Purpose of review
Dengue, chikungunya and zika have caused significant epidemics in the Caribbean in recent years. This review highlights their impact in Caribbean children.
Recent findings
Dengue has been increasingly intense and severe, seroprevalence is 80–100% in the Caribbean, children have increased attributable morbidity and mortality. Severe dengue, especially dengue with haemorrhage was significantly associated with haemoglobin SC disease and multiple organ-systems involved. These included the gastrointestinal and haematologic systems with extremely high lactate dehydrogenases and creatinine phosphokinases and severely abnormal bleeding indices. Despite appropriate interventions, mortality was highest within the first 48 h of admission. Chikungunya, a togavirus, affected 80% of some Caribbean populations. Paediatric presentations included high fever, skin, joint and neurological manifestations. Children less than 5 years of age had the highest morbidity and mortality. This maiden chikungunya epidemic was explosive and overwhelmed public health systems. Zika, another flavivirus, has a seroprevalence of 15% in pregnancy, so the Caribbean remains susceptible. Paediatric complications include pregnancy losses, stillbirths, Congenital Zika syndrome, Guillain–Barre syndrome, acute disseminated encephalomyelitis and transverse myelitis. Neurodevelopment stimulation programs for zika-exposed infants have been effective in improving language and positive behaviour scores.
Summary
Caribbean children remain at risk for dengue, chikungunya and zika, with high attributable morbidity and mortality.
Keywords: Caribbean, chikungunya, dengue, Jamaica, zika
INTRODUCTION
Arboviruses have caused multiple epidemics in the Americas including the Caribbean in recent years (Table 1) [1–5]. The WHO listed dengue among the ‘Top Ten Threats to Global Health’ in 2019, when over 3.1 million cases were reported from the region, the highest number ever recorded by the Pan American Health Organisation (PAHO) and WHO, with 28 203 severe cases and 1773 deaths [1,2]. Chikungunya resulted in maiden regional epidemics in 2014–2015 [3,4]. Zika's maiden epidemic resulted in the WHO's declaration of a ‘Public Health Emergency of International Concern’ (PHEIC) in 2016 [5]. All three viruses now co-circulate continually in the region [6]. Arboviral infections result from bites of Aedes aegypti and Aedes albopictus mosquitoes. We report herein on dengue, chikungunya and zika virus infections in Caribbean children.
Table 1.
Dengue, chikungunya and zika infections in Caribbean populationsa
| Country/territory | Total population (2020) [1,2] | Dengue incidence #/100 000 (2019) [3] | Zika incidence #/100 000 (2016) [4] | Chikungunya incidence #/100 000 (2014) [4] |
| Aruba and Bonaire | 107 877 | 1187.38 | 617.54 | 443.1 |
| Antigua and Barbuda | 97 929 | 35.29 | 509.57 | 1604.4 |
| Anguilla | 15 003 | 35.29 | 241.18 | 612.5 |
| Bahamas | 402 365 | 6.7 | 5.60 | 24.4 |
| Barbados | 288 231 | 40.91 | 256.01 | 615.6 |
| Belize | 415 962 | 3485.86 | 224.52 | 0.9 |
| Caribbean Netherlands | 26 223 | 1187.38 | 340.00 | - |
| Cayman Islands | 65 722 | 221.67 | 422.81 | 379.6 |
| Cuba | 11 309 865 | 28.37 | 0.03 | 0 |
| Dominica | 72 422 | 144.54 | 1660.81 | 5154.8 |
| Dominican Republic | 11 118 543 | 194.8 | 49.15 | 5182.5 |
| Grenada | 113 788 | – | 382.88 | 2814.5 |
| Guadeloupe | 400 124 | 719.38 | 6629.30 | 17 517.2 |
| Guyana | 754 144 | 29.41 | 4.80 | 9.5 |
| Haiti | 11 750 245 | 0.84 | 27.29 | 627.2 |
| Jamaica | 2 992 531 | 260.61 | 258.22 | 54.2 |
| Martinique | 375 265 | – | 9265.66 | 556 703.8 |
| Montserrat | 4992 | – | 140.00 | 2380 |
| Puerto Rico | 2 860 853 | 1.01 | 974.46 | 941.2 |
| Sint Maarten (Dutch) | 42 876 | 397.40 | 560.98 | 15 755.1 |
| St Kitts and Nevis | 53 199 | 104.55 | 1119.23 | 1284.3 |
| St Lucia | 183 627 | 11.11 | 531.71 | 541.7 |
| Saint Martin (French) | 38 666 | 812.50 | 9208.33 | 1175.0 |
| St Vincent and Grenadines | 110 940 | 11 | 579.41 | 1352.4 |
| St Barthelemy | 9877 | 122.22 | 11 511.1 | 17 247.2 |
| Suriname | 599 673 | 15.14 | 635.22 | 224.5 |
| Trinidad/Tobago | 1 399 488 | 30.30 | 47.11 | 21.7 |
| Turks and Caicos | 38 717 | 67.86 | 384.31 | 39.6 |
| Virgin Islands (UK) | 104 425 | 278.57 | 11 511.1 | 1231.30 |
| Virgin Islands (USA) | 30 321 | – | 1849.51 | 1620.0 |
| Caribbean | 44 012 651 |
Dominican Republic reported 53 dengue-related deaths. Jamaica recorded 24 dengue-related deaths, for a case fatality rate (CFR) of 0.318. Dengue, Chikungunya, and Zika incidence – are calculated from number of locally transmitted suspected and laboratory confirmed cases per 100 000 population. Suspect Chikungunya cases – are fever more than 38 °C, severe arthralgia, or arthritis, not explained by other medical conditions, occurring within 2 weeks of onset of symptoms. Confirmed chikungunya cases – are suspected cases with CHIKV-specific test confirmed (viral isolation, RT-PCR, IgM, or four-fold increase in CHIKV-specific IgG antibodies). References: Countries in the world by population, as at 8 December, 2022, UN estimates and worldometers. https://www.worldometers.info/world-population/population-by-country/ [accessed 12 December 2022]; About 25% of the population in the Caribbean and Latin America is aged less than 15 years https://www.statista.com/statistics/264683/top-fifty-countries-with-the-highest-population-density/ [accessed 12 December 2022]; Pan American Health Organization/World Health Organization. Epidemiological update: dengue. 7 February 2020, Washington, D.C. PAHO/WHO. 2020; https://bit.ly/314Snw4 [accessed 21 December, 2022]; Caribbean Public Health Agency. State of Public Health in the Caribbean Region 2014–2016. Building resilience to immediate and increasing threats: vector-borne diseases and childhood obesity. Port of Spain, Trinidad, and Tobago: CARPHA; 2017; Case definitions for congenital syndrome associated with Zika virus infection is available at: http://www.paho.org/hq/index.php?option=com_content&view=article&id=11117&Itemid=41532&lang=en; PAHO/WHO Case definitions for suspected and confirmed Zika cases is available at: http://www.paho.org/hq/index.php?option=com_content&view=article&id=11117&Itemid=41532&lang=en.
For years with the highest reported incidence.
Box 1.
no caption available
The Caribbean constitutes over 7000 islands, 44 countries or territories, which are bordered by North, Central and South America and the Caribbean Sea, Atlantic Ocean and the Gulf of Mexico. The Caribbean has 44 012 651 people and represents 0.56% of the world's population (Table 1) [7]. Of these, 74% live in urban settings and 25% are aged less than 15 years [7,8]. Cuba, the Dominican Republic and Haiti's populations each constitute over 11 million (Table 1) [7]. The Caribbean peoples are diverse in their culture, ethnicity and socioeconomic status with a gross national income ranging from $63 370 USD per capita in the Cayman Islands to $1250 USD in Haiti for this tourism-dependent region [9,10]. European-based languages are spoken; these include Spanish (64%), French (25%), English (14%), Dutch and Creoles. The trade winds blow across the region at 10–20 mph creating rainforest tropical climates with the long rainy season from May to October and mean temperatures of 82oC annually. The Caribbean is challenged by climate change, hurricanes and arboviral epidemics [10,11].
DENGUE
Dengue is a flavivirus, with four serotypes. Infection with one serotype increases disease severity with reinfection of subsequent serotypes. Dengue has been causing global epidemics since the 1800s and is now a risk to over half of the world's population. Symptoms develop 4–10 days after the bite of an infected mosquito. It presents as a severe undifferentiated febrile illness in young children, or as ‘nonsevere dengue’, which is a biphasic illness, with ‘no warning signs’ (fever and two of the following – nausea, vomiting, rash, myalgia, leukopenia, positive tourniquet test), or with ‘warning signs’ (severe abdominal pain, persistent vomiting, rapid breathing, bleeding gums, fatigue restlessness and hematemesis) [12]. ‘Severe dengue’ is characterized by plasma leakage, fluid retention, severe bleeding and severe multiorgan impairment, which may lead to death [12].
In the Caribbean, dengue is epidemic, endemic or hyperendemic, and all four serotypes have circulated. The 2018–2019 epidemic was especially severe (Table 1) [13]. During 2009–2011, dengue seroprevalence was 83% (80 –100%) in pregnant women from 10 Caribbean countries: Antigua-Barbuda, Belize, Bermuda, Dominica, Grenada, Jamaica, Montserrat, St. Kitts-Nevis, St. Lucia and St. Vincent-Grenadines [14]. In Barbados, from 2008 to 2016, there were three cyclical epidemics of dengue fever, with prevalence in febrile patients ranging from 27.5 to 453.9 per 100 000 [15]. Dengue was endemic year-round with surges in the rainy season [15]. Among laboratory-confirmed cases, the case fatality rate was 0.4% (10/3994) [15]. In Jamaica, dengue outbreaks have increased in severity, with 5461 dengue-reported cases in 2007, 5903 in 2012 and 10 411 in 2018–2019 [16]. Jamaica's national case fatality rate also increased from 0.46% in 2007, 0.39% in 2012 to 0.83% in 2018–2019 [16]. These mortality rates exceed PAHO's dengue-attributable mortality threshold of 0.05% for the Americas [17].
Children are significantly affected by dengue fever epidemics within the Caribbean [16,17,18▪▪,19–23,24▪]. Jamaica has reported trends of dengue in children over the years [16,18▪▪,19–21,24▪]. During the 2018–2019 epidemic, Jamaican children were most significantly affected with increased attributable morbidity and mortality [16,18▪▪,24▪]. Those under 15 years of age represented 41% of the total reported 10 411 cases and 42% of those who were hospitalized [16]. Jamaica reported 86 deaths during the 2018–2019 dengue epidemic, of which 53 (61.6%) occurred in children less than 15 years [16]. The serotype DENV-3 was circulating during this epidemic.
Lue et al.[18▪▪] conducted a study in 339 children and adolescents aged zero to 15 years with suspected or confirmed dengue who were hospitalized in five hospitals across Jamaica during the 2018–2019 epidemic (Table 2). Of these, 220 (78.9%) had a positive laboratory confirmation with 218 (71.8%) (nonstructural protein) NS1 antigen-positive, 23 (6.8%) dengue reverse transcriptase–polymerase chain reaction (RT-PCR) positive and an overlap of 21 (7.5%) with both RT-PCR and NS1 antigen positive. Using the WHO/PAHO classification of dengue, 68 (20.1%) of the total 339 cases had severe dengue, of which 40 (58.8%) had haemorrhaged. Two hundred and eighteen patients (64.3%) had dengue with warning signs and 53 (15.6%) had dengue without warning signs. Children ages 1–10 years were the most affected – 245 (72.3%). Sickle cell disease genotype, Haemoglobin SC, was associated with severe dengue with haemorrhage (P = 0.005). The most common clinical presentations included fever (99.1%), vomiting (65.8%), headache (54.9%), abdominal pain/loss of appetite/lethargy (53%), diarrhoea (36.3%), arthralgia (33.3%) and rash (28.9%). Three hundred and thirty-four (98.5%) cases had organ-system involvement. The most common organ systems involved were gastrointestinal (93.5%), hematologic (91.7%) and musculoskeletal (53.1%). Those with increasing disease severity had more organ-systems involved with 11.5% having five to seven organ-systems affected.
Table 2.
Age groups, clinical manifestations, abnormal laboratory investigations, and organ-system involvement in children hospitalized during the 2018–2019 dengue epidemic in Jamaica
| Dengue without warning signs (n = 53) | Dengue with warning signs (n = 218) | Severe dengue without haemorrhagic features (n = 28) | Severe dengue with haemorrhagic features (n = 40) | Total (n = 339) | Mortality cases (n = 17) | |
| Age group | Number (%) | Number (%) | Number (%) | Number (%) | TOTAL (%) | Number (%) |
| <1 year | 7 (2.1) | 24 (7.1) | 4 (1.2) | 3 (0.9) | 38 (11.2) | 1 (5.9) |
| 1–5 years | 20 (5.9) | 69 (20.4) | 13 (3.8) | 17 (5.0) | 119 (35.1) | 9 (52.9) |
| 6–10 years | 14 (4.1) | 91 (26.8) | 7 (2.1) | 14 (4.1) | 126 (37.2) | 6 (35.3) |
| 11–15 years | 10 (2.9) | 33 (9.7) | 4 (1.2) | 6 (1.8) | 53 (15.6) | 1 (5.9) |
| Missing data | 2 (0.6) | 1 (0.3) | 0 | 0 | 3 (0.9) | 0 |
| Most common clinical manifestations | Number (%) | Number (%) | Number (%) | Number (%) | Total (%) | Number (%) |
| Fever | 51 (15.0) | 217 (64.0) | 28 (8.3) | 40 (11.8) | 336 (99.1) | 17 (100) |
| Vomiting | 30 (8.8) | 145 (42.8) | 17 (5.0) | 31 (9.1) | 223 (65.8) | 12 (70.6) |
| Headache | 25 (7.4) | 124 (36.6) | 15 (4.4) | 22 (6.5) | 186 (54.9) | 0 |
| Abdominal pain | 10 (2.9) | 124 (36.6) | 21 (6.2) | 27 (8.0) | 182 (53.7) | 10 (58.8) |
| Lethargy | 0 | 137 (40.4) | 17 (5.0) | 26 (7.7) | 180 (53.1) | 14 (82.4) |
| Loss of appetite | 15 (4.4) | 124 (36.6) | 16 (4.7) | 25 (7.4) | 180 (53.1) | 13 (76.5) |
| Diarrhoea | 15 (4.4) | 76 (22.4) | 9 (2.7) | 23 (6.8) | 123 (36.3) | 13 (76.5) |
| Arthralgia | 20 (5.9) | 65 (19.2) | 13 (3.8) | 15 (4.4) | 113 (33.3) | 4 (23.5) |
| Rash | 19 (5.6) | 61 (18.0) | 7 (2.1) | 11 (3.2) | 98 (28.9) | 2 (11.8) |
| Hypotension | 0 | 42 (12.4) | 15 (4.4) | 21 (6.2) | 78 (23) | 11 (64.7) |
| Hepatomegaly | 0 | 38 (11.2) | 12 (3.5) | 20 (5.9) | 70 (20.6) | 10 (58.8) |
| Documented shock | 0 | 0 | 6 (1.8) | 13 (3.8) | 19 (5.6) | 10 (58.8) |
| Laboratory investigations | Number (%) | Number (%) | Number (%) | Number (%) | Total (%) | Number (%) |
| Leukopenia | 22 (6.5) | 124 (36.6) | 14 (4.1) | 9 (2.7) | 169 (49.9) | 3 (17.6) |
| Thrombocytopenia | 34 (10.0) | 187 (55.2) | 26 (7.7) | 36 (10.6) | 283 (83.5) | 15 (88.2)∗ |
| Prolonged PT | 0 | 2 (0.6) | 1 (0.3) | 11 (3.2) | 14 (4.1) | 10 (58.8) |
| Prolonged PTT | 9 (2.7) | 78 (23.0) | 18 (5.3) | 26 (7.7) | 131 (38.6) | 12 (70.6) |
| Elevated AST | 25 (7.4) | 163 (48.1) | 27 (8.0) | 30 (8.8) | 245 (72.3) | 15 (88.2) |
| Elevated ALT | 11 (3.2) | 89 (26.3) | 20 (5.9) | 27 (8.0) | 147 (43.4) | 14 (82.4) |
| Elevated LDH | 15 (4.4) | 106 (31.3) | 18 (5.3) | 25 (7.4)∗∗ | 164 (48.4) | 10 (58.8) |
| Elevated CPK | 7 (2.1) | 49 (14.5) | 10 (2.9) | 18 (5.3)∗∗∗ | 84 (24.8) | 10 (58.8) |
| Organ-systems involved | Number (%) | Number (%) | Number (%) | Number (%) | Total (%) | Number (%) |
| Gastrointestinal | 37 (10.9) | 213 (62.8) | 28 (8.3) | 39 (11.5) | 317 (93.5) | 17 (100) |
| Haematologic | 39 (11.5) | 204 (60.2) | 28 (8.3) | 40 (11.8) | 311 (91.7) | 17 (100) |
| Musculoskeletal | 26 (7.7) | 108 (31.9) | 19 (5.6) | 27 (8.0) | 180 (53.1) | 12 (70.6) |
| Cardiac | 0 | 44 (13.0) | 19 (5.6) | 24 (7.1) | 87 (25.7) | 13 (76.5) |
| Respiratory | 0 | 5 (1.5) | 18 (5.3) | 18 (5.3) | 41 (12.1) | 9 (52.9) |
| Renal | 1 (0.3) | 15 (4.4) | 5 (1.5) | 20 (5.9) | 41 (12.1) | 14 (82.4) |
| Central nervous system | 3 (0.9) | 3 (0.9) | 2 (0.6) | 13 (3.8) | 21 (6.2) | 7 (41.2) |
The P values included in the Table were statistically significant with regards to the abnormal laboratory investigations and severe dengue with haemorrhage/mortality as shown by the asterisks (∗P = 0.003; ∗∗P < 0.001; ∗∗∗P = 0.002). Comparisons were made between groups using Student's t test for normally distributed parametric data. Chi-square analysis, or Fisher's exact test, was used for categorical variables. Continuous variables were analysed using Student's t test. A P value less than 0.05 was considered statistically significant. The ’total’ column represents the sum of the numbers in the rows for ’dengue without warning signs‘, ’dengue with warning signs‘, 'severe dengue without haemorrhage‘, and ‘severe dengue with haemorrhage’. The percentages, except for the age groups, will not add up to 100%. The percentages were calculated as a proportion of the total cases of 339 that were included in the study. Data from Lue et al.[18▪▪].
The most common abnormal haematologic laboratory investigation was thrombocytopenia in 283 (83.5%) subjects and was severe in 125 (36.9%) with platelet count less than 50 × 109/l [18▪▪]. Leucopenia was observed in 169 (49.9%), and prolonged partial thromboplastin time in 131 (38.6%). The most common abnormal biochemical laboratory investigation was elevated aspartate aminotransferase (AST) in 245 (72.3%). A three to ten times increase in the upper limit of normal for age was statistically significant in those with dengue with warning signs (P < 0.001). One hundred and forty-seven (43.4%) had elevated alanine aminotransferase (AST), 164 (48.4%) had elevated lactate dehydrogenase (LDH) and 84 (24.8%) had elevated creatine phosphokinase (CPK), as high as 121 560 U/l. Elevated LDH and CPK were associated with severe dengue with haemorrhage, P = less than 0.001 and 0.002, respectively. Higher levels of biochemical markers were observed in those with increasing disease severity.
Of the total 339 cases, 17 (5%) died [18▪▪]. The ages ranged from 7 months to 15 years. The majority, 16 (94.1%) had severe dengue, of which 15 haemorrhaged. All had hematologic and gastrointestinal involvement, with 11 (64.7%) having five to seven organ-systems involved. The most common clinical presentations in those who died included fever (100%), diarrhoea (76.5%), vomiting (70.6%), hypotension (64.7%), abdominal pain, hepatomegaly and shock in 58.8%. The most common abnormal laboratory investigations included thrombocytopenia (88.2%) with 76.5% noted to be severe (P = 0.003), elevated AST 15 (88.2%), elevated alanine transaminase (ALT) 14 (82.4%), prolonged partial thromboplastin time (70.6%), prolonged prothrombin time/elevated LDH and CPK (58.8%). Eleven of the 17 deaths (64.7%) occurred within 24–48 h of presentation to the hospital, despite receipt of crystalloids, colloids and blood products. Pregnant Jamaican women who were hospitalized with severe dengue during the 2018–2019 epidemic had perinatal outcomes, including pregnancy losses, stillbirths and preterm births [19].
Previous Caribbean studies included a 2016 report from Jamaica on the 2012 epidemic where delayed presentation and short stature were significantly associated with severe dengue [20]. Children with sickle cell disease had longer hospital stays. The case fatality rate was 3.73% and four of the five deaths were using nonsteroidal anti-inflammatory drugs (NSAIDs) [20]. In the same epidemic, Hemoglobin SC genotype was significantly associated with attributable mortality [21]. A Dominican Republic study in 2014 reported severe dengue presenting with rash (P < 0.01), severe thrombocytopenia (P <0.01), anaemia (P < 0.01) and their association with increased mortality [22]. A 2015 study in hospitalized Barbadian children, reported atypical presentations involving the gastrointestinal and respiratory systems, less than 20% had severe dengue and attributable mortality was 1.7% [23].
CHIKUNGUNYA
Chikungunya means ‘that which bends up’ in the Makonde African dialect and was first identified in Tanzania in the early 1950s. This togavirus, primarily of the Asian genotype, was first isolated in the Americas from two autochthonous cases in the Caribbean Island of Martinique in late 2013 with explosive epidemics developing rapidly in the region and over 1.6 million chikungunya cases were reported by October 2015 [3]. The Caribbean was not spared (Table 1) [25–30,31▪▪,32–38]. Anzinger et al.[31▪▪] reported an 83.6% chikungunya seroprevalence in Jamaican antenatal populations. Chikungunya seroprevalence postepidemic ranged from 17 to 79% in Saint Martin, Guadeloupe, Martinique, Puerto Rico and Haiti. After an incubation period of 3–7 days (range 1–12), chikungunya presents abruptly with high fever, rash and arthralgia or arthritis, lasting for weeks, months or years, and maybe recurrent.
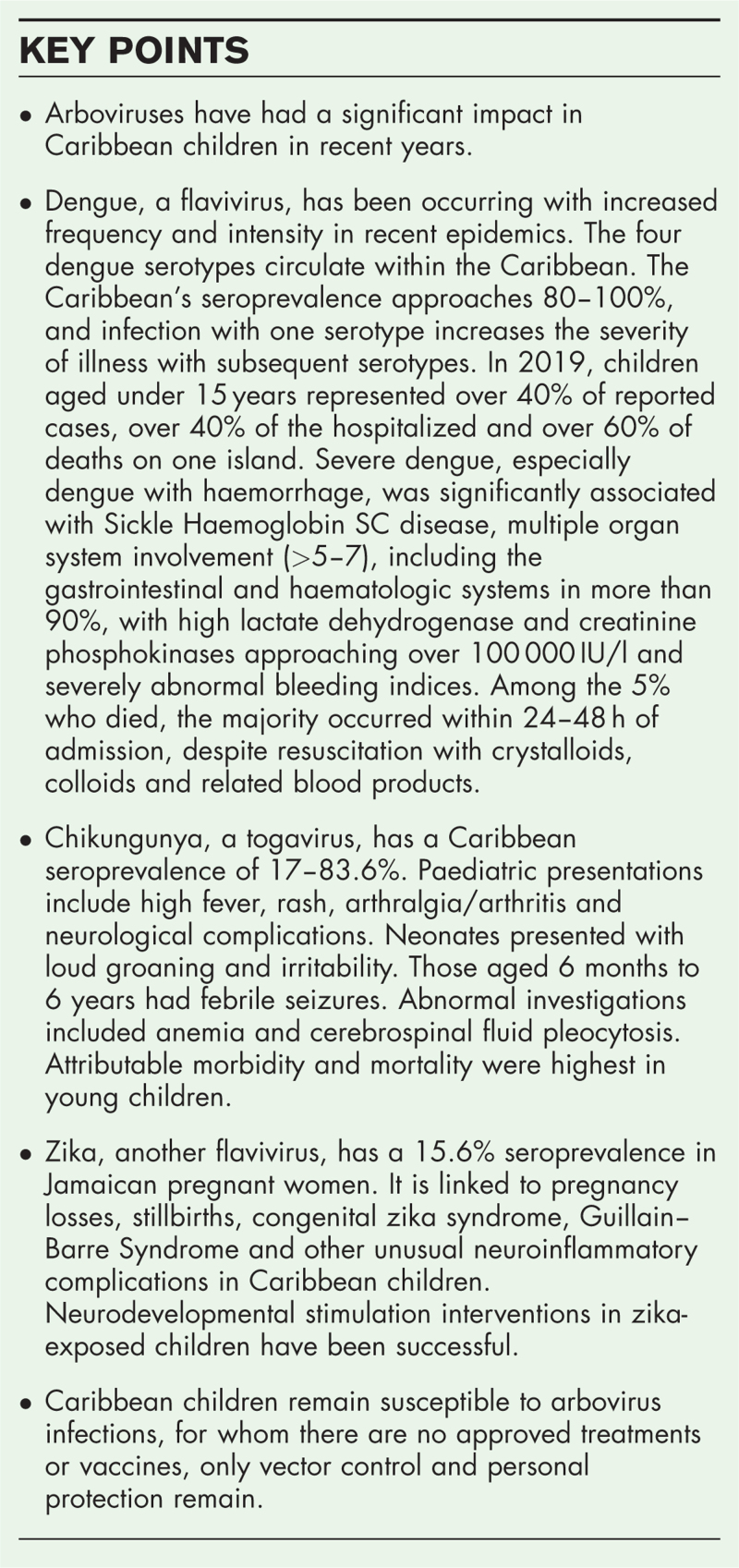
Chikungunya has been described in children from several Caribbean islands [32–38]. In Jamaica, hospitalized children came from households with multiple symptomatic cases and presented with high fever, maculopapular rash, joint pains and varied specific age-related manifestations (Fig. 1) [32]. Newborns (30% of this cohort) had loud groaning and irritability; febrile seizures were evident in those aged 6 months to 6 years, and neurologic involvement occurred in 24%, overall (Fig. 1) [32]. Laboratory anomalies included anaemia and cerebrospinal fluid pleocytosis, few had severe organ-system manifestations, and there were no deaths in this cohort [32]. In Suriname, ambulatory paediatric cases were mild, presenting primarily with headache and vomiting [33]; whereas Barbados described children with primarily joint pains and rash, with less than 10% hospitalized and recovering within 2 weeks [34]. In Puerto Rico, perinatally acquired infection occurred in newborns whose mothers were symptomatic within 5 days of delivery; their presentations included fever, apnoea, poor suck, cyanosis, peripheral oedema, associated with leukopenia, or leukocytosis, thrombocytopenia, elevated hepatic enzymes and prolonged bleeding indices [35]. In Jamaica, mother-to-child transmission of chikungunya presented within 72 h of life with neonatal hypotension, acrocyanosis and respiratory distress, which resulted in death within 24–48 h in two children [36]. Children aged less than 5 years and the elderly had the highest risk for chikungunya morbidity among hospitalized cases in Puerto Rico and excess mortality in Jamaica using data acquired from population-based death certificates [37,38].
FIGURE 1.
Skin and joint manifestations in hospitalized Jamaican children with chikungunya fever key: erythematous patches of the dorsum of the foot and distal lower limb and oedema and erythema of the joints of the left great toe – infant (a), numerous vesicular lesions (early phase) and macular hyperpigmented lesions (late phase) of the abdominal wall – infant (b), hyperpigmented macules on the abdomen – infant (c), bullous lesions of the extensor surface of the lower limbs and denudation and hyperpigmentation of the diaper area – infant (d), arthritis, left second toe, infant (e), desquamation of the skin, infant (f), erythematous papular rash with desquamation of the shoulder – older child (g), erythematous papular rash (h), urticarial rash of the chest and abdomen – older child (i), erythematous maculopapular rash of the chest and abdomen – older child (j).
ZIKA
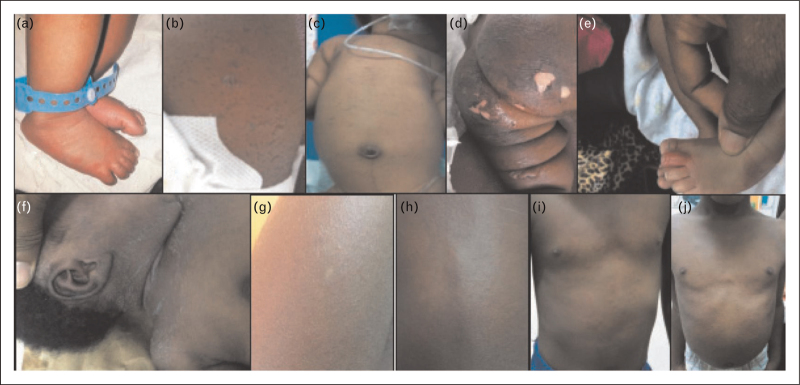
Zika, is another flavivirus whose envelope proteins share a 50% homology with dengue and was isolated in Uganda's ZIKA forest in 1947. Phylogenetic studies confirmed the arrival of the zika virus (ZIKV) in Jamaica, the Dominican Republic and Haiti, over 9 months before the formal identification of the first clinical case [39,40▪▪]. Zika has penetrated the Caribbean region (Table 1) [25,39,40▪▪,41–50,51▪▪,52–54,55▪▪,56–65]. The link of zika to congenital zika syndrome (CZS) and Guillain–Barre syndrome (GBS) has been established in the Caribbean, along with other intrauterine pregnancy complications, febrile illnesses, and unusual neurological complications in children (Figs. 2(a–e) and 3(a and b)) [40▪▪,41–50,51▪▪,52–54,55▪▪,56–65]. In French Guiana, maternofoetal transmission occurred in 26%; among ZIKV-positive foetuses/newborns, 20% had moderate signs, 21% had severe signs of CZS and 14% had foetal loss [44]. In the French territories of the Americas, 5% of ZIKV-positive pregnancies were not carried to term or were stillborn; neurological and ocular defects characteristic of CZS were seen in 7% and microcephaly occurred in 5.8% [45]. A Dominican Republic study reported widespread morbidity and affected pregnancies with 10% foetal losses [46]. In Trinidad and Tobago, antenatal ultrasonography detected brain abnormalities suggestive of CZS in 8% of women infected with ZIKV [47]. Jamaica reported on a new trend of microcephaly and arthrogryposis at three hospitals, during the zika epidemic (Fig. 2a–e) [48]. The Jamaica cohort within the ZIKAction Pediatric Registry reported that 58.5% of children with suspected CZS had congenital microcephaly and 28.3% had severe microcephaly, between June 2016 and October 2019 [49]. Craniofacial disproportion was seen in 37.8%. Among those who had hearing, or ophthalmic evaluation, 55% had abnormal hearing and 25% had abnormal ocular findings.
FIGURE 2.
Panels (a, b, c above) show female infant at age 6 weeks (sucking at mother's breast), showing severe microcephaly, sloping fore-head, facial disproportion with ‘over-sized’ facial features, appearance of proptosis, horizontal nystagmus with bilateral optic atrophy. Infant also displays clenched upper limbs with cortical fisting, diastasis of ‘recti abdomini’ muscles, severe arthrogryposis and ‘rocker bottom’ feet. Panels (d and e, above) reveal infant's MRI of the skull and brain displaying marked microcephaly, collapsed skull bones with extensive scalp folding. There is decreased hemispheric parenchymal volume loss with decreased salvation and evidence of calcification (d). There are septations in the occipital horns of the lateral ventricles as well as evidence of a vermian hypoplasia, in keeping with a Dandy Walker variant. Mother gave signed, written, informed consent with her permission for these photographs to be used for the purposes of medical education, publication and research.
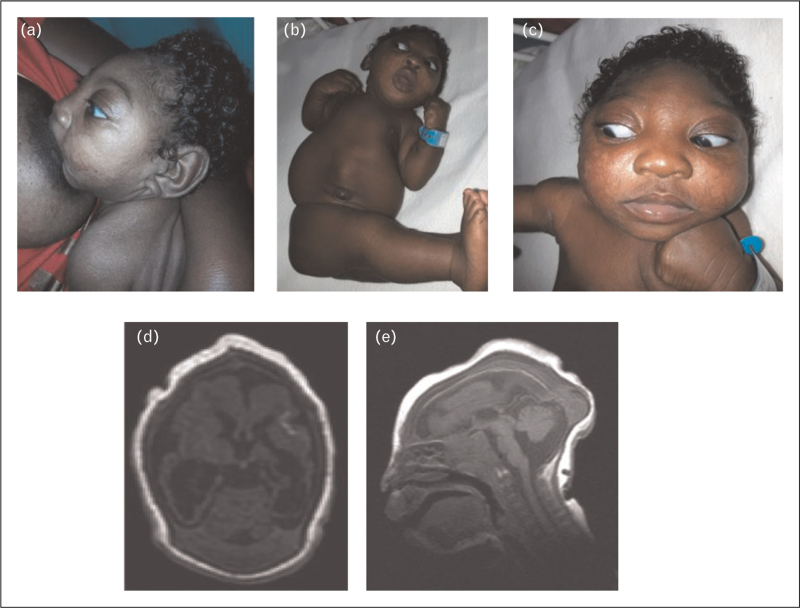
FIGURE 3.
(a) An axial T2 fluid-attenuated inversion recovery (FLAIR) MRI brain showing high signal intensity of the right crus cerebri (yellow arrow). (b) T2-weighted sagittal MRI of the cervical and thoracic spine showing high signal intensity C2 to T4.
Of interest, has been the evidence of teratogenicity and neurodevelopmental outcomes in infants with in-utero exposure to ZIKV without microcephaly or features of CZS at birth [50,51▪▪,52]. In Puerto Rico, a retrospective study of infants born to mothers with confirmed ZIKV infection found ocular findings in 50% of babies with microcephaly and in 31% who are normocephalic [50]. In Grenada, 31% of normocephalic ZIKV-exposed children had deficits in visual acuity and 23% deficits in contrast sensitivity [51▪▪]. Martinique described a ZIKV-exposed infant without microcephaly who had features of a torpedo maculopathy [52]. Developmental delay has been reported as an outcome in some cohorts of normocephalic prenatal ZIKV-exposed children. The French territories cohort showed no significant difference in developmental assessment results in in-utero ZIKV-exposed and unexposed normocephalic toddlers at 24 months of age [53]. In Grenada, normocephalic ZIKV-exposed and unexposed children assessed between 22 and 30 months of age, had no significant difference in scores for cognitive, motor or language development [51▪▪]. In Puerto Rico, lower receptive language scores at ages 3–12 months were documented in normocephalic infants with prenatal ZIKV exposure [53]. Another Puerto Rican study reported a cohort of ZIKV-exposed children, 97.4% of whom were normocephalic at birth, 17.5% failed age-appropriate vision screening and one-third had developmental delay, particularly in the language domain [55▪▪]. Also of concern is an increased prevalence of epilepsy documented in ZIKV-exposed infants in longitudinal Caribbean studies [54,56].
Acute ZIKV infection in Caribbean children has been associated with significant morbidity. In Jamaica, at the height of the ZIKV epidemic, unusual cases of neuroinflammation including acute myelitis, acute disseminated encephalomyelitis and Guillain–Barre syndrome were reported in adolescents (Fig. 3a and b) [57]. In Grenada, ZIKV IgM-positive children with acute neuroinflammation, meningoencephalitis and acute disseminated encephalomyelitis were also reported [58]. In Puerto Rico, children have also been represented in cohorts of Guillain–Barre syndrome associated with acute ZIKV infection [59,60]. Caribbean children now remain at high risk for complications from future zika outbreaks, with low postepidemic seroprevalence rates of 15.8% (using highly specific ZIKV tests) in Jamaican pregnant women, to 42% Martinique and Suriname [31▪▪].
MANAGEMENT
Clinically, these arboviral infections present with fever, rash, joint pains and other systemic symptoms, although the majority are asymptomatic. Dengue is biphasic and the critical phase is complicated with organ-system involvement, haemorrhage and shock in severe cases [18▪▪]. Chikungunya presents with fever, skin, severe arthritis and neurological complications. The postinfectious perinatal, neurological and developmental complications of zika are characteristic.
Local and regional diagnostic laboratories define the temporal circulation of these arboviruses and inform communities and physicians to guide patient care. Diagnosis is first suggested on clinical suspicion (Table 1). Laboratory diagnostics include – viral culture from tissue specimens, RT-PCR and plaque reduction neutralization tests (zika PRNT), antigen tests (dengue NS1 antigen) and serology including immunoglobulin (Ig)G and IgM (Table 1). Laboratory diagnosis is challenging, especially for zika and dengue serology because of their shared homologous envelope proteins. CZS is also challenging to define and link to laboratory-confirmed ZIKV infection and many infants are born to asymptomatic mothers (Table 1). These are ‘Category I Notifiable Medical Conditions’ that require immediate reporting by the most rapid means available to the Public Health Authorities to facilitate investigation, although national public health systems are often overwhelmed in epidemics.
Supportive care is given for all three arboviruses, and there are no known viral cures [66]. Although many Food and Drug Administration (FDA)-approved compounds have shown anti-ZIKV activity. Home treatment for dengue involves ensuring adequate fluid balance with appropriate oral intake, the passage of urine, evaluation for ‘warning signs’ and daily evaluation in an ambulatory clinic, with monitoring of the clinical status and platelet count. Fever is controlled with acetaminophen. NSAIDs and anticoagulants are contraindicated, especially during the thrombocytopenic phase. Children on antihypertensives may manifest hypotension as a sign of increased vascular permeability. Diabetic patients with inadequate hydration may develop osmotic diuresis and shock. Those with ‘warning signs’ should be hospitalized, given intravenous fluids (Lactated Ringer's, or isotonic saline) while ensuring adequate urine output, monitoring the vital signs, fluid and electrolyte balance and haematocrit. Those with severe dengue and circulatory collapse, should receive oxygen and increased boluses of crystalloids; or colloids/fresh frozen plasma, if the haematocrit is rising; or blood, if the haematocrit is falling. Multiple organ system evaluation and ongoing support must be ensured. Chikungunya is supported with bed rest, fluids, analgesics, drugs for tenosynovitis and arthritis, and psychosocial interventions for complications [67]. This maiden chikungunya epidemic overwhelmed Jamaica's healthcare system [32]. Zika is managed with psychosocial support and a multidisciplinary approach, including deferral of pregnancy during epidemics [68]. Intravenous immune gamma globulin and prednisone may be administered for immune-mediated complications.
Caribbean Columbia has documented the deficient psychosocial and economic support, stigma, abandonment or frustration experienced by families whose ZIKV-exposed children are intellectually impaired [69▪]. However, several positive outcomes have been observed in Caribbean neurocognitive intervention programs. In Antigua and Barbuda, St Vincent and in the Grenadines, St Kitts and Dominica, neurodevelopmental stimulation of zika-exposed infants has been successful in improving language and positive behaviors. [70▪▪]. In Grenada, a controlled neurodevelopment stimulation intervention for ZIKV-exposed children who were born with normal head circumference and who were older than 2 years, showed subsequent improved language development and positive behaviors in preparation for school readiness [71▪▪]. Jamaica has documented the usefulness of and adherence to a ZIKApp in pregnancy to identify arbovirus symptoms early in pregnancy to thereby facilitate early diagnosis of infections and maximize maternal care [72▪▪]. The ZIKAction research initiative continues to elucidate these arboviruses in pregnant women, infants and children in Jamaica and Haiti [16,18▪▪,19,31▪▪,32,43,48,49,57,58,61–65,72▪▪].
PREVENTION
There are no WHO/PAHO-approved dengue, chikungunya or zika vaccines for use in the Caribbean, except for the DengvaxiaR vaccine in USA's endemic territories and the French Caribbean, where they are now in clinical trials [73,74]. Killed chikungunya virus vaccines have not yet been licensed and several zika virus vaccines remain under development. Personal prevention with environmental vector surveillance and control measures must be implemented and sustained, including mosquito avoidance behaviors, repellants, larvicides (Abate) and adulticides (Malathion) as recommended by PAHO/WHO and re-emphasized in Jamaica and the US Virgin Islands [24▪,75▪].
The effects of climate change in the Caribbean have been studied for over three decades, using dengue as the model [76–79]. Climate variability with increased rainfall and temperature have contributed to increased dengue transmission and outbreaks, with a shorter life cycle of the domesticated A. aegypti mosquito vector. The vector lives and breeds in settled water around humans, with a major recently observed change in its adaptive behaviour of breeding in underground drains and septic tanks [77]. It is expected that climate change will potentially continue to drive-up the incidence and prevalence of these arbovirus infections, thereby increasing the attributable risks in the vulnerable childhood population of these small island developing states.
CONCLUSION
Dengue, chikungunya and zika arboviral infections have contributed to significant attributable morbidity and mortality in Caribbean children. Given the absence of approved treatments and vaccines in this population, community education and early diagnosis, with supportive clinical care must be administered to improve outcomes. Climate services and health operations, including preventive personal and environmental measures must also be implemented continuously to reduce community exposures to bites of the Aedes spp. mosquito vector, which is endemic in these tropical island rainforests.
Acknowledgements
This project has received funding from the European Union's Horizon 2020 research and Innovation Program under grant agreement No. 734857.
We are grateful to all the collaborators of the ZIKAction Research Initiative and all other Caribbean and international professionals in healthcare who continue to document the impact of Zika, Dengue and Chikungunya in the Caribbean. We hope this review article will be useful in improving the prevention and supportive care of all our Caribbean children and their families who are at risk for arbovirus infections and complications.
Author contributions: C.D.C.C. conceptualized and wrote the manuscript. A.L. wrote the section on the 2018–2019 dengue epidemic in Jamaica. R.M.C. wrote about the neurodevelopmental complications of zika. All co-authors reviewed and approved the final manuscript for publication.
Financial support and sponsorship
This project has received funding from the European Union's Horizon 2020 research and Innovation Program under grant agreement No. 734857.
Conflicts of interest
There are no conflicts of interest.
REFERENCES AND RECOMMENDED READING
Papers of particular interest, published within the annual period of review, have been highlighted as:
▪ of special interest
▪▪ of outstanding interest
REFERENCES
- 1. WHO. Ten Threats to Global Health in 2019. Available at: https://www.who.int/news-room/spotlight/ten-threats-to-global-health-in-2019. [Accessed 21 December 2022] [Google Scholar]
- 2. PAHO. Cases of dengue in the Americas exceeded three million in 2019. Available at: https://www3.paho.org/hq/index.php?option=com_content&view=article&id=15722:cases-of-dengue-in-the-americas-exceeded-3-million-in-2019&Itemid=0&lang=en#gsc.tab=0; published 12 February 2020. [Accessed 21 December 2022] [Google Scholar]
- 3. PAHO. Cases of chikungunya in the Americas exceed 1.6 million by Oct 15 2015. Available at: https://www3.paho.org/hq/index.php?option=com_content&view=article&id=11329 : 2015-millones-casos-chikungunya-americas-desde-2013&Itemid=0&lang=en#gsc.tab=0/ . [Accessed 22 December 2022] [Google Scholar]
- 4. Centers for Disease Control and Prevention. Chikungunya in the Americas. Available at: http://www.cdc.gov/chikungunya/geo/americas.html. [Accessed 22 December 2022] [Google Scholar]
- 5. Chan M. WHO Director-General summarizes the outcome of the Emergency Committee on regarding clusters of microcephaly and Guillain Barre syndrome. 1 February, 2016. Available at: www.who.int/mediacentre/news/statements/2016/emergency-committee-zika-microcephaly/en/. [Accessed 22 December 2022] [Google Scholar]
- 6. PAHO. Epidemiological update: dengue, chikungunya and zika in the context of Covid-19. Published 23 December, 2021. Available at: https://iris.paho.org/handle/10665.2/55639/. [Accessed 21 December 2022] [Google Scholar]
- 7. Countries in the world by population, as 8 December, 2022, UN estimates and worldometers. https://www.worldometers.info/world-population/population-by-country. [Accessed 12 December 2022] [Google Scholar]
- 8. About 25% of the population in the Caribbean and Latin America is aged less than 15 years. Available at: https://www.statista.com/statistics/264683/top-fifty-countries-with-the-highest-population-density. [Accessed 12 December 2022] [Google Scholar]
- 9. Gross national income (GNI) per capita in Latin America and the Caribbean in 2020, by country (in U.S. dollars). Available at: https://www.statista.com/statistics/1066610/gross-national-income-per-capita-latin-america-caribbean. [Accessed 12 December 2022] [Google Scholar]
- 10. Mooney H, Zegarra MA. Extreme Outlier: the pandemic's unprecedented shock to tourism in Latin America and the Caribbean. International-American Development Bank. 2020. Available at: https://publications.iadb.org/en/extreme-outlier-pandemics-unprecedented-shock-tourism-latin-america-and-caribbean. [Accessed 22 December 2022] [Google Scholar]
- 11. Hambleton IR, Selvi M Jeyaseelan, Madhuvanti M, Murphy (2020) COVID-19 in the Caribbean small island developing states: lessons learnt from extreme weather events. Lancet Global Health 8: E1114–E1115. Available at: https://www.thelancet.com/journals/langlo/article/PIIS2214-109X(20)30291-6/fulltext. [Accessed 22 December 2022] [Google Scholar]
- 12.Srikiatkhachorn A, Rothman AL, Gibbons RV, et al. Dengue—how best to classify it. Clin Infect Dis 2011; 53:563–567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Pan American Health Organization/World Health Organization. Epidemiological update: Dengue. 7 February 2020, Washington, D.C. PAHO/WHO. 2020. Available at: https://bit.ly/314Snw4 [Accessed 21 December 2022] [Google Scholar]
- 14.Wood H, Drebot MA, Dewailly E, et al. Seroprevalence of seven zoonotic pathogens in pregnant women from the Caribbean. Am Trop Med Hyg 2014; 91:642–644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Douglas KO, Dutta SK, Martina B, et al. Dengue fever and severe dengue in Barbados, 2008-2016. Trop Med Infect Dis 2020; 5:68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Webster-Kerr K. Trends in dengue: the Jamaican Experience over 40 years. In: Proceedings of the 3rd International ZIKA and Aedes-related International Conference, 2020; 13–16 February 2020; Washington, DC, USA and presented at: ZIKAction 2020. Available at: https://wwwzikaconferencecom/scientific-program. [Accessed 21 December 2022] [Google Scholar]
- 17.dos Santos TH, San Martin JL, Castellanos LG, Espinal MA. Dengue in the Americas: Honduras’ worst outbreak. Lancet 2019; 394:2149. [DOI] [PubMed] [Google Scholar]
- 18▪▪.Lue AM, Richards-Dawson M-AEH, Gordon-Strachan GM, et al. Severity and outcomes of dengue in hospitalized Jamaican children in 2018-2019 during an epidemic surge in the Americas. Front Med 2022; 9:889998. [DOI] [PMC free article] [PubMed] [Google Scholar]; This manuscript describes dengue in hospitalized children during the 2018–2019 epidemic in Jamaica, which disproportionately affected the children in the region and in Jamaica. Hospitalized children had dengue with multiple (5–7) organ systems involved, including gastrointestinal and haematologic systems in more than 90%, with high lactate dehydrogenase and creatinine phosphokinases approaching over 100 000 IU/l and abnormal bleeding indices. Mortality was highest in the first 24–48 h of admission, despite appropriate interventions.
- 19. Archer M, Campbell L. Outcomes of dengue in hospitalized pregnant women and their babies, Victoria Jubilee Maternity Hospital, in Kingston, Jamaica. Poster presentation. Third International ZIKA and Aedes-related Conference, Washington D.C., United States of America, 13–16 February 2020. [Google Scholar]
- 20.Davidson TD, Vickers I, Christie CD. Outcome of dengue in hospitalized Jamaican children. West Indian Med J 2017; 65:442–449. [Google Scholar]
- 21.Rankine-Mullings A, Reid ME, Moo Sang M, et al. A retrospective analysis of the significance of haemoglobin SS and SC in disease outcome in patients with sickle cell disease and dengue fever. EBioMedicine 2015; 2:937–941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Alfredo J, Mena Lora JF, Morales A, et al. Disease severity and mortality caused by dengue in a Dominican pediatric population. Am J Trop Med Hyg 2014; 90:169–172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kumar A, Gittens-St Hilair M, Jason V, et al. The clinical characteristics and outcome of children hospitalized with dengue in Barbados, an English Caribbean country. J Infect Dev Ctries 2015; 9:394–401. [DOI] [PubMed] [Google Scholar]
- 24▪. Webster-Kerr K. Vitals. A Quarterly Report of the Jamaican Ministry of Health. April 2022. Available at: https://www.moh.gov.jm/wp-content/uploads/2022/05/Vitals-April-2022_updated-1.pdf. [Accessed 22 December 2022]. [Google Scholar]; Description of the dengue epidemic from 2018 through 2020 in Jamaica, emphasizing the epidemiology, mitigation, control, and prevention.
- 25. Caribbean Public Health Agency. State of Public Health in the Caribbean Region 2014-2016. Building resilience to immediate and increasing threats: vector-borne diseases and childhood obesity. Port of Spain, Trinidad, and Tobago: CARPHA; 2017. [Google Scholar]
- 26.Dorléans F, Hoen B, Najioullah F, et al. Outbreak of chikungunya in the French Caribbean Islands of Martinique and Guadeloupe: findings from a hospital-based surveillance system (2013–2015). Am J Trop Med Hyg 2018; 98:1819–1825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Mowatt L, Jackson ST. Chikungunya in the Caribbean: an epidemic in the making. Infect Dis Ther 2014; 3:63–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Van Bortel W, Dorleans F, Rosine J, et al. Chikungunya outbreak in the Caribbean region, December 2013 to March 2014, and the significance for Europe. Euro Surveill 2014; 19:ii=20759. [DOI] [PubMed] [Google Scholar]
- 29.Pham PN, Williams LT, Obot U, et al. Epidemiology of Chikungunya fever outbreak in Western Jamaica during July-December 2014. Res Rep Trop Med 2017; 8:7–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Duncan J, Gordon-Johnson KA, Tulloch-Reid MK, et al. Chikungunya: important lessons from the Jamaican experience. Rev Panam Salud Publica 2017; 41:e60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31▪▪.Anzinger JJ, Mears CD, Ades AE, et al. ZIKAction Consortium. Antenatal seroprevalence of zika and chikungunya viruses, Kingston Metropolitan Area, Jamaica, 2017–2019. Emerg Infect Dis 2022; 28:473–475. [DOI] [PMC free article] [PubMed] [Google Scholar]; This article describes seroprevalence in Jamaica from a representative antenatal population of 83.6% for chikungunya, and 15.6% for zika, using highly specific serologic tests (given the 50% homology shared envelope proteins between dengue and zika, with possible false positives with less specific tests).
- 32.Christie CDC, Melbourne-Chambers R, Ennevor J, et al. Chikungunya in Jamaica - public health effects and clinical features in children. West Indian Med J 2016; 65:431–437. [Google Scholar]
- 33.van Genderen FT, Krishnadath I, Sno R, et al. First chikungunya outbreak in Suriname; clinical and epidemiological features. PLoS Negl Trop Dis 2016; 10:e0004625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kumar A, Best C, Benskin G. Epidemiology clinical and laboratory features and course of chikungunya among a cohort of children during the first Caribbean epidemic. J Trop Pediatr 2017; 63:43–49. [DOI] [PubMed] [Google Scholar]
- 35.Rodríguez-Nieves M, García-García I, García-Fragoso L. Perinatally acquired chikungunya infection: the Puerto Rico experience. Pediatr Infect Dis J 2016; 35:1163. [DOI] [PubMed] [Google Scholar]
- 36.Evans-Gilbert T. Chikungunya and neonatal immunity: fatal vertically transmitted chikungunya infection. Am J Trop Med Hyg 2017; 96:913–915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Hsu CH, Cruz-Lopez F, Vargas Torres D, et al. Risk factors for hospitalization of patients with chikungunya virus infection at sentinel hospitals in Puerto Rico. PLoS Negl Trop Dis 2019; 13:e0007084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Freitas ARR, Donalisio MR. Excess deaths associated with the chikungunya epidemic of 2014 in Jamaica were higher among children under 5 and over 40 years of age, an analysis based on official data. Pathog Glob Health 2019; 113:27–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Metsky HC, Matranga CB, Wohl S, et al. Zika virus and spread in the Americas. Nature 2017; 546:411–415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40▪▪.Alam MM, Mavian C, Okech BA, et al. Analysis of zika virus sequence data associated with a school cohort in Haiti. Am J Trop Med Hyg 2022; 107:873–880. [DOI] [PMC free article] [PubMed] [Google Scholar]; Virus sequencing and phylogenetic analysis of zika isolated from school children with acute undifferentiated febrile illness and mosquitoes identified confirmed specific viral clades of zika from as early as 2014 and again in 2016 in Haiti, suggesting this was the earliest isolate identified in the Western hemisphere, and Haiti might have been a point source for zika transmission in the Caribbean.
- 41.Francis L, Hunte SA, Valadere AM, et al. Zika virus outbreak in 19 English and Dutch-speaking Caribbean countries and territories, 2015-2016. Rev Panam Salud Publica 2018; 42:e120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Lednicky J, Beau De Rochars VM, El Badry M, et al. Zika virus outbreak in Haiti in 2014: molecular and clinical data. PLoS Negl Trop Dis 2016; 10:e0004687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Webster-Kerr KR, Christie C, Grant A, et al. Emergence of Zika virus epidemic and the national response in Jamaica. West Indian Med J 2016; 65:243–249. [DOI] [PubMed] [Google Scholar]
- 44.Pomar L, Malinger G, Benoist G, et al. Association between Zika virus and fetopathy: a prospective cohort study in French Guiana. Ultrasound Obstet Gynecol 2017; 49:729–736. [DOI] [PubMed] [Google Scholar]
- 45.Hoen B, Schaub B, Funk A, et al. Pregnancy outcomes after ZIKV infection in French Territories in the Americas. N Engl J Med 2018; 378:985–994. [DOI] [PubMed] [Google Scholar]
- 46.Peña F, Pimentel R, Khosla S, et al. Zika virus epidemic in pregnant women, Dominican Republic, 2016–2017. Emerg Infect Dis 2019; 25:247–255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Sohan K, Cyrus CA. Ultrasonographic observations of the fetal brain in the first 100 pregnant women with Zika virus infection in Trinidad and Tobago. Int J Gynaecol Obstet 2017; 139:278–283. [DOI] [PubMed] [Google Scholar]
- 48.James-Powell T, Brown Y, Christie CD, et al. Trends of microcephaly and severe arthrogryposis in three urban hospitals following the Zika, Chikungunya and Dengue fever epidemics of 2016 in Jamaica. West Indian Med J 2017; 66:10–19. [Google Scholar]
- 49.Ruiz-Burga E, De Siqueira IC, Melbourne-Chambers R, et al. Health outcomes of children born/suspected with Zikv: protocol for the Zikaction Paediatric Registry in Latin America and the Caribbean. J Clin Trials 2021; 11:474. [Google Scholar]
- 50.Gely-Rojas L, García-Fragoso L, Negrón J, et al. Congenital Zika syndrome in Puerto Rico, beyond microcephaly, a multiorgan approach. P R Health Sci J 2018; 37:S73–S76. [PubMed] [Google Scholar]
- 51▪▪.Blackmon K, Evans R, Fernandes M, et al. Neurodevelopment in normocephalic children with and without prenatal Zika virus exposure. Arch Dis Child 2022; 107:244–250. [DOI] [PMC free article] [PubMed] [Google Scholar]; ZIKA-exposed children who were normocephalic had normal neurodevelopment and head growth in the first 2 years of life, although there were selective visual system abnormalities.
- 52.Mesnard C, Benzekri R, Chassery M, et al. Ocular manifestations in Congenital Zika syndrome: about a case of torpedo maculopathy. Am J Ophthalmol Case Rep 2020; 18:100626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Grant R, Fléchelles O, Tressières B, et al. In utero Zika virus exposure and neurodevelopment at 24 months in toddlers normocephalic at birth: a cohort study. BMC Med 2021; 19:12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Valdes V, Zorrilla CD, Gabard-Durnam L, et al. Cognitive development of infants exposed to the Zika Virus in Puerto Rico. JAMA Netw Open 2019; 2:e1914061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55▪▪.Alvarado-Domenech LI, Rivera-Amill V, Appleton AA, et al. Early childhood neurodevelopmental outcomes in children with prenatal zika virus exposure: a cohort study in Puerto Rico. J Pediatr 2022; 247:38.e5–45.e5. [DOI] [PMC free article] [PubMed] [Google Scholar]; Neurodevelopmental abnormalities in zika-exposed children, including optic, audiologic, development, and language impairment suggested evaluation for long-term intellectual impairment to intervene with neurostimulation and optimise cognitive development and school readiness.
- 56.Blackmon K, Waechter R, Landon B, et al. Epilepsy surveillance in normocephalic children with and without prenatal Zika virus exposure. PLoS Negl Trop Dis 2020; 14:e0008874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Melbourne-Chambers R, Christie CD, Greenaway E, Bullock R. Acute paralysis and neuro-inflammation in Jamaican children during Zika virus and Dengue epidemics of 2016. West Indian Med J 2016; 65:425–430. [Google Scholar]
- 58.Nelson B, Melbourne-Chambers R, Christie CDC. Meningo-encephalo-myelitis in children during the zika virus epidemic in Grenada. WIMJ Open 2018; 5:43–46. [Google Scholar]
- 59.Dirlikov E, Medina NA, Major CG, et al. Acute zika virus infection as a risk factor for Guillain-Barré syndrome in Puerto Rico. JAMA 2017; 318:1498–1500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Dirlikov E, Major CG, Medina NA, et al. Clinical features of Guillain-Barré syndrome with vs without zika virus infection, Puerto Rico, 2016. JAMA Neurol 2018; 75:1089–1097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Christie C, Giaquinto C. Unravelling the paediatric and perinatal Zika virus epidemic through population-based research. West Indian Med J 2016; 65:239–242. [DOI] [PubMed] [Google Scholar]
- 62. Christie CD, Thorne C, for the ZIKAction Research Consortium. Overview and preliminary results of the Zika Vertical Transmission Study in Jamaica. Abstract and platform presentation, 3rd International ZIKA and Aedes-related Infections Conference; 13–16 February 2020; Metro Marriott Hotel, Washington DC, United States of America 2020. Available at: https://www.zikaconferencecom/scientific-program// [Accessed 21 December 2022] [Google Scholar]
- 63.Ades AE, Thorne C, Soriano-Arandes A, et al. Researching ZIKA in pregnancy: lessons for global preparedness. Lancet Infect Dis 2020; 20:e61–e68. [DOI] [PubMed] [Google Scholar]
- 64.Ades AE, Brickley EB, Alexander N, et al. ZIKA Consortia Vertical Transmission Study Group. ZIKA virus infection in pregnancy: a protocol for the joint analysis of the prospective cohort studies of the ZIKAlliance, ZIKAPlan and ZIKAction consortia. BMJ Open 2020; 10:e035307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Ades AE, Soriano-Arandes A, Alarcon A, et al. Vertical transmission of Zika virus and its outcomes: a Bayesian synthesis of prospective studies. Lancet Infect Dis 2021; 21:537–545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. PAHO. Dengue Guidelines for Patient Care in the Region of the Americas. Second edition ed. Pan American Health Organization (2016). [Google Scholar]
- 67.Ward CE, Chapman JI. Chikungunya in children: a clinical review. Pediatr Emerg Care 2018; 34:510–515. [DOI] [PubMed] [Google Scholar]
- 68.Dyer O. Jamaica advises women to avoid pregnancy as Zika virus approaches. BMJ 2016; 352:i383. [DOI] [PubMed] [Google Scholar]
- 69▪.Marbán-Castro E, Enguita-Fernàndez C, Romero-Acosta KC, et al. One feels anger to know there is no one to help us!. Perceptions of mothers of children with Zika virus-associated microcephaly in Caribbean Colombia: a qualitative study. PLoS Negl Trop Dis 2022; 16:e0010328. [DOI] [PMC free article] [PubMed] [Google Scholar]; This qualitative study identified psychosocial and economic barriers, stigma, abandonment and frustration of families of ZIKA-exposed children with impaired development and called for local, regional and international commitment to improve and sustain the appropriate healthcare and resources for these children and their families.
- 70▪▪.McNelis K, Prasanphanich N, Martin-Herz SP, et al. Adaptation of Essential Care for Every Baby educational program to improve infant outcomes in the context of Zika. BMC Pediatr 2022; 22:669. [DOI] [PMC free article] [PubMed] [Google Scholar]; This study reported on a neurostimulation intervention for zika-exposed infants in four Caribbean islands to improve neurodevelopmental outcomes.
- 71▪▪.Waechter R, Burgen KS, Punch B, et al. Improving neurodevelopment in Zika-exposed children: a randomized controlled trial. PLoS Negl Trop Dis 2022; 16:e0010263. [DOI] [PMC free article] [PubMed] [Google Scholar]; A neurodevelopment stimulation interventional program for zika-exposed infants improved their language and positive behaviour scores towards optimizing school readiness.
- 72▪▪.Ruiz-Burga E, Bruijning-Verhagen P, Palmer P, et al. the ZIKAction Consortium. Detection of potential arbovirus infections and pregnancy complications in pregnant women in Jamaica Using a Smartphone App (ZIKApp). JMIR Form Res 2022; 6:e34423. [DOI] [PMC free article] [PubMed] [Google Scholar]; This study described the utility of a ZIKAPP in pregnancy to facilitate early identification of arbovirus infections to thereby facilitate early and appropriate interventions.
- 73. Sanofi. FDA Approves DengvaxiaR for the prevention of dengue in individuals ages nine through 16 living in U.S. endemic areas 2019. Available at: http://www.news.sanofi.us/2019-05-01-FDA-approves-Dengvaxia-R-forthe-prevention-of-dengue-in-individuals-ages-9-through-16-living-in-US-endemic-areas. [Accessed 21 December 2022] [Google Scholar]
- 74. Dengue vaccine strategy in children aged nine to 17 years in the French Caribbean (DengueSEA). Available at: https://clinicaltrials.gov/ct2/show/NCT04839757. [Accessed 7 January 2023] [Google Scholar]
- 75▪.Browne AS, Rickless D, Hranac CR, et al. Spatial, sociodemographic, and weather analysis of the zika virus outbreak: U.S. Virgin Islands, January 2016-January 2018. Vector Borne Zoonotic Dis 2022; 22:600–605. [DOI] [PubMed] [Google Scholar]; Tracking sociodemographic and geospatial factors associated with cases of a point source zika epidemic, identified the weather, temperature, and water-related factors and associations to facilitate optimal vector control of this epidemic.
- 76.Stewart-Ibarra AM, Romero M, Hinds AQJ, et al. Co-developing climate services for public health: stakeholder needs and perceptions for the prevention and control of Aedes-transmitted diseases in the Caribbean. PLoS Negl Trop Dis 2019; 13:e0007772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Chadee DD, Martinez R. Aedes aegypti (L.) in Latin American and Caribbean region: with growing evidence for vector adaptation to climate change? Acta Trop 2016; 156:137–143. [DOI] [PubMed] [Google Scholar]
- 78.Méndez-Lázaro P, Muller-Karger FE, Otis D, et al. Assessing climate variability effects on dengue incidence in San Juan, Puerto Rico. Int J Environ Res Public Health 2014; 11:9409–9428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Jury MR. Climate influence on dengue epidemics in Puerto Rico. Int J Environ Health Res 2008; 18:323–334. [DOI] [PubMed] [Google Scholar]