Abstract
Introduction
Endotracheal intubation and positive pressure ventilation following delivery are required in 32.9% of neonates <31 weeks gestational age and in 5.9% of older newborn babies [1]. Competency in intubation is important, yet opportunities for learners to develop this skill in the clinical environment are limited. Direct laryngoscopy (DL) provides a direct view of the airway during intubation. Unfortunately, visualization of the airway is only available to the primary operator, preventing supervising instructors from simultaneously viewing the airway and allowing them to provide real-time feedback to learners. Video laryngoscopy (VL) is a specialized clinical instrument that utilizes an indirect view of the airway that is digitally projected onto a screen via camera, which allows multiple simultaneous viewers to view the airway during intubation attempts and permits instructors to provide real-time feedback to learners accordingly.
Objectives
This systematic review explores whether VL-supported learning is superior to DL for the development of skill in neonatal intubation.
Methods
Systematic searches of MEDLINE, EMBASE, CINAHL and the Cochrane Library were conducted without language restrictions. Studies published between January 2011 and November 2021 were examined. Randomized controlled trials (RCTs) comparing the effectiveness of VL versus DL for supporting neonatal intubation learning were included. Rate of successful intubation was the primary outcome measure. Both authors independently extracted study data and conducted risk of bias assessment.
Results
Four RCTs met the inclusion criteria, with two incorporating crossover designs. Each examined the effectiveness of VL versus DL, with concurrent supervisor support, as a tool for learning neonatal intubation in medical residents. All studies reported significantly higher intubation success rates with VL.
Conclusion
VL and real-time supervisor feedback is a more effective tool for supporting the development of neonatal intubation skill, compared with DL. Future investigations should include learners from other professions whose scope of practice includes neonatal intubation (eg, respiratory therapists).
Key Words: allied health personnel, education, infant, intratracheal, intubation, laryngoscopy, newborn
INTRODUCTION
Endotracheal intubation and positive pressure ventilation following delivery are required in 32.9% of premature neonates <31 weeks gestational age and 5.9% of those ≥31 weeks gestational age [1]. Endotracheal intubation of neonates and infants is also required for situations such as surfactant administration, resuscitation outside the post-natal period, or to secure an airway in the operating room, although the frequency of these events is unclear.
Endotracheal intubation is an invasive procedure used to secure an airway by passing an endotracheal tube (ETT) through the glottis and into the trachea. Neonatal intubation can be more complex than that of older children or adults due to the unique airway morphology and physiology of neonates. Neonatal intubation success rates are inversely proportional to neonatal intubation experience [2] and the definition of a successful intubation varies in the literature [2]. Consequences of failed intubations to the neonatal patient include airway injury, hypoxia and hemodynamic instability [3]. As a result, it is important that health care professionals become competent in intubation. Intubation is a skill required of many health care professionals (eg, respiratory therapy students, medical residents) and is difficult to master [3]. Learners may receive didactic education and hands-on practice with task trainers and/or simulation mannequins before progressing to a clinical, or patient care, setting. However, using task trainers and mannequins does not allow for the real-time problem solving associated with neonatal intubation and/or environmental stressors typically experienced in the clinical setting [4]. Furthermore, the anatomy of many mannequins does not change which prevents learners from experiencing dynamic, anatomical changes in real-time [5]. Once in the clinical setting, there are often limited opportunities to further develop proficiency in intubation due to factors such as the increased use of noninvasive ventilation and increasing number of learners requiring practice [3, 6, 7].
Traditionally, intubation is performed by direct laryngoscopy (DL) using a conventional laryngoscope. When a learner performs DL, they have a direct line of sight view (ie, direct view) of the patient’s airway. If the learner requires assistance during an intubation attempt, the small space and mouth opening prevent the supervisor (ie, instructor, supervising professional) from also visualizing the airway [7] and the supervisor must rely on verbal descriptions from the learner to provide support.
Since the 2010s, video laryngoscopy (VL) has routinely become integrated into practice [6]. VL provides indirect visualization of the airway via an internal camera which projects an image onto a video screen [8]. The use of the screen with VL allows the learner intubating, as well as the supervisor to visualize the patient’s anatomy on a video monitor. This may prove to be advantageous when learners are intubating, as both the learner and their supervisor can visualize the airway and provide real-time coaching [7]. Additionally, intubation attempts can be recorded using a video laryngoscope which may be viewed at a later time for debriefing and learning purposes [7].
Despite these benefits, VL has not fully replaced DL [9], so it is important that learners also develop competence in DL. VL can be adapted to assist the learner in developing direct visualization skills for DL. For example, the VL setup can be modified so that only the supervisor is able to view the screen. The learner, forced to use a direct view of the airway, practices their DL technique, while the supervisor is able to provide real-time feedback [10].
Objective
While other studies have investigated the use of VL for intubation in adult [11], neonatal [3, 12] or paediatric [13] patients, a synthesis of data on its use as a teaching tool when intubating neonatal patients has not been completed. It is important to establish whether the use of VL with concurrent coaching by a supervisor increases intubation learning and success, due to the limited opportunities for practice. The purpose of this systematic review is to address the question “Does the use of VL, accompanied by coaching from a supervisor with an indirect view of the airway, improve the rate of neonatal intubation success (compared with DL) in learners?”.
METHODS
Data sources and search strategies
This systematic review was conducted in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines [14]. A systematic literature search of four databases (PubMed, CINAHL, EMBASE and the Cochrane Library) and Clinicaltrials.gov [15] was conducted (January 2011 to November 1, 2021). No limits were placed on the language of publication. Search terms used in CINAHL, EMBASE and the Cochrane Library were neonatal AND video laryngoscope AND intubation AND learner OR teach. MeSH terms and synonyms were determined and included infant, education, newborn and intubated. The PubMed database search was completed on November 1, 2021 (see Appendix 11). Searches yielded 13 unique studies. Of these, four studies met the inclusion criteria and nine were unrelated or did not meet the eligibility requirements. Reference lists of included studies were searched for relevant papers.
Study selection
Both authors independently assessed the title and abstract of articles according to the eligibility criteria and removed all duplicates. Each author read and assessed each chosen full-text article for inclusion criteria. Differences in study selection were resolved through discussion. Studies were included in the review if they met the following criteria: (1) study participants: learners in a health profession or medical education programme with limited experience in neonatal intubation; (2) study intervention: compared VL to DL along with coaching as a teaching tool for intubation of preterm or term human neonates or infants; (3) outcome: successful endotracheal intubation; and (4) study design: randomized controlled trials (RCTs) (as observational studies would not answer the research question). Studies comparing VL to DL as a teaching tool for intubation on mannequins or in a simulated environment were excluded as this has been previously reviewed in both the neonatal [16] adult [17] contexts.
Data extraction
The following data was extracted independently by both authors: hospital type, participant demographics, study population size, patient gestational age, intervention and primary outcome measures. Differences in the extracted data were resolved through discussion.
Risk of bias assessment
Both authors independently assessed the risk of bias for each study using the Cochrane Risk of Bias 2 (RoB2) tool [18] or the RoB2 for Crossover trials [19]. Differences in assessments were resolved through discussion and consensus.
RESULTS
Search results
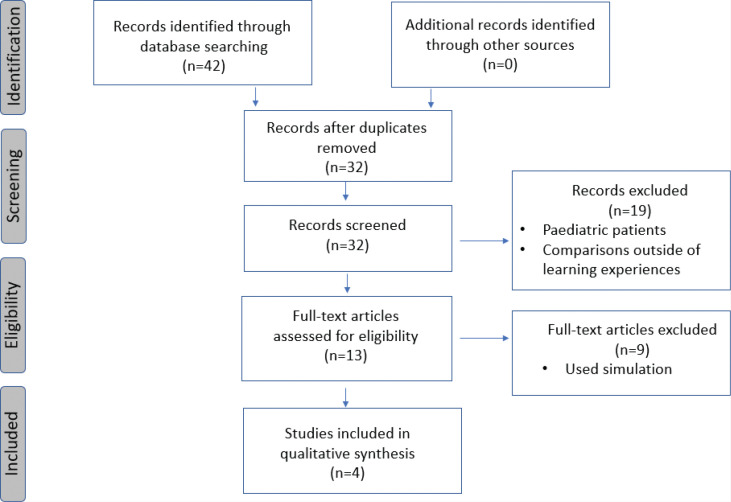
A total of 42 studies were identified through the initial search (Figure 1). After removing 10 duplicates, each author screened the title and abstracts to exclude papers that did not meet the inclusion criteria. These studies were excluded because they included only paediatric patients or only compared VL to DL outside of a teaching context. The second round of screening was completed by reviewing the full text of the remaining 13 eligible studies. Of the 13 eligible studies, nine were excluded as they investigated the use of VL versus DL in simulations using mannequins or focused on the use of VL for intubation, not as a teaching tool. Four studies met all inclusion criteria for this review: two parallel RCT [7, 10] and two RCTs with crossover [6, 20].
FIGURE 1.
Flow diagram of systematic search results
Study characteristics
Characteristics of included studies are summarized in Appendix 22 with extracted data in Table 1. Four RCTs [6, 7, 10, 20] met the inclusion criteria for this review, with two using crossover designs [6, 20]. All four RCTs were conducted in hospital settings of a neonatal intensive care unit (NICU), labour and delivery ward, or operating room. Participants in the studies were anesthesiology residents, paediatric residents, or residents in a combined medicine-paediatrics programme with limited prior experience intubating neonates. The patients were preterm or term neonates between 1 day and 6 months of age. All studies used successful intubation as the primary outcome, although there were differences in the number of attempts that qualified as a successful intubation. Overall, the trials deemed intubation as successful if it occurred in three or fewer attempts.
TABLE 1.
Characteristics of the included studies
| Study, year and location | Hospital type | Participants | Patient gestational age | Study details | Intervention | Primary outcome measures | Outcome |
|---|---|---|---|---|---|---|---|
| O’Shea et al. (2015) Australia | Tertiary Perinatal Centre – Urban (7500 births per year) | Pediatric residents in first 6 months of training (n=36) |
26–32 weeks | Single centre RCT 206 intubations (VL: 104; CL: 102) |
Use of video laryngoscope for neonatal intubation by learner Supervisor with access to screen offers verbal assistance for intubation with standardized coaching approach Standardized debriefing was offered following intubation attempts. |
First attempt intubation success | Success rate: VL: 66%; CL: 41% Unadjusted OR=2.81 with 95% CI (1.54–5.17), P<0.01 |
| Moussa et al., (2016) Canada | Single Centre, Tertiary Academic Hospital – Urban (3500 births per year) | Pediatric residents in first 3 years of residency Phase 1 n=34 Phase 2 n=23 |
25–34 weeks | Single centre RCT with crossover of the experimental group 268 intubations (VL:125; CL:143) |
Video laryngoscope used with indirect vision during neonatal intubation Supervisor with access to video screen for verbal assistance |
Successful intubation in three or fewer attempts | Success rate: VL: 75.2%; CL:63.4% Likelihood ratio –1.20 95% CI (–2.31 to –0.10), P=0.03 |
| Volz et al., (2018) USA | Tertiary Academic Hospital – Urban (Number of births not provided) | First and second year pediatric or medicine-pediatric residents n=40 |
27–37 weeks | Single centre RCT 101 intubations (VL:37; CL: 80 (includes 40 neonates randomized to the VL group who were too small for VL blade) |
Resident coaching during direct laryngoscopy with the use of video as a coaching tool Supervisor with access to video screen for verbal assistance. Standardization of coaching language |
Successful intubation, within two attempts | Success rate: VL: 57%; CL: 33% (results reflect patients <1000 g intubated using CL), P<0.02 |
| Saran et al., (2019) India | Tertiary Academic Hospital – Urban (Number of births not provided) | Anesthesiology residents in first or second year (n=24) |
Term Patients between 1 day and 6 months | Single centre Crossover RCT 144 intubations (36 in each crossover group) |
Use of video laryngoscope for neonatal and infant intubation with verbal assistance from supervisor Both supervisor and trainee with visual access to video screen |
First attempt intubation success | Success rate: VL: 83.3%; CL: 44.4%, Likelihood ratio=1.98 and P≤0.001 |
RCT = randomized controlled trial; VL = video laryngoscopy; CL = conventional laryngoscopy.
Outcomes
A total of 719 intubations were analyzed across the studies and all four studies demonstrated a significantly higher intubation success rate in the VL versus the DL group (Table 1).
O’Shea et al. [7] compared VL and DL intubation success rates and the effect of premedication on intubation success in 206 neonates. There was a significantly higher success rate in the VL versus the DL groups regardless of premedication status. The success rates for both VL and DL were higher when the patients were premedicated versus when they were not (not premedicated: VL: 66% [69/104]; DL: 41% [42/102], P<0.001; premedicated: VL: 72% [56/78]; DL: 44% [35/79], P<0.001). The present study was one of two studies in this review where researchers did not permit learners to view the intubation video monitor when performing VL so that they could develop skill in DL (ie, the VL functioned as a DL). The authors concluded that this led to a significant improvement in DL.
Volz et al. [10] analyzed 101 intubations that included structured coaching during intubation attempts. There was a significantly higher success rate in the VL versus the DL group (VL: 57% (35/61); DL: 33% (13/40), P<0.02). The VL device used in the present study could not intubate neonates weighing less than 1000 g, so these patients were moved to the DL group if they had been randomized to the VL arm. The present study was one of two that had learners develop DL skills by using the VL to perform DL by not viewing the camera video feed. The authors concluded that learners who performed DL while being coached by a supervisor with a monitor view of the airway demonstrated improved success rates compared with DL.
Moussa et al. [6] used a crossover design. In phase 1, the two groups included a VL group and a DL group (213 intubations). In phase 2, the VL group switched to using DL while the phase 1 DL group continued using DL (55 intubations). In phase 1, VL demonstrated a significantly higher success rate than DL (VL: 75.2% [84/112]; DL: 63.4% [64/101], P=0.03). When the VL group subsequently performed DL, the DL intubation success rate was almost equal to that of the DL group which did not have prior VL experience (VL: 63.4% vs. 63.0%, P=0.5). The present study was the only one to investigate the retention of skills with one group completing DL in both phases of the study. The phase 2 DL group had a higher success rate than they did in phase 1 (phase 1: 63%, phase 2: 77%, P=0.10), although it was not significant. The present study did not provide information on the time between phases.
Finally, a crossover study by Saran et al. [20] analyzed 144 intubations and reported that VL had a significantly higher success rate in both phases of the study (phase 1: VL: 80.5% [29/36], DL: 41.6% [15/36], P≤0.0007; phase 2 [crossover]: VL: 86.1% [31/36], DL: 47.2% [17/36], P≤0.0004). The present study did not provide information on the time between phases.
Risk of bias
Risk of bias assessment is presented in Table 2. Given the nature of the intervention, neither learners nor supervisors could be blinded to the type of laryngoscope being used (ie, VL vs. DL). In all studies, participants in each arm received the same education regarding intubation and were familiarized with the equipment for VL and DL. For the two studies incorporating a crossover design, it was not clear if a washout period was incorporated to minimize any carryover (or transfer of skill) effect. However, the results from each study do not indicate that carryover occurred. All four studies were deemed to be a low risk of bias.
TABLE 2.
Methodological appraisals of included studies
| Randomized control trials without crossover | ||||||
|---|---|---|---|---|---|---|
| Study, year | Randomization process | Deviations from intended interventions | Missing outcome data | Measurement of the outcome | Selection of reported results | Overall |
| O’Shea et al., 2015 | Low | Low | Low | Low | Low | Low |
| Volz et al, 2018 | Low | Low | Low | Low | Low | Low |
Sterne JAC, Savović J, Page MJ, et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ 2019;366:l4898.
| Randomized control trials with crossover | |||||||
| Study, year | Randomi-zation process | Carryover effects | Deviations from intended interventions | Missing outcome data | Measurement of the outcome | Selection of reported results | Overall |
| Saran et al., 2019 | Low | Low | Low | Low | Low | Low | Low |
| Moussa et al., 2016 | Low | Low | Low | Low | Low | Low | Low |
Higgins J, Li T, Altman D, Curtin F, Senn S. Revised Cochrane risk of bias tool for randomized trials (RoB 2) Additional considerations for crossover trials. 2021.
DISCUSSION
The neonatal airway is smaller than that of adults. The neonatal tongue and occiput are larger, the larynx is more cephalad, and the epiglottis hangs lower over the airway [20]. Neonates have a higher oxygen consumption and lower oxygen reserves than adult patients [20]. These factors combined can make neonates harder to intubate and more likely to decompensate during intubation attempts, compared with adults [21]. It is important for clinicians to learn how to intubate this patient age group to minimize adverse events associated with unsuccessful or prolonged intubation attempts.
In the clinical setting, there are limited opportunities to develop skill in intubation because of an increased use of noninvasive ventilation, increasing numbers of learners requiring opportunities to perform this skill, and varying levels of patient acuity [3, 6, 7]. Thus, it is important to optimize potential learning opportunities. Using VL provides both the learner and supervisor with the intubation view presenting the opportunity for real-time coaching and feedback during intubation attempts, and may support attainment of competency with fewer attempts [7].
The use of VL during neonatal intubation as a teaching tool led to significantly higher intubation success rates when compared with DL. VL allows both supervisors and learners to view the airway and for the supervisor to provide immediate feedback based on what they see. Moussa [6] reported that almost 50% of all failed attempts within the DL group were from difficulties identifying and visualizing the glottis. The authors reported that with VL, the supervisor was able to recognize and correct these problems with visualization. Two studies blocked learners’ views of the video monitor to force them to develop DL skills, while providing their supervisor real-time access to the video for coaching purposes [7, 10]. Both studies concluded that this improved DL intubation success rates and suggested that VL can be used to teach DL skills.
Intubating with a video laryngoscope also provides an opportunity for learners to view recordings of previous intubation attempts. O’Shea et al. [7] incorporated debriefing in their study and suggest that this may have contributed to the learners’ development of skill. As this was the only study comparing VL to DL as a teaching tool that used debriefing post-intubation, and the impact of this debriefing was not evaluated, it is not clear what impact debriefing may have had.
Saran et al. [20] included older infants (up to 6 months) in their study and excluded any pre-term babies, whereas the other studies included in this review limited intubations to preterm and term neonates. The authors of that study reported an overall increased success rate when VL was used as the teaching tool when intubating larger infants. The inclusion of older, larger infants may have impacted results, but as the impact of infant age and size were not evaluated, it is unclear what impact these may have had.
Strengths
To the authors’ knowledge, this is the first systematic review synthesizing information on the use of VL compared with DL as a teaching tool for neonatal intubation. This review included RCTs with low risk of bias.
Limitations and future research
The present study has some limitations. Few studies met the inclusion criteria. Although the studies were of high quality, sample sizes were small and participants were from medical residencies, not from other professions where intubation is a required competency (eg, respiratory therapy, paramedicine) and results may not be generalizable across professions. Furthermore, this review does not investigate other outcomes associated with VL compared with DL (eg, time to first intubation, adverse events) therefore additional research is warranted to determine if VL is superior to DL with respect to these outcomes.
Three studies included in this review excluded patients with airway anomalies [6, 7, 20] and one study only allowed experienced residents to intubate infants weighing less than 750 g [6]. It is not clear if the results of this review would also hold true when applied to difficult airways. The use of VL as a teaching tool when intubating stable neonatal patients with difficult airways warrants further investigation.
Three studies defined an intubation attempt as the insertion of the laryngoscope blade into the mouth [6, 7, 10] and one study did not provide a definition [20]. Studies used different definitions of intubation success (Table 1). The use of varying definitions for each intubation attempts and success prevents pooling of data for meta-analysis. Future studies should control for both definitions.
Two studies included in this review used standardized guidance tools or scripts if coaching was required during an intubation attempt [7, 10] and one used debriefing [7]. Inconsistent coaching approaches or coaches’ intubation experience could impact learner success [7]. Although it seems that standardized coaching methods could be beneficial teaching tools, further investigation into how each strategy might impact the learning experience in the context of neonatal intubation is warranted.
Only one study considered transfer of skill (from VL to DL) [6] but did so within a limited time frame (exact duration not provided). Future studies should examine whether the improved success rate associated with the use of VL as a teaching tool is maintained over time.
No study included in this review considered retention of skill beyond the clinical rotation. Future studies should consider whether the use of VL as a teaching tool leads to retention of intubation competence.
A limiting factor to the applicability of the results to this review is the cost of VL systems compared with DL (both equipment purchases and processing between patients). These systems may also not be as readily available as DL across training locations [20]. Blades sizes indicated for infants less than 1 kg (00) are not available in all VL systems [10], which limits the use of VL to larger infants.
CONCLUSION
The use of VL as a teaching tool during neonatal intubation led to significantly higher intubation success rates compared with the use of DL. VL can also be used to improve intubation success when teaching DL skills by turning the video monitor away from the learner and allowing the instructor to provide real-time feedback. Its use has the potential to enhance the development of learners’ skills where access to neonatal intubations can be limited. For future studies, it is important to standardize the coaching styles used by supervisors. Future studies should also incorporate learners from other health care fields where intubation is part of the scope of practice (eg, respiratory therapy).
Acknowledgments
The authors would like to acknowledge Meaghan Mamye for her contribution in reviewing this review and Dr Robert Gilbert for his guidance and support and for his contribution in reviewing this review.
Footnotes
Supplementary materials are available at https://www.cjrt.ca/wp-con-tent/uploads/Supplement-cjrt-2022-056.docx.
Supplementary materials are available at https://www.cjrt.ca/wp-con-tent/uploads/Supplement-cjrt-2022-056.docx.
DISCLOSURES
Contributors
JM conceptualized this review as a course requirement for HSCE 4220 (Critical Research Appraisal and Practice, Dalhousie University). Subsequent to this, both authors contributed equally to all parts of this review.
Funding
The present study did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Competing interests
All authors have completed the ICMJE uniform disclosure form at www.icmje.org/coi_disclosure.pdf and declare: no financial relationships with any organizations that might have an interest in the submitted work in the previous 3 years; no other relationships or activities that could appear to have influenced the submitted work.
Ethical approval
Ethical requirement of Research Ethics Board approval for this project was formally waived by the institution.
REFERENCES
- 1.Beltempo M, Shah P, Yoon EW, Chan P, Balachandran N. Canadian Neonatal Network Annual Report. 2020. <http://www.canadianneonatalnetwork.org/portal/Portals/0/2020%20CNN%20report_Oct%201%20Final.pdf> (Accessed September 6, 2022). [Google Scholar]
- 2.Sawyer T, Foglia E, Hatch LD, et al. Improving neonatal intubation safety: A journey of a thousand miles. J Neonatal Perinatal Med 2017;10(2):125–31. 10.3233/NPM-171686 [DOI] [PubMed] [Google Scholar]
- 3.Lingappan K, Arnold JL, Fernandes CJ, Pammi M. Videolaryngoscopy versus direct laryngoscopy for tracheal intubation in neonates. Cochrane Database Syst Rev 2018;6(6):CD009975. 10.1002/14651858.CD009975.pub3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Soghier LM, Walsh HA, Goldman EF, Fratantoni KR. Simulation for neonatal endotracheal intubation training: How different is it from clinical practice? Simul Healthc 2021;17(1):e83–e90. 10.1097/SIH.0000000000000551 [DOI] [PubMed] [Google Scholar]
- 5.Assaad MA, Lachance C, Moussa A. Learning neonatal intubation using the videolaryngoscope: A randomized trial on mannequins. Simul Healthc 2016;11(3):190–3. 10.1097/SIH.0000000000000141 [DOI] [PubMed] [Google Scholar]
- 6.Moussa A, Luangxay Y, Tremblay S, et al. Videolaryngoscope for teaching neonatal endotracheal intubation: A randomized controlled trial. Pediatrics 2016;137(3):e20152156. 10.1542/peds.2015-2156 [DOI] [PubMed] [Google Scholar]
- 7.O’Shea JE, Thio M, Kamlin CO, et al. Videolaryngoscopy to teach neonatal intubation: A randomized trial. Pediatrics 2015;136(5):912–9. 10.1542/peds.2015-1028 [DOI] [PubMed] [Google Scholar]
- 8.Zhou M, Xi X, Li M, et al. Video laryngoscopy improves the success of neonatal tracheal intubation for novices but not for experienced medical staff. Front Pediatr 2020;8:445. 10.3389/fped.2020.00445 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Klabusayová E, Klučka J, Kosinová M, et al. Videolaryngoscopy vs. direct laryngoscopy for elective airway management in paediatric anaesthesia: A prospective randomised controlled trial. Eur J Anaesthesiol 2021;38(11):1187–93. 10.1097/EJA.0000000000001595 [DOI] [PubMed] [Google Scholar]
- 10.Volz S, Stevens TP, Dadiz R. A randomized controlled trial: Does coaching using video during direct laryngoscopy improve residents’ success in neonatal intubations? J Perinatol 2018;38(8):1074–80. 10.1038/s41372-018-0134-7 [DOI] [PubMed] [Google Scholar]
- 11.Hansel J, Rogers AM, Lewis SR, Cook TM, Smith AF. Videolaryngoscopy versus direct laryngoscopy for adults undergoing tracheal intubation. Cochrane Database Syst Rev 2022;4(4):CD011136. 10.1002/14651858.CD011136.pub3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Howard-Quijano KJ, Huang YM, Matevosian R, Kaplan MB, Steadman RH. Video-assisted instruction improves the success rate for tracheal intubation by novices. Br J Anaesth 2008;101(4):568–72. 10.1093/bja/aen211 [DOI] [PubMed] [Google Scholar]
- 13.Abdelgadir IS, Phillips RS, Singh D, Moncreiff MP, Lumsden JL. Videolaryngoscopy versus direct laryngoscopy for tracheal intubation in children (excluding neonates). Cochrane Database Syst Rev 2017;5(5):CD011413. 10.1002/14651858.CD011413.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021;372:n71. 10.1136/bmj.n71 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.US National Library of Medicine . <https://clinicaltrials.gov/> (Accessed on November 1, 2021). [DOI] [PubMed]
- 16.Johnston LC, Chen R, Whitfill TM, Bruno CJ, Levit OL, Auerbach MA. Do you see what I see? A randomised pilot study to evaluate the effectiveness and efficiency of simulation-based training with videolaryngoscopy for neonatal intubation. BMJ Simul Technol Enhanc Learn 2015;1(1): 12–8. 10.1136/bmjstel-2015-000031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.van Schuppen H, Wojciechowicz K, Hollmann MW, Preckel B. Tracheal intubation during advanced life support using direct laryngoscopy versus Glidescope® videolaryngoscopy by clinicians with limited intubation experience: A systematic review and meta-analysis. J Clin Med 2022; 11(21):6291. 10.3390/jcm11216291 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sterne JAC, Savović J, Page MJ, et al. RoB 2: A revised tool for assessing risk of bias in randomised trials. BMJ 2019;366:l4898. 10.1136/bmj.l4898 [DOI] [PubMed] [Google Scholar]
- 19.Higgins J, Li T, Altman D, Curtin F, Senn S. Revised Cochrane risk of bias tool for randomized trials (RoB 2) Additional considerations for crossover trials. 2021. <https://www.riskofbias.info/welcome/rob-2-0-tool/rob-2-for-crossover-trials> (Accessed January 6, 2022). [Google Scholar]
- 20.Saran A, Dave NM, Karnik PP. Efficacy and safety of videolaryngoscopy-guided verbal feedback to teach neonatal and infant intubation. A prospective randomised cross over study. Indian J Anaesth 2019;63(10):791–6. 10.4103/ija.IJA_823_18 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Page NE, Giehl M, Luke S. Intubation complications in the critically ill child. AACN Clin Issues 1998;9:25–35. 10.1097/00044067-199802000-00003 [DOI] [PubMed] [Google Scholar]