Abstract
Branchial anomalies are heterogeneous congenital malformations that form secondary to incomplete closure of pharyngeal clefts and pouches. There have been no reports of branchial cleft cysts causing carotid artery compression and hypertension. We report a large branchial cleft cyst causing suspected secondary hypertension from carotid artery compression.
Keywords: branchial cleft cyst, carotid artery, hypertension, secondary hypertension
Branchial anomalies are congenital malformations that form secondary to incomplete closure of pharyngeal clefts and pouches. We report a large branchial cleft cyst causing suspected secondary hypertension from carotid artery compression.
1. INTRODUCTION
Branchial structures are heterogeneous congenital malformations that form secondary to incomplete closure of pharyngeal clefts and pouches, which start to develop during the fourth week of gestation. 1 They are the second most common etiology of a congenital neck mass. 1 While branchial cysts are present at birth, they may remain unnoticed and asymptomatic for years. 2 By the time surgical excision is considered, nearly one third of cysts have developed a prior infection. 3 During infection, the cysts may become inflamed and enlarged with associated symptoms of fever and pain. 2 An incomplete resection of the cyst may lead to recurrence. 1 In some instances, branchial cleft cysts may develop within a constrained deep neck space, which may lead to cranial nerve (CN) neuropathy. 4 However, there have not been reported cases of branchial cleft cysts causing carotid artery compression and hypertension. In this case, we report a rare instance of an extremely large, compressive branchial cleft cyst causing ipsilateral hypoglossal nerve weakness and suspected secondary hypertension from carotid artery compression.
2. CASE REPORT
A 59‐year‐old female with a history of asthma, bronchitis, diabetes mellitus, hypertension, and transient ischemic attack, presented to clinic for evaluation of a large left neck mass. It started at the size of a golf ball and steadily enlarged over the last 25 years. She noted that the mass would swell during throat infections. She reported dysphagia but denied any dysphonia or pain associated with the mass. She noted gradual pressure on her neck and change in articulation over the past few years and developed difficulty lying flat on her back. She was a never smoker and never tobacco chewer and had no history of alcohol use. Of note, she had severe hypertension that was inadequately controlled despite being on 30 mg isosorbide mononitrate sustained release and 40 mg lisinopril daily. She eventually saw an otolaryngologist at an outside facility and underwent needle drainage of the cyst, which evacuated 200 mL of brown fluid. No specimen was sent for cytopathology evaluation, however. The patient was then referred to head and neck surgery at our institution.
On physical exam, she was noted to have a massive left neck mass with limitation in left tongue movement and baseline leftward tongue deviation. She had undergone a contrasted computed tomography (CT) examination of her neck 4 years prior, which had revealed a 17‐centimeter cystic mass which appeared to be causing mass effect along the left parapharyngeal space and obliterated the internal jugular vein (IJV) (Figure 1). Clinically, the mass was noted to extend from the lower parotid to the clavicle (Figure 2). Her referring physician had ordered a repeat CT scan to update the characterization of the mass, but she did not complete this. We discussed the lack of cytopathology and updated imaging. We additionally discussed treatment options and alternatives including observation, fine needle aspiration (FNA), and excision, and the patient elected to proceed with excision.
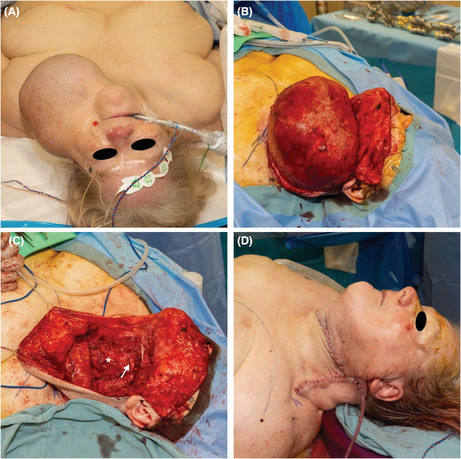
FIGURE 1.
On axial view, the preoperative computed tomography (CT) imaging of the branchial cleft cyst shows a cystic mass measuring greater than 17 centimeters in longest dimension with associated left common carotid artery compression (white arrow) without stenosis relative to contralateral carotid artery (A). Coronal CT view shows rightward tracheal and parapharyngeal deviation secondary to mass effect (B).
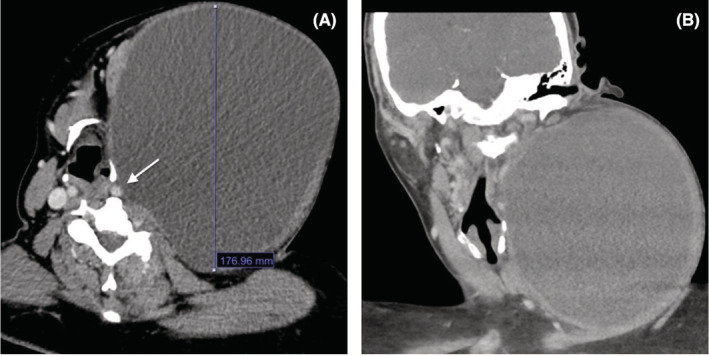
FIGURE 2.
The preoperative exam reveals findings of a massive left neck cyst (A). The in situ preserved cyst wall are noted after raising subplatysmal flaps (B). After cyst excision, the common carotid artery (white star) and hypoglossal nerve (white arrow) are visualized (C). Excess skin and subcutaneous fat is resected after excision of the cyst (D).
Intraoperatively, a modified Blair incision was marked extending for 25 centimeters directly overlying the center of the mass. Subplatysmal flaps were meticulously raised overlying the mass, and the sternocleidomastoid muscle (SCM) was noted to be extremely thinned from the bulk of the mass. The CNXI was seen entering the SCM as we separated the muscle off the tumor. However, the nerve passed through the mass proximally and was sacrificed. The remaining fascial attachments of the tumor were released from the paraspinal muscles laterally and deeply. The tumor was noted to extend deep to the digastric tendon, lateral to the common carotid artery, and hypoglossal nerve. No splaying of the internal and external carotid artery was noted, and no cyst tract was noted during the procedure. The left IJV was diminutive and was clipped. The tumor was completely removed without rupturing the capsule and was sent to pathology for permanent section. The preserved SCM was sutured to the digastric tendon and parotid‐masseteric fascia to provide soft tissue coverage for the carotid artery.
Histopathology demonstrated a benign lymphoepithelial cyst focally lined with benign squamous, ciliated, and mucinous cells, consistent with branchial cleft cyst (Figure 3). The cyst measured 22.0 × 18.0 × 13.5 cm, weighed 2.58 kg, and had an intact capsule. Sectioning revealed an abundant amount of brown, cloudy, and thin fluid, and an aggregate of tan‐brown, pasty, and thick material.
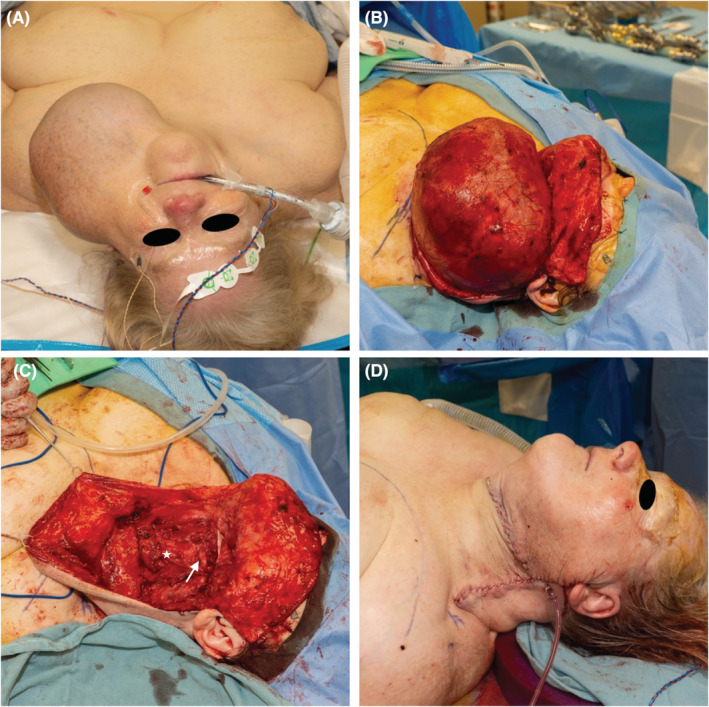
FIGURE 3.
The low power photomicrograph shows a cyst lined with stratified squamous epithelium (A). The higher power photomicrograph shows a lymphoepithelial cyst lined with benign squamous, ciliated, and mucinous cells, consistent with branchial cleft cyst (B).
Within the first postoperative day, she developed relative hypotension, with systolic/diastolic blood pressure of 103/68 mm of mercury (mm Hg) compared to her preoperative blood pressure of 181/103 mm Hg. She was evaluated by our hospitalist service for blood pressure management, and, initially, her antihypertensive medications were held but were resumed on the second postoperative day. Her averaged postoperative mean arterial pressure (MAP) improved to 97 mm Hg from 125 mm Hg.
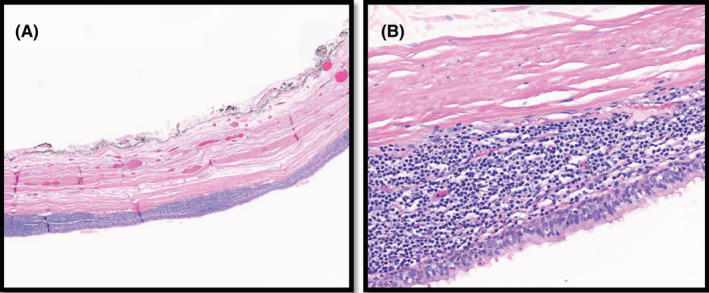
The patient was seen again in clinic 1 month from her surgery and was healing excellently (Figure 4). While being managed on the same preoperative medications, her blood pressure was 150/82 (MAP of 105), indicating a persistent postoperative improvement in blood pressure. She had a small amount of excess skin around the surgical site, but she did not desire further revision at that time and was content with the results of her surgery.
FIGURE 4.

The 1‐month postoperative exam demonstrates resolution of the left neck swelling and a flat, curvilinear scar on both front view (A) and side view (B).
3. DISCUSSION
Branchial cleft cysts are congenital masses but the age at presentation has been reported to range from 3 months to 70 years. 4 They have been known to cause compressive neuropathies of cranial nerves IX, X, XII. Up to 95% of branchial anomalies originate from the second branchial remnants. 5 Given the location of our patient's mass lateral to the common carotid artery (CCA) and deep to the SCM, it was suspected to be a Bailey type II second branchial cleft cyst. 4 , 6 Imaging findings on ultrasound include a round to ovoid, centrally anechoic mass with thin walls. 7 CT imaging may show homogeneously hypoattenuation with well‐circumscribed walls. 7 FNA is indicated for cytologic evaluation, which may demonstrate keratinizing squamous epithelial cells with subepithelial lymphoid aggregation. 8 , 9 The differential diagnosis for a unilateral neck mass includes adenopathy, lymphoma, cystic hygroma, neurofibromas, tuberculosis, parotid gland lesion, carotid body tumors. 8
The standard of care for treatment of branchial anomalies is surgical excision. Most are treated with a transcervical approach, although this may be combined with transoral or transmandibular approaches. The transoral approach is typically limited to smaller, mobile pre‐styloid cysts that can be excised with limited exposure, while the transcervical approach is often required for lesions involving the post‐styloid space. 10 The addition of a mandibulotomy may assist approach to cysts with extensive involvement of the internal carotid artery and skull base. 10 , 11 Complications of surgery include cranial nerve and vascular injury, fistula, hematoma, seroma, and scar formation. 8 Other treatment options, including cyst marsupialization and sclerotherapy, have shown variable success. 8 , 12
Improvement in hypertension after excision of a branchial cleft cyst has not previously been documented. It may be that changes in arterial vascular architecture and flow parameters or alteration of carotid baroreflex receptor sensitivity secondary to the mass affected the patient's blood pressure. 13 , 14 Sasaki et al. 14 demonstrated markers of increased vascular stiffness and resistance, including higher resistance index, pulsatility index, and intima‐media thickness of the CCA, were significantly associated with the development of hypertension. It may be that the size of the mass and degree of compression on the carotid artery increased vascular resistance and subsequently the patient's blood pressure. Timmers et al., 15 demonstrated treatment of head and neck tumors may decrease baroreflex sensitivity, which may be an additional etiology for the improvement in blood pressure. Future studies investigating the baroreflex sensitivity and blood pressure alteration in patients undergoing surgical treatment of neck masses may be of interest.
4. CONCLUSION
Branchial cleft cysts are the second most common congenital neck mass. They may develop within small‐volume neck spaces and cause cranial nerve palsies secondary to mass effect. Left untreated, branchial cleft cysts may increase in size enough to cause local vascular compression and secondary hypertension. Surgical treatment to relieve compression may improve blood pressure in conjunction with appropriate medical management.
AUTHOR CONTRIBUTIONS
Noah Shaikh: Conceptualization; data curation; investigation; methodology; writing – original draft; writing – review and editing. Sara Ibrahim‐Shaikh: Conceptualization; writing – original draft; writing – review and editing. Esra Alshaikhnasser: Data curation; investigation; writing – original draft; writing – review and editing. Saddhana Kukkala: Conceptualization; data curation; writing – review and editing. Levi Stevens: Data curation; investigation; writing – review and editing. Jeffson Chung: Conceptualization; data curation; investigation; methodology; writing – original draft; writing – review and editing.
CONFLICT OF INTEREST STATEMENT
This work was not funded and there are no conflicts of interest.
ETHICAL APPROVAL
This case report was reviewed and determined exempt by the institutional review board (IRB) of West Virginia University (WVU). Additionally, a written informed consent form was completed by the patient.
ACKNOWLEDGMENTS
We thank the Department of Otolaryngology at West Virginia University for their support.
Shaikh N, Ibrahim‐Shaikh S, Alshaikhnasser E, Kukkala S, Stevens L, Chung J. Excision of massive left branchial cleft cyst with secondary hypertension. Clin Case Rep. 2023;11:e7131. doi: 10.1002/ccr3.7131
DATA AVAILABILITY STATEMENT
Research data is available on request.
REFERENCES
- 1. Waldhausen JH. Branchial cleft and arch anomalies in children. Semin Pediatr Surg. 2006;15(2):64‐69. [DOI] [PubMed] [Google Scholar]
- 2. Lofgren D, Shermetaro C, Coste AH. Branchial cleft cyst. 2020. [PubMed]
- 3. Schroeder JW Jr, Mohyuddin N, Maddalozzo J. Branchial anomalies in the pediatric population. Otolaryngol Head Neck Surg. 2007;137(2):289‐295. [DOI] [PubMed] [Google Scholar]
- 4. Magdy EA, Fadali GA, Seif‐Elnasr M, Fathalla MF. Unusual isolated parapharyngeal second branchial cleft cyst: a case report and literature review. Case Rep Otolaryngol. 2020;2020:8814071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Agaton‐Bonilla FC, Gay‐Escoda C. Diagnosis and treatment of branchial cleft cysts and fistulae. A retrospective study of 183 patients. Int J Oral Maxillofac Surg. 1996;25(6):449‐452. [DOI] [PubMed] [Google Scholar]
- 6. Bailey H. Branchial Cysts and Other Essays on Surgical Subjects in the Facio‐Cervical Region. Lewis; 1929. [Google Scholar]
- 7. Koeller KK, Alamo L, Adair CF, Smirniotopoulos JG. Congenital cystic masses of the neck: radiologic‐pathologic correlation. Radiographics. 1999;19(1):121‐146; quiz 152–123. [DOI] [PubMed] [Google Scholar]
- 8. Zaifullah S, Yunus MR, See GB. Diagnosis and treatment of branchial cleft anomalies in UKMMC: a 10‐year retrospective study. Eur Arch Otorhinolaryngol. 2013;270(4):1501‐1506. [DOI] [PubMed] [Google Scholar]
- 9. Regauer S, Gogg‐Kamerer M, Braun H, Beham A. Lateral neck cysts–the branchial theory revisited. A critical review and clinicopathological study of 97 cases with special emphasis on cytokeratin expression. APMIS. 1997;105(8):623‐630. [PubMed] [Google Scholar]
- 10. Yang YN, Hong YT. Intraoral approach for parapharyngeal branchial cleft cysts. Ear Nose Throat J. 2022;1455613211067846. [DOI] [PubMed] [Google Scholar]
- 11. Cohen SM, Burkey BB, Netterville JL. Surgical management of parapharyngeal space masses. Head Neck. 2005;27(8):669‐675. [DOI] [PubMed] [Google Scholar]
- 12. Churchill P, Otal D, Pemberton J, Ali A, Flageole H, Walton JM. Sclerotherapy for lymphatic malformations in children: a scoping review. J Pediatr Surg. 2011;46(5):912‐922. [DOI] [PubMed] [Google Scholar]
- 13. Shah‐Becker S, Pennock M, Sinoway L, Goldenberg D, Goyal N. Baroreceptor reflex failure: review of the literature and the potential impact on patients with head and neck cancer. Head Neck. 2017;39(10):2135‐2141. [DOI] [PubMed] [Google Scholar]
- 14. Sasaki N, Maeda R, Ozono R, Nakano Y, Higashi Y. Common carotid artery flow parameters predict the incidence of hypertension. Hypertension. 2021;78(6):1711‐1718. [DOI] [PubMed] [Google Scholar]
- 15. Timmers HJ, Karemaker JM, Wieling W, et al. Arterial baroreflex and peripheral chemoreflex function after radiotherapy for laryngeal or pharyngeal cancer. Int J Radiat Oncol Biol Phys. 2002;53(5):1203‐1210. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Research data is available on request.


