INTRODUCTION
Suicidal behavior can be broadly subdivided into suicide-related behavior and suicide-related communication. Amidst the broad array of confusing terms with varying meanings, the terms as used in this guideline have been clarified for the sake of uniformity of communication and approach between clinicians [Table 1].[1-3] A simple schematic outline of self-injurious behavior is given below [Figure 1].[4]
Table 1.
Definition of common terminology used in this guideline
| Suicidal ideation- Thoughts about self-harm, with deliberate consideration or planning of possible techniques of causing one’s own death[1] |
| Suicide attempt- A self-inflicted, potentially injurious behavior with a non-fatal outcome for which there is evidence (either explicit or implicit) of intent to die[2] |
| Aborted or interrupted attempt -Aborted suicide attempt-potentially self-injurious behavior with evidence (either explicit or implicit) that the person intended to die but stopped the attempt before physical damage occurred.[3] |
| Suicide- The act of intentionally causing one’s death[1] Self-harm/Deliberate self-harm/Non-suicidal self-injury- When an individual engages in inflicted self-damage to the surface of his/her body with the expectation that the injury will lead to minor or moderate physical harm, thus, suicidal intent is absent. The absence of suicidal intent can either be stated or inferred from the circumstances.[1] Suicide-related communication involves suicidal threat and suicidal plan. |
| Suicidal threat- Any interpersonal action, verbal or non-verbal, without a direct self-injurious component, that a reasonable person would interpret as communicating or suggesting that suicidal behaviour might occur in the near future[2] |
| Suicidal plan- Proposed method of carrying out a design that will lead to a potentially self-injurious outcome[2] |
Figure 1.
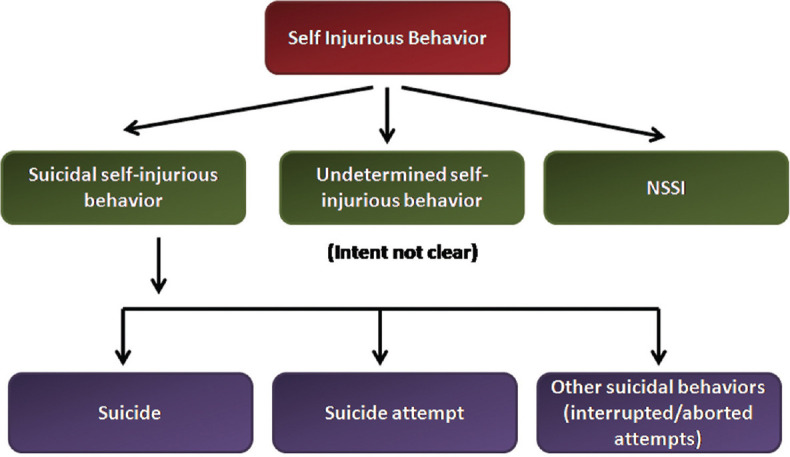
Classification of self-injurious behavior[4]. (NSSI- Non-suicidal self-injury)
EPIDEMIOLOGY
Across the world, nearly 8,00,000 people die by suicide every year, and nearly 74% of suicides occur in low- and middle-income countries. According to WHO’s Global Health Estimates, the global age-standardized suicide death rate (SDR) was 9.0 per 1,00,000 population for 2019.[5] Suicide is the second most common cause of death among young people aged 15–29 years of both sexes globally. Suicide rates in India are one of the highest globally and account for 26.6% of global suicide deaths. The suicide deaths for 2020 released by the National Crime Records Bureau (NCRB) in 2021 showed a rate of 11.3 per lakh population, the actual figure amounting to 1,53,052 deaths.[6] This was the highest number of suicides recorded by India since 1971 which is quite alarming! According to NCRB data over the last few years, individuals belonging to 18–29-year age-group is the most vulnerable group accounting for almost 35% of all cases of suicide. Within this group, there is an increasing trend of student suicides which have multiple reasons including academic pressure. Although suicide in women is decreasing, India still contributes 36% of global suicides in women in 15–39-year age-group. Intimate partner violence is one of the most important causes of suicides in married women of India. The most common methods of suicide (in decreasing frequency) are hanging, consuming poison, drowning and self-immolation. In terms of gender, the rate of completed suicides has been gradually increasing in favor of males with the latest data showing almost 2.5 times more men dying by suicide than women. However, attempted suicides are a greater problem in the women of our country. Thus, appropriate prevention measures at the community level along with proper risk assessment become essential for identifying those at risk and taking appropriate measures.
BASIC STEPS OF RISK ASSESSMENT
Engagement and Therapeutic Alliance- This is the most crucial step in risk assessment because if this step is not successfully negotiated, information derived from the patient may not be meaningful and adequate. The clinician must use empathy, active listening, respect, and supportive and non-judgmental attitude toward the patient in order to build proper therapeutic alliance. Simple questions like, “Things seem to be a bit difficult for you these days” can go a long way in making the patient relaxed and open up. Proper alliance will lead to honest disclosure on the part of the patient. Wherever possible, the clinician must try to engage the family members and/or immediate support system. The family may be a very important source of additional information and support.
Psychiatric Evaluation: A thorough psychiatric evaluation is the next most important step in risk assessment. Majority of those who die by suicide have been found to have an underlying psychiatric disorder. Disorders commonly associated with suicidal behavior include depressive and mixed episodes, schizophrenia, substance use disorders (especially alcohol), anxiety disorders, borderline personality disorders, and adjustment disorders. Substance use disorder, especially alcohol, confers a risk of 15–23% for suicide. Comorbidity of substance abuse with an Axis I disorder like bipolar disorder and depressive disorder significantly elevates the risk than either condition alone through the common pathway of impulsivity, aggression, and hostility. Among those with bipolar disorder, depressive and mixed episodes pose the greatest risk. History of current and past psychiatric diagnosis, treatment, and family history of psychiatric disorders must be probed. A brief mental status examination should be done. History of coping with stresses must be elicited—whether the person has been able to manage stressful situations in the past or resorted to maladaptive ways of coping. Additional information should be gathered wherever available from friends, families, and treatment records.
Risk Factors: There are several risk factors which have been variably linked to suicide [Table 2].[3] During elicitation of risk factors, the clinician should take note of modifiable risk factors so that these can be addressed.
Protective Factors: It is important to enquire about factors which may act as “suicide-counters” in individuals harboring suicidal behaviors [Table 3].[3] Knowledge of protective factors help in therapeutic intervention in individuals showing suicidal behavior.
Warning Signs: Unlike risk factors, warning signs denote imminent risk for suicide just like a sudden chest pain serves as a warning sign for heart attack. Thus, warning signs denote more proximal relation to suicidal behavior apart from being subjective in nature and easily identifiable by lay persons. The working group of the American Association of Suicidology met in 2003 and developed a consensus list of warning signs which denote heightened risk of suicide [Table 4].[7]
-
Suicide Enquiry- Suicide enquiry involves probing suicidal ideation, plans, intent, and lethality. For those who have presented with a recent attempt, enquiry should be made about all these aspects when he/she had made the attempt and also his/her current suicidal ideation. Past attempts should also be probed with special reference to attempts made in the recent past and the most severe attempts.
-
Ideation: Eliciting ideation could begin with simple questions like “Have you ever felt that life was not worth living?” or “Have thoughts of harming yourself crossed your mind?”. Once the response is in the affirmative, the clinician can go ahead with more specific questions to find out the following:
Frequency, intensity and duration (in the last 48 hours, past month)
“How often do you think about suicide?”
“Could you rate the intensity of those thoughts on a scale of 1 to 10? How long do they typically last?”
-
Suicide Plan: Once suicidal ideation is elicited, the clinician should make specific enquiry about the presence of a suicidal plan and whether the subject has taken any steps to put the plan into action. Questions should probe the following areas:
Timing, location, lethality, access to means, preparatory acts
“Do you have a plan of how you would kill yourself?”
“Have you made any specific preparations?”
“Do you have poison/weapons/drugs at home?”
Intent: Suicidal intent reflects the intensity of a patient’s wish to die and can be assessed by determining the patient’s motivation for suicide as well as the seriousness and extent of his or her aim to die, including any associated behaviors or planning for suicide.[3]
Lethality of Suicidal Behavior—Objective danger to life associated with a suicide method or action. Lethality is to be assessed objectively by the clinician and may not always coincide with an individual’s expectation of what is medically dangerous. For example, in many cases of impulsive acts of pesticide poisoning, the victim consumes pesticide on the spur of the moment without a strong intention to die but the lethality of the agent mostly leads to the unfortunate death of the individual.
-
Table 2.
Risk factors for suicide (modifiable factors in bold)[3]
| Past suicide attempt |
| Current or lifetime psychiatric disorders |
|
Alcohol and abuse of other substances Recent stressful life events (Especially financial/relational loss) |
| Family history of suicide |
| Chronic medical illness |
| History of physical/sexual abuse |
|
Access to lethal means Hopelessness/despair Anhedonia Impulsivity Recent discharge from a psychiatric facility |
| Poor support system |
Table 3.
Protective factors for suicide[3]
| Children at home |
| Sense of responsibility to family |
| Pregnancy/motherhood |
| Religiosity/spirituality |
| Life satisfaction |
| Reality testing ability |
| Positive coping skills |
| Positive problem-solving skills |
| Positive social support and bonding |
| Positive therapeutic relationships |
| Easy access to support for help seeking |
Table 4.
Warning signs of suicide[7]
| Verbal |
| No reason for living; no sense of purpose in life |
| Feeling trapped-like there’s no way out |
| I am a burden on others |
| People would be better off without me |
| Behavioral |
| Acting reckless or engaging in risky activities, seemingly without thinking |
| Increasing alcohol or drug use |
| Withdrawing from friends, family, or society |
| Tidying up affairs, making arrangements |
| Psychological |
| Anxiety, agitation, unable to sleep, or sleeping all the time |
| Dramatic changes in mood |
| Hopelessness |
| Rage, anger, seeking revenge |
| Command hallucinations |
Corroborative History- Following a suicide enquiry from the subject, corroborative history should always be sought from family members, friends, accompanying persons, treating physicians, and past medical records. This is often helpful in clarifying doubts, getting a more definite picture, especially when there is a discrepancy between the patient’s expressed intent and his acts. This also helps in building a support network which is essential in planning management.
RISK ASSESSMENT IN VARIOUS SETTINGS
Emergency Department-Many a times, a psychiatrist is asked to assess risk in general emergency settings where patients present with suicide attempts. In such situations, one is often faced with a crowded, noisy setting, an unfamiliar, uncooperative, or intoxicated patient. It is difficult to carry out assessment in such situations, and the clinician needs to wait till the situation becomes favorable or conducive to assessment. Sometimes the patient may become drowsy from the effects of intoxication and medical management and stabilization of the patient becomes a priority. A scheme for risk assessment in emergency settings is outlined in Figure 2.[8,9]
Figure 2.
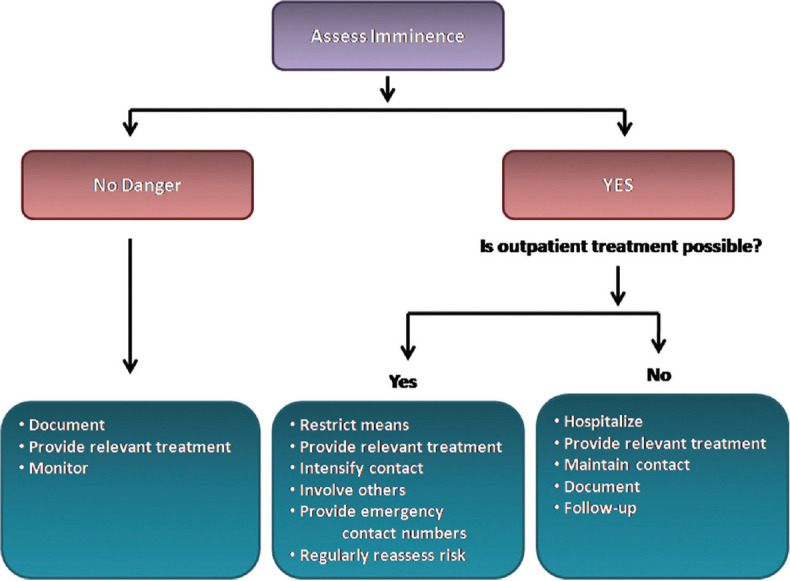
Outlines a simple scheme for managing suicidal behavior in an emergency setting[8,9]
Inpatient Setting- All patients admitted with severe mental illness and substance abuse should undergo risk assessment. Repeat assessments should be done whenever there is a change in treatment settings, worsening of the clinical condition of the patient or there is appearance of a new psychosocial stressor. Since the period immediately after discharge confers high risk of suicide, early follow-up assessments with risk estimation should be carried out.
Observation by nursing staff and attendants in inpatient settings- Hospitalized patients having high risk for suicide should be regularly placed on observation protocols. The protocol may require continuous and close observation, or periodic checks every 15 minutes. Periodic checks should be done in an unpredictable manner at varying time intervals. Randomly varied checks make it difficult for a hospitalized patient to plan suicide. Such patients should be placed closest to the nursing station and should have a roommate or an attendant. Need for careful observation should be clearly explained to the attendant.[10] A thorough inspection of all items that could be used for self-harm must be done and also an inspection of potential ligature points in the ward. Alerting the ward staff and attendants is very essential in such cases.
Outpatient Setting- The clinician should keep in mind the fluctuating nature of suicidality over time. They should be especially cautious when the patient reports sudden, unexpected improvement in mood, or shows refusal or reluctance to adhere to treatment. Using information from close family members and associates becomes vital in such cases—both for better assessment and development of support system.
Use of Assessment tools- Though there are various standardized assessment tools including objective rating scales and self-report measures, it is advisable not to rely on a single assessment instrument for determining risk of suicide. Such instruments should never replace a thorough clinical evaluation based on the standard methods of risk assessment [Table 5].[7,11] Basic goals and techniques of management of acute suicidal crisis are enumerated in Tables 6[12] and 7, respectively. Management approach should also take note of several factors which determine the need to hospitalize [Table 8][3] or favor treatment on outpatient basis [Table 9].[3]
Table 5.
| Risk Level | Risk/Protective Factor | Suicidality | Possible Interventions |
|---|---|---|---|
| High | Psychiatric diagnoses with severe symptoms or acute precipitating event; protective factors not relevant; Substance abuse/dependence; severe depression, command hallucinations; poor support system | Potentially lethal suicide attempt or persistent ideation with strong intent or suicide rehearsal | Admission generally indicated unless a significant change reduces risk. Suicide precautions |
| Moderate | Multiple risk factors, few protective factors; moderate depression; support system inconsistent | Suicidal ideation with plan, but no intent or behavior. Preparatory acts are usually absent | Admission may be necessary depending on risk factors. Develop crisis plan including safety planning. Give emergency/crisis numbers |
| Low | Modifiable risk factors, strong protective factors; good support system | Thoughts of death, no plan, intent, or behavior | Outpatient referral, symptom reduction. Give emergency/crisis numbers |
Table 8.
Factors determining the decision to hospitalize[3]
| Strongly consider hospitalization under the following situations: |
| 1. Prior attempt of high lethality |
| 2. Well-thought-out plan |
| 3. Access to lethal means |
| 4. Uncommunicative |
| 5. Recent major loss |
| 6. Social isolation |
| 7. Hopelessness |
| 8. History of impulsive, high-risk behavior |
| 9. Active substance abuse or dependence |
| 10. Untreated mood, psychotic, or personality disorder |
| After a suicide attempt or aborted suicide attempt if: |
| 1. Patient is psychotic |
| 2. Attempt was violent, near-lethal, or premeditated |
| 3. Precautions were taken to avoid rescue or discovery |
| 4. Persistent plan and/or intent is present |
| 5. Distress is increased or patient regrets surviving |
| 6. Patient is male, older than age 45 years, especially with new onset of psychiatric illness or suicidal thinking |
| 7. Patient has limited family and/or social support |
| 8. Current impulsive behavior, severe agitation, poor judgment, or refusal of help is evident |
| 9. Patient has change in mental status with a metabolic, toxic, infectious, or other etiology requiring further workup in a structured setting |
| In the presence of suicidal ideation with: |
| 1. Specific plan with high lethality |
| 2. High suicidal intent |
Table 9.
Factors favoring discharge from ER/Outpatient management[3]
| Release from emergency department with follow-up recommendations may be possible: |
| After a suicide attempt or in the presence of suicidal ideation/plan when: Suicidality is a reaction to precipitating events (e.g., exam failure, relationship difficulties), particularly if the patient’s view of situation has changed since coming to emergency department |
| Plan/method and intent have low lethality |
| Patient has stable and supportive living situation |
| Patient is able to cooperate with recommendations for follow-up, with treater contacted, if possible, if patient is currently in treatment |
| Outpatient management may be considered under the following situations: |
| No history of potentially lethal attempts |
| Lack of plan/intent; cooperative family member or other adults |
| Removal or lack of availability of lethal means |
| Communicative |
| Availability of intensive outpatient care |
| Good social support |
| Hopefulness |
| Patient has chronic suicidal ideation and/or self-injury without prior medically serious attempts, if a safe and supportive living situation is available and outpatient psychiatric care is ongoing |
Table 6.
Managing a patient with acute suicidal behavior[12]
| The basic goals in management are the following |
| Ensure immediate safety of the patient |
| Stabilize/manage medical complications if any |
| Protect the patient from self-harm |
| Effect immediate change |
| Shift focus from crisis to resolution |
| Detect and solve, as far as possible, the acute problem that precipitated the crisis |
| Involve family, partner, social support network |
| Diagnose and treat the underlying problem that predisposed the patient to suicidal behavior. |
Table 7.
Techniques of management of acute suicidal crisis
| Remove the means (agent) |
| Safety planning |
| Planning for the future (immediate) |
| Decrease isolation (social support) |
| Decrease high-risk behavioral factors |
| Decrease high-risk environmental factors |
| Decrease anxiety and agitation (psychological perturbation) |
| Medication management |
| Consider hospitalization (if required) |
EMERGENCY NON-PHARMACOLOGICAL MEASURES
Safety Plan Intervention (SPI)- It is one of the most popular and well-recommended measures to deal with acute suicidal crisis. It is a brief cognitive intervention typically lasting 20–45 minutes which provides the suicidal patient with a specified and prioritized set of coping strategies and sources of support which may be used if suicidal thoughts emerge suddenly [Table 10].[13] A safety plan is best developed in collaboration with the patient. Assistance of family members/close contacts may be sought if required. The Government of India has launched a nationwide 24-hour tele-mental health service which will also double-up as a suicide helpline and is available in many regional languages. The numbers are 14416 and 1-800-91-4416 and may be provided to patients.
Table 10.
Steps of a typical safety plan[13]
| Identifying warning signs of suicide- “Intense agitation and anxiety” |
| “Severe mood fluctuations” |
| Internal coping strategies- Things that I can do to distract myself without |
| contacting anyone-“Watching sports”, “listening to music” |
| Socialization strategies for distraction and support-Socializing with other people in their natural social environment (friends, neighbors) or visiting healthy social settings (library, coffee shop) |
| Social contacts for help in resolving the suicide crisis (close friends, family members) |
| Professional and agency contacts to help resolve a crisis (local hospital, suicide helpline) |
| Restricting the available means in the nearby environment (home, hostel) |
No-suicide Contract- This is a verbal or written agreement between the patient and the clinician which requests the patient from engaging in suicidal behavior in case of sudden crisis. Suicide contracts as effective methods of reducing suicide have limited evidence. Moreover, it is based on “subjective belief” and may lead to a false sense of security on the part of the clinician. Hence, it is not routinely recommended and should not be used in psychotic, agitated, impulsive, intoxicated, and those with cognitive deficits.[3]
Activating Psychosocial Support-In consultation with the suicidal patient, psychosocial support may be activated by reaching out to family or friends and community resources, and provide details of community services including crisis lines. The main methods of activating psychosocial support are: a. attending to existing relationships, b. building new relationships, c. modifying reactions toward others, d. utilizing family support.
Psychotherapy- Cognitive behavior therapy-based interventions focused on suicide prevention have been found effective in patients with suicidal behavior. Dialectical behavior therapy, wherever available, should be offered to patients with borderline personality disorder and history of recent self-directed violence. Problem-solving therapy has also been found to be effective in reducing suicidal behavior.[9]
EMERGENCY SOMATIC TREATMENTS
Electroconvulsive therapy (ECT)- ECT reduces suicidal behavior in the short term. Its efficacy has been established in acutely suicidal patients, especially those suffering from unipolar depressive disorder.[14,15]
Lithium- Lithium has established efficacy in reducing suicidality in patients with bipolar disorder and major depressive disorder. However, the immediate risk of overdosage with lithium in an actively suicidal patient has to be kept in mind. Steps like prescription of very short duration, supervised medications, and keeping medicines under lock (wherever feasible) should be discussed.[16]
Antidepressants- Antidepressant treatment is generally recommended in treatment of suicidal behavior in cases with unipolar depression. The efficacy of fluoxetine and venlafaxine has been proved in reducing depression and suicidality in adult and geriatric population. There are concerns of antidepressant-induced suicidality for which the treating team must psycho-educate the patient and the family members wherever applicable. Particular attention to this aspect must be paid during treatment for the first one month, especially among adolescents.[17]
Ketamine- Studies have shown that ketamine is effective in rapidly reducing suicidal ideation, even with a single dose of 0.5 mg/kg. Ketamine is usually administered as an iv infusion. Though the Va/DOD Clinical Practice Guidelines[16] recommend its use, the major issue concerning ketamine is that the benefits have been found to be short term and the trials have been carried out on small patient groups. Hence, the use of ketamine infusion in suicidal behavior still remains off-label.[18] Ketamine is a controlled substance which is used as an intravenous or intramuscular injection solution for induction and maintenance of general anesthesia. Ketamine needs to be used with caution due to associated side effects related to hemodynamic stability, emergent reactions like vivid dreams, hallucinations, respiratory depression, and drug-induced liver injury, among others. The intranasal preparation, esketamine, has been approved by the Food and Drug Administration (FDA) in August, 2020, to “treat depressive symptoms in adults with major depressive disorder with acute suicidal ideation and behavior.” Potential risks associated with esketamine include sedation, dissociation, and abuse or misuse, and in the USA, its use is subject to strict safety controls on dispensing and administration. It has to be dispensed and administered only in certified healthcare settings, and patients must be monitored inside the healthcare setting after administration for a minimum of two hours until patients are safe[19]
Clozapine – Clozapine has been found to reduce suicides and suicide attempts in patients with schizophrenia and may be considered in this group of patients.[20]
Measures to control acute anxiety and agitation- These measures are often indicated in controlling severe agitation and anxiety in actively suicidal patients and can be useful in the immediate management. Injectable antipsychotics and benzodiazepines may be used for this purpose in the emergency treatment setting. Benzodiazepines are sometimes used for treating severe anxiety associated with suicidality. We lack adequate evidence to support this recommendation. Moreover, benzodiazepines can frequently be used as means of suicide and can also cause disinhibition in some patients. However, these drugs may be effective in treating severe insomnia associated with suicidality.[19]
LONG-TERM MANAGEMENT OF SUICIDAL BEHAVIOR
Brief Interventions and follow-up
The World Health Organization (WHO) Brief Intervention and Contact (BIC) treatment modality consists of a one-hour individual information session as close to the time of discharge as possible and, after discharge, nine follow-up contacts (phone calls or visits, as appropriate) according to a specific time-line up to 18 months (at 1, 2, 4, 7, and 11 week(s), and 4, 6, 12, and 18 months), conducted by a person with clinical experience (e.g., doctor, nurse, and psychologist). The information relates to psychological and social distress that often underlies suicidal behavior, risk, and protective factors for suicidal behaviors, basic community-specific epidemiology of suicide, repetition of suicidal behaviors, alternatives for constructive instead of self-destructive coping strategies, and contacts/referral options. WHO BIC has been found to significantly decrease suicides among patients with a history of suicide attempt in low- to middle-income countries (e.g., China, Iran, India, Brazil, and Sri Lanka).[21] This could be an effective model of post-discharge aftercare in individuals admitted for suicidal behavior in addition to the usual treatment modality.[19]
Management of Chronic Suicidal Behavior- Individuals with high chronic risk are those individuals having chronic disabling medical/psychiatric condition with chronic suicidal ideation. They are at a high risk of becoming suicidal in the event of sudden unexpected crisis. Apart from treatment of the chronic condition, these individuals should have a properly designed safety plan in place and undergo regular risk assessments on follow-up visits. Individuals with moderate chronic risk have a similar profile except for a stronger support system and coping reserves. They should be managed on similar lines.[3]
MEDICOLEGAL ASPECTS OF SUICIDE
According to Section 309, Indian Penal Code, whoever attempts to commit suicide and does any act toward commission of such an offence shall be punished with simple imprisonment for a term which may extend to one year (or with fine, or with both). This has been criticized as a regressive legislation. Attempt to die by suicide is discussed in Section 115 of MHCA 2017.[21] Part 1 of the section states that “Notwithstanding anything contained in Section 309 of the IPC, any person who attempts to die by suicide shall be presumed, unless proved otherwise, to have severe stress and shall not be tried and punished under the said Code.” It has an “overriding” effect on Section 309, IPC. Part 2 of the section states that “the appropriate government shall have the duty to provide care, treatment and rehabilitation to a person who has attempted suicide.” Thus, following implementation of MHCA, Section 309 IPC has become redundant in that people who attempt suicide can’t be punished. However, the reporting may need to be done as per local state government rules.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders:DSM 5. 5th ed. Arlington, VA: American Psychiatric Association; 2013. [Google Scholar]
- 2.Silverman MM, Berman AL, Sanddal ND, O’carroll PW, Joiner TE. Rebuilding the tower of Babel:A revised nomenclature for the study of suicide and suicidal behaviors. Part 2:Suicide-related ideations, communications, and behaviors. Suicide Life Threat Behav. 2007;37:264–77. doi: 10.1521/suli.2007.37.3.264. [DOI] [PubMed] [Google Scholar]
- 3.Jacobs DG, Baldessarini RS, Conwell Y, Fawcett JA, Horton L, Meltzer H, et al. Practice Guideline for the Assessment and Treatment of Patients with Suicidal Behaviors. American Psychiatric Association. 2003 [Google Scholar]
- 4.Posner K, Brodsky B, Yershova K, Buchanan J, Mann J. Nock MK, editor. The classification of suicidal behavior. The Oxford Handbook of Suicide and Self-Injury. Oxford Library of Psychology (2014 online edn, Oxford Academic, 1 July 2014) [Last accessed on 2022 Sep 15]. Available from:https://doi.org/10.1093/oxfordhb/97801953885650.001.0001 .
- 5.WHO. Global Health Estimates 2019: Deaths by cause, age, sex, by country and by region, 2000–2019. 2020 [Google Scholar]
- 6.National Crime Record Bureau. Accidental Deaths and Suicide in India. New Delhi: Government of India; 2020. [Google Scholar]
- 7.Rudd MD, Berman AL, Joiner TE, Jr, Nock MK, Silverman MM, Mandrusiak M, et al. Warning signs for suicide:Theory, research, and clinical applications. Suicide Life Threat Behav. 2006;36:255–62. doi: 10.1521/suli.2006.36.3.255. [DOI] [PubMed] [Google Scholar]
- 8.Buzan RD, Weissberg MP. Suicide: Risk factors and therapeutic considerations in the emergency department. J Emerg Med. 1992;10:335–43. doi: 10.1016/0736-4679(92)90340-y. [DOI] [PubMed] [Google Scholar]
- 9.Vijayakumar L, Vijayakumar V. Emergency management of suicidal behavior. In: Thara R, Vijayakumar L, editors. Emergencies in Psychiatry in Low and Middle Income Countries. Routledge; 2017. [Google Scholar]
- 10.Shindhe SS, Nagarajaiah, Reddemma K, Suresh BM, Sindhe S. Prevention of inpatient suicide, saving lives:Preventing avoidable deaths in hospital. Ind J Psy Nursing. 2013;5:53–5. [Google Scholar]
- 11.Substance Abuse and Mental Health Services Administration. Suicide Assessment Five-step Evaluation and Triage for clinicians (SAFE-T) Available from:https://store.samhsa.gov/product/SAFE-T-Pocket-Card-Suicide-Assessment-Five-Step-Evaluation-and-Triage-for-Clinicians/sma09-4432 .
- 12.Framework for Suicide Risk Assessment and Management for NSW Health Staff. Available from:www.health.nsw.gov.au .
- 13.Stanley B, Brown GK. Safety planning intervention:A brief intervention to mitigate suicide risk. Cogn Behav Pract. 2012;19:256–64. [Google Scholar]
- 14.Fink M, Kellner CH, McCall WV. The role of ECT in suicide prevention. J ECT. 2014;30:5–9. doi: 10.1097/YCT.0b013e3182a6ad0d. [DOI] [PubMed] [Google Scholar]
- 15.Department of Veteran Affairs, Department of Defence. VA/DODClinical practice guideline for the assessment and management of patients at risk for suicide. 2019. Available from:https://www.healthquality.va.gov/guidelines/mh/srb/
- 16.Li K, Zhou G, Xiao Y, Gu J, Chen Q, Xie S, et al. Risk of suicidal behaviors and antidepressant exposure among children and adolescents:A meta-analysis of observational studies. Front Psychiatry. 2022;13:880496. doi: 10.3389/fpsyt.2022.880496. doi:10.3389/fpsyt. 2022.880496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Schaffer A, Isometsä ET, Tondo L, Moreno DH, Sinyor M, Kessing LV, et al. Epidemiology, neurobiology and pharmacological interventions related to suicide deaths and suicide attempts in bipolar disorder:Part I of a report of the International Society for Bipolar Disorders Task Force on Suicide in Bipolar Disorder. Aust N Z J Psychiatry. 2015;49:785–802. doi: 10.1177/0004867415594427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Baldacara L, Grudtner RR, Leite VS, Porto DM, Robis KP, Fidalgo TM, et al. Brazilian Psychiatric Association guidelines for the management of suicidal behavior. Part 2. Screening, intervention, and prevention. Braz J Psychiatry. 2021;43:538–49. doi: 10.1590/1516-4446-2020-1108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Meltzer HY, Alphs L, Green AI, Altamura AC, Anand R, Bertoldi A, et al. Clozapine treatment for suicidality in schizophrenia International Suicide Prevention Trial (InterSePT) Arch Gen Psychiatry. 2003;60:82–91. doi: 10.1001/archpsyc.60.1.82. [DOI] [PubMed] [Google Scholar]
- 20.Vijayakumar L, Umamaheswari C, Shujaath Ali ZS, Devaraj P, Kesavan K. Intervention for suicide attempters:A randomized controlled study. Indian JPsychiatry. 2011;53:244–8. doi: 10.4103/0019-5545.86817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ministry of Law and Justice. The Mental Healthcare Act;Gazette of India. 2017. [Last accessed on 2022 Sept 22]. Available from:http://www.egazette.nic.in/


