Abstract
The severely atrophic maxilla can present with some challenges during treatment planning with communication between those performing the surgical and prosthetic aspects of the treatment as well as communication with the patient as to what is being suggested for treatment. This article simplifies the communication and understanding of treating the severely atrophic maxilla and based on the Bedrossian classification gives a guideline for the surgical approach to be adapted based on the patient residual anatomy.
Keywords: Atrophic maxilla, Zygomatic implants, Pterygoid implants, Treatment planning
1. Introduction
A frequent occurrence with patients who have been in a full arch removable maxillary prosthesis is significant alveolar resorption that hampers implant placement. Lack of stimulation within the bone by either teeth or implants results in negative volumetric changes that are complicated in the posterior maxilla by sinus enlargement. Following tooth extraction or periodontal bone loss, a cascade starts of inevitable bone remodeling of the alveolar ridge. This remodeling occurs in a three-dimensional manner with loss to both height and width of the residual ridge resulting in inadequate bone for implant placement without augmentation procedures. When an advanced level of bone resorption has occurred in the maxilla, only a limited number of surgical options are available. Those may include tilted implants to avoid the pneumatized sinuses with a resulting prosthesis with premolar occlusion or significant osseous grafting in those deficient areas to permit implant placement in those areas lacking sufficient bone to house implants. Augmentation procedures add to the treatment time and the cost of the total treatment to achieve implant placement and restoration to return the patient to function. Non-grafting solutions to these clinically challenging situations has been presented which include tilted implants, zygomatic implants and pterygoid implants to utilize what bone volume is present.1 Zygomatic implants have been in successful use to allow osseous grafting of the maxillary sinus and deficient ridge to be avoided and still permit implant placement in distant available bone.2,3 Although zygomatic implants are more complex to place and require a higher surgical skill level, their survival rates are similar to those of standard endosteal implants.4 Zygomatic implants are useful in treating and managing the severely atrophic maxilla.5
Clinical evaluation utilizing panoramic and/or CBCT radiographs of the patient is performed to determine what the volume of bone is present in the areas of missing teeth to allow treatment planning options to treat the patient with an implant based approach. The evaluation needs to include determining the appropriate incisal edge position, need for lip support and the appropriate vertical dimension of occlusion.
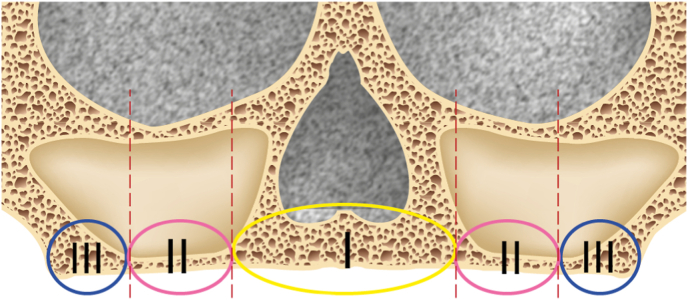
Physiological bone remodeling can be associated with genetically low maxillary bone density and is observed at a faster more profound rate then in the mandible. This may be accelerated by traumatic induced resorption (ex: long term denture wear) leading to the bone available in the anterior and posterior areas without augmentation to allow placement of implants. Potential available bone sites are identified using the Bedrossian classification of the maxilla to identify zones that implants may be placed into.6,7 (Fig. 1) The Bedrossian classification gives a guideline for the surgical approach to be adapted. This is done by reviewing the patient's panoramic radiograph. The maxilla is divided into different zones; Zone I - Between canine to canine, Zone II - bicuspids, Zone III– molars and Zone IV – zygoma. The presence or absence of bone in these zones determines the surgical approach to be adapted.
Fig. 1.
The Bedrossian zone classification of the maxilla. (Zone I = premaxilla, Zone II = premolars, Zone III = molars and Zone IV = zygomatic process).
One of the methods for decision making in the atrophic maxilla is to follow the Bedrossian classification, a radiographic classification based on the systematic assessment of the available bone. This takes into consideration the relationship between the alveolus, nasal floor and the position and size of maxillary sinus. With the Bedrossian zone classification when adequate bone is present that can accommodate implant placement without augmentation, treatment would follow these guidelines. Adequate volume of bone in zones I, II and III would be treated with 4–8 implants placed in an axial (non-angled) direction. When inadequate bone is present in zone III, but is sufficient volume in zones I and II then the ALL-on-X approach would be followed with 4–6 implants placed axially or angled (tilted) achieve the widest arch spread for better A-P ratio. A maxilla that has adequate bone only in zones I and IV with insufficient volume in zones II and III treatment would allow placement of 2–4 implants in zone one and a zygomatic implant bilaterally in zone IV.8 When bone is also present in zone III, as well as zones I and IV, pterygoid implants can be placed into zone III to augment the implants in zones I and IV.9 Inadequate bone in zones I and II, without bone augmentation may be treated with dual bilateral (quad) zygomatic implants. When spread of the zygomatic implants in each quadrant has the implant platforms with inadequate spread and sufficient bone is present in zone III, pterygoid implants may be added to increase the A-P spread to allow restoration of the arch.
2. Zone based treatment planning
Based on bone availability the severely atrophied maxilla is divided into three types, 1, 2A and 2B.
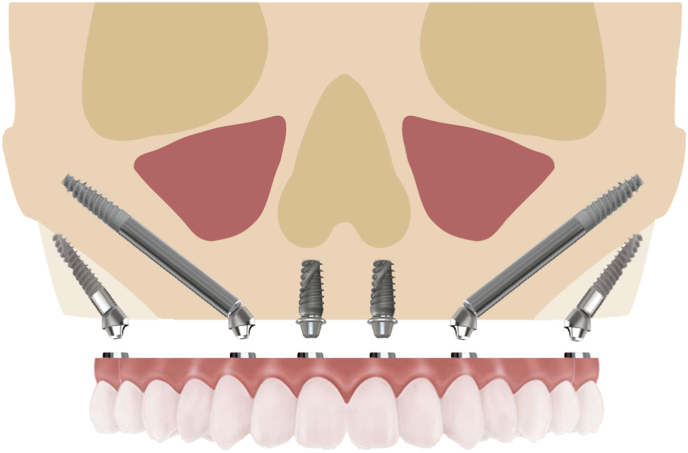
2.1. Type 1
A type 1 maxillary arch presents with a premaxilla (zone II) with a height of 10 mm or greater and a width of 5 mm or greater (Fig. 2). This will allow placement of 2–4 regular platforms axial or tilted (depending on anterior sinus wall proximity) dental implants in the zone I with no grafting needed as implant can be placed into native bone and no biological complication are expected (no fenestration, dehiscence) requiring grafting. Posteriorly, a single zygomatic implant is placed bilaterally with its platform at the 1st molar position providing a good A-P spread and no distal cantilever prosthetically.10 (Fig. 3) Those patients with a mandibular 2nd molar or larger arch length, may require a cantilever distal to the zygomatic implant (Fig. 4). When a cantilever is not required, cleansability is greater for the patient then those cases with a cantilever present. The disadvantages to this type approach are the zygoma position at the 1st molar places it in a more vertical orientation with the apical portion of the implant closer to the orbit and blocking the placement of an anterior zygomatic implant if required in the future (Fig. 5). The result provides adequate A-P spread to restore a type 1 resorbed maxillary arch (Fig. 6).
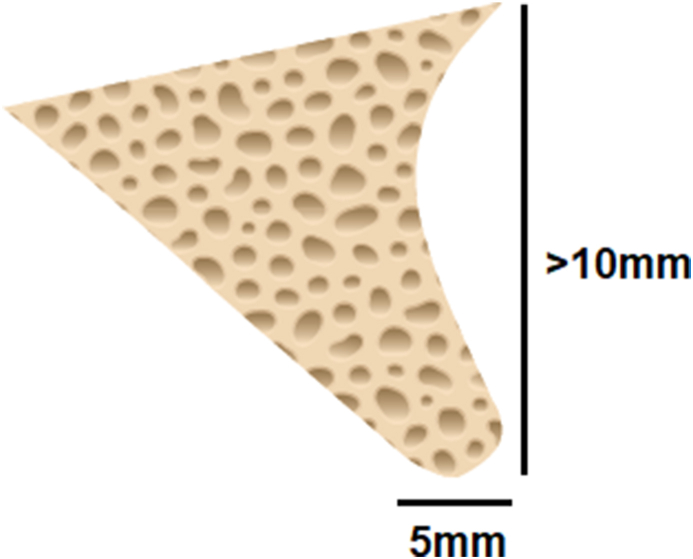
Fig. 2.
Cross-section of the premolar area of the maxilla (zone II) that presentes with 10 mm + height and 5 mm + width for implant placement.
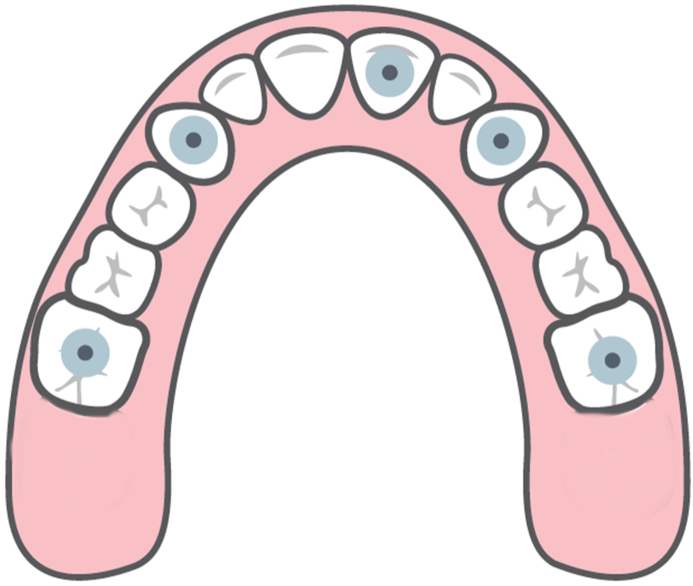
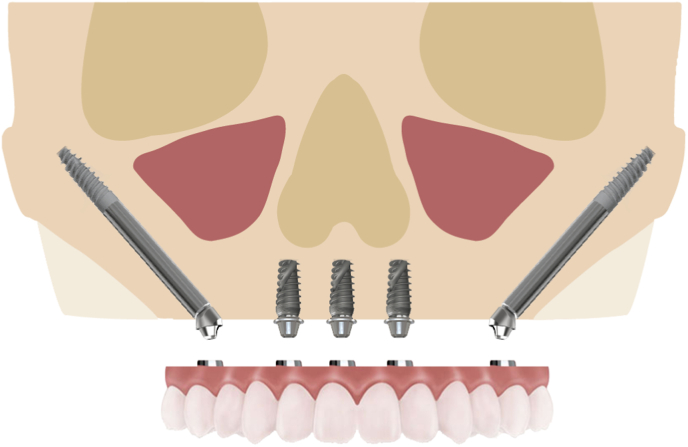
Fig. 3.
A-P spread with placement of a zygomatic implant bilaterally at the 1st molar position and standard implants in zones I and II.
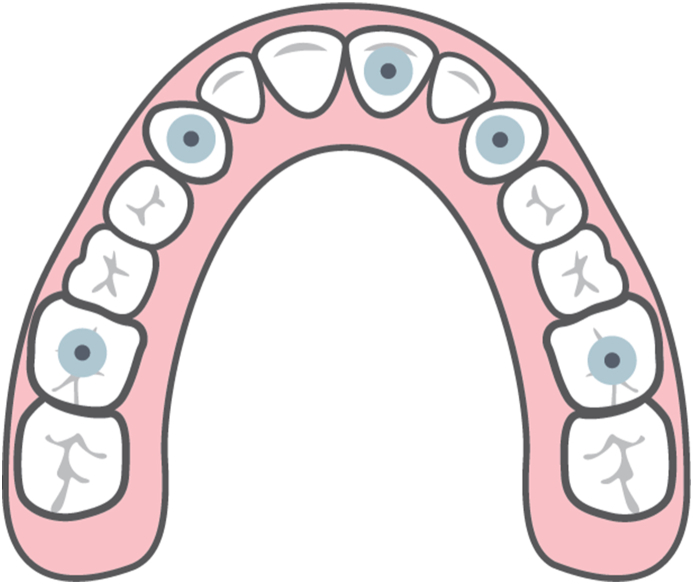
Fig. 4.
A type I maxillary treatment with a cantilever distal to the 1st molar position of the zygomatic implant.
Fig. 5.
Illustration of a type I implant treatment demonstrating the apical position of the zygomatic implant in relation to the orbit blocking potential for future placement of another zygomatic implant mesial to it should it be required later.
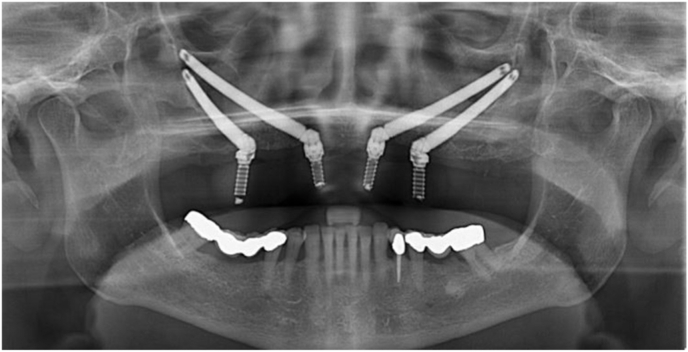
Fig. 6.
Panoramic radiograph demonstrating zygomatic implant placement with traditional implants in the anterior and premolar areas in a type 1 configuration.
2.2. Type 2
The type 2 resorbed maxillary arch is divided into subcategory A and B depending on the degree of resorption. Long-term survival of the anterior implants may be questionable due to the native anatomical limitations related to the bone quantity and quality availability and thus the possibility of surgical modification in case of failure should be predicted.
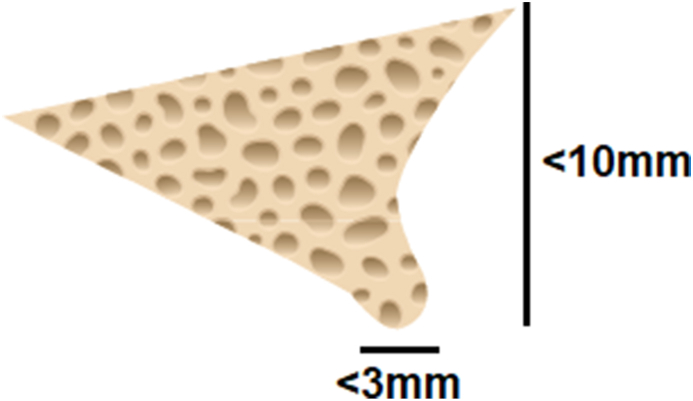
2.3. Type 2 A
This type and subcategory present with an atrophic premaxilla (zone I) with a height of 10 mm and width between 3 and 5 mm (Fig. 7). This is allows the placement of 2 narrow diameter axial positioned implants, Vomer or nasalus implants. Bone grafting can be expected at the time of the implant surgery due to possible fenestration and dehiscence. Posteriorly, a single zygomatic implant is placed with its platform positioned in the 2nd premolar position. Pterygoid implants are placed to allow support in the molar area without the need for sinus augmentation in the molar area and improve AP spread while voiding a posterior cantilever (Fig. 8). Should in the future the anterior axial implants fail, a second zygomatic implant may be placed (Fig. 9). The disadvantage to this approach is patient hygiene is more difficult to reach around the restored pterygoid implants as their position is at or distal to the natural 2nd molar position. Impression capture during the restorative phase may also present with some challenges due to the pterygoid implants position. Position of the pterygoid implants provides maximized A-P spread and occlusion with whatever teeth or implants are present in the mandibular arch (Fig. 10).
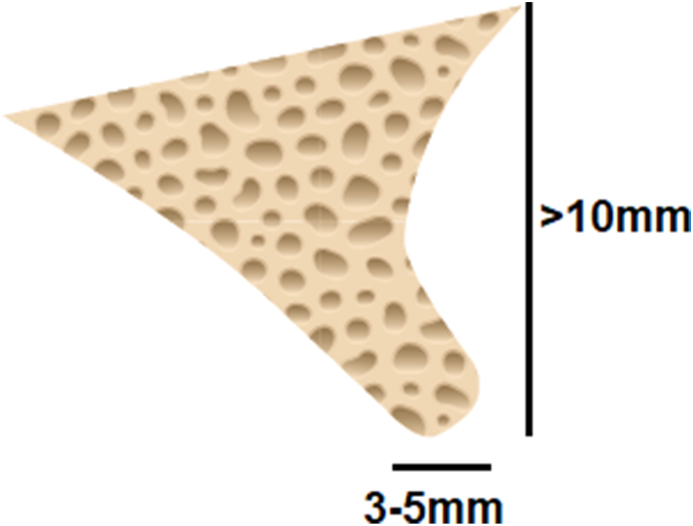
Fig. 7.
Cross-section of the anterior area of the maxilla (zone I) that presentes with 10 mm height and 3–5 mm width for implant placement.
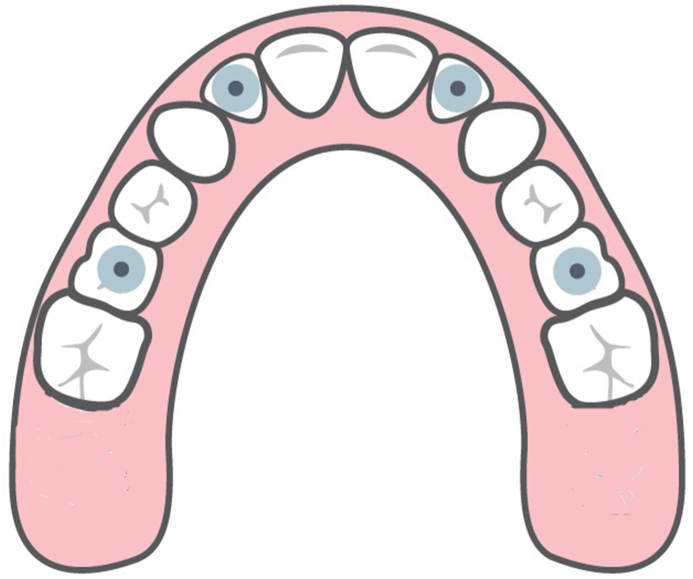
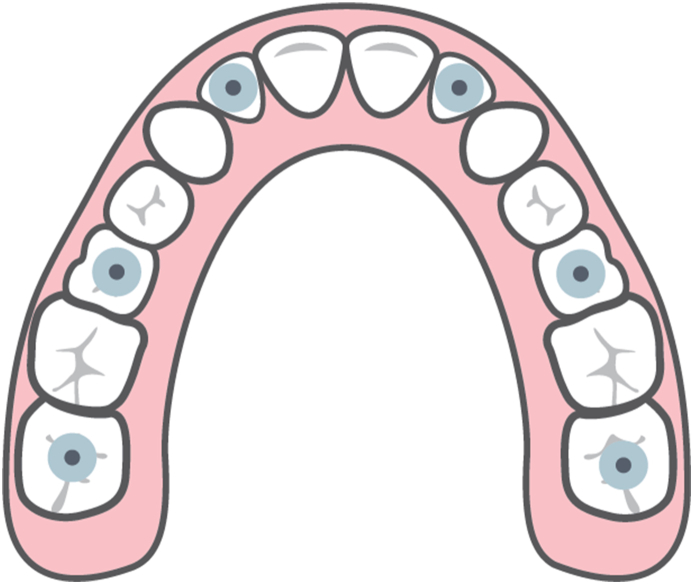
Fig. 8.
Platform position in a type 2A implant treatment presents with good A-P spread and no distal cantilever on the prosthesis.
Fig. 9.
Illustration of implant positions in a type 2A case with anterior implants, bilateral single zygomatic implants and pterygoid implants.
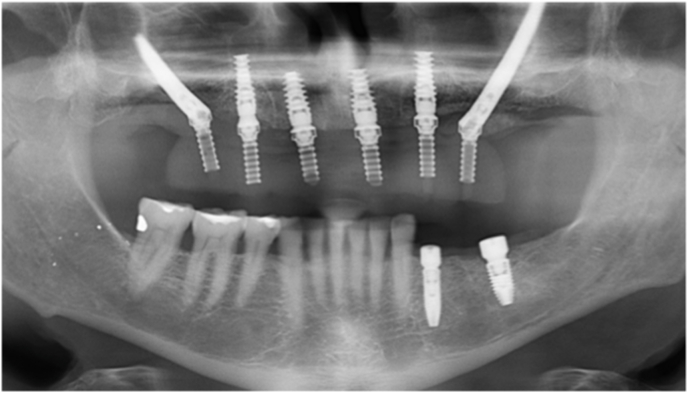
Fig. 10.
Panoramic radiograph demonstrating zygomatic in a type 2A configuration.
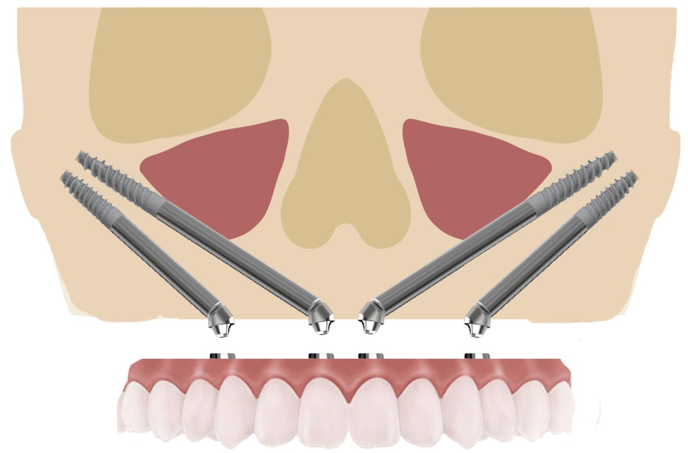
2.4. Type 2B
This type and subcategory present with a severely atrophic premaxillae (zone I) with insufficient height, width and angulation issues to permit implant placement (Fig. 11). The premaxillary resorption extends to the nasal floor and thus dental implant without prior grafting are not indicated. The resorptive presentation due to angulation issues may not allow implant placement to permit restoration even following grafting. Bilateral double zygomatic implant placement (referred to as “quad” zygoma implants) is indicated with implant platform placement at the canine/lateral positions and 2nd Premolar positions allows stability of the planned prosthesis but termination of the prosthetics at the 1st molar with a resulting cantilever.11,12 (Fig. 12, Fig. 13, Fig. 14) Quad zygomas have been reported to have comparable success rates as bilateral single zygomatic implants but offer better implant platform spread in those cases that will not permit anterior implant placement.13,14 Pterygoid implants may be added to improve the AP spread and reduce the cantilever depending on the opposing dentition and occlusion (Fig. 15, Fig. 16, Fig. 17). As with type 2A, hygiene is more difficult for the patient due to the position of pterygoid implants if they are added and the cantilever if they are not added. Additionally, impression capture during the restorative phase may also present with some challenges due to the pterygoid implants position, as well as insertion of the prosthesis at placement.
Fig. 11.
Maxillary anterior area presenting with severe aptrophy preventing implant placement in the anterior due to minimal height, width and angulation issues to the premaxilla.
Fig. 12.
Platform positions in a type 2B implant treatment presents with presence of distal cantilever on the prosthesis.
Fig. 13.
Implant placement in a type 2B configuration with bilateral zygomatic implants with distal cantilevers prosthetically.
Fig. 14.
Panoramic radiograph demonstrating zygomatic in a type 2B configuration.
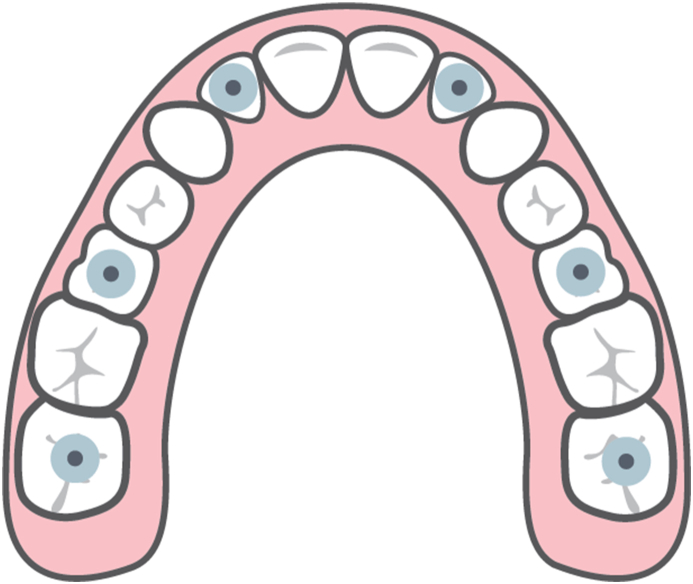
Fig. 15.
Platform position in a type 2B implant treatment presents with good A-P spread and no distal cantilever on the prosthesis.
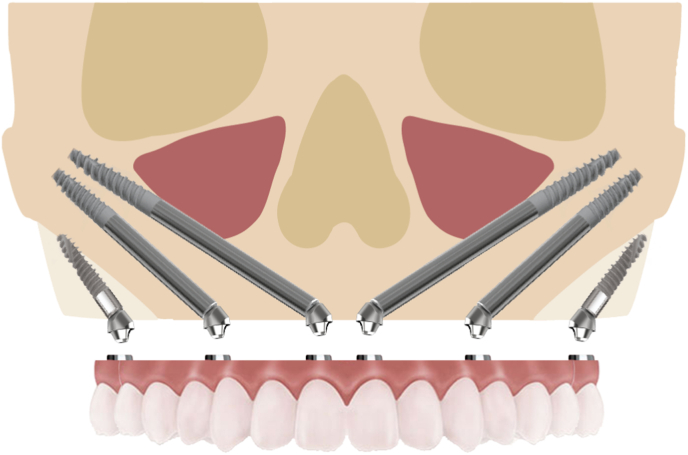
Fig. 16.
Implant placement in a type 2B configuration with bilateral zygomatic implants and pterygoid implants.
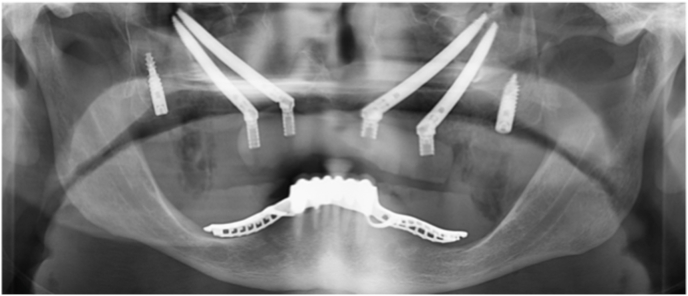
Fig. 17.
Panoramic radiograph demonstrating zygomatic in a type 2B configuration with addition of pterygoid implants.
3. Conclusion
Patients may present either after long periods of maxillary denture wear or following loss of the dentition related to severe periodontal issues that result in severe atrophy of the maxilla that hamper implant placement to allow restoration of the arch. Extensive bone grafting may be performed but those procedures increase the treatment costs. Additionally, treatment time may be drastically increased precluding some patients from accepting treatment.
The decision making presented herein is clinical based on the radiographic appearance of the patient acquired during treatment planning. This will help aid the practitioner in discussion with the patient as to what treatment options are available and also to those only performing the restorative aspects of treatment in discussion with the surgeon when formulating the joint treatment plan that will be then discussed with the patient.
Author contributions
*Provided clinical information and technical details for the paper, reviewed article draft and provided editorial input.
**Wrote the article draft and edited based on other author feedback.
***Reviewed article draft and provided editorial input.
Financial support
None.
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Availability of data and material
Not applicable.
Declaration of competing interest
The authors report no conflict of interests or commercial financial relationship.
Acknowledgements
None.
References
- 1.Cooper L.F., Thalji G., Al-Tarawneh S. Are nongrafting solutions viable for dental implant treatment in limited bone volume? Comp Cont Educ Dent. 2020 Jul/Aug;41(7):368–376. quiz 377. PMID: 32687381. [PubMed] [Google Scholar]
- 2.Sales P.H., Gomes M.V., Oliveira-Neto O.B., de Lima F.J., Leão J.C. Quality assessment of systematic reviews regarding the effectiveness of zygomatic implants: an overview of systematic reviews. Med Oral Patol Oral Cir Bucal. 2020 Jul 1;25(4):e541–e548. doi: 10.4317/medoral.23569. PMID: 32520920; PMCID: PMC7338062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Maló P., Nobre Mde A., Lopes A., Ferro A., Moss S. Five-year outcome of a retrospective cohort study on the rehabilitation of completely edentulous atrophic maxillae with immediately loaded zygomatic implants placed extra-maxillary. Eur J Oral Implant. 2014 Autumn;7(3):267–281. PMID: 25237671. [PubMed] [Google Scholar]
- 4.Yalçın M., Can S., Akbaş M., et al. Retrospective analysis of zygomatic implants for maxillary prosthetic rehabilitation. Int J Oral Maxillofac Implants. 2020 Jul/Aug;35(4):750–756. doi: 10.11607/jomi.8196. PMID: 32724927. [DOI] [PubMed] [Google Scholar]
- 5.Petrungaro P.S., Kurtzman G.M., Gonzales S., Villegas C. Zygomatic implants for the management of severe alveolar atrophy in the partial or completely edentulous maxilla. Comp Cont Educ Dent. 2018 Oct;39(9):636–645. PMID: 30299113. [PubMed] [Google Scholar]
- 6.Bedrossian E. In: Implant Treatment Planning for the Edentulous Patient: A Graftless Approach to Immediate Loading. Bedrossian E., editor. Mosby Elsevier; Missouri: 2011. Systematic pretreatment evaluation of the edentulous maxilla; pp. 37–40. [Google Scholar]
- 7.Sadowsky S.J., Bedrossian E. Evidenced-based criteria for differential treatment planning of implant restorations for the partially edentulous patient. J Prosthodont. 2013 Jun;22(4):319–329. doi: 10.1111/jopr.12014. Epub 2013 Feb 6. PMID: 23387389. [DOI] [PubMed] [Google Scholar]
- 8.Candel-Martí E., Carrillo-García C., Peñarrocha-Oltra D., Peñarrocha-Diago M. Rehabilitation of atrophic posterior maxilla with zygomatic implants: review. J Oral Implantol. 2012 Oct;38(5):653–657. doi: 10.1563/AAID-JOI-D-10-00126. Epub 2011 Feb 18. PMID: 21332329. [DOI] [PubMed] [Google Scholar]
- 9.Candel E., Peñarrocha D., Peñarrocha M. Rehabilitation of the atrophic posterior maxilla with pterygoid implants: a review. J Oral Implantol. 2012 Sep;38:461–466. doi: 10.1563/AAID-JOI-D-10-00200. Epub 2011 May 13. PMID: 21568718. [DOI] [PubMed] [Google Scholar]
- 10.Migliorança R.M., Coppedê A., Dias Rezende R.C., de Mayo T. Restoration of the edentulous maxilla using extrasinus zygomatic implants combined with anterior conventional implants: a retrospective study. Int J Oral Maxillofac Implants. 2011 May-Jun;26(3):665–672. PMID: 21691615. [PubMed] [Google Scholar]
- 11.Davó R., David L. Quad zygoma: technique and realities. Oral Maxillofac Surg Clin. 2019 May;31(2):285–297. doi: 10.1016/j.coms.2018.12.006. PMID: 30947849. [DOI] [PubMed] [Google Scholar]
- 12.Duan Y., Chandran R., Cherry D. Influence of alveolar bone defects on the stress distribution in quad zygomatic implant-supported maxillary prosthesis. Int J Oral Maxillofac Implants. 2018 May/Jun;33(3):693–700. doi: 10.11607/jomi.4692. PMID: 29763505. [DOI] [PubMed] [Google Scholar]
- 13.Aboul-Hosn Centenero S., Lázaro A., Giralt-Hernando M., Hernández-Alfaro F. Zygoma quad compared with 2 zygomatic implants: a systematic review and meta-analysis. Implant Dent. 2018 Jan 29 doi: 10.1097/ID.0000000000000726. Epub ahead of print. PMID: 29394179. [DOI] [PubMed] [Google Scholar]
- 14.Petrungaro P.S., Gonzales S., Villegas C., Yousef J., Arango A. A retrospective study of a multi-center case series of 452 zygomatic implants placed over 5 Years for treatment of severe maxillary atrophy. Comp Cont Educ Dent. 2020 Apr;41(4):232–241. PMID: 32255655. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.