findings from repeated cross-sectional surveys in 2015–16 and 2018–19. The Lancet Public Health. 2020;5(12):e639–49. doi: 10.1016/S2468-2667(20)30145-6. [DOI] [PubMed] [Google Scholar]
- 32.Huang C, Koplan J, Yu S, Li C, Guo C, Liu J, Li H, Kegler M, Redmon P, Eriksen M. Smoking experimentation among elementary school students in China: influences from peers, families, and the school environment. PLoS ONE. 2013;8(8):e73048. doi: 10.1371/journal.pone.0073048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Avenevoli S, Merikangas KR. Familial influences on adolescent smoking. Addiction. 2003;98:1–20. doi: 10.1046/j.1360-0443.98.s1.2.x. [DOI] [PubMed] [Google Scholar]
- 34.Harakeh Z, Scholte RH, De Vries H, Engels RC. Parental rules and communication: their association with adolescent smoking. Addiction. 2005;100(6):862–70. doi: 10.1111/j.1360-0443.2005.01067.x. [DOI] [PubMed] [Google Scholar]
- 35.Leonardi-Bee J, Jere ML, Britton J. Exposure to parental and sibling smoking and the risk of smoking uptake in childhood and adolescence: a systematic review and meta-analysis. Thorax. 2011;66(10):847–55. doi: 10.1136/thx.2010.153379. [DOI] [PubMed] [Google Scholar]
- 36.Sullivan KM, Bottorff J, Reid C. Does mother’s smoking influence girls’ smoking more than boys’ smoking? A 20-year review of the literature using a sex- and gender-based analysis. Subst Use Misuse. 2011;46(5):656–68. doi: 10.3109/10826084.2010.528122. [DOI] [PubMed] [Google Scholar]
- 37.Wang Y, Ho SY, Wang MP, Lo WS, Lai HK, Lam TH. Hong Kong Chinese adolescents’ self-reported smoking and perceptions of parenting styles. Int J Behav Med. 2015;22(2):268–75. doi: 10.1007/s12529-014-9436-0. [DOI] [PubMed] [Google Scholar]
- 38.Kobus K. Peers and adolescent smoking. Addiction. 2003;98:37–55. doi: 10.1046/j.1360-0443.98.s1.4.x. [DOI] [PubMed] [Google Scholar]
- 39.Hall JA, Valente TW. Adolescent smoking networks: the effects of influence and selection on future smoking. Addict Behav. 2007;32(12):3054–9. doi: 10.1016/j.addbeh.2007.04.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Morrison A. En MCINTYRE D.,‘Schools and socialization’. Manchester: In.: Penguin books inc; 1971. [Google Scholar]
- 41.Cummings KM, Shah D, Centers for Disease Control and Prevention (CDC) Trends in smoking initiation among adolescents and young adults–United States, 1980–1989. MMWR Morb Mortal Wkly Rep. 1995;44(28):521–5. [PubMed] [Google Scholar]
- 42.Gilpin EA, Pierce JP. Trends in adolescent smoking initiation in the United States: is tobacco marketing an influence? Tob Control. 1997;6(2):122–7. doi: 10.1136/tc.6.2.122. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data relevant to the study are included in the article or uploaded as online supplemental information.