Abstract
Introduction and importance
Lateral ankle ligament reconstruction failures are increasingly frequent. To our knowledge no reports of using a new arthroscopic anatomical reconstruction with a gracilis autograft to treat an ankle re-injury have been described.
Case presentation
A 19-year-old man presented with a right ankle injury resulting in isolated lateral ankle instability. The clinical examination showed significant laxity. The MRI confirmed a grade 3 tear of the lateral ligament complex. Arthroscopic anatomical reconstruction with a gracilis autograft was performed and the patient was able to return to all of his activities. Eighteen months after the primary reconstruction, he had another high-energy injury. Despite rehabilitation, he experienced isolated lateral instability. Arthrography confirmed graft failure. The patient underwent a new anatomical reconstruction with the controlateral gracilis autograft, with no difficulties. At 6 months, he had returned to all of his activities, with no limitations or discomfort.
Clinical discussion
Articular hypermobility, hindfoot varus and/or excess weight should be looked for or treated to explain the graft failure. Other therapeutic options are possible for revision surgery such as non-anatomical tenodesis, allografts or artificial ligaments.
Conclusion
Arthroscopic anatomical reconstruction of the lateral ligaments of the ankle with a new arthroscopic anatomical reconstruction procedure seems to be feasible. Other studies are needed to define the therapeutic strategy for ligament reconstruction graft failures.
Keywords: Lateral ankle instability, Anatomic lateral reconstruction, Arthroscopy
Highlights
-
•
Ankle sprains are one of the most common injuries.
-
•
Lateral ankle ligament reconstruction re-injuries or failures are increasingly frequent.
-
•
There is no consensus on the management of reconstruction after ankle re-injury or graft failure.
-
•
New arthroscopic reconstruction with the contralateral gracilis autograft is a feasible option.
1. Introduction
Ankle sprains are one of the most common injuries, involving the lateral ligaments in 85 % of the cases [1], [2]. One of the most important intermediate and long-term risks of ankle sprain is chronic lateral instability which occurs in 30–40 % of cases, thus explaining the increase in the number of surgical procedures [3].
Surgery involves repairing or reconstructing the lateral ligaments. Both short and long term results are good with even better results with anatomical techniques [4], [5]. Anatomical reconstruction with hamstring autografts are increasingly frequent with results that are as good as those of the gold standard: the modified Bröstrom-Gould technique [5], [6]. The arthroscopic approach reduces the complication rate with faster recovery, while effectively treating associated lesions [7].
Because of the increasing number of surgical procedures, the number of failures or re-injury has also increased. The rate of recurrent instability in the literature is as high as 26 % following a Bröstrom-Gould procedure [8].
After unsuccessful ligament repair and when revision surgery is necessary, anatomical reconstruction is the technique of choice, but with poorer results than primary reconstruction [9]. However, there is no consensus, and the data are limited on the management of reconstruction graft failures. To our knowledge no case of revision surgery following ankle re-injury or failure of an anatomical arthroscopic reconstruction with a gracilis autograft by a new reconstruction with a gracilis autograft has been described.
We report the case of an ankle re-injury after anatomical reconstruction of the lateral ligament complex (ATFL and CFL) with a gracilis autograft treated with a new anatomical reconstruction with the contralateral gracilis autograft. This paper was written according to SCARE guidelines [10].
Presentation of Case (with video illustration).
A 19-year-old man suffered a severe basketball injury of the right ankle in December 2017. This ankle had not been previously injured. His only other medical history was asthma with a normal body mass index (BMI) (=21 kg/m2). He was a non-smoker. The patient was referred by his general practitioner after three months of rehabilitation due to isolated chronic instability. The clinical examination showed frontal and sagittal instability of the right ankle compared to the contralateral. It was flexible and pain free. There was no generalized articular hypermobility (Beighton score = 2) [11]. Hind foot alignment and X-rays were normal. MRI showed a grade 3 tear of the lateral ligaments (ATFL and CFL) with no osteochondral lesions or other ligament injuries (syndesmosis, deltoid).
Because of the ligament lesions and the persistent instability despite rehabilitation, in May 2018 the patient underwent arthroscopic reconstruction of the lateral ligaments of the ankle with a gracilis autograft using the technique by Guillo et al. modified by Lopes et al. [12], [13], [14]. The procedure was performed with the patient in the supine position, with a pneumatic tourniquet (on the thigh), by a surgeon experienced arthroscopic ankle surgery. Classic arthroscopic material was used (4-mm 30° arthroscope; 3 mm bone/soft tissue shaver). The graft was attached to the talus and calcaneum with tenodesis screws (Bio-Tenodesis Screw®, Arthrex, Naples, Fl, USA). Peroneal fixation was achieved with a cortical endobutton (ACL TightRope®, Arthrex, Naples, Fl, USA). The rest of the arthroscopic exploration of the ankle was normal. Immediate postoperative weight-bearing was allowed with a walking boot for 2 weeks. There were no prophylactic antithrombic. Rehabilitation was begun on postoperative week 2. Seven months after surgery, the ankle was stable, flexible, and pain free, and the patient had returned to all activities (including basketball) with no limitations or discomfort. The patient had another high-energy basketball injury to the right ankle in November 2019. There was no other medical history, his BMI was still normal (=21.5 kg/m2). The clinical examination showed frontal and sagittal plane instability without pain or stiffness. Despite rehabilitation, the ankle was unstable and the patient was apprehensive during sports. The MRI showed a CFL tear and a heterogenous appearance to the ATFL with no clear tear. Ultrasound and arthrography showed a complete ligament graft tear. There were no osteochondral lesions or other ligament injuries (syndesmosis, deltoid). An analysis of the bone tunnels did not show any malposition or widening [12], [13], [14] (Fig. 1).
Fig. 1.
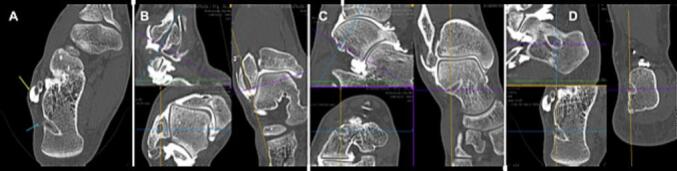
A,B,C,D Imagerie Pre-op.
Due to the graft rupture and persistent instability despite 6 months of rehabilitation, in May 2020 the patient underwent revision lateral ligament reconstruction of the ankle with a new arthroscopic anatomical autograft procedure. The contralateral gracilis tendon was used. The procedure was performed by the same surgeon. The surgical technique was similar, with, in particular, the use of the initial tunnels, without difficulty. The rest of the arthroscopic exploration was normal (Fig. 2, Fig. 3, Fig. 4; Video 1, Video 2). The postoperative follow-up protocol was identical to the first procedure.
Fig. 2.

Per operative arthroscopic view.
Fig. 3.

A,B,C Surgical step.
Fig. 4.

Per operative arthroscopic view after reconstruction.
Five months after surgery, the ankle was stable, flexible and pain free. The patient had returned to running and could perform single leg hops. At 6 months he had returned to all his activities, in particular basketball.
Twenty-four months after surgery, he was not limited in his activities, in particular high intensity sports. He has not had any new injuries to the ankle. There were no complications from surgery, in particular infectious, thromboembolic or neurovascular.
2. Discussion
We report the case of ankle re-injury after anatomical ligament reconstruction of the lateral ligaments (AFTL and CLF) of the ankle with a gracilis autograft treated with a new anatomical reconstruction with contralateral gracilis autograft. To our knowledge there are no similar cases in the literature. This is a feasible technique with no formal contraindications. This option is interesting as it is nearly identical to the primary reconstruction. In case of malposition, tunnels can be easily repositioned using well known references [12], [13], [14].
To explain the failure of a primary ligament reconstruction of the ankle, possible causes must be looked for. Articular hypermobility is a frequent cause, especially following repair. Indeed, Park et al. reported a failure rate of 10.8 % in the group without hypermobility compared to 45.2 % in the group with, following a modified Broström procedure [15]. Hindfoot varus is also a well-known cause of ankle instability as shown by Larsen et al. [16]. Finally, Vuurberg et al. have shown that excess weight and a high BMI are also risk factors [17]. None of these criteria were found in our patient. The new high-energy injury seems to be the only explanation for the rupture of the first graft.
Other therapeutic options could have been considered for the revision. Non-anatomical stabilization with tenodesis, using, for example the fibularis brevis could have been performed. However, Vuurberg et al. have shown that the functional outcome of these techniques is poorer than that of anatomical techniques and ankle biomechanics are not restored [4], [5]. They should probably be limited to second intention repairs or for less demanding patients. To decrease morbidity of the donor site, an allograft could have been used. However, these are not always available and are more expensive. For the moment, the literature does not clearly show an advantage between either the auto or allograft for this indication [18]. As with ACL ligamentoplasty revisions, the surgery can be perform in one stage and the most important thing therefore seems to be the management of the tunnels and the bone stock [19]. Artificial ligaments could be another option because compared to ligament repair, they provide comparable results in primary procedures [20]. However, they have not been compared to graft reconstructions and have not been evaluated in revision surgeries.
3. Conclusion
Ankle re-injury after arthroscopic anatomical reconstruction of the lateral ligaments with a gracilis autograft is rare, but the incidence is growing due to the increasing number of surgeries for chronic lateral ankle instability. In case of unsuccessful conservative treatment, a new arthroscopic reconstruction with the contralateral gracilis autograft is a feasible option. It seems indicated because of better long- and short-term results with anatomical and arthroscopic techniques in primary surgery. Other larger, comparative studies are needed to define the therapeutic strategy for ankle re-injury after lateral ligament reconstructions.
The following are the supplementary data related to this article.
Final view.
Renamed_ec725.
Sources of funding
N/A
Ethical approval
Study exempt from ethical approval.
Consent
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Research registration
N/A
Provenance and peer-reviewed
Not commissioned, externally peer-reviewed.
Garantor
Ronny Lopes
CRediT authorship contribution statement
Clément GUYONNET: Formal analysis, Data Curation, Writing, Visualization.
Ronny LOPES: Conceptualization, Methodology, Validation, Investigation, Resources, Supervision, Performed surgery.
Declaration of competing interest
One of the authors is a consultant for Arthrex. The other authors declares no conflicts of interest.
References
- 1.Fong D.T.P., Hong Y., Chan L.K., Yung P.S.H., Chan K.M. A systematic review on ankle injury and ankle sprain in sports. Sports Med. 2007;37(1):73–94. doi: 10.2165/00007256-200737010-00006. [DOI] [PubMed] [Google Scholar]
- 2.Maffulli N., Ferran N.A. Management of acute and chronic ankle instability. J. Am. Acad. Orthop. Surg. 2008 Oct;16(10):608–615. doi: 10.5435/00124635-200810000-00006. [DOI] [PubMed] [Google Scholar]
- 3.Herzog M.M., Kerr Z.Y., Marshall S.W., Wikstrom E.A. Epidemiology of ankle sprains and chronic ankle instability. J. Athl. Train. 2019 Jun;54(6):603–610. doi: 10.4085/1062-6050-447-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Vuurberg G., Pereira H., Blankevoort L., van Dijk C.N. Anatomic stabilization techniques provide superior results in terms of functional outcome in patients suffering from chronic ankle instability compared to non-anatomic techniques. Knee Surg. Sports Traumatol. Arthrosc. 2018 Jul;26(7):2183–2195. doi: 10.1007/s00167-017-4730-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Noailles T., Lopes R., Padiolleau G., Gouin F., Brilhault J. Non-anatomical or direct anatomical repair of chronic lateral instability of the ankle: a systematic review of the literature after at least 10 years of follow-up. Foot Ankle Surg. 2018 Apr;24(2):80–85. doi: 10.1016/j.fas.2016.10.005. [DOI] [PubMed] [Google Scholar]
- 6.Xu X., Hu M., Liu J., Zhu Y., Wang B. Minimally invasive reconstruction of the lateral ankle ligaments using semitendinosus autograft or tendon allograft. Foot Ankle Int. 2014 Oct;35(10):1015–1021. doi: 10.1177/1071100714540145. [DOI] [PubMed] [Google Scholar]
- 7.Attia A.K., Taha T., Mahmoud K., Hunt K.J., Labib S.A., d’Hooghe P. Outcomes of open versus arthroscopic Broström surgery for chronic lateral ankle instability: a systematic review and meta-analysis of comparative studies. Orthop. J. Sports Med. 2021 Jul;9(7) doi: 10.1177/23259671211015207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Li X., Killie H., Guerrero P., Busconi B.D. Anatomical reconstruction for chronic lateral ankle instability in the high-demand athlete: functional outcomes after the modified Broström repair using suture anchors. Am. J. Sports Med. 2009 Mar;37(3):488–494. doi: 10.1177/0363546508327541. [DOI] [PubMed] [Google Scholar]
- 9.Eble S.K., Hansen O.B., Patel K.A., Drakos M.C. Lateral ligament reconstruction with hamstring graft for ankle instability: outcomes for primary and revision cases. Am. J. Sports Med. 2021 Aug;49(10):2697–2706. doi: 10.1177/03635465211026969. [DOI] [PubMed] [Google Scholar]
- 10.Agha R.A., Franchi T., Sohrabi C., Mathew G., Kerwan A., SCARE Group The SCARE 2020 guideline: updating consensus Surgical CAse REport (SCARE) guidelines. Int. J. Surg. Lond. Engl. 2020 Dec;84:226–230. doi: 10.1016/j.ijsu.2020.10.034. [DOI] [PubMed] [Google Scholar]
- 11.Beighton P., Horan F. Orthopaedic aspects of the Ehlers-Danlos syndrome. J. Bone Joint Surg. Br. 1969 Aug;51(3):444–453. [PubMed] [Google Scholar]
- 12.Guillo S., Archbold P., Perera A., Bauer T., Sonnery-Cottet B. Arthroscopic anatomic reconstruction of the lateral ligaments of the ankle with gracilis autograft. Arthrosc. Tech. 2014 Oct;3(5):e593–e598. doi: 10.1016/j.eats.2014.06.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lopes R., Noailles T., Brulefert K., Geffroy L., Decante C. Anatomic validation of the lateral malleolus as a cutaneous marker for the distal insertion of the calcaneofibular ligament. Knee Surg. Sports Traumatol. Arthrosc. 2018 Mar;26(3):869–874. doi: 10.1007/s00167-016-4250-7. [DOI] [PubMed] [Google Scholar]
- 14.Lopes R., Decante C., Geffroy L., Brulefert K., Noailles T. Arthroscopic anatomical reconstruction of the lateral ankle ligaments: a technical simplification. Orthop. Traumatol. Surg. Res. 2016 Dec;102(8S):S317–S322. doi: 10.1016/j.otsr.2016.09.003. [DOI] [PubMed] [Google Scholar]
- 15.Park K.H., Lee J.W., Suh J.W., Shin M.H., Choi W.J. Generalized ligamentous laxity is an independent predictor of poor outcomes after the modified Broström procedure for chronic lateral ankle instability. Am. J. Sports Med. 2016 Nov;44(11):2975–2983. doi: 10.1177/0363546516656183. [DOI] [PubMed] [Google Scholar]
- 16.Larsen E., Angermann P. Association of ankle instability and foot deformity. Acta Orthop. Scand. 1990 Apr;61(2):136–139. doi: 10.3109/17453679009006505. [DOI] [PubMed] [Google Scholar]
- 17.Vuurberg G., Altink N., Rajai M., Blankevoort L., Kerkhoffs G.M.M.J. Weight, BMI and stability are risk factors associated with lateral ankle sprains and chronic ankle instability: a meta-analysis. J. ISAKOS. 2019 Nov;4(6):313–327. doi: 10.1136/jisakos-2019-000305. [DOI] [PubMed] [Google Scholar]
- 18.Brambilla L., Bianchi A., Malerba F., Loppini M., Martinelli N. Lateral ankle ligament anatomic reconstruction for chronic ankle instability: allograft or autograft? A systematic review. Foot Ankle Surg. Off. J. Eur. Soc. Foot Ankle Surg. 2020 Jan;26(1):85–93. doi: 10.1016/j.fas.2018.11.014. [DOI] [PubMed] [Google Scholar]
- 19.Kamath G.V., Redfern J.C., Greis P.E., Burks R.T. Revision anterior cruciate ligament reconstruction. Am. J. Sports Med. 2011 Jan;39(1):199–217. doi: 10.1177/0363546510370929. [DOI] [PubMed] [Google Scholar]
- 20.Ulku T.K., Kocaoglu B., Tok O., Irgit K., Nalbantoglu U. Arthroscopic suture-tape internal bracing is safe as arthroscopic modified Broström repair in the treatment of chronic ankle instability. Knee Surg. Sports Traumatol. Arthrosc. 2020 Jan;28(1):227–232. doi: 10.1007/s00167-019-05552-w. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Final view.
Renamed_ec725.


