Abstract
Butyrate and indole-3-propionic acid represent the CNS-available gut microbiota metabolites exhibiting potentially beneficial effects on human brain function and being tested as antidepressants. Astrocytes represent one of the putative targets for the gut metabolites; however, the mechanism of action of butyrate and indole-3-propionic acid is not well understood. In order to test this mechanism, a human astrocyte cell-line culture was treated with the compounds or without them, and the supernatants were collected for the analysis of ATP and glutamate gliotransmitter release with the use of luminescent and fluorescent methods, respectively. A 10-min incubation of astrocytes with 1–5 mM butyrate increased the ATP gliotransmitter release by 78% (95%CI: 45–119%), p < 0.001. The effect was found to be mediated by the cytosolic Ca2+ mobilization. Both 10-min and 24-h treatments with indole-3-propionic acid produced no significant effects on the release of gliotransmitters. The results for glutamate release were inconclusive due to a specific glutamate release pattern discovered in the tested model. This preliminary report of butyrate-induced ATP gliotransmitter release appears to provide a novel mechanistic explanation for the beneficial effect of this gut microbiota metabolite on brain function; however, the results require further evaluation in more composed models.
Keywords: gut microbiota, probiotics, metabolites, butyrate, indole-3-propionic acid, gliotransmitters, ATP, astrocytes, antidepressant, mechanism of action
1. Introduction
Human intestines are inhabited by trillions of microorganisms being collectively called the gut microbiota, that constitute an indispensable component of the human holobiont system [1,2]. The quality of gut microbiota and their interaction with the host appear to significantly impact human development and adult physiology, also in terms of neuropsychological functioning and relevant pathology [3]. The mechanisms underlying these effects are outlined by the gut–brain axis (GBA) signaling. The GBA involves multiple pathways and messengers such as the vagus nerve [4], the hypothalamic–pituitary–adrenal axis [5], microbiota-derived neurotransmitters and their precursors [6,7], neurotrophic factors [8], the immune system [9], and bacterial metabolites [10]. The latter include a set of thousands of specific chemical compounds that reach distant tissues, including the central nervous system (CNS), and play a role in the homeostasis of the human organism [1,10,11].
Among the metabolites produced by the human gut microbiota, butyrate (BUT) and indole-3-propionic acid (IPA) are of special interest to neuropsychiatry as both are absorbed from the gastrointestinal tract, penetrate the blood–brain barrier [11], and are capable of interacting with the brain components. BUT is one type of the body’s short-chain fatty acids (SCFA), which constitute the family of major gut microbial metabolites [12]. SCFA are produced in the colon largely by the bacterial fermentation of dietary fibers and resistant starch [12,13]. BUT may interact with the brain cells by binding to free fatty acid receptors (FFAR) [10], among others, thus contributing to anti-neuroinflammatory, and consequently antidepressant and pro-cognitive, effects [14,15,16,17,18,19,20,21,22,23]. IPA is a tryptophan derivative, which is present in the human body only thanks to microbe-mediated metabolism [24]. IPA binds to aryl hydrocarbon receptor (AhR) which regulates the transcription of genes [11], leading to neuroprotective and cytokine-suppressing effects in the astrocytes [22,25]. However, the molecular mechanisms of beneficial actions of both BUT and IPA are not fully understood.
Astrocytes represent an abundant cell type in the CNS, playing a critical role in brain function [26]. Astrocytes help maintain the homeostasis of neuronal synapses. They respond to neurotransmission by releasing their own substances, called gliotransmitters, to control neuronal excitability and synaptic information-processing, thus contributing to synaptic plasticity [27], and the impairment of gliotransmission may contribute to brain pathology [28,29]. Among the well-studied gliotransmitters are adenosine 5′-triphosphate (ATP) and glutamate (Glu). Astrocyte-released ATP controls purinergic neurotransmission in a long-lasting manner. It modulates enduring changes in glutamatergic and γ-aminobutyric acid synaptic efficacy [30]. Impaired ATP release from brain astrocytes may be a cause of depressive-like behavior in several animal models [31,32,33], and ATP administration or the induction of its specific release from astrocytes results in rapid antidepressant-like effects [34]. Glu is best known as a neurotransmitter, and the astrocytes uptake synaptically released Glu to optimize neuronal function and prevent excitotoxicity [35]. However, recent scientific interests have also focused on Glu as a gliotransmitter [27,35]. Although the clinical significance of the astroglial-released Glu remains to be elucidated, it appear to synchronize excitatory and inhibitory neuronal firing, thus contributing to brain homeostasis [35].
BUT and IPA have been found to influence vitally important astrocyte functions [22,36,37,38]. However, it is unknown whether the metabolites are capable of modulating the gliotransmitter release as well. Such a hypothesis is mechanistically justified, as the activation of the molecular targets for BUT and IPA—which are expressed in astrocytes [39,40]—has the potential to increase cytosolic Ca2+ levels [41,42], the major mediator of the release of ATP and Glu from the cells [27]. Based on this hypothesis, the aim of the present study is to evaluate the effects of BUT and IPA on ATP and Glu gliotransmitter release from cultured human astrocytes and to check whether the mechanism is dependent on cytosolic Ca2+ mobilization [43]. Here, we present the preliminary results of the research.
2. Results
2.1. The Effect of the Tested Gut Metabolites on Cell Viability
Before the main analyses were performed, the astrocyte cells’ viability was determined under the influence of the tested gut microbiota metabolites to exclude their toxicity. There were no significant effects of BUT (up to 25 mM) and IPA (up to 0.25 mM) on astrocytes viability after 24-h treatment, and the mean viabilities of the cells treated with BUT and IPA ranged from 92% to 105% of the control cells.
2.2. ATP and Glu Release Dynamics
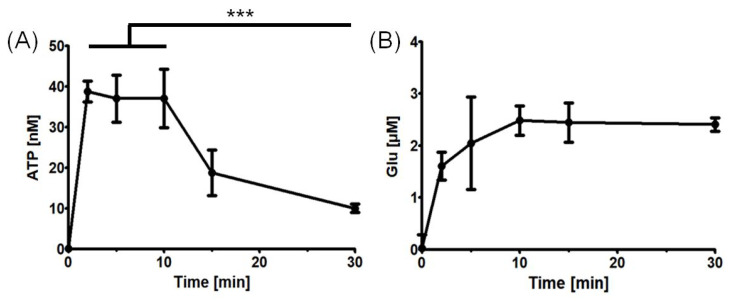
Then, in order to validate the research model, the dynamics of ATP and Glu release were investigated without the tested gut metabolites addition. The release of ATP and Glu from the astrocyte culture was found to be time-dependent. ATP was released rapidly [44], with maximum extracellular concentrations reached at 2–10 min, and with the significant decrease afterwards likely due to the action of ectonucleotidases [45]. On the other hand, extracellular Glu accumulated during the first 10 min and appeared not to decrease later on (Figure 1).
Figure 1.
ATP and Glu release dynamics from the astrocyte cultures. (A) ATP release after cell wash and fresh experimental medium addition at various time points. ATP concentration was found to be significantly reduced at 30 min as compared with at 2–10 min (Welch’s t-test, *** p < 0.001). (B) Glu release after cell wash and HEPES-buffered solution addition at various time points. The points represent the mean estimates, whereas the whiskers indicate the standard errors of means. Number of biological replicates n ≥ 4 for each time point.
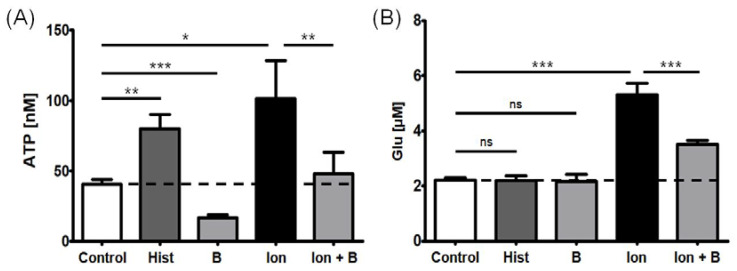
2.3. ATP and Glu Release in Response to Control Compounds
In order to further determine the nature of ATP and Glu gliotransmitter release from the tested astrocytes, several control compounds were used. Ionomycin—a Ca2+ ionophore that increases the cytosolic Ca2+ concentration mainly by facilitating the transport of the ions across the plasma membrane and from intracellular stores [46]—significantly increased ATP and Glu release; both effects were attenuated by the concomitant presence of an intracellular Ca2+ chelator [47]—BAPTA-AM. However, histamine—a molecule that mobilizes cytosolic Ca2+ in response to histamine H1 receptor activation, in a mode mediated by phospholipase C (PLC) and inositol 1,4,5-trisphosphate (IP3) [48]—evoked an enhanced ATP release, but not Glu, in the tested astrocyte cell line. Furthermore, BAPTA-AM could significantly reduce baseline ATP release, but not Glu release, in the cells treated with no Ca2+-mobilizing agents (Figure 2).
Figure 2.
Effect of 10-min treatment with positive controls (histamine 100 μM and ionomycin 5 μM) and a negative control (BAPTA-AM 50 μM 30-min pre-treatment) on (A) ATP and (B) Glu release from the astrocyte cultures. The effect of BAPTA-AM was tested in the presence and absence of ionomycin. The bars represent the mean estimates, whereas the whiskers indicate standard errors of means. Dashed lines indicate the level of ATP and Glu released in control conditions (fresh experimental medium or HEPES buffered Ca2+-containing solution, respectively). The number of biological replicates n ≥ 9 for each condition. One-way analysis of variance with post hoc Dunnett’s test, significance level α = 0.05. * p < 0.05, ** p < 0.01, *** p < 0.001. ns—not significant, Hist—histamine, B—BAPTA-AM, Ion—ionomycin, Ion + B—ionomycin following 30-min pre-incubation with BAPTA-AM.
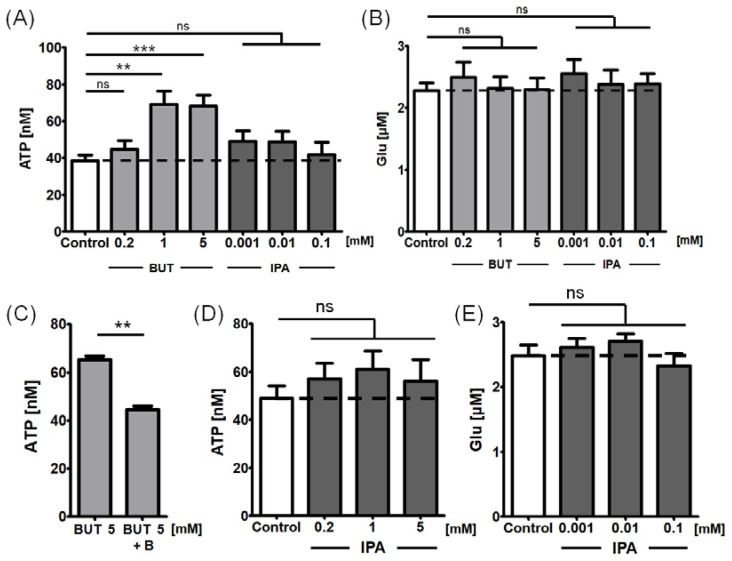
2.4. The Effects of the Tested Gut Metabolites on ATP and Glu Release
In concentrations of 1–5 mM, 10-min incubation with BUT significantly increased the release of ATP from the astrocyte cell cultures by 78% (95% confidence intervals: 45–119%) (Figure 3A); there was a significant BUT concentration-dependent trend in ATP release (p < 0.001). The reported BUT effect was significantly attenuated when the cells were pre-incubated for 30 min with BAPTA-AM 50 μM, suggesting at least partial cytosolic Ca2+-dependent mechanism (Figure 3C). On the other hand, BUT in concentrations of up to 5 mM had no significant effect on Glu release from astrocytes (Figure 3B).
Figure 3.
Effects of BUT and IPA on ATP and Glu release from the cultured astrocytes. (A) Effect on ATP release following 10-min treatment. (B) Effect on Glu release following 10-min treatment. (C) Attenuation of the BUT effect on ATP release by 30-min pre-incubation with BAPTA-AM 50 μM. (D) Effect on ATP release following 24-h pre-treatment with IPA. (E) Effect on Glu release following 24-h pre-treatment with IPA. The bars represent the mean estimates, whereas the whiskers indicate standard errors of means. Dashed lines indicate the levels of ATP and Glu release in control conditions (fresh experimental medium or HEPES buffered Ca2+-containing solution, respectively). Number of biological replicates n ≥ 9 for each condition. One-way analysis of variance with post hoc Dunnett’s test, significance level α = 0.05. ** p < 0.01, *** p < 0.001. ns—not significant, B—BAPTA-AM.
IPA produced a significant effect on neither ATP nor Glu releases from the tested cells, both following a 10-min treatment (Figure 3A,B) and after 24-h pre-incubation (Figure 3D,E).
3. Discussion
An appropriate gut microbiota composition and the intake of specific probiotic products allow for the body’s supply with bacterial metabolites such as BUT and IPA [10,11,49]. After being absorbed into the bloodstream, BUT and IPA penetrate the blood–brain barrier [11]. The metabolites are known to exhibit beneficial effects on the CNS’s components [14,15,16,17,18,19,20,21,23,25] including the astrocytes [22], which substantially contribute to the CNS’s function [26]. Until now, however, it was not known whether the metabolites modify astrocytic gliotransmitter release, the process important in cognition and mood regulation [27]. The present study is the first to demonstrate that BUT, at high CNS concentrations, but likely not IPA, increases ATP release from human astrocyte cultures in a cytosolic Ca2+-dependent manner. The results help to develop understanding of the mechanism of the effects of beneficial gut microbiota metabolites on the CNS function and in neuropsychiatric treatment.
Impaired ATP release from astrocytes located in the prefrontal cortex and the hippocampi has been suggested to cause major depression [31]. Mice that were susceptible to chronic social defeat were found to present with about 20% lower ATP abundance in their brains as compared with controls. Moreover, the specific blockade of the cytosolic Ca2+-dependent release of ATP from astrocytes in these mice caused depressive-like symptoms that could be rescued by the administration of ATP or the 2.5-fold astrocyte-specific activation of ATP release [34]. Concordantly, fluoxetine, a clinically used antidepressant medication, increased the ATP gliotransmission in the mouse model, and another molecular Ca2+-related disruption of astrocyte-specific ATP release impeded fluoxetine-induced anti-depressive action as examined in the tail-suspension test [50]. Moreover, the blockade of Ca2+-independent ATP release from astrocytes was found to cause neuronal synaptic dysfunction and depressive-like symptoms in mice that were reversed by ATP supplementation [51]. Notably, electroconvulsive and sleep-deprivation clinical therapies for depression were also reported to induce ATP release from astrocytes [52].
In light of the above-mentioned evidence, the BUT-induced Ca2+-mediated release of astrocytic ATP reported in our study appears to be an important factor contributing to the anti-depressive effects of BUT. These antidepressant-like actions of BUT were reported in several animal models [14,15,16,17,18,19,20,21], but have never been attributed to increased ATP release from astrocytes. As such, our study provides a novel mechanistic insight into BUT’s biological properties. This may further endorse specific gut-microbiota-targeted interventions in the adjunctive treatment of depression and support the rationale for testing BUT itself as potential antidepressant in clinical trials, which has now started to take place [53,54].
To assess the clinical relevance of the reported ATP-releasing effect, the critical question is whether the tested BUT concentrations are reached in the brain. In the human brain, a 0.02 mM concentration of BUT was reported [55]; however, it is not known whether the brain samples were of sufficient quality in that study to reliably represent BUT concentrations, which are unstable in aqueous solutions [56], and the characteristics of the brain donors were not reported [55]. In mice orally supplemented with BUT-producing Clostridium butyricum probiotic, BUT concentrations in the brain were in a range of 0.4–0.8 mM [57,58]. Despite scarce data, it may be generalized that brain levels of BUT may be highly variable, being dependent on the substrate availability, gut microbiota composition, and intestinal physical conditions [49], not to mention the ability of BUT to be absorbed and distributed into the brain [59]. The concentrations of ≥1 mM (which were effective in the present study) might be naturally achieved in astrocyte surroundings at most temporarily. However, such levels may be reached in vivo if a specific probiotic preparation is administered or likely during oral BUT supplementation; in fact, high daily doses of BUT are applied in animal studies (0.4–1.2 g/kg body mass) [15,16,17,20] and clinical trials (about 6 g) [60,61] to reveal CNS-relevant outcomes.
Interestingly, in our study, IPA demonstrated no significant effect on ATP release in either short- (10 min) or long-term (24 h) treatments. The latter incubation time was additionally applied due to a putative IPA mechanism of action dependent on AhR-mediated gene-transcription regulation [11]. Based on our insignificant results, it may be hypothesized that the AhR expressed in astrocytes may not be coupled with intracellular Ca2+ signaling [40,62] and not involved in ATP gliotransmitter release.
Insignificant results for Glu release obtained under both BUT and IPA influences require some discussion in light of the effect reported for control compounds. In the applied astrocyte cell line model, only the incubation with ionomycin resulted in a significant rise in Glu release, consistently with the fundamental report in this topic by Parpura et al. [63]. However, histamine—in contrast with the research by Kárpáti et al. [48]—failed to induce Glu release. Similarly, cytosolic Ca2+ chelator, BAPTA-AM, did not affect baseline Glu as expected [47], but only ionomycin-induced release. All of this data may suggest that the mechanism of Glu release in the examined astrocyte cultures occurs in response to high cytosolic Ca2+ levels which may only result after opening the cytosol to extracellular space and intracellular stores [46], but not physiologically increased intracellular Ca2+ levels resulting from the activation of the PLC-IP3 cascade pathway [48]. Meanwhile, the baseline Glu release may be Ca2+-independent [27]. These findings might further imply relative insensitivity of the Glu exocytotic machinery to Ca2+ in the tested cells. It is noteworthy that the human cortical astrocyte cells used in the present study were of fetal origin, obtained from a 19-week-old fetus. Vesicular glutamate transporters that are involved in Ca2+-dependent Glu gliotransmission may be expressed in delay during the prenatal development, as reported in the rats [64]; this may provide some possible explanation for the reported phenomenon of Glu release. Ultimately, the obtained insignificant results for Glu astrocytic release following BUT and IPA treatments should be regarded as inconclusive due to the discovered limitation of the model.
Our study presents another limitation as well. Firstly, it was carried out in a single cell-line culture, and—although it showed revealing results supported by multiple control-compounds treatments—it requires confirmation in another astrocyte model, also with regard to the discussed abovementioned Glu-release uncertainty. Secondly, it would be valuable to further explore the mechanism of BUT-induced ATP release to understand which molecules mediate the intracellular signaling leading to the effect; moreover, the question remains of how the effect influences adjacent neurons and brain function, and this could be examined by cell co-cultures and in pre-clinical models. Thirdly, the reported effect may not be specific to BUT, and other SCFA or similar compounds, which share FFAR-mediated mechanisms of action [10], may produce comparable astrocytic ATP releases. Finally, before BUT supplementation is widely recommended, the safety of its high doses should be clarified, as a controversy persists on whether BUT protects or promotes the development of colon cancer [65] and obesity [66]. Despite the limitations, our preliminary study may provide a novel mechanistic explanation for the beneficial effect of BUT on the CNS function.
4. Materials and Methods
4.1. Reagents
BUT, IPA, histamine, ionomycin, 1,2-bis(2-aminophenoxy)ethane-N,N,N′,N′- tetraacetic acid tetrakis(acetoxymethyl ester) (BAPTA-AM), 3-(4,5-dimethylthiazol-2-yl)- 2,5-diphenyltetrazolium bromide (MTT), dimethyl sulfoxide (DMSO), trypsin-EDTA solution, NaCl, KCl, MgCl2, CaCl2, glucose, and 4-(2-hydroxyethyl)-1-piperazineethane- sulfonic acid (HEPES) were purchased from Sigma-Aldrich (Saint Louis, MO, USA). Dulbecco’s Phosphate Buffered Saline was obtained from Biowest (Nuaillé, France). Astrocyte Medium, Astrocyte Growth Supplement, fetal bovine serum (FBS), penicillin/streptomycin solution, and poly-L-lysine were obtained from ScienCell Research Laboratories (Carlsbad, CA, USA).
4.2. Human Astrocyte Cell Culture
The study was performed with the use of a commercially available astrocyte cell line isolated from human cerebral cortex (ScienCell Research Laboratories, cat no. 28523). The cell culture was maintained at 37 °C in a humidified atmosphere of 5% CO2, in dishes coated with poly-L-lysine. The cells were grown in Astrocyte Medium supplemented with 2% FBS, 10% Astrocyte Growth Supplement, and 1% penicillin/streptomycin solution. Pure Astrocyte Medium was used as the experimental medium. The astrocyte culture was maintained according to the protocol recommended by ScienCell Research Laboratories.
4.3. Cell Viability MTT Test
In order to assess whether BUT and IPA are non-toxic to the cultured astrocytes, cell viability was evaluated using the colorimetric MTT assay. The cells were seeded onto a 96-well plate to a final density of 1.5 × 104 cells/well. After 24 h of culture, the cells were exposed to BUT (up to 25 mM) and IPA (up to 0.25 mM) for the next 24 h. After the incubation time with the compounds, MTT solution was added to the cell culture for another four hours to let the mitochondrial succinate-tetrazolium reductase system convert yellow tetrazolium MTT into purple formazan. The absorbance was measured at λ = 570 nm by BioTek EL ×800 microplate reader (BioTek; Winooski, VT, USA); the value was proportional to the number of viable cells. The viability was calculated as a proportion of the absorbance of investigated samples to the absorbance of control samples (cells not treated with BUT and IPA).
4.4. ATP and Glu Release Dynamics
For the assessment of ATP and Glu release from astrocytes in the function of time, the cells were seeded onto a 96-well plate to a final density of 1.5 × 104 cells/well for 24 h. Afterwards, the cells were washed and supplied with fresh experimental medium (in case of ATP assessment) or HEPES-buffered solution (HBS; 120 mM NaCl, 5 mM KCl, 1 mM MgCl2, 1.5 mM CaCl2, 10 mM glucose, 25 mM HEPES; pH = 7.4; in case of Glu assessment). After the incubations lasting 2, 5, 10, 15, or 30 min, the supernatants were collected and subjected for the measurands evaluation. For ATP, the luminescence-based test “ATP Detection Assay Kit—Luminescence” (Cayman; Ann Arbor, MI, USA; cat no. 700410) was applied according to the protocol recommended by the producer, and luminescence was assessed with the use of a Synergy H1 plate reader (Biotek; Winooski, VT, USA). For Glu measurement, the fluorescence-based test “Glutamate Assay Kit (Fluorometric)” (Abcam; Cambridge, UK; cat no. ab138883) was used according to the protocol recommended by the producer, and fluorescence (excitation λ = 550 nm, emission λ = 590 nm) was assessed with the use of a Victor X4 multilabel plate reader (PerkinElmer; Waltham, MA, USA).
4.5. Effect of the Control and Tested Compounds on ATP and Glu Release
For the assessment of ATP and Glu release in response to positive controls (histamine [48] and ionomycin [46,63]) and a negative control (BAPTA-AM [47]), as well as under the influence of BUT and IPA treatments, the cells were seeded onto a 96-well plate to a final density of 1.5 × 104 cells/well. After 24 h, the cultures were washed and exposed to the control substances (histamine 100 μM or ionomycin 5 μM), and the tested compounds (BUT range of 0.2–5 mM and IPA range of 0.001–0.1 mM) dissolved in fresh experimental medium or HBS buffer (for ATP and Glu assessment, respectively) or with no addition of these substances. The exposition time was 10 min. Then, the supernatants were collected for the immediate analysis of the measurands that was carried out as described above. Before the cell culture wash, the cells were optionally pre-incubated with BAPTA-AM (cytosolic Ca2+ chelator) for 30 min or IPA for 24 h.
4.6. Data Analysis
All of the experimental procedures to examine BUT’s and IPA’s effects on the ATP and Glu concentrations in the supernatants were performed in three biological replicates, and each such experiment was independently repeated at least three times (nine samples in total for each experimental condition). Each individual supernatant sample was analyzed in two technical replicates, which were averaged before further analysis. One-way analysis of variance (ANOVA) with Dunnett’s post-hoc test was used to test the null hypotheses of no difference in the mean concentrations of measurands between the cells treated with specific concentrations of the tested compounds in comparison with those untreated. The contrast analysis was optionally used to evaluate the concentration-dependent trend in the effects. Statistical significance was set at α = 0.05. STATISTICA software version 13.3 was used in the analysis (Statsoft; Tulsa, OK, USA).
5. Conclusions
This is the first report to preliminarily demonstrate BUT—in high brain concentrations—to increase ATP gliotransmitter release from the cultured human astrocytes in a cytosolic Ca2+-dependent manner; IPA was found to not significantly affect ATP release. The findings appear to provide a novel mechanistic explanation for the beneficial effect of BUT on CNS function. This may further endorse testing of BUT-producing gut-microbiota-targeted interventions and BUT supplementation as potential antidepressants. The results of BUT’s and IPA’s effects on Glu release remain inconclusive. The reported findings require confirmation and further testing in basic and pre-clinical settings.
Acknowledgments
We thank Wioletta Grabowicz, Agnieszka Janas, and Małgorzata Majczyk, as well as the team of Department of Molecular Carcinogenesis, Medical University of Lodz for the technical assistance during the research work.
Author Contributions
Conceptualization, M.S.K.; methodology, M.S.K.; validation, M.S.K.; formal analysis, M.S.K.; investigation, M.S.K. and P.S.; resources, M.S.K.; data curation, M.S.K.; writing—original draft preparation, M.S.K.; writing—review and editing, M.S.K. and P.S.; visualization, M.S.K.; supervision, M.S.K. and E.K.; project administration, M.S.K.; funding acquisition, M.S.K. and E.K. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
The data presented in this study are openly available in the Mendeley Data repository at digital object identifier: 10.17632/f9y2dcfb99.1.
Conflicts of Interest
The authors declare no conflict of interest. The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript; or in the decision to publish the results.
Funding Statement
This research was funded by the grant MINIATURA-5 no. 2021/05/X/NZ3/00557 from the National Science Center of Poland (https://ncn.gov.pl/, accessed on 19 February 2023; the grant received by M.S.K.) and supported by the grant no. 503/5-108-03/503-51-001-19-00 from the Medical University of Lodz (https://umed.pl/, accessed on 19 February 2023; received by E.K.).
Footnotes
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
References
- 1.Valdes A.M., Walter J., Segal E., Spector T.D. Role of the Gut Microbiota in Nutrition and Health. BMJ. 2018;361:k2179. doi: 10.1136/bmj.k2179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gilbert S.F., Tauber A.I. Rethinking Individuality: The Dialectics of the Holobiont. Biol. Philos. 2016;31:839–853. doi: 10.1007/s10539-016-9541-3. [DOI] [Google Scholar]
- 3.Dash S., Syed Y.A., Khan M.R. Understanding the Role of the Gut Microbiome in Brain Development and Its Association With Neurodevelopmental Psychiatric Disorders. Front. Cell Dev. Biol. 2022;10:880544. doi: 10.3389/fcell.2022.880544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Breit S., Kupferberg A., Rogler G., Hasler G. Vagus Nerve as Modulator of the Brain–Gut Axis in Psychiatric and Inflammatory Disorders. Front. Psychiatry. 2018;9 doi: 10.3389/fpsyt.2018.00044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Frankiensztajn L.M., Elliott E., Koren O. The Microbiota and the Hypothalamus-Pituitary-Adrenocortical (HPA) Axis, Implications for Anxiety and Stress Disorders. Curr. Opin. Neurobiol. 2020;62:76–82. doi: 10.1016/j.conb.2019.12.003. [DOI] [PubMed] [Google Scholar]
- 6.Tillmann S., Awwad H.M., Eskelund A.R., Treccani G., Geisel J., Wegener G., Obeid R. Probiotics Affect One-Carbon Metabolites and Catecholamines in a Genetic Rat Model of Depression. Mol. Nutr. Food Res. 2018;62:e1701070. doi: 10.1002/mnfr.201701070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chen Y., Xu J., Chen Y. Regulation of Neurotransmitters by the Gut Microbiota and Effects on Cognition in Neurological Disorders. Nutrients. 2021;13:2099. doi: 10.3390/nu13062099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Dehghani F., Abdollahi S., Shidfar F., Clark C.C.T., Soltani S. Probiotics Supplementation and Brain-Derived Neurotrophic Factor (BDNF): A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Nutr. Neurosci. 2022:1–11. doi: 10.1080/1028415X.2022.2110664. [DOI] [PubMed] [Google Scholar]
- 9.Rutsch A., Kantsjö J.B., Ronchi F. The Gut-Brain Axis: How Microbiota and Host Inflammasome Influence Brain Physiology and Pathology. Front. Immunol. 2020;11:604179. doi: 10.3389/fimmu.2020.604179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Krautkramer K.A., Fan J., Bäckhed F. Gut Microbial Metabolites as Multi-Kingdom Intermediates. Nat. Rev. Microbiol. 2021;19:77–94. doi: 10.1038/s41579-020-0438-4. [DOI] [PubMed] [Google Scholar]
- 11.Descamps H.C., Herrmann B., Wiredu D., Thaiss C.A. The Path toward Using Microbial Metabolites as Therapies. EBioMedicine. 2019;44:747–754. doi: 10.1016/j.ebiom.2019.05.063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.O’Riordan K.J., Collins M.K., Moloney G.M., Knox E.G., Aburto M.R., Fülling C., Morley S.J., Clarke G., Schellekens H., Cryan J.F. Short Chain Fatty Acids: Microbial Metabolites for Gut-Brain Axis Signalling. Mol. Cell. Endocrinol. 2022;546:111572. doi: 10.1016/j.mce.2022.111572. [DOI] [PubMed] [Google Scholar]
- 13.Silva Y.P., Bernardi A., Frozza R.L. The Role of Short-Chain Fatty Acids From Gut Microbiota in Gut-Brain Communication. Front. Endocrinol. 2020;11:25. doi: 10.3389/fendo.2020.00025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Valvassori S.S., Varela R.B., Arent C.O., Dal-Pont G.C., Bobsin T.S., Budni J., Reus G.Z., Quevedo J. Sodium Butyrate Functions as an Antidepressant and Improves Cognition with Enhanced Neurotrophic Expression in Models of Maternal Deprivation and Chronic Mild Stress. Curr. Neurovasc. Res. 2014;11:359–366. doi: 10.2174/1567202611666140829162158. [DOI] [PubMed] [Google Scholar]
- 15.Valvassori S.S., Resende W.R., Budni J., Dal-Pont G.C., Bavaresco D.V., Reus G.Z., Carvalho A.F., Goncalves C.L., Furlanetto C.B., Streck E.L., et al. Sodium Butyrate, a Histone Deacetylase Inhibitor, Reverses Behavioral and Mitochondrial Alterations in Animal Models of Depression Induced by Early- or Late-Life Stress. Curr. Neurovasc. Res. 2015;12:312–320. doi: 10.2174/1567202612666150728121121. [DOI] [PubMed] [Google Scholar]
- 16.Resende W.R., Valvassori S.S., Réus G.Z., Varela R.B., Arent C.O., Ribeiro K.F., Bavaresco D.V., Andersen M.L., Zugno A.I., Quevedo J. Effects of Sodium Butyrate in Animal Models of Mania and Depression: Implications as a New Mood Stabilizer. Behav. Pharmacol. 2013;24:569. doi: 10.1097/FBP.0b013e32836546fc. [DOI] [PubMed] [Google Scholar]
- 17.Wei Y.B., Melas P.A., Wegener G., Mathé A.A., Lavebratt C. Antidepressant-Like Effect of Sodium Butyrate Is Associated with an Increase in TET1 and in 5-Hydroxymethylation Levels in the Bdnf Gene. Int. J. Neuropsychopharmacol. 2015;18:pyu032. doi: 10.1093/ijnp/pyu032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Zhu H., Huang Q., Xu H., Niu L., Zhou J.-N. Antidepressant-like Effects of Sodium Butyrate in Combination with Estrogen in Rat Forced Swimming Test: Involvement of 5-HT1A Receptors. Behav. Brain Res. 2009;196:200–206. doi: 10.1016/j.bbr.2008.08.039. [DOI] [PubMed] [Google Scholar]
- 19.Yamawaki Y., Fuchikami M., Morinobu S., Segawa M., Matsumoto T., Yamawaki S. Antidepressant-like Effect of Sodium Butyrate (HDAC Inhibitor) and Its Molecular Mechanism of Action in the Rat Hippocampus. World J. Biol. Psychiatry. 2012;13:458–467. doi: 10.3109/15622975.2011.585663. [DOI] [PubMed] [Google Scholar]
- 20.Yamawaki Y., Yoshioka N., Nozaki K., Ito H., Oda K., Harada K., Shirawachi S., Asano S., Aizawa H., Yamawaki S., et al. Sodium Butyrate Abolishes Lipopolysaccharide-Induced Depression-like Behaviors and Hippocampal Microglial Activation in Mice. Mol. Brain Res. 2018;1680:13–38. doi: 10.1016/j.brainres.2017.12.004. [DOI] [PubMed] [Google Scholar]
- 21.Schroeder F.A., Lin C.L., Crusio W.E., Akbarian S. Antidepressant-Like Effects of the Histone Deacetylase Inhibitor, Sodium Butyrate, in the Mouse. Biol. Psychiatry. 2007;1:55–64. doi: 10.1016/j.biopsych.2006.06.036. [DOI] [PubMed] [Google Scholar]
- 22.Garcez M.L., Tan V.X., Heng B., Guillemin G.J. Sodium Butyrate and Indole-3-Propionic Acid Prevent the Increase of Cytokines and Kynurenine Levels in LPS-Induced Human Primary Astrocytes. Int. J. Tryptophan Res. 2020;13:1178646920978404. doi: 10.1177/1178646920978404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kimura I., Ichimura A., Ohue-Kitano R., Igarashi M. Free Fatty Acid Receptors in Health and Disease. Physiol. Rev. 2020;100:171–210. doi: 10.1152/physrev.00041.2018. [DOI] [PubMed] [Google Scholar]
- 24.Wikoff W.R., Anfora A.T., Liu J., Schultz P.G., Lesley S.A., Peters E.C., Siuzdak G. Metabolomics Analysis Reveals Large Effects of Gut Microflora on Mammalian Blood Metabolites. Proc. Natl. Acad. Sci. USA. 2009;106:3698–3703. doi: 10.1073/pnas.0812874106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Konopelski P., Mogilnicka I. Biological Effects of Indole-3-Propionic Acid, a Gut Microbiota-Derived Metabolite, and Its Precursor Tryptophan in Mammals’ Health and Disease. Int. J. Mol. Sci. 2022;23:1222. doi: 10.3390/ijms23031222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Verkhratsky A., Nedergaard M. Physiology of Astroglia. Physiol. Rev. 2018;98:239–389. doi: 10.1152/physrev.00042.2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Harada K., Kamiya T., Tsuboi T. Gliotransmitter Release from Astrocytes: Functional, Developmental and Pathological Implications in the Brain. Front. Neurosci. 2016;9:499. doi: 10.3389/fnins.2015.00499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Pillai A.G., Nadkarni S. Amyloid Pathology Disrupts Gliotransmitter Release in Astrocytes. PLOS Comput. Biol. 2022;18:e1010334. doi: 10.1371/journal.pcbi.1010334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Piacentini R., Puma D.D.L., Mainardi M., Lazzarino G., Tavazzi B., Arancio O., Grassi C. Reduced Gliotransmitter Release from Astrocytes Mediates Tau-Induced Synaptic Dysfunction in Cultured Hippocampal Neurons. Glia. 2017;65:1302–1316. doi: 10.1002/glia.23163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Boué-Grabot E., Pankratov Y. Modulation of Central Synapses by Astrocyte-Released ATP and Postsynaptic P2X Receptors. Neural Plast. 2017;2017:9454275. doi: 10.1155/2017/9454275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Illes P., Rubini P., Yin H., Tang Y. Impaired ATP Release from Brain Astrocytes May Be a Cause of Major Depression. Neurosci. Bull. 2020;36:1281–1284. doi: 10.1007/s12264-020-00494-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lin S., Huang L., Luo Z., Li X., Jin S., Du Z., Wu D., Xiong W., Huang L., Luo Z., et al. The ATP Level in the Medial Prefrontal Cortex Regulates Depressive-like Behavior via the Medial Prefrontal Cortex-Lateral Habenula Pathway. Biol. Psychiatry. 2022;92:179–192. doi: 10.1016/j.biopsych.2022.02.014. [DOI] [PubMed] [Google Scholar]
- 33.Anderson G. Amyotrophic Lateral Sclerosis Pathoetiology and Pathophysiology: Roles of Astrocytes, Gut Microbiome, and Muscle Interactions via the Mitochondrial Melatonergic Pathway, with Disruption by Glyphosate-Based Herbicides. Int. J. Mol. Sci. 2023;24:587. doi: 10.3390/ijms24010587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Cao X., Li L.-P., Wang Q., Wu Q., Hu H.-H., Zhang M., Fang Y.-Y., Zhang J., Li S.-J., Xiong W.-C., et al. Astrocyte-Derived ATP Modulates Depressive-like Behaviors. Nat. Med. 2013;19:773–777. doi: 10.1038/nm.3162. [DOI] [PubMed] [Google Scholar]
- 35.Mahmoud S., Gharagozloo M., Simard C., Gris D. Astrocytes Maintain Glutamate Homeostasis in the CNS by Controlling the Balance between Glutamate Uptake and Release. Cells. 2019;8:184. doi: 10.3390/cells8020184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Spichak S., Donoso F., Moloney G.M., Gunnigle E., Brown J.M., Codagnone M., Dinan T.G., Cryan J.F. Microbially-Derived Short-Chain Fatty Acids Impact Astrocyte Gene Expression in a Sex-Specific Manner. Brain Behav. Immun. Health. 2021;16:100318. doi: 10.1016/j.bbih.2021.100318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Wang C., Zheng D., Weng F., Jin Y., He L. Sodium Butyrate Ameliorates the Cognitive Impairment of Alzheimer’s Disease by Regulating the Metabolism of Astrocytes. Psychopharmacology. 2022;239:215–227. doi: 10.1007/s00213-021-06025-0. [DOI] [PubMed] [Google Scholar]
- 38.Yang T., Rodriguez V., Malphurs W.L., Schmidt J.T., Ahmari N., Sumners C., Martyniuk C.J., Zubcevic J. Butyrate Regulates Inflammatory Cytokine Expression without Affecting Oxidative Respiration in Primary Astrocytes from Spontaneously Hypertensive Rats. Physiol. Rep. 2018;6:e13732. doi: 10.14814/phy2.13732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Falomir-Lockhart L.J., Cavazzutti G.F., Giménez E., Toscani A.M. Fatty Acid Signaling Mechanisms in Neural Cells: Fatty Acid Receptors. Front. Cell. Neurosci. 2019;13:162. doi: 10.3389/fncel.2019.00162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Rothhammer V., Kenison J.E., Li Z., Tjon E., Takenaka M.C., Chao C.-C., de Lima K.A., Borucki D.M., Kaye J., Quintana F.J. Aryl Hydrocarbon Receptor Activation in Astrocytes by Laquinimod Ameliorates Autoimmune Inflammation in the CNS. Neurol. Neuroimmunol. Neuroinflammat. 2021;8:e946. doi: 10.1212/NXI.0000000000000946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Miletta M.C., Petkovic V., Eblé A., Ammann R.A., Flück C.E., Mullis P.-E. Butyrate Increases Intracellular Calcium Levels and Enhances Growth Hormone Release from Rat Anterior Pituitary Cells via the G-Protein-Coupled Receptors GPR41 and 43. PLoS ONE. 2014;9:e107388. doi: 10.1371/journal.pone.0107388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Larigot L., Juricek L., Dairou J., Coumoul X. AhR Signaling Pathways and Regulatory Functions. Biochim. Open. 2018;7:1–9. doi: 10.1016/j.biopen.2018.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Xiong Y., Sun S., Teng S., Jin M., Zhou Z. Ca2+-Dependent and Ca2+-Independent ATP Release in Astrocytes. Front. Mol. Neurosci. 2018;11:224. doi: 10.3389/fnmol.2018.00224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Kuga N., Sasaki T., Takahara Y., Matsuki N., Ikegaya Y. Large-Scale Calcium Waves Traveling through Astrocytic Networks In Vivo. J. Neurosci. 2011;31:2607–2614. doi: 10.1523/JNEUROSCI.5319-10.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Grković I., Drakulić D., Martinović J., Mitrović N. Role of Ectonucleotidases in Synapse Formation During Brain Development: Physiological and Pathological Implications. Curr. Neuropharmacol. 2019;17:84–98. doi: 10.2174/1570159X15666170518151541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Dedkova E.N., Sigova A.A., Zinchenko V.P. Mechanism of Action of Calcium Ionophores on Intact Cells: Ionophore-Resistant Cells. Membr. Cell Biol. 2000;13:357–368. [PubMed] [Google Scholar]
- 47.Kim H., Lee B.-H., Choi S.-H., Kim H.-J., Jung S.-W., Hwang S.-H., Rhim H., Kim H.-C., Cho I.-H., Nah S.-Y. Gintonin Stimulates Gliotransmitter Release in Cortical Primary Astrocytes. Neurosci. Lett. 2015;603:19–24. doi: 10.1016/j.neulet.2015.07.012. [DOI] [PubMed] [Google Scholar]
- 48.Kárpáti A., Yoshikawa T., Nakamura T., Iida T., Matsuzawa T., Kitano H., Harada R., Yanai K. Histamine Elicits Glutamate Release from Cultured Astrocytes. J. Pharmacol. Sci. 2018;137:122–128. doi: 10.1016/j.jphs.2018.05.002. [DOI] [PubMed] [Google Scholar]
- 49.Olsson L.M., Boulund F., Nilsson S., Khan M.T., Gummesson A., Fagerberg L., Engstrand L., Perkins R., Uhlén M., Bergström G., et al. Dynamics of the Normal Gut Microbiota: A Longitudinal One-Year Population Study in Sweden. Cell Host Microbe. 2022;30:726–739.e3. doi: 10.1016/j.chom.2022.03.002. [DOI] [PubMed] [Google Scholar]
- 50.Kinoshita M., Hirayama Y., Fujishita K., Shibata K., Shinozaki Y., Shigetomi E., Takeda A., Le H.P.N., Hayashi H., Hiasa M., et al. Anti-Depressant Fluoxetine Reveals Its Therapeutic Effect Via Astrocytes. EBioMedicine. 2018;32:72–83. doi: 10.1016/j.ebiom.2018.05.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Jun M., Xiaolong Q., Chaojuan Y., Ruiyuan P., Shukun W., Junbing W., Li H., Hong C., Jinbo C., Rong W., et al. Calhm2 Governs Astrocytic ATP Releasing in the Development of Depression-like Behaviors. Mol. Psychiatry. 2018;23:883–891. doi: 10.1038/mp.2017.229. [DOI] [PubMed] [Google Scholar]
- 52.Koizumi S. Glial Purinergic Signals and Psychiatric Disorders. Front. Cell. Neurosci. 2022;15:822614. doi: 10.3389/fncel.2021.822614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Verbeke K. Effects of Butyrate on Affective Processes. [(accessed on 11 July 2021)];2021 Clinical Trial Registration NCT04722549; clinicaltrials.gov. Available online: https://clinicaltrials.gov/ct2/show/NCT04722549.
- 54.Chatterjee S. Microbiome Targeted Oral Butyrate Therapy in Gulf War Multisymptom Illness. [(accessed on 13 February 2023)];2022 Clinical Trial Registration NCT05367245; clinicaltrials.gov. Available online: https://clinicaltrials.gov/ct2/show/NCT05367245.
- 55.Bachmann C., Colombo J.-P., Berüter J. Short Chain Fatty Acids in Plasma and Brain: Quantitative Determination by Gas Chromatography. Clin. Chim. Acta. 1979;92:153–159. doi: 10.1016/0009-8981(79)90109-8. [DOI] [PubMed] [Google Scholar]
- 56.Cayman Chemical Sodium Butyrate. 2014. [(accessed on 19 February 2023)]. Product Information. Available online: https://fnkprddata.blob.core.windows.net/domestic/data/datasheet/CAY/13121.pdf.
- 57.Liu J., Sun J., Wang F., Yu X., Ling Z., Li H., Zhang H., Jin J., Chen W., Pang M., et al. Neuroprotective Effects of Clostridium Butyricum against Vascular Dementia in Mice via Metabolic Butyrate. BioMed Res. Int. 2015;2015:412946. doi: 10.1155/2015/412946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Barber T.W., Brockway J.A., Higgins L.S. The Density of Tissues in and About the Head. Acta Neurol. Scand. 1970;46:85–92. doi: 10.1111/j.1600-0404.1970.tb05606.x. [DOI] [PubMed] [Google Scholar]
- 59.Yang T., Magee K.L., Colon-Perez L.M., Larkin R., Liao Y.-S., Balazic E., Cowart J.R., Arocha R., Redler T., Febo M., et al. Impaired Butyrate Absorption in the Proximal Colon, Low Serum Butyrate and Diminished Central Effects of Butyrate on Blood Pressure in Spontaneously Hypertensive Rats. Acta Physiol. Oxf. Engl. 2019;226:e13256. doi: 10.1111/apha.13256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Smith R.C. Sodium Butyrate as a Treatment for Improving Cognitive Function in Schizophrenia. [(accessed on 13 February 2023)];2016 Clinical Trial Registration NCT02654405; clinicaltrials.gov. Available online: https://clinicaltrials.gov/ct2/show/NCT02654405.
- 61.Dalile B., Vervliet B., Bergonzelli G., Verbeke K., Van Oudenhove L. Colon-Delivered Short-Chain Fatty Acids Attenuate the Cortisol Response to Psychosocial Stress in Healthy Men: A Randomized, Placebo-Controlled Trial. Neuropsychopharmacology. 2020;45:2257–2266. doi: 10.1038/s41386-020-0732-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Huang Y.-J., Hung C.-C., Hsu P.-C., Lee P.-Y., Tsai Y.-A., Hsin Y.-C., Lee X.-T., Chou C.-C., Chen M.-L., Tarng D.-C., et al. Astrocytic Aryl Hydrocarbon Receptor Mediates Chronic Kidney Disease-Associated Mental Disorders Involving GLT1 Hypofunction and Neuronal Activity Enhancement in the Mouse Brain. Glia. 2022;9:499. doi: 10.1002/glia.24326. [DOI] [PubMed] [Google Scholar]
- 63.Parpura V., Basarsky T.A., Liu F., Jeftinija K., Jeftinija S., Haydon P.G. Glutamate-Mediated Astrocyte-Neuron Signalling. Nature. 1994;369:744–747. doi: 10.1038/369744a0. [DOI] [PubMed] [Google Scholar]
- 64.Ohmomo H., Ehara A., Yoshida S., Shutoh F., Ueda S., Hisano S. Temporally Distinct Expression of Vesicular Glutamate Transporters 1 and 2 during Embryonic Development of the Rat Olfactory System. Neurosci. Res. 2011;70:376–382. doi: 10.1016/j.neures.2011.05.005. [DOI] [PubMed] [Google Scholar]
- 65.Lupton J.R. Microbial Degradation Products Influence Colon Cancer Risk: The Butyrate Controversy. J. Nutr. 2004;134:479–482. doi: 10.1093/jn/134.2.479. [DOI] [PubMed] [Google Scholar]
- 66.Liu H., Wang J., He T., Becker S., Zhang G., Li D., Ma X. Butyrate: A Double-Edged Sword for Health? Adv. Nutr. 2018;9:21–29. doi: 10.1093/advances/nmx009. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data presented in this study are openly available in the Mendeley Data repository at digital object identifier: 10.17632/f9y2dcfb99.1.