Abstract
Nurse practitioner (NP) and physician assistant (PA) prescribing can increase access to buprenorphine treatment for opioid use disorder. In this cross-sectional study, we used deidentified claims from approximately 90% of U.S. retail pharmacies (2017–2018) to examine the association of state policies with the odds of receiving buprenorphine treatment from an NP/PA versus a physician, overall and stratified by urban/rural status. From 2017 to 2018, the percentage of buprenorphine treatment episodes prescribed by NPs/PAs varied widely across states, from 0.4% in Alabama to 57.2% in Montana. Policies associated with greater odds of buprenorphine treatment from an NP/PA included full scope of practice (SOP) for NPs, full SOP for PAs, Medicaid pay parity for NPs (reimbursement at 100% of the fee-for-service physician rate), and Medicaid expansion. Although most findings with respect to policies were similar in urban and rural settings, the association of Medicaid expansion with NP/PA buprenorphine treatment was driven by rural counties.
Keywords: nurse practitioners, physician assistants, buprenorphine, opioid use disorder, behavioral health care, Medicaid
Introduction
The United States continues to face an opioid overdose crisis, with many individuals unable to access effective treatment (Jones et al., 2015; Patrick et al., 2020). Buprenorphine, a partial opioid agonist, is an effective and widely used treatment for opioid use disorder (OUD) that can be delivered in office-based settings (Connery, 2015). However, buprenorphine treatment utilization among people with OUD is limited, in part due to the lack of buprenorphine prescribers (Dick et al., 2015; McBain et al., 2020). In July 2020, 18% of urban counties and 43% of rural counties lacked a physician waivered to prescribe buprenorphine (Andrilla & Patterson, 2021).
Nurse practitioners (NPs) and physician assistants (PAs) are an important resource for health care in rural and underserved communities (Barnes et al., 2018; Buerhaus et al., 2015; Cawley et al., 2016; Davis et al., 2018; Xue et al., 2019), and since becoming eligible to apply for waivers to prescribe buprenorphine with the 2016 passage of the Comprehensive Addiction and Recovery Act (CARA, 2016), NPs and PAs have played an increasingly important role in the effective treatment of OUD in those communities. Between 2016 and 2019, over 12,000 NPs and PAs obtained buprenorphine waivers (Barnett et al., 2019), driving a 111% increase in waivered prescribers per 100,000 population in rural areas, where NPs and PAs accounted for over half of newly waivered prescribers (Barnett et al., 2019).
Although CARA has expanded the workforce available to prescribe buprenorphine, many waivered clinicians do not actively prescribe (Thomas et al., 2017), and state policies may influence the prescribing of buprenorphine by NPs and PAs. Scope of practice (SOP) laws in many states limit NPs’ abilities to practice and prescribe medications without physician oversight or collaboration (American Association of Nurse Practitioners, 2021) or prevent PAs from performing one or more elements of practice (American Association of Physician Assistants, 2020). Less restrictive SOP laws have been associated with more waivered NPs but not PAs (Auty et al., 2020; Barnett et al., 2019; Spetz et al., 2019, 2021) and higher rates of buprenorphine prescribing by NPs (Nguyen et al., 2021). State Medicaid policies also play an important role in states’ response to the opioid crisis, as Medicaid is the largest payer for treatment of substance use disorders (Medicaid and CHIP Payment and Access Commission [MACPAC], 2017b; Orgera & Tolbert, 2019). Medicaid expansion under the Affordable Care Act has increased access to buprenorphine treatment (Clemans-Cope et al., 2017; Saloner et al., 2018; Wen et al., 2017) and may be particularly important for increasing access to treatment from NPs and PAs, who provide buprenorphine treatment to a higher proportion of Medicaid enrollees than do physicians (IMPAQ International, 2019). Medicaid reimbursement policies may also influence NP/PA buprenorphine prescribing. In many states, Medicaid reimbursement for NPs and PAs is up to 25% less than that received by physicians (Harkless & Vece, 2018). In states with Medicaid pay parity (i.e., where NPs and PAs are reimbursed at equal rates as physicians), practices may have greater incentive to employ NPs and PAs and accept Medicaid patients (Barnes et al., 2017). Policies that increase access to buprenorphine treatment for Medicaid enrollees may also have spillover effects for non-Medicaid populations (Abraham et al., 2021).
New Contributions
Although previous studies have examined the association of state SOP laws with the number of waivered NPs/PAs and rates of buprenorphine prescribing by NPs, studies have not yet examined to what extent Medicaid expansion and Medicaid reimbursement parity are associated with buprenorphine prescribing among NPs and PAs (Schuler et al., 2020). In addition, few studies have evaluated the relationship between state policies and the contribution of NPs and PAs to buprenorphine prescribing, relative to physicians. To address this gap in the literature, we used 2017 to 2018 deidentified pharmacy claims to describe patterns of buprenorphine prescribing by NPs and PAs and examine the association of state policies with the odds of receiving buprenorphine treatment from an NP/PA versus a physician. We hypothesized that full SOP for NPs and PAs, Medicaid pay parity for NPs, and Medicaid expansion would be associated with greater odds of receiving buprenorphine treatment from an NP/PA.
Because the implications of state policies may differ in urban and rural settings, we conducted stratified analyses by county urban/rural status. Contextual differences between urban and rural areas may influence the relationship between state policies and provision of buprenorphine treatment by NPs/PAs versus physicians. Rural areas face many challenges in addressing the opioid crisis, including challenges with health care coverage and access, social stigma against medication-based treatment for OUD, workforce shortages, and lack of mental health and psychosocial support services (Andrilla et al., 2019; National Judicial Opioid Task Force, 2019; Rosenblatt et al., 2015).
Conceptual Framework
The conceptual framework underlying this study is informed by the Andersen Behavioral Model of Health Service Use (Figure 1). Our conceptual framework illustrates that both individual and environmental factors (community characteristics and federal and state policies) influence treatment for OUD, including type of treatment received (office-based buprenorphine treatment, buprenorphine treatment in opioid treatment facilities, non-buprenorphine treatment, no treatment) and provider type (physician or NP/PA). Predisposing factors (individual factors such as age, gender, race/ethnicity), enabling factors (individual factors such as insurance; community factors such as urbanicity, median income, uninsured rate, health professional shortage area [HPSA] status, active non-NP/PA buprenorphine prescribers), and need factors (community fatal overdose count and county population) may influence treatment for OUD. In this study, we focus on state policies most likely to influence NP/PA provision of buprenorphine treatment either directly (e.g., restrictive SOP laws may limit the ability of NPs/PAs to provide buprenorphine treatment) or indirectly by increasing provider capacity (e.g., Medicaid expansion increases demand for buprenorphine treatment resulting in more clinicians choosing to prescribe buprenorphine; Medicaid pay parity may lead to an increase in practicing NPs/PAs, including those waivered to prescribe buprenorphine).
Figure 1.
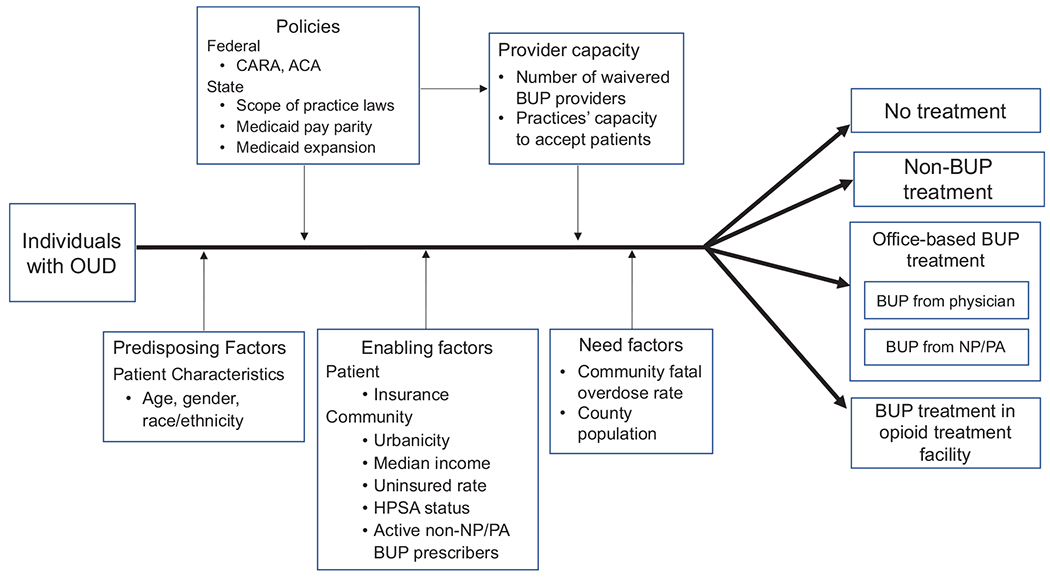
Conceptual Framework.
Method
Data
We used de-identified retail pharmacy claims for 2017 to 2018 from the IQVIA Real World Data-Longitudinal Prescriptions (IQVIA, n.d.). These data capture approximately 90% of all prescriptions filled at retail pharmacies in all 50 states and the District of Columbia and include information about the prescription, payer, patient demographics, and prescribing clinician specialty and location. The study was approved with a waiver of consent by the authors’ institutional review board.
Variables
Buprenorphine Treatment Episodes.
We identified new buprenorphine treatment episodes that started with the date of the first observed fill of a prescription for a buprenorphine formulation with an FDA (Food and Drug Administration)-approved indication for OUD treatment following a 90-day period with no supply from any previously filled buprenorphine prescription (Stein et al., 2021). The episode ended with the last day’s supply of buprenorphine for the last filled buprenorphine prescription, with no more than a 30-day gap in the patient’s buprenorphine supply. We excluded episodes in which the first observed prescription occurred between January and March 2017 to ensure we did not include episodes continuing from 2016. We also excluded episodes from Tennessee, which did not allow PA and NP prescribing of buprenorphine during this period (Moore, 2019), and episodes for which county information was unavailable. We categorized prescribers by provider type: NP, PA, or physician, and attributed buprenorphine treatment episodes to the prescriber who wrote the most days of supply of buprenorphine during the episode.
Patient and Episode Characteristics.
Patients were categorized by age group (18–25 years, 26–35, 36–45, 46–55, 56–65, 65+), sex, and the payment source responsible for the most days of supply during the buprenorphine episode (Medicaid, Medicare, commercial insurance, cash payment, discount cards/voucher/coupon/rebate, or other including Tricare or workers compensation).
Community Characteristics.
We identified the county in which the treatment episode occurred based on the prescriber’s 5-digit Federal Information Processing Standards code. We identified urban/rural status based on Rural Urban Continuum Codes (RUCC) from the Area Health Resources Files (AHRF): urban (RUCC 1, 2, or 3) or rural (RUCC 4, 5, 6, 7, 8, or 9; National Center for Health Statistics, 2014). We also used the AHRF to identify primary care and mental health care HPSAs and county population (U.S. Department of Health and Human Services Health Resources and Services Administration, n.d.). We obtained county-level estimates of median household income and percent of uninsured adults from the American Community Survey (U.S. Census Bureau, 2011). We used the multiple-cause-of-death mortality file from the Centers for Disease Control and Prevention to calculate Ruhm adjusted 2016 county fatal overdose counts for deaths due to any drug (Centers for Disease Control and Prevention, 2020; Ruhm, 2018). We used the buprenorphine prescriber data from IQVIA to estimate the number of active non-NP/PA buprenorphine prescribers by county.
State Policies.
Consistent with previous studies (Barnes et al., 2017; Barnett et al., 2019), we characterized states as having full SOP for PAs if they had all six “essential elements” of practice, as defined by the American Association of Physician Assistants (2020) and restricted SOP otherwise, and state SOP for NPs as full SOP versus restricted or reduced SOP, as defined by the American Association of Nurse Practitioners (2021; Phillips, 2016). These policies were identified as of 2016 to coincide with the passage of CARA (Online Appendix Table A-1). We used information from the Kaiser Family Foundation to identify states that expanded Medicaid coverage under the Affordable Care Act (Kaiser Family Foundation, n.d.). Although Medicaid reimbursement policies for NPs and PAs overlap in many states, we defined pay parity based on NP reimbursement rates because PAs do not bill directly in all states (American Association of Physician Assistants, 2021; MACPAC, 2017a). We identified states with Medicaid pay parity for NPs (i.e., reimbursement of NPs at 100% of the fee-for-service physician rate) using data from the 2016 Advanced Practice Registered Nurse legislative update and 2016 Medicaid fee-for-service physician payment policies reported by the MACPAC (2017a; Phillips, 2016).
Statistical Analysis
We first calculated the number and unadjusted percentages of buprenorphine treatment episodes overall and by patient and community characteristics. We then calculated the number and percentage of buprenorphine treatment episodes prescribed by an NP/PA overall and by patient, community, and state policy characteristics.
We used adjusted logistic regression models to evaluate the association of state policies with the odds of receiving buprenorphine treatment from an NP/PA versus a physician. We examined these associations overall and stratified by county urban/rural status. Models were adjusted for episode year, buprenorphine episode payer, patient sex and age group, primary care and mental health care HPSA status, median family income quartile, percent uninsured quartile, county population quartile, county fatal overdose count quartile, and number of active non-NP/PA buprenorphine prescribers. We report adjusted odds ratios with 95% confidence intervals (CIs), clustered by state and person ID to account for individuals with multiple episodes.
Results
NPs and PAs were the primary prescribers for 8.9% of the slightly fewer than 1 million new buprenorphine episodes identified during 2017 to 2018 (Table 1). The most frequent payer of buprenorphine treatment episodes was Medicaid (40.5%), followed by commercial insurance (20.0%). The majority of episodes occurred in urban counties (87.1%), primary care HPSAs (93.0%), and mental health care HPSAs (93.3%). The percentage of buprenorphine treatment episodes prescribed by NPs/PAs from 2017 to 2018 varied widely across states, ranging from 0.4% in Alabama to 57.2% in Montana (Online Appendix A-2).
Table 1.
Characteristics of Buprenorphine Treatment Episodes, 2017 to 2018.
| Characteristic | N (%) |
|---|---|
| Total episodes | 953,858 (100%) |
| Year | |
| 2017 | 513,676 (53.9%) |
| 2018 | 440,182 (46.2%) |
| Primary prescriber | |
| NP/PA | 84,763 (8.9%) |
| Physician | 869,095 (91.1%) |
| Multiple prescribers | |
| Yes | 274,199 (28.8%) |
| No | 679,659 (71.3%) |
| Patient gender | |
| Female | 399,876 (41.9%) |
| Male | 553,982 (58.1%) |
| Patient age | |
| 18–25 | 103,617 (10.9%) |
| 26–35 | 377,663 (39.6%) |
| 36–45 | 245,865 (25.8%) |
| 46–55 | 130,488 (13.7%) |
| 56–65 | 73,891 (7.8%) |
| 65+ | 22,334 (2.4%) |
| Buprenorphine episode payer | |
| Commercial | 190,470 (20.0%) |
| Medicaid | 386,135 (40.5%) |
| Medicare | 70,315 (7.4%) |
| Cash | 91,978 (9.6%) |
| Discount/voucher/coupon/rebate | 113,261 (11.9%) |
| Other | 101,699 (10.7%) |
| County urban/rural status | |
| Urban | 830,468 (87.1%) |
| Rural | 123,390 (12.9%) |
| Primary care HPSA | |
| Yes | 887,391 (93.0%) |
| No | 66,467 (7.0%) |
| Mental health care HPSA | |
| Yes | 889,779 (93.3%) |
| No | 64,079 (6.7%) |
| Population quartile | |
| 1st quartile (lowest population) | 88,696 (9.3%) |
| 2nd quartile | 20,349 (2.1%) |
| 3rd quartile | 22,623 (2.4%) |
| 4th quartile (highest population) | 822,190 (86.2%) |
| Median family income quartile | |
| 1st quartile (lowest median income) | 77,031 (8.1%) |
| 2nd quartile | 148,535 (15.6%) |
| 3rd quartile | 166,229 (17.9%) |
| 4th quartile (highest median income) | 461,729 (48.4%) |
| Uninsured rate quartile | |
| 1st quartile (lowest uninsured rate) | 307,053 (32.2%) |
| 2nd quartile | 279,817 (29.3%) |
| 3rd quartile | 202,388 (21.2%) |
| 4th quartile (highest uninsured rate) | 164,600 (17.3%) |
| Fatal overdose (OD) count quartile, previous year | |
| 1st quartile (lowest OD count) | 29,369 (3.1%) |
| 2nd quartile | 59,627 (6.3%) |
| 3rd quartile | 140,737 (14.8%) |
| 4th quartile (highest OD count) | 724,125 (75.9%) |
| Number of active non-NP/PA buprenorphine prescribers by county FIPS | |
| 1st quartile (fewest prescribers) | 16,783 (1.8%) |
| 2nd quartile | 46,067 (4.8%) |
| 3rd quartile | 128,784 (13.5%) |
| 4th quartile (most prescribers) | 760,780 (79.8%) |
Note. HPSA = health professional shortage area; FIPS = Federal Information Processing Standards code.
From 2017 to 2018, the percentage of buprenorphine treatment episodes delivered by NPs and PAs increased from 4.6% to 12.8%, with the overall multivariable regression results showing that the odds of receiving buprenorphine treatment from an NP/PA nearly tripled (adjusted odds ratio [aOR] = 2.86, 95% CI = [2.82, 2.91]; Table 2). Compared with episodes paid for by commercial insurance, those paid for by Medicaid or Medicare had greater odds of being prescribed by an NP/PA. Medicaid episodes in particular had 47% greater odds of being prescribed by an NP/PA versus a physician (aOR = 1.47, 95% CI = [1.44, 1.50]). Individuals receiving buprenorphine from prescribers in rural areas, primary care HPSAs, and mental health care HPSAs also had greater odds of receiving buprenorphine treatment from an NP/PA.
Table 2.
Association of Patient, Community, and State Policy Characteristics with Provision of Buprenorphine Treatment by Nurse Practitioners/Physician Assistants, Overall and by County Urban/Rural Status, 2017 to 2018.
| Unadjusted rate of buprenorphine treatment by NP/PA (%) | Adjusted odds ratios (95% CI) |
|||
|---|---|---|---|---|
| Overall | Urban | Rural | ||
| Patient/episode characteristics | ||||
| Year | ||||
| 2017 | 4.6 | Ref | Ref | Ref |
| 2018 | 12.8 | 2.86 (2.82–2.91) | 2.88 (2.83–2.93) | 2.72 (2.61–2.83) |
| Patient sex | ||||
| Female | 8.7 | Ref | Ref | Ref |
| Male | 8.2 | 0.96 (0.95–0.98) | 0.96 (0.94–0.98) | 0.98 (0.94–1.02) |
| Patient age | ||||
| 18–25 | 8.8 | 1.10 (1.08–1.13) | 1.10 (1.07–1.13) | 1.10 (1.03–1.18) |
| 26–35 | 8.4 | Ref | Ref | Ref |
| 36–45 | 8.0 | 0.97 (0.95–0.99) | 0.96 (0.94–0.98) | 1.01 (0.96–1.06) |
| 46–55 | 8.6 | 1.04 (1.01–1.06) | 1.04 (1.01–1.06) | 1.05 (0.98–1.12) |
| 56–65 | 8.8 | 1.03 (1.00–1.06) | 1.01 (0.98–1.05) | 1.13 (1.03–1.23) |
| 65+ | 9.1 | 1.03 (0.98–1.09) | 1.03 (0.97–1.09) | 1.08 (0.93–1.25) |
| Buprenorphine episode payer | ||||
| Commercial | 6.8 | Ref | Ref | Ref |
| Medicaid | 10.6 | 1.47 (1.44–1.50) | 1.50 (1.46–1.53) | 1.26 (1.19–1.34) |
| Medicare | 9.1 | 1.30 (1.25–1.34) | 1.31 (1.26–1.36) | 1.18 (1.08–1.29) |
| Cash | 6.8 | 1.03 (1.00–1.06) | 1.05 (1.02–1.09) | 0.90 (0.82–0.98) |
| Discount/voucher/coupon/rebate | 5.6 | 0.87 (0.84–0.89) | 0.88 (0.85–0.91) | 0.74 (0.67–0.81) |
| Other | 7.2 | 1.01 (0.98–1.04) | 1.02 (0.99–1.06) | 0.91 (0.83–0.99) |
| Community characteristics | ||||
| Urban/rural status | ||||
| Urban | 8.2 | Ref | — | — |
| Rural | 9.9 | 1.20 (1.16–1.24) | — | — |
| Primary care HPSA | ||||
| Yes | 8.6 | 1.13 (1.08–1.18) | 1.31 (1.24–1.39) | 0.80 (0.75–0.86) |
| No | 6.3 | Ref | Ref | Ref |
| Mental health care HPSA | ||||
| Yes | 8.6 | 1.20 (1.15–1.26) | 1.14 (1.08–1.20) | 0.92 (0.83–1.02) |
| No | 5.8 | Ref | Ref | Ref |
| Population quartile | ||||
| First quartile (lowest population) | 10.8 | Ref | Ref | Ref |
| Second quartile | 7.4 | 0.71 (0.66–0.76) | 0.75 (0.66–0.85) | 0.64 (0.59–0.70) |
| Third quartile | 8.8 | 0.86 (0.81–0.91) | 0.89 (0.80–1.00) | 0.87 (0.81–0.94) |
| Fourth quartile (highest population) | 8.7 | 1.05 (1.01–1.10) | 1.20 (1.12–1.29) | 0.91 (0.85–0.98) |
| Median family income quartile | ||||
| First quartile (lowest median income) | 9.1 | Ref | Ref | Ref |
| Second quartile | 7.6 | 0.89 (0.86–0.93) | 0.92 (0.88–0.97) | 0.89 (0.84–0.94) |
| Third quartile | 7.6 | 0.86 (0.83–0.89) | 0.94 (0.90–0.99) | 0.68 (0.64–0.73) |
| Fourth quartile (highest median income) | 9.0 | 0.97 (0.94–1.01) | 1.05 (1.00–1.10) | 0.82 (0.76–0.90) |
| Uninsured rate quartile | ||||
| First quartile (lowest uninsured rate) | 9.1 | Ref | Ref | Ref |
| Second quartile | 10.1 | 1.35 (1.32–1.38) | 1.44 (1.41–1.47) | 0.96 (0.91–1.01) |
| Third quartile | 9.1 | 1.39 (1.36–1.43) | 1.48 (1.43–1.52) | 1.03 (0.95–1.12) |
| Fourth quartile (highest uninsured rate) | 6.1 | 1.13 (1.09–1.18) | 1.18 (1.14–1.23) | 1.08 (0.99–1.19) |
| Fatal overdose (OD) count quartile, previous year | ||||
| First quartile (lowest OD count) | 9.6 | Ref | Ref | Ref |
| Second quartile | 9.0 | 1.24 (1.18–1.32) | 1.06 (0.95–1.18) | 1.28 (1.20–1.37) |
| Third quartile | 8.7 | 1.23 (1.16–1.31) | 0.99 (0.89–1.10) | 1.32 (1.23–1.42) |
| Fourth quartile (highest OD count) | 8.2 | 1.20 (1.13–1.28) | 0.97 (0.87–1.08) | 1.41 (1.28–1.55) |
| Number of active non-NP/PA buprenorphine prescribers | ||||
| First quartile (fewest prescribers) | 10.9 | Ref | Ref | Ref |
| Second quartile | 7.0 | 0.62 (0.58–0.66) | 0.66 (0.58–0.76) | 0.56 (0.52–0.61) |
| Third quartile | 10.0 | 0.69 (0.64–0.74) | 0.75 (0.66–0.86) | 0.85 (0.79–0.91) |
| Fourth quartile (most prescribers) | 8.6 | 0.87 (0.82–0.93) | 0.59 (0.51–0.67) | 0.79 (0.72–0.86) |
| State policies | ||||
| Full SOP for NPs | ||||
| Yes | 9.2 | 2.11 (2.07–2.15) | 2.17 (2.13–2.21) | 2.02 (1.92–2.13) |
| No | 6.6 | Ref | Ref | Ref |
| Full SOP for PAs | ||||
| Yes | 9.6 | 1.30 (1.27–1.33) | 1.34 (1.31–1.37) | 1.16 (1.09–1.24) |
| No | 8.2 | Ref | Ref | Ref |
| Medicaid pay parity for NPs | ||||
| Yes | 9.3 | 1.20 (1.18–1.22) | 1.23 (1.21–1.26) | 1.25 (1.19–1.31) |
| No | 7.0 | Ref | Ref | Ref |
| State Medicaid expansion | ||||
| Yes | 9.2 | 1.06 (1.03–1.08) | 0.99 (0.97–1.02) | 1.47 (1.36–1.59) |
| No | 6.6 | Ref | Ref | Ref |
Note. HPSA = health professional shortage area; SOP = scope of practice.
Overall, state policy characteristics associated with greater odds of receiving buprenorphine treatment from an NP/PA versus a physician included full SOP for NPs (aOR = 2.11, 95% CI = [2.07, 2.15]), full SOP for PAs (aOR = 1.30, 95% CI = [1.27, 1.33]), Medicaid pay parity for NPs (aOR = 1.20, 95% CI = [1.18, 1.22]), and state Medicaid expansion (aOR = 1.06, 95% CI = [1.03, 1.08]; Table 2). When regressions were stratified by urban and rural counties, findings with respect to policies were similar. For example, the association of full SOP for PAs with buprenorphine treatment from an NP/PA was slightly stronger in urban counties (aOR = 1.34, 95% CI = [1.31, 1.37]) than in rural counties (aOR = 1.16, 95% CI = [1.09, 1.24]). The exception was Medicaid expansion, which was associated with nearly 50% greater odds of buprenorphine treatment from an NP/PA in rural counties (aOR = 1.47, 95% CI = [1.36, 1.59]) but was not significantly associated with buprenorphine treatment from an NP/PA in urban counties. Findings did not differ appreciably in a sensitivity analysis excluding states that changed their SOP laws during 2017 to 2018: South Dakota, Virginia, and Illinois.
We conducted two sensitivity analyses to examine the extent to which our findings are driven by payer: one excluding episodes with Medicaid as the primary payer and one limited to episodes with Medicaid as the primary payer (Online Appendix Tables A-3 and A-4). In the non-Medicaid subgroup, the associations of state policies with NP/PA buprenorphine treatment were similar or slightly stronger, and Medicaid expansion was associated with greater odds of NP/PA buprenorphine treatment in both rural and urban counties. In the Medicaid subgroup, we observed similar findings with regard to NP SOP and Medicaid pay parity, though the strength of these associations was slightly weaker. Full SOP for PAs was associated with greater odds of buprenorphine treatment from an NP/PA overall and in urban counties but not in rural counties. Notably, in the Medicaid subgroup, state Medicaid expansion was associated with 67% greater odds of buprenorphine treatment from an NP/PA in rural counties (OR = 1.67, 95% CI = [1.48, 1.90]) but lower odds of buprenorphine treatment from an NP/PA overall and in urban counties.
Discussion
This study is one of the first to use all-payer pharmacy claims to examine the association of state policies with buprenorphine prescribing by NPs and PAs. Nationally, the percentage of buprenorphine treatment episodes delivered by NPs/PAs nearly tripled from 2017 to 2018, likely driven by the increase in waivered NPs and PAs during this period. The wide variation across states in the share of buprenorphine treatment episodes delivered by NPs/PAs, ranging from <1% in Alabama to 57% in Montana, suggests that state policies likely influence buprenorphine prescribing among NPs and PAs.
Consistent with previous findings, our results suggest that restrictive state SOP laws may be creating substantial barriers to prescribing buprenorphine (Auty et al., 2020; Barnett et al., 2019; Nguyen et al., 2021; Spetz et al., 2019, 2021). In several previous studies, less restrictive SOP laws have been associated with greater waiver uptake among NPs but not among PAs (Auty et al., 2020; Barnett et al., 2019; Spetz et al., 2019), potentially because laws in all states require PAs to work in collaboration with physicians, and fewer PAs than NPs practice in primary care or psychiatry (Barnett et al., 2019). In contrast, we found that both full SOP for NPs and full SOP for PAs were associated with greater odds of receiving buprenorphine treatment from an NP/PA versus a physician. Although SOP laws have not been associated with waiver uptake among PAs in previous studies, we found that waivered PAs prescribe more buprenorphine in states with less restrictive SOP laws, suggesting that SOP laws may influence the volume of buprenorphine prescribing among waivered PAs. However, our finding should be interpreted with caution as our study was cross-sectional in nature. Our finding that less restrictive SOP laws for NPs are associated with more NP buprenorphine treatment is consistent with Nguyen et al., who found that among a commercially insured and Medicare Advantage population, NPs wrote 2.7% of buprenorphine prescriptions in states with less restrictive SOP laws and 1.1% in states with more restrictive SOP laws between the third quarter of 2016 and the third quarter of 2018 (Nguyen et al., 2021). Given that commercial insurance covered only 20% of buprenorphine treatment episodes from 2017 to 2018, 40% of buprenorphine treatment episodes were covered by Medicaid, and many patients paid via cash, discount/voucher/coupon/rebate, or other sources such as Tricare or workers compensation, our work highlights the importance of examining patterns of buprenorphine treatment among multiple payers.
To our knowledge, no studies have examined the association of Medicaid pay parity with delivery of OUD treatment by NPs and PAs. We found that Medicaid pay parity for NPs was associated with greater odds of receiving buprenorphine treatment from an NP/PA, regardless of episode payer. In a previous study, Barnes et al. (2017) found that in states with full SOP and Medicaid pay parity at 100% of physician rates, NPs were more likely to practice in primary care, and a higher number of practices employing NPs accepted Medicaid. Reimbursement parity is particularly important for NPs who practice independently and may incentivize NPs to practice in areas with provider shortages (Bischof & Greenberg, 2021). Further investigation is needed to better understand the implications of Medicaid pay parity for treatment of OUD by NPs and PAs, including the implications for provider mix and financial stability of practices that provide OUD treatment.
Previous evidence suggests that state Medicaid expansion significantly increased buprenorphine prescribing in expansion counties (Saloner et al., 2018), and OUD treatment covered by Medicaid increased more in states with Medicaid expansion than those without (Clemans-Cope et al., 2017; Wen et al., 2017). Medicaid expansion has also been associated with increased OUD medication prescribing to Medicare Part D beneficiaries, suggesting positive spillover effects for non-Medicaid populations (Abraham et al., 2021). Although we cannot make causal inferences with these cross-sectional analyses, we found that Medicaid expansion was associated with greater odds of receiving buprenorphine treatment from an NP/PA versus a physician in rural counties, and the results of our subgroup analysis suggest potential spillover to non-Medicaid populations. Although not causal, the association we observe suggests that Medicaid expansion may play an important role in increasing access to buprenorphine treatment from NPs/PAs in rural areas, where many NPs and PAs were the first waivered clinicians in their counties (Barnett et al., 2019). Rural NPs and PAs may also work in smaller practices that disproportionately benefit from Medicaid expansion. Compared with urban NPs, rural NPs more often report being the only provider in their practice or working alongside only one or two other providers (Germack et al., 2022).
We interpret these results in the context of several limitations. Most importantly, our observational methods only allow us to determine associations and cannot establish a causal effect of state policies on buprenorphine prescribing by NPs/PAs. Future work should incorporate longitudinal data and causal inference methods to establish the effects of these policies. Although IQVIA captures 90% of retail pharmacy claims with no known systematic variation by region or type of organization, it is possible that our results do not generalize to the 10% of claims not captured by IQVIA. The data are limited to filled buprenorphine prescriptions; we have no information about unfilled prescriptions, prescriptions filled at pharmacies not in the IQVIA data, or buprenorphine obtained without a prescription. Our analysis included 1,804 counties, indicating that in 2017 to 2018 approximately 1,200 U.S. counties did not have an active buprenorphine prescriber. Although we limited our analyses to buprenorphine formulations with an FDA-approved indication for OUD treatment, individuals may receive buprenorphine for off-label treatment of pain. Additional state policies may influence NP and PA prescribing (Spetz et al., 2021), and further work is needed to consider the effects of those policies. We used policies identified as of 2016 to coincide with the passage of CARA, but it is possible some states may have subsequently changed their policies. Finally, NP/PA activities may not be fully captured in pharmacy claims. It is possible that some NP/PA prescriptions are attributed to physicians, which would lead us to underestimate the number of buprenorphine prescriptions dispensed by NPs/PAs.
Conclusion
At a time when the opioid crisis appears to be worsening, with over 90,000 overdose deaths in 2020 (Ahmad et al., 2021), many primary care physicians appear to remain reluctant to prescribe buprenorphine (Huhn & Dunn, 2017; McGinty et al., 2020), and many patients continue to face barriers to accessing buprenorphine treatment (Patrick et al., 2020), it is critical to identify policies associated with the increased provision of buprenorphine for OUD. Our findings suggest that state policies, including less restrictive SOP laws, Medicaid pay parity policies, and Medicaid expansion, may increase the capacity of the NP/PA workforce to provide buprenorphine treatment for OUD. In rural areas, where access to buprenorphine treatment is often limited (Andrilla et al., 2019; Rosenblatt et al., 2015), policies such as Medicaid expansion may be particularly important to increase access to buprenorphine treatment. Longitudinal analyses to assess the effects of such policies on access to buprenorphine treatment and the quality of treatment provided as well as the effects of evolving policies related to telehealth, reimbursement, and insurance coverage for substance use disorders will play an important role in public health efforts to expand access to effective treatment for individuals with OUD.
Supplementary Material
Funding
The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported by the National Institute on Drug Abuse (NIDA) through P50DA046351 and R01DA045800.
Footnotes
Declaration of Conflicting Interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Supplemental Material
Supplemental material for this article is available online.
References
- Abraham AJ, Lawler EC, Harris SJ, Bagwell Adams G, & Bradford WD (2021). Spillover of Medicaid expansion to prescribing of opioid use disorder medications in Medicare part D. Psychiatric Services. Advance online publication. 10.1176/appi.ps.202000824 [DOI] [PubMed] [Google Scholar]
- Ahmad FB, Rossen LM, & Sutton P (2021). Provisional drug overdose death counts. https://www.cdc.gov/nchs/nvss/vsrr/drug-overdose-data.htm
- American Association of Nurse Practitioners. (2021). State practice environment. Retrieved May 7, 2021, from https://www.aanp.org/advocacy/state/state-practice-environment
- American Association of Physician Assistants. (2020). The six key elements of a modern PA practice act. https://www.aapa.org/download/29342/
- American Association of Physician Assistants. (2021). How Medicaid covers PA services. https://www.aapa.org/advocacy-central/reimbursement/medicaid/624/
- Andrilla CHA, Moore TE, Patterson DG, & Larson EH (2019). Geographic distribution of providers with a DEA waiver to prescribe buprenorphine for the treatment of opioid use disorder: A 5-year update. Journal of Rural Health, 35, 108–112. 10.1111/jrh.12307 [DOI] [PubMed] [Google Scholar]
- Andrilla CHA, & Patterson DG (2021). Tracking the geographic distribution and growth of clinicians with a DEA waiver to prescribe buprenorphine to treat opioid use disorder. The Journal of Rural Health, 38, 87–92. 10.1111/jrh.12569 [DOI] [PubMed] [Google Scholar]
- Auty SG, Stein MD, Walley AY, & Drainoni M-L (2020). Buprenorphine waiver uptake among nurse practitioners and physician assistants: The role of existing waivered prescriber supply. Journal of Substance Abuse Treatment, 115, Article 108032. 10.1016/jjsat.2020.108032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barnes H, Maier CB, Altares Sarik D, Germack HD, Aiken LH, & McHugh MD (2017). Effects of regulation and payment policies on nurse practitioners’ clinical practices. Medical Care Research and Review, 74(4), 431–451. 10.1177/1077558716649109 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barnes H, Richards MR, McHugh MD, & Martsolf G (2018). Rural and nonrural primary care physician practices increasingly rely on nurse practitioners. Health Affairs, 37(6), 908–914. 10.1377/hlthaff.2017.1158 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barnett ML, Lee D, & Frank RG (2019). In rural areas, buprenorphine waiver adoption since 2017 driven by nurse practitioners and physician assistants. Health Affairs (Project Hope), 38(12), 2048–2056. 10.1377/hlthaff.2019.00859 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bischof A, & Greenberg S (2021). Post COVID-19 reimbursement parity for nurse practitioners. OJIN: The Online Journal of Issues in Nursing, 26(2), Article 3. 10.3912/OJIN.Vol26No02Man03 [DOI] [Google Scholar]
- Buerhaus PI, DesRoches CM, Dittus R, & Donelan K (2015). Practice characteristics of primary care nurse practitioners and physicians. Nursing Outlook, 63(2), 144–153. 10.1016/j.outlook.2014.08.008 [DOI] [PubMed] [Google Scholar]
- Cawley JF, Lane S, Smith N, & Bush E (2016). Physician assistants in rural communities. Journal of the American Academy of Physician Assistants, 29(1), 42–45. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. (2020). Drug overdose deaths. https://www.cdc.gov/drugoverdose/deaths/index.html
- Clemans-Cope L, Lynch V, Epstein M, & Kenney G (2017). Medicaid coverage of effective treatment for opioid use disorder.
- Comprehensive Addiction and Recovery Act of 2016, S.524, 114th Cong. (2016).
- Connery HS (2015). Medication-assisted treatment of opioid use disorder. Harvard Review of Psychiatry, 23(2), 63–75. 10.1097/hrp.0000000000000075 [DOI] [PubMed] [Google Scholar]
- Davis MA, Anthopolos R, Tootoo J, Titler M, Bynum JPW, & Shipman SA (2018). Supply of healthcare providers in relation to county socioeconomic and health status. Journal of General Internal Medicine, 33(4), 412–414. 10.1007/s11606-017-4287-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dick AW, Pacula RL, Gordon AJ, Sorbero M, Burns RM, Leslie D, & Stein BD (2015). Growth in buprenorphine waivers for physicians increased potential access to opioid agonist treatment, 2002-11. Health Affairs (Project Hope), 34(6), 1028–1034. 10.1377/hlthaff.2014.1205 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Germack HD, Harrison J, Poghosyan L, & Martsolf GR (2022). Practice patterns, work environments, and job outcomes of rural and urban primary care nurse practitioners. Medical Care Research and Review, 79(1), 161–170. [DOI] [PubMed] [Google Scholar]
- Harkless G, & Vece L (2018). Systematic review addressing nurse practitioner reimbursement policy: Part one of a four-part series on critical topics identified by the 2015 nurse practitioner research agenda. Journal of the American Association of Nurse Practitioners, 30(12), 673–682. 10.1097/JXX.0000000000000121 [DOI] [PubMed] [Google Scholar]
- Huhn AS, & Dunn KE (2017). Why aren’t physicians prescribing more buprenorphine? Journal of Substance Abuse Treatment, 78, 1–7. 10.1016/jjsat.2017.04.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- IMPAQ International. (2019). Buprenorphine prescribing by nurse practitioners, physician assistants, and physicians after CARA 2016. https://www.macpac.gov/publication/buprenorphine-prescribing-by-nurse-practitioners-physician-assistants-and-physicians-after-cara-2016/?sfw=pass1619209149
- IQVIA: Real World Data and Insights. (n.d.). https://www.iqvia.com/solutions/%0Dreal-world-evidence/real-world-data-and-insights
- Jones CM, Campopiano M, Baldwin G, & McCance-Katz E (2015). National and state treatment need and capacity for opioid agonist medication-assisted treatment. American Journal of Public Health, 105(8), e55–e63. 10.2105/AJPH.2015.302664 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaiser Family Foundation. (n.d.). Status of state action on the Medicaid expansion decision. https://www.kff.org/health-reform/state-indicator/state-activity-around-expanding-medicaid-under-the-affordable-care-act/
- McBain RK, Dick A, Sorbero M, & Stein BD (2020). Growth and distribution of buprenorphine-waivered providers in the United States, 2007–2017. Annals of Internal Medicine, 172(7), 504–506. 10.7326/m19-2403 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGinty EE, Stone EM, Kennedy-Hendricks A, Bachhuber MA, & Barry CL (2020). Medication for opioid use disorder: A national survey of primary care physicians. Annals of internal medicine, 173(2), 160–162. 10.7326/M19-3975 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Medicaid and CHIP Payment and Access Commission. (2017a). State Medicaid fee-for-service physician payment policies. https://www.macpac.gov/publication/states-medicaid-fee-for-service-physician-payment-policies/?sfw=pass1620560395
- Medicaid and CHIP Payment and Access Commission. (2017b). Report to congress on Medicaid and CHIP June 2017: Chapter 2—Medicaid and the opioid epidemic. https://www.macpac.gov/wp-content/uploads/2017/06/Medicaid-and-the-Opioid-Epidemic.pdf
- Moore DJ (2019). Nurse practitioners’ pivotal role in ending the opioid epidemic. Journal for Nurse Practitioners, 15(5), 323–327. 10.1016/j.nurpra.2019.01.005 [DOI] [Google Scholar]
- National Center for Health Statistics. (2014). 2013 NCHS urban-rural classification scheme for counties (Vol. 2). [PubMed] [Google Scholar]
- National Judicial Opioid Task Force. (2019). Promising strategies in providing opioid use disorder treatment to rural, frontier, and other underserved communities. https://www.ncsc.org/__data/assets/pdf_file/0019/17614/oud-txt-in-rural-areas-final.pdf
- Nguyen T, Muench U, Andraka-Christou B, Simon K, Bradford WD, & Spetz J (2021). The association between scope of practice regulations and nurse practitioner prescribing of buprenorphine after the 2016 opioid bill. Medical Care Research and Review, 79(2), 290–298. 10.1177/10775587211004311 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Orgera K, & Tolbert J (2019). The opioid epidemic and Medicaid’s role in facilitating access to treatment. https://www.kff.org/medicaid/issue-brief/the-opioid-epidemic-and-medicaids-role-in-facilitating-access-to-treatment/
- Patrick SW, Richards MR, Dupont WD, McNeer E, Buntin MB, Martin PR, Davis MM, Davis CS, Hartmann KE, Leech AA, Lovell KS, Stein BD, & Cooper WO (2020). Association of pregnancy and insurance status with treatment access for opioid use disorder. JAMA Network Open, 3(8), Article e2013456. 10.1001/jamanet-workopen.2020.13456 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Phillips SJ (2016). 28th Annual APRN legislative update. The Nurse Practitioner, 41(1), 21–48. [DOI] [PubMed] [Google Scholar]
- Rosenblatt RA, Andrilla CHA, Catlin M, & Larson EH (2015). Geographic and specialty distribution of US physicians trained to treat opioid use disorder. Annals of Family Medicine, 13, 23–26. 10.1370/afm.1735 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ruhm CJ (2018). Corrected US opioid-involved drug poisoning deaths and mortality rates, 1999-2015. Addiction, 113(7), 1339–1344. 10.1111/add.14144 [DOI] [PubMed] [Google Scholar]
- Saloner B, Levin J, Chang H-Y, Jones C, & Alexander GC (2018). Changes in buprenorphine-naloxone and opioid pain reliever prescriptions after the affordable care act Medicaid expansion. JAMA Network Open, 1(4), Article e181588. 10.1001/jamanetworkopen.2018.1588 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schuler MS, Heins SE, Smart R, Griffin BA, Powell D, Stuart EA, Pardo B, Smucker S, Patrick SW, Pacula RL, & Stein BD (2020). The state of the science in opioid policy research. Drug and Alcohol Dependence, 214, Article 108137. 10.1016/j.drugalcdep.2020.108137 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spetz J, Chapman S, Tierney M, Phoenix B, & Hailer L (2021). Barriers and facilitators of advanced practice registered nurse participation in medication treatment for opioid use disorder: A mixed methods study. Journal of Nursing Regulation, 12(2), 5–22. 10.1016/S2155-8256(21)00052-1 [DOI] [Google Scholar]
- Spetz J, Toretsky C, Chapman S, Phoenix B, & Tierney M (2019). Nurse practitioner and physician assistant waivers to prescribe buprenorphine and state scope of practice restrictions. JAMA, 321(14), 1407–1408. 10.1001/jama.2019.0834 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stein BD, Jones CM, Smart R, Sheng F, & Sorbero M (2021). Patient, prescriber, and community factors associated with filled naloxone prescriptions among patients receiving buprenorphine 2017-18. Drug and Alcohol Dependence, 221, Article 108569. 10.1016/j.drugalcdep.2021.108569 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thomas CP, Doyle E, Kreiner PW, Jones CM, Dubenitz J, Horan A, & Stein BD (2017). Prescribing patterns of buprenorphine waivered physicians. Drug and Alcohol Dependence, 181, 213–218. 10.1016/j.drugalcdep.2017.10.002 [DOI] [PubMed] [Google Scholar]
- U.S. Census Bureau. (2011). Selected housing characteristics, 2007-2011 American Community Survey 5-year estimates. https://www.census.gov/programs-surveys/acs
- U.S. Department of Health and Human Services Health Resources and Services Administration. (n.d.). Area health resources files. 2006-2019. https://data.hrsa.gov/topics/health-workforce/ahrf
- Wen H, Hockenberry JM, Borders TF, & Druss BG (2017). Impact of Medicaid expansion on Medicaid-covered utilization of buprenorphine for opioid use disorder treatment. Medical Care, 55(4), 336–341. 10.1097/MLR.0000000000000703 [DOI] [PubMed] [Google Scholar]
- Xue Y, Smith JA, & Spetz J (2019). Primary care nurse practitioners and physicians in low-income and rural areas, 2010-2016. JAMA, 321(1), 102–105. 10.1001/jama.2018.17944 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


