Abstract
Polypharmacy is a common problem among older adults, as they are more likely to have multiple chronic conditions and may experience fragmentation of care among specialists. The Geriatrics 5Ms framework offers a person-centered approach to address polypharmacy and optimize medications, including deprescribing when appropriate. The elements of the Geriatrics 5Ms, which align with the approach of the Age-Friendly Health Systems initiative, include consideration of Medications, Mind, Mobility, Multicomplexity, and What Matters Most. Each M domain impacts and is impacted by medications, and learning about the patient’s goals through questions guided by the Geriatrics 5Ms may inform an Age-Friendly medication optimization plan. While research on the implementation of each of the elements of the Geriatrics 5Ms shows benefit, further research is needed to study the impact of this framework in clinical practice.
Key Points
| The Geriatrics 5Ms of Mobility, Mind, Medications, Multicomplexity, and What Matters Most can help clinicians address polypharmacy among older adults, by addressing how each M domain impacts and is impacted by Medications. |
| The Age-Friendly Health Systems approach to medication management can help align medication use with what matters to the patient. |
| Further research is needed to study the impact of an Age-Friendly approach to polypharmacy in older adults and others across the lifespan. |
Introduction: An Age-Friendly Approach to Medications in Older Adults
Clinicians are eager for efficient approaches to the challenge of polypharmacy, typified by an older adult with multiple chronic conditions taking five or more medications, whether appropriate or potentially inappropriate. Polypharmacy may be thought of as an issue borne from multiple ‘solutions’ to separate problems, a consequence of a healthcare system that facilitates isolated disease management and siloed care. Together with the fact that the population as a whole is aging and comorbidities are on the rise, complex medication regimens will continue to proliferate, including in younger populations [1]. Polypharmacy increases the risks of frailty, falls, healthcare utilization, and mortality, yet clinicians may lack training in practical approaches to optimizing medications and minimizing risk [2]. Many tools exist to assist clinicians in optimizing medications in older adults, including the American Geriatric Society Beers Criteria, STOPP/START, and deprescribing guidelines [2–7]; however, these approaches typically focus primarily on the medications themselves, including risks, adverse effects, and interactions.
The Geriatrics 5Ms framework [8] can help clinicians approach medication optimization in a holistic manner, by considering, in additions to Medications, the domains of Mobility, Mind, Multicomplexity, and What Matters Most. By exploring how each of these M domain impacts and is impacted by medications, including how these domains may affect adherence to medications, clinicians can align medication use with what matters to a patient and their loved ones. Consideration of individual patient preferences and context remains critical. What matters to our patients, whether that be independence, spending time with family, continuing to engage with certain activities, or something directly related to their healthcare, must be accounted for with a person-centered vision of medication management.
The Geriatrics 5Ms framework was initially developed by geriatricians to broadly but concisely capture areas of focus in older adult care [8, 9]. The 5Ms align with the Age-Friendly Health Systems initiative [10], a model for evidence-based care of older adults that emerged around the same time, and focuses on implementing the 4Ms of Mobility, Medications, Mentation, and What Matters in healthcare settings (of note, the 4Ms do not include Multicomplexity, and list Mentation instead of Mind) [11, 12]. Initially conceived of through a collaboration between the John A. Hartford Foundation and the Institute for Healthcare Improvement in response to an evolving healthcare system and an aging population, the Age-Friendly Health Systems approach was designed and piloted with experts in implementation science, patient safety, and quality improvement with the goal of creating a system that could better prevent avoidable harms, provide higher quality care to those with serious illness or at the end of life, and build stronger support for caregivers and families all while reducing costs [13, 14]. While the Age-Friendly 4Ms does not include Multicomplexity, we include it here in the Geriatrics 5Ms as it can inform a holistic approach to medication management in older adults. Here, we outline the ways in which the Geriatrics 5Ms can be used as an integrated set for thoughtfully approaching medication optimization in older adults, and describe its use in clinical innovation and health profession education. Finally, we outline challenges in implementing an Age-Friendly approach to medication management, along with suggestions for future research in this important area.
The Geriatrics 5Ms and Age-Friendly Medication Management
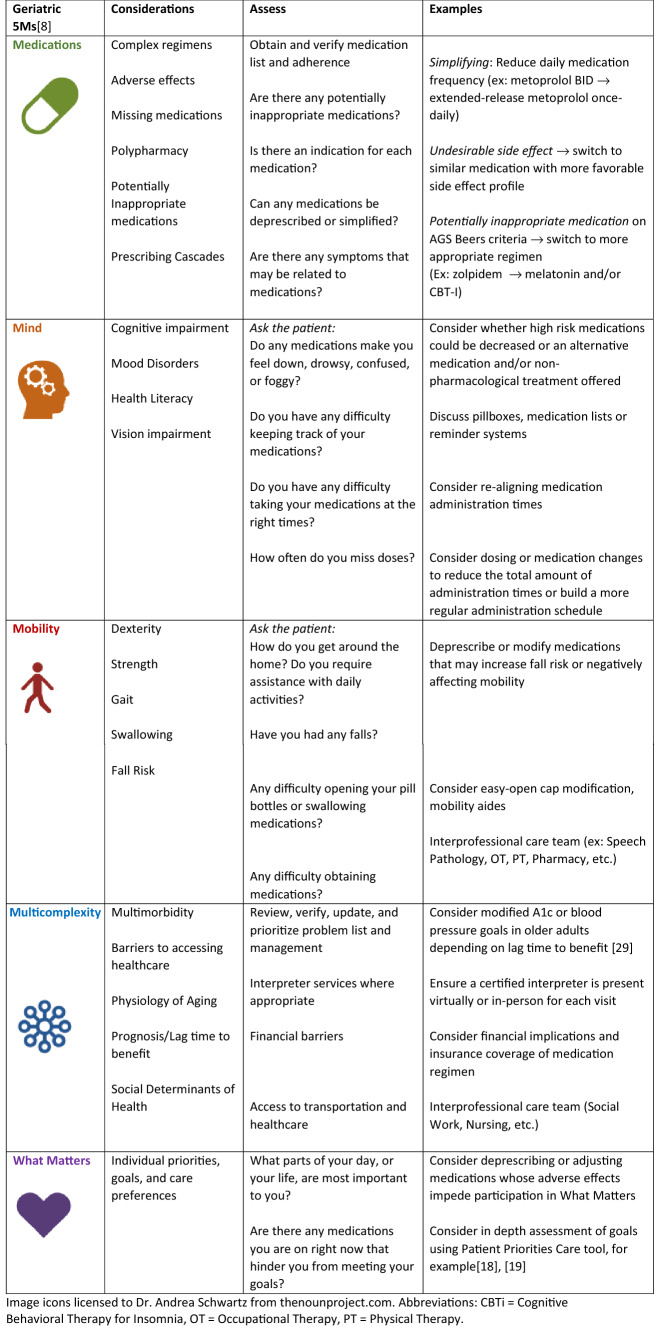
The Geriatrics 5Ms provides a memorable framework to guide medication optimization in older adults with multiple chronic conditions and polypharmacy. In Table 1, we describe how each M domain impacts and is impacted by Medications, along with examples of considerations for clinicians and patients. Appropriate prescribing starts with matching each medication with an indication, avoiding drug–drug interactions, and weighing risks and benefits [15]. To deliver Age-Friendly medication management, the Geriatrics 5Ms help the clinician meet the patient’s needs beyond their specific medical problems. A deeper understanding of the patient’s experiences with medications and healthcare and how they align with their health and life goals is gained by engaging and centering the patient and, potentially, their families or caregivers through an exploration of each of the 5Ms and their interconnections.
Table 1.
An Age-Friendly approach to polypharmacy and deprescribing using the geriatric 5Ms
Consider Mobility: if the patient has difficulty swallowing their pills, poor dexterity, or issues opening pill bottles because of arthritis, these findings may affect the medications and formulations they are prescribed. Conversely, if their medications are causing orthostatic hypotension or dizziness, thereby increasing fall risk, Mobility will be deeply affected by Medications [16]. This same principle is consistent for the other M domains. In the Mind domain (also referred to as Mentation in the Age-Friendly 4Ms), cognitive impairment may lead to difficulties organizing and adhering to a complex medication regimen, while some medications may contribute to confusion, delirium, or mood symptoms and may warrant consideration of deprescribing [17]. With Multicomplexity, insufficient finances to purchase medications, caregiver burden, or residing in a care facility may affect how medications are accessed, and what we prescribe potentially affects prognosis and frailty. Most importantly, when we ask the patient What Matters to them, we learn which treatments they are willing to tolerate and which they find burdensome; a communication tool such as Patient Priorities Care may help clarify their preferences and goals [18, 19]. Additionally, prescribing mis-aligned with What Matters, such as inadequate pain control, can impede patients from doing what they enjoy and reaching their goals. Addressing medications in older patients by considering each of the Geriatrics 5Ms can help clinicians deliver Age-Friendly person-centered care.
Additionally, the 5Ms are broad enough to be potentially applicable beyond the geriatric population and across the lifespan, such as when caring for people with cognitive impairment, physical disabilities that may make administering medications difficult, comorbidities due to chronic disease sequelae, congenital disorders, the activities of caregivers, and end-of-life care for all ages. An Age-Friendly approach to medications could yield benefits beyond older adults, whether proactively applied or as part of a deprescribing or medication-optimization plan.
Clinical Implementation of the Geriatrics 5Ms and the Age-Friendly Health Systems Approach
Research is emerging on how application of the Age-Friendly approach can influence patient care and show a promising benefit [20]. While evidence is emerging about the implementation of the 4Ms framework as a set, evidence for interventions within each M domain has been shown to lead to improvements in health status, safer mobility, and reductions in overprescribing—indicating that focusing on these domains leads to the predicted clinical benefit [12]. One quality improvement initiative found that implementing the 4Ms to focus on risk stratification of patients and medication safety led to providers having a better understanding of care plans and interventions in high-risk patients, simplification of medication regimens with improvement in medication adherence, and importantly, a reduction in hospitalizations and re-admissions [21]. In a rural care setting a focus on the 4Ms was used to develop a screening program for geriatric health issues such as cognitive impairment, malnutrition, and frailty, with subsequent as-needed intervention including exercise programs and cognitive therapy. After identifying these conditions in their study population and stratifying, follow-up evaluations demonstrated improvements after a year in measures of physical and mental status such as the Timed Up and Go Test and the Cornell Scale for Depression in Dementia, respectively [22]. Beyond primary care, specialists have considered how the Geriatrics 5Ms can be applied to the care of their complex patients in a variety of specialties [23–25] and settings, including the intensive care unit [26]. These frameworks have been applied to guidelines for prescribing statins in older adults [25, 27] and many areas of research remain to study the impact of these approaches.
Age-Friendly Health Professions Education and the Geriatrics 5Ms
Educational curricula using the 4Ms or 5Ms help provide a common language and structure for health professions trainees early in their training, and provide a framework for deeper dives on polypharmacy and deprescribing [15, 28, 29]. Recognizing the challenges and opportunities with providing care to an aging population, health profession education programs are developing creative modules guided by these frameworks [30–32]. At our own institution, we developed the Geriatrics 5Ms pocket card for medical and dental students as a teaching tool that could be carried on the wards as a resource to guide holistic care for older patients [33], as well as home visits with older adult patients grounded in the concepts of the 5Ms [34]. One small longitudinal pilot of an interactive case-based workshop for primary care residents found high satisfaction amongst participants and improved confidence in applying the elements of the 5Ms in older adult care, with 83% of participants indicating an interest in utilizing medication and pharmacy resources at the conclusion of the workshop compared with 19% prior [35]. Interprofessional training, with trainee representation including pharmacy, social work, nursing, and psychology learners among others, has also been implemented to teach Age-Friendly care [32, 36]. Continuing education for practicing clinicians [37] offers further opportunities to use the shared language of the 5Ms to create a memorable approach to addressing medications in older adults.
Challenges Applying the Geriatrics 5Ms to Medication Management and to Deprescribing
While the Geriatrics 5Ms offer a helpful guide for approaching medication management in older adults by considering Mobility, Mind, Multicomplexity, and What Matters Most, challenges remain in its implementation. For example, in the context of a patient encounter where use of the Geriatrics 5Ms may suggest changes or reductions in medications to minimize their impact on mobility or mentation, there may be challenges to implementing a deprescribing plan [38]. First, polypharmacy often implies a clinically complex patient. Multiple conditions with interacting and compounding pathophysiology and sequelae may be difficult to approach in a typical encounter limited by time, expertise, or emergent concerns. When it comes to deprescribing, these may be particularly sensitive discussions and recommendations as patients and/or their caregivers may not fully understand the reasons for deprescribing, may have concerns about discontinuing or changing a medication they had been taking for potentially years, or there may not have been enough time to establish a trustworthy patient-physician rapport for shared decision making [39–41]. Confronting some of the uncertainties that come with deprescribing are more easily embraced if pursued holistically, as a thoughtful application of the 5Ms reveals the complexities and power of the Medications domain and their tendency to influence and be influenced by the other M domains. There may be hesitancy to adjust or discontinue medications from other specialists or missing/inaccessible information from non-communicating online medical records [42]. Managing multiple conditions can mean encountering conflicting disease-specific guidelines, uncertainties about the indirect effects of deprescribing, and evolving goals of care. Patients may also be reluctant to stop or to make changes to a regimen that has been satisfactory for many years. In the era of COVID-19 and an increase in virtual visits, this may lead to additional hesitancy to deprescribe particularly with visits conducted over the phone and a lack of an in-person physical examination, though telehealth may provide opportunities to gain a new lens on a patient’s medication use [43, 44]. Finally, inequities related to socioeconomic status, proximity to healthcare centers, and systemic disparities in healthcare create additional barriers for the most vulnerable patients, with the potential consequences being further preventable harms [38, 45].
Conclusion: The Geriatrics 5Ms and Medication Management
The Geriatrics 5Ms and the Age-Friendly Health System offer a path to approach polypharmacy in a person-centered way. Importantly, the 5Ms are not a checklist, rather, a philosophy and a language that encourage flexibility and individualization during the visit. For this reason, the 5Ms may be helpful beyond the older adult population including patients with chronic diseases and polypharmacy who could benefit from medication optimization and deprescribing. Providers may utilize or inquire about any number of the 5Ms in a single visit, though attention should be paid to all dimensions over the long term. Coordinated or interprofessional care models also work well with the 5Ms by lowering communication barriers between clinicians to better streamline a patient’s healthcare. Education on the 5Ms to the next generation of healthcare professionals is ongoing and robust. However, large research trials on how the 5Ms may benefit patient care are lacking. How recommendations originating from a 5Ms approach translate to deprescribing, reduced hospitalizations, or improved quality of life remain important research questions, to which the ongoing implementation of the Age-Friendly Health Systems initiative may be poised to offer answers [46].
In conclusion, the Geriatrics 5Ms allow for holistic and adaptable decision making guided by patient preference and evidence-based medicine to optimize medications for patients with (or without) polypharmacy. Age-Friendly medication optimization, including thoughtful deprescribing when appropriate, may improve patient quality of life along with the experience of care for the patient and provider [47, 48]. This Age-Friendly approach will benefit medication management for patients across the lifespan [49]. With the 5Ms and appropriate support, prescribers in partnership with their patients and care team can be better equipped to optimize polypharmacy to support what matters most to our patients.
Declarations
Funding
AWS reports receiving support from the Harvard Medical School Dean’s Innovation award for education. PJM did not receive financial support for this work.
Conflict of interest
AWS serves as a faculty member for the Institute for Healthcare Improvement’s Age-Friendly Health Systems initiative and on the Veteran Affairs national Age-Friendly steering committee. PJM has no disclosures or potential conflicts of interest to report. Some of this material is the result of work supported with resources and the use of facilities at the Veterans Affairs Boston Healthcare System and the New England Geriatric Research Education and Clinical Center. The views expressed in this article are those of the authors and do not necessarily reflect the position or policy of the Department of Veterans Affairs or the US government.
Ethics approval
Not applicable.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Availability of data and material
Not applicable.
Code availability
Not applicable.
Authors’ contributions
PJM was responsible for the initial conception of the paper, relevant literature review, and drafting the manuscript and response to reviewer comments. AWS was responsible for the initial conception of the paper, critical editing and revisions throughout the writing and revision process, and submission of the final manuscript. PJM and AWS have read and approved the final version of the manuscript and agreed to be accountable for the work.
References
- 1.Khezrian M, McNeil CJ, Murray AD, Myint PK. An overview of prevalence, determinants and health outcomes of polypharmacy. Ther Adv Drug Saf. 2020;11:2042098620933741. doi: 10.1177/2042098620933741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Halli-Tierney AD, Scarbrough C, Carroll DG. Polypharmacy: evaluating risks and deprescribing. AFP. 2019;100(1):32–38. [PubMed] [Google Scholar]
- 3.Thompson W, et al. Tools for deprescribing in frail older persons and those with limited life expectancy: a systematic review. J Am Geriatr Soc. 2019;67(1):172–180. doi: 10.1111/jgs.15616. [DOI] [PubMed] [Google Scholar]
- 4.Scott IA, et al. Reducing inappropriate polypharmacy: the process of deprescribing. JAMA Intern Med. 2015;175(5):827–834. doi: 10.1001/jamainternmed.2015.0324. [DOI] [PubMed] [Google Scholar]
- 5.2019 American Geriatrics Society Beers Criteria® Update Expert Panel American Geriatrics Society 2019 Updated AGS Beers Criteria® for potentially inappropriate medication use in older adults. J Am Geriatr Soc. 2019;67(4):674–694. doi: 10.1111/jgs.15767. [DOI] [PubMed] [Google Scholar]
- 6.Gallagher P, Ryan C, Byrne S, Kennedy J, O’Mahony D. Screening tool of older person’s prescriptions (STOPP) and screening tool to alert doctors to right treatment (START), consensus validation. Int J Clin Pharmacol Ther. 2008;46:72–83. doi: 10.5414/CPP46072. [DOI] [PubMed] [Google Scholar]
- 7.Phung E, Triantafylidis L, Zhang HM, Yeh IM. New media, part 5: online deprescribing tools. J Palliat Med. 2018;21(2):269–270. doi: 10.1089/jpm.2017.0688. [DOI] [Google Scholar]
- 8.Tinetti M, Huang A, Molnar F. The geriatrics 5M’s: a new way of communicating what we do. J Am Geriatr Soc. 2017;65(9):2115. doi: 10.1111/jgs.14979. [DOI] [PubMed] [Google Scholar]
- 9.Molnar F, Huang A, Tinetti M. Update: the public launch of the geriatric 5Ms. Can Geriatr Soc J CME 2017 Apr 28. Available from: http://canadiangeriatrics.ca/wp-content/uploads/2017/04/UPDATE-THE-PUBLIC-LAUNCH-OF-THE-GERIATRIC-5MS.pdf. Accessed 16 Mar 2023
- 10.IHI, Institute for Healthcare Improvement. What is an age-friendly health system? Available from: http://www.ihi.org:80/Engage/Initiatives/Age-Friendly-Health-Systems/Pages/default.aspx. Accessed 21 Dec 2020.
- 11.Mate KS, Berman A, Laderman M, Kabcenell A, Fulmer T. Creating age-friendly health systems: a vision for better care of older adults. Healthcare (Amst). 2018;6(1):4–6. doi: 10.1016/j.hjdsi.2017.05.005. [DOI] [PubMed] [Google Scholar]
- 12.Mate K, et al. Evidence for the 4Ms: interactions and outcomes across the care continuum. J Aging Health. 2021 doi: 10.1177/0898264321991658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Fulmer T, Mate KS, Berman A. The age-friendly health system imperative. J Am Geriatr Soc. 2018;66(1):22–24. doi: 10.1111/jgs.15076. [DOI] [PubMed] [Google Scholar]
- 14.Allen K, Ouslander JG. Age-friendly health systems: their time has come. J Am Geriatr Soc. 2018;66(1):19–21. doi: 10.1111/jgs.15134. [DOI] [PubMed] [Google Scholar]
- 15.Hawley CE, Triantafylidis LK, Phillips SC, Schwartz AW. Brown bag simulation to improve medication management in older adults. MedEdPORTAL. 2019;15:10857. doi: 10.15766/mep_2374-8265.10857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Thwaites JH. Practical aspects of drug treatment in elderly patients with mobility problems. Drugs Aging. 1999;14(2):105–114. doi: 10.2165/00002512-199914020-00003. [DOI] [PubMed] [Google Scholar]
- 17.Triantafylidis LK, Clemons JS, Peron EP, Roefaro J, Zimmerman KM. Brain over bladder: a systematic review of dual cholinesterase inhibitor and urinary anticholinergic use. Drugs Aging. 2018;35(1):27–41. doi: 10.1007/s40266-017-0510-6. [DOI] [PubMed] [Google Scholar]
- 18.Tinetti ME, et al. Association of patient priorities-aligned decision-making with patient outcomes and ambulatory health care burden among older adults with multiple chronic conditions: a nonrandomized clinical trial. JAMA Intern Med. 2019;179(12):1688. doi: 10.1001/jamainternmed.2019.4235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Moye J, Driver JA, Owsiany MT, et al. Assessing What Matters Most in Older Adults With Multicomplexity. Gerontologist. 2021;62(4):e224–e234. doi: 10.1093/geront/gnab071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Farrell TW, Volden TA, Butler JM, et al. Age-friendly care in the Veterans Health Administration: past, present, and future. J Am Geriatr Soc. 2023;71(1):18–25. doi: 10.1111/jgs.18070. [DOI] [PubMed] [Google Scholar]
- 21.Guth A, Chou J, Courtin SO, Ford C, Hennawi G, Brandt N. An interdisciplinary approach to implementing the age-friendly health system 4Ms in an ambulatory clinical pathway with a focus on medication safety. J Gerontol Nurs. 2020;46(10):7–11. doi: 10.3928/00989134-20200909-02. [DOI] [PubMed] [Google Scholar]
- 22.Lundy J, Hayden D, Pyland S, Berg-Weger M, Malmstrom TK, Morley JE. An age-friendly health system. J Am Geriatr Soc. 2021;69(3):806–812. doi: 10.1111/jgs.16959. [DOI] [PubMed] [Google Scholar]
- 23.Kochar B, Ufere NN, Ritchie CS, Lai JC. The 5Ms of geriatrics in gastroenterology: the path to creating age-friendly care for older adults with inflammatory bowel diseases and cirrhosis. Clin Transl Gastroenterol. 2022;13(1):e00445. doi: 10.14309/ctg.0000000000000445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Liu CK. Mobility and what matters: moving kidney care toward the 4Ms of an age-friendly health system. Kidney Med. 2022;4(6):100481. doi: 10.1016/j.xkme.2022.100481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hawley CE, Roefaro J, Forman DE, Orkaby AR. Statins for primary prevention in those aged 70 years and older: a critical review of recent cholesterol guidelines. Drugs Aging. 2019;36(8):687–699. doi: 10.1007/s40266-019-00673-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Geen O, Perrella A, Rochwerg B, Wang XM. Applying the geriatric 5Ms in critical care: the ICU-5Ms. Can J Anaesth. 2022;69(9):1080–1085. doi: 10.1007/s12630-022-02270-9. [DOI] [PubMed] [Google Scholar]
- 27.Shah RC, Supiano MA, Greenland P. Aligning the 4Ms of age-friendly health systems with statin use for primary prevention. J Am Geriatr Soc. 2020;68(3):463–464. doi: 10.1111/jgs.16325. [DOI] [PubMed] [Google Scholar]
- 28.Sehgal M, Nassetta KR, Bamdas JAM, Sourial M. First do no ‘pharm’: educating medical and pharmacy students on the essentials of medication management. Curr Pharm Teach Learn. 2019;11(9):920–927. doi: 10.1016/j.cptl.2019.05.006. [DOI] [PubMed] [Google Scholar]
- 29.Triantafylidis LK, Phillips SC, Hawley CE, Schwartz AW. Finding the sweet spot: an interactive workshop on diabetes management in older adults. MedEdPORTAL. 2019;15:10845. doi: 10.15766/mep_2374-8265.10845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Goldberg GR, Solis G, John JT, Olvet DM, Kranz KA. 4Ms for early learners: a skills-based geriatrics curriculum for second-year medical students. MedEdPORTAL. 2022;18:11264. doi: 10.15766/mep_2374-8265.11264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Michener A, Fessler E, Gonzalez M, Miller RK. The 5 M’s and more: a new geriatric medical student virtual curriculum during the COVID-19 pandemic. J Am Geriatr Soc. 2020;68(11):E61–E63. doi: 10.1111/jgs.16855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Wu BJ, Honan L, Tinetti ME, Marottoli RA, Brissette D, Wilkins KM. The virtual 4Ms: a novel curriculum for first year health professional students during COVID-19. J Am Geriatr Soc. 2021;69(6):E13–16. doi: 10.1111/jgs.17185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Holliday AM, Hawley CE, Schwartz AW. Geriatrics 5Ms pocket card for medical and dental students. J Am Geriatr Soc. 2019;67(12):E7–9. doi: 10.1111/jgs.16226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Goldlist K, Beltran CP, Rhodes-Kropf J, Sullivan AM, Schwartz AW. Out of the classroom, into the home: Medical and dental students' lessons learned from a Geriatrics home visit. J Am Geriatr Soc. 2022;70(9):2659–2665. doi: 10.1111/jgs.17968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Phillips SC, Hawley CE, Triantafylidis LK, Schwartz AW. Geriatrics 5Ms for primary care workshop. MedEdPORTAL. 2019;15:10814. doi: 10.15766/mep_2374-8265.10814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Schwartz AW, et al. A workshop for interprofessional trainees using the geriatrics 5Ms framework. J Am Geriatr Soc. 2020;68(8):1857–1863. doi: 10.1111/jgs.16574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Levine SA, et al. Practicing physician education in geriatrics: lessons learned from a train-the-trainer model. J Am Geriatr Soc. 2007;55(8):1281–1286. doi: 10.1111/j.1532-5415.2007.01205.x. [DOI] [PubMed] [Google Scholar]
- 38.Doherty AJ, et al. Barriers and facilitators to deprescribing in primary care: a systematic review. BJGP Open. 2020;4(3):bjgpopen20X101096. [DOI] [PMC free article] [PubMed]
- 39.Hahn EE, et al. Patient and physician perspectives of deprescribing potentially inappropriate medications in older adults with a history of falls: a qualitative study. J Gen Intern Med. 2021;36(10):3015–3022. doi: 10.1007/s11606-020-06493-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Linsky A, Simon SR, Bokhour B. Patient perceptions of proactive medication discontinuation. Patient Educ Couns. 2015;98(2):220–225. doi: 10.1016/j.pec.2014.11.010. [DOI] [PubMed] [Google Scholar]
- 41.Pickering AN, et al. Older patient and caregiver perspectives on medication value and deprescribing: a qualitative study. J Am Geriatr Soc. 2020;68(4):746–753. doi: 10.1111/jgs.16370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Goyal P, et al. Physician perspectives on deprescribing cardiovascular medications for older adults. J Am Geriatr Soc. 2020;68(1):78–86. doi: 10.1111/jgs.16157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Elbeddini A, Prabaharan T, Almasalkhi S, Tran C, Zhou Y. Barriers to conducting deprescribing in the elderly population amid the COVID-19 pandemic. Res Soc Adm Pharm. 2021;17(1):1942–1945. doi: 10.1016/j.sapharm.2020.05.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Moo LR. Home video visits: two-dimensional view of the geriatric 5 M’s. J Am Geriatr Soc. 2020;68(11):2425–2427. doi: 10.1111/jgs.16843. [DOI] [PubMed] [Google Scholar]
- 45.Farrell TW, et al. Exploring the intersection of structural racism and ageism in healthcare. J Am Geriatr Soc. 2022;70(12):3366–3377. doi: 10.1111/jgs.18105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Church K, Munro S, Shaughnessy M, Clancy C. Age-Friendly Health Systems: Improving care for older adults in the Veterans Health Administration. Health Serv Res. 2023;58(Suppl 1):5–8. doi: 10.1111/1475-6773.14110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Low CE, et al. Deprescribing in hospice patients: discontinuing aspirin, multivitamins, and statins. Mayo Clin Proc Innov Qual Outcomes. 2021;5(4):721–726. doi: 10.1016/j.mayocpiqo.2021.06.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Green AR, Aschmann H, Boyd CM, Schoenborn N. Assessment of patient-preferred language to achieve goal-aligned deprescribing in older adults. JAMA Netw Open. 2021;4(4):e212633. doi: 10.1001/jamanetworkopen.2021.2633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Loewenthal J, Javedan H, Schwartz AW. Overcoming Inertia: an Exercise in Clinical Reasoning. J Gen Intern Med. 2020;35(9):2771–2775. doi: 10.1007/s11606-020-05928-6. [DOI] [PMC free article] [PubMed] [Google Scholar]