Abstract
Background:
The use of cannabis among older adults is increasing in the United States. While cannabis use has been suggested to help alleviate chronic symptoms experienced by older adults, its potential adverse effects may lead to unintended consequences, including increased acute healthcare utilization related to its use. The objective of this study was to examine trends in cannabis-related emergency department (ED) visits in California.
Methods:
Using data from the Department of Healthcare Access and Information, we conducted a trend analysis of cannabis-related ED visits from all acute care hospitals in California from 2005 to 2019. For each calendar year, we determined the cannabis-related ED visit rate per 100,000 ED visits for adults aged ≥65 utilizing primary or secondary diagnosis codes. We estimated the absolute and relative changes in overall cannabis-related visit rates during the study period and by subgroup, including age (65–74, 75–84, ≥85), race/ethnicity, sex, payer/insurance, Charlson comorbidity index score, and cannabis-related diagnosis code.
Results:
The cannabis-related ED visit rate increased significantly for adults aged ≥65 and all subgroups (p < 0.001). The overall rate increased from 20.7 per 100,000 visits in 2005 to 395.0 per 100,000 ED visits in 2019, a 1804% relative increase. By race/ethnicity, older Black adults had the highest ED visit rate in 2019 and the largest absolute increase while older males had a higher ED visit rate in 2019 and a greater absolute increase than older women. Older adults with a higher Charlson score had a higher ED visit rate in 2019 and a larger absolute increase during the study period.
Conclusion:
Cannabis-related ED visits are increasing among older adults in California and are an adverse effect of cannabis use. Asking about cannabis use and providing education about its use should be a part of routine medical care for older adults.
Keywords: Cannabis, Marijuana, Emergency Department, Substance Use
Introduction
The use of cannabis by older adults increased sharply over the past two decades in the United States (US)1 with the legalization for medical and recreational purposes in many states. While there is limited evidence that cannabis may be helpful for specific conditions,2–3 older adults are increasingly using cannabis to treat a wide range of symptoms and conditions, including recreationally,4 and their perceived risk of regular cannabis use is decreasing.5 However, older adults, due to the physiological changes related to aging, medication use, and increased comorbidity, are at high risk for adverse effects of any psychoactive substance, including cannabis.6–7
Cannabis is associated with a range of acute adverse effects that can require emergency care and detrimental for older adults, who are already the most frequent utilizers of the emergency department (ED).8 Cannabis can slow reaction time and impair attention,9–10 leading to injuries including falls. Cannabis use is also associated with increased risk for psychosis, delirium, paranoia, and other acute psychiatric symptoms.11 The use of cannabis can cause acute physiological changes that can exacerbate cardiovascular and pulmonary diseases.12–15 Additionally, there are potential drug interactions that can lead to adverse effects16 and cannabinoid hyperemesis syndrome is related to cannabis use.17 Many of these complications have resulted in the need for acute clinical care in EDs.18–20
Cannabis-related ED visits have increased in the US, with one study finding a 12.1% average annual increase from 2006 to 2014 in cannabis-associated ED visits.21 This included a sharp increase among adults aged ≥65 who, while having lower overall rates of cannabis-associated ED visits compared to younger adults, had the largest one-year increase from 2017 to 2018 compared to all other age groups.21 A study focused on adults aged ≥50 found that cannabis use increased the likelihood of ED visits due to injury.22 Despite the increase in cannabis use and its potential for adverse effects requiring emergency care in this age group, there has been little research focusing on cannabis-related ED visits among older adults. In 1996, California became the first state in the country to legalize medical cannabis and in 2016 passed Proposition 64, which legalized the use, sale, and cultivation of recreational cannabis.23 We aim to help fill this knowledge gap by examining trends in the rates of cannabis-related ED visits among older adults aged ≥65 and to examine trends among subgroups of older adults in the state of California.
Methods
Study Design and Data Source
This was a retrospective cohort study of adults aged ≥65 using visit-level data from 2005 through 2019 from all non-federal acute care hospitals across the state of California using non-public data from the California Department of Healthcare Access and Information (HCAI). All licensed hospitals in California are subject to mandatory reporting of utilization data in a standardized format to HCAI. The number of hospitals with EDs ranged from 316 to 335 facilities during the study period. Data presented in this study represent unique ED encounters from hospitals providing emergency medical services licensed by the State of California, which were available in two separate non-public HCAI research data sources: Patient Discharge Data (PDD) and Emergency Department and Ambulatory Surgery Data (EDAS). ED encounters resulting in admission to the same hospital are combined with the inpatient record and only reported in the PDD; all other ED encounters are reported in the EDAS. For this study, same-hospital ED admissions from the PDD were combined with ED encounters from the EDAS to construct a complete ED utilization database for analysis including all non-duplicative ED encounters reported to HCAI. Detailed descriptions of these data sources can be found elsewhere.24 This study followed the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) reporting guideline for cross-sectional studies.
Measures
Data consisted of demographic characteristics including age, sex, race/ethnicity, and expected payer as well as up to 25 diagnoses based on the International Classification of Disease (ICD)-9 or 10 Revision Clinical Modification diagnoses codes (diagnosis coding transitioned from ICD-9 to ICD-10 beginning October 1, 2015). Cannabis-related ED visits were defined by any primary or secondary diagnosis of non-dependent abuse or unspecified use, dependence, or poisoning.
Statistical analysis
For each calendar year, we determined the number and rate per 100,000 ED visits for overall cannabis-related ED visits among adults aged ≥65 and estimated trends between 2005–2019. We stratified individual trends of cannabis-related ED visits per 100,000 ED visits by age groups (65–74, 75–84, and ≥85), race/ethnicity (Hispanic/Latino, Non-Hispanic White, Non-Hispanic Black, Non-Hispanic Asian/Pacific Islander, and Non-Hispanic Other), sex (male and female), and payer/insurance (private, Medicare, Medi-Cal the state Medicaid program, self-pay). The Charlson comorbidity index score was calculated with the enhanced coding algorithm provided by Quan et al25 for both ICD-9 and ICD-10 coding and stratified by the following scores: 0, 1, 2, and ≥3. Finally, cannabis diagnoses were divided into three categories: 1. cannabis abuse and unspecified use, 2. cannabis dependence, and 3. poisoning by cannabis, lysergide, and psychodysleptics (which were combined into one category with ICD-9). Linear trend p-values were calculated for the overall trend and across subgroups. Statistical significance was defined as a p-value <0.05 All statistical analyses were conducted with IBM SPSS Statistics (version 27.0; SPSS, Inc, Chicago, IL). This study was approved by UCSD’s Human Research Protections Program.
Results
Cannabis-related ED visits significantly increased in California among adults aged ≥65 from a total of 366 visits in 2005, a rate of 20.7 per 100,000 ED visits to 12,167 visits in 2019; a rate of 395.0 per 100,000 ED visits (Figure 1), which is an absolute increase of 374.3 and a 1808.2% relative increase. Table 1 presents cannabisrelated ED visit trends stratified by patient characteristics. There were significant increases (linear trend p-value <0.001) for all subgroups. By age group, adults aged 65–74 had the highest rate in 2019 (714.5 per 100,000 ED visits) while also having the largest increase in absolute increase compared to adults aged 75–84 and those aged ≥85. Adults aged 75–84, meanwhile had the largest relative percent change with a 2208.3% increase. By race/ethnicity, older Black adults had the highest rate in 2019 (887.5 per 100,000 ED visits) and the largest absolute increase compared to older adults of other races/ethnicities. Older males had a higher ED visit rate in 2019 (598.7 per 100,000 ED visits) compared to older females (235.2 per 100,000 ED visits) although older females had a larger relative percent increase (2375.8% vs. 1531.3%). Older adults without health insurance had the highest rate in 2019 (460.7 per 100,000 ED visits) and the largest absolute (460.3 per 100,000 ED visits) and relative (3099.3%) increases compared to those with health insurance. Older adults with a higher Charlson comorbidity index score also had the highest rate in 2019 (491.2 per 100,000 ED visits) and the largest absolute increase compared to those with lower comorbidity scores; however, those with the lowest comorbidity score had the highest relative increase (2379.2%). Finally, the “cannabis abuse and unspecified use” category comprised nearly all cannabis-related ED visits each year with 369.4 per 100,000 ED visits in 2019 with the largest absolute (350.4 per 100,000 ED visits) and relative (1844.2%) increases compared to the other categories.
Figure 1:
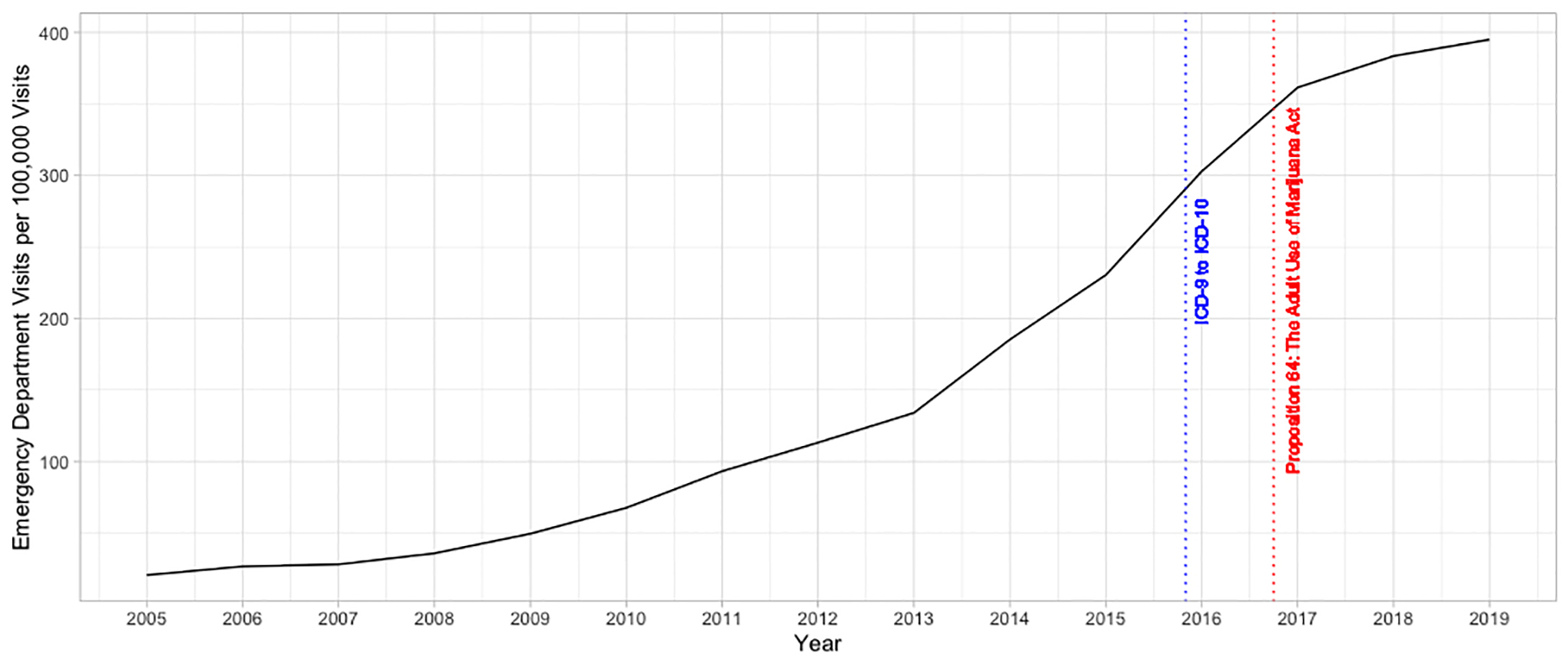
Trend in Cannabis-related Emergency Department visit rate per 100,000 visits among adults aged 65 years and older in California, 2005–2019
Table 1:
Trends in Cannabis-related Emergency Department visit rate per 100,000 visits among adults aged 65 years and older in California overall and by demographics, health insurance, comorbidity, and cannabis diagnosis categories, 2005–2019
| Emergency Department Visits per 100,000 | Change from 2005 to 2019 | ||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 2005 | 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | 2013 | 2014 | 2015a | 2016 | 2017 | 2018 | 2019 | Absolute change | Relative % change | |
| Overall | 20.7 | 26.8 | 28.2 | 35.9 | 49.6 | 67.7 | 93.3 | 111.3 | 134.1 | 185.4 | 230.5 | 302.9 | 361.5 | 383.5 | 395.0 | 374.3 | 1808.2 |
| Age | |||||||||||||||||
| 65–74 | 44.9 | 53.3 | 60.6 | 76.3 | 103.9 | 139.8 | 194.8 | 237.4 | 273.9 | 367.1 | 453.2 | 575.5 | 672.7 | 700.8 | 714.5 | 669.6 | 1491.3 |
| 75–84 | 8.4 | 14.1 | 11.2 | 15.7 | 19.8 | 30.8 | 38.3 | 42.1 | 51.3 | 74.7 | 92.7 | 134.1 | 169.3 | 183.1 | 193.9 | 185.5 | 2208.3 |
| ≥85 | 2.1 | 5.6 | 4.2 | 3.7 | 8.6 | 8.3 | 11.4 | 10.2 | 14.7 | 19.2 | 23.0 | 29.6 | 39.0 | 47.7 | 39.2 | 37.1 | 1766.7 |
| Race/Ethnicity | |||||||||||||||||
| Hispanic or Latino | 15.3 | 25.4 | 19.5 | 26.4 | 36.6 | 39.4 | 57.0 | 65.9 | 76.1 | 92.3 | 114.4 | 155.6 | 183.9 | 206.6 | 195.4 | 180.1 | 1177.1 |
| White | 19.0 | 23.1 | 25.7 | 32.1 | 47.5 | 67.3 | 96.8 | 119.0 | 137.2 | 197.2 | 255.6 | 345.6 | 425.6 | 448.3 | 462.3 | 443.3 | 2333.2 |
| Black | 80.3 | 105.9 | 108.7 | 134.5 | 154.2 | 222.8 | 268.0 | 316.1 | 424.6 | 543.9 | 610.4 | 731.5 | 781.8 | 837.7 | 887.5 | 807.2 | 1005.2 |
| Asian/Pacific Islander | 4.9 | 3.1 | 2.9 | 5.4 | 8.3 | 5.5 | 14.0 | 13.1 | 17.9 | 26.7 | 33.4 | 39.7 | 50.6 | 58.5 | 57.0 | 52.1 | 1063.3 |
| Other | 9.8 | 17.0 | 13.7 | 30.4 | 41.4 | 47.3 | 49.7 | 84.3 | 90.6 | 155.0 | 200.2 | 232.0 | 301.1 | 322.8 | 402.2 | 392.4 | 4004.1 |
| Unknown | 8.9 | 7.8 | 22.2 | 14.3 | 15.7 | 41.9 | 63.5 | 117.2 | 100.8 | 157.8 | 206.5 | 276.9 | 351.6 | 354.1 | 414.0 | 405.1 | 4551.7 |
| Sex | |||||||||||||||||
| Male | 36.7 | 48.8 | 50.8 | 64.2 | 89.0 | 114.8 | 161.1 | 190.5 | 233.5 | 309.6 | 384.7 | 486.6 | 572.2 | 584.4 | 598.7 | 562.0 | 1531.3 |
| Female | 9.5 | 11.3 | 12.4 | 16.0 | 21.8 | 34.0 | 44.6 | 57.6 | 61.2 | 93.5 | 115.0 | 163.8 | 200.2 | 227.6 | 235.2 | 225.7 | 2375.8 |
| Health Insurance | |||||||||||||||||
| Private | 14.5 | 25.3 | 31.4 | 46.9 | 54.1 | 74.9 | 93.4 | 124.5 | 129.1 | 208.8 | 273.1 | 333.0 | 394.6 | 438.2 | 425.4 | 410.9 | 2833.8 |
| Medicare | 21.0 | 26.2 | 26.8 | 32.6 | 46.2 | 64.8 | 91.2 | 109.4 | 132.0 | 180.9 | 226.5 | 298.7 | 357.7 | 378.0 | 391.1 | 370.1 | 1762.4 |
| Medi-Cal | 37.5 | 38.8 | 49.8 | 60.0 | 87.8 | 91.4 | 132.4 | 152.4 | 155.8 | 213.7 | 211.8 | 320.5 | 382.2 | 366.0 | 384.6 | 347.1 | 925.6 |
| Self-Pay | 14.4 | 34.6 | 30.7 | 78.5 | 102.3 | 119.6 | 115.2 | 177.7 | 215.0 | 227.3 | 262.2 | 321.5 | 336.4 | 426.1 | 460.7 | 446.3 | 3099.3 |
| Charlson comorbidity index score | |||||||||||||||||
| 0 | 12.0 | 15.9 | 18.0 | 22.8 | 36.2 | 51.3 | 71.3 | 93.6 | 102.8 | 148.6 | 185.4 | 235.6 | 268.2 | 293.8 | 297.5 | 285.5 | 2379.2 |
| 1 | 28.3 | 34.2 | 33.5 | 40.5 | 51.5 | 74.1 | 105.6 | 119.0 | 148.0 | 202.7 | 259.9 | 307.7 | 369.7 | 375.9 | 407.0 | 378.7 | 1338.2 |
| 2 | 31.7 | 39.9 | 38.8 | 44.0 | 63.6 | 81.9 | 112.2 | 137.0 | 161.4 | 216.7 | 255.9 | 363.9 | 440.3 | 470.2 | 474.0 | 442.3 | 1395.3 |
| ≥3 | 30.9 | 40.1 | 41.6 | 57.3 | 69.1 | 85.1 | 109.9 | 128.7 | 157.5 | 211.2 | 259.5 | 365.9 | 448.9 | 472.0 | 491.2 | 460.3 | 1489.6 |
| Cannabis diagnosis categories | |||||||||||||||||
| Abuse/Use | 19.0 | 24.0 | 24.7 | 31.6 | 43.8 | 59.3 | 81.5 | 96.8 | 116.7 | 164.2 | 208.3 | 277.1 | 339.4 | 356.1 | 369.4 | 350.4 | 1844.2 |
| Dependence | 1.0 | 1.4 | 1.6 | 2.4 | 3.4 | 4.7 | 7.9 | 10.4 | 12.6 | 14.4 | 15.9 | 18.1 | 13.6 | 15.8 | 15.3 | 14.3 | 1430.0 |
| Poisoning b | 0.9 | 1.6 | 2.1 | 2.1 | 2.5 | 4.4 | 4.8 | 7.1 | 5.8 | 8.1 | 7.6 | 9.4 | 10.9 | 14.2 | 13.3 | 12.4 | 1377.8 |
All linear trends p<0.001
Change in ICD-9 to ICD-10 on October 1, 2015
Includes cannabis, lysergide and psychodysleptics
Discussion
Cannabis-related ED visits increased sharply in California among older adults over a 15-year period. While there was a significant increase in cannabis-related ED use among all subgroups of older adults, we identified key subgroups with higher rates and larger increases in cannabis-related ED visits (Figure 2). We found that adults aged 65–74, older males, and those with more comorbidities had higher ED visit rates in 2019, while those with marked relative increases included adults aged 75–84, older females, older adults without health insurance, and those with the lowest comorbidity. Older Black adults had the highest rate of ED visits among all subgroups examined during the study period, consistent with a previous study that showed that among older adults who used cannabis, being Black was associated with an increased likelihood of ED visits.22 While older Black adults had a higher prevalence of cannabis use than other races and ethnicities in the past,26 this gap considerably narrowed. Still, limited information exists on cannabis use patterns among older Black adults and specific risk factors that could influence cannabis-related ED visits. This must be a focus for future studies, given the high ED rates found in this study.
Figure 2:
Infographic on key findings
Our study is consistent with the literature that shows an increase in acute medical services rendered related to cannabis use nationally and in other states over the past two decades.21, 27–28 The few studies focused on older adults examined how cannabis use may be related to injuries or trauma that necessitates ED use22,29 and not overall epidemiological patterns of cannabis-related ED visits. Our findings, in a state with both legalized medical and recreational cannabis use since 2016, show that older adults experienced significant increases in cannabis-related ED visits. Interestingly, the ED rate appeared to increase sharply between 2013 and 2017, but then the rate of increase levels off in 2017 after the implementation of Proposition 64. Therefore, the availability of recreational cannabis does not appear to correlate with a higher rate of increase in cannabis-related ED visits among older people. However, high ED rates among older adults with higher comorbidity are concerning as cannabis has been associated with acute cardiac, respiratory, and psychiatric effects.13–19 It is important to note that our study also found a higher relative increase in cannabis-related ED visits among older adults with the lowest comorbidity, emphasizing that all older adults may be at risk regardless of the presence of chronic diseases. All older adults, therefore, should be asked about cannabis use and have discussions about its use with their clinicians.
This study has several important limitations. First, we acknowledge that our study includes the transition from ICD-9 to ICD-10, which is a limitation for any trend analysis. Given that the current ICD-10 has more specific cannabis-related diagnoses, this may have increased rates of cannabis-related ED visits from 2015 to 2016. Despite this limitation, we felt it was important to include all 15 years to demonstrate changes in the rate of cannabis-related ED visits among all older populations. Furthermore, we utilized several strategies to address this, including keeping cannabis-related diagnoses consistent during the transition and not including ICD-10 codes for the category of “adverse effects of cannabis,” which did not have comparable diagnoses codes in ICD-9. Our sensitivity analysis showed that this cannabis-related category would have made up <2% of the overall cannabis-related ED visit rate, while poisonings or adverse effects of lysergide and psychodysleptics accounted for <0.1%. Additionally, we cannot differentiate the type of cannabis involved, route of use, or distinguish between medical versus recreational use. This study also captured ED visits and not individuals. Further, there is heterogeneity in coding among clinicians, which is inherent in all studies using administrative data. This may also include a reporting bias, as clinicians may have been more aware of the possible role of cannabis in ED presentations later in the study period. Finally, our study is limited to the state of California and does not include Veterans Administration facilities, and results from this study are not generalizable nationally or to other states.
The need for acute medical care is an adverse effect of cannabis use among older adults and is increasing sharply in California. Given the higher risk for adverse effects related to cannabis,6–7 all older adults, regardless of health status, should be regularly asked about their use of cannabis and assessed for problematic use. Despite the currently limited evidence to help balance the risks and benefits of cannabis use,30 clinicians should educate and discuss cannabis use in the context of health as part of routine medical care for older adults. This is also important for patients immediately after an acute episode in the ED, so they are aware that cannabis may have contributed to their visit. While there is great interest among older adults in using cannabis to treat chronic symptoms,4 discussions about the potential health-related harms of cannabis should be had, especially among older adults with multimorbidity.
Key Points:
Cannabis-associated emergency department visits are significantly increasing among older adults aged 65 and older in California.
All older adults should be screened for cannabis use.
Education and discussions with older adults about cannabis use should be included within routine medical care.
Why Does This Matter?
Older adults are at higher risk for adverse health effects associated with psychoactive substances including cannabis.
Acknowledgements
Disclosures:
Sponsor’s Role: Authors receive grant funding from the NIH including NIDA (PI Han: K23DA043651). The funding agency had no role in the study design, methods, interpretation of findings, or preparation of the manuscript. Findings from this paper were presented as an oral presentation at the American Geriatrics Society National Meeting 2022 in Orlando, FL.
Footnotes
Conflict of Interest: The authors have no conflicts.
References
- 1.Han BH, Palamar JJ. Trends in Cannabis Use Among Older Adults in the United States, 2015–2018. JAMA Intern Med. 2020;180(4):609–611. doi: 10.1001/jamainternmed.2019.7517 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Nugent SM, Morasco BJ, O’Neil ME, et al. The Effects of Cannabis Among Adults With Chronic Pain and an Overview of General Harms: A Systematic Review. Ann Intern Med. 2017;167(5):319–331. doi: 10.7326/M17-0155 [DOI] [PubMed] [Google Scholar]
- 3.Whiting PF, Wolff RF, Deshpande S, et al. Cannabinoids for Medical Use: A Systematic Review and Meta-analysis. JAMA. 2015;313(24):2456–2473. doi: 10.1001/jama.2015.6358 [DOI] [PubMed] [Google Scholar]
- 4.Yang KH, Kaufmann CN, Nafsu R, et al. Cannabis: An Emerging Treatment for Common Symptoms in Older Adults. J Am Geriatr Soc. 2021;69(1):91–97. doi: 10.1111/jgs.16833 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Han BH, Funk-White M, Ko R, Al-Rousan T, Palamar JJ. Decreasing perceived risk associated with regular cannabis use among older adults in the United States from 2015 to 2019. J Am Geriatr Soc. 2021;69(9):2591–2597. doi: 10.1111/jgs.17213 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kuerbis A Substance Use among Older Adults: An Update on Prevalence, Etiology, Assessment, and Intervention. Gerontology. 2020;66(3):249–258. doi: 10.1159/000504363 [DOI] [PubMed] [Google Scholar]
- 7.Han BH, Moore AA. Prevention and Screening of Unhealthy Substance Use by Older Adults. Clin Geriatr Med. 2018;34(1):117–129. doi: 10.1016/j.cger.2017.08.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rubin R The Costs of US Emergency Department Visits. JAMA. 2021;325(4):333. doi: 10.1001/jama.2020.26936 [DOI] [PubMed] [Google Scholar]
- 9.McCartney D, Arkell TR, Irwin C, McGregor IS. Determining the magnitude and duration of acute Δ9-tetrahydrocannabinol (Δ9-THC)-induced driving and cognitive impairment: A systematic and meta-analytic review. Neurosci Biobehav Rev. 2021;126:175–193. doi: 10.1016/j.neubiorev.2021.01.003 [DOI] [PubMed] [Google Scholar]
- 10.Boggs DL, Cortes-Briones JA, Surti T, et al. The dose-dependent psychomotor effects of intravenous delta-9-tetrahydrocannabinol (Δ9-THC) in humans. J Psychopharmacol. 2018;32(12):1308–1318. doi: 10.1177/0269881118799953 [DOI] [PubMed] [Google Scholar]
- 11.Moore TH, Zammit S, Lingford-Hughes A, et al. Cannabis use and risk of psychotic or affective mental health outcomes: a systematic review. Lancet. 2007;370(9584):319–328. doi: 10.1016/S0140-6736(07)61162-3 [DOI] [PubMed] [Google Scholar]
- 12.Grotenhermen F Pharmacokinetics and pharmacodynamics of cannabinoids. Clin Pharmacokinet. 2003;42(4):327–360. doi: 10.2165/00003088-200342040-00003 [DOI] [PubMed] [Google Scholar]
- 13.Ashton CH. Pharmacology and effects of cannabis: a brief review. Br J Psychiatry. 2001;178:101–106. doi: 10.1192/bjp.178.2.101 [DOI] [PubMed] [Google Scholar]
- 14.Mittleman MA, Lewis RA, Maclure M, Sherwood JB, Muller JE. Triggering myocardial infarction by marijuana. Circulation. 2001;103(23):2805–2809. doi: 10.1161/01.cir.103.23.2805 [DOI] [PubMed] [Google Scholar]
- 15.Jouanjus E, Lapeyre-Mestre M, Micallef J; French Association of the Regional Abuse and Dependence Monitoring Centres (CEIP-A) Working Group on Cannabis Complications*. Cannabis use: signal of increasing risk of serious cardiovascular disorders. J Am Heart Assoc. 2014;3(2):e000638. Published 2014 Apr 23. doi: 10.1161/JAHA.113.000638 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Antoniou T, Bodkin J, Ho JM. Drug interactions with cannabinoids. CMAJ. 2020;192(9):E206. doi: 10.1503/cmaj.191097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sorensen CJ, DeSanto K, Borgelt L, Phillips KT, Monte AA. Cannabinoid Hyperemesis Syndrome: Diagnosis, Pathophysiology, and Treatment-a Systematic Review. J Med Toxicol. 2017;13(1):71–87. doi: 10.1007/s13181-016-0595-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Roberts BA. Legalized Cannabis in Colorado Emergency Departments: A Cautionary Review of Negative Health and Safety Effects. West J Emerg Med. 2019;20(4):557–572. doi: 10.5811/westjem.2019.4.39935 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Takakuwa KM, Schears RM. The Emergency Department Care of the Cannabis and Synthetic Cannabiniod Patient: A Narrative Review. International Journal of Medicine. 2021,40(10). 10.1186/s12245-021-00330-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hall KE, Monte AA, Chang T, et al. Mental Health-related Emergency Department Visits Associated With Cannabis in Colorado. Acad Emerg Med. 2018;25(5):526–537. doi: 10.1111/acem.13393 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Roehler DR, Hoots BE, Holland KM, Baldwin GT, Vivolo-Kantor AM. Trends and characteristics of cannabis-associated emergency department visits in the United States, 2006–2018. Drug Alcohol Depend. 2022;232:109288. doi: 10.1016/j.drugalcdep.2022.109288 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Choi NG, Marti CN, DiNitto DM, Choi BY. Older adults’ marijuana use, injuries, and emergency department visits. Am J Drug Alcohol Abuse. 2018;44(2):215–223. doi: 10.1080/00952990.2017.1318891 [DOI] [PubMed] [Google Scholar]
- 23.California Department of Cannabis Control. California’s cannabis laws. Available at: https://cannabis.ca.gov/cannabis-laws/laws-and-regulations. Accessed August 1, 2022.
- 24.California Department of Health Care Access and Information. Emergency department encounters. Available at: https://hcai.ca.gov/data-and-reports/healthcare-utilization/emergency-department. Accessed August 1, 2022.
- 25.Quan H, Sundararajan V, Halfon P, et al. Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Med Care. 2005;43:1130–1139. [DOI] [PubMed] [Google Scholar]
- 26.Han BH, Sherman S, Mauro PM, Martins SS, Rotenberg J, Palamar JJ. Demographic trends among older cannabis users in the United States, 2006–13. Addiction. 2017;112(3):516–525. doi: 10.1111/add.13670 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Bollom A, Austrie J, Hirsch W, et al. Emergency Department Burden of Nausea and Vomiting Associated With Cannabis Use Disorder: US Trends From 2006 to 2013. J Clin Gastroenterol. 2018;52(9):778–783. doi: 10.1097/MCG.0000000000000944 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Tolan NV, Terebo T, Chai PR, et al. Impact of marijuana legalization on cannabis-related visits to the emergency department. Clin Toxicol (Phila). 2022;60(5):585–595. doi: 10.1080/15563650.2021.2012576 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lank PM, Crandall ML. Outcomes for older trauma patients in the emergency department screening positive for alcohol, cocaine, or marijuana use. Am J Drug Alcohol Abuse. 2014;40(2):118–124. doi: 10.3109/00952990.2014.880450 [DOI] [PubMed] [Google Scholar]
- 30.Keyhani S, Steigerwald S, Ishida J, et al. Risks and Benefits of Marijuana Use: A National Survey of U.S. Adults. Ann Intern Med. 2018;169(5):282–290. doi: 10.7326/M18-0810 [DOI] [PMC free article] [PubMed] [Google Scholar]


