Background and epidemiology: Acute myocardial infarction in women aged 18 to 49 is rare, accounting for only 115 deaths in 1998/99 in Canada.1 Shortly after oral contraceptives became widely available, a 1963 report identified them as a risk factor for myocardial infarction.2 Subsequent studies showed that women who took oral contraceptives and were heavy smokers were at 30 times greater risk for myocardial infarction than were women with neither risk factor.3 Partly in response to these adverse effects, oral contraceptives with lower doses of estrogen and varying types of progestogens were developed. These newer contraceptives, containing second-generation progestogens (mainly levonorgestrel), appeared to be an improvement over the earlier ones, but risks of arterial disease and myocardial infarction remained.
Oral contraceptives containing third-generation progestogens (gestodene or desogestrel) have recently been marketed. There is conflicting evidence regarding the cardiovascular risks of these newer agents. Some studies showed no significant difference in the risk of myocardial infarction between women reporting prior use of second-generation oral contraceptives and those reporting use of third-generation products.4
In a recent paper Tanis and colleagues5 used the knowledge that third-generation products are widely used in the Netherlands to conduct a case–control study there involving women aged 17 to 49 who had been admitted to hospital following a myocardial infarction. The age-matched control subjects were women living in the community who had not been admitted to hospital for that reason. The odds ratio (OR) for myocardial infarction among women who used any oral contraceptive was 2.0 (95% confidence interval [CI] 1.5–2.8). Among women who used a second-generation oral contraceptive the adjusted OR was 2.5 (95% CI 1.5–4.1), whereas among women who reported using a third-generation oral contraceptive the adjusted OR was 1.3 (95% CI 0.7–2.5). ORs were adjusted for age, area of residence and calendar year of the index event; smoking status; presence or absence of hypertension, hypercholesterolemia, diabetes, obesity (a body mass index of at least 27.3) and a family history of cardiovascular disease; level of education; and alcohol intake.
Interpretation of results from such retrospective studies is always impeded by the possibility of bias. In a secondary analysis the authors compared women who had no major cardiovascular risk factors:5 the risk of myocardial infarction associated with taking any oral contraceptive was 3 times higher than the risk associated with not taking an oral contraceptive. In Canada about 18% of women aged 15 to 49 take oral contraceptives.6
Clinical management: Advice to women about contraception should include information on the risks associated with pregnancies and abortions, and on the efficacy and risks of various methods of contraception. For oral contraceptives, it appears that third-generation products may be slightly less of a risk factor for myocardial infarction than second-generation products.
Smoking remains the most important risk factor for myocardial infarction in women aged 18 to 49. Tanis and colleagues found that women who did not take oral contraceptives but who smoked had an adjusted OR for myocardial infarction of 7.9 (95% CI 4.9–12.9) compared with women who did not smoke. In another recent study the risk of myocardial infarction was 32 times higher (95% CI 12–81) among women who both smoked heavily and took oral contraceptives than among women who did neither.7
Control and prevention: Despite the findings of Tanis and colleagues, the overall evidence makes it unclear whether third-generation oral contraceptives pose less of a risk for myocardial infarction than their second-generation counterparts. However, whatever the patient's choice, she should be advised that the risk of myocardial infarction increases with age, that smoking remains a very strong risk factor, and that smoking and taking oral contraceptives may put them at very high risk. As with patients of any age, demonstrable gains in risk reduction are possible by paying attention to treating hypertension and lowering elevated cholesterol levels.
John Hoey CMAJ
Figure.
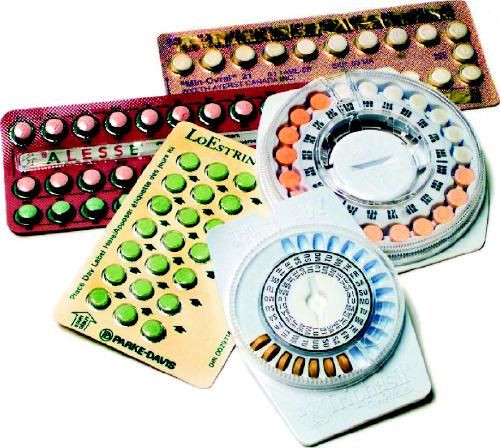
Photo by: Canapress
References
- 1.Canadian Mortality Database (special tabulations) and Canadian Hospital Morbidity Database (special tabulations). Ottawa: Statistics Canada.
- 2.Boyce J, Fawcett JW, Noall EWP. Coronary thrombosis and Conovid. Lancet 1963;1:111. [DOI] [PubMed]
- 3.Shapiro S, Slone D, Rosenberg L, Kaufman DW, Stolley PD, Miettinen OS. Oral-contraceptive use in relation to myocardial infarction. Lancet 1979;1:743-7. [DOI] [PubMed]
- 4.Dunn N, Thorogood M, Faragher B, de Caestecker L, MacDonald TM, McCollom C, et al. Oral contraceptives and myocardial infarction: results of the MICA case–control study. BMJ 1999;319;1579-83 [DOI] [PMC free article] [PubMed]
- 5.Tanis BC, van den Bosch MAAJ, Kemmeren JM, Cats VM, Helmerhorst FM, Algra A, et al. Oral contraceptives and the risk of myocardial infarction. N Engl J Med 2001;345:1787-93. [DOI] [PubMed]
- 6.Wilkins K, Johansen H, Beaudet MP, Neutel CI. Oral contraceptive use. Health Rep 2000; 11 (4): 25-37. [PubMed]
- 7.Rosenberg L, Palmer JR, Rao RS, Shapiro S. Low-dose oral contraceptive use and the risk of myocardial infarction. Arch Intern Med 2001; 161: 1065-70. [DOI] [PubMed]


