Abstract
Although ADHD and negative parenting are established predictors of youth outcomes, their independent and interactive effects on youth social functioning remain unclear. We tested childhood ADHD symptoms and negative parenting as independent and interactive predictors of prospective change in social problems across a four-year follow-up. At baseline, families of 221 (33% female) children with (n = 94) and without ADHD were rigorously assessed including observed positive and negative parenting behavior, youth ADHD symptoms, as well as multi-informant ratings of youth social problems at multiple occasions. Based on multiple regression with robust standard errors and full-information maximum likelihood procedures to address missing data, ADHD symptoms positively predicted social problems, even with control of observed parenting behavior, child age and sex, oppositional defiant disorder symptoms, and baseline social problems. Additionally, a child ADHD symptoms x negative parenting interaction uniquely predicted separate parent- and teacher-rated social problems where ADHD symptoms positively predicted social problems exclusively in the context of high (+1SD) and very high (+2 SD) negative parenting, respectively. When ADHD was separated into distinct dimensions (i.e., inattention, hyperactivity), an interaction between inattention symptoms and negative parenting approached significance such that inattention symptoms positively predicted parent-rated social problems in the context of high negative parenting. We discuss the interaction between parenting and ADHD symptoms in predictions of youth social problems and implications for intervention.
Keywords: ADHD, Attention-deficit/hyperactivity disorder, Negative parenting, Social problems
Consisting of key constructs such as social skills, social status, and friendship (Rose-Krasnor 1997), individual differences in youth social functioning uniquely predict important outcomes including academic achievement, substance use, and depression (Fleming et al. 2005; Greene et al. 1999; Katz et al. 2011; Malecki and Elliot 2002). Beyond these behavioural and emotional outcomes, social functioning is related to physical health as well: social isolation and loneliness positively predict inflammation (Eisenberger et al. 2017), which negatively affects mood (Irwin and Miller 2007) and cardiovascular functioning (Libby 2006). Thus, to promote positive physical and mental health outcomes, identifying determinants of youth social functioning and/or social difficulties will elucidate logical targets for intervention.
Poor social functioning is a hallmark feature of youth with attention-deficit/hyperactivity disorder (ADHD; see Nijmeijer et-al.2008 and Nixon 2001 for reviews), including peer rejection, social skills deficits, and fewer friendships relative to their typically developing peers (Hoza et al. 2005b; Hoza 2007; Humphreys et al. 2016). Critically, these social problems are highly treatment resistant (Hoza et al. 2005a) and persist across development, even when ADHD symptoms remit (Lee et al. 2008). For example, adolescents with relative elevations in symptoms of ADHD during childhood experienced fewer friendships and greater rejection relative to comparison youth (Bagwell et al. 2001). Although ADHD is diversely associated with multiple indicators of social dysfunction, the literature consists largely of cross-sectional studies, especially without clarification of potential moderators to identify critical subgroups of youth vulnerable to the development of social difficulties, thereby hampering efforts to identify those most in need of intervention.
ADHD represents the extreme end of a naturally occurring continuum (Larsson et al. 2012; Lubke et al. 2009). Whereas categorically-defined ADHD has shown considerable diagnostic instability over time and may mask important within group heterogeneity, continuous approaches to ADHD have demonstrated enhanced predictive validity across multiple measures of impairment relative to nominal approaches (e.g., Lahey and Willcutt 2010). Additionally, given that ADHD consists of separable inattention and hyperactivity-impulsivity dimensions, examining their potentially unique patterns of association with social functioning is strongly indicated. For example, in the context of social interactions, hyperactivity may manifest as social intrusion or verbal/physical aggression whereas inattention may contribute to distractibility (Nijmeijer et al. 2008). Using ADHD subtypes, children with ADHD-inattentive type made fewer responses and had worse memory for conversations relative to ADHD-combined type or comparison youth in the context of a novel chat room task (Mikami et al. 2007). In contrast, relative to other subgroups, youth with ADHD-combined type (i.e., elevated inattentive and hyperactive symptoms) made more frequent hostile remarks on the same measure (Mikami et al. 2007) and were more aggressive (Wheeler Maedgen and Carlson 2000) than children with the predominantly inattentive symptoms. Dimensionally, ADHD symptoms were positively related to peer dislike in a community sample (Diamantopoulou et al. 2005). With additional control of IQ and executive functioning, ADHD symptoms inversely predicted social preference and positively predicted aggression in school-aged children (Diamantopoulou et al. 2007). Because different configurations of ADHD, based on the total number of symptoms and diagnostic subtypes, are associated with diverse measures of social functioning, future studies must attend to these issues to improve specificity of predictive models across development.
Like ADHD, parenting behavior is central to the development of youth social functioning. Whereas positive parenting is related to social adjustment and prosocial behaviors in children (Koblinsky et al. 2006), exposure to extreme negative parenting (e.g., abuse, neglect, hostility) predicts social problems such as bullying and/or victimization (Lereya et al. 2013). Even normative levels of negative parenting (e.g., criticism, inconsistent discipline) are related to social dimensions (e.g., aggression, social preference) in expected directions in children with and without ADHD (Bank, L., et al. 2004; Brown and Bakken 2011; Kaiser et al. 2011; Kawabata et al. 2011). Moreover, intervention-induced reductions in negative parenting, coupled with increased positive parenting behaviors, predicted improved youth social competence (Webster-Stratton et al. 2001), suggesting the plausible causal role of parenting in youth social functioning.
Predictions of social functioning from parenting behavior may consist of multiple mediating pathways. Attachment and social learning theories posit modeling as a central mechanism through which children apply social behaviors observed in the family environment to peer interactions (Brown and Bakken 2011). Parenting behavior can also influence the development of emotion regulation and cognitive processes that are essential to social functioning (Morris et al. 2017). Additionally, parenting may affect social information processing and children’s perceptions of their peers: children who experienced more positive parenting were less likely to make negative attributions of their peers; fewer negative attributions, in turn, predicted greater peer acceptance (Rah and Parke 2008). Although the pathways through which parenting influences social behavior may differ across positive and negative parenting dimensions, exposure to negative parenting behavior is a strong candidate risk factor for offspring social dysfunction. Thus, children with symptoms of ADHD, who are susceptible to poor social functioning, may be particularly vulnerable to social difficulties in the context of negative parenting behavior. Despite distinct literatures investigating symptoms of ADHD and negative parenting with respect to social outcomes, few studies have evaluated their independent and interactive predictions of youth social problems.
Symptoms of childhood ADHD plausibly interact with parenting behavior to predict individual differences in youth social problems. First, families of children with ADHD are characterized by elevated conflict and reduced parental sensitivity/warmth (Keown 2012; Pressman et al. 2006). Second, considering its significant heritability (Faraone and Larsson 2018), biological parents of youth with ADHD are vulnerable to significant ADHD symptoms themselves, which predict both self-reported and observed negative parenting behavior (Harvey et al. 2003; Mokrova et al. 2010). Moreover, youth ADHD symptoms are reliably associated with parent stress (Theule et al. 2013), which similarly elicits negative parenting (Crnic et al. 2005). Finally, because authoritative parenting beliefs were more strongly associated with peer rejection in 6–12-year-old boys diagnosed with ADHD than controls (Hinshaw et al. 1997), social outcomes in youth with ADHD may be particularly sensitive to the influence of parenting behavior. Overall, whereas positive parenting behavior may promote positive social development, despite youth ADHD symptom levels, negative parenting behavior may exacerbate social problems subsequent to symptoms of youth ADHD, although few studies have tested this hypothesis directly. In three separate models, Kaiser et al. (2011) found that an ADHD x negative parenting interaction was unrelated to youth social dysfunction; rather, self-reported parenting behavior mediated the relationship between ADHD and child aggression and social skills. However, because cross-sectional designs lend poor resolution to testing interactions (McClelland and Judd 1993), evaluation of youth ADHD x parenting behavior interactions should be prioritized in repeated measures designs. Further, cross-sectional designs limit interpretation of the direction of the effects as children’s social difficulties and ADHD could elicit negative parenting behavior, highlighting the importance of temporally-ordered strategies to test hypothesized associations. Finally, the current study employs objectively-coded observations of parenting behavior, which increments predictions beyond self-report and mitigates important biases (e.g., desirability effect) associated with self-report data (Locke and Prinz 2002).
The current study had two aims: 1) to test the independent association of youth ADHD symptoms and observed negative parenting with separate parent and teacher ratings of social problems in youth followed prospectively for 4 years and 2) to test their interaction with control of child age and sex as well as baseline social problems. Follow-up exploratory analyses were conducted separately with inattention and hyperactivity dimensions of ADHD, given their differential association with social functioning (Mikami et al. 2007; Wheeler Maedgen and Carlson 2000). In all models, we controlled for baseline oppositional defiant disorder (ODD) symptoms, based on the disorder’s significant covariation with social behavior (Greene et al. 2002) and ADHD (Jensen et al. 1997). Finally, we controlled for baseline observed positive parenting as positive and negative parenting are differentially associated with child outcomes (Caron et al. 2006). We hypothesized that ADHD symptoms and negative parenting would independently predict escalating social problems. Secondarily, we hypothesized that the ADHD symptoms x negative parenting interaction would significantly predict multi-informant rated social problems for youth exposed to higher levels of negative parenting. Finally, we tested an exploratory three-way interaction among inattention, hyperactivity, and negative parenting to evaluate whether combinations of these symptom dimensions predicted social problems. Given the exploratory nature of this final aim, we did not specify a priori hypotheses.
Method
Participants
The present sample consisted of 221 youth with (n = 94) and without ADHD (n = 124) and their families. Three participants were missing ADHD diagnostic data from the Diagnostic Interview Schedule for Children (DISC-IV) Parent Edition (Shaffer et al. 2000), the primary diagnostic tool to ascertain ADHD status. At baseline (i.e., Wave 1) participating children ranged in age from 5 to 10 years old and at follow-up, approximately 4 years later (i.e., Wave 3), their ages ranged from 9 to 15 years old (Table 1). Ethnically diverse youth (51.6% Caucasian; 9.1% African American; 12.2% Hispanic; 3.6% Asian; 23.5% Mixed/Other/Unknown) and their families were recruited from a large metropolitan city in the Western U.S. To recruit families, flyers were mailed to local schools, pediatric offices, and clinical service providers. Additionally, presentations were made to ADHD self-help groups and referrals from mental health clinics were gathered. For the current study, inclusion criteria were English fluency and living with a biological caregiver at least halftime. Participants with an IQ below 70, a history of seizure autism spectrum, or other neurological condition were excluded.
Table 1.
Descriptive statistics of demographics and key variables
| Variable | M (SD) or % of Sample | Range | n |
|---|---|---|---|
|
| |||
| Wave 1 Age | 7.42 (1.12) | 5–10 | 221 |
| Wave 3 Age | 12.10 (1.32) | 9–15 | 174 |
| Sex (% Male) | 67.42 | - | 221 |
| Race-Ethnicity | |||
| Caucasian | 51.58 | - | 114 |
| Hispanic | 12.22 | - | 27 |
| African American | 9.05 | - | 20 |
| Asian | 3.62 | - | 8 |
| Mixed/Other/Unknown | 23.53 | - | 52 |
| Wave 1 ODD Symptoms (DBD) | 1.91 (2.42) | 0–8 | 215 |
| Wave 1 ADHD Symptoms | |||
| Total Symptoms (DBD) | 8.15 (5.91) | 0–18 | 215 |
| Inattention Symptoms (DBD) | 4.51 (3.35) | 0–9 | 215 |
| Hyperactivity Symptoms (DBD) | 3.63 (3.20) | 0–9 | 214 |
| Wave 1 Observed Parenting | |||
| Positive Parenting (Praise) | 0.52 (.46) | 0–2.67 | 173 |
| Negative Parenting (Negative Talk) | 0.39 (.37) | 0–2.28 | 173 |
| Wave 1 Social Problems | |||
| Parent-Rated Social Problems (CBCL) | 3.63 (3.49) | 0–16 | 219 |
| Teacher-Rated Social Problems (TRF) | 3.26 (3.87) | 0–18 | 151 |
| Wave 3 Social Problems | |||
| Parent-Rated Social Problems (CBCL) | 2.69 (2.97) | 0–17 | 156 |
| Teacher-Rated Social Problems (TRF) | 1.77 (3.14) | 0–12 | 66 |
ODD Oppositional Defiant Disorder, DBD Disruptive Behavior Disorders Rating Scale, ADHD Attention-Deficit/Hyperactivity Disorder, CBCL Child Behavior Checklist, TRF Teacher Report Form
Procedures
Following an initial phone screen, eligible families who elected to participate were mailed rating scales to assess child functioning. With consent from families, teachers were mailed parallel forms to gather additional information about child functioning in the school setting. Families also completed a laboratory-based assessment conducted by graduate students in clinical psychology or B.A. level staff blind to youth diagnostic status at baseline. However, given the nature of the assessments, staff working with families could likely discern diagnostic status during the study visit. After informed consent and youth assent were obtained, parents completed a structured diagnostic interview (i.e., DISC-IV; see measure section for more detail) and rating scales assessing child functioning across social, emotional, and academic domains. Youth concurrently completed standardized tests examining academic achievement and cognitive functioning as well as interviews evaluating social-emotional functioning. Participating families were invited to complete laboratory follow-up assessments at Waves 2 and 3, which took place about two and 4 years later, respectively. Follow-up assessments were similar to those at Wave 1 in terms of key constructs and methods. For the present study, we examined baseline (i.e., Wave 1) predictors and Wave 3 social outcomes. Approximately 80% of the initial Wave 1 sample consisting of 221 participants was reevaluated at Wave 3 (n = 175). To incentivize continued participation, children and families were paid at a higher rate at each Wave of data collection. Perhaps most importantly, across the life of the study, families were provided with detailed clinical assessment summaries wherein key diagnostic, cognitive, academic, and socio-emotional domains of functioning were described. Moreover, specific referrals, treatment recommendations and principles, etc. were included in these written reports.
Notably, Wave 3 participants had significantly lower Wave 1 observed negative parenting [t(171) = 3.06, p < 0.01] and Wave 1 teacher-rated social problems [t(146) = 2.23, p = 0.02] compared to youth who did not participate at Wave 3. No other significant differences in child demographic and clinical variables (i.e., age, sex, and ethnicity, ADHD status or symptoms, ODD symptoms, Wave 1 parent-rated social problems) were observed. Sex of the participating parent did not differ either. The University of California, Los Angeles Institutional Review Board approved all study procedures.
Measures
Diagnostic Interview Schedule for Children (DISC-IV)
Participating parents completed the ADHD module of the DISC-IV, Parent Edition (Shaffer et al. 2000). The DISC-IV is a computer-assisted, fully structured interview with strong psychometric properties, including a test–retest reliability of r = 0.79 after 1 year as well as an internal consistency of 0.84 for symptoms and 0.77 for criterion in a large community sample (see Shaffer et al. 2000). The ADHD module assesses for child symptoms based on DSM-IV criteria as well as impairment across multiple settings. The measure was used to determine ADHD diagnostic status.
Disruptive Behavior Disorder Rating Scale (DBD)
At Wave 1, parents and teachers completed the DBD, which examines DSM–IV ADHD symptoms. Response options on the DBD range from 0 = not at all to 3 = very much (Pelham Jr. et al. 1992). The values of 0 and 1 are recoded into 0s, indicating the absence of the symptom; whereas values of 2 and 3 are recoded into 1s, indicating the presence of the symptom. The measure is highly valid for the assessment of ADHD and ODD in school-age children (Owens and Hoza 2003). We combined parent and teacher data, at the item level, using an OR algorithm. That is, if a symptom was endorsed by a parent or teacher as “very much” or “pretty much,” that symptom was coded positively. The total number of symptoms ranged from 0 to 18, paralleling the number of DSM-IVADHD symptoms. If the symptom was missing for one of the informants, we used the data from the single informant. Combining data across informants, without weighting particular informants or symptoms, accurately diagnoses as well or better than more complex approaches (Piacentini et al. 1992) and is valid in the diagnosis and assessment of ADHD (Lahey et al. 1998). Finally, the dimensional OR algorithm was shown to be a better predictor of internalizing and externalizing symptoms as well as social problems relative to an AND algorithm or single informant report (Shemmassian and Lee 2016). The approach of combining parent and teacher DBD ratings has the added benefit of reducing the number of statistical tests. In our sample, total youth ADHD symptoms demonstrated excellent internal consistency (α = 0.93). Likewise, we summed the 9 inattention and 9 hyperactivity symptoms yielding dimensional inattention (α = 0.90) and hyperactivity (α = 0.89) scores. Finally, the total the Wave 1 ODD score (α = 0.87) from the DBD was controlled in all analyses.
Observed Parenting Behavior
At Wave 1, families completed the Dyadic Parent Child Interaction Coding System (DPICS; Eyberg et al. 2005). Parent and child behaviors were coded continuously. Subsequently, composites were created (Chronis-Tuscano et al. 2008; Eyberg et al. 2001). Negative parenting consisted of hostile or critical comments, negative commands, and condescending remarks. Positive parenting was estimated through counts of parental praise, including positive attributions for a child’s behavior. For each category, counts were summed and corrected for variation in the length of the interaction task. All coders completed extensive training to ensure adherence to the DPICS protocol and for reliability. The intraclass correlations for each parenting behavior variable exceeded 0.70. We used negative total as an index of negative parenting and controlled for praise (i.e., positive parenting). Behavioral counts were then divided by the total number of minutes of the interaction to account for slight variation in the total time. Previously, these positive and negative dimensions of parenting behavior differentiated children with behavior problems from healthy controls across multiple studies (Lee et al. 2010; Chronis et al., 2008) and were sensitive to change following parenting inventions (Schuhmann et al. 1998).
Child Behavior Checklist/Teacher Report Form (CBCL/TRF)
At all Waves, parents and teachers completed the CBCL and TRF, respectively (Achenbach and Rescorla 2001). Each of the 113 items were rated from 0 = not true to 2 = very true/often true. The manual reports the reliability of both the CBCL and TRF Social Problems Subscales to be good (α = 0.82; Achenbach and Rescorla 2001). Additionally, the test-retest reliability for the both the parent (r = 0.90) and teacher (r = 0.95) Social Problems subscales is very high (Achenbach and Rescorla 2001). For the present study, we used the Wave 3 CBCL and TRF Social Problems narrowband raw scores as the primary outcomes. Additionally, we controlled for Wave 1 CBCL Social Problems raw score in predictions of Wave 3 CBCL Social Problems. A parallel approach (i.e., control of Wave 1 TRF Social Problems) was used in predictions of Wave 3 teacher-rated Social Problems on the TRF.
Data Analytic Procedures
We tested the independent and interactive prospective association of baseline ADHD symptoms and observed negative parenting on multi-informant ratings of youth Social Problems four to six years later (i.e., Wave 3). Further we examined the independent and interactive predictions of separate dimensions of ADHD (i.e., inattention, hyperactivity) and negative parenting on Wave 3 Social Problems. Seventy percent of Wave 3 TRF Social Problems and 29% of Wave 3 CBCL Social Problems were missing. We implemented full information maximum likelihood (FIML) procedures in Stata 14.2 (i.e., method mlmv) with robust standard errors to address non-normality and to accommodate missing data. FIML, a state-of-the-art missing data technique, enhances the accuracy and power of analyses relative to other approaches and is preferred to multiple imputation when testing interactions (Enders 2010; Schafer and Graham 2002). Moreover, this approach performs well even in cases of extreme missingness (Schlomer et al. 2010). As required for the use of FIML (Li 2013), the sample met the assumption of missing at random (MAR) based on the covariate-dependent missingness extension of Little’s test of MCAR. For ADHD total symptoms, the test was non-significant for parent- [χ2(81) = 67.55, p = 0.86] and teacher[χ2(96) = 106.46, p = .22] rated Social Problems at Wave 3 when including fully observed covariates (i.e., child age and sex), supporting the use of FIML. With respect to the separate dimensions of inattention and hyperactivity, covariate-dependent missingness extension of Little’s test of MCAR was also non-significant for parent- [χ2(111) = 77.15, p = 0.99] and teacher-rated Social Problems [χ2(129) = 128.11, p = 0.51]. Although the data meets the assumption of MAR and the mechanism of missingness has been proposed to have a greater impact on estimates than the proportion of missing data (Tabachnick and Fidell 2012), the teacher analyses in the present study should be interpreted cautiously given the high percentage of missing teacher outcome data.
We employed multiple regression to evaluate prospective predictions of parent- and teacher-rated youth Social Problems from baseline ADHD symptoms and observed negative parenting. Following entry of covariates and all main effects, we entered the ADHD x negative parenting interaction term; if significant, we evaluated the simple slopes. To improve specificity of predictions, we conducted exploratory analyses testing the independent and interactive association of Wave 1 inattention, hyperactivity, and negative parenting on Wave 3 parent- and teacher-rated Social Problems. To examine the interactions, we entered the covariates and main effects followed by these terms: 1) inattention x negative parenting, 2) hyperactivity x negative parenting, 3) inattention x hyperactivity, and 4) inattention x hyperactivity x negative parenting.
We considered multiple statistical approaches before employing regressions. First, given the use of separate parent and teacher informants, we calculated the alpha level at 0.025 (i.e., 0.05/2). Given that this study utilized the same measure across multiple informants, the use of formal Bonferroni correction was contraindicated given its violation of the assumption of independence. Overall, an alpha of 0.025 balances Type I and Type II error (Perneger 1998) without being overly punitive in the context of interactions, which are difficult to detect (McClelland and Judd 1993). We also median-centered all predictors (Kraemer and Blasey 2004) to reduce multicollinearity. Power analyses using G*Power 3.1 software (Faul et al. 2007) were implemented to determine the minimum sample size needed to detect a small effect (i.e., 0.2) at α = 0.025 with seven to 12 predictors (the maximum number of predictors in any model within the current study). The program indicated that a sample size of 158 would be needed for the present study in models with 12 predictors. Therefore, our sample of 221 youth was sufficiently large to detect a small effect at an alpha of 0.025. Preliminary analyses (see below for details) included calculations of variance inflation factors to evaluate multicollinearity.
Results
Correlations
A correlation matrix of all study variables is provided in Table 2. Child age and sex (male = 1) were unrelated to Social Problems in early adolescence. The positive association between observed negative parenting and Wave 3 parent- and teacher -rated Social Problems approached significance (p = 0.05). All ADHD variables (i.e., total, inattention, hyperactivity) were positively correlated with Wave 3 Social Problems across informants. The ODD symptoms variable was positively correlated with parent-reported Social Problems at Wave 3, but this association only approached significance for teacher-rated Social Problems. As expected, Wave 1 and Wave 3 Social Problems were significantly related across parent and teacher report. Although the correlation between Wave 3 parent- and teacher-rated Social Problems approached significance, the fact that it did not meet the significance threshold is unsurprising as informant discrepancies of social functioning are commonly observed (Gresham et al. 2010; Renk 2005).
Table 2.
Correlations among covariates, ADHD symptoms, negative parenting, and social problems
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | |
|---|---|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||||
| 1. Age | – | ||||||||||
| 2. Sex | −0.06 | – | |||||||||
| 3. Positive Parenting (PCI) | −0.19* | 0.11 | – | ||||||||
| 4. Wave 1 CBCL Social Problems | 0.10 | 0.03 | 0.01 | – | |||||||
| 5. Wave 1 TRF Social Problems | −0.07 | 0.11 | −0.02 | 0.42* | – | ||||||
| 6. ODD Symptoms (DBD) | −0.05 | 0.12 | 0.02 | 0.52* | 0.54* | – | |||||
| 7. Negative Parenting (PCI) | −0.08 | 0.06 | −0.02 | 0.05 | 0.15 | 0.10 | – | ||||
| 8. ADHD Total Symptoms (DBD) | −0.10 | 0.16* | 0.11 | 0.52* | 0.49* | 0.63* | 0.23* | – | |||
| 9. ADHD Inattention Symptoms (DBD) | −0.01 | 0.10 | 0.09 | 0.58* | 0.34* | 0.46* | 0.20* | 0.91* | – | ||
| 10. ADHD Hyperactivity Symptoms (DBD) | −0.17* | 0.19* | 0.11 | 0.45* | 0.53* | 0.67* | 0.21* | 0.90* | 0.63* | – | |
| 11. Wave 3 CBCL Social Problems | −0.02 | −0.08 | 0.00 | 0.61* | 0.32* | 0.28* | 0.17 | 0.44* | 0.40* | 0.39* | – |
| 12. Wave 3 TRF Social Problems | 0.21 | 0.14 | 0.10 | 0.37* | 0.48* | 0.26† | 0.27 | 0.43* | 0.41* | 0.39* | 0.26† |
PCI Parent-Child Interaction, CBCL Child Behavior Checklist, TRF Teacher Report Form, ODD Oppositional Defiant Disorder, DBD Disruptive Behavior Disorders Rating Scale, ADHD Attention-Deficit/Hyperactivity Disorder
p ≤ 0.025
p ≤ 0.05
Preliminary Analyses
We calculated the variance inflation factor values prior to running the regressions. Following expert recommendations (e.g., Kraemer and Blasey 2004), we median centered the predictors to address multicollinearity, which substantially reduced variance inflation factor values. No variance inflation factor exceeded 3.1, which is well-below the standard cutoff of 10 (Hair Jr. et al. 1995).
Wave 3 Parent-Rated Social Problems
ADHD Symptoms and Negative Parenting
Utilizing centered predictors, we tested the association of baseline ADHD symptoms, observed negative parenting, and their interaction as prospective predictors of Wave 3 parent-rated Social Problems controlling for child age and sex, positive parenting, Wave 1 ODD symptoms, and Wave 1 CBCL Social Problems.
Model 1 tested the main effects of ADHD symptoms and negative parenting. Negative parenting at Wave 1 was unrelated to Wave 3 parent-rated Social Problems beyond ADHD symptoms and covariates (b = 0.83, SE = 0.80, p = 0.30; Table 3); however, baseline ADHD symptoms positively predicted parent-reported Wave 3 Social Problems over and above negative parenting and covariates (b = 0.11, SE = 0.04, p = 0.01, beta = 0.21; Table 3), with the standardized regression coefficient reflecting a small effect size base on Cohen’s (1988) guidelines.
Table 3.
Main and interactive effects of ADHD symptoms and negative parenting behavior in predictions of wave 3 parent- and teacher-rated social problems
| Dependent variable | Predictors | Model 1 |
Model 2 |
||||||
|---|---|---|---|---|---|---|---|---|---|
| b | SE | β | p | b | SE | β | p | ||
|
| |||||||||
| Wave 3 Parent-Rated Social Problems (CBCL) | Age | −0.23 | 0.19 | −0.09 | 0.22 | −0.27 | 0.19 | −0.10 | 0.15 |
| Sex | 0.41 | 0.44 | 0.07 | 0.35 | 0.34 | 0.44 | 0.05 | 0.43 | |
| Positive Parenting (PCI) | −0.06 | 0.38 | −0.01 | 0.87 | −0.16 | 0.36 | −0.02 | 0.66 | |
| Wave 1 Parent-Rated Social Problems (CBCL) | 0.47 | 0.10 | 0.56 | <0.001 | 0.47 | 0.10 | 0.56 | <0.001 | |
| ODD (DBD) | −0.18 | 0.11 | −0.15 | 0.10 | −0.19 | 0.11 | −0.16 | 0.08 | |
| Negative Parenting (PCI) | 0.83 | 0.80 | 0.10 | 0.30 | 0.81 | 0.77 | 0.10 | 0.29 | |
| ADHD Symptoms (DBD) | 0.11 | 0.04 | 0.21 | 0.01 | 0.09 | 0.04 | 0.18 | 0.04 | |
| ADHD Symptoms × Negative Parenting | 0.25 | 0.11 | 0.18 | 0.025 | |||||
| Wave 3 Teacher-Rated Social Problems (TRF) | Age | −0.42 | 0.32 | −0.15 | 0.18 | −0.40 | 0.30 | −0.14 | 0.18 |
| Sex | 0.20 | 0.73 | 0.03 | 0.78 | 0.27 | 0.70 | 0.04 | 0.69 | |
| Positive Parenting (PCI) | 0.87 | 0.80 | 0.12 | 0.27 | 0.54 | 0.72 | 0.07 | 0.45 | |
| Wave 1 Teacher-Rated Social Problems (TRF) | 0.39 | 0.24 | 0.48 | 0.10 | 0.36 | 0.25 | 0.42 | 0.14 | |
| ODD (DBD) | −0.03 | 0.27 | −0.03 | 0.90 | −0.04 | 0.23 | −0.03 | 0.87 | |
| Negative Parenting (PBI) | 0.93 | 1.24 | 0.11 | 0.45 | 2.00 | 1.41 | 0.22 | 0.15 | |
| ADHD Symptoms (DBD) | 0.08 | 0.12 | 0.15 | 0.51 | 0.03 | 0.13 | 0.05 | 0.82 | |
| ADHD Symptoms × Negative Parenting | 0.52 | 0.21 | 0.34 | 0.01 | |||||
b unstandardized regression coefficient, SE standard error, β standardized coefficient included to indicate effect size (p-values based on unstandardized regression coefficients), PCI Parent-Child Interaction, CBCL Child Behavior Checklist, ODD Oppositional Defiant Disorder, DBD Disruptive Behavior Disorder Rating Scale, ADHD Attention-Deficit/Hyperactivity Disorder, TRF Teacher Report Form
In Model 2 (Table 3), we entered the ADHD symptoms x negative parenting interaction, which significantly predicted Wave 3 CBCL Social Problems (b = 0.25, SE = 0.11, p = 0.025, beta = 0.18; Table 3). Following established guidelines (Aiken and West 1991), we tested simple slopes at high (+1 SD) and low (−1 SD) levels of observed negative parenting. At high levels of negative parenting, ADHD symptoms positively predicted parent-rated Wave 3 Social Problems (b = 0.21, SE = 0.05, p < 0.001) with rigorous control of child age and sex, positive parenting, Wave 1 ODD symptoms, and Wave 1 CBCL Social Problems (Fig. 1). In contrast, at low levels of negative parenting, ADHD symptoms were unrelated to Wave 3 parent-rated Social Problems (b = 0.02, SE = 0.06, p = 0.70). Overall, ADHD symptoms predicted worse parent-rated Social Problems approximately four years later only in the context of elevated negative parenting during childhood.
Fig. 1.
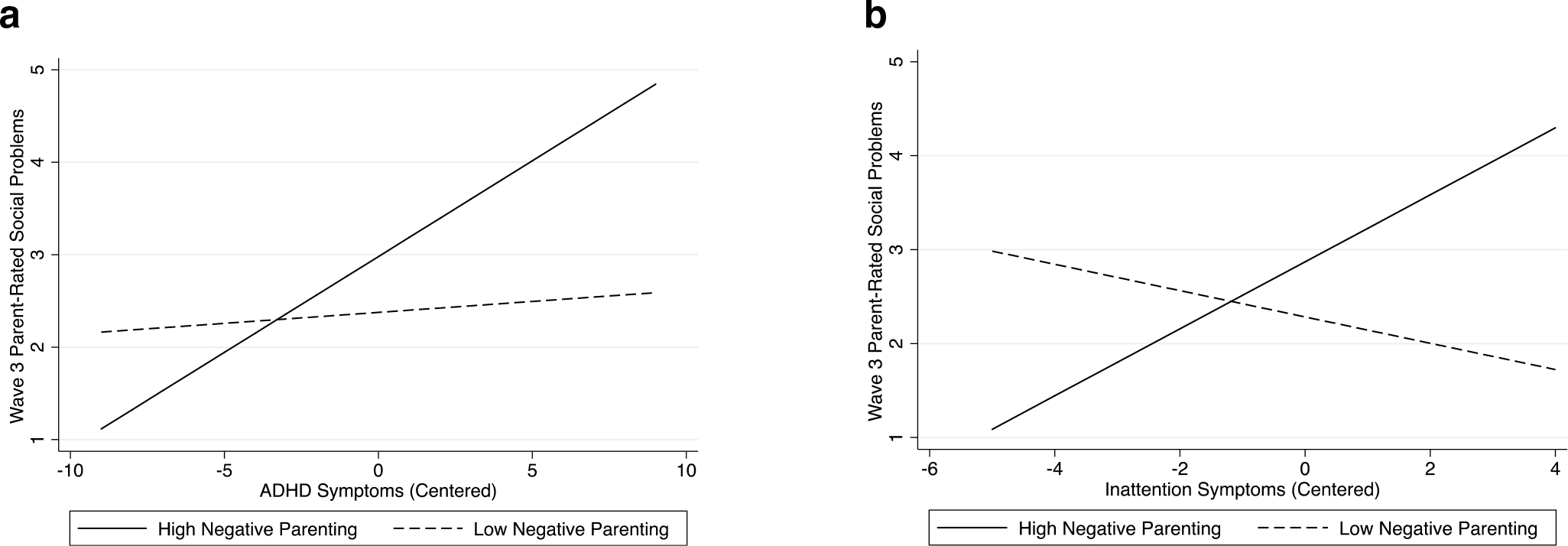
a The interactive effect of total ADHD symptoms and negative parenting on predicted values of Wave 3 parent-rated Social Problems. b The interactive effect of inattention symptoms and negative parenting on predicted values of Wave 3 parent-rated Social Problems. Both graphs hold covariates and other predictors (i.e., hyperactivity symptoms in panel b) at their respective means
Inattention Symptoms, Hyperactivity Symptoms, and Negative Parenting
To improve the specificity of predictions, we explored the association of baseline inattention symptoms, hyperactivity symptoms, observed negative parenting, and their interactions as prospective predictors of parent-rated Social Problems four years later using identical covariates.
In Model 1 (Table 4), with control of child age and sex, positive parenting, as well as baseline ODD symptoms and CBCL Social Problems, neither Wave 1 negative parenting (b = 0.82, SE = 0.80, p = 0.30), inattention symptoms (b = 0.09, SE = 0.06, p = 0.15), nor hyperactivity symptoms (b = 0.13, SE = 0.10, p = 0.16) significantly predicted Wave 3 CBCL Social Problems (see Table 4 for effect sizes).
Table 4.
Main and interactive effects of inattention symptoms, hyperactivity symptoms, and negative parenting behavior in predictions of wave 3 parent- and teacher-rated social problems
| Dependent variable | Predictors | Model 1 |
Model 2 |
Model 3 |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| b | SE | β | p | b | SE | β | p | b | SE | β | p | ||
|
| |||||||||||||
| Wave 3 Parent-Rated Social Problems (CBCL) | Age | −0.22 | 0.20 | −0.09 | 0.25 | −0.27 | 0.18 | −0.10 | 0.14 | −0.24 | 0.18 | −0.09 | 0.19 |
| Sex | 0.42 | 0.44 | 0.07 | 0.34 | 0.30 | 0.42 | 0.05 | 0.47 | 0.25 | 0.42 | 0.04 | 0.56 | |
| Positive Parenting (PCI) | −0.06 | 0.38 | −0.01 | 0.87 | −0.20 | 0.35 | −0.03 | 0.56 | −0.17 | 0.35 | −0.03 | 0.62 | |
| Wave 1 Parent-Rated Social Problems (CBCL) | 0.47 | 0.10 | 0.56 | <0.001 | 0.46 | 0.09 | 0.54 | <0.001 | 0.45 | 0.09 | 0.53 | <0.001 | |
| ODD Symptoms (DBD) | −0.20 | 0.13 | −0.16 | 0.11 | −0.19 | 0.12 | −0.16 | 0.12 | −0.19 | 0.12 | −0.16 | 0.12 | |
| Negative Parenting (PCI) | 0.82 | 0.80 | 0.10 | 0.30 | 0.26 | 0.91 | 0.03 | 0.77 | 0.91 | 0.81 | 0.12 | 0.25 | |
| Inattention Symptoms | 0.09 | 0.06 | 0.10 | 0.15 | 0.01 | 0.06 | 0.01 | 0.87 | 0.04 | 0.06 | 0.04 | 0.55 | |
| Hyperactivity Symptoms | 0.13 | 0.10 | 0.15 | 0.16 | 0.19 | 0.08 | 0.20 | 0.025 | 0.17 | 0.08 | 0.19 | 0.03 | |
| Inattention Symptoms × Negative Parenting | 0.71 | 0.28 | 0.29 | 0.01 | 0.67 | 0.30 | 0.28 | 0.026 | |||||
| Hyperactivity Symptoms × Negative Parenting | −0.28 | 0.27 | −0.13 | 0.29 | −0.28 | 0.30 | −0.12 | 0.34 | |||||
| Inattention Symptoms × Hyperactivity Symptoms | 0.00 | 0.02 | 0.00 | 0.99 | 0.01 | 0.02 | 0.03 | 0.54 | |||||
| Inattention Symptoms × Hyperactivity Symptoms × Negative Parenting | 0.11 | 0.07 | 0.14 | 0.10 | |||||||||
| Wave 3 Teacher-Rated Social Problems (TRF) | Age | −0.54 | 0.31 | −0.19 | 0.08 | −0.38 | 0.27 | −0.11 | 0.15 | ||||
| Sex | 0.23 | 0.72 | 0.03 | 0.75 | 0.67 | 0.66 | 0.08 | 0.30 | |||||
| Positive Parenting (PCI) | 1.01 | 0.85 | 0.14 | 0.23 | 0.81 | 0.73 | 0.09 | 0.27 | |||||
| Wave 1 Teacher-Rated Social Problems (TRF) | 0.43 | 0.24 | 0.52 | 0.07 | 0.57 | 0.22 | 0.56 | 0.01 | |||||
| ODD Symptoms (DBD) | 0.05 | 0.25 | 0.04 | 0.83 | 0.00 | 0.18 | 0.00 | 0.98 | |||||
| Negative Parenting (PCI) | 1.19 | 1.12 | 0.14 | 0.28 | 0.07 | 1.21 | 0.01 | 0.95 | |||||
| Inattention Symptoms | 0.25 | 0.16 | 0.26 | 0.11 | −0.09 | 0.20 | −0.08 | 0.65 | |||||
| Hyperactivity Symptoms | −0.22 | 0.22 | −0.22 | 0.30 | −0.25 | 0.22 | −0.20 | 0.27 | |||||
| Inattention Symptoms × Negative Parenting | 1.05 | 0.47 | 0.32 | 0.025 | |||||||||
| Hyperactivity Symptoms × Negative Parenting | 0.59 | 0.46 | 0.19 | 0.19 | |||||||||
| Inattention Symptoms × Hyperactivity Symptoms | −0.08 | 0.04 | −0.17 | 0.08 | |||||||||
| Inattention Symptoms × Hyperactivity Symptoms × Negative Parenting | 0.49 | 0.11 | 0.49 | <0.001 | |||||||||
b unstandardized regression coefficient, SE standard error, β standardized coefficient included to indicate effect size (p-values based on unstandardized regression coefficients), PCI Parent-Child Interaction, CBCL Child Behavior Checklist, ODD Oppositional Defiant Disorder, DBD Disruptive Behavior Disorder Rating Scale, ADHD Attention-Deficit/Hyperactivity Disorder, TRF Teacher Report Form
Subsequently, we entered four interaction terms (i.e., inattention x negative parenting, hyperactivity x negative parenting, inattention x hyperactivity, inattention x hyperactivity x negative parenting) to test for a three-way interaction among key predictors in Model 2. However, the three-way interaction was nonsignificant with a small effect size (b = 0.11, SE = 0.07, p = 0.10, beta = 0.14; Table 4); therefore, the term was dropped and we tested the remaining three two-way interactions as simultaneous predictors of Wave 3 parent-reported Social Problems.
With inclusion of all two-way interaction terms in Model 3, the inattention symptoms x negative parenting interaction showed a moderate effect size of beta = 0.28 and approached significance in predicting Wave 3 Social Problems (b = 0.67, SE = 0.30, p = 0.026; Table 4). Consistent with the American Statistics Association’s concerns with reducing statistical inference to a single cutoff based on an identified p value (Wasserstein and Lazar 2016), we tested the simple slopes of inattention symptoms at high (+1SD) and low (−1SD) levels of negative parenting to inform how meaningful the interaction might be. Inattention symptoms positively predicted Wave 3 Social Problems as rated by parents at high levels (+1SD) of negative parenting (b = 0.35, SE = 0.14, p = 0.01) with control of child age and sex, positive parenting, Wave 1 ODD symptoms, and Wave 1 CBCL Social Problems (Fig. 1). However, inattention symptoms were unrelated to parent-rated Wave 3 Social Problems at low levels (−1SD) of negative parenting (b = −0.15, SE = 0.11, p = 0.20). These preliminary findings suggest an inattention x negative parenting interaction approaching significance in the prediction of parent-reported Social Problems, although replication is necessary to increase confidence in the effect. In particular, inattention symptoms, not hyperactivity, predicted greater Wave 3 CBCL Social Problems specifically in the context of high negative parenting.
Wave 3 Teacher-Rated Social Problems
ADHD Symptoms and Negative Parenting
To combat shared method variance, we constructed parallel models to test predictions of Wave 3 teacher reported Social Problems, controlling for child age and sex, positive parenting, Wave 1 ODD symptoms, and Wave 1 TRF Social Problems, from baseline ADHD symptoms and observed negative parenting.
Model 1 tested the main effects of baseline ADHD symptoms and negative parenting on Wave 3 TRF Social Problems. Neither negative parenting (b = 0.93, SE = 1.24, p = 0.45) nor ADHD symptoms (b = 0.08, SE = 0.12, p = 0.51) at Wave 1 independently predicted Wave 3 teacher-rated Social Problems at Wave 3 beyond the described covariates (see Table 3 for effect sizes).
To test their interaction, in Model 2, we evaluated the ADHD symptoms x negative parenting interaction in predicting Wave 3 TRF Social Problems. The ADHD x negative parenting interaction significantly predicted Wave 3 teacher-rated Social Problems (b = 0.52, SE = 0.21, p = 0.01, beta = 0.34; Table 3) with a moderate effect size. ADHD symptoms were unrelated to Wave 3 Social Problems at high (b = 0.28, SE = 0.15, p = 0.06) and low (b = −0.11, SE = 0.15, p = 0.45) levels negative parenting. Therefore, we probed the interaction at very high (+2 SD) and very low (−2 SD) levels of negative parenting to isolate where the simple slopes differed from zero in the context of more extreme levels of negative parenting. At very high levels of negative parenting, inattention symptoms positively predicted Wave 3 Social Problems (b = 0.47, SE = 0.20, p = 0.02; Fig. 2). Importantly, 2 SD above the centered mean of negative parenting (i.e., 0.84) is well below the maximum level of negative parenting in the sample (i.e., 1.99), suggesting that testing at this very high level of negative parenting is defensible. Conversely, at very low levels of negative parenting, inattention was unrelated to Wave 3 Social Problems (b = −0.31, SE = 0.20, p = 0.12). Similar to Wave 3 CBCL analyses, when exposed to high negative parenting, greater childhood ADHD symptoms predicted higher Wave 3 Social Problems according to the TRF, although this was only in the context of a more extreme level of negative parenting for teacher report.
Fig. 2.
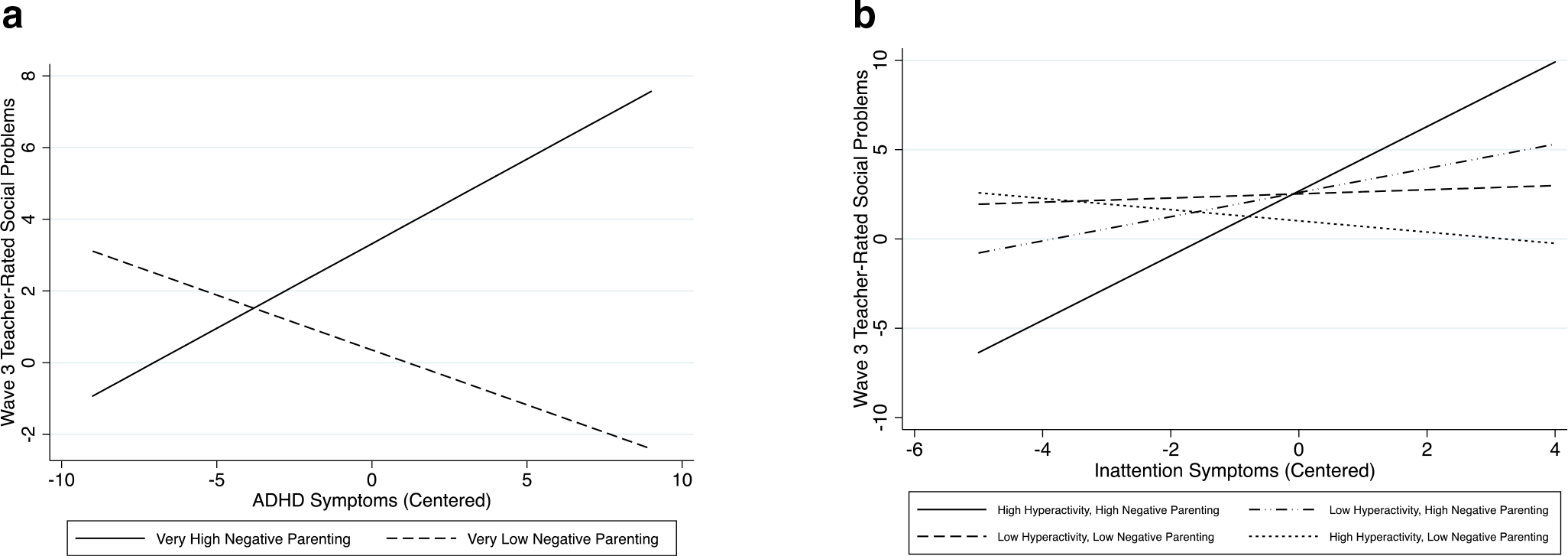
a The interactive effect of total ADHD symptoms and negative parenting on predicted values of Wave 3 teacher-rated Social Problems. b The interactive effect of inattention symptoms, hyperactive symptoms, and negative parenting on predicted values of Wave 3 teacher-rated Social Problems. Both graphs hold covariates at their respective means
Inattention Symptoms, Hyperactivity Symptoms, and Negative Parenting
Next, we tested the association of Wave 1 inattention symptoms, hyperactivity symptoms, observed negative parenting, and their interactions as prospective predictors of teacher-rated Social Problems. In Model 1, as with Wave 3 parent-rated Social Problems (i.e., CBCL), neither Wave 1 negative parenting (b = 1.19, SE = 1.12, p = 0.28), inattention symptoms (b = 0.25, SE = 0.16, p = 0.11), nor hyperactivity symptoms (b = −0.22, SE = 0.22, p = 0.30) independently predicted Wave 3 TRF Social Problems with control of child age and sex, positive parenting, and baseline ODD symptoms, TRF Social Problems (see Table 4 for effect sizes).
To test possible interactive effects in predictions of Wave 3 teacher-rated Social Problems, in Model 2, we entered interaction terms as follows: 1) inattention x negative parenting, 2) hyperactivity x negative parenting, 3) inattention x hyperactivity, and 4) inattention x hyperactivity x negative parenting. In contrast to parent-rated Social Problems, a significant three-way interaction with a large effect size was identified (b = 0.49, SE = 0.11, p < 0.001, beta = 0.49; Table 4); therefore, we probed the interaction to determine the effect of inattention symptoms on teacher-rated Social Problems at varying levels (i.e., +1 SD, −1 SD) of hyperactivity and negative parenting. At high (+1 SD) levels of hyperactivity and negative parenting, inattention symptoms positively predicted Wave 3 Social Problems per teacher report (b = 0.97, SE = 0.34, p < 0.01; Fig. 2). Additionally, inattention symptoms were inversely related to Wave 3 Social Problems in the context of high hyperactivity and low negative parenting (b = −1.13, SE = 0.45, p = 0.01). In contrast, there was no significant relationship between inattention symptoms and Social Problems with the following combinations of hyperactivity and negative parenting: 1) low hyperactivity and high negative parenting (b = −0.02, SE = 0.22, p = 0.94) and 2) low hyperactivity and low negative parenting (b = 0.20, SE = 0.24, p = 0.39). Unlike Wave 3 parent-rated Social Problems, inattention symptoms predicted increased Wave 3 TRF Social Problems in the context of high negative parenting coupled with high hyperactive symptoms. Interestingly, inattention symptoms inversely predicted teacher-reported Social Problems in the context of high hyperactivity and low negative parenting.
Discussion
Given persuasive evidence that ADHD and negative parenting are each associated with youth social functioning, we tested their independent and interactive effects on multi-informant ratings of social problems in a sample of 221 children with and without ADHD followed prospectively for approximately four years, with stringent control of child age and sex, positive parenting, ODD symptoms, and baseline social problems. We review several key findings consistent with our initial hypotheses: 1) ADHD symptoms uniquely predicted parent-rated social problems and 2) ADHD symptoms positively predicted social problems in the context of elevated negative parenting across separate parent and teacher ratings. Notably, for teacher report of social problems, it was only in the context of very high levels (i.e., + 2SD) of negative parenting. This pattern of results is largely consistent with the separate ADHD and parenting literatures (e.g., Bank et al. 2004; Brown and Bakken 2011; Nixon 2001), but suggest continued research considering the interactive association of ADHD and negative parenting.
With respect to exploratory analyses examining the separable dimensions of ADHD, an inattention symptoms x negative parenting interaction approached significance. Specifically, inattention, but not hyperactivity, positively predicted parent-rated social problems in the context of elevated negative parenting. In terms of teacher-rated social problems, a three-way interaction was identified whereby inattention symptoms positively predicted higher social problems only in the presence of high negative parenting and high hyperactivity. Additionally, inattention symptoms were inversely related to social problems in the context of high hyperactivity and low negative parenting.
That ADHD symptoms predicted social problems about four years later primarily in the context of negative parenting underscores their synergistic role. Without consideration of parenting behavior, ADHD symptoms were inversely correlated with social skills across parent and teacher report (Feldman et al. 2017; Humphreys et al. 2016) in the same sample. Additionally, youth with ADHD continue to experience social problems (e.g., rejection)in adolescence and the effect size is large (Bagwell et al. 2001). The current findings suggest that the putative role of ADHD symptoms in the development of social dysfunction must be considered the context of parenting behavior. A prior cross-sectional study of ADHD and parenting identified significant main and meditational effects on child aggression and social skills (Kaiser et al. 2011); however, negative parenting did not moderate the relationship between ADHD and social outcomes (Kaiser et al. 2011). Given the challenge of detecting moderation, including low power (McClelland and Judd 1993), key design features should be prioritized, such as prospective longitudinal designs. Exposure to negative parenting during childhood remains stable over time (Serbin et al. 1998), suggesting that parents may continuously model ineffective interpersonal interactions. Based on social learning theory, children learn and implement behavior they have observed in others (e.g., parents) in their own interactions with peers (Putallaz and Heflin 1990). Given that hyperactivity contributes to social intrusiveness (Wheeler Maedgen and Carlson 2000) and inattention compromises focus during peer interactions (Mikami et al. 2007), elevated ADHD symptoms in the context of negative parenting may promote use of maladaptive social strategies derived from parent-child interactions (Putallaz and Heflin 1990). Passive and evocative genotype-environment correlations may also contribute to the present findings, potentially reflecting correlated genetic influences on parenting behavior and social functioning. Finally, because disruptive child behavior elicits negative parenting (Scaramella and Leve 2004), children with ADHD are susceptible to increased exposure to poor social modeling.
Elucidating the underlying mechanisms of ADHD symptoms x negative parenting’s effect on social problems is necessary to identify targets for intervention. As outlined above, social learning theory suggests that when parents utilize negative strategies, children may enact this behavior with peers. This conceptualization should be tested empirically by examining observational learning as a mechanism of the relationship between negative parenting and social problems in children with symptoms of ADHD. Such empirical studies could clarify how interventions designed to enhance positive parenting and reduce negative parenting yield benefits across behavioral and social outcomes. Youth executive functioning (EF) represents another candidate mechanism. Consisting of cognitive processes that support goal directed behavior (Nigg 2017), EF has been proposed as critical for the support of social functioning (Barkley 2012). Further, individual differences in EF are sensitive to caregiving behaviors (Bernier et al. 2010; Roskam et al. 2014) and EF deficits are central to youth ADHD (Willcutt et al. 2005); therefore, testing youth EF in mechanistic models is a priority, including whether positive parenting may buffer the impact of negative parenting on social problems in the same contexts. Finally, in light of the affective nature of social interaction, emotion regulation may be a particularly important mechanism to consider, as negative parenting predicts difficulties with emotion regulation and blunted neurobiological responses to social reward (Morris et al. 2017). Multiple mediational models should be utilized to simultaneously test the putative mechanisms (e.g., modeling, EF, emotion regulation) underlying predictions of social problems from ADHD symptoms x negative parenting in order to determine which specific pathway represents the most critical target for intervention.
The current findings were largely consistent across Wave 3 parent- and teacher-report for interactions between total ADHD symptoms and negative parenting. In contrast, a slightly different pattern of results emerged for our exploratory examination of the inattention x hyperactivity x negative parenting interaction. In light of the exploratory nature of the three-way interactions, we did not have specific a priori hypotheses and have attempted to conceptualize these findings based upon extant literature. In the current study, inattention symptoms positively predicted parent-rated social problems at Wave 3 when children also experienced high negative parenting, though the interaction only approached significance relative to the alpha of 0.025. Critically, however, guidelines from the American Statistics Association’s statement on p-values explain that “practices that reduce data analysis or scientific inference to mechanical ‘bright-line’ rules (such as ‘p < 0.05’) for justifying scientific claims or conclusions can lead to erroneous beliefs and poor decision making” (Wasserstein and Lazar 2016, p. 131). This perspective emphasizes the need for full transparency of reporting and the importance of enabling readers to utilize such statistical information to inform their own inferences. Because the finding in this study just exceeded the corrected alpha of 0.025, we determined that it may meaningfully suggest that it is specifically the dimension of inattention in ADHD that exerts influence on parent report of youth social problems in the context of elevated negative parenting. However, we acknowledge that readers may come to a different conclusion. If a similar pattern emerges in future studies, it would be important for interventions to emphasize targeting inattention symptoms to improve social outcomes.
In contrast to parent-rated social problems, there was a strong association of baseline inattention and Wave 3 teacher-rated social problems among children with elevated hyperactivity and exposed to elevated negative parenting. Although inattention and negative parenting interactively predicted more social problems approximately four years later across informants, teacher ratings suggest that elevated hyperactivity was also critical. This variation may reflect deviations in parent- and teacher-report of youth social functioning broadly as parent and teacher ratings of social skills are not well correlated and depend on the setting (Gresham et al. 2010; Van der Oord et al. 2005). For example, the correspondence in ratings increases when comparing two teachers versus a parent and teacher (Gresham et al. 2010), and the agreement between teachers and peers is also stronger than parent and teacher ratings of social competence (Renk and Phares 2004). Taken together, this evidence demonstrates the influence of a common setting (i.e., school) on ratings of social behavior. Interestingly, in the context of high hyperactivity and low negative parenting, inattention symptoms were inversely associated with Wave 3 teacher report of social problems. This suggests that low levels of negative parenting may buffer against predictions of social problems (at school) from inattention and hyperactivity. Perhaps inattention and hyperactivity may serve a positive function for social interaction (e.g., for initiating conversation) in the context of low negative parenting. This hypothesis could be tested experimentally wherein negative parenting is manipulated prior to a live or simulated social interaction with peers. Overall, the findings outlined in this paragraph must be viewed as preliminary in nature, especially given the relative instability of three-way interactions in non-experimental designs and the considerable amount of missing teacher data at Wave 3; thus, these interpretations are highly speculative and replication in other samples is imperative.
The results of this study have important implications for intervention. Crucially, social dysfunction is a key source of impairment for children and adolescents with ADHD, which negatively impacts quality of life (Wehmeier et al. 2010), yet social skills training interventions for this population yield little improvement in social functioning (Storebø et al. 2011). The present findings instead suggest that clinicians treating youth with elevations in ADHD symptoms must attend not only to social functioning, but also the putative role of negative parenting behavior in catalyzing this dysfunction. Thus, multimodal approaches, incorporating parent management, may improve social development (Kaminski et al. 2008). Although there is meta-analytic evidence that increasing positive parenting behaviors (e.g., labeled praise, contingent rewards) reduces symptoms (Kaminski et al. 2008), the current results indicated that prioritizing a reduction in negative parenting behavior is particularly important to buffer against the effect of ADHD symptoms on social problems. Subsequent studies must also evaluate positive parenting as a moderator of predictions of youth social problems from ADHD symptoms to clarify which dimension of parenting behavior is most important to target during intervention in order to gain desired improvements in social functioning. Although parents can benefit from learning skills to enhance parenting approaches, the present study suggests that the need for intervention depends on the level of symptoms. Specifically, after negative parenting rises above a particular threshold, interventions to improve social functioning are warranted as ADHD symptom severity increases. Thus, more intensive interventions might be offered as a function of symptom severity, comorbidity, and reaching the negative parenting threshold. This tailored approach is consistent with NIMH’s Research and Domain Criteria, which seeks to individualize care to improve treatment outcomes (Cuthbert and Insel 2013; Insel et al. 2010). To that end, children at the greatest risk for developing social problems based on ADHD symptom severity and negative parenting could be identified to receive parenting interventions and social skills training. Finally, this study reinforces the need to incorporate social outcomes in treatment studies to better identify the approach that can simultaneously reduce symptoms of ADHD and minimize social problems, which increase risk for the development of depression (Feldman et al. 2017).
Despite several strengths of the study (i.e., prospective design, observed parenting data, multi-informant ratings), there are relevant limitations to note as well. First, we included social problems as a single index of social functioning despite the multi-dimensional nature of this construct (Rose-Krasnor 1997). Second, our sample consisted primarily of mothers. Although most research examining the role of parenting on youth outcomes has focused on mothers, it is important that efforts to involve fathers in treatment and research are made (Fabiano 2007). Third, the present study did not incorporate youth-reported social problems. As youth spend more time with peers than family members and are more sensitive to peer influence during adolescence (Brown and Larson 2009), it will be important to also evaluate self-report of social functioning in future studies as well. Finally, given the instability of interactions coupled with the fact that the current sample had significant missing teacher data and is not nationally representative of children or of youth specifically with ADHD, replicability and generalizability may be limited. To review, negative parenting moderated prospective predictions of social functioning from early ADHD symptoms whereby youth with elevated ADHD who experience negative parenting are particularly at risk. Future studies should evaluate underlying mechanisms and test whether reductions in negative parenting reduce social problems in youth with elevations in symptoms of ADHD. Clinicians should carefully evaluate parenting approaches in families of youth with ADHD to identify those who might benefit most from parent training and/or social skills interventions.
Funding
Michelle C. Fenesy is supported through a National Institute of Mental Health Predoctoral Fellowship (5T32MH015750-38).
Footnotes
Compliance with Ethical Standards
Conflict of Interest The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Ethical Approval The study was approved by the University of Californa, Los Angeles Institutional Review Board.
Informed Consent Informed consent was obtained from all parents who participated in the study.
References
- Achenbach TM, & Rescorla L (2001). ASEBA school-age forms & profiles. Burlington: University of Vermont, Research Center for Children, Youth, and Families. [Google Scholar]
- Aiken LS, & West SG (1991). Multiple regression: Testing and interpreting interactions. Thousand Oaks: Sage Publications, Inc. [Google Scholar]
- Bagwell CL, Molina BS, Pelham WE, & Hoza B (2001). Attention-deficit hyperactivity disorder and problems in peer relations: Predictions from childhood to adolescence. Journal of the American Academy of Child & Adolescent Psychiatry, 40(11), 1285–1292. 10.1097/00004583-200111000-00008. [DOI] [PubMed] [Google Scholar]
- Bank L, Burraston B, & Snyder J (2004). Sibling conflict and ineffective parenting as predictors of adolescent boys’ antisocial behavior and peer difficulties: Additive and interactional effects. Journal of Research on Adolescence, 14(1), 99–125. 10.1111/j.1532-7795.2004.01401005.x. [DOI] [Google Scholar]
- Barkley RA (2012). Executive functions: What they are, how they work, and why they evolved. New York: Guilford Press. [Google Scholar]
- Bernier A, Carlson SM, & Whipple N (2010). From external regulation to self-regulation: Early parenting precursors of young children’s executive functioning. Child Development, 81(1), 326–339. 10.1111/j.1467-8624.2009.01397.x. [DOI] [PubMed] [Google Scholar]
- Brown BB, & Bakken JP (2011). Parenting and peer relationships: Reinvigorating research on family–peer linkages in adolescence. Journal of Research on Adolescence, 21(1), 153–165. 10.1111/j.1532-7795.2010.00720.x. [DOI] [Google Scholar]
- Brown BB, & Larson J (2009). Peer relationships in adolescence. In Lerner RM & Steinberg L (Eds.), Handbook of adolescent psychology: Vol. 2. Contextual influences on adolescent development (3rd ed., pp. 74–103). Hoboken: Wiley. [Google Scholar]
- Caron A, Weiss B, Harris V, & Catron T (2006). Parenting behavior dimensions and child psychopathology: Specificity, task dependency, and interactive relations. Journal of Clinical Child and Adolescent Psychology, 35(1), 34–45. 10.1207/s15374424jccp3501_4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chronis-Tuscano A, Raggi VL, Clarke TL, Rooney ME, Diaz Y, & Pian J (2008). Associations between maternal attention-deficit/hyperactivity disorder symptoms and parenting. Journal of Abnormal Child Psychology, 36(8), 1237–1250. 10.1007/s10802-008-9246-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen J (1988). Statistical power analysis for the behavioral sciences (2nd ed.). Hillsdale: Lawrence Erlbaum. [Google Scholar]
- Crnic KA, Gaze C, & Hoffman C (2005). Cumulative parenting stress across the preschool period: Relations to maternal parenting and child behaviour at age 5. Infant and Child Development, 14(2), 117–132. 10.1002/icd.384. [DOI] [Google Scholar]
- Cuthbert BN, & Insel TR (2013). Toward the future of psychiatric diagnosis: The seven pillars of RDoC. BMC Medicine, 11(1), 126. 10.1186/1741-7015-11-126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Diamantopoulou S, Henricsson L, & Rydell AM (2005). ADHD symptoms and peer relations of children in a community sample: Examining associated problems, self-perceptions, and gender differences. International Journal of Behavioral Development, 29(5), 388–398. 10.1177/01650250500172756. [DOI] [Google Scholar]
- Diamantopoulou S, Rydell AM, Thorell LB, & Bohlin G (2007). Impact of executive functioning and symptoms of attention deficit hyperactivity disorder on children’s peer relations and school performance. Developmental Neuropsychology, 32(1), 521–542. 10.1080/87565640701360981. [DOI] [PubMed] [Google Scholar]
- Eisenberger NI, Moieni M, Inagaki TK, Muscatell KA, & Irwin MR (2017). In sickness and in health: The co-regulation of inflammation and social behavior. Neuropsychopharmacology, 42(1), 242–253. 10.1038/npp.2016.141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Enders CK (2010). Applied missing data analysis. New York: Guilford Press. [Google Scholar]
- Eyberg SM, Funderburk BW, Hembree-Kigin TL, McNeil CB, Querido JG, & Hood KK (2001). Parent-child interaction therapy with behavior problem children: One and two year maintenance of treatment effects in the family. Child and Family Behavior Therapy, 23(4), 1–20. 10.1300/J019v23n04_01. [DOI] [Google Scholar]
- Eyberg SM, Nelson MM, Duke M, & Boggs SR (2005). Manual for the dyadic parent-child interaction coding system. Gainesville: University of Florida. Retrieved from http://pcit.phhp.ufl.edu/measures. [Google Scholar]
- Fabiano GA (2007). Father participation in behavioral parent training for ADHD: Review and recommendations for increasing inclusion and engagement. Journal of Family Psychology, 21(4), 683–693. 10.1037/0893-3200.21.4.683. [DOI] [PubMed] [Google Scholar]
- Faraone SV, & Larsson H (2018). Genetics of attention deficit hyperactivity disorder. Molecular Psychiatry, 24, 562–575. 10.1038/s41380-018-0070-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Faul F, Erdfelder E, Lang A-G, & Buchner A (2007). G*power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behavior Research Methods, 39, 175–191. 10.3758/BF03193146. [DOI] [PubMed] [Google Scholar]
- Feldman JS, Tung I, & Lee SS (2017). Social skills mediate the association of ADHD and depression in preadolescents. Journal of Psychopathology and Behavioral Assessment, 39(1), 79–91. 10.1007/s10862-016-9569-3. [DOI] [Google Scholar]
- Fleming CB, Haggerty KP, Catalano RF, Harachi TW, Mazza JJ, & Gruman DH (2005). Do social and behavioral characteristics targeted by preventive interventions predict standardized test scores and grades? Journal of School Health, 75(9), 342–349. 10.1111/j.1746-1561.2005.00048.x. [DOI] [PubMed] [Google Scholar]
- Greene RW, Biederman J, Faraone SV, Wilens TE, Mick E, & Blier HK (1999). Further validation of social impairment as a predictor of substance use disorders: Findings from a sample of siblings of boys with and without ADHD. Journal of Clinical Child Psychology, 28(3), 349–354. 10.1207/S15374424jccp280307. [DOI] [PubMed] [Google Scholar]
- Greene RW, Biederman J, Zerwas S, Monuteaux MC, Goring JC, & Faraone SV (2002). Psychiatric comorbidity, family dysfunction, and social impairment in referred youth with oppositional defiant disorder. American Journal of Psychiatry, 159(7), 1214–1224. 10.1176/appi.ajp.159.7.1214. [DOI] [PubMed] [Google Scholar]
- Gresham FM, Elliott SN, Cook CR, Vance MJ, & Kettler R (2010). Cross-informant agreement for ratings for social skill and problem behavior ratings: An investigation of the social skills improvement system—Rating scales. Psychological Assessment, 22(1), 157–166. 10.1037/a0018124. [DOI] [PubMed] [Google Scholar]
- Hair JF Jr., Anderson RE, Tatham RL, & Black WC (1995). Multivariate Data Analysis (3rd ed.). New York: Macmillan. [Google Scholar]
- Harvey E, Danforth JS, McKee TE, Ulaszek WR, & Friedman JL (2003). Parenting of children with attention-defecit/hyperactivity disorder (ADHD): The role of parental ADHD symptomatology. Journal of Attention Disorders, 7(1), 31–42. 10.1177/108705470300700104. [DOI] [PubMed] [Google Scholar]
- Hinshaw SP, Zupan BA, Simmel C, Nigg JT, & Melnick S (1997). Peer status in boys with and without attention-deficit hyperactivity disorder: Predictions from overt and covert antisocial behavior, social isolation, and authoritative parenting beliefs. Child Development, 68(5), 880–896. 10.2307/1132039. [DOI] [PubMed] [Google Scholar]
- Hoza B (2007). Peer functioning in children with ADHD. Journal of Pediatric Psychology, 32(6), 655–663. 10.1093/jpepsy/jsm024. [DOI] [PubMed] [Google Scholar]
- Hoza B, Gerdes AC, Mrug S, Hinshaw SP, Bukowski WM, Gold JA, et al. (2005a). Peer-assessed outcomes in the multimodal treatment study of children with attention deficit hyperactivity disorder. Journal of Clinical Child and Adolescent Psychology, 34(1), 74–86. 10.1207/s15374424jccp3401_7. [DOI] [PubMed] [Google Scholar]
- Hoza B, Mrug S, Gerdes AC, Hinshaw SP, Bukowski WM, Gold JA, Kraemer HC, Pelham WE, Wigal T, & Arnold LE (2005b). What aspects of peer relationships are impaired in children with attention-deficit/hyperactivity disorder? Journal of Consulting and Clinical Psychology, 73(3), 411–423. 10.1037/0022-006X.73.3.411. [DOI] [PubMed] [Google Scholar]
- Humphreys KL, Galán CA, Tottenham N, & Lee SS (2016). Impaired social decision-making mediates the association between ADHD and social problems. Journal of Abnormal Child Psychology, 44(5), 1023–1032. 10.1007/s10802-015-0095-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Insel T, Cuthbert B, Garvey M, Heinssen R, Pine DS, Quinn K, … Wang P (2010). Research domain criteria (RDoC): Toward a new classification framework for research on mental disorders. American Journal of Psychiatry, 167(7), 748–751. 10.1176/appi.ajp.2010.09091379. [DOI] [PubMed] [Google Scholar]
- Irwin MR, & Miller AH (2007). Depressive disorders and immunity: 20 years of progress and discovery. Brain, Behavior, and Immunity, 21(4), 374–383. 10.1016/j.bbi.2007.01.010. [DOI] [PubMed] [Google Scholar]
- Jensen PS, Martin D, & Cantwell DP (1997). Comorbidity in ADHD: Implications for research, practice, and DSM-V. Journal of the American Academy of Child & Adolescent Psychiatry, 36(8), 1065–1079. 10.1097/00004583-199708000-00014. [DOI] [PubMed] [Google Scholar]
- Kaiser NM, McBurnett K, & Pfiffner LJ (2011). Child ADHD severity and positive and negative parenting as predictors of child social functioning: Evaluation of three theoretical models. Journal of Attention Disorders, 15(3), 193–203. 10.1177/1087054709356171. [DOI] [PubMed] [Google Scholar]
- Kaminski JW, Valle LA, Filene JH, & Boyle CL (2008). A meta-analytic review of components associated with parent training program effectiveness. Journal of Abnormal Child Psychology, 36(4), 567–589. 10.1007/s10802-007-9201-9. [DOI] [PubMed] [Google Scholar]
- Katz SJ, Conway CC, Hammen CL, Brennan PA, & Najman JM (2011). Childhood social withdrawal, interpersonal impairment, and young adult depression: A mediational model. Journal of Abnormal Child Psychology, 39(8), 1227–1238. 10.1007/s10802-011-9537-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kawabata Y, Alink LR, Tseng WL, Van Ijzendoorn MH, & Crick NR (2011). Maternal and paternal parenting styles associated with relational aggression in children and adolescents: A conceptual analysis and meta-analytic review. Developmental Review, 31(4), 240–278. 10.1016/j.dr.2011.08.001. [DOI] [Google Scholar]
- Keown LJ (2012). Predictors of boys’ ADHD symptoms from early to middle childhood: The role of father–child and mother–child interactions. Journal of Abnormal Child Psychology, 40(4), 569–581. 10.1007/s10802-011-9586-3. [DOI] [PubMed] [Google Scholar]
- Koblinsky SA, Kuvalanka KA, & Randolph SM (2006). Social skills and behavior problems of urban, African American preschoolers: Role of parenting practices, family conflict, and maternal depression. American Journal of Orthopsychiatry, 76(4), 554–563. 10.1037/0002-9432.76.4.554. [DOI] [PubMed] [Google Scholar]
- Kraemer HC, & Blasey CM (2004). Centring in regression analyses: A strategy to prevent errors in statistical inference. International Journal of Methods in Psychiatric Research, 13(3), 141–151. 10.1002/mpr.170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lahey BB, & Willcutt EG (2010). Predictive validity of a continuous alternative to nominal subtypes of attention-deficit/hyperactivity disorder for DSM–V. Journal of Clinical Child & Adolescent Psychology, 39(6), 761–775. 10.1080/15374416.2010.517173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lahey BB, Pelham WE, Stein MA, Loney JAN, Trapani C, Nugent K, … & Gold E (1998). Validity of DSM-IV attention-deficit/hyperactivity disorder for younger children. Journal of the American Academy of Child & Adolescent Psychiatry, 37(7), 695–702. 10.1097/00004583-199807000-00008. [DOI] [PubMed] [Google Scholar]
- Larsson H, Anckarsater H, Råstam M, Chang Z, & Lichtenstein P (2012). Childhood attention-deficit hyperactivity disorder as an extreme of a continuous trait: A quantitative genetic study of 8,500 twin pairs. Journal of Child Psychology and Psychiatry, 53(1), 73–80. 10.1111/j.1469-7610.2011.02467.x. [DOI] [PubMed] [Google Scholar]
- Lee SS, Lahey BB, Owens EB, & Hinshaw SP (2008). Few preschool boys and girls with ADHD are well-adjusted during adolescence. Journal of Abnormal Child Psychology, 36(3), 373–383. 10.1007/s10802-007-9184-6. [DOI] [PubMed] [Google Scholar]
- Lee SS, Chronis-Tuscano A, Keenan K, Pelham WE, Loney J, Van Hulle CA, et al. (2010). Association of maternal dopamine transporter genotype with negative parenting: Evidence for gene x environment interaction with child disruptive behavior. Molecular Psychiatry, 15(5), 548–558. 10.1038/mp.2008.102. [DOI] [PubMed] [Google Scholar]
- Lereya ST, Samara M, & Wolke D (2013). Parenting behavior and the risk of becoming a victim and a bully/victim: A meta-analysis study. Child Abuse & Neglect, 37(12), 1091–1108. 10.1016/j.chiabu.2013.03.001. [DOI] [PubMed] [Google Scholar]
- Li C (2013). Little’s test of missing completely at random. Stata Journal, 13(4), 795–809. [Google Scholar]
- Libby P (2006). Inflammation and cardiovascular disease mechanisms. The American Journal of Clinical Nutrition, 83(2), 456S–460S. [DOI] [PubMed] [Google Scholar]
- Locke LM, & Prinz RJ (2002). Measurement of parental discipline and nurturance. Clinical Psychology Review, 22(6), 895–929. 10.1016/S0272-7358(02)00133-2. [DOI] [PubMed] [Google Scholar]
- Lubke GH, Hudziak JJ, Derks EM, van Bijsterveldt TC, & Boomsma DI (2009). Maternal ratings of attention problems in ADHD: Evidence for the existence of a continuum. Journal of the American Academy of Child & Adolescent Psychiatry, 48(11), 1085–1093. 10.1097/chi.0b013e3181ba3dbb. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Malecki CK, & Elliot SN (2002). Children’s social behaviors as predictors of academic achievement: A longitudinal analysis. School Psychology Quarterly, 17(1), 1–23. 10.1521/scpq.17.1.1.19902. [DOI] [Google Scholar]
- McClelland GH, & Judd CM (1993). Statistical difficulties of detecting interactions and moderator effects. Psychological Bulletin, 114(2), 376–390. 10.1037/0033-2909.114.2.376. [DOI] [PubMed] [Google Scholar]
- Mikami AY, Huang-Pollock CL, Pfiffner LJ, McBurnett K, & Hangai D (2007). Social skills differences among attention-deficit/hyperactivity disorder types in a chat room assessment task. Journal of Abnormal Child Psychology, 35(4), 509–521. 10.1007/s10802-007-9108-5. [DOI] [PubMed] [Google Scholar]
- Mokrova I, O’Brien M, Calkins S, & Keane S (2010). Parental ADHD symptomology and ineffective parenting: The connecting link of home chaos. Parenting: Science and Practice, 10(2), 119–135. 10.1080/15295190903212844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morris AS, Criss MM, Silk JS, & Houltberg BJ (2017). The impact of parenting on emotion regulation during childhood and adolescence. Child Development Perspectives, 11(4), 233–238. 10.1111/cdep.12238. [DOI] [Google Scholar]
- Nigg JT (2017). On the relations among self-regulation, self-control, executive functioning, effortful control, cognitive control, impulsivity, risk-taking, and inhibition for developmental psychopathology. Journal of Child Psychology and Psychiatry, 58(4), 361–383. 10.1111/jcpp.12675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nijmeijer JS, Minderaa RB, Buitelaar JK, Mulligan A, Hartman CA, & Hoekstra PJ (2008). Attention-deficit/hyperactivity disorder and social dysfunctioning. Clinical Psychology Review, 28(4), 692–708. 10.1016/j.cpr.2007.10.003. [DOI] [PubMed] [Google Scholar]
- Nixon E (2001). The social competence of children with attention deficit hyperactivity disorder: A review of the literature. Child Psychology and Psychiatry Review, 6(4), 172–180. 10.1017/S1360641701002738. [DOI] [Google Scholar]
- Owens J, & Hoza B (2003). Diagnostic utility of DSM-IV-TR symptoms in the prediction of DSM-IV-TR ADHD subtypes and ODD. Journal of Attention Disorders, 7(1), 11–27. 10.1177/108705470300700102. [DOI] [PubMed] [Google Scholar]
- Pelham WE Jr., Gnagy EM, Greenslade KE, & Milich R (1992). Teacher ratings of DSM–III–R symptoms for the disruptive behavior disorders. Journal of the American Academy of Child & Adolescent Psychiatry, 31, 210–218. 10.1097/00004583-199203000-00006. [DOI] [PubMed] [Google Scholar]
- Perneger TV (1998). What’s wrong with Bonferroni adjustments. BMJ, 316(7139), 1236–1238. 10.1136/bmj.316.7139.1236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Piacentini JC, Cohen P, & Cohen J (1992). Combining discrepant diagnostic information from multiple sources: Are complex algorithms better than simple ones? Journal of Abnormal Child Psychology, 20(1), 51–63. 10.1007/BF00927116. [DOI] [PubMed] [Google Scholar]
- Pressman LJ, Loo SK, Carpenter EM, Asarnow JR, Lynn D, McCracken JT, et al. (2006). Relationship of family environment and parental psychiatric diagnosis to impairment in ADHD. Journal of the American Academy of Child & Adolescent Psychiatry, 45(3), 346–354. 10.1097/01.chi.0000192248.61271.c8. [DOI] [PubMed] [Google Scholar]
- Putallaz M, & Heflin A (1990). Parent-child interaction. In Asher SR & Coie JD (Eds.), Peer rejection in childhood (pp. 189–216). New York: Cambridge University Press. [Google Scholar]
- Rah Y, & Parke RD (2008). Pathways between parent–child interactions and peer acceptance: The role of children’s social information processing. Social Development, 17(2), 341–357. 10.1111/j.1467-9507.2007.00428.x. [DOI] [Google Scholar]
- Renk K (2005). Cross-informant ratings of the behavior of children and adolescents: The “gold standard”. Journal of Child and Family Studies, 14(4), 457–468. 10.1007/s10826005-7182-2. [DOI] [Google Scholar]
- Renk K, & Phares V (2004). Cross-informant ratings of social competence in children and adolescents. Clinical Psychology Review, 24(2), 239–254. 10.1016/j.cpr.2004.01.004. [DOI] [PubMed] [Google Scholar]
- Rose-Krasnor L (1997). The nature of social competence: A theoretical review. Social Development, 6(1), 111–135. 10.1111/j.1467-9507.1997.tb00097.x. [DOI] [Google Scholar]
- Roskam I, Stievenart M, Meunier JC, & Noël MP (2014). The development of children’s inhibition: Does parenting matter? Journal of Experimental Child Psychology, 122, 166–182. 10.1016/j.jecp.2014.01.003. [DOI] [PubMed] [Google Scholar]
- Scaramella LV, & Leve LD (2004). Clarifying parent–child reciprocities during early childhood: The early childhood coercion model. Clinical Child and Family Psychology Review, 7(2), 89–107. 10.1023/B:CCFP.0000030287.13160.a3. [DOI] [PubMed] [Google Scholar]
- Schafer JL, & Graham JW (2002). Missing data: Our view of the state of the art. Psychological Methods, 7(2), 147–177. 10.1037//1082-989X.7.2.147. [DOI] [PubMed] [Google Scholar]
- Schlomer GL, Bauman S, & Card NA (2010). Best practices for missing data management in counseling psychology. Journal of Counseling Psychology, 57(1), 1–10. 10.1037/a0018082. [DOI] [PubMed] [Google Scholar]
- Schuhmann EM, Foote RC, Eyberg SM, Boggs SR, & Algina J (1998). Efficacy of parent-child interaction therapy: Interim report of a randomized trial with short-term maintenance. Journal of Clinical Child Psychology, 27, 34–45. 10.1207/s15374424jccp2701_4 [DOI] [PubMed] [Google Scholar]
- Serbin LA, Cooperman JM, Peters PL, Lehoux PM, Stack DM, & Schwartzman AE (1998). Intergenerational transfer of psychosocial risk in women with childhood histories of aggression, withdrawal, or aggression and withdrawal. Developmental Psychology, 34(6), 1246–1262. 10.1037/0012-1649.34.6.1246. [DOI] [PubMed] [Google Scholar]
- Shaffer D, Fisher P, Lucas CP, Dulcan MK, & Schwab-Stone ME (2000). NIMH diagnostic interview schedule for children version IV (NIMH DISC-IV): Description, differences from previous versions, and reliability of some common diagnoses. Journal of the American Academy of Child & Adolescent Psychiatry, 39(1), 28–38. 10.1097/00004583-200001000-00014. [DOI] [PubMed] [Google Scholar]
- Shemmassian SK, & Lee SS (2016). Predictive utility of four methods of incorporating parent and teacher symptom ratings of ADHD for longitudinal outcomes. Journal of Clinical Child & Adolescent Psychology, 45(2), 176–187. 10.1080/15374416.2014.971457. [DOI] [PubMed] [Google Scholar]
- Storebø OJ, Skoog M, Damm D, Thomsen PH, Simonsen E, & Gluud C (2011). Social skills training for attention deficit hyperactivity disorder (ADHD) in children aged 5 to 18 years. Cochrane Database of Systematic Reviews, 12, CD008223. [DOI] [PubMed] [Google Scholar]
- Tabachnick BG, & Fidell LS (2012). Using multivariate statistics (6th ed.). Needham Heights: Allyn & Bacon. [Google Scholar]
- Theule J, Wiener J, Tannock R, & Jenkins JM (2013). Parenting stress in families of children with ADHD: A meta-analysis. Journal of Emotional and Behavioral Disorders, 21(1), 3–17. 10.1177/1063426610387433. [DOI] [Google Scholar]
- Van der Oord S, Van der Meulen EM, Prins PJ, Oosterlaan J, Buitelaar JK, & Emmelkamp PM (2005). A psychometric evaluation of the social skills rating system in children with attention deficit hyperactivity disorder. Behaviour Research and Therapy, 43(6), 733–746. 10.1016/j.brat.2004.06.004. [DOI] [PubMed] [Google Scholar]
- Wasserstein RL, & Lazar NA (2016). The ASA’s statement on p-values: Context, process, and purpose. The American Statistician, 70(2), 129–133. 10.1080/00031305.2016.1154108. [DOI] [Google Scholar]
- Webster-Stratton C, Reid MJ, & Hammond M (2001). Preventing conduct problems, promoting social competence: A parent and teacher training partnership in head start. Journal of Clinical Child Psychology, 30(3), 283–302. 10.1207/S15374424JCCP3003_2. [DOI] [PubMed] [Google Scholar]
- Wehmeier PM, Schacht A, & Barkley RA (2010). Social and emotional impairment in children and adolescents with ADHD and the impact on quality of life. Journal of Adolescent Health, 46(3), 209–217. 10.1016/j.jadohealth.2009.09.009. [DOI] [PubMed] [Google Scholar]
- Wheeler Maedgen J, & Carlson CL (2000). Social functioning and emotional regulation in the attention deficit hyperactivity disorder subtypes. Journal of Clinical Child Psychology, 29(1), 30–42. 10.1207/S15374424jccp2901_4. [DOI] [PubMed] [Google Scholar]
- Willcutt EG, Doyle AE, Nigg JT, Faraone SV, & Pennington BF (2005). Validity of the executive function theory of attention-deficit/hyperactivity disorder: A meta-analytic review. Biological Psychiatry, 57(11), 1336–1346. 10.1016/j.biopsych.2005.02.006. [DOI] [PubMed] [Google Scholar]


