Abstract
Aim
This study aims to synthesize evidence on nurses' involvement in artificial intelligence research for managing falls in older adults.
Background
Artificial intelligence techniques are used to analyse health datasets to aid clinical decision making, patient care and service delivery but nurses' involvement in this area of research for managing falls in older adults remains unknown.
Evaluation
A scoping review was conducted. CINAHL, the Cochrane Library, Embase, MEDLI and PubMed were searched. Results were screened against inclusion criteria. Relevant data were extracted, and studies summarized using a descriptive approach.
Key Issues
The evidence shows many artificial intelligence techniques, particularly machine learning, are used to identify falls risk factors and build predictive models that could help prevent falls in older adults, with nurses leading and participating in this research.
Conclusion
Further rigorous experimental research is needed to determine the effectiveness of algorithms in predicting aspects of falls in older adults and how to implement artificial intelligence tools in gerontological nursing practice.
Implications for Nursing Management
Nurses should pursue interdisciplinary collaborations and educational opportunities in artificial intelligence, so they can actively contribute to research on falls management. Nurses should facilitate the collection of digital falls datasets to support this emerging research agenda and the care of older adults.
Keywords: artificial intelligence, falls, machine learning, natural language processing, nursing
1. INTRODUCTION
Falls are the second leading cause of unintentional injury‐related mortality worldwide, after road traffic injuries. It is estimated that there are 37.3 million severe falls annually that require medical attention, of which 684,000 are fatal (World Health Organization, 2021). Falls can occur for many reasons. Biological factors include age, gender and physical health problems such as orthostatic hypotension, decreased visual acuity, impairments in gait, balance and cognition among others (Peltzer et al., 2013). Socio‐economic risk factors associated with higher likelihood of a fall can encompass an individuals' educational level, while behavioural aspects can include actions such as consuming excessive amounts of alcohol or taking certain medications. Falls can also be attributed to environmental risk factors such as difficult stairs, poor lighting and slippery or uneven surfaces both indoors and outdoors (Jiang et al., 2019). While many falls are nonfatal, bruising and lacerations, head injuries and fractures can inhibit mobility and cause long‐term physical and mental health issues (Ganz & Latham, 2020). Around 40% to 60% of falls lead to injuries, 30% to 50% of these being minor, 5% to 6% major (excluding fractures) and 5% fractures. Up to 1% of falls in older people result in a hip fracture. Injuries are the fifth most common cause of death in older people and falls are the most common cause of injury‐related death in persons over 75 years (Kenny et al., 2012; World Health Organization, 2021). Furthermore, psychological complications, such as a fear of falling, can also compromise the independence of older adults, limit their daily activities and lead to a dependency on formal and informal care (Schoene et al., 2019).
Falls also impact the provision of health services. More than €25 billion is spent in falls related health care costs in the European Union each year, expenditure that is set to increase to approximately €45 billion by 2050 due to ageing populations across the continent (Turner et al., 2015). Furthermore, Hartholt et al. (2012) examined the spectrum of costs associated with falls in the Netherlands including family physician consultations, hospital stays and outpatient visits, long‐term care and home care costs and found the mean cost per fall was €9370. This figure was higher for women (Bowen & Mason, 2012) than men (Waters et al., 2009) and increased with age, with patients 85 years and older who had fallen costing more than those aged 65–69 years. Similarly, in the United States, fall‐related injuries result in 2.8 million emergency departments visits each year, along with 800,000 hospital stays (Bergen et al., 2016), costing up to $49.5 billion US dollars annually (Florence et al., 2018).
Managing falls can be addressed in a number of ways. Preventative strategies can involve removing hazards in home and hospital environments and providing assistive modifications (e.g., shower chairs or handrails), or reviewing footwear, medications, cognition and vision (Leung, 2021). However, early identification of at‐risk individuals can be difficult, given that many factors can contribute to a fall particularly among older age groups. While a multidisciplinary approach is often adopted, nurses undertake a lot of the day‐to‐day work in falls prevention by gathering and interpreting fall‐related paper‐based and digital data (Johnson et al., 2011). The use of technologies to detect and reduce falls like depth cameras, floor sensors and wearable devices with accelerometers is also increasing (Wang et al., 2020), while digital programmes, exergames and robots are being used to improve gait, balance, mobility and strength (Stanmore et al., 2019). Nurses are often involved in implementing these types of interventions with at‐risk older adults in both hospital and community settings.
1.1. Artificial intelligence (AI)
AI is an emerging technological trend that is being used in falls management and encompasses a range of advanced computational techniques. Although many definitions exist, a recent high‐level expert group on AI described it as ‘software (and possibly also hardware) systems designed by humans that, given a complex goal, act in the physical or digital dimension by perceiving their environment through data acquisition, interpreting the collected structured or unstructured data, reasoning on the knowledge, or processing the information, derived from this data and deciding the best action(s) to take to achieve the given goal. AI systems can either use symbolic rules or learn a numeric model, and they can also adapt their behaviour by analysing how the environment is affected by their previous actions’ (Samoili et al., 2020). Contemporary forms of AI such as machine learning (e.g., supervised, unsupervised and reinforcement learning), natural language processing, fuzzy logic and expert systems among others are being developed and tested to help predict, prevent and detect falls (Ng et al., 2021). A recent systematic review of machine learning trends for fall detection and prevention found 33 studies, most of which used datasets from wearable and sensor devices and were tested on younger participants in controlled laboratory settings to build predictive models (Usmani et al., 2021). However, this review included only machine learning, excluding other AI domains and included studies from only three bibliographic databases (Google Scholar, IEEE Xplore and Science Direct), missing key sources of biomedical, health and nursing research. Additionally, nurses as a key professional group involved in falls management were not identified in the review and few clinical implications were presented. Furthermore, a number of reviews of AI in nursing encompass all areas of practice but do not report nurses' contribution to this specific area of research and detailed descriptions of falls related studies are missing (O'Connor et al., 2022; Seibert et al., 2021; von Gerich et al., 2022). Hence, a review that focuses on nurses' involvement in research on AI for falls management in older adults is warranted, to understand what advanced computational techniques are employed to try to improve falls management in older adult care, and how the nursing profession contributes to this area of research and practice.
2. METHODS
The review aimed to identify and summarize studies on nurses' involvement in AI‐based falls research and the potential impact these advanced computational approaches may have on the care of older adults. The review was registered on the OSF Registries (https://www.cos.io/products/osf-registries) and the Preferred Reporting Items for Systematic reviews and Meta‐Analyses extension for Scoping Reviews (PRISMA‐ScR) Checklist was followed (see Appendix S1).
2.1. Search strategy and screening
Several scoping searches were undertaken to identify search terms relevant for AI, falls, older adults and nursing. Relevant MeSH terms, Emtree terms and subject headings were also added. The term ‘logistic regression’ was not included for pragmatic reasons due to the limited time and resources available to undertake the review, although some applications of this type of probability modelling are considered forms of AI (Beam & Kohane, 2018). Two separate searches were run across five bibliographic databases, that is, CINAHL (EBSCOhost), the Cochrane Library, Embase, MEDLINE (Ovid) and PubMed Central. The first, broad search was run on 10 November 2021 and encompassed terms for AI, falls management and older adults (e.g., ‘aging’, ‘older adult*’, ‘artificial intelligence’, ‘machine learning’, ‘fall*’ and ‘accidental falls’) to help identify pertinent literature that may involve nurses in its design or conduct (Appendix S2). Two thousand and twelve results were found and downloaded to Rayyan software (https://www.rayyan.ai/), with duplicates removed before screening. Studies were screened according to title, abstract and full text by two reviewers working independently. The second search was run on 5 February 2022 and focused specifically on nursing within the AI for falls management domain (Appendix S2). One hundred and thirty‐seven results were returned which were subsequently screened by title, abstract and full text via Rayyan by two reviewers working independently (Figure 1). Consensus discussion helped resolve any disagreements during screening. Inclusion and exclusion criteria were developed using the Population, Intervention, Comparator, Outcome, Setting/Study and Timeframe framework (Table 1).
FIGURE 1.
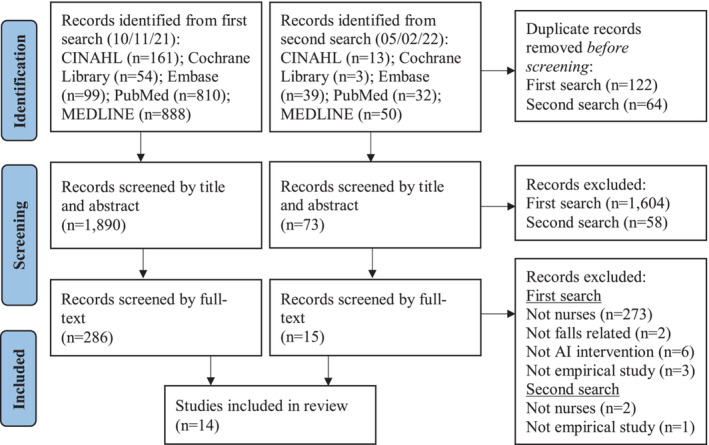
Flow diagram of the screening process
TABLE 1.
Inclusion and exclusion criteria for the review
| Inclusion criteria | Exclusion criteria |
|---|---|
| Population: Older adults (average age 60 years or more) and mixed populations if older adults comprised the majority of participants. Nurses also had to be involved in some aspect of the design or conduct of the research study, either as participants or members of the research team | Child and adults under 60 years of age |
| Intervention: Any artificial intelligence technique applied to an area of falls management | Artificial intelligence techniques or systems that were simulated, prototyped, not based on real‐world datasets, or where no specific artificial intelligence methods were described |
| Comparison: No comparator was used | |
| Outcomes: All outcomes | None |
| Settings: All settings (acute, primary or community care, long‐term/residential care) | None |
| Study design: All types of studies designs (quantitative, qualitative, mixed methods) | None |
| Timeframe: None, given the recent emergence of artificial intelligence in health care | |
| Publication type: Peer‐reviewed articles in English language journals | Conference proceedings, dissertations and theses, discussion and editorial articles, grey literature and literature reviews |
2.2. Data extraction and analysis
Microsoft Excel was used to create a data extraction template that was adapted from the Cochrane Effective Practice and Organisation of Care Review Group data collection checklist. The data extracted from each study included the first author, year, country, research aims/objectives, study design, setting, data collection, participants, AI intervention and results/outcomes (Table 2). The included studies were summarized using a descriptive approach.
TABLE 2.
Study characteristics
| Author, year, country, lead | Research aim(s) | Study design, setting, data collection | Participants | AI techniques | Results/outcomes |
|---|---|---|---|---|---|
| Ağartioğlu Kundakçi et al. (2020), Turkey, Lead author: nursing faculty | To examine the costs of falls in older people living in the community and the costs of fall prevention interventions implemented by nurses, using a decision tree model. To also determine the factors affecting the cost of falls. |
Study design: costing and cost‐effectiveness study Setting: hospital, emergency department Data collection: primary and secondary—data collection form on sociodemographic characteristics, 10‐item questions on falls and three‐item questions on costs of falls. Patient files were reviewed retrospectively via the Hospital Information Management System. |
Numbers: 2075 Type: patients admitted to a hospital due to falls in the community Gender: 65.16% were females Age: mean age 76.77 ± 7.83 Ethnicity: not reported |
Decision tree model used for economic evaluation (1‐year Markov model cycle was applied). Sensitivity analysis was based on cost parameters and the costs were increased or reduced by 25% | The average cost for a person admitted to a hospital due to falls was $396.51 ± $1429.35. It was determined that costs varied according to the type of the injury. The total cost increased as the age increased (r = .23, P < .001). Three scenarios tested were costly but also more effective. |
| Beauchet et al. (2018), France, Lead author: medical faculty | To examine performance criteria for fall prediction using artificial neural networks (ANNs) analysis in older inpatients hospitalized in acute care medical wards. |
Study design: quantitative—observational prospective cohort design Setting: hospital—10 acute care medical wards Data collection: primary—bedside clinical assessment within 24 h of admission including mobility and cognitive impairment to gather baseline data. |
Numbers: 848 (training n = 678 and testing n = 170) Type: older inpatients Gender: 41.8% female Age: 83.0 ± 7.2 years Ethnicity: not reported |
Three feed forward ANNs, that is, multilayer perceptron, averaged neural network and neuroevolution of augmenting topologies | ANNs showed a high specificity (regardless of which was used) with the highest value reported was multilayer perceptron (99.8%). Sensitivity was lower, with values ranging between 98.4% and 14.8%. This combined artificial intelligence (AI) approach should be used more as a diagnostic test than a screening test when considering older inpatients in acute care. |
| Cho et al. (2019), South Korea, Lead author: nursing faculty | To assess if longitudinal electronic medical record (EMR) data could be utilized to calculate the risk of inpatient falls and assess their accuracy compared with existing fall‐risk assessment tools. |
Study design: retrospective study Setting: Two tertiary hospitals with different EMR systems Data collection: secondary—development cohort: 220 events from the event‐reporting system and an additional 18 cases from chart reviews conducted after prefiltering the free‐text entries validation cohort: 292 falls identified from the reporting system and chart reviews. |
Numbers: 14,307 (development) and 21,172 (validation) Type: hospitalized inpatients admitted to six nursing units Gender: 43.03% and 52.90% female Age: majority 65+ years Ethnicity: not reported |
Probabilistic Bayesian network model (standard nursing terminologies mapped to local EMR data elements to develop and validate the fall‐risk prediction model) | Initial model had an error rate of 11.7% and a spherical payoff of 0.91, with a c‐statistic of 0.96. This represents far superior performance compared with the existing fall‐risk assessment tool (c‐statistic = 0.69). The cross‐site validation revealed an error rate of 4.87% and a spherical payoff of 0.96, with a c‐statistic of 0.99. The calibration curves for the model displayed more reliable results than the fall‐risk assessment tools alone. Nursing intervention data showed potential contributions to reducing the variance in the fall rate as did the risk factors of individual patients. |
| Cho et al. (2021), South Korea, Lead author: nursing faculty | To determine the impact of an electronic analytic tool (developed in Cho et al., 2019) for predicting fall risk on patient outcomes and nurses' responses. |
Study design: Nonrandomized controlled trial using an interrupted time series design Setting: 12 medical‐surgical nursing units at a public hospital Data collection: secondary—a fall prediction analytic tool was integrated into the EMR system and deployed in six nursing units with 204 nurses automatically receiving the prediction results on a daily basis. |
Numbers: All nurses (n = 204), 24,336 (intervention) and 18,140 (control) older patients Type: inpatients Gender: 51.41% and 49.91% female Age: mean age 61.45 and 65.30 years Ethnicity: not reported |
Analytic tool based on a probabilistic Bayesian network model (standard nursing terminologies mapped to local EMR data elements to develop and validate the fall‐risk prediction model) | Number of patient falls differed between the control (n = 382) and intervention (n = 325) units. Mean fall rate increased from 1.95 to 2.11 in control units and decreased from 1.92 to 1.79 in intervention units. Immediate reduction was 29.73% in the intervention group (z = −2.06, P = .039) and 16.58% in the control group (z = −1.28, P = .20), but there was no ongoing effect. The injury rate did not differ significantly between the two groups. Analytic tool may help with awareness of falls risk, leading to positive changes in nurses' interventions over time. |
| Greene et al. (2014), Ireland, Lead author: computer science faculty | To examine the utility of a range of individual assessments with older adults to screen for frailty and falls risk in older adults. |
Study design: quantitative —not explicitly reported Setting: clinic in a hospital Data collection: primary—geriatric and clinical assessments, falls history and a platform with inertial and pressure sensors to quantify the balance and mobility of older adults using three physical assessments (timed up and go [TUG], five times sit to stand and quiet standing balance. |
Numbers: 124 Type: community‐dwelling older adults Gender: 33 males and 91 females Age: at least 65 years old Ethnicity: not reported |
Support vector machines (SVM)—separate models were generated to classify participants using features from each test separately and the combined features from all three tests | In classifying falls history, combining sensor data from the TUG, FTSS and quiet standing balance tests to a single classifier model per gender yielded mean cross validated classification accuracy of 87.58% for the male model and 78.11% for the female model. The combination of the three tests, quantified using body‐worn inertial sensors, could lead to better methods for assessing falls risk. |
| Jung et al. (2020), South Korea, Lead author: nursing | To develop fall‐risk prediction models using EMR data and to evaluate the predictive performance of these models by comparing the results to those from the Hendrich II Fall Risk Model Validation (HIIFRM). |
Study design: quantitative—not explicitly reported Setting: a tertiary acute care hospital Data collection: secondary—165 features on falls risk extracted from clinical guidelines and existing literature. Data on fall‐related features extracted from 10 EMR sources. |
Numbers: 15,480 (fallers n = 310, nonfallers n = 15,170) Type: hospital inpatients Gender: 60% male in fallers and 53.7% in nonfallers Age: mean age 62.9 ± 14.7 in fallers Ethnicity: not reported |
Logistic regression, Cox PH regression and decision tree algorithms used to develop fall prediction models | Logistic regression had the highest predictive performance, with the exception of area under the curve (AUC), the time‐dependent sensitivity, specificity and positive predictive value of Cox PH regression were all slightly lower than those of the HIIFRM. The prediction performance of the decision tree was poorer. The models could be implemented in a clinical decision support system to automatically predict a patient's risk of falling. |
| Lee et al. (2010), Taiwan, Lead author: nursing faculty | To identify critical factors related to patient falls (outcome variable focused on injury or not after a fall event). |
Study design: quantitative—not explicitly reported Setting: hospital—1000‐bed medical centre employing about 800 nurses in southern Taiwan Data collection: secondary—72 fall‐related variables extracted from a web‐based incident reporting system developed by the nursing department. |
Numbers: 725 Type: fall incidents Gender: male n = 437 (60.3%) Age: 66–93 years n = 309 (42.6%); 1–65 years n = 416 (51.4%) Ethnicity: not reported |
ANN used to explore the relationship between the identified predictors and the outcome variables in constructing the model; multivariate stepwise logistic regression used to confirm impact of identified variables | The ANN model produced the following results: a receiver operating character (ROC) curve indicated 77% accuracy, the positive predictive value (PPV) was 68% and the negative predictive value (NPV) was 72%, while the multivariate stepwise logistic regression only identified three variables (fall assessment, anti‐psychosis medication and diuretics) as significant predictors with ROC curve of 42%, PPV of 26.24% and NPV of 87.12%. |
| Lee et al. (2020), South Korea, Lead author: nursing faculty | To compare six machine learning methods to identify predictive factors in resident falls in nursing homes. |
Study design: quantitative—not explicitly reported Setting: care home—60 nursing homes across 17 provinces in South Korea Data collection: secondary—fall‐related data based on chart reviews and participating organizations provided information on residents and staff related data via regular surveys in 2017. |
Numbers: not reported Type: nursing home residents Gender: female mean 78.95% Age: mean age 83.6 years Ethnicity: not reported |
Random forests (RF), logistic regression, support vector machines (SVM—linear, polynomial, radial and sigmoid) | Random forest was the most accurate model (0.883), followed by the logistic regression model, SVM linear and polynomial SVM (0.867). RF was a powerful algorithm to discern predictors of falls in nursing homes. For effective fall management, researchers should consider organizational characteristics and personal factors. |
| Makino et al. (2021), Japan, Lead author: medical faculty | To develop a simplified decision tree algorithm for fall prediction using easily measurable predictors with longitudinal cohort data. |
Study design: longitudinal observational study Setting: community centres Data collection: primary—baseline survey of fall predictors and follow‐up survey on recent falls, from a subcohort of a population‐based national cohort. TUG was assessed in two trials by nurses and gait speed measured in five trials. |
Numbers: 2520 Type: community‐dwelling older adults Gender: 1303 female (51.7%) Age: 71.1 years (±4.7) Ethnicity: not reported |
Decision tree analysis (C5.0 algorithm) to identify the optimal and minimum combination of risk factors necessary to predict the fall status of older adults | The decision tree model outperformed the logistic regression model with respect to AUC, accuracy, sensitivity, PPV and NPV. It consisted of common and easily measurable fall predictors, and the algorithm can explain the reasons for risk stratification; therefore, it can be implemented in clinical practice for early screening of fall risk and promotion of timely strategies for fall prevention. |
| Nakatani et al. (2020), Japan, Lead author: pharmaceutical company | To verify whether hospital inpatient falls can be predicted through unstructured nursing records obtained from EMRs using a natural language processing (NLP) and machine learning. |
Study design: quantitative—case–control study Setting: hospital—EMR of an acute hospital with 606 beds Data collection: secondary—335 patients with one or more fall incidents (fallers) were identified from the incident reports of the hospital. As a control group, 408 patients without falls (nonfallers) were randomly selected. |
Numbers: 743 (335 fallers, 408 nonfallers) Type: hospital inpatients Gender: 156 (45.6%) female fallers and 186 (54.4%) female nonfallers Age: 67.0 years (SD 17.1) |
Algorithm for NLP and a machine learning tool called Concept Encoder (used morphological analysis) | The prediction of falls using the dataset showed high accuracy, with an area under the ROC curve, sensitivity, specificity and odds ratio of mean 0.834 (SD 0.005), mean 0.769 (SD 0.013), mean 0.785 (SD 0.020) and mean 12.27 (SD 1.11) for five independent experiments, respectively. NLP algorithm combined with machine learning can effectively extract risk factors for falls from nursing records. |
| Nakanishi et al. (2021), Japan, Lead authors: information science and nursing faculty | To construct and test an algorithm for a fall‐risk assessment to identify essential risk factors for falls in hospitalized patients. |
Study design: quantitative—not explicitly reported Setting: hospital based Data collection: secondary—data from an electronic medical chart system (36 fall‐risk factors between nonfall and fall groups). |
Numbers: Nonfall (n = 56,673) and fall (n = 238) Gender: male 52.7% nonfall and male 58.4% fall group Age: median age 67.0 nonfall group and 71.5 years fall group Ethnicity: not reported |
Logistic regression used to identify important falls risk factors and decision tree analysis (on nine risk factors) used to classify the severity of falls risk (low, moderate, high, extra high) | Important risk factors were: (1) fall history, (2) muscle weakness of the lower limbs, (3) use of a walking aid, (4) stagger, (5) presence of infusion routes/tubes, (6) impaired judgement/comprehension, (7) impaired consciousness, (8) delirium, (9) use of sleeping drug, (10) urine or faecal incontinence, (11) need of toileting assistance and (12) night urination. The algorithm considered the correlation between fall‐risk factors. Nurses may be able to evaluate falls risk level and provide preventive interventions for patients using this approach. |
| Rabe et al. (2020), Germany, Lead author: technology company | To study the discriminative ability of a falls risk score with the aid of machine learning models. |
Study design: descriptive evaluation ‐ retrospective analysis Setting: not clear Data collection: primary—falls risk assessment (smartphone‐based video analysis with nursing staff capturing a senior person's gait) followed by a mobility test, a questionnaire assessing further falls risk factors via the app (self‐assessments or completed with the help of nursing staff). |
Numbers: 242 seniors Type: 131 seniors (54.1%) were living in nursing homes, 34 (14.1%) in assisted living facilities and 77 (31.8%) at home Gender: 169/242 participants (69.9%) were female Age: mean age of 84.6 years Ethnicity: not reported |
Multiple learning models were used, that is, logistic regression, Gaussian naïve Bayes, gradient boosting, support vector classification, random forest | The performance metrics (AUC, sensitivity, specificity and accuracy) for the logistic regression model were 0.9, 100%, 52% and 73%; the Gaussian naïve Bayes models were 0.9, 100%, 52% and 73%; the gradient boosting model were 0.85, 88%, 62% and 73%; the support vector classification models were 0.84, 88%, 67% and 76%; and the random forests models were 0.84, 88%, 57% and 70%. The falls risk app could support caretakers to conduct a valid falls risk assessment. |
| Yang et al. (2021), USA, Lead author: nursing faculty | To determine if machine learning (ML) can predict falls based on data from community‐dwelling older adults. |
Study design: quantitative—retrospective cohort study Setting: public health—the Behavioral Risk Factor Surveillance System (BRFSS), a national survey on noninstitutionalized adults on their health‐related risk behaviours Data collection: secondary—individuals older than 60 years who responded to BRFSS falls questions. |
Numbers: 214,777 (training 75%, testing 25%) Type : community‐dwelling older adults Gender: female 61.2%, male 38.8% Age: 70.27 (SD 6.76) |
Random forests compared with logistic regression | Regarding fall prediction, the random forest classifier achieved 33% sensitivity, 41% positive predictive value and 37% F1‐measure on the default threshold value of 50%, as compared with 70% sensitivity, 34% positive predictive value and 50% F1‐measure on the decreased threshold value of 30%. This was statistically significantly worse in predicting falls, compared with logistic regression. Model performance was too low to be clinically useful. |
| Yokota et al. (2017), Japan, Lead author: health care information management faculty | To create a system to assist nurses in evaluating the fall risk of patients and to evaluate the fall risk of a certain day using the patient's status, attributes and location information on that previous day. |
Study design: quantitative—not explicitly reported Setting: hospital EMR Data collection: secondary—intensity‐of‐nursing‐care‐needs data and patients' hospital admission or discharge movement data for general hospital wards, data on patients' characteristics and activities, data from admitting hospital ward and fall report data from an incident reporting system. |
Numbers: 1950 cases of falls were identified (0.16%) Type: remaining 1,221,737 cases being nonfalls (99.84%) Gender: 51.5% males and 48.5% females Age: average age of 62.4 years |
Support vector machines model used for training the data (all features were used) | The model showed clear sensitivity and specificity toward unknown data and determined whether a patient will fall on the following day by using their status and other information on the current day. Using this model, nurses in charge may be able to determine the degree of fall risk objectively, without having to spend time gathering new information. |
Note: AI, artificial intelligence; ANN, artificial neural network; AUC, area under the curve; BRFSS, Behavioral Risk Factor Surveillance System; CI, confidence interval; EMR, electronic medical record; FTSS, five times sit to stand; HIIFRM, Hendrich II Fall Risk Model Validation; ML, machine learning; NLP, natural language processing; NPV, negative predictive value; PPV, positive predictive value; RF, random forests; SD, standard deviation; SVM, support vector machines; ROC, receiver operating characteristic; TUG, timed up and go.
3. RESULTS
Fourteen empirical studies were included, published between 2010 and 2021. Four were located in South Korea and four in Japan, with one study being conducted in Taiwan, Turkey, Ireland, France, Germany and the United States (Figure 2). The study designs were all quantitative in nature, using retrospective case–control or cohort designs, with some not explicitly reporting the methodology used. Nine studies employed secondary analysis on existing falls related datasets from electronic health records, chart reviews, clinical guidelines or published scientific literature, web‐based reporting systems, national surveys or registry data (Cho et al., 2019, 2021; Jung et al., 2020; Lee et al., 2010, 2020; Nakanishi et al., 2021; Nakatani et al., 2020; Yang et al., 2021; Yokota et al., 2017). Four studies conducted primary research by collecting falls associated data via geriatric or clinical assessments of older adults, physical and mobility assessments using sensors to detect risk factors and self‐reported questionnaires completed by older participants (Beauchet et al., 2018; Greene et al., 2014; Makino et al., 2021; Rabe et al., 2020). Only one study used a combination of primary and secondary falls data for analysis (Ağartioğlu Kundakçi et al., 2020). The setting for the majority of included studies was a hospital clinic or hospital‐based electronic medical record (EMR), with one taking place in a care home (Lee et al., 2020), and one in community centres (Makino et al., 2021). Another study used a population health survey dataset from non‐institutionalized adults (Yang et al., 2021) and one included a variety of settings in primary care (Rabe et al., 2020) (Table 2).
FIGURE 2.
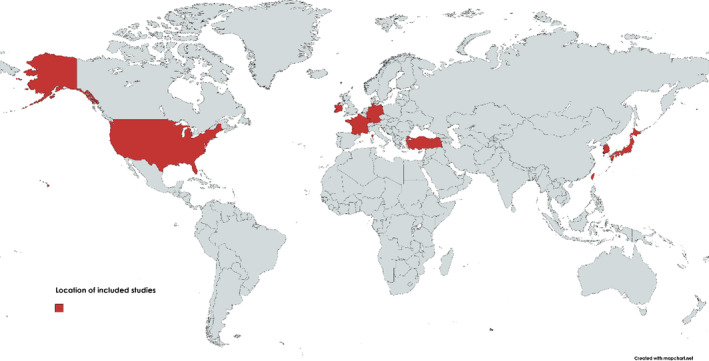
Location of included studies (using https://mapchart.net/)
3.1. AI techniques for falls management in older adult care
All 14 studies utilized one or more supervised machine learning methods, predictive algorithms that build mathematical models from a training dataset that contains variables and outcomes of interest (Table 2). The algorithm ‘learns’ patterns and relationships within a dataset to predict an outcome, without being explicitly programmed (Beam & Kohane, 2018). Three studies employed a decision tree supervised learning method to calculate the cost of nursing interventions for preventing falls or classify risk factors to predict falls in the elderly (Ağartioğlu Kundakçi et al., 2020; Makino et al., 2021; Nakanishi et al., 2021). Greene et al. (2014) and Yokota et al. (2017) employed a support vector machines model to screen and classify older adults for falls risk based on a comprehensive clinical dataset. Two studies used artificial neural networks to predict falls from 10 factors identified via structured data within a nursing incident reporting database, preselected from a set of 72 based on univariate correlation with occurrence of falls (Beauchet et al., 2018; Lee et al., 2010).
Two studies employed Bayesian networks, a graphical model that denotes probabilistic relationships between variables. Cho et al. (2019) extracted nursing notes and statements from a hospital EMR and chart reviews from units with high falls rates to help predict the risk of inpatient falls using a probabilistic Bayesian network model. In a follow‐up study, this fall prediction analytical tool was integrated into a hospital EMR which generated a 24‐h falls risk prediction for each patient and triggered an ‘at‐risk’ alert on the system along with a care plan of falls interventions prioritized according to patients' individual risk factors (Cho et al., 2021). Four studies compared a range of machine learning techniques to determine their predictive performance for assessing falls risk among older people, with some comparing them against standardized falls risk assessment tools and two reported logistic regression had the highest predictive performance (Jung et al., 2020; Lee et al., 2020; Rabe et al., 2020; Yang et al., 2021). Finally, Nakatani et al. (2020) was the only study that used natural language processing in conjunction with a specially designed machine learning algorithm called Concept Encoder, employing morphological analysis to determine meaning in language, to help predict inpatient hospital falls from unstructured nursing records.
3.2. Nurses' involvement in AI research for falls management
The level of nursing involvement in AI research to help manage falls in older adults varied. In eight studies, nurses were the lead researcher or lead author (Ağartioğlu Kundakçi et al., 2020; Cho et al., 2019, 2021; Jung et al., 2020; Lee et al., 2010, 2020; Nakanishi et al., 2021; Yang et al., 2021), while four studies were led by other scientific disciplines including medicine, computer science, health economics and health information management. Two studies were directed by commercial companies, a pharmaceutical enterprise and a technology company that specialized in AI motion analysis. Only one study was co‐led by two scientific faculty from both nursing and information science (Nakanishi et al., 2021) and two studies included nurses as part of the research team, where they participated in conceiving, designing and conducting the experiments and writing the scientific manuscript (Beauchet et al., 2018; Yokota et al., 2017).
In four cases, nurses were actively involved in collecting the falls dataset used in the research. In Beauchet et al. (2018), nurses in a hospital undertook routine assessments with older inpatients covering medication, mobility, cognitive impairment, informal carer and social services, along with falls history and falls risk, as well as recording falls incidents. Similarly, in Greene et al. (2014), a comprehensive geriatric assessment was undertaken by nurses at a hospital clinic, which included visual acuity and visual contrast sensitivity tests, blood pressure and maximum grip strength measurements, balance and mobility tests using inertial sensors and an examination of frailty status. Nurses also assisted in Makino et al. (2021) by assessing falls in older persons via a baseline and follow‐up survey, approximately 48 months later, while also investigating prescribed medications and medical history, and measuring gait speed and timed up and go. Lastly, nursing staff in Rabe et al. (2020) conducted a fall‐risk assessment where mobility was captured via video and followed by an in‐depth questionnaire completed via a smartphone application.
One study did not involve nurses directly but used secondary data from nursing records in an EMR which included patient statements, nursing observations and vital signs, nursing assessments, medical treatments, medication administration, patient messages and other comments from nurses were also used (Nakatani et al., 2020). Interestingly, Cho et al. (2021) was the only study where nurses in clinical practice used an AI‐based system across six hospital units for real‐world clinical validation. The AI‐based fall prediction tool was trialled alongside a standardized falls risk assessment to determine which was more accurate in identifying older patients at risk of falling and to encourage nurses to implement falls prevention strategies, with the intervention group implementing more falls risk targeted interventions. While the other 13 studies utilized real falls related data to train and test predictive algorithms, these were not implemented in an AI‐based tool/system that nurses could use to inform decision making and the delivery of older adult care.
4. DISCUSSION
This review synthesized evidence on nurses' involvement in AI research for managing falls in older adults. It found that machine learning techniques were the most common method used, primarily to identify factors that could more accurately predict falls in older adults, and in some cases compared these to standardized falls risk assessment tools. The widespread use of machine learning in falls research has been reported (Usmani et al., 2021), although natural language processing, fuzzy logic, computer vision and other AI techniques are starting to be utilized more (O'Connor et al., 2022). Some research also suggests that logistic regression can perform just as well as machine learning for clinical prediction models (Christodoulou et al., 2019). Furthermore, the studies in this review noted some common limitations when using AI such as datasets with missing or incomplete falls related information, often from one source organization within a particular geographic region and short timeframe, which could impact the quality of predictive models. These issues have been widely reported in AI literature (Bates et al., 2021). Hence, AI approaches used in managing falls in older adults needs further exploration, alongside developing longitudinal datasets that are as comprehensive as possible, to help build robust predictive models with clinical utility.
This review also highlighted that most studies only reported the potential of AI to improve falls prediction, with only a single study deploying an AI analytical tool with nurses in a hospital to help identify at‐risk older adults. Many studies have taken a similar approach to developing algorithms (Bargiotas et al., 2021; Usmani et al., 2021), without moving beyond assessing their predictive performance to examine if and how they could fit into care pathways and be interpreted by clinicians to inform decision making and the care delivery. Furthermore, no study in the review examined how AI could be utilized to identify and support an older person who experienced a fall, through the use of physiological or environmental sensors or other integrated systems such as smart homes. There is a growing literature in the engineering and computer science fields addressing this (Bet et al., 2019) which nurses should be cognisant of and become involved in.
The review findings also emphasized that nurses are leading some AI research for falls management in older adults but other professions such as medicine, computer science and engineering are also active in this field, and multidisciplinary collaborations are common, which is mirrored by other reviews of AI in nursing (Ng et al., 2021; O'Connor et al., 2022; von Gerich et al., 2022). Ronquillo et al. (2021) recommend nurses become more active in AI initiatives in health care to ensure these approaches are developed and applied appropriately, with practical and clinical utility in mind. Education and training may be required to upskill nurses in areas of informatics such as AI (Booth et al., 2021), so they can participate and lead this type of research, facilitate the collection of falls related digital datasets and use AI‐based technologies in their practice to enhance older adult care.
4.1. Strengths and limitations
The review was strengthened by using an open access platform to register the planned research, employing a rigorous database search, screening studies using independent reviewers and utilizing international best practice guidelines to improve the transparency and reporting of the review. However, as the search terms focused on the nursing profession specifically, other literature from computer science, engineering and related fields that are developing and testing AI techniques for falls management were not included. In addition, alternative sources of scientific studies such as conference proceedings, theses, pre‐print and discursive articles were not included which may limit the comprehensiveness and utility of the review findings somewhat. Critical appraisal of the included studies was not conducted, so the methodological quality and the overall weight of evidence in this area remain largely unknown. Therefore, the results of the review should be interpreted with caution.
5. CONCLUSION
As ageing societies become commonplace, the risk of and impact from falls among older adults will continue to grow, making AI research on falls management an important area that the nursing profession should contribute to. This review highlighted how nurses have participated to date in is emerging research area, along with the potential that AI techniques have in identifying relevant risk factors and building predictive models that could be used by nurses to manage falls among older people. While the evidence base is preliminary, there are some early indications that developing and testing AI could lead to more robust predictive analytical systems that support improvements in gerontological nursing practice and patient care.
6. IMPLICATIONS FOR NURSING MANAGEMENT
Several key implications emerged from the review findings. First, more rigorous experimental research is needed to determine how effective AI techniques are in predicting aspects of falls in older adults and the impact these models have on nurses' decision making and the delivery of personalized care. More implementation science that examines how to deploy AI‐based technologies with nurses who care for older adults across a range of acute and primary care settings could facilitate a better understanding of whether these predictive tools have practical and clinical utility in assessing and managing falls. Second, nurses should pursue interdisciplinary collaborations in AI research for managing falls to harness a range of expertise, ensuring a holistic approach to supporting older people is taken. Third, educational opportunities should be created for nurses to learn about machine learning, natural language processing and AI more generally, so the profession has knowledge and skills to participate and lead AI research that facilitates older adult care. Fourthly, more digital datasets of falls risk factors or conditions that lead to an actual fall in ageing populations could be created to support future AI research. This would help ensure algorithms being developed and tested have rich data from which to build predictive models that accurately reflect the real life of older adults, enabling nurses to improve the management of falls in this key patient group.
CONFLICT OF INTEREST
The authors declare no conflict of interest.
ETHICAL STATEMENT
Ethical approval was not required for this work, as it is a review of the literature and involved no collection or analysis of primary data.
Supporting information
Appendix S1. Preferred Reporting Items for Systematic reviews and Meta‐Analyses extension for Scoping Reviews (PRISMA‐ScR) Checklist
Appendix S2. Search strategies for CINAHL (EBSCO)
O'Connor, S. , Gasteiger, N. , Stanmore, E. , Wong, D. C. , & Lee, J. J. (2022). Artificial intelligence for falls management in older adult care: A scoping review of nurses' role. Journal of Nursing Management, 30(8), 3787–3801. 10.1111/jonm.13853
Funding information
This research did not receive any specific grant from funding agencies in the public, commercial or not‐for‐profit sectors.
REFERENCES
- Ağartioğlu Kundakçi, G. , Yılmaz, M. , & Sözmen, M. K. (2020). Determination of the costs of falls in the older people according to the decision tree model. Archives of Gerontology and Geriatrics, 87, 104007. 10.1016/j.archger.2019.104007 [DOI] [PubMed] [Google Scholar]
- Bargiotas, I. , Kalogeratos, A. , Limnios, M. , Vidal, P. P. , Ricard, D. , & Vayatis, N. (2021). Revealing posturographic profile of patients with Parkinsonian syndromes through a novel hypothesis testing framework based on machine learning. PLoS ONE, 16(2), e0246790. 10.1371/journal.pone.0246790 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bates, D. W. , Levine, D. , Syrowatka, A. , Kuznetsova, M. , Craig, K. J. T. , Rui, A. , Jackson, G. P. , & Rhee, K. (2021). The potential of artificial intelligence to improve patient safety: A scoping review. NPJ Digital Medicine, 4(1), 54. 10.1038/s41746-021-00423-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beam, A. L. , & Kohane, I. S. (2018). Big data and machine learning in health care. JAMA: The Journal of the American Medical Association, 319(13), 1317–1318. 10.1001/jama.2017.18391 [DOI] [PubMed] [Google Scholar]
- Beauchet, O. , Noublanche, F. , Simon, R. , Sekhon, H. , Chabot, J. , Levinoff, E. J. , Kabeshova, A. , & Launay, C. P. (2018). Falls risk prediction for older inpatients in acute care medical wards: Is there an interest to combine an early nurse assessment and the artificial neural network analysis? The Journal of Nutrition, Health & Aging, 22(1), 131–137. 10.1007/s12603-017-0950-z [DOI] [PubMed] [Google Scholar]
- Bergen, G. , Stevens, M. R. , & Burns, E. R. (2016). Falls and fall injuries among adults aged ≥65 years—United States, 2014. MMWR. Morbidity and Mortality Weekly Report, 65(37), 993–998. 10.15585/mmwr.mm6537a2 [DOI] [PubMed] [Google Scholar]
- Bet, P. , Castro, P. C. , & Ponti, M. A. (2019). Fall detection and fall risk assessment in older person using wearable sensors: A systematic review. International Journal of Medical Informatics (Shannon, Ireland), 130, 103946. 10.1016/j.ijmedinf.2019.08.006 [DOI] [PubMed] [Google Scholar]
- Booth, R. G. , Strudwick, G. , McBride, S. , O'Connor, S. , & Solano López, A. L. (2021). How the nursing profession should adapt for a digital future. BMJ: British Medical Journal, 373, n1190. 10.1136/bmj.n1190 [DOI] [Google Scholar]
- Bowen, M. , & Mason, T. (2012). Forensic and non‐forensic psychiatric nursing skills and competencies for psychopathic and personality disordered patients. Journal of Clinical Nursing, 21(23–24), 3556–3564. 10.1111/j.1365-2702.2011.03970.x [DOI] [PubMed] [Google Scholar]
- Cho, I. , Boo, E.‐H. , Chung, E. , Bates, D. W. , & Dykes, P. (2019). Novel approach to inpatient fall risk prediction and its cross‐site validation using time‐variant data. Journal of Medical Internet Research, 21(2), e11505. 10.2196/11505 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cho, I. , Jin, I. S. , Park, H. , & Dykes, P. C. (2021). Clinical impact of an analytic tool for predicting the fall risk in inpatients: Controlled interrupted time series. JMIR Medical Informatics, 9(11), e26456. 10.2196/26456 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Christodoulou, E. , Ma, J. , Collins, G. S. , Steyerberg, E. W. , Verbakel, J. Y. , & Van Calster, B. (2019). A systematic review shows no performance benefit of machine learning over logistic regression for clinical prediction models. Journal of Clinical Epidemiology, 110, 12–22. 10.1016/j.jclinepi.2019.02.004 [DOI] [PubMed] [Google Scholar]
- Florence, C. S. , Bergen, G. , Atherly, A. , Burns, E. , Stevens, J. , & Drake, C. (2018). Medical costs of fatal and nonfatal falls in older adults. Journal of the American Geriatrics Society (JAGS), 66(4), 693–698. 10.1111/jgs.15304 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ganz, D. A. , & Latham, N. K. (2020). Prevention of falls in community‐dwelling older adults. The New England Journal of Medicine, 382(8), 734–743. 10.1056/NEJMcp1903252 [DOI] [PubMed] [Google Scholar]
- Greene, B. R. , Doheny, E. P. , Kenny, R. A. , & Caulfield, B. (2014). Classification of frailty and falls history using a combination of sensor‐based mobility assessments. Physiological Measurement, 35(10), 2053–2066. 10.1088/0967-3334/35/10/2053 [DOI] [PubMed] [Google Scholar]
- Hartholt, K. A. , Polinder, S. , van der Cammen, T. J. , Panneman, M. J. , van der Velde, N. , van Lieshout, E. M. , Patka, P. , & Van Beeck, E. F. (2012). Costs of falls in an ageing population: A nationwide study from the Netherlands (2007–2009). Injury, 43(7), 1199–1203. 10.1016/j.injury.2012.03.033 [DOI] [PubMed] [Google Scholar]
- Jiang, Y. , Xia, Q. , Wang, J. , Zhou, P. , Jiang, S. , Diwan, V. K. , & Xu, B. (2019). Environmental risk factors associated with falls among older people living in long‐term aged care facilities: A prospective study. The Lancet, 394, S23. 10.1016/s0140-6736(19)32359-1 [DOI] [Google Scholar]
- Johnson, M. , George, A. , & Tran, D. T. (2011). Analysis of falls incidents: Nurse and patient preventive behaviours. International Journal of Nursing Practice, 17(1), 60–66. 10.1111/j.1440-172X.2010.01907.x [DOI] [PubMed] [Google Scholar]
- Jung, H. , Park, H. A. , & Hwang, H. (2020). Improving prediction of fall risk using electronic health record data with various types and sources at multiple times. CIN: Computers, Informatics, Nursing, 38(3), 157–164. 10.1097/CIN.0000000000000561 [DOI] [PubMed] [Google Scholar]
- Kenny, R. A. , Romero‐Ortuno, R. , & Cogan, L. (2012). Falls. Medicine, 41(3), 155–159. 10.1016/j.mpmed.2012.12.007 [DOI] [Google Scholar]
- Lee, S.‐K. , Ahn, J. , Shin, J. H. , & Lee, J. Y. (2020). Application of machine learning methods in nursing home research. International Journal of Environmental Research and Public Health, 17(17), 6234. 10.3390/ijerph17176234 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee, T.‐T. , Liu, C.‐Y. , Kuo, Y.‐H. , Mills, M. E. , Fong, J.‐G. , & Hung, C. (2010). Application of data mining to the identification of critical factors in patient falls using a web‐based reporting system. International Journal of Medical Informatics (Shannon, Ireland), 80(2), 141–150. 10.1016/j.ijmedinf.2010.10.009 [DOI] [PubMed] [Google Scholar]
- Leung, M. (2021). Approach to: Fall in the elderly population. McGill Journal of Medicine, 19(1). 10.26443/mjm.v19i1.313 [DOI] [Google Scholar]
- Makino, K. , Lee, S. , Bae, S. , Chiba, I. , Harada, K. , Katayama, O. , Tomida, K. , Morikawa, M. , & Shimada, H. (2021). Simplified decision‐tree algorithm to predict falls for community‐dwelling older adults. Journal of Clinical Medicine, 10(21), 5184. 10.3390/jcm10215184 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nakanishi, T. , Ikeda, T. , Nakamura, T. , Yamanouchi, Y. , Chikamoto, A. , & Usuku, K. (2021). Development of an algorithm for assessing fall risk in a Japanese inpatient population. Scientific Reports, 11(1), 17993. 10.1038/s41598-021-97483-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nakatani, H. , Nakao, M. , Uchiyama, H. , Toyoshiba, H. , & Ochiai, C. (2020). Predicting inpatient falls using natural language processing of nursing records obtained from Japanese electronic medical records: Case‐control study. JMIR Medical Informatics, 8(4), e16970. 10.2196/16970 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ng, Z. Q. P. , Ling, L. Y. J. , Chew, H. S. J. , & Lau, Y. (2021). The role of artificial intelligence in enhancing clinical nursing care: A scoping review. Journal of Nursing Management. 10.1111/jonm.13425 [DOI] [PubMed] [Google Scholar]
- O'Connor, S. , Yan, Y. , Thilo, F. J. , Felzmann, H. , Dowding, D. , & Lee, J. J. (2022). Artificial intelligence in nursing and midwifery: A systematic review. Journal of Clinical Nursing. 10.1111/jocn.16478 [DOI] [PubMed] [Google Scholar]
- Peltzer, K. , Chatterji, S. , Hestekin, H. , O'Driscoll, T. , Williams, J. S. , & Kowal, P. (2013). Measuring prevalence and risk factors for fall‐related injury in older adults in low‐ and middle‐income countries: Results from the WHO Study on Global AGEing and Adult Health (SAGE). Retrieved from Geneva, Switzerland: http://cdrwww.who.int/healthinfo/sage/SAGEWorkingPaper6_Wave1Falls.pdf
- Rabe, S. , Azhand, A. , Pommer, W. , Müller, S. , & Steinert, A. (2020). Descriptive evaluation and accuracy of a mobile app to assess fall risk in seniors: Retrospective case‐control study. JMIR Aging, 3(1), e16131. 10.2196/16131 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ronquillo, C. E. , Peltonen, L.‐M. , Pruinelli, L. , Chu, C. H. , Bakken, S. , Beduschi, A. , Cato, K. , Hardiker, N. , Junger, A. , Michalowski, M. , Nyrup, R. , Rahimi, S. , Reed, D. N. , Salakoski, T. , Salanterä, S. , Walton, N. , Weber, P. , Wiegand, T. , Topaz, M. , & Topaz, M. (2021). Artificial intelligence in nursing: Priorities and opportunities from an international invitational think‐tank of the Nursing and Artificial Intelligence Leadership Collaborative. Journal of Advanced Nursing, 77(9), 3707–3717. 10.1111/jan.14855 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Samoili, S. , López Cobo, M. , Gómez, E. , De Prato, G. , Martínez‐Plumed, F. , & Delipetrev, B. (2020). AI Watch: Defining artificial intelligence—Towards an operational definition and taxonomy of artificial intelligence. Retrieved from Luxembourg: https://publications.jrc.ec.europa.eu/repository/bitstream/JRC118163/jrc118163_ai_watch._defining_artificial_intelligence_1.pdf
- Schoene, D. , Heller, C. , Aung, Y. N. , Sieber, C. C. , Kemmler, W. , & Freiberger, E. (2019). A systematic review on the influence of fear of falling on quality of life in older people: Is there a role for falls? Clinical Interventions in Aging, 14, 701–719. 10.2147/CIA.S197857 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seibert, K. , Domhoff, D. , Bruch, D. , Schulte‐Althoff, M. , Fürstenau, D. , Biessmann, F. , & Wolf‐Ostermann, K. (2021). Application scenarios for artificial intelligence in nursing care: Rapid review. Journal of Medical Internet Research, 23(11), e26522. 10.2196/26522 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spiegel, B. , Fuller, G. , Lopez, M. , Dupuy, T. , Noah, B. , Howard, A. , Albert, M. , Tashjian, V. , Lam, R. , Ahn, J. , Dailey, F. , Rosen, B. T. , Vrahas, M. , Little, M. , Garlich, J. , Dzubur, E. , IsHak, W. , & Danovitch, I. (2019). Virtual reality for management of pain in hospitalized patients: A randomized comparative effectiveness trial. PLoS ONE, 14(8), e0219115. 10.1371/journal.pone.0219115 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stanmore, E. K. , Mavroeidi, A. , de Jong, L. D. , Skelton, D. A. , Sutton, C. J. , Benedetto, V. , Munford, L. A. , Meekes, W. , Bell, V. , & Todd, C. (2019). The effectiveness and cost‐effectiveness of strength and balance Exergames to reduce falls risk for people aged 55 years and older in UK assisted living facilities: A multi‐centre, cluster randomised controlled trial. BMC Medicine, 17(1), 49. 10.1186/s12916-019-1278-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Turner, S. , Kisser, R. , & Rogmans, W. (2015). Falls among older adults in the EU‐28: Key facts from the available statistics. Retrieved from Amsterdam: https://eupha.org/repository/sections/ipsp/Factsheet_falls_in_older_adults_in_EU.pdf
- Usmani, S. , Saboor, A. , Haris, M. , Khan, M. A. , & Park, H. (2021). Latest research trends in fall detection and prevention using machine learning: A systematic review. Sensors (Basel, Switzerland), 21(15), 5134. 10.3390/s21155134 [DOI] [PMC free article] [PubMed] [Google Scholar]
- von Gerich, H. , Moen, H. , Block, L. J. , Chu, C. H. , DeForest, H. , Hobensack, M. , Michalowski, M. , Mitchell, J. , Nibber, R. , Olalia, M. A. , Pruinelli, L. , Ronquillo, C. E. , Topaz, M. , & Peltonen, L.‐M. (2022). Artificial intelligence‐based technologies in nursing: A scoping literature review of the evidence. International Journal of Nursing Studies, 127, 104153. 10.1016/j.ijnurstu.2021.104153 [DOI] [PubMed] [Google Scholar]
- Wang, X. , Ellul, J. , & Azzopardi, G. (2020). Elderly fall detection systems: A literature survey. Frontiers in Robotics and AI, 7, 71. 10.3389/frobt.2020.00071 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Waters, D. , Crisp, J. , Rychetnik, L. , & Barratt, A. (2009). The Australian experience of nurses' preparedness for evidence‐based practice. Journal of Nursing Management, 17(4), 510–518. 10.1111/j.1365-2834.2009.00997.x [DOI] [PubMed] [Google Scholar]
- World Health Organization . (2021). Falls. Fact Sheets. Retrieved from https://www.who.int/news-room/fact-sheets/detail/falls
- Yang, R. , Plasek, J. M. , Cummins, M. R. , & Sward, K. A. (2021). Predicting falls among community‐dwelling older adults: A demonstration of applied machine learning. CIN: Computers, Informatics, Nursing, 39(5), 273–280. 10.1097/CIN.0000000000000688 [DOI] [PubMed] [Google Scholar]
- Yokota, S. , Endo, M. , & Ohe, K. (2017). Establishing a classification system for high fall‐risk among inpatients using support vector machines. CIN: Computers, Informatics, Nursing, 35(8), 408–416. 10.1097/CIN.0000000000000332 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix S1. Preferred Reporting Items for Systematic reviews and Meta‐Analyses extension for Scoping Reviews (PRISMA‐ScR) Checklist
Appendix S2. Search strategies for CINAHL (EBSCO)


