Abstract
This study aims to examine the effectiveness of chair yoga therapy on improving functional status and daily life activity scores in older female adults with knee osteoarthritis living in the community. A quasi-experimental design was adopted. In total, 85 female participants with knee osteoarthritis were assigned to the chair yoga therapy intervention group (n = 43) or the comparison (n = 42) group. A 12-week chair yoga exercise program was provided to the intervention group two times per week from January to April 2020. The primary outcomes, which include changes in physical functional ability, body mass index, and biophysiological indicators, were evaluated for all participants in the pre- and post-measures time periods. The analysis shows that the participants had a significantly higher level of functional fitness and daily life activity scores after the chair yoga intervention. This finding indicates that the chair yoga program was effective in improving the functional fitness and daily life activity scores of community-dwelling elderly females with knee osteoarthritis.
Keywords: effect, chair yoga therapy, knee osteoarthritis, functional fitness, daily life activities
1. Introduction
The rapid growth of the geriatric population is a prevalent phenomenon worldwide [1]. Aging accelerates the deterioration of physiological and psychological health, resulting in increased occurrences of falls, morbidity, depression, neuro-related diseases, and mortality [2]. These age-related diseases lead to dependence, disability, and a poor quality of life, which worsen the severity and complexity of diseases. Recently, osteoarthritis has rapidly increased due to aging populations, with a worldwide prevalence of 22.9% among individuals aged 40 years or over [3]. In Taiwan, the current prevalence of osteoarthritis among the older population is about 37% in individuals over 50 years old [4]. Among degenerative diseases, osteoarthritis is the major cause of long-term disability among older adults in Taiwan, affecting 3.45 million people [5]. The etiology of osteoarthritis consists of aging, occupational injury, chronic inflammation, a history of trauma, hereditary factors, and obesity, with approximately one-third of the elderly population suffering from injury, pain, and discomfort [6]. Women have a significantly higher risk of osteoarthritis than men, especially in the postmenopausal period. Pains in the knee and hip joints, namely, knee osteoarthritis and hip fracture, are the chief complaints from osteoarthritis patients. In addition, osteoarthritis is accompanied by pain, stiffness, and reduced physical functions, leading to limitations in walking capacity and physical activity, as well as decrements in the activities of daily living (ADL) [7,8,9]. The restrictive capacity of knee osteoarthritis increases the risk of geriatric symptoms and disease, including falling, emotional problems, lower quality of life, and psychosocial distress [10,11].
Exercise is a core nonpharmacological therapy approach for managing osteoarthritis problems, decreasing stiffness, and increasing joint stability and mobility. The effects of exercise improve functional ability in knee osteoarthritis. Participating in isokinetic and eccentric contraction exercise programs, land-based exercises, and flexibility exercises is recommended for training knee osteoarthritis, with benefits such as strengthening the muscles around the knee, including the quadriceps, lateral knee muscle, and hamstring muscle [12,13]. Yoga practice builds muscle strength, improves joint flexibility, and increases the degree of motion, strengthening muscles, imparting flexibility, and improving physical balance [14]. Regular exercise has numerous mental health benefits for older adults [15]. Numerous evidence-based randomized home-visit trials have shown the benefits of exercise interventions, such as aerobic, resistance, or mind–body exercise [16]. The effectiveness of multiple-fitness training reduces the risk of frailty, disability, and morbidity in all ages [10,17,18]. Furthermore, low-impact exercise has positive effects on reducing pain and tenderness from knee osteoarthritis as well as improving physical function and range of motion [19].
Yoga is a low-impact and moderate-intensity exercise characterized by its slowness, training of core muscles, flexibility, physical coordination, non-competitiveness, and ease of access; therefore, yoga is highly recommended as an exercise program for the elderly to improve their fitness [9,18,20]. Previous studies have demonstrated the positive relationship between regular engagement with yoga and health outcomes in terms of reducing blood pressure and fall-related injury, enhancing mobility, and reducing depression and stress. Moonaz et al. suggested that yoga is a better type of exercise for older people with arthritic hips, improving muscle strength, joint flexibility, and physical balance compared with a comparison group [21]. Nevertheless, the reported effects of yoga on knee osteoarthritis are inconsistent. Traditional yoga is similar to static stretching, which includes spinal/leg flexion and rotation while standing or lying on the floor, and those poses may discourage the elderly from participating in the relatively risky exercise [22,23]. However, yoga is not merely a form of exercise that strengthens muscles, imparts flexibility, or improves physical balance; it also positively affects the mental and spiritual domains of health. The provision of regular yoga exercise in community settings can improve the flexibility and physical coordination of older adults with osteoarthritis. Chair yoga exercise, supported by chair equipment, provides a relatively safe and stable environment for the elderly with osteoarthritis to enhance their muscle endurance and flexibility compared with yoga in a standing pose [17,22,24].
Findings from two intervention studies have shown that chair yoga therapy can reduce depression and pain and increase life satisfaction in older adults with osteoarthritis [11,25]. However, not many chair yoga intervention studies have been performed to date. Knee osteoarthritis is common in older female adults, and it is regarded as a serious health issue for those with a previous history of falls or who are living without a caretaker [11,19,22,23,25,26]. For these reasons, we study chair yoga as a culturally acceptable method to develop a functional fitness and daily life activity improvement strategy for older female adults with osteoarthritis. An expressive chair yoga therapy intervention, which has not yet been tested in Taiwan, can be tailored to the needs, predispositions, and preferences of older female adults with knee osteoarthritis, improving their functional fitness and daily life activity scores. Therefore, the purpose of this study is to explore the effects of chair yoga therapy interventions on the functional fitness and daily life activity scores of older female adults with knee osteoarthritis in Taiwan.
2. Methods
2.1. Study Design and Procedure
Quasi-experimental research is conducted in southern Taiwan with a sample population of older female adults with knee osteoarthritis who are more than 65 years of age. Two communities were selected as study sites to recruit participants. To avoid bias, the two communities were assigned to either the comparison or intervention group using a random number generator. The recruitment activities took place in the two communities on the same day. Subsequently, the participants completed a form to consent to their involvement in the study. The inclusion criteria for this study were as follows: (a) woman aged 65 years old or above; (b) self-reported history of knee osteoarthritis diagnosed by physicians; (c) capable of mobility with assistive devices; (d) limited in participating in any kinds of standing exercise; and (e) currently not participating in chair yoga or an exercise program and has not participated in any other exercise research projects during past six months. Moreover, participants with the following conditions were excluded from the study: diagnosis of dementia, disabilities, or incapability of communication. Participants in the intervention group received additional structured chair yoga therapy sessions. The comparison group participated in regular activities in the community and received the same scale tests at the same time points as the intervention group. This study assessed and compared changes in the functional fitness scores of participants in each group using a senior functional fitness test at 12 weeks from the baseline. It also assessed the change in the IADL of participants at 12 weeks from the baseline.
Sample size calculation was based on the hypothesis to estimate the mean difference between the two independent groups (intervention and comparison) using an independent t-test. The inputs for sample size calculation (G*Power software) were effect size (d) = 0.8, two-sided alpha error = 0.05, power = 0.8, and allocation ratio = 1 [27]. The sample size in each group was 36 participants, with a total sample size of 72 study participants. Of the 89 potential subjects who were screened, 85 were enrolled and assigned to the intervention (n = 43) or comparison group (n = 42).
2.2. Research Instrument
A senior functional fitness test developed by Rikli and Jones (2013) was used to assess physical statuses [17]. The 7-item senior functional fitness test was administered through interviews and assessed independent lower- and upper-body strength, aerobic endurance, lower- and upper-body flexibility, and agility/dynamic balance. Two professional research assistants conducted the measurements. All tests were conducted with strict adherence to the senior fitness test instruction manual [28]. All measures were test–retested, and the best value for each test was recorded for analysis. The intraclass correlation coefficient values for all tests were higher than 0.98 in this study.
The structured questionnaire adopted in this study comprised demographic questions (e.g., age, education, and number of chronic diseases), and a Chinese version of the Lawton Instrumental Daily Living Scale (IADL) was used to assess eight primary and psychological functions [29]. The IADL scale is used to identify how an elderly subject carries out daily activities, recording improvements or deterioration over time [30]. It was originally designed to monitor prognosis and treatment in chronically ill elderly patients; however, it is now being used to evaluate the independent abilities of older adults in a wide range of settings. Its summary score ranges from 9 to 20 points, with a score of 20 meaning they are independent and a score of 9 meaning they need assistance or supervision in performing tasks. The Chinese version of the scale was reported to have established validity and reliability [31]. Cronbach’s alpha for the IADL used in this study was 0.89, demonstrating good internal consistency.
2.3. Chair Yoga Intervention Technique
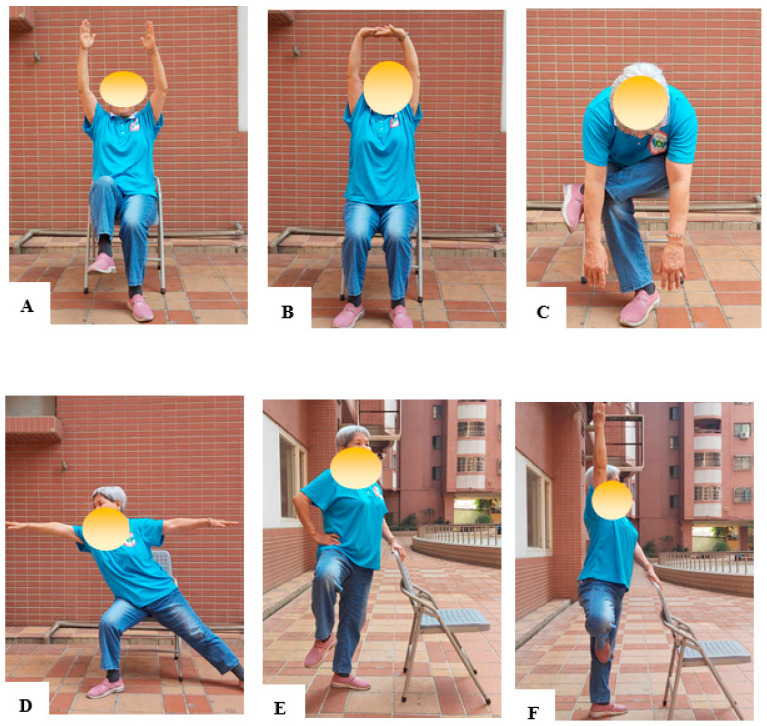
The chair yoga program was designed based on the results of a previous study [32]. The program development included a preliminary review and evaluated content validity using an index created by a panel of five geriatric experts in the fields of nursing, occupational therapy, geriatric medicine, and long-term care. Table 1 provides a brief explanation of the content of the chair yoga therapy activities. Trained yoga personnel from the institute conducted 110-min sessions of chair yoga intervention. Such sessions were held twice weekly for a duration of 12 weeks. Most of the yoga postures were completed in a sitting posture. This was followed by a few standing postures, and during the final posture, participants were again seated to rest and breathe. The chair yoga intervention focuses on balance and postures that ultimately improve confidence and build the physical functions of older adults in the community, such as muscle strength, flexibility, and balance capabilities. The classes emphasized breathing throughout all postures. Additionally, yoga postures were appropriately modified in case of disease-related complications or any other critical issue after discussion with the yoga instructor. Examples of chair yoga training are shown in Figure 1. The chair yoga program is demonstrated in Youtube videos [33].
Table 1.
Content of the chair yoga therapy activities.
| Time | Session | Activity Content |
|---|---|---|
| 15 min | Warm-up activities |
|
| 50 min | Main course (1) |
|
| 10 min | Break | Break |
| 20 min | Main course (2) | Balance training while standing (a total of six movements, including down dog while standing, lifting the knees while standing, and the tree pose) |
| 15 min | Cooling down and relaxation |
|
Figure 1.
The various chair yoga positions performed by participants are shown in this figure. Some examples are (A) reaching both arms forward and waving them up and down, (B) seated mountain pose, (C) down dog with chair, (D) hero pose, (E) Lifting the knees while standing, (F) tree pose.
2.4. Ethical Considerations
All participants provided written consent. No identifying personal data are included in this paper. This study was approved by the appropriate institutional review board (National Cheng Kung University, Taiwan). Approval for this study was obtained on 10 March 2020 via letter number NCKU-IRB-2020-207. All study-related documents along with a detailed protocol have been submitted to NCKU. Any changes in protocol and protocol deviations or violations were reported by investigators of NCKU.
2.5. Statistical Analysis
Data analysis was performed in SPSS software (version 24.0, IBM). The continuous variable was reported as mean ± standard deviation based on the distribution of data. The data normality test was carried out from the pre- and post-test functional fitness and daily life activity scores. The normality test value shows a normal distribution because the significance value (p) of the Kolmogorov–Smirnov test is >0.05. In this study, t-tests or an ANOVA analysis of variance were used for comparing continuous variables among or between subgroups. An ANOVA analysis of covariance was also used to compare functional fitness and daily life activity scores between the groups when scores differed significantly at baseline. Statistical significance was considered if the p-value was less than 0.05 at 95% confidence.
3. Results
3.1. Demographics of Participants
In this study, 89 participants met the criteria, and 4 participants withdrew from the program without any notice. Thus, a total of 85 participants, including 43 in the intervention group and 42 in the comparison group, completed all parts of the study. The mean age of the participants was 77.52 ± 6.15 years. In total, 41.65% of participants were illiterate, and the participants had an average of 1.46 types of chronic diseases. Overall, no substantial difference between the two groups was observed. Table 2 shows the demographic characteristics of the study participants.
Table 2.
Demographic characteristics of study participants in the intervention and comparison groups at baseline.
| Variables | Intervention (n = 43) | Comparison (n = 42) | t | X 2 | p | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| M | SD | n | % | M | SD | n | % | ||||
| Age (years old) | 76.37 | 6.08 | 78.66 | 6.18 | −1.03 | 0.306 | |||||
| Education (degree) | 4.37 | 0.225 | |||||||||
| Illiterate | 15 | 34.9 | 21 | 50.0 | |||||||
| Elementary | 18 | 41.9 | 18 | 42.9 | |||||||
| Junior high school | 7 | 16.3 | 0 | 0 | |||||||
| ≥Senior high school | 3 | 7.0 | 3 | 7.1 | |||||||
| Number of chronic diseases (number) | 1.57 | 0.93 | 1.35 | 1.39 | 0.51 | 0.608 | |||||
| DBP (mmHg) | 137.02 | 14.75 | 137.83 | 15.69 | −0.137 | 0.889 | |||||
| SBP (mmHg) | 72.46 | 13.26 | 67.70 | 10.32 | 1.01 | 0.317 | |||||
| HR (bpm) | 75.65 | 10.61 | 75.10 | 6.77 | 0.14 | 0.880 | |||||
| BMI (kg/m2) | 24.81 | 3.11 | 25.69 | 3.82 | −0.707 | 0.486 | |||||
| Hand grip strength (kg) | 17.80 | 2.72 | 15.88 | 3.40 | 1.72 | 0.093 | |||||
| Lower-limb muscle strength (time/30 s) | 8.20 | 2.62 | 7.70 | 2.83 | 0.57 | 0.554 | |||||
| Upper-limb muscle strength (time/30 s) | 12.58 | 2.82 | 12.38 | 2.13 | 0.21 | 0.824 | |||||
| Static balance (degree) | 7.71 | 8.26 | 3.81 | 3.88 | 1.43 | 0.161 | |||||
| Agility and dynamic balance (degree) | 9.83 | 3.20 | 11.58 | 4.28 | −1.01 | 0.316 | |||||
| Lower-limb flexibility (cm) | −0.92 | 10.60 | −4.46 | 11.40 | 0.90 | 0.378 | |||||
| Upper-limb flexibility (cm) | −13.87 | 17.29 | −7.40 | 13.48 | −1.16 | 0.257 | |||||
| Daily life activities (degree) | 20.15 | 4.13 | 22.01 | 5.12 | 0.60 | 0.11 | |||||
Note. DBP = diastolic blood pressure; SBP = systolic blood pressure; HR = heart rate; BMI = body mass index.
3.2. Differences in Functional Fitness and Daily Life Activities of the Two Groups
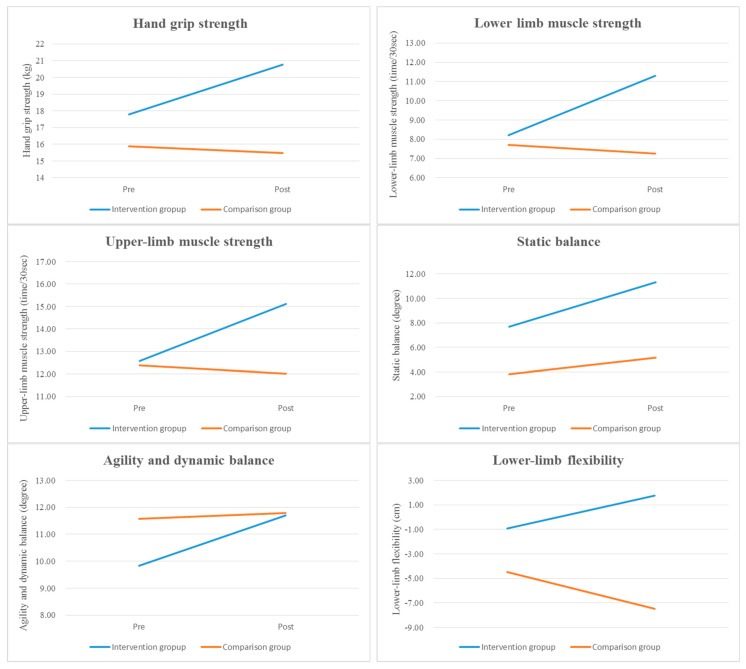
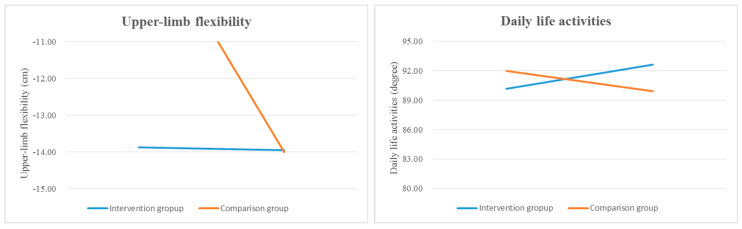
The results of between-group comparisons in functional fitness and daily life activity scores are shown in Table 3 and Figure 2. Hand grip strength, lower- and upper-limb muscle strength, static balance, agility and dynamic balance, lower-limb flexibility, and daily life activities significantly improved in the intervention group when compared with the comparison group at post-test (all p < 0.001), and there was a statistically significant difference in the scores of the intervention group (Scheffe’s test result: ① > ②). However, no significant between-group differences were observed for upper-limb flexibility at post-test (p = 0.965). Moreover, the chair yoga activity program considerably increased the participants’ daily life activity scores, with the Cohen’s d effect size of the intervention being 3.06.
Table 3.
Group comparisons in changes in functional fitness and daily life activities.
| Variables | Pre-Test | Post-Test | Estimate (β) | SE | Wald χ2 | p | 95% CI | Scheffé | |
|---|---|---|---|---|---|---|---|---|---|
| M ± SD | M ± SD | LL | UL | ||||||
| Hand grip strength | |||||||||
| ①Intervention | 17.80 ± 2.72 | 20.75 ± 3.72 | |||||||
| ②Comparison | 15.88 ± 3.40 | 15.47 ± 3.94 | |||||||
| Intercept | 15.88 | 0.75 | 16.89 | <0.001 *** | 14.36 | 21.34 | |||
| Pre (I/C) a | −0.76 | 1.05 | −0.73 | 0.463 | −2.82 | 1.27 | |||
| Intervention (post/pre) b | −1.02 | 0.19 | −5.27 | <0.001 *** | −1.43 | −0.64 | |||
| Group difference from pre to post c | 2.09 | 0.31 | 6.52 | <0.001 *** | 1.46 | 2.73 | ① > ② | ||
| Lower-limb muscle strength | |||||||||
| ①Intervention | 8.20 ± 2.62 | 11.30 ± 4.33 | |||||||
| ②Comparison | 7.70 ± 2.83 | 7.26 ± 2.71 | |||||||
| Intercept | 7.70 | 0.39 | 2.64 | <0.001 *** | 6.27 | 12.78 | |||
| Pre (I/C) a | −0.02 | 0.50 | −0.05 | 0.861 | −1.01 | 0.95 | |||
| Intervention (post/pre) b | −0.06 | 0.15 | −0.48 | 0.001 ** | −0.27 | 0.25 | |||
| Group difference from pre to post c | 0.19 | 0.32 | 0.58 | <0.001 *** | 0.46 | 0.93 | ① > ② | ||
| Upper-limb muscle strength | |||||||||
| ①Intervention | 12.58 ± 2.82 | 15.12 ± 5.09 | |||||||
| ②Comparison | 12.38 ± 2.13 | 12.02 ± 3.45 | |||||||
| Intercept | 12.38 | 0.56 | 10.25 | <0.001 *** | 11.43 | 16.14 | |||
| Pre (I/C) a | −0.47 | 0.25 | −1.87 | 0.482 | −0.98 | 0.04 | |||
| Intervention (post/pre) b | −1.28 | 0.43 | −2.98 | 0.003 ** | −2.12 | −0.45 | |||
| Group difference from pre to post c | 2.23 | 0.48 | 4.64 | <0.001 *** | 1.28 | 3.15 | ① > ② | ||
| Static balance | |||||||||
| ①Intervention | 7.71 ± 8.26 | 11.32 ± 9.92 | |||||||
| ②Comparison | 3.81 ± 3.88 | 5.17 ± 4.89 | |||||||
| Intercept | 3.81 | 0.87 | 8.70 | <0.001 *** | 3.27 | 12.54 | |||
| Pre (I/C) a | −1.14 | 4.37 | −0.26 | 0.793 | −6.71 | 5.42 | |||
| Intervention (post/pre) b | −0.76 | 0.23 | −3.30 | 0.001 ** | −1.21 | −0.31 | |||
| Group difference from pre to post c | 3.87 | 0.72 | 5.31 | <0.001 *** | 2.44 | 5.29 | ① > ② | ||
| Agility and dynamic balance | |||||||||
| ①Intervention | 9.83 ± 3.20 | 11.70 ± 2.25 | |||||||
| ②Comparison | 11.58 ± 4.28 | 11.78 ± 4.13 | |||||||
| Intercept | 11.58 | 3.06 | 0.70 | <0.001 *** | 8.93 | 12.86 | |||
| Pre (I/C) a | 2.15 | 3.06 | 0.70 | 0.825 | −3.82 | 7.14 | |||
| Intervention (post/pre) b | −1.62 | 0.35 | −4.38 | <0.001 *** | −2.19 | 0.93 | |||
| Group difference from pre to post c | 5.32 | 1.47 | 3.65 | <0.001 *** | 2.31 | 8.24 | ① > ② | ||
| Lower-limb flexibility | |||||||||
| ①Intervention | −0.92 ± 10.60 | 1.75 ± 7.93 | |||||||
| ②Comparison | −4.46 ± 11.40 | −7.46 ± 10.67 | |||||||
| Intercept | −4.46 | 3.25 | 0.80 | <0.001 *** | −8.25 | 2.38 | |||
| Pre (I/C) a | −4.24 | 4.56 | −0.99 | 0.320 | −12.28 | 3.41 | |||
| Intervention (post/pre) b | −1.22 | 0.87 | −1.40 | 0.001 ** | −2.91 | 0.79 | |||
| Group difference from pre to post c | 6.01 | 1.62 | 3.70 | <0.001 *** | 2.83 | 9.19 | ① > ② | ||
| Upper-limb flexibility | |||||||||
| ①Intervention | −13.87 ± 17.29 | −13.95 ± 15.92 | |||||||
| ②Comparison | −7.40 ± 13.48 | −14.00 ± 16.74 | |||||||
| Intercept | −7.40 | 0.39 | 2.65 | 0.006 ** | −15.53 | −5.83 | |||
| Pre (I/C) a | −0.02 | 0.50 | −0.05 | 0.961 | −1.01 | 0.96 | |||
| Intervention (post/pre) b | −0.03 | 0.09 | −0.26 | 0.792 | −0.18 | 0.15 | |||
| Group difference from pre to post c | −0.01 | 0.17 | −0.04 | 0.965 | −0.33 | 0.46 | |||
| Daily life activities | |||||||||
| ①Intervention | 90.15 ± 4.13 | 92.63 ± 0.40 | |||||||
| ②Comparison | 92.01 ± 5.12 | 89.92 ± 0.47 | |||||||
| Intercept | 92.01 | 3.84 | 3.92 | <0.001 *** | 87.22 | 94.29 | |||
| Pre (I/C) a | −3.02 | 5.18 | −0.57 | 0.562 | −13.15 | 7.12 | |||
| Intervention (post/pre) b | −2.80 | 1.07 | −2.61 | <0.001 *** | −4.90 | 0.71 | |||
| Group difference from pre to postc | 9.62 | 2.03 | 4.74 | <0.001 *** | 5.65 | 12.62 | ① > ② | ||
Note. CI = confidence interval; LL = lower limit; UL = upper limit; I = intervention group; C = comparison group; Pre = pre-test; Post = post-test. a Reference group: Comparison; b Reference group: Pre-test; c Reference group: Comparison × Pre-test. ** p < 0.01; *** p < 0.001.
Figure 2.
Time−dependent tendencies in functional fitness and daily life activities for the two groups. Note. Pre = pre-test; Post = post-test.
4. Discussion
This study explores the effects of chair yoga therapy interventions on the functional fitness and daily life activities of older female adults with knee osteoarthritis in communities in Taiwan. According to the outcome, this study shows that implementing the chair yoga program regularly for 12 weeks, two times a week, effectively improved functional fitness and daily life activity scores. The chair yoga program involved swinging the arms in natural parabolas, along with repeated supporting movements, resulting in muscle contractions, which improved muscle strength and endurance. Previous studies have shown similar results, namely, that chair yoga exercises increase both upper- and lower-extremity muscle strength [34,35,36]. Park et al. performed a pilot study on a retirement community and found that agility and dynamic balance increased by 10.43% after yoga therapy intervention during a 12-week period, indicating that chair yoga may be a promising intervention to manage functional fitness and improve daily life activities, thereby reducing fall risk for older female adults with knee osteoarthritis [26]. In another study, Niemelä et al. and Kertapati et al. reported significant changes in both knee extension and quadriceps strength [37,38]. Furthermore, Baum et al. reported significant changes in physical performance after 26 weeks of chair yoga exercise [39]. Based on the conclusions of these studies, chair yoga can potentially mitigate the functional fitness problem in older adults with knee osteoarthritis [32,40,41,42]. Moreover, when combining regular breathing with upper- and lower-limb stretching, blood circulation and oxygen uptake can be facilitated, leading to improvements in functional fitness. Therefore, chair yoga enhances muscular strength, body flexibility, and respiratory function. The positive effects we observed for static and dynamic balance, agility, and lower- and upper-limb muscle strength were similar to those reported by Cheung et al. (2017) and Park et al. (2017), indicating that chair yoga can enhance balance and physical function [26,43].
Furthermore, the effect of chair yoga therapy has also been evaluated regarding its improvements in daily life activities among older female adults with knee osteoarthritis, and in the long term, it can prevent falls or the fear of falling as well as their possible complications. It also helps older adults to enhance their muscles and body flexibility, reduce stress, depression, and chronic pain, and enhance overall well-being and quality of life, meaning that such an intervention increases the daily life activity scores in older adults. Overall, our study results suggest that the implementation of a chair yoga program enhances daily life activity scores among older community-dwelling female adults with knee osteoarthritis. Our study results also resonate with the findings of prior research—chair yoga therapy had a positive short-term effect in increasing daily life activity scores [44]. Moreover, the chair yoga program uses stretching and flexion movements to extend the spine, back, and thighs, which can improve function and daily life activity scores. This finding was similar to a previous report suggesting that balneotherapy improved functional limitations and ameliorated the quality of life [45]. Currently, one of the most frequently prescribed nonpharmacological treatments for osteoarthritis diseases is balneotherapy [46], and it can be combined with different treatment modalities, such as massage, exercise, and health education [47].
Chair yoga exercises complement and add value to existing therapy, improving functional fitness. Balance control yoga exercises are taught in clinical practice because yoga actively engages the mind and body. Yoga exercises result in considerable improvements in the balance and daily life activity scores of older female adults. Balance and daily life activity problems for the elderly with knee osteoarthritis have always been a field of concern for comprehensive geriatric care because, often due to associated multi-morbidities, they lead to high-cost intervention and management, which can result in neglect, further deteriorating the functional status of the elderly population. Owing to such concerns, our study proposes chair yoga exercises as an effective means to improve functional fitness problems and daily life activity scores in the elderly through a more culturally acceptable form of exercise. Involving psychosocial, emotional, and physical functions during chair yoga can improve quality of life, which has been one of the prime aims of elderly long-term care amongst geriatricians.
However, this study has several limitations that must be acknowledged. First, because of community limitations in cooperation, this study was quasi-experimental, which may limit the external validity. Randomized controlled trials could be used to measure the effectiveness of the chair yoga intervention. Second, the intervention was implemented in the community; therefore, the results cannot be generalized to other long-term care institutions. Third, the study outcome was measured based on the pre- and post-test results obtained after the twelve-week intervention. Future studies should consider collecting follow-up data and designing a series study to examine the relationship between the intervention frequency and duration of the chair yoga program. Fourth, there were limitations with this study due to the small sample size, and future studies are needed to explore the other potential benefits of different chair yoga programs for older female adults. Fifth, this study did not include male subjects as a sample population. Future studies must develop interventions with multiple modalities and invite community agencies and leaders to cooperate as partners in implementing health-promoting activities to ensure maximum efficacy.
5. Conclusions
Our study’s goal was to apply chair yoga therapy for the nonpharmacologic management of knee osteoarthritis in older community-dwelling female adults. Chair yoga therapy is a feasible and effective intervention for older female adults with knee osteoarthritis, with beneficial effects on functional fitness and daily life activity scores. The WHO recommends the adaptation of interventions based on individual physical capacities to improve healthy aging. Thus, interventions with chair yoga therapy can enable older adults with knee osteoarthritis to adopt and practice the therapy at home as part of their daily life, lessening the risk of their disease progressing to disability.
Acknowledgments
The authors acknowledge all those who provided help for data collection.
Author Contributions
All authors made significant contributions to the preparation and intellectual content of this manuscript. H.H. and Y.-C.S. made substantial contributions to the conception or design of the work. B.-O.L. and C.-T.Y. made substantial contributions to the acquisition, analysis, and/or interpretation of data. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
The Institutional Review Board and the Research Ethics Committee of the National Cheng Kung University, Taiwan (NCKU-IRB-2020-207), approved the study.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The data of the current study are available from the corresponding author upon reasonable request.
Conflicts of Interest
The authors declare no conflict of interest.
Funding Statement
This research received no external funding.
Footnotes
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
References
- 1.United Nations . World Population Prospects The 2017 Revision. United Nations; New York, NY, USA: 2017. [Google Scholar]
- 2.Preston J., Biddell B. The physiology of ageing and how these changes affect older people. Medicine. 2021;49:1–5. doi: 10.1016/j.mpmed.2020.10.011. [DOI] [Google Scholar]
- 3.Cui A., Li H., Wang D., Zhong J., Chen Y., Lu H. Global, regional prevalence, incidence and risk factors of knee osteoarthritis in population-based studies. EClinicalMedicine. 2020;29:100587. doi: 10.1016/j.eclinm.2020.100587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lin F.H., Chen H.C., Lin C., Chiu Y.L., Lee H.S., Chang H., Huang G.S., Chang H.L., Yeh S.J., Su W., et al. The increase in total knee replacement surgery in Taiwan: A 15-year retrospective study. Medicine. 2018;97:e11749. doi: 10.1097/MD.0000000000011749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lu M.C., Liu K.C., Lai N.S., Koo M. Higher incidence of rheumatoid arthritis in patients with symptomatic osteoarthritis or osteoarthritis-related surgery: A nationwide, population-based, case–control study in Taiwan. BMJ Open. 2015;5:e008513. doi: 10.1136/bmjopen-2015-008513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Man-Ger S.M., Beier F., Pest M.A. Recent developments in emerging therapeutic targets of osteoarthritis. Curr. Opin. Rheumatol. 2017;29:96–102. doi: 10.1097/BOR.0000000000000351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Felson D.T., Gale D.R., Gale M.E., Niu J., Hunter D.J., Goggins J., Lavalley M.P. Osteophytes and progression of knee osteoarthritis. Rheumatology. 2005;44:100–104. doi: 10.1093/rheumatology/keh411. [DOI] [PubMed] [Google Scholar]
- 8.Tew G.A., Howsam J., Hardy M., Bissell L. Adapted yoga to improve physical function and health-related quality of life in physically inactive older adults: A randomised controlled pilot trial. BMC Geriatr. 2017;17:131. doi: 10.1186/s12877-017-0520-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Noradechanunt C., Worsley A., Groeller H. Thai yoga improves physical function and well-being in older adults: A randomised controlled trial. J. Sci. Med. Sport. 2017;20:494–501. doi: 10.1016/j.jsams.2016.10.007. [DOI] [PubMed] [Google Scholar]
- 10.Rydwik E., Frändin K., Akner G. Effects of a physical training and nutritional intervention program in frail elderly people regarding habitual physical activity level and activities of daily living-A randomized controlled pilot study. Arch. Gerontol. Geriatr. 2010;51:283–289. doi: 10.1016/j.archger.2009.12.001. [DOI] [PubMed] [Google Scholar]
- 11.Park J., McCaffrey R., Newman D., Cheung C., Hagen D. The effect of Sit ‘N’ Fit chair yoga among community-dwelling older adults with osteoarthritis. Holist. Nurs. Pract. 2014;28:247–257. doi: 10.1097/HNP.0000000000000034. [DOI] [PubMed] [Google Scholar]
- 12.Hammami N., Jdidi H., Khezami M.A., Ghidaoui L., Talbi A., Hannachi C., Farinha P.M., Behlouli E., Bouassida A., Dziri C., et al. Isokinetic strengthening and neuromuscular electrical stimulation protocol impact on physical performances, functional status and quality of life in knee osteoarthritis overweight/obese women. Knee. 2022;39:106–115. doi: 10.1016/j.knee.2022.09.004. [DOI] [PubMed] [Google Scholar]
- 13.Coudeyre E., Jegu A.G., Giustanini M., Marrel J.P., Edouard P., Pereira B. Isokinetic muscle strengthening for knee osteoarthritis: A systematic review of randomized controlled trials with meta-analysis. Ann. Phys. Rehabil. Med. 2016;59:207–215. doi: 10.1016/j.rehab.2016.01.013. [DOI] [PubMed] [Google Scholar]
- 14.Bull F.C., Al-Ansari S.S., Biddle S., Borodulin K., Buman M.P., Cardon G., Carty C., Chaput J.-P., Chastin S., Chou R., et al. World Health Organization 2020 guidelines on physical activity and sedentary behaviour. Br. J. Sports Med. 2020;54:1451–1462. doi: 10.1136/bjsports-2020-102955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kazeminia M., Salari N., Vaisi-Raygani A., Jalali R., Abdi A., Mohammadi M., Daneshkhah A., Hosseinian-Far M., Shohaimi S. The effect of exercise on anxiety in the elderly worldwide: A systematic review and meta-analysis. Health Qual. Life Outcomes. 2020;18:363. doi: 10.1186/s12955-020-01609-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Zhao J.L., Jiang W.T., Wang X., Cai Z.D., Liu Z.H., Liu G.R. Exercise, brain plasticity, and depression. CNS Neurosci. Ther. 2020;26:885–895. doi: 10.1111/cns.13385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Rikli R.E., Jones C.J. Development and validation of criterion-referenced clinically relevant fitness standards for maintaining physical independence in later years. Gerontologist. 2013;53:255–267. doi: 10.1093/geront/gns071. [DOI] [PubMed] [Google Scholar]
- 18.Halder K., Chatterjee A., Pal R., Tomer O.S., Saha M. Age related differences of selected Hatha yoga practices on anthropometric characteristics, muscular strength and flexibility of healthy individuals. Int. J. Yoga. 2015;8:37–46. doi: 10.4103/0973-6131.146057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Furtado G., Uba-Chupel M., Carvalho H., Souza N., Ferreira J., Teixeira A. Effects of a chair-yoga exercises on stress hormone levels, daily life activities, falls and physical fitness in institutionalized older adults. Complement. Clin. Pract. 2016;24:123–129. doi: 10.1016/j.ctcp.2016.05.012. [DOI] [PubMed] [Google Scholar]
- 20.Cramer H., Ward L., Saper R., Fishbein D., Dobos G., Lauche R. The safety of yoga: A systematic review and meta-analysis of randomized controlled trials. Am. J. Epidemiol. 2015;182:281–293. doi: 10.1093/aje/kwv071. [DOI] [PubMed] [Google Scholar]
- 21.Moonaz S.H., Bingham C.O., Wissow L., Bartlett S.J. Yoga in sedentary adults with arthritis: Effects of a randomized controlled pragmatic trial. J. Rheumatol. 2015;42:1194–1202. doi: 10.3899/jrheum.141129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Marques M., Chupel M.U., Furtado G.E., Minuzzi L.G., Rosado F., Pedrosa F., Ferreira J.P., Teixeira A.M. Influence of chair-based yoga on salivary anti-microbial proteins, functional fitness, perceived stress and well-being in older women: A pilot randomized controlled trial. Eur. J. Integr. Med. 2017;12:44–52. doi: 10.1016/j.eujim.2017.04.008. [DOI] [Google Scholar]
- 23.Karydaki M., Dimakopoulou E., Margioti E., Lyras V., Apostolopoulos X., Papagianni M., Vlachogianni A., Theodorelou M., Sakka P. Comparison of resistance and chair yoga training on subjective sleep quality in MCI women. Int. J. Kinesiol. Sports Sci. 2017;5:26–34. doi: 10.7575/aiac.ijkss.v.5n.1p.26. [DOI] [Google Scholar]
- 24.Lien T.C., Cheng H.F. The development of the well-being scale for elders in Taiwan. Guid. Q. 2015;51:29–37. [Google Scholar]
- 25.Mooventhan A., Nivethitha L. Evidence based effects of yoga practice on various health related problems of elderly people: A review. J. Bodyw. Mov. Ther. 2017;21:1028–1032. doi: 10.1016/j.jbmt.2017.01.004. [DOI] [PubMed] [Google Scholar]
- 26.Park J., McCaffrey R., Newman D., Liehr P., Ouslander J.G. A pilot randomized controlled trial of the effects of chair yoga on pain and physical function among community-dwelling older adults with lower extremity osteoarthritis. J. Am. Geriatr. Soc. 2017;65:592–597. doi: 10.1111/jgs.14717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hsiao C.Y., Chen K.M., Tsai H.Y., Huang H.T., Cheng Y.Y., Tsai A.Y. Self-perceived health and sleep quality of community older adults after acupunch exercises. Am. J. Geriatr. Psychiatr. 2018;26:511–520. doi: 10.1016/j.jagp.2018.01.199. [DOI] [PubMed] [Google Scholar]
- 28.Rikli R.E., Jones C.J. Senior Fitness Test Manual. 2nd ed. Human Kinetics; Champaign, IL, USA: 2013. [Google Scholar]
- 29.Graf C. The Lawton instrumental activities of daily living scale. Am. J. Nurs. 2008;108:52–62. doi: 10.1097/01.NAJ.0000314810.46029.74. [DOI] [PubMed] [Google Scholar]
- 30.Fredman L., Ranker L.R., Strunin L., Smith M.L., Applebaum K.M. Caregiving intensity and mortality in older women, accounting for time-varying and lagged caregiver status: The caregiver-study of osteoporotic fractures study. Gerontologist. 2019;59:e461–e469. doi: 10.1093/geront/gny135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Liao W.L., Chang Y.H. Age trajectories of disability in instrumental activities of daily living and disability-free life expectancy among middle-aged and older adults in Taiwan: An 11-year longitudinal study. BMC Geriatr. 2020;20:530. doi: 10.1186/s12877-020-01939-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Yao C.T., Tseng C.H. Effectiveness of chair yoga for improving the functional fitness and well-being of female community-dwelling older adults with low physical activities. Top. Geriatr. Rehabilit. 2019;35:248–254. doi: 10.1097/TGR.0000000000000242. [DOI] [Google Scholar]
- 33.Yao C.T., Shen L.W., Tseng C.H., Lin Y.M. Increase Muscle Strength: Chair Yoga for Older Adults [Video]. YouTube. 2018. [(accessed on 8 March 2023)]. Available online: https://www.youtube.com/watch?v=UsgdEdJFyYE.
- 34.Sousa N., Mendes R., Abrantes C., Sampaio J., Oliveira J. Effectiveness of combined exercise training to improve functional fitness in older adults: A randomized controlled trial. Geriatr. Gerontol. Int. 2014;14:892–898. doi: 10.1111/ggi.12188. [DOI] [PubMed] [Google Scholar]
- 35.Gothe N.P., McAuley W. Yoga is as good as stretching–strengthening exercises in improving functional fitness outcomes: Results from a randomized controlled trial. J. Gerontol. A Biol. Sci. Med. Sci. 2016;71:406–411. doi: 10.1093/gerona/glv127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Orr R. Contribution of muscle weakness to postural instability in the elderly. A systematic review. Eur. J. Phys. Rehabil. Med. 2010;46:183–220. [PubMed] [Google Scholar]
- 37.Niemelä K., Väänänen I., Leinonen R., Laukkanen P. Benefits of home-based rocking-chair exercise for physical performance in community-dwelling elderly women: A randomized controlled trial. Aging Clin. Exp. Res. 2011;23:279–287. doi: 10.1007/BF03337754. [DOI] [PubMed] [Google Scholar]
- 38.Kertapati Y., Sahar J., Nursasi A.Y. The effects of chair yoga with spiritual intervention on the functional status of older adults. Enferm. Clin. 2018;28:70–73. doi: 10.1016/S1130-8621(18)30040-8. [DOI] [Google Scholar]
- 39.Baum E.E., Jarjoura D., Polen A.E., Faur D., Rutecki G. Effectiveness of a group exercise program in a long-term care facility: A randomized pilot trial. J. Am. Med. Dir. Assoc. 2003;4:74–80. doi: 10.1016/S1525-8610(04)70279-0. [DOI] [PubMed] [Google Scholar]
- 40.Nguyen M.H., Kruse A. The effects of Tai Chi training on physical fitness, perceived health, and blood pressure in elderly Vietnamese. Open Access J. Sports Med. 2012;3:7–16. doi: 10.2147/OAJSM.S27329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Rieping T., Furtado G.E., Letieri R.V., Chupel M.U., Colado J.C., Hogervorst E., Filaire E., Teixeira A.M.M.B., Ferreira J.P. Effects of different chair-based exercises on slivary bomarkers and fnctional atonomy in istitutionalized older women. Res. Q. Exerc. Sport. 2019;90:36–45. doi: 10.1080/02701367.2018.1563272. [DOI] [PubMed] [Google Scholar]
- 42.Tulloch A., Bombell H., Dean C., Tiedemann A. Yoga-based exercise improves health-related quality of life and mental well-being in older people: A systematic review of randomised controlled trials. Age Ageing. 2018;47:537–544. doi: 10.1093/ageing/afy044. [DOI] [PubMed] [Google Scholar]
- 43.Cheung C., Wyman J.F., Bronas U., McCarthy T., Rudser K., Mathiason M.A. Managing knee osteoarthritis with yoga or aerobic/strengthening exercise programs in older adults: A pilot randomized controlled trial. Rheumatol. Int. 2017;37:389–398. doi: 10.1007/s00296-016-3620-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Chou C., Hwang C., Wu Y. Effect of exercise on physical function, daily living activities, and quality of life in the frail older adults: A meta-analysis. Arch. Phys. Med. Rehabil. 2012;93:237–244. doi: 10.1016/j.apmr.2011.08.042. [DOI] [PubMed] [Google Scholar]
- 45.Tognolo L., Coraci D., Fioravanti A., Tenti S., Scanu A., Magro G., Maccarone M.C., Masiero S. Clinical impact of balneotherapy and therapeutic exercise in rheumatic diseases: A lexical analysis and scoping review. Appl. Sci. 2022;12:7379. doi: 10.3390/app12157379. [DOI] [Google Scholar]
- 46.Fioravanti A. Foreword: Balneotherapy in rheumatic diseases. Int. J. Biometeorol. 2020;64:903–904. doi: 10.1007/s00484-020-01936-7. [DOI] [PubMed] [Google Scholar]
- 47.Gutenbrunner C., Bender T., Cantista P., Karagülle Z. A proposal for a worldwide definition of health resort medicine, balneology, medical hydrology and climatology. Int. J. Biometeorol. 2010;54:495–507. doi: 10.1007/s00484-010-0321-5. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data of the current study are available from the corresponding author upon reasonable request.