Abstract
Aims
We aim (i) to redesign sepsis's clinical pathway and fit the organizational requirements of a novel machine‐learning algorithm incorporating a novel biomarker test and (ii) to assess adoption drivers of the new combined technology.
Background
There is an urgent need to achieve sepsis' early detection and diagnostic excellence.
Methods
A qualitative study based on semi‐structured interviews conducted at the target site and across other Italian hospitals. A content analysis was undertaken, emergent themes were selected and categorized, and interviews were conducted until saturation was reached.
Results
Sixteen nurses (10 at the target site and six across other hospitals) and nine non‐nursing professionals (seven at the target site and two across other hospitals) were interviewed. An organizational redesign was identified as the primary adoption driver. Even though nurses perceived workload increase related to the machine‐learning component, technology acceptability was relatively high, as the standardization of tasks was perceived as crucial to improving professional satisfaction.
Conclusions
A novel business‐oriented solution based on machine learning requires interprofessional integration, new professional roles, infrastructure improvement, and data integration to be effectively implemented.
Implications for Nursing Management
Lessons learned from this study suggest the need to involve nurses in the early stages of the design of new machine‐learning technologies and the importance of training nurses on sepsis management through the support of disruptive technological innovation.
Keywords: artificial intelligence, biomarker, machine learning, nursing and hospital practice, sepsis
1. BACKGROUND
Sepsis is a complex time‐dependent, life‐threatening illness caused by a dysregulated immune host response to infection (Singer et al., 2016). Delays in the identification and treatment of sepsis during its early stages can contribute significantly to adverse outcomes until death, making it vital to achieving an early diagnosis (Angus & Bindman, 2022). Worldwide there are an estimated 49 million cases of sepsis each year, and a mortality rate ranging from 20% to 40%, as sepsis remains the most frequent cause of in‐hospital death and emergency readmission in the United States (Rudd et al., 2020).
Several efforts have been made to improve the diagnosis of sepsis, all based on the hypothesis that identifying sepsis at an earlier stage will improve outcomes by reducing the time‐to‐antibiotics and total costs of care (Agnello et al., 2020; Piva et al., 2021). These attempts exclusively focused on hospital settings and mainly fell into four categories: (i) guidelines to standardize the clinical pathway; (ii) diagnostic criteria to automatize sepsis surveillance; (iii) artificial intelligence‐based tools, such as machine‐learning; and (iv) new biomarker essays (Angus & Bindman, 2022).
Tuscany, a region located in central Italy with about 3.8 million inhabitants, is characterized by an advanced regional health care system at the frontline of innovation to fight sepsis. Since 2016, Tuscany has integrated two approaches in hospital practice: (i) the new agreed ‘golden hour’ model aiming to harmonize the diagnostic workup and early treatment strategies (Calci et al., 2018) and (ii) the use of diagnostic scores and indicators based on non‐specific sepsis' parameters (Rhodes et al., 2017). Despite these valuable efforts, sepsis' early diagnosis to be achieved before the patient meets established signs or symptoms remains complex and uncertain. More than 15,000 cases of sepsis are expected each year in Tuscany, with a 33% increase in hospitalizations in more recent years (Toscana, 2019). However, data derived from administrative databases are underestimated as the actual incidence increases and may be accelerated by the COVID‐19 virus, which can lead to sepsis and increase the risk for other infections causing sepsis (Zhou et al., 2020).
This study relies on the know‐how gained by the Tuscany Region in managing and treating sepsis and documents the current evolution of sepsis' early detection approaches through a clinical observational study carried out at San Donato Hospital—the most significant health unit of Arezzo located in Tuscany, Italy—since June 2019 to validate a novel combined technology.
‘Monocyte Distribution Width’ is a new biomarker developed by Beckman Coulter and recently validated in hospital practice of the Emergency Department for the early diagnosis of sepsis, showing an optimal sensitivity and specificity ranging from 0.645 to 0.920 and from 0.604 to 0.929 (Agnello et al., 2020). Through whole blood withdrawal, the new biomarker test allows measurements of the standard deviation of the mean monocytes volume based on morphological changes in circulating monocytes. The predictive proficiency of the biomarker can be used by a prototype version of a new machine‐learning‐based sepsis detection algorithm (Islam et al., 2019), able to alert nurses and doctors when a suspect of sepsis occurs and builds a patient's risk score simply by entering in a PC some medical measurements (e.g., vital parameters and clinical observations).
Exploring multifactorial determinants of technology acceptance by nurses and other professionals is strategic for management to support adoption within a health organization through tailored strategies leading to organizational flexibility (Manetti et al., 2017, 2020). A qualitative research design was employed to generate rich information allowing for an in‐depth understanding of nurses' and other professionals' determinants, motivations, and emotional perceptions concerning technology adoption and organizational change. Indeed, qualitative techniques are appropriate in the early stages of research when the need for collecting more information (e.g., participants' observation) is particularly relevant. The aim of this qualitative study was twofold: (i) redesign the sepsis clinical pathway at San Donato Hospital to fit the organizational requirements of the new integrated approach and (ii) assess organizational and human factors of nurses and other relevant health workers to accelerate adoption into nursing and interprofessional practice.
2. METHODS
2.1. Study design
According to the study's descriptive aim, a qualitative research design was performed using inductive content analysis that allowed the authors to systematically organize data from a semi‐structured interview study in a structured way (Vaismoradi et al., 2013). Data were reported here according to consolidated criteria for qualitative research (Tong et al., 2007).
2.2. Data collection
Preliminary data on the clinical pathway and hospital organization were collected within a desk analysis to help the interview guide design and facilitate interviews. The desk analysis was conducted but not limited to sepsis' regional regulations, clinical guidelines, hospital data, and terminology. Subsequently, data were collected within a semi‐structured interview study between November 2020 and December 2021. The interviews were undertaken by two researchers (S. M. and M. C.) either in face‐to‐face or telematic mode (via Skype or Teams) depending on the availability of the respondent and the COVID‐19 restrictions at the time. One researcher worked as co‐facilitator, ensuring that each interview was audio‐recorded and observed participants' non‐verbal behaviour utilizing a specific observation grid. Before starting each interview, opening instructions were provided. A multidisciplinary expert panel defined the interview guide, including specific questions to guide the discussion (Table 1). The interviews had an average duration of 50 min. Interviews were conducted until saturation—defined as no new themes emerged—was reached. The transcripts were returned to participants for comments and corrections, and no interviews were repeated.
TABLE 1.
The interview guide
| Semi‐structured interview protocol |
|---|
|
2.3. Participant selection and setting
Senior nurses and other expert non‐nursing professionals were recruited at San Donato Hospital (Arezzo, Italy) alongside the clinical study based on purposeful sampling (Morse & Field, 1995). We employed the snowball technique (Naderifar et al., 2017) to enrol nursing staff, nursing directors, nursing managers, and non‐nursing professionals across other teaching hospitals in Tuscany Region (Italy) with deep know‐how in managing and treating sepsis. Purposive sampling was guided by the research aim to obtain the saturation of the topics under study. An over‐recruitment was performed to allow for potential dropout. Participants were contacted via email and informed about the study aims. If participants agreed to proceed with the recruitment, they received further information and the interview protocol (Table 1). The participant sample consisted of 16 nurses (10 at the target site and six across other hospitals), seven physicians (five at the target site and two across other hospitals), and two laboratory technicians, all recruited at the target site. Participants' socio‐demographic characteristics are summarized in Table 2.
TABLE 2.
Participants' socio‐demographic characteristics
| Sample (N) | Percentage (%) | |
|---|---|---|
| Distribution by gender | ||
| Male | 10 | 40% |
| Female | 15 | 60% |
| Total | 25 | 100% |
| Distribution by age | ||
| 30–49 years | 17 | 68% |
| 50–62 years | 5 18,76 | 20% |
| 63–70 years | 3 | 12% |
| Distribution by years of experience | ||
| 10–19 years | 17 | 68% |
| 20–29 years | 3 | 12% |
| 30 years or more | 5 | 20% |
| Distribution by hospital | ||
| Target site | 17 | 68% |
| Other hospitals | 8 | 32% |
| Distribution by professional role | ||
| Nurse managers/directors | 6 | 24% |
| Nurse staff | 10 | 40% |
| Physicians | 7 | 28% |
| Lab technicians | 2 | 8% |
| Distribution by hospital department | ||
| Management | 3 | 12% |
| Emergency department | 10 | 40% |
| Infectious disease | 5 | 20% |
| Geriatrics | 5 | 20% |
| Laboratory | 2 | 8% |
2.4. Data analysis
Two researchers (S. M. and M. C.) debriefed immediately after each interview to share their observations and facilitate the recording of essential details; transcribed each interview verbatim; made notes while reading; identified key sentences and words to freely generate emergent themes; grouped, organized and abstracted themes; discussed data saturation considered the achievement of replication in themes. Two researchers (A. D. B. and E. L.) independently read the transcripts and defined codes and themes. The inductive content analysis was conducted with NVivo V.10.1.1 software (QSR International, Melbourne, Victoria, Australia). Finally, the team of four researchers discussed themes and sub‐themes to define them more clearly and reach a consensus. Three senior participants checked the agreed version of themes and sub‐themes, and their views were incorporated into the final version (Table 3).
TABLE 3.
Results of the content analysis: Emergent themes and sub‐themes from semi‐structured interviews
| Theme | Sub‐theme | Verbatim quotation |
|---|---|---|
| Organizational change | Nursing routinary task | ‘Measuring MDW values does not add new activities because the blood sample can be taken from the patient as a part of a standard blood test. [..] A standard blood test is a routinary task both for confirmed and suspected sepsis (…)’ [nurse, san Donato Hospital] |
| Trust in technological innovation | ‘Arriving at a trusted version of an AI/ML algorithm assessing sepsis' patient risk stratification and scores will be a long process requiring interprofessional skills integration. I, personally, trust technological innovation and think it can be a valuable help in my daily work.’ [nurse manager, san Donato Hospital] | |
| New professional role | ‘It is necessary to demonstrate, in some ways, that relying on an automatic algorithm for (sepsis) detection stratification does not lead us to an additional overload increase (…). We are working understaffed. What about thinking about new professional roles, such as ‘specialized IT nurses’ according to the UK model, for instance?’ [clinical manager, san Donato Hospital] | |
| Infrastructure | ‘(…) every day, we face the limitations of the hospital's technological infrastructure, which is limited by bandwidth, obsolete, and slow. (…) moreover, to date, we have no form of information and database integration, even between different departments of the same hospital. I do not see AI/ML as a priority now. We must invest in redesigning current infrastructure and realizing data integration as starting points and see facts before talking and think big.’ [nurse manager, other hospitals in Tuscany] | |
| COVID‐19's pressure | ‘The wakes of COVID‐19 pandemic have fostered the use of both [the combined technology] in the wards of ordinary hospitalization (emergency department, geriatrics, infectious disease, gynaecology, post‐surgical department). In this sense, the health care emergency has legitimized this innovative approach among doctors, becoming a routinary tool faster than ever. We (nurses) have benefited from its standardization’. [nurse, san Donato Hospital] | |
| Laboratory workload | ‘To avoid an increased workload for lab technicians, the company should win the tender to become routine technology in CBC test reporting.’ [laboratory technicians, san Donato Hospital] | |
| Innovation uptake | ‘The ML tool can surely bring us benefits in the medium‐long term. However, in the short term, we [nurses] see an increase in our daily work due to the manual entry of several parameters; the need for training; the potential need for IT support; the need to interface with physicians and other colleagues to be sure to interpret scores' algorithm correctly’. [nurse, san Donato Hospital] | |
| Centralization of treatment | We need to centralize sepsis diagnosis in hospital practice to guarantee a high standard of equity and care and reduce unwarranted variabilities across hospitals through new technologies and highly skilled professionals. [clinical manager, san Donato Hospital] | |
| Human factors | Decision‐making tool | ‘There may also be a kind of a tendency to rely more on the diagnostic algorithm result than on professionals' competencies and experiences.’ [physician, san Donato Hospital] |
| Future development | ‘We need to bring this technology to the patient's bedside and make it portable to speed up MDW detection. Sepsis evolves quickly, so we do not have much time, and sending samples to the lab wastes valuable time.’ [clinical manager, san Donato Hospital] | |
| Usability and acceptance | The diagnostic machinery is very easy to use, set up and maintain, but the lack of a user interface is a not trivial limitation for our [laboratory technicians'] work. The absence of an automatic data transmission protocol and the difficulty in approaching the ML algorithm make the training phase quite challenging for us. [laboratory technician, san Donato Hospital] | |
| Emotional perceptions | Frustration and unsatisfaction | ‘It is very frustrating when patients arrive in the emergency room with no specific symptoms and their conditions worsen within a short period, putting their lives at risk. I feel helpless and many times wonder if I have done enough.’ [nurse, san Donato Hospital] |
| Support need | ‘We [nurses] need support in identifying sepsis because the numbers are incredibly significant and the current standard of care is insufficient to play this battle fairly. We feel left to ourselves.’ [nurse, san Donato Hospital] | |
| Learning plasticity | We're used to being flexible and dynamic in our work in the emergency department, so learning how to use new technology and a new protocol would not be a big deal.’ [nurse manager, san Donato Hospital] |
The desk analysis let the authors draft a preliminary version of the current sepsis' clinical pathway mapping at the target site. The process‐flow model was designed using the Business Process Mapping Notation, an engineering technique exploiting graphical symbols to represent the flow of actions in a business‐like logic. The initial version of the model was employed to facilitate interviews, and subsequent versions, including pathway redesign, were created using insights from interviews. The clinical pathway was mapped into three hospital units: (i) Emergency Department; (ii) internal or post‐operatory medicine (e.g., geriatrics, infectious diseases, gynaecology, and traumatology); and (iii) hospital laboratory medicine.
2.5. Rigour
The criteria of credibility, transferability, dependability, and confirmability ensure the trustworthiness of this qualitative study (Data S1) (Polit & Tatano Beck, 2020).
2.6. Ethical considerations
The study was approved by the Ethical Committee for Clinical Experimentation of the Tuscany Region South‐Est on the 20th of May 2019 (Approval Number 14911). It was conducted following the principles of the Declaration of Helsinki (‘World Medical Association Declaration of Helsinki,’ 2013). The engagement of nurses and other professionals was based on voluntary participation, and informed consent was presented before the interview. Transcriptions were stored in a server protected by a password and accessible only to the team members. An alphanumeric code was given to each participant to guarantee confidentiality.
3. RESULTS
3.1. Clinical pathway mapping
The current clinical pathway (Data S2) was redesigned, considering changes to tasks and responsibilities, highlighted in red, that the introduction of the new integrated approach required (Figures 1 and 2).
FIGURE 1.
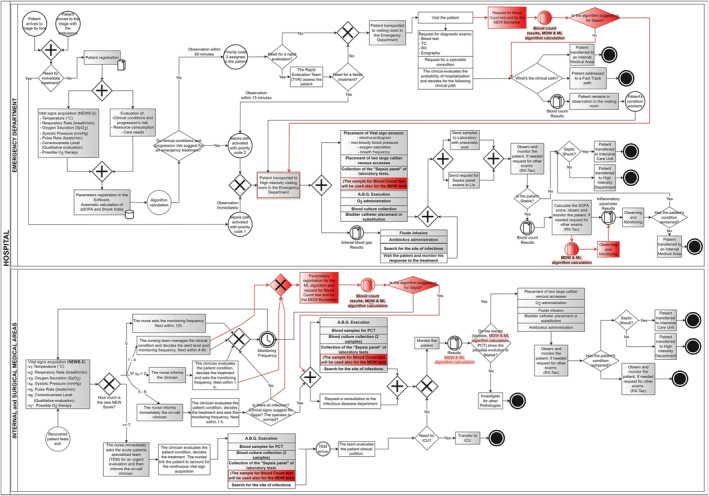
Process flow of emergency department and internal and surgical departments. In grey, the activities and tasks performed by nurses; in red, the activities introduced by the new technology combined (MDW analyser and ML algorithm).
FIGURE 2.
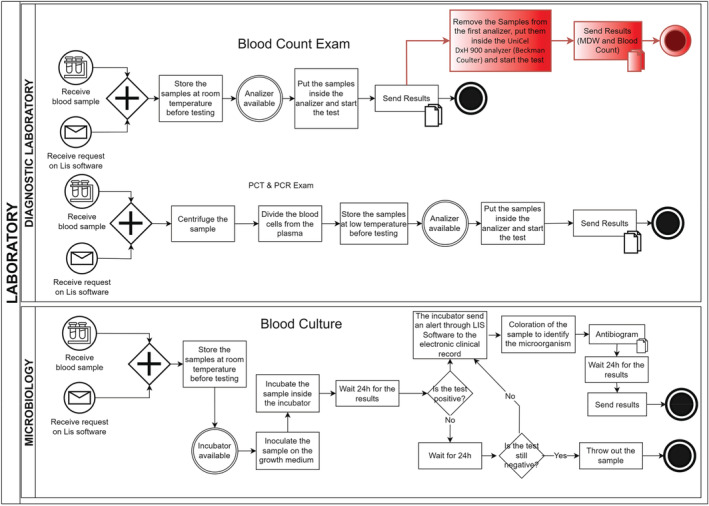
Process flow of hospital laboratory medicine. In grey, the activities and tasks performed by nurses; in red, the activities introduced by the new technology combined (MDW analyser and ML algorithm).
Combining the novel biomarker test into a novel predictive machine‐learning‐based algorithm mainly changed the identification process. The new biomarker test was performed at the end of the observation task, between the vital sign acquisition and the investigation for inflammatory markers. Given the optimal diagnostic accuracy for sepsis prediction, the biomarker test allowed to quickly target a patient as suspected sepsis. At this point, a prototype version of the smart predictive tool incorporated the biomarker values along with other vital signs. The machine‐learning algorithm outcomes were interpreted and combined with clinical judgements by physicians—in the first instance—and subsequently by nurses when a sort of standardization was reached. Changes to the process‐flow diagram involved only the case of patients characterized by non‐specific and non‐severe symptomatology, that is, ‘patients with suspected sepsis but unconfirmed infection’ according to the definition of the sepsis' international guidelines (Evans et al., 2021), as the integrated approach can improve only the identification phase (supplementary material S3).
3.2. Drivers to the adoption
We identified three main emergent themes in the semi‐structured interviews: (1) organizational change, (2) human factors, and (3) emotional perceptions. Each theme contains several sub‐themes (Table 3).
3.2.1. Organizational change
Nurses were identified as the primary professional category affected by the organizational change induced by the novel integrated approach and those who mainly required a speeding‐up of a new hospital organizational configuration. In terms of workload, nurses felt the novel biomarker test was a suitable tool that did not involve additional activities since it was included in the routine task of a standard blood count test planned in the current clinical pathway. On the other hand, nurses were worried about the workload increase due to the introduction and use of the predictive algorithm and the training needs for practical use and interpretation of the new instrument. The manual entry of several medical measurements (e.g., vital parameters, clinical observations, family, and medical histories) along with the biomarker value through a PC interface; the need for training to interpret algorithm results; the potential need for technical support during the use of the tool in case of malfunctions were perceived as additional tasks to their consolidated activities and work routines. Moreover, nurses agreed with the proposal of physicians to introduce the new technology in the middle of the identification phase, conditioning its use on clinical judgement and qualitative observation, as it was targeted at patient groups more vulnerable to the current approach, that is, defined as ‘patients with suspected sepsis but unconfirmed infection’ by Evans et al. (2021). The number of the biomarker tests in the hospital can impact the speed and timing of diagnosis, that is, the availability of a single diagnostic tool to be shared between multiple departments could slow down the whole process in the identification phase. Hence, the suitability to define specific and shared procedures for managing and using the available biomarker tests was highlighted during nurses' interviews.
3.2.2. Human factors
Nurses highlighted the rapidity of the test biomarker execution and the algorithm time processing, and the need to refine the development of the smart prototype (e.g., PC interface). As further development orientation, nurses stressed the opportunity to avoid the step of manual entry of data by co‐designing a next‐generation tool that automatically incorporated data from different hospital sources, such as electronic health records and monitoring devices acquiring vital signs. Moreover, a future development was perceived as implementing the biomarker to make it portable.
The resource use was highly dependent on the context where the analysis was conducted. The sepsis analyser resulted efficient in hospitals with a large team of trained health care professionals and laboratory technicians that can immediately perform the test. Although it remains a tool that can provide a great information source concerning early diagnosis, the results provided by the new integrated approach, on the other hand, can lead to a bias for health professionals who could rely all the decision‐making on the algorithm outcome, forgetting the importance of clinical judgement integration, which remains fundamental.
3.2.3. Emotional perceptions
The adoption of the novel integrated approach significantly influenced nurses' routine work. Nurses agreed that a new biomarker parameter with a good predictive power, which can potentially be incorporated into the predictive algorithm along with other vital‐sign data, could better support the decision‐making process and speed up the patient treatment through the early administration of antibiotics. The increase of the biomarker value was perceived as key to helping physicians and, consequently, nurses in early diagnosis and prospective evaluations even before the symptoms of sepsis are fully clear, particularly in the case of ‘patients with non‐specific and non‐severe symptomatology’ (Evans et al., 2021). The set of actions to perform the new biomarker test was maintained the same; however, there was an increasing trend of requests to perform standard blood count tests to assess the biomarker values for a suspected sepsis patient. This slight change in the process, which mainly affected laboratory technicians (Data S4), meant a significant improvement in professional satisfaction in the long term. Despite the workload increase due to data insert and interpretation of the machine‐learning‐based algorithm, nurses sought to promote adoption, which in a long time could lead to an improvement in their satisfaction and comfort/mental wellbeing.
4. DISCUSSION
This study aimed to redesign the current sepsis' clinical pathway after introducing a novel combined approach for early diagnosis. Furthermore, we investigated human and emotional drivers of adopting a novel machine‐learning algorithm that is predictive of sepsis and incorporates Monocyte Distribution Width, a novel biomarker recently validated in hospital practice. The study benefited from the observational clinical study started in June 2019 at San Donato Hospital (Arezzo, Italy) and is still ongoing. In this sense, our study shed new light on multidimensional factors that may positively or negatively influence the adoption process and the specific needs of the complex interprofessional hospital ecosystem.
The emergent themes highlighted concern in particular aspects of organizational change, human factors, and nurses' emotional perceptions.
Regarding organizational change, the inclusion of the biomarker test in clinical practice does not seem to modify nursing routinary tasks, as the blood sample can be taken from the patient as part of a standard count blood test, which is a usual activity both for confirmed and suspected sepsis. Moreover, nurses expressed confidence that the machine‐learning tool will benefit them in the medium to long term and the awareness of the need for interprofessional skills integration. However, in the short time, they perceived an increase in their daily work related to the machine‐learning component due to manual entry of different parameters, the need for training, the potential need for technical support, and the need to interface with physicians and other colleagues to be sure they are interpreting the algorithm score correctly. At the same time, some nurses perceived the priority of investment in infrastructure and specific projects to realize data integration rather than in machine‐learning development. Some of them support the idea of defining a new role for nurses dedicated to Information Technology (Zadvinskis et al., 2018).
Laboratory technicians perceived an increase in their workload activity for the need to retest the blood sample. This aspect did not represent a constraint in other hospital settings, where the biomarker analyser is the primary machine to perform standard blood count tests.
Physicians were very interested in technology adoption both in terms of work simplification, thanks to the introduction of a new tool to reduce discretion, and better patient care, especially compared with the increased tendency to incur legal issues. At the same time, consistent with recent literature, an important theme emerging by physicians was the need to centralize sepsis diagnosis in hospital practice to guarantee a high standard of equity and quality of care and reduce unwarranted variabilities across hospitals through the use of new technologies and highly skilled professionals (Evans et al., 2021). Physicians used the new combined technology during the COVID‐19 pandemic to identify sepsis early in hospitalized patients. This facilitated the subsequent widespread use of this technology by Emergency Department nurses (Ognibene et al., 2020).
The need for organizational change was considered one of the most critical barriers that could be mitigated by reconfiguring the service and the professionals involved to create the conditions to exploit all the advantages of the new technology. For example, one of the solutions proposed by the stakeholders, useful to optimize the time related to the execution of the test and the tracking of the instrument, was to provide the availability of a portable diagnostic device at the bedside of the patient, which would allow accurate identification of the pathology in a short time and a substantial reduction in the time to antibiotics.
The other two main emergent themes are human factors and nurses' emotional perceptions. In particular, some nursing staff interviewed reported the risk of relying more on the algorithm results than on professionals' competencies and experiences. Indeed, the diffusion of machine‐learning systems in clinical and nursing practice leads to questioning of new ethical and legal issues. Physicians and nurses are the principal responsible for patient care outcomes; if technology is necessary and helpful support, it does not replace professionals' skills and judgement. Systems and technologies that assist in clinical practice are added to, not replacements for, the health care professionals' knowledge and skills (Evans et al., 2021; Fowler, 2015). One of the critical concerns of artificial intelligence practitioners today is managing bias. Every health care professional who uses new technologies or helps build them has a responsibility to ask about the data used to train the system and how the system results are checked for bias (Robert, 2019). Another bias to consider is the transparency of the algorithm. Adopting a new artificial intelligence system requires that operators understand how the machine‐learning processes the results. Health care professionals need to understand and trust the artificial intelligence's recommendations and how the computer makes its decision. For this reason, an important question to ask the management when implementing new technologies is how the results will be monitored to judge the accuracy of recommended decisions. New ethical stances help artificial intelligence teams solve bias issues by making specific statements about the fairness, accountability, and transparency of data used in building machine‐learning systems (Robert, 2019).
A series of final recommendations by exploiting the study results were drawn for the Italian national health system and public institutions to facilitate the adoption of the novel combined technology in hospital practice.
Firstly, while current regional and national guidelines tried to reduce inter‐hospital variation in sepsis treatment, at the same time, they over‐generalized the complexity around sepsis without ad‐hoc treatment procedures. For this reason, the novel combined approach may become a driver for a more automatized, personalized, and patient‐centred way of organizing sepsis management and treatment, where the new biomarker test would be a key parameter for defining and stratifying patient risk. The novel combined technology could help identify unestablished signs or symptoms that can reliably predict sepsis by combining the biomarker values with other clinical parameters collected from different sources into a trusted machine‐learning algorithm (Islam et al., 2019).
Secondly, the management of change following the introduction of the novel approach in clinical practice should support doctors and nurses through different strategies, including training programs, the availability of expert professionals during the implementation of the diagnostic algorithm and the possibility of reporting critical issues for improvement relating to clinical, organizational, ethical, and legal aspects, during and after the adoption phase.
Thirdly, the new combined technology adoption is related to the proper dissemination to the public and society, including public awareness campaigns. Commissioners and policymakers need to be aware of the complexity of sepsis management and the scaling‐up to promote a redesign of the whole system and overcome other potential barriers, such as privacy and security issues and technical problems, such as data formatting and network architecture. Finally, strong collaboration and cooperation between all actors involved in the adoption process are vital in achieving prospective diagnosis and early treatment.
5. LIMITATIONS
This study presents several limitations to be considered, mainly related to the exploited qualitative methodology. The sample of respondents was not randomized but based on a convenience sample and collected on a voluntary basis, incurring the risk of introducing a recruitment bias. A snowball technique was used for enlisting respondents. It may have generated a positivist trend, as the most prone stakeholders to change and innovation may be the most interested in being recruited.
6. CONCLUSIONS
This study investigated multifactorial drivers of different professional groups that are crucial to facilitating technology adoption in hospital practice. Studies that combine clinical pathway mapping and qualitative analysis can be a great tool to support disruptive technology innovation. The novel business‐oriented solution, based on machine‐learning for sepsis early detection, requires interprofessional integration, new professional roles, infrastructure improvement, data integration, and new ethical/legal rules to guarantee transparency to be effectively implemented. Lessons learned from this study suggest the need to involve nurses in the early stages of the design of new machine‐learning technologies and the importance of training nurses on sepsis management through the support of disruptive technological innovation.
7. IMPLICATIONS FOR NURSING MANAGEMENT
The insights of the study may be relevant for nursing and hospital management.
Firstly, predicting sepsis using machine learning could significantly improve patient safety, quality of care, and clinical performance indicators, guiding nurses and physicians to actively monitor and take preventive actions to improve the patients' condition. The adoption of the combined technology for early detection of sepsis may save health care resources and increase the desired sensitivity or specificity, resulting in a decreased number of false alarms and with a positive impact on all the dimensions of quality improvement, that is, appropriateness, effectiveness, efficiency, accessibility, timeliness and safety (Islam et al., 2019; Wu et al., 2021),
Secondly, the use of machine learning in the daily practice of nurses enhances their role in the early identification of sepsis and provides visibility and professional satisfaction, preventing health professionals' unhappiness, frustration and anxiety (Gonçalves et al., 2020).
Thirdly, nurse managers are called upon to encourage continuous training for their staff about sepsis management and implementing a standardized protocol, bundle, and guidelines into clinical practice (Kleinpell, 2017).
Finally, key factors that positively influence the adoption of new machine‐learning tools are represented by peer influence and stakeholder involvement from the early stages. The user experience helps ensure convergence between the needs of health care professionals, also related to the organizational context, and the possibilities offered by the new technologies, thus promoting their adoption in professional practice. The involvement of nurses and other health care professionals in the early development stages of a new machine‐learning system design allows the sharing of scientific knowledge, theoretical skills and experiences that guide the development of the new project in a patient‐centred way.
Nurses are increasingly called upon to participate in such ethical assessments concerning artificial intelligence projects applied to clinical practice to ensure the best possible care for each patient. Nursing experience, knowledge, and skills increasingly require learning new ways of thinking about information processing. If artificial intelligence technologies can increasingly support nurses, they will never be replaced by them (OMS, 2019).
CONFLICTS OF INTEREST
The authors declare no competing interests.
ETHICS STATEMENT
The study was approved by the Ethical Committee for Clinical Experimentation of the Tuscany Region South‐Est on the 20th of May 2019 (Approval Number 14911). It was conducted following the principles of the Declaration of Helsinki. The engagement of nurses and other professionals was based on voluntary participation, and informed consent was presented before the interview. Transcriptions were stored in a server protected by a password and accessible only to the team members. An alphanumeric code was given to each participant to guarantee confidentiality.
Supporting information
Data S1. Supporting Information
ACKNOWLEDGMENTS
The authors would like to thank all the anonymous study participants. Open Access Funding provided by Scuola Superiore Sant'Anna within the CRUI‐CARE Agreement. [Correction added on 28 November 2022, after first online publication: CRUI‐CARE funding statement has been added.]
Manetti, S. , Cumetti, M. , De Benedictis, A. , & Lettieri, E. (2022). Adoption of novel biomarker test parameters with machine learning‐based algorithms for the early detection of sepsis in hospital practice. Journal of Nursing Management, 30(8), 3754–3764. 10.1111/jonm.13807
Funding information This study was coordinated by Sant'Anna School of Advanced Studies and funded by Beckman Coulter Foundation. The views expressed are those of the authors and not necessarily those of Beckman Coulter Srl.
[Correction added on 15 December 2022, after first online publication: The third author's surname has been corrected from ‘Benedectis’ to ‘Benedictis’ in this version.]
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions.
REFERENCES
- Agnello, L. , Bivona, G. , Vidali, M. , Scazzone, C. , Giglio, R. V. , Iacolino, G. , Iacona, A. , Mancuso, S. , Ciaccio, A. M. , Lo Sasso, B. , & Ciaccio, M. (2020). Monocyte distribution width (MDW) as a screening tool for sepsis in the emergency department. Clinical Chemistry and Laboratory Medicine (CCLM), 58(11), 1951–1957. 10.1515/cclm-2020-0417 [DOI] [PubMed] [Google Scholar]
- Angus, D. C. , & Bindman, A. B. (2022). Achieving diagnostic excellence for Sepsis. JAMA, 327(2), 117–118. 10.1001/jama.2021.23916 [DOI] [PubMed] [Google Scholar]
- Calci, C. M. , Causin, F. , Bertini, E. A. , Fabbri, A. , Brambilla, A. M. , Pontoni, E. , Causin, F. , Pagnozzi, F. , Innocenti, F. , Aprà, F. , Ruggiano, G. , Giannazzo, G. , Di Paco, I. , Calci, M. , Zanobetti, M. , Camaiori, R. , Pini, R. , Sbrojavacca, R. , Russo, S. , & … For, R . (2018). La Gestione Della Sepsi Nell’ Adulto in Pronto Soccorso E Medicina D' Urgenza in Italia. Critical Care Medicine, 46(11), 1–2.28863012 [Google Scholar]
- Evans, L. , Rhodes, A. , Alhazzani, W. , Antonelli, M. , Coopersmith, C. M. , French, C. , Machado, F. R. , Mcintyre, L. , Ostermann, M. , Prescott, H. C. , Schorr, C. , Simpson, S. , Wiersinga, W. J. , Alshamsi, F. , Angus, D. C. , Arabi, Y. , Azevedo, L. , Beale, R. , Beilman, G. , … Levy, M. (2021). Surviving sepsis campaign: International guidelines for management of sepsis and septic shock 2021. Intensive Care Medicine, 47(11), 1181–1247. 10.1007/s00134-021-06506-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fowler, M. (2015). The guide to the code of ethics for nurses with interpretive statements: Development, interpretation, and application (edition, 2 ed.). A. N. Association [ed.]. [Google Scholar]
- Gonçalves, L. S. , Amaro, M. L. M. , Romero, A. L. M. , Schamne, F. K. , Fressatto, J. L. , & Bezerra, C. W. (2020). Implementation of an artificial intelligence algorithm for sepsis detection. Revista Brasileira de Enfermagem, 73(3), e20180421. 10.1590/0034-7167-2018-0421 [DOI] [PubMed] [Google Scholar]
- Islam, M. M. , Nasrin, T. , Walther, B. A. , Wu, C.‐C. , Yang, H.‐C. , & Li, Y.‐C. (2019). Prediction of sepsis patients using machine learning approach: A meta‐analysis. Computer Methods and Programs in Biomedicine, 170, 1–9. 10.1016/j.cmpb.2018.12.027 [DOI] [PubMed] [Google Scholar]
- Kleinpell, R. (2017). Promoting early identification of sepsis in hospitalized patients with nurse‐led protocols. Critical Care, 21(1), 10. 10.1186/s13054-016-1590-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manetti, S. , Burns, R. M. , & Turchetti, G. (2017). Evidence‐gathering across industry and academia on early Health Technology Assessment (HTA) of medical devices: survey design and piloting. In EMBEC & NBC 2017 (pp. 631–634). Springer, Singapore. [Google Scholar]
- Manetti, S. , Vainieri, M. , Guidotti, E. , Zuccarino, S. , Ferré, F. , Morelli, M. S. , & Emdin, M. (2020). Research protocol for the validation of a new portable technology for real‐time continuous monitoring of early warning score (EWS) in hospital practice and for an early‐stage multistakeholder assessment. BMJ Open, 10(12), 1–7. 10.1136/bmjopen-2020-040738 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morse, J. M. , & Field, P. A. (1995). Qualitative research Methods for health professionals. SAGE Publications, Inc. [Google Scholar]
- Naderifar, M. , Goli, H. , & Ghaljaie, F. (2017). Snowball sampling: A purposeful method of sampling in qualitative research. Strides in development of Medical Education, 14(3). 10.5812/sdme.67670 [DOI] [Google Scholar]
- Ognibene, A. , Lorubbio, M. , Magliocca, P. , Tripodo, E. , Vaggelli, G. , Iannelli, G. , Feri, M. , Scala, R. , Tartaglia, A. P. , Galano, A. , Pancrazzi, A. , & Tacconi, D. (2020). Elevated monocyte distribution width in COVID‐19 patients: The contribution of the novel sepsis indicator. Clinica Chimica Acta, 509, 22–24. 10.1016/j.cca.2020.06.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- OMS . (2019). Towards the development of guidance on ethics and governance of artificial intelligence for health (issue October).
- Piva, E. , Zuin, J. , Pelloso, M. , Tosato, F. , Fogar, P. , & Plebani, M. (2021). Monocyte distribution width (MDW) parameter as a sepsis indicator in intensive care units. Clinical Chemistry and Laboratory Medicine (CCLM), 59(7), 1307–1314. 10.1515/cclm-2021-0192 [DOI] [PubMed] [Google Scholar]
- Polit, D. F. , & Tatano Beck, C. (2020). Nursing research: Generating and assessing evidence for nursing practice. Wolters Kluwer. [Google Scholar]
- Rhodes, A. , Evans, L. E. , Alhazzani, W. , Levy, M. M. , Antonelli, M. , Ferrer, R. , Kumar, A. , Sevransky, J. E. , Sprung, C. L. , Nunnally, M. E. , Rochwerg, B. , Rubenfeld, G. D. , Angus, D. C. , Annane, D. , Beale, R. J. , Bellinghan, G. J. , Bernard, G. R. , Chiche, J.‐D. , Coopersmith, C. , … Dellinger, R. P. (2017). Surviving Sepsis campaign: International guidelines for Management of Sepsis and Septic Shock: 2016. Intensive Care Medicine, 43(3), 304–377. 10.1007/s00134-017-4683-6 [DOI] [PubMed] [Google Scholar]
- Robert, N. (2019). How artificial intelligence is changing nursing. Nursing Management, 50(9), 30–39. 10.1097/01.NUMA.0000578988.56622.21 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rudd, K. E. , Johnson, S. C. , Agesa, K. M. , Shackelford, K. A. , Tsoi, D. , Kievlan, D. R. , Colombara, D. V. , Ikuta, K. S. , Kissoon, N. , Finfer, S. , Fleischmann‐Struzek, C. , Machado, F. R. , Reinhart, K. K. , Rowan, K. , Seymour, C. W. , Watson, R. S. , West, T. E. , Marinho, F. , Hay, S. I. , … Naghavi, M. (2020). Global, regional, and national sepsis incidence and mortality, 1990–2017: Analysis for the global burden of disease study. The Lancet, 395(10219), 200–211. 10.1016/S0140-6736(19)32989-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singer, M. , Deutschman, C. S. , Seymour, C. W. , Shankar‐Hari, M. , Annane, D. , Bauer, M. , Bellomo, R. , Bernard, G. R. , Chiche, J.‐D. , Coopersmith, C. M. , Hotchkiss, R. S. , Levy, M. M. , Marshall, J. C. , Martin, G. S. , Opal, S. M. , Rubenfeld, G. D. , van der Poll, T. , Vincent, J.‐L. , & Angus, D. C. (2016). The third international consensus definitions for Sepsis and septic shock (Sepsis‐3). JAMA, 315(8), 801–810. 10.1001/jama.2016.0287 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tong, A. , Sainsbury, P. , & Craig, J. (2007). Consolidated criteria for reporting qualitative research (COREQ): A 32‐item checklist for interviews and focus groups. International Journal for Quality in Health Care, 19(6), 349–357. 10.1093/intqhc/mzm042 [DOI] [PubMed] [Google Scholar]
- Toscana, R. (2019). Lotta alla sepsi. Documento di indirizzo.
- Vaismoradi, M. , Turunen, H. , & Bondas, T. (2013). Content analysis and thematic analysis: Implications for conducting a qualitative descriptive study. Nursing and Health Sciences, 15(3), 398–405. 10.1111/nhs.12048 [DOI] [PubMed] [Google Scholar]
- World Medical Association Declaration of Helsinki . (2013). 64thWMAGeneral Assembly, Fortaleza Brazil, October 2013. World Medical Association Declaration of Helsinki Ethical Principles for Medical Research Involving Human Subjects. JAMA, 310(20), 2191. 10.1001/jama.2013.281053 [DOI] [PubMed] [Google Scholar]
- Wu, M. , Du, X. , Gu, R. , & Wei, J. (2021). Artificial intelligence for clinical decision support in Sepsis. Frontiers in Medicine, 8, 665464. 10.3389/fmed.2021.665464 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zadvinskis, I. M. , Garvey Smith, J. , & Yen, P.‐Y. (2018). Nurses' experience with health information technology: Longitudinal qualitative study. JMIR Medical Informatics, 6(2), e38. 10.2196/medinform.8734 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhou, F. , Yu, T. , Du, R. , Fan, G. , Liu, Y. , Liu, Z. , Xiang, J. , Wang, Y. , Song, B. , Gu, X. , Guan, L. , Wei, Y. , Li, H. , Wu, X. , Xu, J. , Tu, S. , Zhang, Y. , Chen, H. , & Cao, B. (2020). Clinical course and risk factors for mortality of adult inpatients with COVID‐19 in Wuhan, China: A retrospective cohort study. The Lancet, 395(10229), 1054–1062. 10.1016/S0140-6736(20)30566-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data S1. Supporting Information
Data Availability Statement
The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions.


