Abstract
Background:
Nursing home residents face many barriers to access specialist physician outpatient care. However, little data exists on how specialty care use changes when individuals transition to a nursing home in the US.
Methods:
We studied specialist outpatient visits for new long-term care (LTC) residents within one year before and after their transition to nursing home residence using Minimum Data Set v3.0 (MDS) and a 20% sample of Medicare fee-for-service claims in 2014–2018. To focus on residents requiring specialty care at baseline, we limited the cohort to residents with specialty care in the 13–24 months before LTC transition. We then measured the proportion of residents receiving at least one visit in the 12 months before the transition and the 12 months after the transition. We also examined subgroups of residents with a prior diagnosis likely requiring long-term specialty care (e.g., multiple sclerosis). Finally, we examined whether there was continuity of care within the same specialty care provider.
Results:
Among 39,288 new LTC transitions identified in 2016–2017, 17,877 (45.5%) residents had a prior specialist visit 13–24 months before the transition. Among them, the proportion of residents with specialty visits decreased consistently in all specialties in the 12 months after the transition, ranging from a relative decrease of 14.4% for orthopedics to 67.9% for psychiatry. The relative decrease among patients with a diagnosis likely requiring specialty care ranged from 0.9% for neurology in patients with multiple sclerosis to 67.1% for psychiatry in patients with severe mental illness. Among residents who continued visiting a specialist, 78.9% saw the same provider as before the transition.
Conclusions:
Use of specialty care falls significantly after patients transition to a nursing home. Further research is needed to understand what drives this drop in use and whether interventions such as telemedicine can ameliorate potential barriers to specialty care.
Keywords: Nursing home, skilled nursing facility, long-term care, specialist, outpatient
Introduction
The population of Americans requiring institutional long-term care (LTC) will increase substantially in the coming decades.1,2 Many have multiple complex chronic conditions3 that require specialist physician care. However, LTC residents face many barriers to accessing specialty care. Given nursing homes are often understaffed,4,5 residents without family and other social support may not be able to schedule visits or have the necessary support to travel to the specialist. Many nursing home residents also require special transportation, which might be difficult to organize, and specialists are not incentivized to visit residents in nursing homes, as their travel time is not reimbursed.6 Accessing specialists might be especially difficult for otherwise vulnerable groups of residents, such as those with developmental disorders, dementia or mental health issues.7 Although there is limited direct research quantifying the benefits of specialty care among nursing home residents,10,11 decreases in specialty care use could lead to avoidable hospitalizations,8 emergency room visits, potentially inappropriate prescribing,9 and poorer health.
Use of specialty care among US nursing home residents is little studied. Prior research has largely focused on access to and use of specialty care among community-dwelling older adults,12–15 demonstrating increasing use of specialty care. Existing evidence among nursing home residents has mostly focused on cross-sectional, rather than longitudinal, studies of specialty care.16–19 No prior work has examined the transition to a nursing home or the use of specialists among residents with a high need for specialty care. More evidence on utilization of specialty care could guide efforts to improve quality of care, point to areas that could benefit from interventions or higher uptake of telemedicine, and identify groups of residents who might be facing the greatest barriers.
To address this evidence gap, we examined patterns of utilization of specialty care among LTC residents before and after entry to a nursing home. We focused on persons who used specialty care before health events that likely contributed to the LTC transition as well as subgroups of patients diagnosed with diseases likely requiring long-term specialty care, and groups of particularly vulnerable nursing home residents such as those with developmental disabilities or severe mental illness. Directly measuring the clinical need for specialty care and thus comparing the observed use of such care with an “appropriate” level of visits is difficult with routinely collected health care use data.15,20 Therefore, in this study we focused on patients with previous specialty care use, particularly those with diagnoses likely necessitating consistent specialty care, as a proxy for patients with likely ongoing specialty care needs.
Methods
Data source and study population
Using a 20% random sample of Medicare fee-for-service claims and the corresponding Minimum Data Set (MDS) v3.0 files, we identified persons continuously enrolled in Part A and Part B from 2014 to 2018 (or death, if earlier). Based on a previously described algorithm,21,22 we defined our study population of new LTC residents as beneficiaries who moved to a nursing home and stayed at least 180 days without being discharged home (based on MDS records), and did not spend a significant amount of time in a nursing home within 12 months before the move (i.e., no skilled nursing facility stay longer than 14 days). In sensitivity analyses, we also tested limits of 30 or 90 days for skilled nursing facility stays (see Supplemental figure S2). To focus on beneficiaries moving to nursing home for LTC (rather than end-of-life care) and to ensure the same length of follow up period for all persons, we excluded patients who died within 12 months after the transition or used hospice services for more than 14 days within 6 months before or after the transition.
Our observation period was 36 months (24 months before and 12 months after the transition). We defined previous users of specialty care as those with a relevant visit 13–24 months before the transition. This restriction excludes the year prior to LTC transition to minimize the probability that the observed specialty care was directly linked to the health event leading to the transition (e.g., orthopedic surgery care for a hip fracture). This restriction addresses the concern that if we selected patients with specialty care directly before the transition, use would naturally fall after the transition due to regression to the mean. In a sensitivity analysis, we tested how our main results change with different definitions of previous users (using 6 months before and after the transition to capture the outcome (see Supplemental figure S3), and one or two visits within 7–12 months before, one visit in 7–12 moths and 13–18 months, and one visit in 7–12, 13–18, and 19–24 months before the transition to define previous users). Finally, we also tested if the main results were robust to excluding 3 months before and after the transition, as outpatient care during that period is likely to be affected by an acute health event that led to the LTC transition.
As an alternate approach to identify likely specialty care needs, we also identified patients with predefined psychiatric, neurological, cardiac, and other comorbidities with diagnoses recorded in claims before the transition to a nursing home. Recognizing that while there is some evidence that specialty care can lead to better outcomes in acute care settings,23 there is little research focused on whether chronic condition care is improved if specialists are involved.24 Therefore, we selected a set of comorbidities and diagnoses that likely require specialty care based on the input of two authors who are internal medicine specialists (AM, MLB). Finally, we selected the groups of potentially vulnerable residents with developmental disorders, severe mental illness (bipolar disorder, schizophrenia, and other psychotic disorders), and Alzheimer’s disease or other dementia for sensitivity analysis. Variables and codes used to identify these patient groups with the selected diagnoses and conditions are provided in Table S1.
The study was approved by the Office of Human Research Administration at Harvard Medical School. The requirement for informed consent was waived because the data were deidentified.
Outcome measures
Our main outcomes were the count and proportion of beneficiaries receiving at least one specialist visit within the 12 months before and after the transition to LTC in nursing home. We focused on the top 10 specialties by office volume based on specialty codes in visits 13–24 months before the transition. Secondary outcomes included the count of specialist visits per observation period. As a point of comparison, we also captured generalists (defined in this study as physicians of general, internal, family medicine or geriatrics as well as nurse practitioners) who are the most common nursing home clinicians. Specialist physician visits were identified in Part B carrier and outpatient claim files by Healthcare Common Procedure Coding System (HCPCS) codes, provider specialty, place of service, and revenue center codes (Table S1), so that we capture visits provided in “outpatient” settings (which can include any setting of care that is not acute care) and excluded inpatient and emergency department consultations. We tested in a sensitivity analysis if adding inpatient consultations (HCPCS codes 99221-3 and 99251-5, delivered in inpatient place of service or revenue center) change the results meaningfully.
Study variables
We examined the following beneficiary characteristics from Medicare enrollment files: age at the time of transition to a nursing home, sex, race/ethnicity, dual eligibility status (defined as at least one month of dual eligibility for Medicaid in 2014), reason for Medicare enrollment in 2014, state and ZIP code of residence (at the start of 2014), and the number of comorbidities (identified with Chronic Conditions Data Warehouse (CCW) flags in 2014). We also captured flags for severe mental illness; epilepsy; Alzheimer’s disease and other dementias, and developmental disorders using indicators from the CCW;25 and Parkinson’s disease, multiple sclerosis, rheumatoid or psoriatic arthritis, and cancer using as at least one relevant diagnosis in inpatient and outpatient claims from 2014 until the transition to the nursing home (Table S1).
Statistical analysis
We used proportions, median, interquartile range (IQR), mean and standard deviation (SD) to summarize relevant characteristics of the study population. We visualized the trajectories of specialty care at the time of transition to a nursing home by plotting the monthly proportion of beneficiaries with at least one specialist visit from 12 months before to 12 months after the transition. We calculated the change in the proportion of specialty care users within 12 months before and after the transition.
To estimate the continuity of care among patients with specialist visits within 12 months both before and after the transition, we calculated the proportion seeing one of their previous providers at least once at the nursing home, as recorded in the analyzed specialty visits using national provider identifier codes. As a sensitivity analysis and a narrower definition of continuity of care, we calculated the proportion of patients with 80% or greater specialty care visits after LTC transition with a previously seen provider.
Results
We identified 39,288 individuals as new LTC residents at nursing homes who survived at least 12 months after their transition to LTC. Among them, we selected those with a prior specialist visit 13–24 months before the transition (17,877, 45.5%; Table 1).
Table 1.
Characteristics of new LTC residents at nursing homes who were previous users of specialty care
| Specialty visits in LTC | ||||
|---|---|---|---|---|
| Overall | No | Yes | p-value | |
| N | 17,877 | 6,305 (35.3%) | 11,572 (64.7%) | |
| Age (mean, SD) | 80.4 (11.3) | 81.5 (11.0) | 79.7 (11.3) | <0.001 |
| Sex | <0.001 | |||
| Female | 11,900 (66.6%) | 4,391 (69.6%) | 7,509 (64.9%) | |
| Male | 5,977 (33.4%) | 1,914 (30.4%) | 4,063 (35.1%) | |
| Race | 0.028 | |||
| White | 15,587 (87.2%) | 5,447 (86.4%) | 10,140 (87.6%) | |
| Black | 1,568 (8.8%) | 574 (9.1%) | 994 (8.6%) | |
| Other | 722 (4.0%) | 284 (4.5%) | 438 (3.8%) | |
| Dually eligible for Medicaid (%) | 6,293 (35.2%) | 2,095 (33.2%) | 4,198 (36.3%) | <0.001 |
| Reason for Medicare enrollment in 2015a | <0.001 | |||
| Old age | 15,881 (88.8%) | 5,713 (90.6%) | 10,168 (87.9%) | |
| Disability | 1,996 (11.2%) | 592 (9.4%) | 1,404 (12.1%) | |
| Comorbidities | ||||
| Total (median, IQR) | 10 (7–12) | 9 (7–12) | 10 (7–12) | <0.001 |
| Alzheimer’s/other dementia (%) | 11,309 (63.3%) | 4,559 (72.3%) | 6,750 (58.3%) | <0.001 |
| Heart failure (%) | 9,757 (54.6%) | 3,075 (48.8%) | 6,682 (57.7%) | <0.001 |
| Severe mental illness (%) | 2,831 (15.8%) | 996 (15.8%) | 1,835 (15.9%) | 0.916 |
| Liver disease and cirrhosis (%) | 2,395 (13.4%) | 747 (11.9%) | 1,648 (14.2%) | <0.001 |
| Cancer (%) | 2,116 (11.8%) | 553 (8.8%) | 1,563 (13.5%) | <0.001 |
| Epilepsy (%) | 1,887 (10.6%) | 658 (10.4%) | 1,229 (10.6%) | 0.702 |
| Parkinson’s disease (%) | 1,672 (9.3%) | 503 (8.0%) | 1,169 (10.1%) | <0.001 |
| Developmental disorders (%) | 1,201 (6.7%) | 429 (6.8%) | 788 (6.3%) | 0.735 |
| Rheumatoid/psoriatic arthritis (%) | 894 (5.0%) | 266 (4.2%) | 628 (5.4%) | <0.001 |
| Multiple sclerosis (%) | 307 (1.7%) | 64 (1.0%) | 243 (2.1%) | <0.001 |
| Setting (before transition) | <0.001 | |||
| Metropolitan | 6,767 (37.8%) | 2,568 (40.7%) | 4,199 (36.3%) | |
| Micropolitan | 5,935 (33.2%) | 2,032 (32.2%) | 3,903 (33.7%) | |
| Non-metro, non-rural | 4,554 (25.5%) | 1,503 (23.8%) | 3,051 (26.4%) | |
| Rural | 621 (3.5%) | 202 (3.2%) | 419 (3.6%) | |
| US region (before transition) | <0.001 | |||
| West | 1,776 (9.9%) | 614 (9.7%) | 1,162 (10.0%) | |
| Midwest | 5,166 (28.9%) | 1,690 (26.8%) | 3,476 (30.0%) | |
| Northeast | 4,277 (23.9%) | 1,657 (26.3%) | 2,620 (22.6%) | |
| South | 6,658 (37.2%) | 2,344 (37.2%) | 4,314 (37.3%) | |
Patients are considered previous users of specialty care if they had at least one specialist visit 13–24 months before the transition to a nursing home. Visits in LTC are evaluated in the first 12 months after the transition. We used chi-square test for categorical variables and t-test for continuous variables comparisons.
LTC – long-term care. IQR – interquartile range. SD – standard deviation.
A – patients with end stage renal disease are included in the disability category.
Among patients with any previous specialist visit, those who visited a specialist at least once during the first 12 months of LTC were slightly more likely to be male (35.1% vs 30.4%), enrolled in Medicare due to disability (12.1% vs 9.4%), and less likely to have Alzheimer’s disease or other dementia (58.3% vs 72.3%) than those without specialist visits in LTC (Table 1). Patients with most of the other examined comorbidities were more likely to receive specialist visits during LTC. Age, race, dual eligibility for Medicaid, urban or rural setting and region were distributed similarly among those with and without visits in LTC.
Patterns of specialty care
The relative drop in the proportion of residents with specialty visits ranged from 14.4% for orthopedics to 67.9% for psychiatry (Figure 1A and 1B). Results were similar when comparing the total number of visits rather than the proportion of beneficiaries with visits (Figure S1). Among subgroups of potentially vulnerable residents with developmental disorders, severe mental illness, and Alzheimer’s disease or other dementia, there were similar changes in the use of specialty care (Figure 2). The change was similar with different thresholds of days at SNF in the year before the transition to LTC (Figure S2) and different definitions of previous users of specialty care (Figure S3), as well as when inpatient specialist consultations were considered in addition to outpatient visits (Figure S4). The decrease was also similar when 6 months around the transition were excluded (Figure S5). In contrast, among previous specialty care users, the proportion with a generalist visit increased from 87.5% in the 12 months before to 97.8% in the 12 months after the transition (relative increase of 11.8%).
Figure 1.
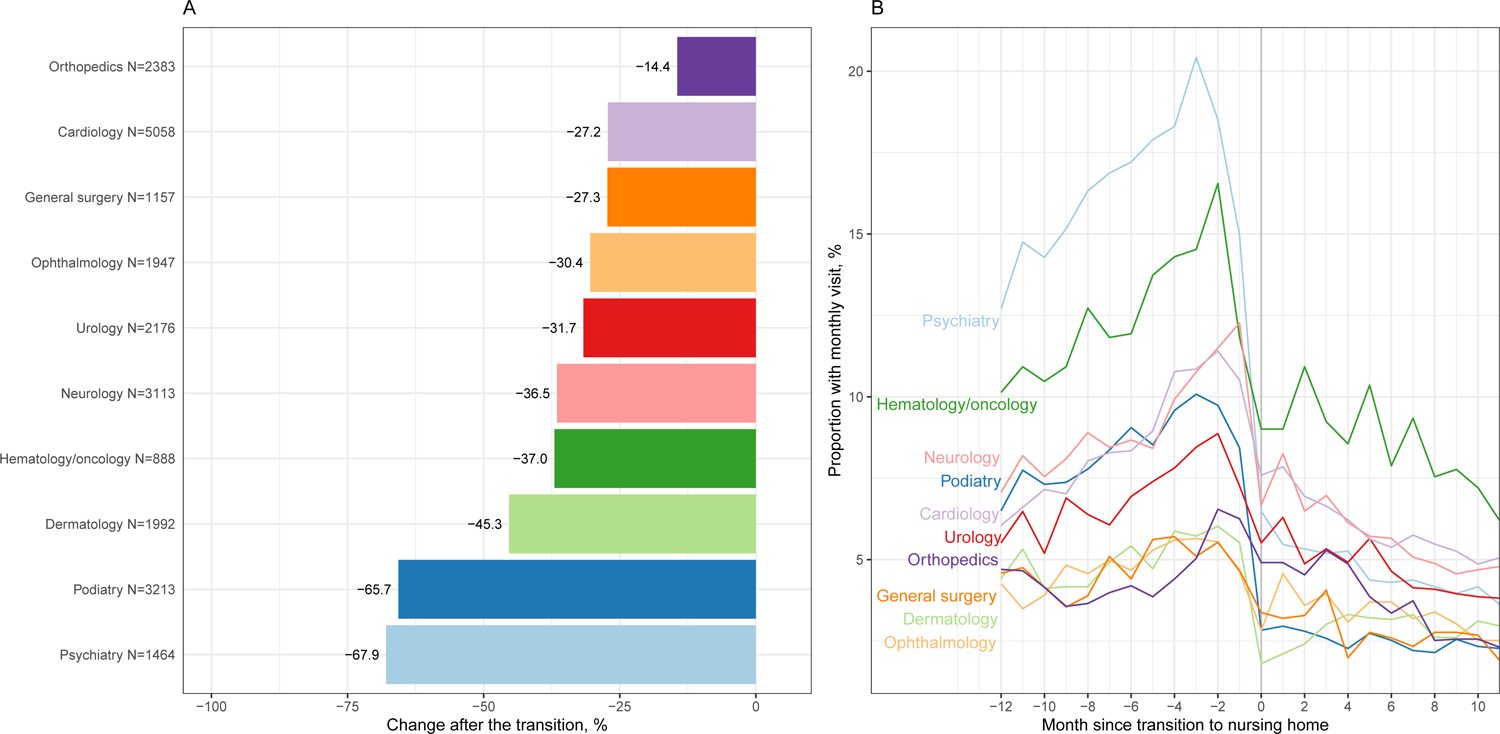
Proportion of previous specialty care users with specialist visit before and after transition to nursing home
A – Relative change in the number of previous users with a specialist visit from 12 months before to 12 months after the transition to nursing home
B – Monthly proportion of previous users with a specialist visit
Figure 2.
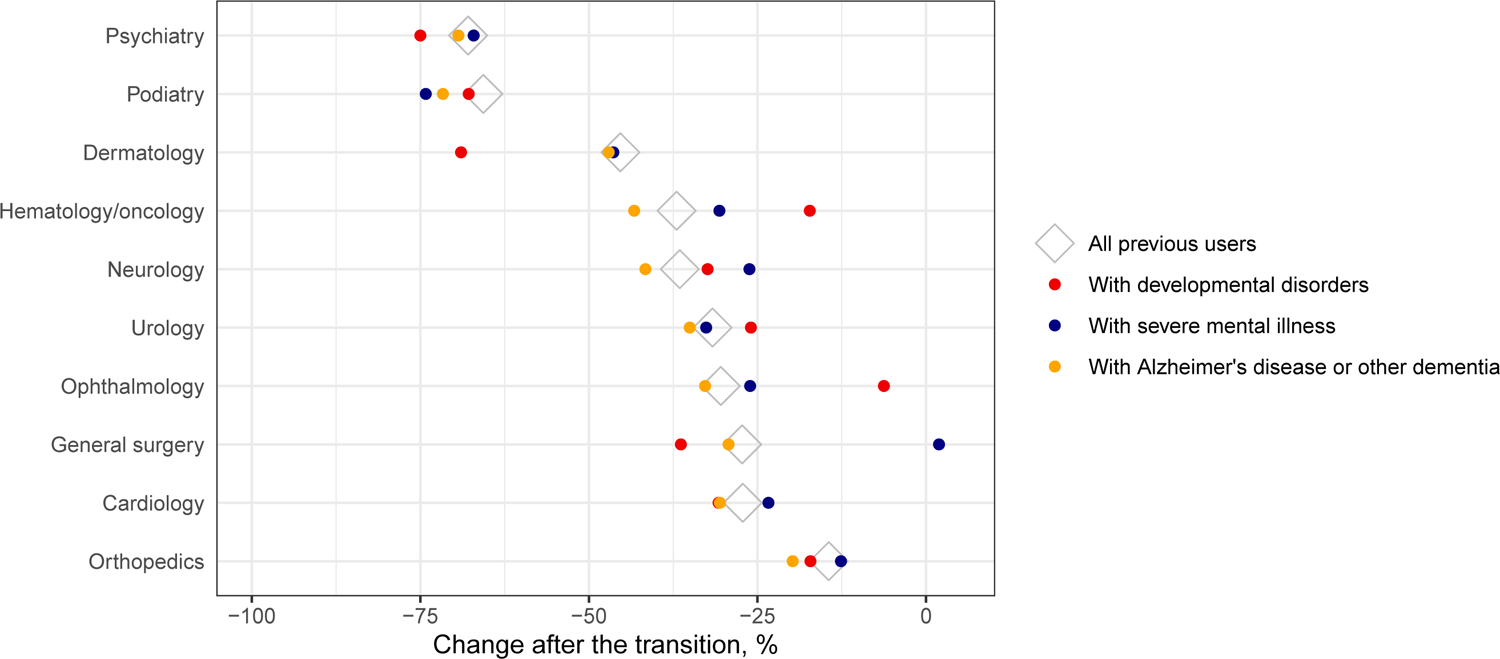
Relative change in the number of previous users with a specialist visit from 12 months before to 12 months after the transition to a nursing home in groups of vulnerable residents
Specialties are ranked by the relative change among all previous users of specialty care (corresponding to the decrease shown in Figure 1A; shown as diamonds here). The relative change in the subgroups of vulnerable patients among the previous users is shown as colored dots (pink – residents with developmental disorders; dark blue – residents with severe mental illness; yellow – residents with Alzheimer’s disease or other dementia).
Among patients with a diagnosis likely requiring specialty care, there was also a drop in specialist use after the transition (Table 2). The relative decrease in the proportion of beneficiaries with relevant specialist visits ranged from 0.9% (neurology for patients with multiple sclerosis) to 67.1% (psychiatry for patients with severe mental illness).
Table 2.
Proportion of previous specialty care users with health conditions potentially requiring specialty care with such a visit before and after transition to a nursing home
| Specialty-Specific Diagnosis | Relevant Specialty | N | 12 months before | 12 months after | % change |
|---|---|---|---|---|---|
| Heart failure | Cardiology | 3,718 | 2,047 | 1,535 | −25.0% |
| Parkinson’s disease | Neurology | 871 | 578 | 434 | −24.9% |
| Epilepsy | Neurology | 616 | 331 | 223 | −32.6% |
| Multiple sclerosis | Neurology | 178 | 110 | 109 | −0.9% |
| Severe mental illness | Psychiatry | 974 | 629 | 207 | −67.1% |
| Cancer | Hematology/oncology | 421 | 260 | 183 | −29.6% |
| Rheumatoid or psoriatic arthritis | Rheumatology | 318 | 205 | 119 | −42.0% |
| Liver disease and cirrhosis | Gastroenterology | 252 | 70 | 46 | −34.3% |
Severe mental illness includes bipolar disorder, schizophrenia, and other psychotic disorders, Diagnoses codes and Chronic Conditions Data Warehouse flags for chronic or potentially disabling conditions used to define each diagnosis group are listed in Supplemental Table S1.
Continuity of specialty care
Among the residents who visited a specialist within the year before as well as after the transition, the majority (78.9% on average across the specialties) were seen at least once by the same provider as before the transition (Table S2). The proportion of continued specialty users visiting the same provider ranged from 62.0% (orthopedics), 72.4% (podiatry) and 72.5% (general surgery), to 82.4% (cardiology and neurology) 84.2% (psychiatry), and 90.0% (hematology and oncology). The results were similar with a narrower definition of continued care (80% or greater specialty care visits after LTC transition with a previously seen provider, Table S2).
Discussion
In a national sample of Medicare beneficiaries, we found that specialty visits decreased substantially upon transition to a nursing home. If the levels of specialty care use prior to their LTC transition captured an appropriate level of care, these findings could suggest substantial lack of access to specialty care in nursing homes. However, we are unable to assess the appropriateness of visit frequency or specialist access before or after the LTC transition with claims data alone. To our knowledge this is the first national examination of specialty care use at the transition to nursing homes in the US. Our results echo use of specialty care in other countries. In France, the proportion of persons with specialty care decreased moderately across most of the specialties.26 But this is not true in all counties. In a cohort of new nursing home residents in Germany, a significant overall decrease in specialty care use was found only for ophthalmology (by 20%), while contacts with neurologists and psychiatrists increased after the transition.27
There was wide variation in the change in use across specialties. The groups of specialties with similar magnitudes of change have some clinical characteristics in common: specialties with a smaller decrease (e.g., orthopedics and cardiology) may reflect care for health conditions that led to the need for institutional LTC, while specialties with larger decreases (e.g., podiatry and dermatology) might be those perceived to provide care for less severe or functionally disabling conditions. In contrast to the decrease in visits by specialists, patients received more visits by generalist providers after the transition, almost certainly due to the mandated regular primary care provider visits for Medicare beneficiaries in nursing facilities. Primary care providers, especially physicians specializing in care for skilled nursing facility residents,27 might take over some routine specialty care for some of the patients. Indeed, care consolidation by a regularly attending nursing home physician might be preferred by some patients than the increasingly fragmented care among multiple specialty providers.13,28,29
Importantly, many services of some of the specialties with the largest drop in use, such as psychiatry or neurology, could be delivered via telemedicine, overcoming the need for transportation as a barrier to specialty care. Indeed, tele-psychiatry30 and telehealth services for patients with Parkinson’s disease31,32 have already been successfully implemented in nursing homes.33 In contrast, specialties requiring specialized physical examination or procedures, such as ophthalmology, are hard to substitute without physically transporting residents to outside offices, via telemedicine or by nursing home primary care provider.
The decrease in specialty care was slightly lower for patients with specific diagnoses identified as requiring specialty care. For example, neurologist visits decreased by 37% overall among previous users, while the relative decrease was by 33%, 25% and 1% for patients with epilepsy, Parkinson’s disease, and multiple sclerosis, respectively. The decrease among such patients is particularly concerning that some may receive less attention than their comorbidities may ideally need.
One unexpected finding is that residents receiving specialty care before as well as after the transition most often continued seeing the same provider. Such consistent continuity of care with the same specialty provider might signal that patients value retaining their outpatient specialty care provider across residential settings. It might also reflect a selection effect – patients who consistently visit specialty providers regardless of their community or nursing home setting are perhaps more likely to have social and financial resources that might also help them keep visiting the same physician. Regardless of the underlying mechanisms, the high prevalence of continuity with prior physicians suggests that for many SNFs, receiving outside specialty care is an established model for residents. More evidence is needed to understand the processes that enable SNFs to have their patients continue to see their specialists.
These results are consistent with other evidence on barriers to specialty care among LTC populations, an issue that has received limited empirical evaluation. In a national survey of German nursing homes, high and unmet needs for specialty care were documented particularly for ophthalmology and urology.19 Research on lack of access to specialty care in the US has focused only on some areas, such as mental and behavioral health services.34 A national study of nursing home administrators in 2017 identified unmet needs for behavioral health services in one-third of nursing homes.7 Half of nursing homes named lack of behavioral health education among staff, and a third noted inadequate coordination with community providers and lack of infrastructure for referrals and transportation of residents as major barriers. Nursing home residents without family caregivers might also have worse access to care – lack of caregiving by a health care proxy was associated with worse quality of care in several studies.35,36 These reported barriers to care, together with the decrease in specialist visits observed in our study, imply that access to specialty care in nursing homes might be suboptimal.
This study has limitations. First, it is important to emphasize that a decrease in specialty care utilization could be clinically justified. In some circumstances, a decrease may reflect a substitution by primary health care services provided directly at the nursing home or changing patient preferences. The optimal frequency of specialty follow up is not known for many diseases and conditions. Some specialty care, for example, provided as part of post-surgical care under a global payment or via informal networks of physicians in the nursing homes was not captured with fee-for-service claims data. Similarly, visits provided by nurse practitioners providing specialty care would be misclassified as generalist visits. Thus, the decrease could potentially be slightly smaller than we observe. However, although specialty care utilization is only a proxy for care need, the consistent and striking drop could signal barriers to access and is, therefore, concerning. Second, this is an observational cohort study, and as such cannot establish causality around the relationship between LTC transition and specialty use as distinct from other concurrent processes. Frequency of visits might change over time regardless of the residential setting, for example, due to regression to the mean after a period of more intense health care use – a bias that we could not completely exclude. To decrease this bias, we restricted our sample to specialty care users 13–24 months rather than immediately before the transition. We also confirmed the findings in a subset of patients with diagnoses likely necessitating regular specialty care. Still, our results should be interpreted as exploratory, especially as moving to a nursing home might be in part motivated by health care preferences and needs changing from single-disease management to more integrated nursing and clinical care with higher presence of the primary care provider. Third, our capacity to identify the barriers for specialty care utilization is limited by the information included in the studied claims and MDS data. For example, we cannot quantify the relative importance of many factors that drive a decrease in specialty care use including lack of available transportation, social or personnel support, patient’s preference to forego specialty care outside the nursing home, and other reasons. We also did not adjust for patient, provider or nursing home factors that might be associated with the probability of continuous specialty care. In the future, it will be important to compare the decrease in use in new residents to that in a reference population of matched persons (e.g., experiencing a hospitalization without an eventual transfer to nursing home for LTC). Finally, it was beyond the scope of this study to investigate whether the observed decrease in specialty care results in worse patient outcomes, such as greater risk of hospitalization.
In conclusion, this study showed a substantial drop in specialty care utilization after transitioning to a nursing home for LTC among persons likely in need of such care, suggesting the existence of potential barriers to care at nursing homes, with likely variation across specialties. Further research should examine the reasons for this decrease and, considering the recent rise in telemedicine use during the COVID-19 pandemic, the potential role of telemedicine to supplement or substitute in-person specialist visits after the LTC transition.
Supplementary Material
Table S1 Codes used to identify patients and specialist visits
Figure S1 Count of specialist visits among the previous specialty care users before and after transition to a nursing home
A – Relative change in the number of specialist visits among the previous users from 12 months before to 12 months after the transition to a nursing home
B – Monthly specialist visits among the previous users of specialty care
Table S2 Continuity of specialty care in residents visiting specialists in the year before and after the transition to a nursing home
Figure S2 Relative change in the number of specialist visits among the previous users after the transition to a nursing home, with different threshold of allowed days in SNF within the year before the transition
Figure S3 Relative change in the number of specialist visits among the previous users in 6 months before to 6 months after the transition to a nursing home, with different definitions of previous care users
Figure S4 Relative change in the number of previous users with a specialist visit in outpatient or inpatient setting from 12 months before to 12 months after the transition to nursing home
Figure S5 Relative change in the number of previous users with a specialist visit before and after the transition to the nursing home, comparing periods of 12 months and 9 months (excluding 6 months around the transition)
Key points.
There is a substantial decline in the use of specialty care after transition to a nursing home, even among those residents with diseases typically requiring regular specialty care.
Most of the patients who continued visiting a specialist after the transition to a nursing home were visiting the same provider that they saw before the transition.
Why does this matter?
The overall clinical quality of care in nursing homes is often suboptimal, with high rates of unnecessary hospitalizations and low-value care like inappropriate medication use. Appropriate outpatient specialty care could improve the quality of medical care in nursing homes but accessing specialty care may be difficult for residents. Understanding potential gaps in specialty care can inform interventions to facilitate appropriate specialty care use such as implementing telemedicine programs. We find that specialty care in US nursing homes decreases across specialties once a patient moves to a nursing home – motivating further research to understand the causes, consequences, and, to the degree this drop in specialty care is harmful, ways to mitigate it.
Acknowledgements
Sponsor’s role
Sponsors of the study had no role in the design, methods, data collection, analysis or preparation of the paper.
Funding
AU: Swiss National Science Foundation Postdoc.Mobility fellowship (P500PM_203170)
AM: National Institute of Mental Health (R01 MH112829)
HAH: National Institute of Mental Health (R01 MH112829)
MLB: National Institute on Aging (R01 AG075507)
Footnotes
Conflict of interest
Authors have no conflict of interests to disclose.
References
- 1.The Future Supply of Long-Term Care Workers in Relation to the Aging Baby Boom Generation | ASPE. https://aspe.hhs.gov/reports/future-supply-long-term-care-workers-relation-aging-baby-boom-generation-0. Accessed June 14, 2022.
- 2.Kaye HS, Harrington C, Laplante MP. Long-term care: Who gets it, who provides it, who pays, and how much? Health Aff. 2010;29(1):11–21. doi: 10.1377/HLTHAFF.2009.0535 [DOI] [PubMed] [Google Scholar]
- 3.Long-term care providers and services users in the United States, 2015–2016. https://stacks.cdc.gov/view/cdc/76253. Accessed June 21, 2022.
- 4.McGarry BE, Grabowski DC, Barnett ML. Severe staffing and personal protective equipment shortages faced by nursing homes during the covid-19 pandemic. Health Aff. 2020;39(10):1812–1821. doi: 10.1377/HLTHAFF.2020.01269 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Geng F, Stevenson DG, Grabowski DC. Daily nursing home staffing levels highly variable, often below CMS expectations. Health Aff. 2019;38(7):1095–1100. doi: 10.1377/HLTHAFF.2018.05322 [DOI] [PubMed] [Google Scholar]
- 6.Levy C, Palat SIT, Kramer AM. Physician Practice Patterns in Nursing Homes. J Am Med Dir Assoc. 2007;8(9):558–567. doi: 10.1016/J.JAMDA.2007.06.015 [DOI] [PubMed] [Google Scholar]
- 7.Orth J, Li Y, Simning A, Temkin-Greener H. Providing Behavioral Health Services in Nursing Homes is Difficult: Findings from a National Survey. J Am Geriatr Soc. 2019;67(8):1713. doi: 10.1111/JGS.16017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Young Y, Barhydt NR, Broderick S, Colello AD, Hannan EL. Factors Associated with Potentially Preventable Hospitalization in Nursing Home Residents in New York State: A Survey of Directors of Nursing. J Am Geriatr Soc. 2010;58(5):901–907. doi: 10.1111/J.1532-5415.2010.02804.X [DOI] [PubMed] [Google Scholar]
- 9.Martinsson G, Fagerberg I, Wiklund-Gustin L, Lindholm C. Specialist prescribing of psychotropic drugs to older persons in Sweden - a register-based study of 188 024 older persons. BMC Psychiatry. 2012;12(1):1–10. doi: 10.1186/1471-244X-12-197 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Nazir A, Smucker WD. Heart Failure in Post-Acute and Long-Term Care: Evidence and Strategies to Improve Transitions, Clinical Care, and Quality of Life. J Am Med Dir Assoc. 2015;16(10):825–831. doi: 10.1016/J.JAMDA.2015.05.006 [DOI] [PubMed] [Google Scholar]
- 11.Heckman GA, Shamji AK, Ladha R, et al. Heart Failure Management in Nursing Homes: A Scoping Literature Review. Can J Cardiol. 2018;34(7):871–880. doi: 10.1016/J.CJCA.2018.04.006 [DOI] [PubMed] [Google Scholar]
- 12.Patel SY, Mehrotra A, Huskamp HA, Uscher-Pines L, Ganguli I, Barnett ML. Trends in Outpatient Care Delivery and Telemedicine During the COVID-19 Pandemic in the US. JAMA Intern Med. 2021;181(3):388–391. doi: 10.1001/JAMAINTERNMED.2020.5928 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Barnett ML, Bitton A, Souza J, Landon BE. Trends in Outpatient Care for Medicare Beneficiaries and Implications for Primary Care, 2000 to 2019. Ann Intern Med. 2021;174(12):1658–1665. doi: 10.7326/M21-1523 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Cassel CK, Reuben DB. Specialization, Subspecialization, and Subsubspecialization in Internal Medicine. N Engl J Med. 2011;364(12):1169–1173. doi: 10.1056/NEJMSB1012647 [DOI] [PubMed] [Google Scholar]
- 15.Clough JD, Patel K, Shrank WH. Variation in Specialty Outpatient Care Patterns in the Medicare Population. J Gen Intern Med. 2016;31(11):1278–1286. doi: 10.1007/S11606-016-3745-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Schulz M, Czwikla J, Tsiasioti C, et al. Differences in medical specialist utilization among older people in need of long-term care - results from German health claims data. Int J Equity Health. 2020;19(1). doi: 10.1186/S12939-020-1130-Z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Shaver NS, Lapenskie J, Smith GA, Hsu AT, Liddy C, Tanuseputro P. How Often, Where, and by Which Specialty Do Long-Term Care Home Residents Receive Specialist Physician Care? A Retrospective Cohort Study. J Appl Gerontol. 2021;40(8):837–846. doi: 10.1177/0733464819901255 [DOI] [PubMed] [Google Scholar]
- 18.Schulz M, Tsiasioti C, Czwikla J, et al. Claims data analysis of medical specialist utilization among nursing home residents and community-dwelling older people. BMC Health Serv Res. 2020;20(1). doi: 10.1186/S12913-020-05548-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Schröder AK, Fassmer AM, Allers K, Hoffmann F. Needs and availability of medical specialists’ and allied health professionals’ visits in German nursing homes: A cross-sectional study of nursing home staff. BMC Health Serv Res. 2020;20(1):1–8. doi: 10.1186/S12913-020-05169-7/FIGURES/3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ganguli I, Wasfy JH, Ferris TG. What Is the Right Number of Clinic Appointments?: Visit Frequency and the Accountable Care Organization. JAMA. 2015;313(19):1905–1906. doi: 10.1001/JAMA.2015.3356 [DOI] [PubMed] [Google Scholar]
- 21.Intrator O, Hiris J, Berg K, Miller SC, Mor V. The residential history file: studying nursing home residents’ long-term care histories(*). Health Serv Res. 2011;46(1 Pt 1):120–137. doi: 10.1111/J.1475-6773.2010.01194.X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Goodwin JS, Li S, Zhou J, Graham JE, Karmarkar A, Ottenbacher K. Comparison of methods to identify long term care nursing home residence with administrative data. BMC Health Serv Res. 2017;17(1). doi: 10.1186/S12913-017-2318-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Harrold LR, Field TS, Gurwitz JH. Knowledge, patterns of care, and outcomes of care for generalists and specialists. J Gen Intern Med 1999 148. 1999;14(8):499–511. doi: 10.1046/J.1525-1497.1999.08168.X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Smetana GW, Landon BE, Bindman AB, et al. A Comparison of Outcomes Resulting From Generalist vs Specialist Care for a Single Discrete Medical Condition: A Systematic Review and Methodologic Critique. Arch Intern Med. 2007;167(1):10–20. doi: 10.1001/ARCHINTE.167.1.10 [DOI] [PubMed] [Google Scholar]
- 25.Chronic Conditions - Chronic Conditions Data Warehouse. https://www2.ccwdata.org/web/guest/condition-categories-chronic. Accessed June 24, 2022.
- 26.Atramont A, Bourdel-Marchasson I, Bonnet-Zamponi D, Tangre I, Fagot-Campagna A, Tuppin P. Impact of nursing home admission on health care use and disease status elderly dependent people one year before and one year after skilled nursing home admission based on 2012–2013 SNIIRAM data. BMC Health Serv Res. 2017;17(1). doi: 10.1186/S12913-017-2620-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ryskina KL, Polsky D, Werner RM. Physicians and Advanced Practitioners Specializing in Nursing Home Care, 2012–2015. JAMA. 2017;318(20):2040–2042. doi: 10.1001/JAMA.2017.13378 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Starfield B, Shi L, Macinko J. Contribution of Primary Care to Health Systems and Health. Milbank Q. 2005;83(3):457–502. doi: 10.1111/J.1468-0009.2005.00409.X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Basu S, Berkowitz SA, Phillips RL, Bitton A, Landon BE, Phillips RS. Association of Primary Care Physician Supply With Population Mortality in the United States, 2005–2015. JAMA Intern Med. 2019;179(4):506–514. doi: 10.1001/JAMAINTERNMED.2018.7624 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Catic AG, Mattison MLP, Bakaev I, Morgan M, Monti SM, Lipsitz L. ECHO-AGE: an innovative model of geriatric care for long-term care residents with dementia and behavioral issues. J Am Med Dir Assoc. 2014;15(12):938–942. doi: 10.1016/J.JAMDA.2014.08.014 [DOI] [PubMed] [Google Scholar]
- 31.Barbour PJ, Arroyo J, High S, Fichera LB, Staska-Pier MM, McMahon MK a. Telehealth for patients with Parkinson’s disease: delivering efficient and sustainable long-term care. Hosp Pract (1995). 2016;44(2):92–97. doi: 10.1080/21548331.2016.1166922 [DOI] [PubMed] [Google Scholar]
- 32.Schneider R, Dorsey ER, Biglan K. Telemedicine Care for Nursing Home Residents with Parkinsonism. J Am Geriatr Soc. 2016;64(1):218–220. doi: 10.1111/JGS.13909 [DOI] [PubMed] [Google Scholar]
- 33.Groom LL, McCarthy MM, Stimpfel AW, Brody AA. Telemedicine and Telehealth in Nursing Homes: An Integrative Review. J Am Med Dir Assoc. 2021;22(9):1784–1801.e7. doi: 10.1016/J.JAMDA.2021.02.037 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Grabowski DC, Aschbrenner KA, Rome VF, Bartels SJ. Quality of mental health care for nursing home residents: A literature review. Med Care Res Rev. 2010;67(6):627–656. doi: 10.1177/1077558710362538 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Grabowski DC, Mitchell SL. Family oversight and the quality of nursing home care for residents with advanced dementia. Med Care. 2009;47(5):568–574. doi: 10.1097/MLR.0B013E318195FCE7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Chou SY. Asymmetric information, ownership and quality of care: an empirical analysis of nursing homes. J Health Econ. 2002;21(2):293–311. doi: 10.1016/S0167-6296(01)00123-0 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1 Codes used to identify patients and specialist visits
Figure S1 Count of specialist visits among the previous specialty care users before and after transition to a nursing home
A – Relative change in the number of specialist visits among the previous users from 12 months before to 12 months after the transition to a nursing home
B – Monthly specialist visits among the previous users of specialty care
Table S2 Continuity of specialty care in residents visiting specialists in the year before and after the transition to a nursing home
Figure S2 Relative change in the number of specialist visits among the previous users after the transition to a nursing home, with different threshold of allowed days in SNF within the year before the transition
Figure S3 Relative change in the number of specialist visits among the previous users in 6 months before to 6 months after the transition to a nursing home, with different definitions of previous care users
Figure S4 Relative change in the number of previous users with a specialist visit in outpatient or inpatient setting from 12 months before to 12 months after the transition to nursing home
Figure S5 Relative change in the number of previous users with a specialist visit before and after the transition to the nursing home, comparing periods of 12 months and 9 months (excluding 6 months around the transition)


