Abstract
BACKGROUND
COVID-19 and diabetes both contribute to large global disease burdens.
PURPOSE
To quantify the prevalence of diabetes in various COVID-19 disease stages and calculate the population attributable fraction (PAF) of diabetes to COVID-19–related severity and mortality.
DATA SOURCES
Systematic review identified 729 studies with 29,874,938 COVID-19 patients.
STUDY SELECTION
Studies detailed the prevalence of diabetes in subjects with known COVID-19 diagnosis and severity.
DATA EXTRACTION
Study information, COVID-19 disease stages, and diabetes prevalence were extracted.
DATA SYNTHESIS
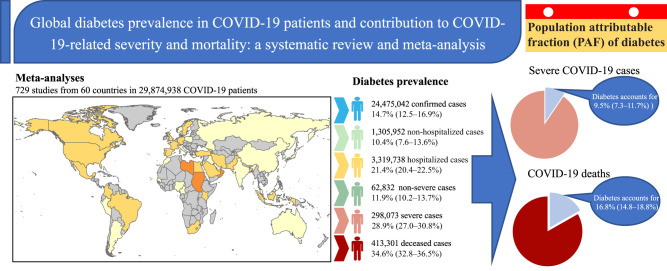
The pooled prevalence of diabetes in stratified COVID-19 groups was 14.7% (95% CI 12.5–16.9) among confirmed cases, 10.4% (7.6–13.6) among nonhospitalized cases, 21.4% (20.4–22.5) among hospitalized cases, 11.9% (10.2–13.7) among nonsevere cases, 28.9% (27.0–30.8) among severe cases, and 34.6% (32.8–36.5) among deceased individuals, respectively. Multivariate metaregression analysis explained 53–83% heterogeneity of the pooled prevalence. Based on a modified version of the comparative risk assessment model, we estimated that the overall PAF of diabetes was 9.5% (7.3–11.7) for the presence of severe disease in COVID-19–infected individuals and 16.8% (14.8–18.8) for COVID-19–related deaths. Subgroup analyses demonstrated that countries with high income levels, high health care access and quality index, and low diabetes disease burden had lower PAF of diabetes contributing to COVID-19 severity and death.
LIMITATIONS
Most studies had a high risk of bias.
CONCLUSIONS
The prevalence of diabetes increases with COVID-19 severity, and diabetes accounts for 9.5% of severe COVID-19 cases and 16.8% of deaths, with disparities according to country income, health care access and quality index, and diabetes disease burden.
Graphical Abstract
Introduction
As of 5 October 2022, the COVID-19 pandemic has infected >619 million people and claimed >6.6 million lives worldwide (1). Barely 1 month after the first reported COVID-19 case in December 2019, diabetes had been identified as a key predictor of poor prognosis in people with COVID-19 (2,3). In various viral pandemics over the past decades, people living with diabetes have consistently demonstrated a markedly greater risk of severe disease outcomes than otherwise. For instance, during the 2003 severe acute respiratory syndrome (SARS) pandemic, diabetes and hyperglycemia were key contributors to SARS-related mortality (4). During the 2009 influenza A (H1N1) pandemic, flu patients with diabetes had a threefold higher risk of hospitalization and a fourfold higher risk of intensive care unit admission than flu patients without diabetes (5). Similarly, during the 2012 Middle East respiratory syndrome coronavirus (MERS-CoV) outbreaks, the infected patients with diabetes demonstrated far more clinical complications and a significantly higher chance of death (6). However, none of these past pandemics achieved a level of global transmission and mortality comparable to that of COVID-19. Despite some having brought global emergencies, these epidemics also were eventually subdued and disappeared. In comparison, COVID-19 is projected to coexist with the human population for a much longer term.
Diabetes is, on its own, a long-existing and significant contributor to the global burden of disease. In 2021, an estimated 537 million individuals (10.5% of the world's adult population) were living with diabetes, and this number is projected to reach 643 million (11.3%) by 2030 and 783 million (12.2%) by 2045 (7). Numerous studies have reported a high prevalence of diabetes among people diagnosed with severe COVID-19 and those who died of COVID-19 (8–11). Most available evidence suggests that the existing diabetic conditions in people with diabetes will significantly increase their risk of COVID-19 disease severity and mortality (12,13). The currently large global burden of disease due to both COVID-19 and diabetes means the overlap of these two epidemics is likely to be a significant public health concern globally. Quantifying the impact of diabetes on the COVID-19 epidemic is crucial for developing intervention strategies for managing COVID-19 to mitigate its disease burden worldwide. However, quantifying the global burden of COVID-19 associated with diabetes is difficult, given the wide regional and economic variations across countries. An empirical prospective cohort study on a global scale to quantify this impact is not practical. Therefore, meta-analyses of diabetes prevalence across various disease stages of COVID-19 may shed light on the impact of diabetes on COVID-19. In particular, we used population attributable fraction (PAF) as an indicator that integrates the prevalence of exposure and relative risk to provide a balanced measure of the likely impact of diabetes on the COVID-19 disease burden (14,15).
In this study, we aim, for the first time, to provide a pooled estimate of diabetes prevalence in different COVID-19 disease stages at the global, regional, and country levels. Based on this, we estimated the PAF of diabetes at each disease stage of COVID-19 progression by using a modified version of the comparative risk assessment (CRA) model.
Methods
Identification and Selection of Qualified Studies
We systematically searched three databases (PubMed, Embase, and Web of Science) to identify peer-reviewed studies published in the English language, up to 24 May 2022, on the prevalence of diabetes in various stratification groups of subjects with COVID-19, such as subjects with confirmed diagnosis of COVID-19 (confirmed) as well as COVID-19 patients who were not hospitalized (nonhospitalized), were hospitalized (hospitalized), had a severity of disease classification of nonsevere (nonsevere), had a severity of disease classification of severe (severe), or had an outcome of death (deceased) (see detailed stratification definitions in Supplementary Material). The search strategy for each database is available in Supplementary Material. The main keywords for the search strategy included “COVID-19,” “SARS-COV-2,” “clinical character*,” “clinical feature*,” “diabet*,” “sugar,” “glycated hemoglobin,” “hyperglyc*,” and “HbA1c.” To supplement the bibliographic database searches and identify additional potential data sources, we scrutinized all relevant meta-analyses identified by our search strategy.
Two authors (R.L. and Q.Y.) independently screened the abstracts of articles retrieved by our searches and reviewed the full texts of potentially eligible studies. Disagreements were resolved through consensus. Studies of any design were eligible, provided that they detailed the prevalence of diabetes in subjects with known COVID-19 diagnosis, severity, or outcomes. The diagnosis of diabetes had to be made by a physician, defined based on measured fasting plasma glucose, oral glucose tolerance test according to World Health Organization (WHO) criteria (16), or HbA1c (17), or self-reported. COVID-19 cases were defined according to WHO criteria of a standard diagnostic flow diagram (18). We first excluded irrelevant studies and meta-analyses, conference abstracts, case series reports, studies without diabetes prevalence data, or studies with a small sample size (<100 confirmed case participants). The flowchart for study selection is shown in Fig. 1. The protocol was registered in the PROSPERO International Prospective Register of systematic reviews (CRD42021265392).
Figure 1.
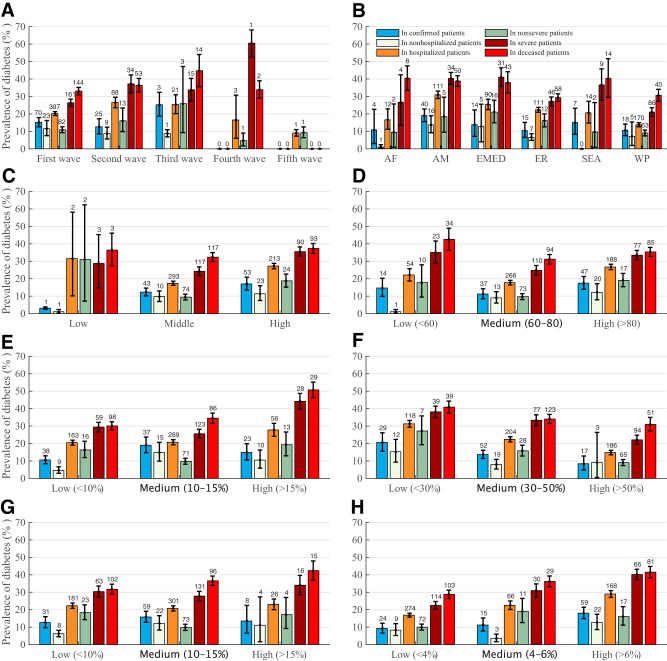
Global prevalence of diabetes by geographical regions and other subgroups for various COVID-19 disease statuses. Prevalence shown by COVID-19 waves (A), WHO geographical regions (B), country income level (C), HAQ (D), diabetes background prevalence (E), undiagnosed diabetes proportion (F), IGT (G), and IFG (H). The color bars denote the prevalence of diabetes for different COVID-19 disease statuses. The error bars represent 95% CI. The figures on the bar are the number of studies for summarizing the pooled prevalence by meta-analysis. AF, Africa region; AM, Americas region; EMED, Eastern Mediterranean region; ER, Europe region; SEA: Southeast Asia region; WP, Western Pacific region.
Data Extraction and Quality Assessment
Two reviewers (R.L. and Q.Y.) used a standardized electronic form to extract the relevant data from the included studies independently. Discrepancies were resolved by consensus between the two reviewers, and a third reviewer (L.Z.) adjudicated the differences if necessary. Variables extracted were study author, publication year, study country, study period, COVID-19 disease status, sample size (the numerators and denominators to compute the prevalence of diabetes), sex, and age. R.L. and Q.Y. contacted the authors of eligible studies to request additional information when the required data could not be extracted from the article. These same reviewers independently appraised within-study bias according to criteria adapted from two published checklists (19,20) (Supplementary Material). L.Z. was consulted to resolve instances of disagreement. We classified studies as having a high risk of bias if scores were lower than seven stars. All other studies were considered to have a low risk of bias.
Meta-analysis of Diabetes Prevalence in Various COVID-19 Disease Stages
We used a random-effects meta-analysis to estimate the overall prevalence of diabetes in COVID-19–positive individuals (21) and applied an arcsine transformation to meet the data normality requirements. The COVID-19 subjects were stratified into six subgroups according to their COVID-19 severity and clinical outcome. Individuals infected by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) were classified as confirmed COVID-19 cases. Some infected individuals would spontaneously recover without a hospital admission and were stratified into the nonhospitalized group. In contrast, infected individuals who were admitted to hospitals were stratified into the hospitalized group. Among the hospitalized individuals, most of them would exhibit mild/moderate symptoms and were stratified into the nonsevere group. The remaining hospitalized individuals who developed dyspnea or required admission to an intensive care unit were stratified into the severe group. The subjects with COVID-related death were stratified into the deceased group. Individual studies usually reported diabetes prevalence in one or several COVID-19 stratification groups or subgroups, and we gathered all the relevant data on diabetes prevalence in these groups/subgroups and reported the pooled values and 95% CI. We also performed sensitivity analyses, including only studies with low risk of bias to assess the robustness of our findings (Supplementary Tables 1–6).
We evaluated between-study heterogeneity using the I2 statistic (22), which estimated the percentage of total variation across studies due to true between-study differences rather than chance. In general, I2 values greater than 60–70% indicate the presence of substantial heterogeneity (23). We used funnel plots and Egger test to detect publication bias. A P value of <0.10 on Egger test was considered indicative of statistically significant publication bias.
Subgroup Analyses and Metaregression
Subgroup analyses were conducted according to COVID-19 pandemic wave (first, second, third, fourth, and fifth; see details in Supplementary Material), WHO geographical regions (Africa, Americas, Eastern Mediterranean, European, Southeast Asia, and Western Pacific), level of country income (low, middle, and high) (24), a country’s health care access and quality index (HAQ) (low, medium, and high) (25), a country’s diabetes disease burden, including diabetes background prevalence (7), undiagnosed diabetes proportion (26), and prediabetes prevalence as determined by the impaired glucose tolerance test (IGT) and/or impaired fasting glucose level (IFG) (7).
Univariable and multivariable metaregression analyses were used to test for the effect of study and participant characteristics (the eight subgroup variables, mean or median age, and proportion of females) on the prevalence estimate. We used stepwise backward manual selection, excluding variables with P > 0.10 (20). For categorical variables, the global P value was considered for inclusion in multivariable models. P < 0.05 was considered statistically significant. Data were analyzed using the meta and metafor packages of the statistical software R, version 4.1.1.
Estimating the PAF of Diabetes for Severe Outcomes of COVID-19
Based on the global pooled prevalence of diabetes in individuals infected with COVID-19 with various levels of severity, we developed a modified version of the comparative risk assessment (CRA) model to estimate PAF of diabetes for greater severity of COVID-19 disease (severe and deceased) (27). The PAF describes the contribution of a risk factor to the burden of disease or death and is expressed as a percentage, which is explained as the reduced proportion of disease burden if the risk factor disappears in the population. The PAF is calculated by two indicators of the relative risk (RR) of disease due to a risk factor and the proportion of the population with the risk factor (P1), PAF = P1(RR-1)/[P1(RR-1) + 1]. Given COVID-19 is an acute infection, we used a modified model to calculate RR of the incidence of severe outcomes in COVID-19 hospitalizations between diabetes patients and patients without diabetes. A detailed description of our methods can be found in Supplementary Material. Using a simulation-based approach, we ran the CRA model to estimate the RR and PAF. These 95% CI generated 10,000 samples in the pooled estimates and applied a triangular distribution. We analyzed PAF of diabetes for worsened outcomes of COVID-19 such as severe severity and COVID-19–related death in all subgroup variables of previous meta-analyses. When possible, we assessed the PAF of diabetes by country. Statistical simulations were done by MATLAB R2021b software.
Results
The Global Prevalence of Diabetes in Individuals With COVID-19 by Disease Stage
A total of 29,874,938 individuals diagnosed with SARS-CoV-2 infection from 60 countries were included in this meta-analysis. Our results demonstrated that the global prevalence of diabetes increased in the groups of individuals with COVID-19 with increasing severity of COVID-19. The pooled prevalence of diabetes was 14.7% (95% CI 12.5–16.9) in the confirmed group, among whom 10.4% (7.6–13.6) of nonhospitalized individuals had diabetes and 21.4% (20.4–22.5) of hospitalized individuals had it. Among hospitalized individuals, the diabetes prevalence was 11.9% (10.2–13.7) in nonsevere COVID-19 patients and 28.9% (27.0–30.8) in severe COVID-19 patients, and 34.6% (32.8–36.5) of deceased COVID-19 patients had diabetes. Heterogeneities were significant in all prevalence estimates (all I2 > 90%). Funnel plots indicated significant publication bias of pooled prevalence in hospitalized (P < 0.01 by Egger test), nonsevere (P < 0.01), severe (P < 0.01), and deceased (P = 0.067) individuals but not in confirmed (P = 0.123) and nonhospitalized (P = 0.650) groups (Table 1).
Table 1.
Global pooled prevalence of diabetes according to COVID-19 disease status
| COVID-19 case type | Pooled prevalence (95% CI) | No. of studies | No. of participants | I 2 | P heterogeneity | P Egger |
|---|---|---|---|---|---|---|
| Confirmed | 14.7% (12.5–16.9) | 100 | 24,475,042 | 1.000 | <0.01 | 0.123 |
| Nonhospitalized | 10.4% (7.6–13.6) | 34 | 1,305,952 | 0.994 | <0.01 | 0.650 |
| Hospitalized | 21.4% (20.4–22.5) | 513 | 3,319,738 | 0.998 | <0.01 | <0.01 |
| Nonsevere | 11.9% (10.2–13.7) | 101 | 62,832 | 0.968 | <0.01 | <0.01 |
| Severe | 28.9% (27.0–30.8) | 216 | 298,073 | 0.992 | <0.01 | <0.01 |
| Deceased | 34.6% (32.8–36.5) | 217 | 413,301 | 0.986 | <0.01 | 0.067 |
Subgroup analyses demonstrated the heterogeneities of the pooled prevalence may originate from temporal and geographical trends, country income, HAQ, and a country’s diabetes disease burden (Supplementary Tables 1–6). Multivariate meta-regression analysis showed that all included variables combined could explain 53–83% of the heterogeneity of the pooled prevalence of diabetes in various COVID-19 stratification groups (Supplementary Tables 7–12).
The Global Prevalence of Diabetes in Individuals With COVID-19 by Temporal and Geographical Trends
When comparing multiple waves of the COVID-19 epidemic globally, the prevalence of diabetes was dynamic and overall increased over time in the confirmed cases with a statistically significant difference (P < 0.01). This trend was similar to that for the pooled prevalence in deceased cases but did not show a significant difference (P = 0.11). COVID-19–infected individuals in the Americas and Eastern Mediterranean had a significantly higher prevalence of diabetes than those in Southeast Asia, Africa, European, and Western Pacific regions (all P < 0.01) (Fig. 1A and B).
Global Prevalence of Diabetes in Individuals With COVID-19 by Country Income and HAQ
Leaving aside low-income countries due to the limited studies, high-income countries had a significantly higher prevalence of diabetes than middle-income countries in each disease stage (all P < 0.01). Likewise, countries with high HAQ also had a significantly higher prevalence than countries with medium HAQ (all P < 0.01). However, countries with low HAQ also had a significantly higher prevalence than countries with medium HAQ (Fig. 1C and D).
Global Prevalence of Diabetes in Individuals With COVID-19 by Country’s Diabetes Disease Burden
Countries with a higher diabetes disease burden always had a higher prevalence of diabetes in individuals with COVID-19. Countries with a high background prevalence of diabetes or prediabetes (IGT or IFG) had a significantly higher prevalence of diabetes than countries with low and medium levels of background prediabetes (most P < 0.01). Moreover, countries with a high proportion of undiagnosed diabetes demonstrated a significantly lower prevalence of diabetes than their low- and medium-level counterparts (all P < 0.01) (Fig. 1E and H).
Global PAF of Diabetes for Presence of Severe Disease and COVID-19–Related Deaths
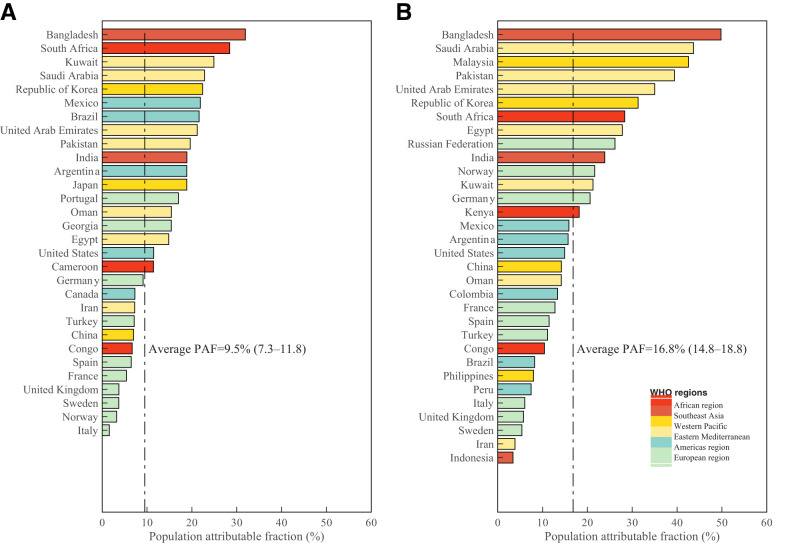
Based on a modified CRA model, we estimated the overall PAF of diabetes to be 9.5% (7.3–11.7) for presence of severe disease in individuals with COVID-19 and 16.8% (14.8–18.8) for COVID-19–related deaths. At the country level, the PAF demonstrated large variations, from 1.6% (−5.5 to 8.7) in Italy to 31.9% (10.4 to 53.5) in Bangladesh, for presence of severe disease and from 3.4% (−21.1 to 27.9) in Indonesia to 49.8% (25.1 to 74.4) in Bangladesh for COVID-19–related deaths (Fig. 2 and Supplementary Tables 13 and 14).
Figure 2.
Estimated PAF of diabetes on presence of severe disease (A) and COVID-19–related deaths (B) in countries from varied geographical regions. The bars denote the PAF in various countries, and the colors represent the various geographical regions. The dashed lines denote the average PAF.
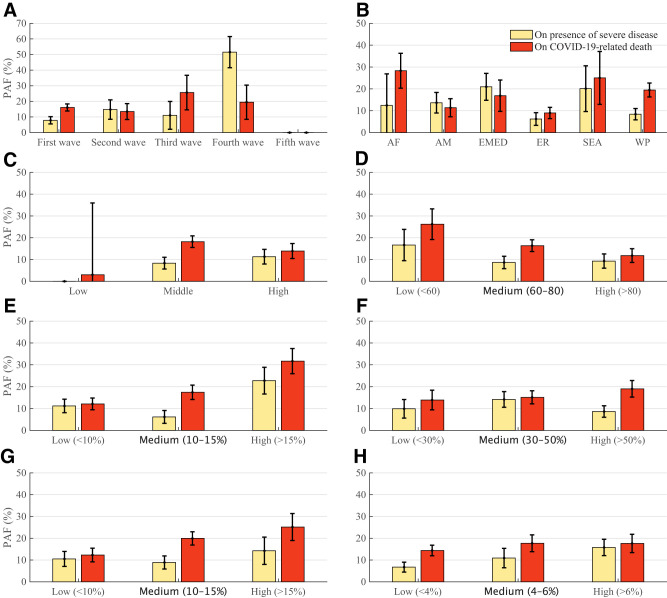
Global PAF of Diabetes in Individuals With COVID-19 by Temporal and Geographical Trends
Subgroup analyses showed that the PAF of diabetes increased with each wave of the COVID-19 epidemic, and the third wave (α dominant) resulted in a higher PAF than the first and second waves (wild strain dominant) (P < 0.01). Although the prevalence of diabetes in the Americas and Eastern Mediterranean regions was higher than that in other regions, the PAF of diabetes was raised in Southeast Asia and Africa regions (Fig. 3A and B) (P < 0.01).
Figure 3.
Estimated PAF of diabetes on presence of severe disease and COVID-19–related deaths by subgroup. PAF shown by COVID-19 waves (A), WHO geographical regions (B), country income level (C), HAQ (D), diabetes background prevalence (E), undiagnosed diabetes proportion (F), IGT (G), and IFG (H). The color bars denote the PAF of diabetes on different worse outcomes of COVID-19 hospitalization. The error bars represent 95% CI. AF, Africa region; AM, Americas region; EMED, Eastern Mediterranean region; ER, Europe region; SEA: Southeast Asia region; WP, Western Pacific region.
Global PAF of Diabetes in Individuals With COVID-19 by Country Income and HAQ
High income and HAQ for a country mean high capacities to reduce the impact of diabetes on the COVID-19 disease burden. Our findings showed that countries with high income and HAQ resulted in lower PAF of diabetes than countries with low and medium income and HAQ (Fig. 3C and D) (P < 0.01).
Global PAF of Diabetes in Individuals With COVID-19 by Country’s Diabetes Disease Burden
A higher diabetes disease burden always contributed more to a country’s COVID-19 disease burden. Countries with high background prevalence of diabetes or prediabetes (IGT or IFG) had a higher PAF of diabetes in individuals with COVID-19 than countries with low and medium prevalence of diabetes (all P < 0.01). Different from the trend of pooled prevalence of diabetes, our finding showed that countries with a high proportion of undiagnosed diabetes also demonstrated a higher PAF of diabetes in individuals with COVID-19 than countries with low and medium proportions of undiagnosed diabetes (P < 0.01).
Conclusions
Our study quantified diabetes prevalence in individuals with COVID-19 and the impact of diabetes on the COVID-19 disease burden. First, our meta-analysis of 729 studies shows that the prevalence of diabetes increases as the severity of COVID increases. In particular, 21.4% of individuals hospitalized with COVID-19 reportedly have diabetes, among whom the diabetes prevalence can be as high as 28.9% in those with severe COVID-19 and even higher (34.6%) in those who died of COVID-19. Notably, this trend is consistent in countries throughout all geographical regions and development statuses. Second, the PAF analysis demonstrated that diabetes contributes to 9.5% of cases with presence of severe disease in individuals with COVID-19 and 16.8% of COVID-19–related deaths. Countries with low HAQ and high diabetes disease burden tended to have higher PAF for adverse outcomes of COVID-19.
Our study demonstrates that the global prevalence of diabetes in severe and deceased individuals with COVID-19 is almost 50% higher than that of all hospitalized individuals. We further demonstrated that diabetes is a major contributing factor for the presence of severe disease in individuals with COVID-19 and COVID-19–related deaths. To the best of our knowledge, this is the first study to quantify the impact of diabetes on the adverse outcomes of COVID-19 at the global level. This finding reinforces the fact that individuals living with diabetes are more likely to progress to severe complications when infected by SARS-CoV-2. Notably, even in the absence of a diabetes diagnosis, hyperglycemia on admission and during hospitalization substantially elevated the risk of progression to severe COVID-19–related complication and mortality (28–30). Although the underlying mechanism of how diabetes interacts with SARS-CoV-2 in the host remains unclear, the complex interplay of inflammation, endothelial dysfunction, and impaired immune modulation due to SARS-CoV-2 infection may contribute to common pathogenic pathways of diabetes and COVID-19. The hyperglycemic environment in patients with diabetes facilitates the proliferation of SARS-CoV-2 (31). Diabetes-induced chronic systemic inflammation and endothelial dysfunction will be exacerbated by the inflammatory responses to the SARS-CoV-2 infection, leading to the microcirculation impairment state. This would result in fatal outcomes such as disseminated intravascular coagulation, thromboembolism, and increased oxidative stress, which leads to multiorgan dysfunction (31,32). In addition, micro- and macrovascular complications of diabetes, such as chronic kidney diseases and cardiovascular diseases, also increase the risk of mortality (31). Therefore, effective glucose control in patients with diabetes is crucial to clinical management to improve the prognosis of SARS-CoV-2 infection.
Our study demonstrates large variations in PAF by country. There are accumulating pieces of evidence that the presence of diabetes could result in more severe complications in individuals infected with SARS-CoV-2 (32,33). In fact, the extent of the impact of diabetes on a country may depend on the level of a country’s economic development, HAQ, and diabetes disease burden. Comprehensive diabetes management and glucose control would also play an important role in reducing the disease burden of diabetes and related mortality of COVID-19 (34).
Our study indicates that the PAF of diabetes to severe COVID-19-related complications is higher in countries with a higher background disease burden of diabetes, both diagnosed and undiagnosed. This finding indicates a potentially masked public health concern in individuals with undiagnosed diabetes when facing the COVID-19 epidemic. Naturally, countries with a higher background diabetes burden would have a higher PAF of diabetes to COVID-19–related complications and mortality. However, the countries with a high proportion of undiagnosed individuals with diabetes, despite a low prevalence of diabetes and prediabetes, could also contribute to a higher PAF to COVID-19–related complications and mortality. This suggests that early diabetes diagnosis plays an important role in reducing the COVID-19 disease burden. In fact, given the long asymptomatic duration of diabetes development, most individuals living with diabetes may not be aware of their condition until symptoms become obvious. Timely diagnosis, together with effective glucose control after diagnosis, may prevent COVID-19–related adverse outcomes at the population level (32,35). Notably, 87.5% of individuals with undiagnosed diabetes lived in low- and middle-income countries where health care resources are strained by the current COVID-19 pandemic (7). These high undiagnosed rates likely contribute to the high COVID-19 severity in these countries.
Our study indicates that the PAF of diabetes is lower in countries with better economic development and higher HAQ. It seems comprehensible that countries with high income and HAQ have better public health resources for diabetes management than resource-limited countries to reduce the impact of diabetes on COVID-19 (34,36). Despite countries with high income and HAQ generally having a high prevalence of diabetes and prediabetes, the PAF of diabetes to severe COVID-19 remains substantially lower than that in low-income and low-HAQ ones. This finding is likely because more diabetes screening and better diabetes control are readily available in high-income and high-HAQ countries (proportion of undiagnosed diabetes <30%) (7). In contrast, low diabetes prevalence in low- and middle-income countries may not represent the actual disease burden of diabetes due to a high proportion of undiagnosed diabetes. Consistently, our findings report a lower prevalence of diabetes in individuals with COVID-19 in low- and middle-income countries but higher PAF of diabetes than otherwise.
Our study has several limitations. First, we included 729 studies, among which 408 (56%) had a high risk of bias. This risk of bias might have affected the precision of our estimate; nevertheless, when pooling only the 321 (44%) studies that had a low risk of bias in a meta-analysis, most of our estimates of prevalence of diabetes did not change considerably (14.7% vs. 16.4%, 10.4% vs. 12.7%, 21.4% vs. 23.2%, 11.9% vs. 14.7%, 28.9% vs. 32.4%, and 34.6% vs. 35.9%). Second, most studies provided the available numerators and denominators of diabetes prevalence in hospitalized patients (70%), and the data were rare for nonhospitalized patients (5%). A small number of included studies may not eliminate the random variation of pooled estimates, which, fortunately, somehow can be overcome by the large sample size. Furthermore, a large number of studies included were from China (27%) and the U.S. (15%), which could affect the generalizability of our findings. Third, our meta-analyses also found significant heterogeneity among studies. We used random-effects models that allow for real differences between individual studies and undertook a metaregression analysis, which explained more than half of this heterogeneity. Fourth, apart from diabetes, other comorbidities, such as hypertension and coronary heart disease, may also influence COVID-19 disease progression outcomes, and further population studies are necessary to identify the confounding effects brought by these comorbidities. Fifth, our search strategy only included articles that specifically mentioned diabetes in the title or abstract. This may miss some studies that reported diabetes prevalence in COVID-19 patients. Sixth, in our study, data from high-income countries, in general, are better represented than data from low-income countries, potentially leading to a publication bias. Seventh, our CRA model assumed the time to progress to COVID-19 severity was similar in individuals with and without diabetes, and this may underestimate the relative risk and PAF and, hence, lead to more conservative conclusions. Finally, our CRA model assumed that all severe COVID-19 outcomes were from hospitalized patients to simplify the estimates of PAF, which could lead to an underestimate of the PAF due to some individuals with severe COVID-19 cases not being admitted to the hospitals.
In conclusion, our study demonstrates that the global prevalence of diabetes is associated with the severity of COVID-19 disease. Further, we are the first to report global estimates of PAF of diabetes contributing to 9.5% of severe COVID-19 cases and 16.8% of COVID-19–related deaths. A high population prevalence of diabetes and prediabetes may be a public health concern during the COVID epidemic. A strategy of sufficient diabetes screening in the community and optimal glucose control for those with diabetes should be effective to prevent COVID-19–related severity and mortality.
Article Information
Funding. This work was supported by the Bill & Melinda Gates Foundation (INV-006104). L.Z. was supported by the National Natural Science Foundation of China (grant number 81950410639), Outstanding Young Scholars Funding (grant number 3111500001), Xi'an Jiaotong University Basic Research and Profession Grant (grant numbers xtr022019003 and xzy032020032), and Xi'an Jiaotong University Young Talent Support Grant (grant number YX6J004). M.S. was supported by the National Natural Science Foundation of China (grant number 12171387), China Postdoctoral Science Foundation (grant number 2018M631134, 2020T130095ZX), and Young Talent Support Program of Shaanxi University Association for Science and Technology (grant number 20210307).
Duality of Interest. No potential conflicts of interest relevant to this article were reported.
Author Contributions. L.Z. and R.L. conceived the study. R.L. and Q.Y. acquired the data. R.L., Q.Y., H.L., L.P., Z.Z., L.Z., and H.S. analyzed and interpreted the data. R.L. drafted the initial manuscript. L.Z., G.Z., M.S., F.C., Z.C., M.R., O.J., and W.H. critically revised the manuscript. All authors reviewed the manuscript and approved the final version.
Footnotes
This article contains supplementary material online at https://doi.org/10.2337/figshare.21965333.
This article is part of a special article collection available at diabetesjournals.org/journals/collection/52/Diabetes-and-COVID-19.
References
- 1. Johns Hopkins University . Coronavirus Resource Center: COVID-19 Tracking. Accessed 26 August 2022. Available from https://coronavirus.jhu.edu
- 2. Khan MMA, Khan MN, Mustagir MG, Rana J, Islam MS, Kabir MI. Effects of underlying morbidities on the occurrence of deaths in COVID-19 patients: a systematic review and meta-analysis. J Glob Health 2020;10:020503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Huang C, Wang Y, Li X, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 2020;395:497–506 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Yang JK, Feng Y, Yuan MY, et al. Plasma glucose levels and diabetes are independent predictors for mortality and morbidity in patients with SARS. Diabet Med 2006;23:623–628 [DOI] [PubMed] [Google Scholar]
- 5. Allard R, Leclerc P, Tremblay C, Tannenbaum TN. Diabetes and the severity of pandemic influenza A (H1N1) infection. Diabetes Care 2010;33:1491–1493 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Alanazi KH, Abedi GR, Midgley CM, et al. Diabetes mellitus, hypertension, and death among 32 patients with MERS-CoV infection, Saudi Arabia. Emerg Infect Dis 2020;26:166–168 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. International Diabetes Foundation . IDF Diabetes Atlas, 10th edition. Brussels, Belgium, International Diabetes Foundation, 2021. Accessed 23 July 2022. Available from https://www.diabetesatlas.org
- 8. Singh AK, Gillies CL, Singh R, et al. Prevalence of co-morbidities and their association with mortality in patients with COVID-19: a systematic review and meta-analysis. Diabetes Obes Metab 2020;22:1915–1924 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Shi Q, Zhang X, Jiang F, et al. Clinical characteristics and risk factors for mortality of COVID-19 patients with diabetes in Wuhan, China: a two-center, retrospective study. Diabetes Care 2020;43:1382–1391 [DOI] [PubMed] [Google Scholar]
- 10. Cariou B, Hadjadj S, Wargny M, et al.; CORONADO investigators . Phenotypic characteristics and prognosis of inpatients with COVID-19 and diabetes: the CORONADO study. Diabetologia 2020;63:1500–1515 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Bradley SA, Banach M, Alvarado N, Smokovski I, Bhaskar SMM. Prevalence and impact of diabetes in hospitalized COVID-19 patients: a systematic review and meta-analysis. J Diabetes 2022;14:144–157 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Singh AK, Khunti K. COVID-19 and diabetes. Annu Rev Med 2022;73:129–147 [DOI] [PubMed] [Google Scholar]
- 13. Ma RCW, Holt RIG. COVID-19 and diabetes. Diabet Med 2020;37:723–725 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Rockhill B, Newman B, Weinberg C. Use and misuse of population attributable fractions. Am J Public Health 1998;88:15–19 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Brooks-Pollock E, Danon L. Defining the population attributable fraction for infectious diseases. Int J Epidemiol 2017;46:976–982 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. WHO . Definition and Diagnosis of Diabetes Mellitus and Intermediate Hyperglycaemia: Report of a WHO/IDF Consultation. 2006. Available from https://apps.who.int/iris/handle/10665/43588. Accessed 29 November 2021
- 17. American Diabetes Association . Diagnosis and classification of diabetes mellitus. Diabetes Care 2012;35(Suppl. 1):S64–S71 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. WHO . Diagnostic Testing for SARS-CoV-2. 2020. Available from https://www.who.int/publications/i/item/diagnostic-testing-for-sars-cov-2. Accessed 29 November 2021 [DOI] [PMC free article] [PubMed]
- 19. Hoy D, Brooks P, Woolf A, et al. Assessing risk of bias in prevalence studies: modification of an existing tool and evidence of interrater agreement. J Clin Epidemiol 2012;65:934–939 [DOI] [PubMed] [Google Scholar]
- 20. Noubiap JJ, Nansseu JR, Nyaga UF, et al. Global prevalence of diabetes in active tuberculosis: a systematic review and meta-analysis of data from 2.3 million patients with tuberculosis. Lancet Glob Health 2019;7:e448–e460 [DOI] [PubMed] [Google Scholar]
- 21. Barendregt JJ, Doi SA, Lee YY, Norman RE, Vos T. Meta-analysis of prevalence. J Epidemiol Community Health 2013;67:974–978 [DOI] [PubMed] [Google Scholar]
- 22. Cochran WG. The combination of estimates from different experiments. Biometrics 1954;10:101–129 [Google Scholar]
- 23. Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med 2002;21:1539–1558 [DOI] [PubMed] [Google Scholar]
- 24. Bank TW. World Bank country and lending groups. Washington, DC, World Bank, 2020. Accessed 23 July 2022. Available from https://datahelpdesk.worldbank.org/knowledgebase/articles/906519-world-bank-country-and-lending-groups
- 25. GBD 2015 Healthcare Access and Quality Collaborators . Healthcare access and quality index based on mortality from causes amenable to personal health care in 195 countries and territories, 1990-2015: a novel analysis from the Global Burden of Disease Study 2015. Lancet 2017;390:231–266 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Ogurtsova K, Guariguata L, Barengo NC, et al. IDF Diabetes Atlas: global estimates of undiagnosed diabetes in adults for 2021. Diabetes Res Clin Pract 2022;183:109118. [DOI] [PubMed] [Google Scholar]
- 27. GBD 2019 Risk Factors Collaborators . Global burden of 87 risk factors in 204 countries and territories, 1990-2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet 2020;396:1223–1249 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Wang W, Shen M, Tao Y, et al. Elevated glucose level leads to rapid COVID-19 progression and high fatality. BMC Pulm Med 2021;21:64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Wang W, Chai Z, Cooper ME, et al. High fasting blood glucose level with unknown prior history of diabetes is associated with high risk of severe adverse COVID-19 outcome. Front Endocrinol (Lausanne) 2021;12:791476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Wang S, Ma P, Zhang S, et al. Fasting blood glucose at admission is an independent predictor for 28-day mortality in patients with COVID-19 without previous diagnosis of diabetes: a multi-centre retrospective study. Diabetologia 2020;63:2102–2111 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Lim S, Bae JH, Kwon HS, Nauck MA. COVID-19 and diabetes mellitus: from pathophysiology to clinical management. Nat Rev Endocrinol 2021;17:11–30 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Kazakou P, Lambadiari V, Ikonomidis I, et al. Diabetes and COVID-19; a bidirectional interplay. Front Endocrinol (Lausanne) 2022;13:780663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Bloomgarden ZT. Diabetes and COVID-19. J Diabetes 2020;12:347–348 [DOI] [PubMed] [Google Scholar]
- 34. Ojeda-Fernández L, Foresta A, Macaluso G, et al. Metformin use is associated with a decrease in the risk of hospitalization and mortality in COVID-19 patients with diabetes: a population-based study in Lombardy. Diabetes Obes Metab 2022;24:891–898 [DOI] [PubMed] [Google Scholar]
- 35. The Lancet Diabetes Endocrinology . COVID-19 and diabetes: a co-conspiracy? Lancet Diabetes Endocrinol 2020;8:801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Ganesh A, Randall MD. Does metformin affect outcomes in COVID-19 patients with new or pre-existing diabetes mellitus? A systematic review and meta-analysis. Br J Clin Pharmacol 2022;88:2642–2656 [DOI] [PMC free article] [PubMed] [Google Scholar]