Abstract
Aim
To investigate the effectiveness of preventive interventions for 8–17‐year‐old children of patients diagnosed with depression, anxiety, or bipolar disorder.
Methods
Sixty‐two families including 89 children received either the more extensive Family Talk Intervention (FTI; n = 35), the brief Let's Talk about Children (LTC; n = 16), or Interventions as Usual (IAU; n = 38) in routine care in adult psychiatry. Parent‐rated questionnaire data were collected at baseline, after 6 and 12 months. We used growth curve models to investigate the effect of intervention on child mental health problems (SDQ‐P Total Difficulties) and perceived parental control of child behaviour (PLOC‐PPC).
Results
Parents in the FTI and LTC groups, versus the IAU group, reported more favourable development in terms of preventing increase in child mental health problems with standardised intervention effects of d = −0.86 and −0.88 respectively, by study end, and reported improved perceived parental control, d = 1.08 and 0.71, respectively, by study end. No significant differences in effect were found when FTI and LTC were compared.
Conclusions
The results support continued use of FTI and LTC in adult psychiatry, and since LTC is a brief intervention, it might be useful as a minimum‐level preventive intervention.
Keywords: children of parents with a mental illness, effectiveness trial, preventive interventions, psychiatry
Abbreviations
- FTI
Family Talk Intervention
- IAU
Interventions as Usual
- LTC
Let's Talk about Children
Key Notes.
The effectiveness of preventive interventions used in adult psychiatry was investigated.
Parents receiving FTI and LTC, compare to IAU, reported more favourable development, and no significant differences were found between FTI and LTC.
The results support continued use of FTI and LTC in adult psychiatry for children of parents with depression, anxiety, and bipolar disorder and the brief LTC intervention might be useful as a minimum‐level preventive intervention.
1. INTRODUCTION
Children of parents with a mental illness have an increased risk of developing mental health problems 1 and of experiencing other adverse life outcomes. 2 Several preventive interventions have therefore been developed for this group of children to promote healthy child development and reduce the risks associated with growing up with a parent with mental illness. 2 The overall effects of such interventions have been explored meta‐analytically, and the results indicate a small but significant intervention effect in terms of reduced internalising symptoms 3 , 4 , 5 , 6 and decreased incidence of mental disorders. 3 , 5 , 6 Results are mixed concerning the effect of interventions on externalising symptoms. 3 , 4 , 6 The developed interventions vary in their approach, components, delivery format, intensity, age range of target children, and family members involved. 3 Investigating possible differences between interventions and extending results to more naturalistic conditions calls for replication trials and studies conducted in various treatment settings and cultural contexts. 3
In Sweden, mental health professionals have a juridical obligation to give needed information, advice, and support to children in families experiencing parental mental illness. 7 In specialised adult psychiatry, various interventions are used in routine care including both interventions specifically developed for children of parents with mental illness and interventions without using a specific manual, 8 however only a smaller part of all patients who are registered as parents in this clinical setting receive interventions focusing on their children. 9
Two of the more widely used manual‐based preventive interventions in specialised adult psychiatry in Sweden are Family Talk Intervention (FTI) 10 and Let's Talk about Children (LTC). 11 , 12 FTI was developed in the United States for children of parents with affective disorders and has been adapted to Nordic conditions 12 and has been found safe and feasible in a Swedish psychiatric context. 13 LTC was developed in Finland, informed by FTI among other methods. 11 The two interventions share many components including psychoeducation, family communication, discussions of child risk and resilience, need for treatment or other support 14 and components to strengthen parenting skills and parenting beliefs. 15 The interventions differ, however, in intensity and in the family members involved, with FTI being more extensive and including the whole family instead of only parents. Furthermore, opening up family communication to gain a shared understanding of parental mental illness is emphasised in FTI and the perspective of every family member is respected, 16 while LTC has a more practical approach in supporting parents and emphasises issues in the child's everyday life. 16 When FTI and LTC have been compared in randomised controlled trials, results have shown that both interventions significantly reduce child mental health problems 12 , 16 and also has the potential to improve family functioning and parenting. 16
The aim of this study was to investigate the effectiveness of FTI and LTC compared with other available interventions in routine care, which will be referred to as Interventions as Usual (IAU). In previous studies comparing FTI and LTC, a comparison group has not been included. In our study, the effectiveness of the interventions was investigated with a focus on change in child mental health problems, as these interventions aim to reduce the risk of developing mental health problems and on change in perceived parental control of child behaviour over time. Perceived parental control is a concept close to parent self‐efficacy beliefs, 17 higher levels of which have been associated with more effective parenting styles and lower levels with both parent and child mental health problems. 18 FTI was originally developed for 8–15‐year‐old children of parents with affective disorders, 10 and the parental diagnoses in focus here were depression, anxiety, and bipolar disorder. The age range of the children was extended to 8–17‐year‐old.
We hypothesised that receiving either FTI or LTC would be associated with better development of both (a) parent‐rated child mental health problems and (b) perceived parental control, relative to IAU. Furthermore, we wanted to explore (c) whether there was a difference in outcome measures between FTI and LTC.
2. METHOD
2.1. Design
The present effectiveness study uses a quasi‐experimental longitudinal design 19 comparing two manual‐based preventive interventions (i.e., FTI and LTC) with other interventions (IAU) used in psychiatric routine care. Non‐random assignment was applied, as families received the intervention available at the psychiatry unit the patient was attending. The study was approved by the Regional Ethics Committee in Gothenburg (Reg. no. 1029‐13).
2.2. Participants
The participants were recruited from patients diagnosed with depression, anxiety, or bipolar disorder, and their partners, if any, who were about to receive an intervention focusing on their children aged 8–17 years as part of the patient's ongoing treatment. Participants should be able to complete a questionnaire independently in Swedish to participate. Exclusion criteria were the following: the family had received a preventive intervention in the previous 12 months; the patient had a main diagnosis of substance use or schizophrenia; or the family was experiencing a severe crisis, such as divorce, violence, or family member death. Reports were not collected for children who were in treatment for depression or anxiety disorder or who were living in out‐of‐home care.
Sociodemographic characteristics of the children and patients are presented in Table 1. The allocation of families in the study groups is shown in Figure 1. Comparison between groups at baseline revealed no significant differences in sociodemographic characteristics.
TABLE 1.
Sociodemographic characteristics of patients and children at baseline, stratified by study group
| Baseline characteristic | FTI | LTC | IAU | p | |||
|---|---|---|---|---|---|---|---|
| n | n | n | |||||
| Patients | |||||||
| Age, M (SD) a | 18 | 43.11 (8.49) | 12 | 39 (6.33) | 27 | 41.26 (7.10) | 0.337 |
| Gender, female (%) | 13 | 68 | 7 | 58 | 20 | 71 | 0.713 |
| Children in family, M (SD) a | 18 | 2.11 (0.96) | 12 | 2.08 (1.00) | 28 | 2.04 (0.79) | 0.960 |
| Civil status (%) | |||||||
| Single | 5 | 28 | 6 | 54.5 | 5 | 18.5 | 0.085 |
| Married/in a relationship | 13 | 72 | 5 | 45.5 | 22 | 81.5 | |
| Social status (%) | |||||||
| Average–high, ≥30 | 11 | 58 | 3 | 25 | 9 | 32 | 0.125 |
| Low, <30 | 8 | 42 | 9 | 75 | 19 | 68 | |
| Reason for contact with psychiatry (%) | |||||||
| Depression/anxiety | 7 | 37 | 9 | 75 | 19 | 68 | 0.051 |
| Bipolar | 12 | 63 | 3 | 25 | 9 | 32 | |
| Children | |||||||
| Age, M (SD) a | 35 | 12.37 (2.70) | 15 | 11.47 (2.45) | 36 | 11.36 (2.96) | 0.277 |
| Gender, female (%) | 16 | 46 | 5 | 33 | 16 | 44 | 0.773 |
| Previous CAMHS contact (%) | |||||||
| Yes | 4 | 11 | 1 | 7 | 11 | 31 | 0.057 |
| No | 31 | 89 | 14 | 93 | 24 | 69 | |
| Living arrangement (%) | |||||||
| Both parents | 25 | 71 | 5 | 33 | 16 | 44 | 0.065 |
| Alternating b | 8 | 23 | 8 | 53 | 12 | 33 | |
| Mainly one parent | 2 | 6 | 2 | 13 | 6 | 17 | |
| Only one parent | 0 | 0 | 0 | 0 | 2 | 6 | |
| Custody (%) | |||||||
| Joint | 34 | 97 | 14 | 93 | 31 | 89 | 0.323 |
| Sole | 1 | 3 | 0 | 0 | 3 | 9 | |
| Other | 0 | 0 | 1 | 7 | 1 | 3 | |
Note: The sum of percentages is out by 1% due to rounding for LTC Living arrangement and IAU Custody.
Abbreviations: CAMHS, Child and Adolescent Mental Health Services; FTI, Family Talk Intervention; IAU, Interventions as Usual; LTC, Let's Talk about Children.
Mean and standard deviation are shown instead of percentage.
Living equal amounts of time alternating between separated parents.
FIGURE 1.
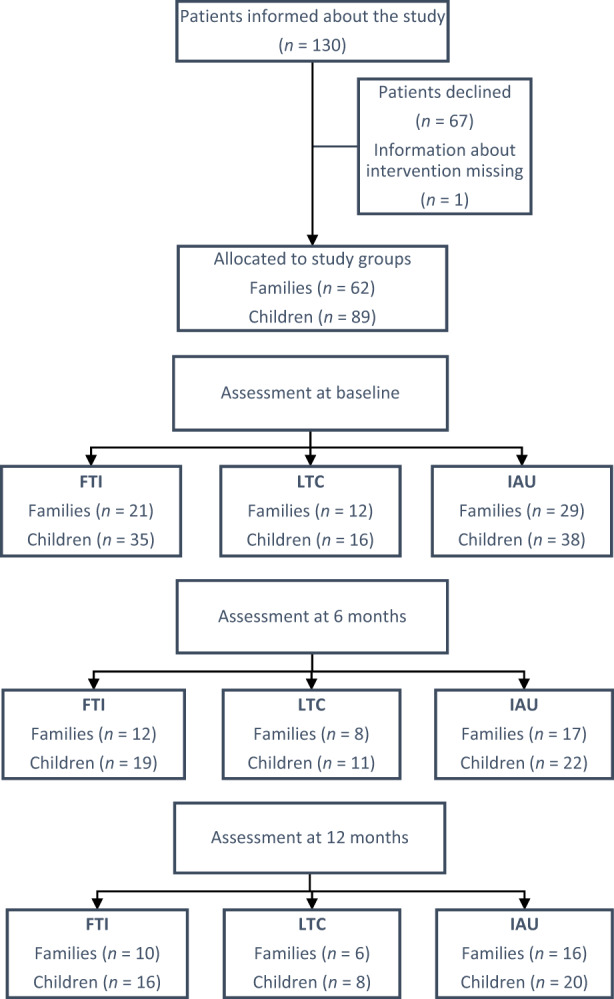
Flowchart of participants. FTI, Family Talk Intervention; IAU, Interventions as Usual; LTC, Let's Talk about Children.
2.3. Procedure
The study setting was 46 psychiatry units in five regions in Sweden. All mental health professionals who initiated preventive interventions during the recruitment period (i.e., September 2014–December 2017) could inform and recruit participants. First, the patient received verbal and written information about the study; if the patient agreed, the partner was informed and asked to participate. Consenting participants completed questionnaires individually and were asked to answer questions about each child aged 8–17 years. It was estimated to take about 30 min to complete the questionnaire, which could be done at the psychiatry unit or at home, either on paper or online. Parent‐rated questionnaire data were collected across three subsequent measurement waves, at the beginning of the intervention and 6 and 12 months after baseline.
During the recruitment period, 130 patients were informed about the study and 63 (48%), with 91 children, agreed to participate in the study. Intervention type was missing for one family, and so 62 families with 89 children (38 girls, 51 boys) were included in the analyses. Reports from one parent, referred to as the primary informant, were used in the analyses for each child. The patient was the primary informant for 80 children, and the partner was the primary informant for nine children in cases when patient rating data were missing or incomplete.
The intended sample size was 300 children, but despite having prolonged inclusion period several times the data collection had to be ended after the inclusion of 91 children.
2.4. Interventions
Family Talk Intervention 10 , 13 (FTI) consists of six to eight face‐to‐face sessions led by a trained professional, including meetings with parents and each child individually and with the whole family. Follow‐up meetings after one and 6 months are recommended. The intervention includes discussing how parental mental illness affects the family, informing children of the parent's mental illness, assessing risk and protective factors in the child's life, and supporting the parents. 10 A manual is followed, and a logbook is used to document meetings and the content covered. Parents receive a self‐help booklet. The manual has been translated and adapted to Swedish conditions. 20
Let's Talk about Children 11 (LTC) consists of one or two face‐to‐face sessions, led by a professional, with the patient or both parents. The discussions concern how parental mental illness affects the family, the child's strengths and vulnerabilities, and how parents can support healthy child development in the child's daily life. 11 LTC is manual based; a logbook used to document content covered, and parents receive the same self‐help booklet as in FTI. The manual has been translated and adapted to Swedish conditions (https://anhoriga.se/globalassets/media/dokument/metoder‐och‐vertyg/barn‐som‐anhorig/fora_barnen_pa_tal_manual‐loggbok.pdf).
Interventions as Usual (IAU) in this study consist of various other interventions available in routine care in Sweden to comply with the legal requirement to give needed information, advice, and support to children of parents with mental illness. 7 The interventions in this group include both interventions focusing on the children during the patient's regular treatment without following any specific manual and interventions specifically developed for children of parents with mental illness other than FTI and LTC. 8 The durations of the interventions in this group ranged from one to 19 meetings or part of meetings. The children participated directly in 35% of these interventions.
Across the three intervention groups, most of the professionals (77%) had over 10 years of work experience. All professionals giving FTI or LTC had formal training in the methods (except for one giving FTI, who collaborated with a trained colleague), and at least half had training in both methods. Half of the professionals responsible for IAU also had training in both FTI and LTC.
2.5. Measures
The mental health professionals reported basic demographic information and reason for contact with psychiatric care for all patients informed of the study. They also completed a questionnaire about each included intervention and answered questions about themselves concerning, age, gender, training, and professional background.
The baseline assessment for patients and partners included demographic questions about the participant (covering age, gender, civil status, number of children, occupation, profession, and education) and their children (covering age, gender, legal custody, residence arrangement, and contact with Child and Adolescent Mental Health Services). The Hollingshead Index of Social Status (range 8–66) 21 was calculated. The following measures were completed by participating parents in each wave:
The Total Difficulties score of the Strength and Difficulties Questionnaire – Parent Version (SDQ‐P) 22 , 23 measures parent‐rated child mental health problems. The measure includes 20 items covering emotional, behavioural, hyperactivity–inattention, and peer problems, responded to on a three‐point scale, with higher scores indicating more problems (range 0–40). The Swedish version of SDQ‐P has displayed adequate psychometric properties. 23 In our study, Cronbach's α at baseline was 0.79.
Perceived parental control of child behaviour was assessed using the subscale Perceived Parental Control (PLOC‐PPC) 17 from the Parental Locus of Control Questionnaire (PLOC). 24 The subscale consists of 10 personalised statements about the parent's experience of control in rearing situations in relation to the child, responded to on a five‐point scale, with higher scores indicating more perceived control. PLOC‐PPC has been found to be a psychometrically adequate measure of perceived control, arguably conceptually close to parental self‐efficacy beliefs. 17 Cronbach's α at baseline was 0.83.
The Clinical Outcomes in Routine Evaluation – Outcomes Measure (CORE‐OM) 25 was used to assess the level of parent distress during the past week. It is a 34‐item self‐report measure whose items are responded to on a five‐point scale, with higher scores indicating more distress. The Swedish version has displayed psychometric properties similar to those of the original English version, and has been found to be a valid measure of psychological symptoms. 26 In this study, the symptoms subscale (range 0–48) was used as a covariate to control for patient symptoms. Cronbach's α was 0.93 at baseline.
2.6. Data analysis
Baseline group differences were investigated using ANOVA for continuous variables and Pearson's chi‐square or Fisher's exact test for categorical variables. Participants completing the follow‐up questionnaires were compared with non‐completers concerning baseline data, using the independent‐sample t‐test and Pearson's chi‐square test.
The analytical approach for evaluating the preventive interventions was multilevel growth curve modelling, 27 which accounted for multiple measurements per child and for siblings nested in families (i.e., a three‐level nested data structure with time nested within children nested within families). The primary outcome measure was the SDQ‐P Total Difficulties score and the secondary outcome measure was the PLOC‐PPC score. The effect was evaluated by investigating the interaction between study group and time. In Model 1, time was included as a covariate (coded baseline = 0, 6 months = 1, and 12 months = 2) and the intervention group variable was defined as a dummy coded factor, with IAU as the reference group. To compare FTI with LTC, we refitted the models to have LTC as the reference. In Model 2, we controlled for the effects of child age and patient symptoms at baseline and of time‐varying patient symptoms during the study, which were all included as grand‐mean‐centred covariates. To complement the investigation of the interaction between study group and time, differences between groups at wave 3 was also investigated. As the sample was small, we used restricted maximum likelihood (REML) as the estimation method. Estimates (b) and standard errors (SE) are presented in unstandardised form. The primary effect sizes for the intervention effect was calculated by multiplying the group by time interactions by 2 and divided by the standard deviation of a population‐based reference group. 17 , 28 Secondary effect sizes were calculated by dividing the wave 3 mean group difference by the standard deviation of a population‐based reference group. 17 , 28 We note that baseline mean differences across groups are accounted for in the primary effect sizes, but not in the secondary. The standardised effect sizes were presented using Cohen's d. 29 The statistical significance level was set at p < 0.05.
We checked for outliers before conducting the multilevel growth curve modelling, excluding one child before the SDQ‐P analysis. Assumptions of normal residuals were found to be fulfilled. We handled missing data in the outcome variables using the maximum likelihood estimation procedure. To avoid reducing the sample size in Model 2, due to occasional missing data concerning the added covariates, we used multivariate imputation by chained equations as implemented in the MICE R package. 30 Data were analysed with IBM SPSS Statistics (version 28) and R Core Team (version 4.1.2).
3. RESULTS
3.1. Comparison between study groups
In total, 91 children were included in the study; however, at baseline parent reports were available for only 86 children (intervention missing, n = 2; parent reports missing, n = 3), and 60 patients completed the baseline measures about themselves. Child and patient characteristics and baseline results were compared, and no significant differences were found between the three study groups concerning demographic data (see Table 1) or in the results for outcome measures or covariates (see Table 2).
TABLE 2.
Means and standard deviations of raw scores for patient and child measures stratified by study group for each wave of data collection
| Variable | FTI | LTC | IAU | p | ||||
|---|---|---|---|---|---|---|---|---|
| n | M (SD) | n | M (SD) | n | M (SD) | |||
| CORE‐OM | Baseline | 18 | 2.34 (0.84) | 12 | 2.42 (0.64) | 27 | 2.30 (0.90) | 0.921 |
| 6 months | 12 | 1.77 (0.75) | 8 | 2.08 (0.68) | 16 | 1.91 (0.91) | ||
| 12 months | 9 | 2.23 (0.60) | 6 | 2.10 (0.73) | 15 | 2.13 (0.72) | ||
| PLOC‐PPC | Baseline | 35 | 3.94 (0.72) | 15 | 3.74 (0.55) | 35 | 3.92 (0.69) | 0.621 |
| 6 months | 19 | 4.31 (0.36) | 11 | 3.98 (0.64) | 21 | 4.10 (0.61) | ||
| 12 months | 14 | 4.43 (0.40) | 7 | 4.06 (0.65) | 19 | 3.73 (0.65) | ||
| SDQ‐P | Baseline | 35 | 8.43 (6.04) | 15 | 7.93 (4.01) | 33 | 9.18 (5.57) | 0.738 |
| 6 months | 19 | 5.89 (3.28) | 11 | 6.82 (6.19) | 21 | 8.86 (5.47) | ||
| 12 months | 14 | 4.57 (3.76) | 7 | 6.00 (6.88) | 18 | 10.72 (7.61) | ||
Abbreviations: CORE‐OM, Clinical Outcome in Routine Evaluation – Outcome Measure, Subscale Symptoms; FTI, Family Talk Intervention; IAU, Interventions as Usual; LTC, Let's Talk about Children; PLOC‐PPC, Parental Locus of Control, Subscale Perceived Parental Control; SDQ‐P Total, Strength and Difficulties Questionnaire – Parent Version, Total Difficulties score.
In wave 2 parent reports were completed for 54 (59%) children and in wave 3 for 46 (50%) children. Comparison between remaining participants and those not completing the questionnaire in waves 2 and 3 revealed no significant differences concerning baseline data. We found no significant differences in the attrition of parent reports between study groups over the three waves.
3.2. Effect of intervention on parent‐rated child mental health problems
A significant group × time interaction for the SDQ‐P Total Difficulties score was found for the FTI and LTC groups, versus the IAU group (see Model 1 in Table 3). Expected average changes in child mental health problems for the three groups are illustrated in Figure 2, which shows expected decreased symptoms in the FTI and LTC groups and expected increased symptoms in the IAU group, resulting in expected standardised differences of d = −0.86 and −0.88, respectively, at the end of the study. When including covariates (Model 2), the effect sizes were reduced, but the interpretation of the fixed effects remained similar, and the group × time interaction effect was significant for both the FTI and LTC groups, versus the IAU group.
TABLE 3.
Estimates from growth curve models fitted to the outcome measures SDQ‐P Total Difficulties Subscale (N = 88) and PLOC‐PPC (N = 89)
| Parameters | SDQ‐P Total Difficulties | PLOC‐PPC | ||||||
|---|---|---|---|---|---|---|---|---|
| Model 1 | Model 2 | Model 1 | Model 2 | |||||
| Est. (SE) | 95% CI | Est. (SE) | 95% CI | Est. (SE) | 95% CI | Est. (SE) | 95% CI | |
| Fixed effects | ||||||||
| Intercept/IAU | 9.11 (0.95)*** | 7.21, 11.02 | 8.42 (0.92)*** | 6.62, 10.22 | 4.00 (0.12)*** | 3.77, 4.23 | 4.01 (0.12)*** | 3.77, 4.25 |
| FTI | −0.73 (1.37) | −3.48, 2.02 | 0.58 (1.27) | −1.91, 3.07 | −0.03 (1.17) | −0.37, 0.31 | −0.11 (0.17) | −0.44, 0.22 |
| LTC | −0.93 (1.71) | −4.36, 2.49 | −0.71 (1.65) | −3.94, 2.52 | −0.29 (0.21) | −0.71, 0.13 | −0.27 (0.21) | −0.68, 0.14 |
| Slope/IAU | 1.12 (0.48)* | 0.15, 2.10 | 1.09 (0.59) | −0.07, 2.46 | −0.09 (0.06) | −0.21, 0.04 | −0.07 (0.06) | −0.19, 0.05 |
| FTI | −2.03 (0.70)** | −3.46, −0.61 | −1.73 (0.77)* | −3.24, −0.22 | 0.35 (0.09)*** | 0.17, 0.53 | 0.30 (0.09)** | 0.13, 0.47 |
| LTC | −2.06 (0.88)* | 3.83, −0.29 | −2.04 (0.98)* | 3.96, −0.12 | 0.23 (0.11)* | 0.005, 0.45 | 0.22 (0.12) | 0.02, 0.46 |
| Child age | −0.61 (0.20)** | −1.00, −0.22 | 0.05 (0.03) | −0.009, 0.11 | ||||
| CORE BL | −0.18 (1.40) | −2.92, 2.56 | −0.07 (0.19) | −0.44, 0.30 | ||||
| CORE Change | 1.25 (1.34) | −1.38, 3.88 | 0.02 (0.16) | −0.29, 0.33 | ||||
| Child age × Time | −0.06 (0.13) | −0.31, 0.19 | −0.009 (0.02) | −0.05, 0.03 | ||||
| CORE BL × Time | 0.74 (1.18) | −1.57, 3.05 | −0.04 (0.14) | −0.31, 0.23 | ||||
| CORE Change × Time | −0.26 (1.26) | −2.73, 2.21 | −0.0007 (0.14) | −0.28, 0.27 | ||||
| Random effects (SD) | ||||||||
| Residuals | 2.51 | 2.47 | 0.27 | 0.28 | ||||
| Level 3 intercept | 2.37 | 2.43 | 0.37 | 0.41 | ||||
| Level 2 intercept | 4.26 | 3.90 | 0.47 | 0.46 | ||||
| Time slope (level 2) | 1.08 | 1.31 | 0.20 | 0.21 | ||||
| Correlation | 0.27 | 0.05 | −0.53 | −0.56 | ||||
Note: The time variable was coded 0, 1, 2. In the total sample, the means, and standard deviations at baseline for the outcome measures were as follows: SDQ‐P Total Difficulties (M = 8.73, SD = 5.5) and PLOC‐PPC (M = 3.87, SD = 0.69).
Abbreviations: BL, baseline; Change, change in patient symptoms during the study; CORE, Clinical Outcome in Routine Evaluation – Outcome Measure: Symptoms Subscale; FTI, Family Talk Intervention; IAU, Interventions as Usual; LTC, Let's Talk about Children; PLOC‐PPC, Parental Locus of Control – Perceived Parental Control Subscale; SDQ‐P, Strength and Difficulties Questionnaire – Parent Version: Total Difficulties Subscale.
*p < 0.05; **p < 0.01; ***p < 0.001.
FIGURE 2.
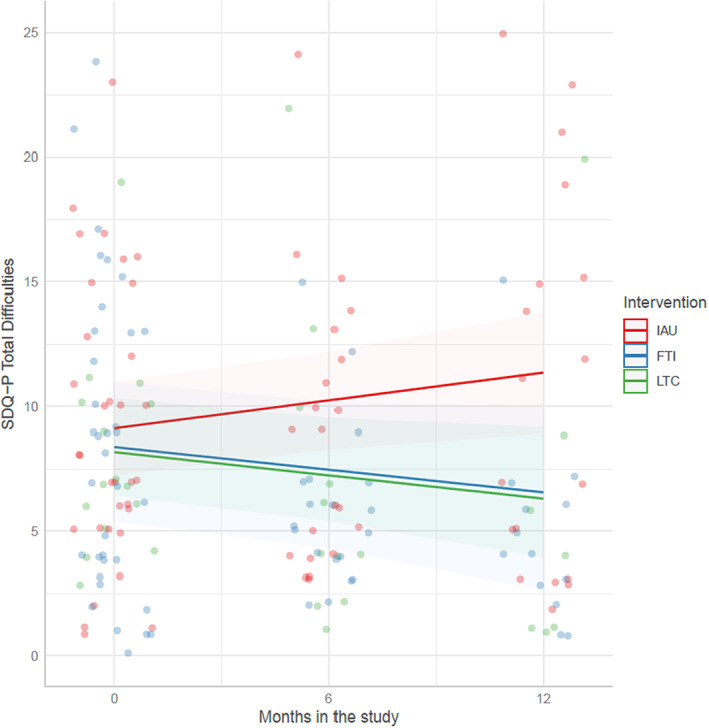
Prototypical trajectories depicting the change in SDQ‐P Total Difficulties score in Model 1 for the study groups. FTI, Family Talk Intervention; IAU, Interventions as Usual; LTC, Let's Talk about Children; SDQ‐P, Strength and Difficulties Questionnaire – Parent Version.
To further investigate the intervention effect, we evaluated the mean difference between study groups in wave 3. In Model 1, the mean difference between the FTI and IAU groups was significant (b = −4.80, SE = 1.82, p = 0.011) with a large effect size (d = −1.02); however, the difference was non‐significant in Model 2 (b = −2.87, SE = 1.60, p = 0.076, d = −0.61). The mean difference between the LTC and IAU groups was significant, with large effect sizes in both models (Model 1: b = −5.05, SE = 2.25, p = 0.028, d = −1.07; Model 2: b = −4.78, SE = 2.28, p = 0.04, d = −1.02).
No significant differences were found in either model when the FTI and LTC groups were compared concerning initial status (Model 1: b = 0.21, SE = 1.74, p = 0.906; Model 2: b = 1.29, SE = 1.71, p = 0.452), rate of change in child mental health problems (Model 1: b = 0.03, SE = 0.90, p = 0.978, d = 0.006; Model 2: b = 0.31, SE = 0.91, p = 0.735, d = 0.07), or mean difference in wave 3 (Model 1: b = 0.26, SE = 2.30, p = 0.912, d = 0.06; Model 2: b = 1.91, SE = 2.19, p = 0.484, d = 0.41).
3.3. Effect of intervention on perceived parental control
We found a significant group × time interaction in the FTI and LTC groups, respectively, versus the IAU group, for change in perceived parental control (Model 1 in Table 3). Figure 3 shows the expected average change for the three groups, and the effect size of the intervention effects of FTI and LTC versus IAU were d = 1.08 and 0.71, respectively, at the end of the study. In Model 2, including covariates, the interaction remained significant for the FTI × IAU comparison, but not for the LTC × IAU comparison; however, the changes in estimates were minor (from 0.23 to 0.22), with the lower boundary of the 95% confidence interval just below zero.
FIGURE 3.
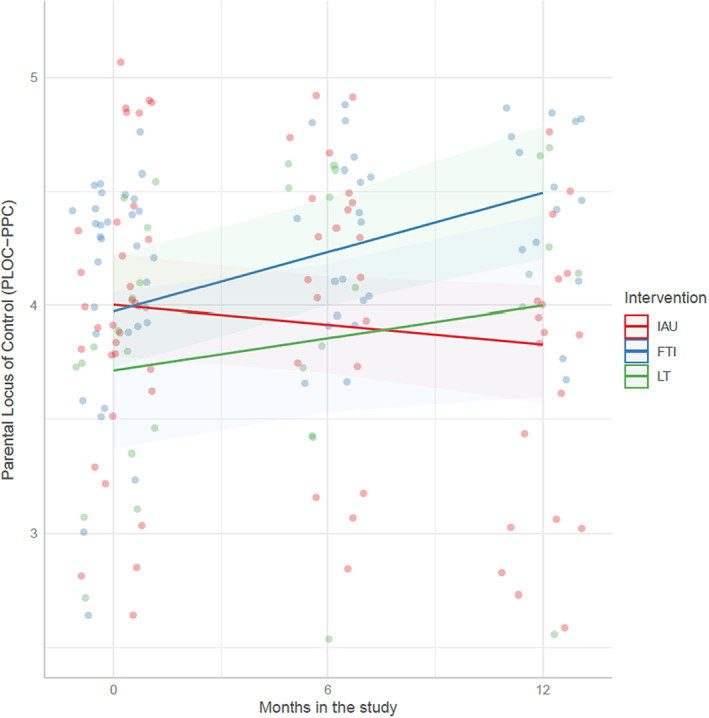
Prototypical trajectories depicting the change in PLOC‐PPC score in Model 1 for the study groups. FTI, Family Talk Intervention; IAU, Interventions as Usual; LTC, Let's Talk about Children; PLOC‐PPC, Parental Locus of Control – Perceived Parental Control Subscale.
The mean difference between groups in wave 3 was significant across the FTI and IAU groups in both models (Model 1: b = 0.67, SE = 0.20, p = 0.001, d = 1.03; Model 2: b = 0.49, SE = 0.20, p = 0.014, d = 0.75). The difference between the LTC and IAU groups in wave 3 was not significant in either model (Model 1: b = 0.17, SE = 0.24, p = 0.487, d = 0.26; Model 2: b = 0.17, SE = 0.24, p = 0.487, d = 0.26).
When comparing the FTI and LTC groups, no significant difference was found in either model concerning initial status (Model 1: b = 0.26, SE = 0.22, p = 0.235; Model 2: b = 0.16, SE = 0.22, p = 0.477), rate of change in perceived parental control over time (Model 1: b = 0.12, SE = 0.11, p = 0.301, d = 0.18; Model 2: b = 0.08, SE = 0.12, p = 0.499, d = 0.12), or mean difference in wave 3 (Model 1: b = 0.50, SE = 0.25, p = 0.053, d = 0.77; Model 2: b = 0.32, SE = 0.25, p = 0.205, d = 0.49).
4. DISCUSSION
This study investigated the effectiveness of preventive interventions used in psychiatric routine care in Sweden for 8–17‐year‐old children of patients with depression, anxiety, or bipolar disorder. The findings indicate that FTI and LTC are associated with more favourable development in terms of preventing increase in parent‐rated child mental health problems compared to IAU. Furthermore, parents in FTI reported enhanced perceived parental control compared to IAU, which was also found for LTC, although evidence was not as strong as for FTI. No significant differences in effect between FTI and LTC were found in this sample.
Previous research has found that preventive interventions for children of parents with mental illness have the potential to reduce child symptoms, 3 , 4 , 5 , 6 and FTI and LTC reportedly both have a positive impact on child mental health problems. 12 , 16 In our study, we found only moderate marginal gains in child mental health problems associated with the FTI and LTC interventions. However, in comparison with the development of the IAU group, these gains were substantial, implying that the FTI and LTC interventions may counteract the increased child mental health problems seen in the IAU group. The intervention effect was large for both interventions in comparison to IAU. Our results are in line with the aims of FTI and LTC that are to reduce risk of symptom development in the children.
In a previous study comparing FTC and LTC, both were found to be associated with improvements in parent‐rated parenting. 16 In our study, we evaluated the effect of the interventions on change in perceived parental control, reflecting the parents' self‐efficacy beliefs about how they can handle difficult rearing situations in relation to their child. 15 We have previously reported that low perceived parental control was significantly associated with more child mental health problems at baseline in this sample, 31 so we wanted to investigate the effects of preventive interventions on such beliefs. Results of Model 1 were in line with our expectations, FTI and LTC were found have a more favourable impact than IAU. In Model 2, when controlling for covariates, the group × time interaction was significant between the FTI and IAU groups, but non‐significant between the LTC and IAU groups. The lower boundary of the 95% CI was, however, only slightly below zero and the effect size was relatively similar to the one derived from Model 1. Given the small sample sizes in these groups, we encourage conservative interpretation of the findings and argue that the significant group × time interaction across the LTC and IAU groups in Model 1 indicates that LTC also has a more favourable impact than does IAU.
The effect size of the mean difference between groups in wave 3 has been calculated to complement the interpretation of the group × time interaction. These results must however be interpreted with caution as the initial status is not accounted for. Nevertheless, the results indicate that the magnitude of the differences between the FTI and LTC groups, versus the IAU group, had a medium to large effect on the SDQ‐P Total Difficulties score. When considering the effect size of the mean differences on PLOC‐PPC, the differences between the FTI and IAU groups were large and medium sized in Models 1 and 2, respectively, whereas between the LTC and IAU groups, the effect sizes were small in both models. The discrepancy between the group × time interaction and the mean group difference in wave 3 is because the IAU group had a higher baseline mean than did the LTC group, although it was not significant given p < 0.05.
When FTI has been compared with LTC in previous research, only small differences have been found. 12 , 16 The results of our study are in line with these previous findings, as we found no significant differences between the FTI and LTC groups in the two outcome measures. However, our study provides limited evidence of the equivalent effects of these interventions and, as noted in previous studies, more research is still needed to better understand which components are effective, if certain subgroups of families would benefit from different interventions and their long‐term effects. 5 , 12 , 16 It is however encouraging that LTC, an intervention designed to be a brief minimum‐level intervention targeting only parents, 11 seems to have more of a short‐term preventive effect on the development of child mental health problems than does IAU; as was also demonstrated to be the case for FTI. Considering that fewer resources are needed to deliver LTC, it might be a method that could be administered to many families as a minimum‐level intervention. In Finland for example, LTC is recommended for every parent who seeks help for mental health problems, followed by FTI which is recommended for families who need more extensive support. 11
On the basis of the included covariates in Model 2, it was possible to evaluate how the patient's level of symptoms influenced the outcome measures, and in this study patients' baseline symptoms and the change in patients' symptoms during the study were not significantly associated with the rate of change in SDQ‐P or PLOC‐PPC. The SDQ‐P results are in line with the findings of Solantaus et al., 12 who found that alleviation of the parents' symptoms was not significantly associated with change in the children's symptoms. Giannakopoulos et al., 16 however, found that alleviation of the parents' symptoms was significantly associated with a decrease in child mental health problems.
The present findings suggest that compared with IAU, FTI and LTC could better prevent an increase in child mental health problems measured 6 and 12 months after the interventions started. The findings also indicate that compared with parents receiving IAU, parents receiving FTI and LTC report a strengthened belief that they can handle their children's difficult behaviours. The present results encourage the continued use of FTI and LTC to support children and parents in contact with adult psychiatry because of depression, anxiety, or bipolar disorder.
4.1. Strengths and limitations
This study advances knowledge of the effectiveness of FTI and LTC when used in routine care, although the results must be interpreted in light of certain limitations. The number of families included in the study was relatively small and randomisation to interventions was not possible as we were constrained by the regular treatment process for the patients. Instead, we controlled statistically for possible between‐group differences in several covariates at baseline. The relatively small number of families in the study groups, in particular in the LTC group, contribute to uncertainty in estimation of effect sizes and parameters. However, the data consisted of longitudinal follow‐ups, with up to three measurement occasions, which reduces the uncertainty in parameter estimation and thereby increase statistical power to detect the true effect sizes. Another limitation is concerned with the heterogeneity of interventions in the IAU group, where a variety of interventions routinely available were included. It is possible that the effectiveness of different approaches within IAU vary, and differences between more homogenous subgroups of IAU and FTI and LTC could show other global results. Furthermore, it is a limitation that the evaluation is based only on parent‐reports, as children's reports could reveal possible differences from the child's perspective, especially when considering that the children are actively included in FTI but not in LTC. Another limitation is the relatively short follow‐up time of 12 months, which limit the evaluation of possible differences between interventions in a longer time perspective. Many of the mental health professionals in all three study groups had training in both FTI and LTC, so spill‐over effects between the interventions were possible.
4.2. Recommendations for future studies
Larger‐scale studies are needed to replicate the preliminary evidence obtained here. The effectiveness also needs to be investigated in longer‐term follow‐up studies. Including multi‐informant reports, especially child reports, would improve our understanding of intervention effects. The support given in IAU varied widely and this points to the need to investigate these interventions in more detail, and the reason to administer which intervention in routine care. Furthermore, studies of the variability of the intervention effect between sub‐groups of families could shed light on which interventions should be offered to whom. Studying parental factors such as perceived parental control would improve our understanding of the possible role of such beliefs in mediating between parent mental health problems and child mental health.
CONFLICT OF INTEREST
Authors have no conflict of interest to declare.
ACKNOWLEDGEMENTS
This work was supported by the Swedish National Board of Health and Welfare (Socialstyrelsen) under registration number 2.7‐38380/2013. We would like to thank the participants for taking part in this project, as well as the research coordinator Pia Svensson and the mental health professionals for assistance with the data collection.
Wirehag Nordh E‐L, Grip K, Thorvaldsson V, Priebe G, Afzelius M, Axberg U. Preventive interventions for children of parents with depression, anxiety, or bipolar disorder: A quasi‐experimental clinical trial. Acta Paediatr. 2023;112:132–142. 10.1111/apa.16555
REFERENCES
- 1. Leijdesdorff S, Van Doesum K, Popma A, Klaassen R, Van Amelsvoort T. Prevalence of psychopathology in children of parents with mental illness and/or addiction: an up to date narrative review. Curr Opin Psychiatry. 2017;30(4):312‐317. doi: 10.1097/YCO.0000000000000341 [DOI] [PubMed] [Google Scholar]
- 2. Reupert A, Maybery D. What do we know about families where parents have a mental illness? A systematic review. Child Youth Serv. 2016;37(2):98‐111. doi: 10.1080/0145935X.2016.1104037 [DOI] [Google Scholar]
- 3. Lannes A, Bui E, Arnaud C, Raynaud J‐P, Revet A. Preventive interventions in offspring of parents with mental illness: a systematic review and meta‐analysis of randomized controlled trials. Psychol Med. 2021;51:2321‐2336. doi: 10.1017/S0033291721003366 [DOI] [PubMed] [Google Scholar]
- 4. Thanhäuser M, Lemmer G, de Girolamo G, Christiansen H. Do preventive interventions for children of mentally ill parents work? Results of a systematic review and meta‐analysis. Curr Opin Psychiatry. 2017;30:283‐299. doi: 10.1097/YCO.0000000000000342 [DOI] [PubMed] [Google Scholar]
- 5. Havinga PJ, Maciejewski DF, Hartman CA, Hillegers MHJ, Schoevers RA, Penninx BWJH. Prevention programmes for children of parents with a mood/anxiety disorder: systematic review of existing programmes and meta‐analysis of their efficacy. Br J Clin Psychol. 2021;60(2):212‐251. doi: 10.1111/bjc.12277 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Loechner J, Starman K, Galuschka K, et al. Preventing depression in the offspring of parents with depression: a systematic review and meta‐analysis of randomized controlled trials. Clin Psychol Rev. 2018;60:1‐14. doi: 10.1016/j.cpr.2017.11.009 [DOI] [PubMed] [Google Scholar]
- 7. Health and Medical Services Act , SFS No. 2017:30. Accessed May 11, 2022. https://www.riksdagen.se/sv/dokument‐lagar/dokument/svensk‐forfattningssamling/halso‐‐och‐sjukvardslag‐201730_sfs‐2017‐30
- 8. Axberg U, Priebe G, Afzelius M, Nordh LW. Barn till föräldrar som har kontakt med vuxenpsykiatrin – Hur har de det? Report in Swedish. Nka; 2020:1. [Google Scholar]
- 9. Afzelius M, Östman M, Råstam M, Priebe G. Parents in adult psychiatric care and their children: a call for more interagency collaboration with social services and child and adolescent psychiatry. Nord J Psychiatry. 2018;72(1):31‐38. doi: 10.1080/08039488.2017.1377287 [DOI] [PubMed] [Google Scholar]
- 10. Beardslee WR, Gladstone TRG, Wright EJ, Cooper AB. A family‐based approach to the prevention of depressive symptoms in children at risk: evidence of parental and child change. Pediatrics. 2003;112(2):e119‐e131. doi: 10.1542/peds.112.2.e119 [DOI] [PubMed] [Google Scholar]
- 11. Solantaus T, Toikka S. The effective family Programme: preventative services for the children of mentally ill parents in Finland. Int J Ment Health Promot. 2006;8(8):1462‐3730. doi: 10.1080/14623730.2006.9721744 [DOI] [Google Scholar]
- 12. Solantaus T, Paavonen JE, Toikka S, Punamäki R‐L. Preventive interventions in families with parental depression: children's psychosocial symptoms and prosocial behaviour. Eur Child Adolesc Psychiatry. 2010;19:883‐892. doi: 10.1007/s00787-010-0135-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Pihkala H, Cederström A, Sandlund M. Beardslee's preventive family intervention for children of mentally ill parents: a Swedish national survey. Int J Ment Health Promot. 2010;12(1):29‐38. doi: 10.1080/14623730.2010.9721804 [DOI] [Google Scholar]
- 14. Marston N, Stavnes K, Van Loon LMA, et al. A content analysis of intervention key elements and assessments (IKEA): what's in the black box in the interventions directed to families where a parent has a mental illness? Child Youth Serv. 2016;37(2):112‐128. doi: 10.1080/0145935X.2016.1104041 [DOI] [Google Scholar]
- 15. Tapias E, Coromina M, Grases N, Ochoa S. Psychological treatments with children of parents with mental illness: a systematic review. Child Youth Care Forum. 2021;50(6):1107‐1130. doi: 10.1007/s10566-021-09608-2 [DOI] [Google Scholar]
- 16. Giannakopoulos G, Solantaus T, Tzavara C, Kolaitis G. Mental health promotion and prevention interventions in families with parental depression: a randomized controlled trial. J Affect Disord. 2021;278:114‐121. doi: 10.1016/j.jad.2020.09.070 [DOI] [PubMed] [Google Scholar]
- 17. Hagekull B, Bohlin G, Hammarberg A. The role of parental perceived control in child development: a longitudinal study. Int J Behav Dev. 2001;25(5):429‐437. doi: 10.1080/01650250042000438 [DOI] [Google Scholar]
- 18. Albanese AM, Russo GR, Geller PA. The role of parental self‐efficacy in parent and child well‐being: a systematic review of associated outcomes. Child Care Health Dev. 2019;45(3):333‐363. doi: 10.1111/cch.12661 [DOI] [PubMed] [Google Scholar]
- 19. Shadish WR, Cook TD. The renaissance of field experimentation in evaluating interventions. Annu Rev Psychol. 2009;60:607‐629. doi: 10.1146/annurev.psych.60.110707.163544 [DOI] [PubMed] [Google Scholar]
- 20. Pihkala H, Renberg H, Söderblom B. Manual för Beardslee's familjeintervention. Translation of the Family Talk Intervention Manual into Swedish . Unpublished manual, n.d.
- 21. Hollingshead AB. The four factor index of social position. Yale J Sociol. 2011;8:21‐52. [Google Scholar]
- 22. Goodman R. Psychometric properties of the strengths and difficulties questionnaire. J Am Acad Child Adolesc Psychiatry. 2001;40(11):1337‐1345. doi: 10.1097/00004583-200111000-00015 [DOI] [PubMed] [Google Scholar]
- 23. Smedje H, Broman J‐E, Hetta J, Von Knorring A‐L. Psychometric properties of a Swedish version of the “Strengths and Difficulties Questionnaire”. Eur Child Adolesc Psychiatry. 1999;8(2):63‐70. [DOI] [PubMed] [Google Scholar]
- 24. Campis LK, Lyman RD, Prentice‐Dunn S. The parental locus of control scale: development and validation. J Clin Child Psychol. 1986;15(3):260‐267. doi: 10.1207/s15374424jccp1503_10 [DOI] [Google Scholar]
- 25. Evans C, Connell J, Barkham M, et al. Towards a standardised brief outcome measure: psychometric properties and utility of the CORE‐OM. Br J Psychiatry. 2002;180:51‐60. doi: 10.1192/bjp.180.1.51 [DOI] [PubMed] [Google Scholar]
- 26. Elfström ML, Evans C, Lundgren J, Johansson B, Hakeberg M, Carlsson SG. Validation of the Swedish version of the clinical outcomes in routine evaluation outcome measure (CORE‐OM). Clin Psychol Psychother. 2013;20(5):447‐455. doi: 10.1002/cpp.1788 [DOI] [PubMed] [Google Scholar]
- 27. Singer JD, Willet JB. Applied Longitudinal Data Analysis. Oxford University Press; 2003. [Google Scholar]
- 28. Björnsdotter A, Enebrink P, Ghaderi A. Psychometric properties of online administered parental strengths and difficulties questionnaire (SDQ), and normative data based on combined online and paper‐and‐pencil administration. Child Adolesc Psychiatry Ment Health. 2013;7(1):40. doi: 10.1186/1753-2000-7-40 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Cohen J. Quantitative methods in psychology. Psychol Bull. 1992;112(1):155‐159. doi: 10.1038/141613a0 [DOI] [PubMed] [Google Scholar]
- 30. van Buuren S, Oudshoorn CGM. MICE: multivariate imputation by chained equations . R package version. 2007;1(3):2007. [Google Scholar]
- 31. Nordh E‐LW, Priebe G, Grip K, Afzelius M, Axberg U. Mental health in children of parents being treated by specialised psychiatric services. Scand J Public Health. 2022. doi: 10.1177/14034948221076208. Online ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]


