Abstract
Introduction
Adolescence is a critical stage of rapid biological, emotional and social change and development. Adolescents and young adults (AYA) with asthma and allergies need to develop the knowledge and skills to self‐manage their health independently. Healthcare professionals (HCP), parents and their wider network play an essential role in supporting AYA in this process. Previous work showed significant limitations in transition care across Europe. In 2020, the first evidence‐based guideline on effective transition for AYA with asthma and allergies was published by EAACI.
Aim
We herein summarize practical resources to support this guideline's implementation in clinical practice.
Methods
For this purpose, multi‐stakeholder Task Force members searched for resources in peer review journals and grey literature. These resources were included if relevant and of good quality and were pragmatically rated for their evidence‐basis and user friendliness.
Results
Resources identified covered a range of topics and targeted healthcare professionals, AYA, parents/carers, schools, workplace and wider community. Most resources were in English, web‐based and had limited evidence‐basis.
Conclusions
This position paper provides a valuable selection of practical resources for all stakeholders to support effective transitional care for AYA with asthma and allergies. Future research should focus on developing validated, patient‐centred tools to further assist evidence‐based transition care.
Keywords: adolescent, allergy, asthma, transition, young adult
Short abstract

Abbreviations
- AYA
adolescents and young adults
- CBT
cognitive‐behavioural therapy
- HCP
healthcare professionals
- MI
Motivational Interviewing
1. BACKGROUND
Adolescence is a challenging time for patients, their parents and their healthcare professionals (HCP). 1 Although Adolescent and Young Adult (AYA) patients are generally not seen as a vulnerable or ‘in need’ group, they have an unexpectedly high risk of morbidity and mortality. This includes a surprisingly high rate of asthma death and fatal anaphylaxis, which peaks in AYA. 2 , 3
The inclusion of adolescent health in the United Nations secretary general's Global Strategy for Women's and Children's Health in 2015 reflects a growing awareness of the importance and specificity of this stage of development. Adolescence is a critical stage of life characterized by rapid biological, emotional and social development, during which skills for a productive, healthy and satisfying life are developed. As part of this period of growth and development, the status of primary relationships and level of autonomy also shifts. The need to take on responsibility for behaviours and learn to cope with everyday events and challenges falls increasingly on the adolescent. 4 Together with these usual developmental tasks, adolescents with an allergic disease face additional challenges that may render them more vulnerable to adverse outcomes. This may include psychological issues (such as poor quality of life) and difficulties around adherence and self‐management (such as risk‐taking behaviours). These are common as AYA explore their boundaries and are influenced by peer pressure as parents ‘let go’. They may include exposure to smoking, alcohol, other recreational drugs or food allergens in social contexts, which that may impact on their asthma control or risk of accidental exposures to foods. 1 Support is therefore vital for this age group.
However, a recent European survey found that most HCP have not received training in how to support adolescents and young adults (AYA) with allergic conditions and do not have an established paediatric to adult healthcare transition process. 5 Ensuring that every adolescent has the knowledge and skills to self‐manage their allergy with confidence is essential for achieving good mental and physical health and development goals and lower risk of adverse outcomes. This is equally necessary when patients stay within the same service as adults, as well as when they are transferred into an adult service, in which case the responsibility for an effective transition is shared by the paediatric and adult teams.
The European Academy of Allergy and Clinical Immunology (EAACI) transition guideline was developed by a multi‐stakeholder Task Force from across Europe using evidence‐based principles and published to support HCP in effectively managing AYA. 4 Its recommendations have been favourably reviewed by AYA and parents from across Europe. 6 This paper aimed to provide HCP (both paediatric and adult, as well as those seeing all ages), AYA and families with practical and targeted resources to support successful self‐management of asthma and allergic conditions.
2. METHODS
The EAACI Adolescent and Young Adult task force (a European multidisciplinary team of professionals and patient representatives) reviewed the resources available to support successful self‐management and selected those that are likely to be most helpful to HCP, AYA, their families and the wider community. Peer review journals and grey literature were searched, including material from websites, publications from patients, scientific and government organizations. Search engines used included PubMed, Medline and EMBASE, as well as generic browsers such as Google and screening of patient organizations for AYA transition material. Members were allocated into areas, each with a designated lead, as follows: Guidelines (KK), Transition programme examples (CG), Transition assessment tools (MVO), Approach to assessing adolescent patients (BD), Transition report and plan for individual patients (BD), Audit and performance indicators (EA), Psychology support training (RK), Self‐management plans (CA, FT), General transition information and advice for patients (TG, HG), Specific transition information and advice for patients (MVO), Allergy passport (PC), Information and advice for schools and the workplace (HP), Information and advice for friends, peers and the wider society (MP). Key search terms were agreed for each area. Any resources found that met our aim were reviewed by the Task Force and included if relevant and deemed of sufficient quality based on the content (scope, evidence‐base/accuracy, usefulness) and form. Searches were undertaken in common European languages and the country of origin is identified in the Toolkit tables. Resources were pragmatically rated in terms of whether the information provided was based on evidence as ‘moderate’ (limited evidence provided, cited or referred to), ‘good’ (some evidence provided, cited or referred to, with limitations) and ‘very good’ (solid evidence provided, cited or referred to). Sources were also subjectively rated with regards to user friendliness as ‘moderate’, ‘good’ or ‘very good’ based on the appropriateness of language/style, clarity and design. Results were reviewed by the core group (MVO, CG with arbitration by GR where needed) and discussed at regular meetings with the rest of the TF to produce a thorough yet pragmatic selection of resources. Web links were tested and functioning at the time of publication.
3. RESULTS—THE TOOLBOX
A summary of the selection of the key resources is presented in Table 1, with further description in Tables 2(for HCP) and 3 (for non‐HCP). Additional resources available for HCP are presented in Table S1 in the online supplement. The vast majority of the 82 resources selected are available only in English and have been developed in English‐speaking countries (UK: 32, USA: 15, Australia: 10, Canada: 5, Ireland: 1) or global organizations (WHO: 4, EAACI: 2). A minority of resources have been developed in other languages in addition to English (USA‐ English and Spanish: 4, Canada‐ English and French: 1, EAACI and EFA‐ multiple languages:1) or in other countries in their own languages (Germany: 4, Denmark: 2). Figure 1 provides an overview of our approach to support an AYA with asthma and allergies. It emphasizes the need for awareness and action and explains how to support transition in an effective manner. A glossary of terms is available in Table S2 in the online supplement.
TABLE 1.
Summary of key transition resources for healthcare professionals as well as adolescents and young adults (AYA), parents, carers and wider family, school, work and wider community
| 1. Key transition resources for healthcare professionals | ||
| Resource (title, reference/link, language, country, year of publication or last update) | Document type | Target audience |
| A. Guidelines and transition programmes | ||
| Allergy‐ and asthma‐specific AYA transition resources | ||
| EAACI guideline on the effective transition of adolescents and young adults with allergy and asthma (English, Europe, 2020) | Guideline | HCP |
| Children and young people's allergy network Scotland. Young People's Transition Pathway to Independent Self‐Management of Allergies (English, Scotland, 2019) | Pathway | HCP |
| Generic AYA Transition Resources | ||
| Got Transition (English, USA, regularly updated) | Toolkit | HCP, AYA, Parents/Families |
| World Health Organization (WHO). Resource bank for Adolescent Health from the interdepartmental working group on adolescent health. (English, World, regularly updated) | Guidelines, norms and standards, training packages, policy, implementation guidance | HCP, Schools |
| B. Transition readiness assessment tools | ||
| Leaving home: Helping teens with allergic conditions become independent (English, US, 2016) | Review paper | HCP |
| ’Ready Steady Go’ Transition Programme (English, UK, regularly updated) | Generic transition programme | HCP, Parent/AYA |
| Transition Readiness Assessment Questionnaire ‘TRAQ’ (English, US, 2021) | Generic transition programme | HCP, Parent/AYA |
| Measuring the preparation for transition from paediatric focused to adult focused health care: The adolescent assessment of preparation for transition (ADAPT) survey (English/Spanish, USA, 2014) | Outcome measure | HCP, Parent/AYA |
| C. Approach to AYA | ||
| General approach including communication skills | ||
| Canadian Association of Paediatric Health Centres ‐ Transition YSHCN Guideline (English, Canada, 2016) | Guideline | HCP |
| Key Principles for Transition of Young People from Paediatric to Adult Health Care (English, Australia 2014) | Guideline | HCP |
| Psychosocial assessment of AYA patients | ||
| Fifteen‐minute consultation: Communicating with young people—how to use HEEADSSS, a psychosocial interview for adolescents (English, UK, 2018) | Consultation tool | HCP |
| D. Transition report | ||
| GOT Transition: Implementation Guide, Core Element 5 ‐ Transfer of Care (English, US, 2020) | Implementation Guide | HCP |
| E. Audit and key performance indicators | ||
| World Health Organization. Quality Assessment Guidebook and Global standards for quality healthcare services for adolescents (English, world, 2009/2015) | Guideline, Standards | HCP |
| F. Resources to help with psychological impact of asthma and allergy | ||
| Getselfhelp (UK) (English, UK. Regularly updated) | Online CBT self‐help and therapy resources | HCP, parents |
| Training in Motivational Interviewing (MI). Royal College of Psychiatrists (English, UK, regularly updated) | Website | HCP |
| 2. Transition resources for adolescents and young adults (AYA), parents, carers and wider family, school, work and wider community | ||
|---|---|---|
| Resource (title, reference/link, language, country, year of publication or last update) | Type | Target Audience |
| A. General transition information and advice | ||
| Generic transition | ||
| Ready Steady Go (English, UK, 2021) | Generic transition programme | AYA, Parents/Families |
| Got Transition (English, USA, 2021) | Toolkit | AYA, Parents/Families |
| Allergy and asthma‐specific transition | ||
| Patient information leaflet’Your transition from children's to adult allergy services' (English, UK, 2021) | Patient information leaflet | AYA |
| Children and young people's allergy network Scotland. Young People's Transition Pathway to Independent Self‐Management of Allergies (English, Scotland, 2019) | Pathway | Sections for AYA and Parents/Families |
| EAACI Guideline (English/French/Italian/Spanish /Portuguese/Greek/Russian/ German/Danish, Europe, 2020. | Lay guideline recommendations | AYA, Parents, caregivers |
| B. Comprehensive resources for specific advice on asthma and allergy | ||
| 250 k Allergy Awareness Project (English, Australia, 2022) | Website | AYA |
| Allergy & Anaphylaxis Australia (English, Australia, 2022) | Website | AYA, parents, caregivers, school, work, wider community, food industry |
| Food Allergy Canada (English/French, Canada, 2021) | Website | AYA, parents, caregivers, school, work, wider community |
| Food Allergy Research & Education (FARE) (English/Spanish, USA, 2022) | Website | AYA, parents, caregivers, school, work, wider community |
| Asthma + Lung UK (English, UK, 2022) | Website | AYA, parents, caregivers, school staff |
| Nottingham Support Group for Carers of Children with (Atopic) Eczema (English, USA, 2022) | Website | Parents, caregivers, AYA |
| Allergy UK (English, UK, regularly updated) | Website | AYA, parents, caregivers, school, work, wider community |
| C. Travel | ||
| 250 K – A youth allergy awareness project by the National Allergy Strategy (English, Australia, 2022) | Webpage | AYA |
| Food Allergy Research & Education (FARE) (English, USA, 2022) | Webpage | AYA |
| D. Career and work advice | ||
| ‘Allergic Living’ (English, USA, 2022) | Webpage article | AYA, parents/caregivers. |
| Health & Safety Authority (English, Ireland, 2022) | Webpage | Not specific |
| 250 K – A youth allergy awareness project by the National Allergy Strategy (English, Australia, 2022) | Webpage | AYA |
| Food Allergy Canada (English, Canada, 2022) | Webpage | AYA |
| E. Resources for Psychological support | ||
| Generic resources for psychological support | ||
| ‘Young minds’ Charity (English, UK, 2022) | Webpage | AYA, parents, friends, schools, youth workers |
| ‘SilverCloud’ (English, UK, 2022) | Online CBT‐based self‐help programme | AYA, parents/carers |
| ‘Online‐therapy.com’ (English, worldwide, 2022) | Online‐based mental health team | AYA, parents |
| ‘Moodgym’ (English, Australia, 2022) | Online CBT‐based resource | AYA, Parents |
| Living Life to the Full (young people section) (English, UK, 2022) | Online self‐help training package based on CBT | AYA, Parents |
| Allergy and asthma‐specific resources for psychological support | ||
| ‘Asthma + Lung UK’ charity (English, UK, 2022) | Webpage | AYA, parents |
| Healthtalk.org (English, UK, 2021) | Webpage | AYA |
| National Eczema Association (English, UA, 2021) | Webpage article | AYA |
| Food Allergy Research and Education (FARE) (English, US, 2022) | Webpage article | AYA |
| Patient voices – ‘Terrific teens’ (English, UK, 2017) | Webpage | AYA, parents |
| F. School advice | ||
| Anaphylaxis Campaign, ‘Making Schools Safer’ Project (English, UK, 2022) | Webpage | AYA, parents |
| Asthma Initiative of Michigan (AIM) (English, USA, 2022) | Webpage | Parent, AYA, school staff |
| AllergyHome (English/Spanish, USA, 2022) | Webpage | Caregivers, other parents |
| Food Allergy & Anaphylaxis Connection Team (FAACT) (English, USA, 2022) | Webpage | AYA, parents, caregivers, school community |
| Allergy & Asthma Network (English/Spanish, USA, 2022) | Webpage | Parents, caregivers |
| G. Resources in other Languages | ||
| EAACI resources for patients (English/other languages, European‐international, 2022) | Portal | AYA, parents, caregivers, schools, other stakeholders |
| European Federation of Allergy and Airways Diseases Patients' Associations (EFA) (English/other languages, European‐international, 2022) | Portal | AYA, parents, caregivers, schools, other stakeholders |
Abbreviations: AYA, Adolescents and young adults; CBT, cognitive‐behavioural therapy; HCP, Healthcare professionals; MI, Motivational Interviewing.
All the web links provided were last accessed on 18/02/2022. The resources listed are described in more detail in Tables 2 and 3.
The evidenced‐based approach was reviewed and agreed by the Task Force members and judged in a pragmatic way into three categories with increasing level of evidence‐based approach: *moderate‐ some evidence‐based approach noted, the resource was included because of well‐rounded clinical and practical (professional) experience; ** good and *** very good.
* User‐friendliness was reviewed and agreed by the Task Force members and judged in a pragmatic way into moderate; ** good; *** very good.
TABLE 2.
Key transition resources for healthcare professionals
| Resource (title, reference/link, language, country, year of publication or last update) | Document type | Target audience | Evidence‐based approach a | User friendliness b | Comments |
|---|---|---|---|---|---|
| A. Guidelines and transition programmes | |||||
| Allergy & asthma specific AYA transition resources | |||||
| EAACI guideline on the effective transition of adolescents and young adults with allergy and asthma https://onlinelibrary.wiley.com/doi/full/10.1111/all.14459 (English, Europe, 2020) | Guideline | HCP | *** | *** |
Specifically addresses transition for AYA with allergies, asthma |
| Children and young people's allergy network Scotland. Young People's Transition Pathway to Independent Self‐Management of Allergies https://www.cyans.scot.nhs.uk/wp‐content/uploads/2019/10/Transition‐allergy‐pathway‐v1.1.pdf?x54518 (English, Scotland, 2019) | Pathway | HCP | * | *** | Includes condition‐specific transition guidance for asthma and allergies, bite‐sized topics, transition plan and example questions for discussion with AYA in clinic. |
| Generic AYA Transition Resources | |||||
| Got Transition (USA) https://www.gottransition.org/ (English, USA, regularly updated) | Toolkit |
HCP, AYA, Parents All |
** | *** | Designed to allow stakeholders to ‘get going’. Describes 6 core elements, consists of a range of helpful figures, tables and leaflets to better understand the transition process. |
| World Health Organization (WHO). Resource bank for Adolescent Health from the interdepartmental working group on adolescent health.https://www.who.int/teams/maternal‐newborn‐child‐adolescent‐health‐and‐ageing/adolescent‐and‐young‐adult‐health/resource‐bank‐for‐adolescent‐health (English, World, regularly updated) | Guidelines, norms and standards, training packages, policy and future directions and implementation guidance | HCP, schools | *** | ** | Generic evidence‐based resources on common AYA challenges and needs produced by multidisciplinary expert panel from WHO. Includes guidelines and training packages on mental health, sexual and reproductive health, youth violence and school health as well as a ‘pocket book’, a ‘job aid’ and a core competencies tool for Primary Care HCP managing AYA. Includes norms and standards for health care and school health services, and standards on drug use prevention and treatment. Policy aspects include a brief on ‘building an adolescent competent workforce’ supporting advocacy to invest in competency‐based educational programmes in adolescent health. |
| B. Transition readiness assessment tools | |||||
| Leaving home: Helping teens with allergic conditions become independent. Stukus DR, Nassef M, Rubin M. Ann Allergy Asthma Immunol. 2016;116(5):388–91. (English, US, 2016) | Review | HCP | ** | *** | Includes overview and checklist of issues to address in food allergy, asthma and allergic rhinitis during transition. |
| ’Ready Steady Go’ Transition Programme https://www.readysteadygo.net/ Nagra A, et al. Arch Dis Child Educ Pract Ed 2015;0:1–8. (English, UK, regularly updated) | Generic transition programme | HCP, Parent/AYA | * | *** | Holistic gradual and tailored approach to transition. Includes introductory information to parents and AYA (leaflet, video) and questionnaires for the 4 gradual stages: ‘Ready’, ‘Steady’, ‘Go’ and ‘Hello to Adult Services’. Promotes AYA's independence by encouraging proactiveness, goal setting, self‐advocacy and shared decision‐making. Involves parents/carers to support AYA and ‘let go’ throughout transition. Covers a number of areas: knowledge, self‐advocacy, health & lifestyle, daily living, leisure, studies/work/future, emotions and transfer. ‘Easy read’ versions in other languages available (English, Dutch, Greek., French, Portuguese). |
| Transition Readiness Assessment Questionnaire ‘TRAQ’ Wood. Acad Pediatr 2014;14(4):415–22. Johnson. J Pediatr Nurs 2021;59:188–195 (English, US, 2021) | Generic transition programme | HCP, Parent/AYA | *** | ** | Single questionnaire covering AYA's individual skills in a range of practical areas related to self‐management: managing medications, appointment keeping, tracking health issues, talking with providers, managing daily activities. Validated, Translation into other languages underway. |
| ADAPT Survey, CEPQM. Measuring the preparation for transition from paediatric focused to adult focused health care: The adolescent assessment of preparation for transition (ADAPT) survey. Boston, MA: Center of Excellence for Pediatric Quality Measurement; July 2014. Patient reported experience measure (PREM) http://www.childrenshospital.org/research/centers‐departmental‐programs/center‐of‐excellence‐for‐pediatric‐quality‐measurement‐cepqm/cepqm‐measures/transition‐from‐child‐focused‐to‐adult‐focused‐care (Overview) http://www.childrenshospital.org/research/centers‐departmental‐programs/center‐of‐excellence‐for‐pediatric‐quality‐measurement‐cepqm/cepqm‐measures/transition‐from‐child‐focused‐to‐adult‐focused‐care/content (Content). (English/Spanish, USA, 2014) | Outcome measure | HCP, Parent/AYA | ** | ** |
The only validated transition specific outcome measure identified. |
| C. Approach to AYA | |||||
| General approach including communication skills | |||||
| Canadian Association of Paediatric Health Centres ‐ Transition YSHCN Guideline Canadian Association of Paediatric Health Centres, 2016. A guideline for transition from paediatric to adult health care for youth with special healthcare needs: a national approach. CAPHC Natl Transitions Community Pract, pp.1–30. (English, Canada, 2016) | Guideline | HCP | *** | ** | Guideline resource with focus on general approach (see Appendix 2, Domain 1). Person‐centred holistic approach, focused approach on adolescent development, scope and timeframe for transition. |
| Key Principles for Transition of Young People from Paediatric to Adult Health Care Agency for Clinical Innovation and Trapeze, The Sydney Children's Hospital Network, 2014. Key principles for transition of young people from paediatric to adult health care. (English, Australia 2014) | Guideline | HCP | *** | ** |
Guideline resource with focus on general approach (see Principle 4 ‐ Good communication and shared responsibility). |
| Psychosocial assessment of AYA patients | |||||
| Fifteen‐minute consultation: Communicating with young people—how to use HEEADSSS, a psychosocial interview for adolescents Doukrou M, Segal TY. Fifteen‐minute consultation: Communicating with young people—How to use HEEADSSS, a psychosocial interview for adolescents. Archives of Disease in Childhood‐Education and Practice. 2018;103(1):15–9. (English, UK, 2018) | Consultation tool | HCP | * | *** | Covers HEADSSS (psychosocial risk assessment tool), CRAFFT (substance use screening tool) and a screening tool to assess depression. HEADSSS stands for ‘Home, Education & Employment, Activities, Drugs/Drinking, Sex, Self‐harm, depression & suicide, Safety (including social media/online)’. CRAFFT stands for ‘Car, Relax, Alone, Forget, Friends, Trouble’. |
| D. Transition report | |||||
| GOT Transition: Implementation Guide, Core Element 5 ‐ Transfer of Care White P, Schmidt A, Ilango S, Shorr J, Beck D, McManus M. Six Core Elements of Health Care Transition TM 3.0: An Implementation Guide. Washington, DC: Got Transition, The National Alliance to Advance Adolescent Health, July 2020. (English, US, 2020) | Implementation Guide from Guideline | HCP | ** | *** | This implementation guide focuses on transfer of care as the one of the six core elements of transitioning youth to an adult healthcare provider. It includes quality improvement considerations, tools and measurements as well as sample transfer of care tools. |
| E. Audit and key performance indicators | |||||
| World Health Organization. Quality Assessment Guidebook: a guide to assessing health services for adolescent clients http://apps.who.int/iris/bitstream/handle/10665/44240/9789241598859_eng.pdf;jsessionid=6E8737D3B6B4AFDAC21599ED17E80E65?sequence=1 (English, world, 2009) Global standards for quality healthcare services for adolescents: a guide to implement a standards‐driven approach to improve the quality of healthcare services for adolescents (English, world, 2015) | Guideline | HCP | ** | ** | ‘Intended to enable public health programme managers to assess the quality of health service provision to adolescents, and to take appropriate action (including problem solving and action planning) where the quality is found wanting’. Suitable for countries with and without agreed upon national quality standards. Includes expected characteristics of adolescent‐friendly services (equitable, accessible, appropriate, acceptable and effective). Provides service assessment preparation information, scoring sheets and interview tools for multiple stakeholders (from healthcare provides to adolescent and community members). Includes a checklist to assess clinical competencies of health workers on a range of areas, for example, sexual health. The 2015 Implementation guide ‘provides detailed guidance on identifying what actions need to be taken to implement the standards at the national, district and facility levels’. |
| F. Resources to help with psychological impact of asthma and allergy | |||||
|
Getselfhelp (UK), Cognitive‐behavioural therapy (CBT) resources Getselfhelp.co.uk (English, UK. Regularly updated) |
Online CBT self‐help and therapy resources | HCP, parents | *** CBT as a therapy has a good evidence base | ** |
CBT self‐help and therapy resources, including worksheets and information sheets and self‐help mp3s |
| Career in CBT, BABCP https://babcp.com/Careers/How‐to‐Choose‐a‐CBT‐Training‐Course (English, UK. Regularly updated) | Information on formal CBT training | HCP | *** CBT as a therapy has a good evidence base | ** | BABCP is the UK professional body for CBT and has a list of accredited training courses offered in the UK |
| Training in Motivational Interviewing (MI). Royal College of Psychiatrists. https://elearning.rcpsych.ac.uk/learningmodules/introductiontomotivational.aspx (English, UK, regularly updated) | Website for Royal College of Psychiatrists | HCP | *** MI as a therapy has a good evidence base | Free training in MI techniques | |
Abbreviations: AYA, Adolescents and young adults; CBT, cognitive‐behavioural therapy; HCP, Healthcare professionals; MI, Motivational Interviewing.
All the web links provided were last accessed on 18/02/2022.
The evidenced‐based approach was reviewed and agreed by the Task Force members and judged in a pragmatic way into three categories with increasing level of evidence‐based approach: *moderate‐ some evidence‐based approach noted, the resource was included because of well‐rounded clinical and practical (professional) experience; ** good and *** very good.
*User‐friendliness was reviewed and agreed by the Task Force members and judged in a pragmatic way into moderate; ** good; *** very good.
FIGURE 1.
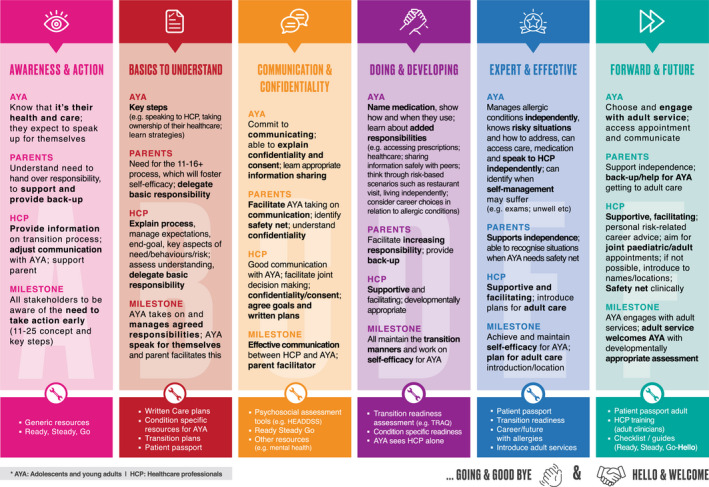
The ‘A to F' of managing transition
TABLE 3.
Transition resources for adolescents and young adults (AYA), parents, carers and wider family, school, work and wider community
| Resource (title, reference/link, language, country, year of publication or last update) | Type | Target Audience | a Evidence base | b User friendliness | Comments |
|---|---|---|---|---|---|
| A. General transition information and advice | |||||
| Generic transition | |||||
| Ready Steady Go https://www.readysteadygo.net/ (English, UK, 2021) | Generic transition programme | AYA, Parents/Families | * | *** | Holistic gradual and tailored approach to transition. Parent and patient area on website with introductory video and written information including PDFs to download about the different steps and questionnaires, including ‘hello to children services', ‘ready’, ‘steady’, ‘go’ and ‘hello to adult services'. ‘Easy read’ versions in other languages available (English, Dutch, Greek., French, Portuguese). |
| Got Transition https://www.gottransition.org/parents‐caregivers/ (English, USA, 2021) | Toolkit | AYA, Parents/Families | * | *** | Patient and parent/caregiver website section with a range of resources in English and Spanish, including introductory information, an infographic for AYA on practical aspects of transition, frequently asked questions, guidance for AYA to set up a medical ID in their smartphone, and a family toolkit (booklet‐type PDF including detailed information on practical aspects of transition, timelines, readiness assessment tools and final readiness quiz). |
| Allergy and asthma‐specific transition | |||||
| Patient information leaflet’Your transition from children's allergy services to adult allergy services'. https://www.evelinalondon.nhs.uk/resources/patient‐information/transition‐to‐adult‐allergy‐for‐children.pdf (English, UK, 2021) | Patient information leaflet | AYA | * | ** | Introductory information leaflet for AYA (age 13–18) with allergies on the transition process in a paediatric allergy service, including stakeholders involved, steps and milestones. |
| Children and young people's allergy network Scotland. Young People's Transition Pathway to Independent Self‐Management of Allergies: https://www.cyans.scot.nhs.uk/wp‐content/uploads/2019/10/Transition‐allergy‐pathway‐v1.1.pdf?x54518 (English, Scotland, 2019) | Pathway | Sections for AYA and Parents/Families | * | *** | HCP Pathway for Young People's Transition for Independent Self‐Management of Allergies. Focus on understanding transition. Includes bespoke areas explaining how transition works |
| EAACI Guideline https://patients.eaaci.org/eaaci‐guideline‐on‐the‐effective‐transition‐of‐adolescents‐and‐young‐adults‐with‐allergy‐and‐asthma/ (English/French/Italian/Spanish /Portuguese/Greek/Russian/ German/Danish, Europe, 2020. | Lay guideline recommendations | AYA, Parents, caregivers | *** | ** | Evidence‐based guideline recommendations adapted to lay language |
| B. Comprehensive resources for specific advice on asthma and allergy | |||||
| 250 k Allergy Awareness Project: https://250k.org.au (English, Australia, 2022) | Website | AYA | * | *** | Specifically addressed to school‐aged teens and young adults, with specific sections for each age group. Focus on food allergy, also covers hay fever, asthma and atopic eczema. Comprehensive resources including explanations, advice and top tips, illustrations and videos. Specific sections addressing food avoidance (prepacked food, eating out, dating, camping, travelling, managing anxiety), and for young adults also moving out, university, workplace, starting a family. Links to action plans for asthma (https://d8z57tiamduo7.cloudfront.net/resources/341‐NAC‐Written‐Asthma‐Action‐Plan‐2015_Colour.pdf), anaphylaxis (https://www.allergy.org.au/hp/anaphylaxis/ascia‐action‐plan‐for‐anaphylaxis) and atopic eczema (https://www.allergy.org.au/images/pcc/ASCIA_Eczema_Action_Plan_2021.pdf) suitable for AYA. Attractive and user friendly. |
| Allergy & Anaphylaxis Australia http://www.allergyfacts.org.au/ (English, Australia, 2022) (some contents translated to other languages) | Website | AYA, parents, caregivers, school, work and wider community, food industry | * | *** | Wide range of resources focused on food allergy and anaphylaxis. Written advice and videos on symptoms, diagnosis, managing reactions, living with the risk in different contexts. Includes chef card template translated to multiple languages including Spanish, Portuguese, French, German, Greek, Croatian, Russian, and many Asian Languages. Specific sections for young adults over 18 and 13–18 year olds, including advice on adapting to secondary school, travelling, dating, AAI use. Also, sections for workplace, food industry and first aid providers. Sections with lay explanations on the full range of allergic conditions, from latex allergy to eosinophilic oesophagitis. |
| Food Allergy Canada https:/ /foodallergycanada.ca/living‐with‐allergies/ongoing‐allergy‐management/teens‐and‐young‐adults/ (English/French, Canada, 2021) | Website | AYA, parents, caregivers, school, work and wider community | * | *** | Focus on food allergy. Specific section for AYA covering reading labels, avoiding cross‐contamination, kitchen tips, recipes and lifestyle issues such as dating, partying and eating out. Attractive and accessible. Advice for high school, workplace, moving out and other environments such as holidays and travelling. |
| Food Allergy Research & Education (FARE) https://www.foodallergy.org/ (English/Spanish, USA, 2022) | Website | AYA, parents, caregivers, school, work and wider community | * | *** | Focus on food allergy. Resources can be searched/filtered by audience (e.g. ‘adolescents’, or ‘college staff'), food allergen and type of resource. Includes toolkits, insights, research and practical tips, covering avoiding allergens and daily life issues such as reading labels, cross‐contamination, shopping, cooking and cleaning safely, recipes, relationships and dating, eating out, travelling and preparing for college. Offers virtual talks for AYA with food allergy willing to connect with peers. |
| Asthma + Lung UK https://www.asthma.org.uk/ (English, UK, 2022) | Website | AYA, parents, caregivers, school staff. | * | *** | Focused on asthma. Covers medical facts, including understanding asthma, triggers, attacks and practical management aspects such as information on medications, asthma plans and practical videos on how to use a wide range of inhalers. |
| Nottingham Support Group for Carers of Children with (Atopic) Eczema http://www.nottinghameczema.org.uk/information/index.aspx (English, UK, 2022) | Website | Parents, caregivers, AYA | * | ** | Addressed to parents of children with atopic eczema. Detailed info leaflets on multiple areas, including understanding eczema, triggers and management including advanced strategies such as wet wraps. Many leaflets are relevant for AYA, particularly those on teenage eczema, eczema and bullying, stress, holidays, travelling or exercise. |
| Allergy UK: http://www.allergyuk.org/ (English, UK, 2022) | Website | AYA, parents, caregivers, school, work and wider community | * | *** | Not AYA‐specific. Comprehensive resources on a wide range of allergic conditions from hay fever to food or venom allergy. Includes factsheets (downloadable pdf) on multiple practical management aspects such as avoidance of environmental or food allergen, food and symptoms diary and how to complete it, advice on shopping and cooking for a restricted diet, allergy recipes and patients' testimonials. Attractive and user friendly. |
| C. Travel | |||||
| 250 K – A youth allergy awareness project by the National Allergy Strategy https://teen.250k.org.au/travelling‐with‐a‐food‐allergy/ (English, Australia, 2022) | Webpage | AYA | * | *** | As above. Includes advice, videos and patient stories on travelling with food allergy. Includes links to Allergy & Anaphylaxis Australia travel information, translated chef cards, and ASCIA travel plan and checklists/help sheets, as well as link to websites offering translated information such as: https://www.allergytranslation.com, https://www.selectwisely.com and https://dietarycard.com |
| Anaphylaxis Campaign https://www.anaphylaxis.org.uk/living‐with‐anaphylaxis/travelling/ (English, UK, 2022) | Webpage | AYA, parents, caregivers | * | *** | As above. Includes free‐download printable resources on: Preparing to Travel, Booking the flight, Airline Allergy Policies, Travel Insurance, Checklist for the flight day, Eating Out with food allergy when abroad. Includes link to websites that offer a free translation dictionary for over 200 allergy‐related words in all European national |
| Food Allergy Research & Education (FARE) (1)https://www.foodallergy.org/resources/traveling‐teen (2)https://www.foodallergy.org/resources?_limit=12&_page=1&type=14 (English, USA, 2022) | Webpage | AYA | * | ** | As above. (1) Advice for AYA with food allergy or anaphylaxis on School Trips and Travel Abroad. (2) Advice before Airline/International travels. Includes free‐download printable resources on checklist to remember before traveling and helpful travel tip sheets specific for some countries (Australia, Brazil, Canada, Germany, Hong Kong, Israel, Italy, Japan, Mexico, New Zealand, Spain, United Kingdom, United States). |
| D. Career and work advice | |||||
| Allergic Living https://www.allergicliving.com/2018/05/15/allergies‐and‐summer‐jobs‐tips‐for‐teenagers‐hunting‐for‐work/ (English, USA, 2022)https://acaai.org/news/back‐school‐year‐far‐back‐normal‐kids‐allergies‐and‐asthma | Webpage article | AYA, parents/caregivers. | * | ** | Advice and patient stories for AYA with asthma and allergy planning for Summer jobs. |
| Health & Safety Authority https://www.hsa.ie/eng/Workplace_Health/Occupational_Asthma_and_Dermatitis/Occupational_Asthma_Frequently_Asked_Questions/ (English, Ireland, 2022)https://acaai.org/news/back‐school‐year‐far‐back‐normal‐kids‐allergies‐and‐asthma | Webpage | Not specific | ** | ** | Information on asthma, work‐related asthma and occupational asthma, triggers, rights and advice for workers and employers. |
| 250 K – A youth allergy awareness project by the National Allergy Strategy https://ya.250k.org.au/food‐allergies‐and‐the‐workplace/ (English, Australia, 2022) https://acaai.org/news/back‐school‐year‐far‐back‐normal‐kids‐allergies‐and‐asthma | Webpage | AYA | * | *** | Advice for AYA with food allergy through their first job experiences |
| Food Allergy Canada https://foodallergycanada.ca/living‐with‐allergies/ongoing‐allergy‐management/adults‐with‐allergies/workplace/ (English, Canada, 2022) | Webpage | AYA | * | ** | Advice for young adults with food allergy at the workplace. |
| E. Resources for Psychological support | |||||
| Generic resources for psychological support | |||||
| ‘Young minds’ Charity https://www.youngminds.org.uk/ (English, UK, 2022) | AYA, parents, friends, schools, youth workers | * | *** | Generic information and practical advice on mental health issues (depression, anxiety, anger, suicidal ideation) including how to start a conversation and support to AYA. Sections for AYA, parents, friends, HCP and schools. Links to parents' helpline, links and support for AYA needing urgent help, and information on how public mental health services work in the UK. Training, consultancy and posters for schools to improve pupils' wellbeing. | |
| ‘Mind’ Charity https://www.mind.org.uk/information‐support/for‐children‐and‐young‐people/ (English, UK, 2022) | AYA, parents, friends/partners | * | ** | Generic information and practical advice on mental health. Sections for AYA, parents and friends/partner. Links to useful contacts, including charities on anxiety or eating disorders, and partner initiatives such as ‘Mental Health at Work’ to support employers and organizations foster wellbeing amongst employees, and ‘SidebySide’ an online mental health peer support initiative. | |
| ‘SilverCloud’ https://www.silvercloudhealth.com/uk/digital‐mental‐health‐support‐to‐young‐people (English, UK, 2022) | Online CBT‐based self‐help mental health support programme | AYA, parents/carers | *** CBT as a therapy has a good evidence base) | ** | Digital mental health self‐help support programme offered to healthcare providers and higher education institutions which may choose to fund this for their patients/students. Aims to help AYA better understand and manage their emotions and feelings. The modules are based on CBT principles. Evidence on cost‐effectiveness. Programmes available in a range of areas including ‘Children and Adolescents’ (focused on anxiety), Higher Education (depression, anxiety, stress, resilience and body image), and non‐AYA‐specific areas such as Wellbeing, Mental Health and Chronic health. |
| ‘Online‐therapy.com’ www.Online‐therapy.com (English, worldwide, 2022) | An online‐based team of consultant therapists, cognitive‐behavioural therapists, practitioners and support staff | AYA, parents | *** CBT as a therapy has a good evidence base | ** | Company offering a mental health support programme based on CBT. Includes an online toolbox and regular communication with a therapist for a monthly subscription fee. Yoga and meditation videos available for fee on the website. World‐wide reach. |
| ‘Beating the Blues’ www.Beatingtheblues.co.uk (English, UK, 2022) | Online CBT‐based programme | Parents | *** CBT as a therapy has a good evidence base | ** |
Online Cognitive‐Behavioural Therapy (CBT) programme for people experiencing mild to moderate depression and/or anxiety. The 8–12 weeks programme consists of eight, one‐hour sessions completed weekly. Single fee for the entire programme. Small fee for UK Primary Care services to offer the programme to patients for free. Evidence on cost‐effectiveness. Recommended by the UK National Institute for Care Excellence. Worldwide reach. |
| ‘Moodgym’ www.Moodgym.au (English, Australia, 2022) | Online CBT‐based independent resource | AYA, Parents | *** CBT as a therapy has a good evidence base | ** | Online interactive self‐help programme aiming to help people learn and practise skills to prevent and manage depression and anxiety, for instance by helping identify problem emotions and developing good coping skills. Includes 5 interactive modules (feelings, thoughts, unwarping, destressing and relationships) with information, exercises, a workbook and feedback. Developed and delivered by the Australian National University. Evidence‐based. Worldwide reach. Fee for 1 year access. |
| Living Life to the Full (young people section) www.Llttfyp.com (English, UK, 2022) | Online self‐help life skills training package based on a CBT approach | AYA, Parents | *** CBT as a therapy has a good evidence base | ** | ‘Online life skills for everyone’. Specific section for AYA (young people, parents, teachers and other staff). Includes online books, worksheets, and a complete online course addressing stress and low mood. Evidence‐based. Website addressed to adults of all ages (https://llttf.com/) offers a wider range of resources, including online courses covering low mood, stress and resilience. The online courses ‘are free for individuals using them in their own lives’. |
| Allergy and asthma‐specific resources for psychological support | |||||
| ‘Asthma + Lung UK’ charity https://www.asthma.org.uk/advice/triggers/ (2020) https://www.asthma.org.uk/advice/manage‐your‐asthma/emotional‐support/anxiety/ (2019) (English, UK, 2022) | Webpage | AYA, parents | * | ** | Information and advice on emotions, depression, anxiety and stress for people (including young adults) with asthma. |
| Healthtalk.org https://healthtalk.org/eczema/emotions‐and‐having‐eczema‐2017 https://healthtalk.org/eczema/emotions‐and‐support‐for‐eczema‐at‐schooluniversity (English, UK, 2021) | Webpage | AYA | * | ** | Run by the Dipex Charity, healthtalk.org focuses on what it's like to live with a health condition by watching other people share their stories. Stories are collected by academic researchers from patient interviews. Includes information and advice on how to cope with negative emotions related to having atopic eczema during teen years, with AYA patients' video testimonials and quotes. Specific section on support for school and university. |
| National Eczema Association https://nationaleczema.org/eczema‐teen‐advice/ (English, USA, 2021) | Webpage article | AYA | * | * | Information and advice on how to cope with atopic eczema during teen years, mainly through AYA patients' testimonials (quotes) |
| Food Allergy Research and Education (FARE) https://www.foodallergy.org/resources/food‐allergy‐anxiety https://www.foodallergy.org/resources/bullying (English, US, 2022) | Webpage article | AYA | * | ** | Patient stories about their anxiety and bullying issues living with food allergy, and what helps them cope better. Includes links to a ‘Teen food allergy support group’. |
| Patient voices – ‘Terrific teens’ https://www.patientvoices.org.uk/terrificteens.htm (English, UK, 2017) | Webpage | AYA, parents | * | ** | Reflective digital stories created to explore the experiences of teenagers and their families living with a range of complex and life‐threatening allergies. |
| F. School advice | |||||
| Anaphylaxis Campaign, ‘Making Schools Safer’ Project. https://www.anaphylaxis.org.uk/campaigning/making‐schools‐safer‐project/ (English, UK, 2022) | Webpage | AYA, parents | *** | *** | Focus on food allergy and anaphylaxis. Comprehensive list of resources for schools, including primary and secondary schools allergy awareness packs, pupils healthcare plans, management of allergic reactions (with link to useful and attractive website www.sparepensinschools.uk), staff allergy and anaphylaxis first aid training, national (children) action plans, allergy bullying and FAQ. |
| Asthma Initiative of Michigan (AIM) https://getasthmahelp.org/schools‐main.aspx (English, USA, 2022) | Webpage | Parent, AYA, school staff | ** | *** | Focus on asthma and the role of schools in helping children and AYA with asthma (‘asthma friendly schools). Range of resources including information on emergency asthma management and proper inhaler use, school‐based asthma management programmes and healthy school environments. |
| AllergyHome https://www.allergyhome.org/resources/resources‐nurses‐educators‐schools‐camps/ (English/Spanish, USA, 2022) | Webpage | Caregivers, other parents | * | *** | Resources to improve awareness on food allergy amongst nurses, school/camps staff and other parents. Includes a 30 min training module and quiz for school staff, short videos for parents and children without food allergies, general information on food allergy and printable posters/tables. Some resources available in Spanish. |
| Food Allergy & Anaphylaxis Connection Team (FAACT) https://FoodAllergyAwareness.org (English, USA, 2022) | Webpage | AYA, parents, caregivers, school community | * | *** | Resources for education and support on food allergy for school staff, peer students and other parents. Includes School Programs for School Personnel, Food Allergy School Letter to Parents and School Lunchroom Poster. |
| Allergy & Asthma Network https://allergyasthmanetwork.org/allergies‐and‐asthma‐at‐school/https://allergyasthmanetwork.org/ (English/Spanish, USA, 2022) | Webpage | Parents, caregivers | * | ** | Focus on asthma and food allergy, not AYA‐specific. Information, advice and free‐download printable documents including a checklist to go back to school, individual healthcare plan, emergency plan and posters on asthma and allergic reactions symptoms, and when to stay at home due to asthma. Some resources available in Spanish. |
| G. Resources in other Languages | |||||
| EAACI resources for patients: https://patients.eaaci.org/eaaci‐member‐patient‐organizations/ (English/other languages, European‐international, 2022) | Portal | AYA, parents, caregivers, schools, other stakeholders | ** | *** | Useful links for country specific websites under” Patients Organization”. Every patient organization has its own resources in local language and some of them also translated to English. Includes patients testimonials. |
| European Federation of Allergy and Airways Diseases Patients' Associations (EFA): http://www.efanet.org/ (English/other languages, European‐international, 2022) | Portal | AYA, parents, caregivers, schools, other stakeholders | ** | ** | ‘Prevent’ section includes information on food labelling tobacco smoking, air quality, chemicals and inequalities. Translated into 46 languages, including all European Languages. |
Abbreviations: AYA, Adolescents and young adults; CBT, cognitive‐behavioural therapy; HCP, Healthcare professionals.
The evidenced‐based approach was reviewed and agreed by the Task Force members and judged in a pragmatic way into three categories with increasing level of evidence‐based approach: *moderate‐ some evidence‐based approach noted, the resource was included because of well‐rounded clinical and practical (professional) experience; ** good and *** very good.
* User‐friendliness was reviewed and agreed by the Task Force members and judged in a pragmatic way into moderate; ** good; *** very good. Some of the lower‐rated or less user‐friendly resources are shown in Table S2. All the web links provided were last accessed on 18/02/2022.
3.1. Healthcare professionals
3.1.1. Transition programmes
HCP touch the lives of AYA during a period of substantial physiological, psychological and social change. Change and desire for autonomy can also mean opportunity, and HCPs can support AYA to develop the knowledge, skills and confidence to self‐manage their own health and well‐being, which will confer lifelong benefits. There is agreement on the importance of education and support of AYA and their families within a multidisciplinary approach. Getting started with AYA‐focussed care is often a challenge for HCPs, who worry about lack of experience, time, resources and competing responsibilities. 5
Resources from healthcare settings (primarily generic but some allergy specific) have been developed to assist HCPs of all disciplines in managing healthcare and transition for the AYA, from starting to further developing a transition service. In Tables 1, 2 and S1 section A, we present our review of guidelines and transition programmes. These resources explain how to facilitate the type of planning, preparation and transfer tools required to ensure optimum transition from paediatric to adult healthcare services for youth with long‐term health needs. They also focus on timing, transfer requirements, and the contributions (roles, tasks) needed by different HCP during the transition process. They include education to upskill HCP and practical sites aimed at AYA and parents with videoclips providing insight into the experience of transition, information to demystify and simplify health‐passports and booklets with useful links. However, the evidence‐base is weak on the effectiveness of these programmes in supporting positive self‐management outcomes. Formal validation is scarce, as are outcome measures specifically for transition.
3.1.2. Tools to assess transition readiness
Transition involves a process of education and empowerment for AYA to become confident to independently self‐manage their chronic condition(s), ideally in good time before they reach the legal adult age and/or their care may be transferred to adult services. For this purpose, a number of psycho‐educational programs, including disease‐specific education and self‐management techniques have been developed for a range of chronic conditions. 7 , 8
AYA differ in their degree of independence, maturity and self‐care skills. Therefore, the transition process needs to be developmentally appropriate and tailored to the individual. The key to an effective transition and successful transfer is the AYA's readiness to transition. Transition readiness refers to the “process of building the capacity of adolescents and those who are involved in his/her medical care to prepare for, enter, continue and complete transition”. 8 Readiness can be assessed by evaluating the AYA's willingness and ability (including the necessary skills) to achieve independence and autonomy in managing their condition. 9 A number of transition readiness measures are available for use in clinical practice, including ‘Ready Steady Go’, ‘OnTRAC’ or ‘TRAQ’ (Tables 1, 2 and S1 section B for selection of resources). 10 , 11 These tools are generally used repeatedly or gradually over the transition process, and they allow: (a) to track AYA's progress and help tailor the transition process to the individual's needs and goals; (b) to identify and promote opportunities for increasing self‐management; and (c) to help identify AYA at risk of poor transfer in whom further support will be required. Nonetheless, a systematic review conducted in 2014 on the methodological quality of available transition readiness and satisfaction measures highlighted that none had well‐established evidence of reliability and validity. 12 AYA's satisfaction with transition programmes has also been assessed as a surrogate of transition effectiveness.
3.1.3. Approach to assessing an adolescent patient including psychosocial assessment
The developmental changes of AYA and the challenges faced by this group require the HCP to adopt a specific approach when communicating and engaging with them. Both the short‐ and long‐term health and wellbeing needs of AYA cannot be viewed in isolation. To deliver developmentally appropriate healthcare, a person‐centred approach to AYA should include the medical, psychological, cultural and social aspects. This includes topics such as sexual health, education or vocational planning, psychological issues and lifestyle (including leisure activities, alcohol and drug use). Consideration should also be given to the different challenges that early and late adolescence may bring (such as moving away from the parent's home), as well as to the development of a stronger sense of self and the need for more independence from parents or caregivers.
AYA with long‐term health needs are at increased risk for mental health issues and have unique psychosocial requirements. 13 , 14 , 15 The HCP is well‐placed to assess and highlight any ongoing concerns and ensure that AYA is provided with the necessary support to prevent the morbidity and mortality associated with mental health problems and risky behaviour. In clinic, the regular use of screening tools for psychosocial assessments, such as HEEADSSS 16 and Youthchat 17 can facilitate this holistic assessment over the transition period.
HCPs should also consider a more condition‐specific approach when interacting with AYA with allergy and asthma to ensure that essential topics are covered, such as asking about ingredients, avoiding food cross‐contamination in shared accommodation, the impact of smoking or environmental allergens in new housing on asthma control. Concise and developmentally appropriate information should be given throughout the transition process to ensure AYA feel equipped to deal with these changes. See Tables 1, 2 and S1, section C for selected resources in this area.
3.1.4. Transition report for individual patient/transfer package
During the transition process, if it is required to transfer AYA's care to adult services, HCP should ensure that they have completed a transfer package (Box 1 and Tables 1, 2 and S1, section D). This will facilitate information sharing and strengthen continuity of care across services.
BOX 1 Transition package overview.
Transfer package should include:
Transfer of care letter / cover letter
Transition report including medical summary (consider adding any relevant previous medical correspondence)
Action plans (food allergy/ asthma/ atopic eczema/allergic rhinitis)
Transition readiness assessment (could include transition plan)
Other items such as fact sheets, patient passport
All HCPs involved in adolescent's care should have a copy of the package.
Framework for transition report:
Demographics
HCPs details: For example, named consultant, named key worker
- Condition‐specific information
- Asthma: control, triggers, treatment, HDU/PICU admission
- Allergic rhinitis/rhinoconjunctivitis: control, triggers, treatment +/− immunotherapy
- Atopic eczema: control, treatment, history of infection, +/− history of immunosuppressants/biologics
- Food Allergy: implicated foods, history of anaphylaxis, treatment
- Other co‐morbidities
Most recent investigations: spirometry, FeNO, blood test, skin prick tests
Self‐management skills: For example, ability to request medication, make appointments, follow treatment plans
Psychosocial information: family, school/work, hobbies, future plans, other
Plan / Goals: details of next appointment/ joint appointment
Report may be a printed form of a fillable PDF form.
The transfer package includes a transition report, relevant action/emergency plans, a transition readiness assessment and other documents such as information sheets about key areas for the AYA. A transfer of care letter to the adult clinician detailing the contents of the transfer package, confirming transfer of care and upcoming appointments can be useful. When preparing the package, HCPs should consider incorporating particular concerns and priorities from AYA's and parents' perspectives.
The transition report is a comprehensive document that outlines the AYA medical history and ensures a holistic approach to the transfer of care. The medical history may include disease course, previous and current treatment, an up‐to‐date management plan as well as any co‐morbidities. Information about adherence, self‐management, school/work, hobbies and AYA's future plans/goals should also be included. The format and content should be acceptable to both the paediatric and adult teams. Providing an updated action/emergency plan will help keep the AYA safe during the transfer of care. Including the most recent transition readiness assessment will allow the adult team to identify the areas where AYA need more support. The transfer package should be distributed to all HCP involved in the patient's care, including the adult team and primary care. It should be written in a manner that AYA and families can understand.
3.1.5. Audit and key performance indicators
Regular audit of a transition service to assess key performance indicators is recommended to facilitate improvements in service provision. 4 The EAACI guideline on AYA transition provided a list of potential audit criteria (Table S3 in the online supplement). Structure, process and outcome can be audited. This ensures the best quality care is followed and clinical practice is evidence‐based. A quality improvement approach of ‘plan, do, study, act’ could be followed. 18 , 19 The audit cycle allows to compare against agreed standards and implement change where necessary to achieve improvements. Regular audit with reflection and review within the multidisciplinary team is advised for continuous improvement. Staff should have protected time for this.
Each country may have a different approach and understanding of audit. Also, different units can devise their own key performance indicators and service specifications. Benchmarking services across a region or country may help drive improvements within a wider approach. 20 , 21
3.1.6. Resources to help HCP address the psychological impact of asthma and allergy in AYA
Identifying and addressing common psychological issues AYA encounter when living with asthma and allergies, such as anxiety, depression or low self‐esteem, is key to preventing morbidity and mortality. A number of resources have been identified to assist in this area (Tables 1, 2 and S1, section F).
Cognitive‐Behavioural Therapy (CBT) is one of the most commonly used psychotherapeutic approaches for treating mental health problems. The core concept is the idea that thoughts, emotions and actions are connected, that is, the way that an individual thinks and feels about something will affect what they do. Another key principle of CBT is that these thoughts and behaviour patterns can be changed. Psychological issues are partly based on unhelpful ways of thinking and learned behaviour patterns. Therefore, improvement occurs with better coping mechanisms and management. A range of online training courses is available on CBT for HCP. The accreditation and level of training provided should be considered carefully.
Motivational Interviewing (MI) is a person‐centred strategy. It is used to elicit patient motivation to change a specific negative behaviour. Much of the online material for MI relates to training in a particular technique. Some organizations offer online MI training, some for free (See Tables 1, 2 and S1, section F).
3.2. Patients and families
3.2.1. General transition information and advice
Throughout the transition process, AYA need to acquire the knowledge and skills to confidently self‐manage their allergies and/or asthma. At the same time, their care may be transferred from a paediatric to an adult service. Parents and caregivers, assisted by HCP, need information and confidence to support their young person through this process and to hand over responsibility for self‐care to the AYA. This requires access to lay information to prepare for the process. Some useful resources are summarized in Tables 1 and 2, section A. They include information on the principles, aims, stakeholders, timelines of transition, as well as key areas for self‐management, common challenges and questions. The information provided will need to be aligned with the resources and services provided locally. Access to transition readiness assessment tools to monitor progress can be very helpful.
3.2.2. Specific advice for AYA and families
Self‐managing asthma and allergies effectively requires AYA to understand their condition, identify and avoid potential triggers and risky situations, manage symptoms—particularly acute emergencies such as asthma attacks or anaphylaxis—and cope with the psychosocial impact of living with these issues in their changing reality. AYA and their support network may feel overwhelmed by the many aspects where AYA need to develop their knowledge and skills to effectively self‐manage their conditions and keep safe. In Table 2, sections B–E, we have selected a range of web‐based resources offering comprehensive information, advice and useful documents on a range of areas relevant to AYA with asthma and allergies, including:
Written action plans are patient‐ or carer‐held instructions that help support self‐management. They have the potential to address barriers to effective treatment, such as a lack of understanding about the condition and medications prescribed. They are recommended by national and international guidelines, 22 and their use can improve management 23 and asthma outcomes. 24 , 25
We advocate the use of a patient‐held, written self‐management plan which provides clear individualized treatment guidance. Many action plans available are designed for parents/carers of young children. However, medical communication should gradually be addressed to the AYA themselves in a clear age‐appropriate language and format. 26 We have not been able to identify adolescent‐focused self‐management plans for different atopic conditions, including much‐needed electronic versions of these, which remains a major gap. Links to action plans for asthma, anaphylaxis and atopic eczema designed to suit all ages, rather than children‐focused, are included in Tables 1 and 2, section B.
Food avoidance and safe food choices (Tables 1 and 2, section B).
For patients with food allergy, avoiding the culprit food(s) is the cornerstone of management to prevent potentially life‐threatening accidental reactions. Avoidance and making safe food choices involve planning/knowing the full list of ingredients in every single food consumed and ensuring/checking the careful storing, handling, and serving of the food to avoid cross‐contamination. This is often challenging for AYA, their families, and their broader network, particularly as many common allergens (cow's milk, egg, nuts) are widely present in our diets. Also, despite the FIC European Regulation 1169/2011 (and now the UK) on Food Information to Consumers and its implementation through national guidelines, information on allergens in both prepacked and non‐prepacked foods is not always easy to find or understand, thus complicating decision‐making for allergic consumers to stay safe. 27 The overuse of precautionary allergen labelling, as well as incorrect or inaccurate labelling, contribute to this problem. AYA will also need to develop cooking skills as they head towards living independently.
Leisure, sports and further education (see Tables 1 and 2, section B)
AYA tend to spend more time away from home and their parents, as the weight of their relationships moves towards friends and peers. As such, parents need to ‘let go’, and AYA need to take increasing responsibility for managing their allergies and asthma. This can be very challenging as many of the lifestyle changes AYA go through involve new situations that may pose risks. For instance, moving from high school to college/university/workplace, sharing accommodation, new friendships, dating, partying, new sports, school trips or international travel. AYA need to learn how to navigate these new situations independently whilst keeping safe. This can be overwhelming for AYA and their parents, who often worry about the risk of life‐threatening allergic reactions or poor disease control as they ‘let go’.
For AYA, sharing or disclosing information about their allergies and asthma with new friends, peers, work colleagues or a partner can be challenging due to feelings of embarrassment, shame or denial. Hence, it is vital to provide AYA and their network with practical resources to promote a supportive environment and help AYA develop the skills and confidence required to share their needs, reduce risks and manage their conditions effectively in the range of new scenarios they will encounter.
Travelling and patient passport (see Tables 1 and 2, section C)
AYA with asthma and allergies and their parents/caregivers often feel anxious when travelling, particularly internationally, probably due to uncertainty around exposures, risks and access to foods, medications or emergency care if required in new environments. Before booking a holiday or making travel arrangements, AYA with food allergies in particular, should spend time planning and gathering information to ensure a safe and enjoyable trip.
HCP should provide AYA with asthma and allergies with resources to assist when travelling, including:
‐ Allergy passport, which is a one‐page letter/card summarizing information on their allergic conditions, allergens involved, severity/nature of diseases and medications to carry. An example of an allergy passport with a checklist suggestion is provided in Figure 2.
FIGURE 2.
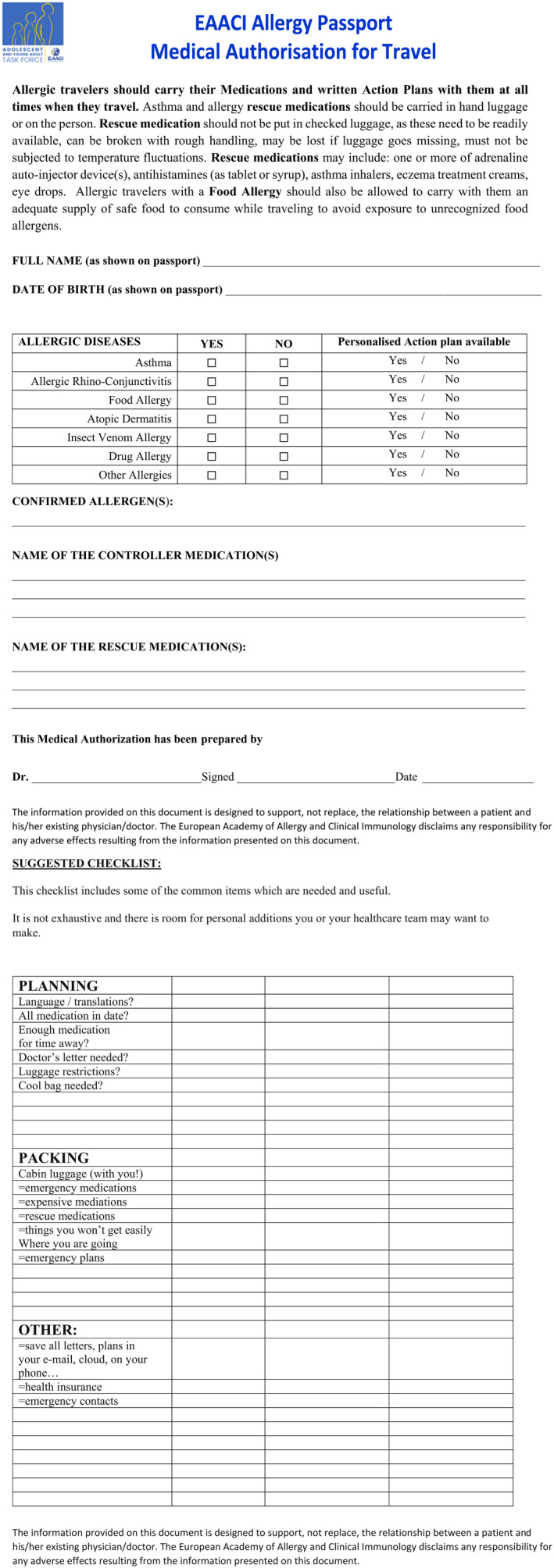
EAACI Allergy Passport ‐ Medical Authorization for Travel
‐ Personal management plans including an Emergency Action Plan for anaphylaxis, asthma exacerbations or severe atopic eczema flares, as required.
‐ Supporting ‘authorization for travel’ forms to carry specific medications or food items within the hand luggage, if required. AYA with asthma and/or at risk of anaphylaxis, asthma inhalers and/or two adrenaline autoinjectors should be always available and not put into the checked luggage.
Whilst traditionally documentation was carried in paper form, documents should also be available electronically on the patients' mobile devices or in their web‐based ‘cloud’ in the required language(s).
Future career choices and work advice (see Tables 1 and 2, section D)
AYA with asthma and allergies should aim at optimal control of their health issues to help them reach their full potential. However, some work‐related exposures may involve a risk. Available studies show that only a few young people with symptoms of asthma, allergic rhinitis or atopic dermatitis received appropriate career guidance by their physicians and took their atopic disease into account when choosing their occupation. 28 There is also evidence that appropriate risk‐related career advice leads to higher use of preventive measures at work in AYA with atopic dermatitis. 28 Therefore, individualized career counselling by HCP on job‐related risks and preventive measures would be an important step in preventing both symptoms/reactions in AYA wishing to begin an occupation and early cessation of the job. For instance, AYA who are allergic to a substance found at the workplace that cannot reliably be avoided, and who develop specific allergic symptoms on contact with that substance, should be advised about and understand the risks involved.
Psychological issues
Identifying and addressing psychological issues has been identified as an important aspect in transition care by AYA and their parents. 6 Access to local mental health resources may vary across countries/regions. A number of websites offer resources for youth going through mental health issues, as well as for their parents, partners and teachers to help support them. These include information and advice on common problems, self‐help initiatives, online CBT for patients and signposting for further support. See Tables 1 and 2 section F.
3.3. Schools, workplace and wider community
3.3.1. Schools and workplace
Education around asthma and allergies is primarily focussed on the home setting. However, children and AYA spend at least a fifth of their waking hours in school, 29 and, later on, in the workplace. The impact of asthma and allergic diseases, including atopic dermatitis, in school–work–life is well recognized. 30 Asthma is the leading chronic condition contributing to school absenteeism. 31 Allergic diseases may lead to AYA feeling different to their peers and stigma and bullying are commonly reported. 32 , 33 , 34 Importantly, emergency situations such as asthma attacks or anaphylaxis often occur in schools. Indeed, anaphylaxis due to food allergy (FA) occurs in schools more than in any other community location. 30 , 35 In this context, awareness and education on asthma and allergies are required to create a supportive environment at schools and the workplace where AYA feel safe and included. A selection of resources in this area is provided in Tables 1 and 2, section F.
Against a backdrop of schools being under increasing pressure to maximize performance with less resources, it is unsurprising that many schools are slow to embrace effective risk minimization management policies for allergy 36 and asthma, since this is not directly relevant to academic attainment targets. Teachers are often unaware of school management plans, with many not competent to manage asthma attacks or severe allergic reactions. 37 So, AYA often need to self‐manage their allergies or asthma at school, to communicate their needs, to prevent or minimize the impact of accidental adverse events, to raise awareness and to cope with any stigma. 38 , 39 , 40 Although there is a paucity of research carried out in work settings, it is likely that similar challenges exist. Standard allergy policies, such as those supplied by Local Authorities, may lack school‐specific practical solutions targeted at the real‐world challenges faced by AYA. 38 An important part of supporting AYA at school and work is to develop age‐appropriate and context‐specific online resources. These resources, if evidence‐based, may promote skills for self‐awareness, self‐management, social awareness, relationships and social decision‐making.
Although online resources targeted to AYA are important, a more effective strategy may be to raise awareness across the whole school community. 38 A whole‐school approach recognizes that all aspects of the school community can impact student health and wellbeing 35 , 36 , 38 in addition to helping reduce the social stigma and bullying associated with allergies or asthma through correcting current misconceptions, improving knowledge, empathy and overall management awareness. Whole‐school risk assessment and appropriate daily risk management may prevent incidents occurring, as well as raise awareness, which may in turn positively impact the quality of life of pupils with food and other allergies and asthma. 38 , 41 , 42 Such an approach could also be applied to the work setting with similar benefits.
3.3.2. Friends, peers, wider society including youth groups and sport/leisure
Civil society has legal and moral obligations towards the individuals who make it up. One of these is to help people feel part of the community in carrying out daily life activities. Equality, inclusiveness, solidarity, dignity, empathy and respect between individuals are human rights based on fundamental values.
AYA strongly feel the influence of friends and peers. This can lead AYA not to reveal their condition(s) out of shame or fear of feeling different, being bullied or being made fun of. This hinders building the support network they need and may put them at risk. Friends, peers and colleagues and the broader community should take allergies and asthma in AYA seriously, understand and respect their needs and adhere to their care plans to help them keep safe. For instance, involving AYA in activities that could pose a risk should be avoided, even if these may seem trivial such as smoking, drinking, tasting food or exchanging tools or equipment.
A range of useful resources has been identified for the broader community in their supporting role to AYA (see Tables 1 and 2, sections B‐F). Portals gathering resources in languages other than English are summarized in Tables 1 and 2, section G.
4. DISCUSSION
Adolescence is a crucial period of change and vulnerability. Transition care for AYA with asthma and allergies is perceived as important by HCP, AYA and their parents alike. 5 , 6 HCP have a pivotal role in advocating for AYA's needs and supporting them to develop the knowledge and skills required to self‐manage their conditions independently beyond adolescence. However, transitional care provision has significant limitations across Europe. The broad scope of AYA healthcare transition, along with competing priorities and limited resources, may lead to HCP feeling overwhelmed when approaching the needs of this age group. 5 , 6
Following on the publication of the EAACI Guideline on effective transition and previous work by the taskforce, this ‘toolbox’ paper provides a careful selection of practical resources to help implement the guideline and assist the multiple stakeholders involved in transition, including paediatric and adult HCP, AYA, their families, school and workplace, and the wider community.
The structured and pragmatic approach, with clear signposting to the resources available, should allow anyone and everyone involved in transition care to identify resources to help meet their needs. This includes from basic elements to get started to more specific resources to further develop services (for instance, by systematically incorporating psychosocial and readiness assessment tools) or to signpost AYA or their families to good quality advice on a particular area (such as travelling or psychological support). The wider use of telemedicine and web‐based resources due to the COVID‐19 pandemic may provide opportunities for more convenient and effective interactions with AYA, and many of the resources selected can be used in this context. 43 , 44 We believe this pragmatic selection of resources is a great opportunity for all stakeholders, particularly HCP, to engage with transition to help meet AYA's needs and improve their long‐term health. This would be equally helpful for AYA with complex multisystem allergic disease as well as AYA with less complex issues who may achieve good self‐management skills with a relatively simple transition approach supported by resources for non‐HCP presented in this work.
5. LIMITATIONS
We are aware of the wide differences regarding service provision and funding across Europe, which may impact on the implementation of the resources presented. Irrespective of the setting, our resources reflect the principles underpinning AYA healthcare transition, that is, the recognition that AYA have specific needs to achieve effective self‐care and they deserve special, developmentally appropriate attention and advice.
The taskforce undertook significant efforts to engage European clinicians and searched in multiple common languages. The materials found to be relevant and of good quality was included, which is mostly in English. This limits its direct applicability and highlights the need for high‐quality resources in other languages. Also, resources are often web links, which may cease to function. To mitigate this, we selected key resources with evidence of longevity, that is, part of large well‐funded programmes, where possible. Some resources may have been developed with the support of third parties, for example, grants of foundations or industry sponsorship.
Many resources presented have been developed by experts with a pragmatic approach, hence lacking methodological rigour, such as formal validation or evidence on effectiveness. Future research should focus on developing validated, patient‐centred tools for an effective transition process and successful transfer to adult care.
The Taskforce hopes that the structure, rationale and breadth of the Toolbox resources included stimulate curiosity, learning and further development of materials in different countries to continue to improve transition care globally.
6. CONCLUSION
Developed by a multidisciplinary Task Force from across Europe, this is the first ‘toolbox’ providing a careful selection of practical resources to help all stakeholders involved in transitional care to help implement the recent EAACI Guideline on effective transition into clinical practice. Addressed at HCP, AYA, families and the wider community, this aimed to support AYA with asthma and allergies develop the knowledge and skills required to effectively self‐manage their health independently. There is a need to monitor guideline implementation and audit practice to ensure evidence‐based standards are met.
AUTHOR CONTRIBUTIONS
GR, MV‐O and CG produced the manuscript concept and design. All authors involved in the acquisition of data including search, and analysis and interpretation of data, and critical revision of the manuscript for important intellectual content. GR and MV‐O obtained funding.
FUNDING INFORMATION
European Academy of Allergy and Clinical Immunology.
CONFLICT OF INTEREST
GR and RK report research funding from Asthma UK and National Institutes of Health Research into the challenges associated with asthma during adolescents. EA reports research funding from the Natasha Allergy research Foundation. KB reports consulting for Aimmune Therapeutics, DBV Technologies, Bencard Allergie, Novartis; and research grants from Aimmune Therapeutics, DBV Technologies, Novartis and Hipp, outside the submitted work. FT reports being a parent of a young adult with food allergy. None of the other authors have anything to disclose. RK reports research funding from Aimmune Therapeutics, Novartis, National Peanut Board, consulting for Aimmune Therapeutics, speaker fees from DBV Technologies and Nutricia.
Supporting information
Table S1 Additional transition resources for healthcare professionals (HCP)
Table S2 Glossary of terms for healthcare professionals (HCP) and patients
Table S3 Suggested audit criteria and key performance indicators
ACKNOWLEDGMENTS
We are grateful to EAACI for funding and Adolescent and Young Adult Task Force which developed this paper. We are also grateful for all the feedback and advice we have received from adolescent and young adult patients and their parents over the years.
Vazquez‐Ortiz M, Gore C, Alviani C, et al. A practical toolbox for the effective transition of adolescents and young adults with asthma and allergies: An EAACI position paper. Allergy. 2023;78:20‐46. doi: 10.1111/all.15533
Marta Vazquez‐Ortiz and Claudia Gore Equally contributed as first authors
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the corresponding author upon reasonable request.
REFERENCES
- 1. Vazquez‐Ortiz M, Angier E, Blumchen K, et al. Understanding the challenges faced by adolescents and young adults with allergic conditions: a systematic review. Allergy. 2020;75(8):1850‐1880. [DOI] [PubMed] [Google Scholar]
- 2. Royal College of Physicians . Why Asthma Still Kills: the National Review of Asthma Deaths (NRAD) Confidential Enquiry Report. RCP; 2014. www.rcplondon.ac.uk/sites/default/files/why‐asthmastill‐kills‐full‐report.pdf [Google Scholar]
- 3. Turner PJ, Gowland MH, Sharma V, et al. Increase in anaphylaxis‐related hospitalizations but no increase in fatalities: an analysis of United Kingdom national anaphylaxis data, 1992‐2012. J Allergy Clin Immunol. 2015;135(4):956‐963.e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Roberts G, Vazquez‐Ortiz M, Knibb R, et al. EAACI guidelines on the effective transition of adolescents and young adults with allergy and asthma. Allergy. 2020;75(11):2734‐2752. [DOI] [PubMed] [Google Scholar]
- 5. Khaleva E, Vazquez‐Ortiz M, Comberiati P, et al. Current transition management of adolescents and young adults with allergy and asthma: a European survey. Clin Transl Allergy. 2020;10:40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Khaleva E, Knibb R, DunnGalvin A, et al. Perceptions of adolescents and young adults with allergy and/or asthma and their parents on EAACI guideline recommendations about transitional care: a European survey. Allergy. 2022;77(4):1094‐1104. [DOI] [PubMed] [Google Scholar]
- 7. McDonagh JE. Transition of care from paediatric to adult rheumatology. Arch Dis Child. 2007;92(9):802‐807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Smith GM, Lewis VR, Whitworth E, Gold DT, Thornburg CD. Growing up with sickle cell disease: a pilot study of a transition program for adolescents with sickle cell disease. J Pediatr Hematol Oncol. 2011;33(5):379‐382. [DOI] [PubMed] [Google Scholar]
- 9. van Staa A, van der Stege HA, Jedeloo S, Moll HA, Hilberink SR. Readiness to transfer to adult care of adolescents with chronic conditions: exploration of associated factors. J Adolesc Health. 2011;48(3):295‐302. [DOI] [PubMed] [Google Scholar]
- 10. Nagra A, McGinnity PM, Davis N, Salmon AP. Implementing transition: ready steady go. Arch Dis Child Educ Pract ed. 2015;100(6):313‐320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Wood DL, Sawicki GS, Miller MD, et al. The transition readiness assessment questionnaire (TRAQ): its factor structure, reliability, and validity. Acad Pediatr. 2014;14(4):415‐422. [DOI] [PubMed] [Google Scholar]
- 12. Stinson J, Kohut SA, Spiegel L, et al. A systematic review of transition readiness and transfer satisfaction measures for adolescents with chronic illness. Int J Adolesc Med Health. 2014;26(2):159‐174. [DOI] [PubMed] [Google Scholar]
- 13. Berkelbach van der Sprenkel EE, Nijhof SL, Dalmeijer GW, et al. Psychosocial functioning in adolescents growing up with chronic disease: the Dutch HBSC study. Eur J Pediatr. 2022;181(2):763‐773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Barlow JH, Ellard DR. The psychosocial well‐being of children with chronic disease, their parents and siblings: an overview of the research evidence base. Child Care Health Dev. 2006;32(1):19‐31. [DOI] [PubMed] [Google Scholar]
- 15. Maurice‐Stam H, Nijhof SL, Monninkhof AS, Heymans HSA, Grootenhuis MA. Review about the impact of growing up with a chronic disease showed delays achieving psychosocial milestones. Acta Paediatr. 2019;108(12):2157‐2169. [DOI] [PubMed] [Google Scholar]
- 16. Doukrou M, Segal TY. Fifteen‐minute consultation: communicating with young people‐how to use HEEADSSS, a psychosocial interview for adolescents. Arch Dis Child Educ Pract ed. 2018;103(1):15‐19. [DOI] [PubMed] [Google Scholar]
- 17. Thabrew H, D'Silva S, Darragh M, Goldfinch M, Meads J, Goodyear‐Smith F. Comparison of YouthCHAT, an electronic composite psychosocial screener, with a clinician interview assessment for Young people: randomized controlled trial. J Med Internet Res. 2019;21(12):e13911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Taylor MJ, McNicholas C, Nicolay C, Darzi A, Bell D, Reed JE. Systematic review of the application of the plan‐do‐study‐act method to improve quality in healthcare. BMJ Qual Saf. 2014;23(4):290‐298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Knudsen SV, Laursen HVB, Johnsen SP, Bartels PD, Ehlers LH, Mainz J. Can quality improvement improve the quality of care? A systematic review of reported effects and methodological rigor in plan‐do‐study‐act projects. BMC Health Serv Res. 2019;19(1):683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Ettorchi‐Tardy A, Levif M, Michel P. Benchmarking: a method for continuous quality improvement in health. Healthc Policy. 2012;7(4):e101‐e119. [PMC free article] [PubMed] [Google Scholar]
- 21. Royal College of Nursing . Understanding benchmarking: RCN guidance for nursing staff working with children and young people. https://www.rcn.org.uk/professional‐development/publications/pub‐006333. Published 2017. Accessed 02 April 2022.
- 22.Rhinitis Management Plan (leaflet made by Guy's and St Thomas' NHS Foundation Trust). https://www.evelinalondon.nhs.uk/resources/patient‐information/your‐rhinitis‐management‐plan‐web.pdf. Published 2019. Accessed 02 April 2022.
- 23.Eczema Action Plan (made by University of Bristol). http://www.bristol.ac.uk/primaryhealthcare/researchthemes/apache/ewap/#:~:text=About%20the%20EWAP,the%20GP%20surgery%20for%20help. Accessed 02 April 2022.
- 24.Treatment Plan for Allergic Rhinitis (Hay Fever) (made by ASCIA Australasian Society of Clinical Immunology and Allergy) https://www.allergy.org.au/images/pcc/ASCIA_Allergic_Rhinitis_Treatment_Plan_2020.pdf. Accessed 02 April 2022.
- 25.Asthma Action Plan Adult (leaflet made by Asthma UK). https://www.asthma.org.uk/globalassets/health‐advice/resources/adults/adult‐asthma‐action‐plan.pdf. Accessed 02 April 2022.
- 26. Parekh‐Hill NA, Wood D, Davis M, Farooq A, Segal TY. Please write to me, not about me: best practice in written communication with young people. Arch Dis Child. 2022;archdischild‐2021‐323393. doi: 10.1136/archdischild-2021-323393 [DOI] [PubMed] [Google Scholar]
- 27. Fiocchi A, Risso D, DunnGalvin A, et al. Food labeling issues for severe food allergic patients. World Allergy Organ J. 2021;14(10):100598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Radon K, Nowak D, Vogelberg C, Rueff F. Career advice for Young allergy patients. Dtsch Arztebl Int. 2016;113(31–32):519‐524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Greenhawt M. Environmental exposure to peanut and the risk of an allergic reaction. Ann Allergy Asthma Immunol. 2018;120(5):476‐481 e473. [DOI] [PubMed] [Google Scholar]
- 30. Zuberbier T, Orlow SJ, Paller AS, et al. Patient perspectives on the management of atopic dermatitis. J Allergy Clin Immunol. 2006;118(1):226‐232. [DOI] [PubMed] [Google Scholar]
- 31. Hsu J, Qin X, Beavers SF, Mirabelli MC. Asthma‐Related School Absenteeism, Morbidity, and Modifiable Factors Am J Prev Med; 51(1): 23–32. [DOI] [PMC free article] [PubMed]
- 32. Cooke F, Ramos A, Herbert L. Food allergy‐related bullying among children and adolescents. J Pediatr Psychol. 2022;47(3):318‐326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Joseph SP, Borrell LN, Lovinsky‐Desir S, Moroko AR, Li S. Bullying and lifetime asthma among children and adolescents in the United States. Ann Epidemiol. 2022;69:41‐47. [DOI] [PubMed] [Google Scholar]
- 34. Charles R, Brand PLP, Gilchrist FJ, Wildhaber J, Carroll W. Why are children with asthma bullied? A risk factor analysis. Arch Dis Child. 2021;archdischild‐2021‐321641;107:612‐615. [DOI] [PubMed] [Google Scholar]
- 35. Muraro A, Agache I, Clark A, et al. EAACI food allergy and anaphylaxis guidelines: managing patients with food allergy in the community. Allergy. 2014;69(8):1046‐1057. [DOI] [PubMed] [Google Scholar]
- 36. Mustafa SS, Russell AF, Kagan O, et al. Parent perspectives on school food allergy policy. BMC Pediatr. 2018;18(1):164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Ercan H, Ozen A, Karatepe H, Berber M, Cengizlier R. Primary school teachers' knowledge about and attitudes toward anaphylaxis. Pediatr Allergy Immunol. 2012;23(5):428‐432. [DOI] [PubMed] [Google Scholar]
- 38. Higgs J, Styles K, Bowyer S, Warner A, Dunn GA. Dissemination of EAACI food allergy guidelines using a flexible, practical, whole school allergy awareness toolkit. Allergy. 2021;76(11):3479‐3488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. DunnGalvin A, Polloni L, Le Bovidge J, et al. Preliminary development of the food allergy coping and emotions questionnaires for children, adolescents, and Young people: qualitative analysis of data on IgE‐mediated food allergy from five countries. J Allergy Clin Immunol Pract. 2018;6(2):506‐513 e511. [DOI] [PubMed] [Google Scholar]
- 40. Sicherer SH, Allen K, Lack G, Taylor SL, Donovan SM, Oria M. Critical issues in food allergy: A National Academies Consensus Report. Pediatrics. 2017;140(2):e20170194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Young MC, Munoz‐Furlong A, Sicherer SH. Management of food allergies in schools: a perspective for allergists. J Allergy Clin Immunol. 2009;124(2):175‐182. e171‐174; quiz 183‐174. [DOI] [PubMed] [Google Scholar]
- 42. Polloni L, Baldi I, Lazzarotto F, et al. Multidisciplinary education improves school personnel's self‐efficacy in managing food allergy and anaphylaxis. Pediatr Allergy Immunol. 2020;31(4):380‐387. [DOI] [PubMed] [Google Scholar]
- 43. Pfaar O, Klimek L, Jutel M, et al. COVID‐19 pandemic: practical considerations on the organization of an allergy clinic‐an EAACI/ARIA position paper. Allergy. 2021;76(3):648‐676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Alvaro‐Lozano M, Sandoval‐Ruballos M, Giovannini M, et al. Allergic patients during the COVID‐19 pandemic‐clinical practical considerations: an European academy of allergy and clinical immunology survey. Clin Transl Allergy. 2022;12(1):e12097. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1 Additional transition resources for healthcare professionals (HCP)
Table S2 Glossary of terms for healthcare professionals (HCP) and patients
Table S3 Suggested audit criteria and key performance indicators
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.


